This randomized clinical trial investigates if starting cardiac rehabilitation exercise training 2 weeks after sternotomy is as effective and safe as starting 6 weeks after sternotomy in cardiac surgery patients.
Key Points
Question
Is starting cardiac rehabilitation exercise training 2 weeks after sternotomy as effective and safe as starting 6 weeks after sternotomy?
Findings
In this assessor-blind, noninferiority, randomized clinical trial of 158 cardiac surgery patients, starting cardiac rehabilitation exercise training 2 weeks after sternotomy was as effective, and likely as safe, as starting 6 weeks after sternotomy.
Meaning
By adopting a progressive individualized approach, patients who have median sternotomy can start cardiac rehabilitation exercise training up to 4 weeks earlier than current guidance and thus potentially complete their recovery sooner.
Abstract
Importance
Guidelines recommend that cardiac rehabilitation (CR) exercise training should not start until 6 weeks after sternotomy, although this is not evidence based. Limited data suggest that starting earlier is not detrimental, but clinical trials are needed.
Objective
To compare the effectiveness and safety of CR exercise training started either 2 weeks (early CR) or 6 weeks (usual-care CR) after sternotomy.
Design, Setting, and Participants
This was an assessor-blind, noninferiority, parallel-group, randomized clinical trial that conducted participant recruitment from June 12, 2017, to March 17, 2020. Participants were consecutive cardiac surgery sternotomy patients recruited from 2 outpatient National Health Service rehabilitation centers: University Hospital, Coventry, UK, and Hospital of St Cross, Rugby, UK.
Interventions
Participants were randomly assigned to 8 weeks of twice-weekly supervised CR exercise training starting either 2 weeks (early CR) or 6 weeks (usual-care CR) after sternotomy. Exercise training adhered to existing guidelines, including functional strength and cardiovascular components.
Main Outcomes and Measures
Outcomes were assessed at baseline (inpatient after surgery), after CR (10 or 14 weeks after sternotomy), and 12 months after randomization. The primary outcome was the change in 6-minute walk test distance from baseline to after CR. Secondary outcomes included safety, functional fitness, and quality of life.
Results
A total of 158 participants (mean [SD] age, 63 [11.5] years, 133 male patients [84.2%]) were randomly assigned to study groups; 118 patients (usual-care CR, 61 [51.7%]; early CR, 57 [48.3%]) were included in the primary analysis. Early CR was not inferior to usual-care CR (noninferiority margin, 35 m); the mean change in 6-minute walk distance from baseline to after CR was 28 m greater in the early CR group (95% CI, −11 to 66; P = .16). Mean differences for secondary outcomes were not statistically significant, indicating noninferiority of early CR. There were 46 vs 58 adverse events and 14 vs 18 serious adverse events in usual-care CR and early CR, respectively. There was no difference between the groups in the likelihood of participants having an adverse or serious adverse event.
Conclusions and Relevance
Starting exercise training from 2 weeks after sternotomy was as effective as starting 6 weeks after sternotomy for improving 6-minute walk distance. With appropriate precautions, clinicians and CR professionals can consider starting exercise training as early as 2 weeks after sternotomy.
Trial Registration
ClinicalTrials.gov Identifier: NCT03223558
Introduction
In the UK, approximately 35 000 patients annually have cardiac surgery requiring median sternotomy.1 Improvements in postoperative care and reduced complication rates have resulted in shorter length of stay, 5 to 7 days on average.2 Despite this, cardiac rehabilitation (CR) is not currently started until 6 weeks after sternotomy owing to concerns about adequate sternal healing.3 With a lack of evidence relating to activity following median sternotomy, clinical recommendations are often conflicting, arbitrary, and anecdotal, thus potentially overly restrictive. The 6-week sedentary period at home after sternotomy may be a missed opportunity for structured rehabilitation and faster recovery.
The British Association for Cardiovascular Prevention and Rehabilitation4 recommends early CR, although this is not clearly defined. A delay in starting CR is known to prolong recovery, increase dependence on family/carers, and cause frustration, particularly for those of working age.5,6 This can contribute to anxiety and depression after cardiac surgery. Furthermore, any delay can attenuate the benefits of CR7 and negatively affect compliance and adherence if the patient perceives the need for rehabilitation has passed.
Evidence from several studies suggests that overly restrictive sternal precautions may in fact contribute to poor health, particularly in the older adult population.6,8,9 Furthermore, intrathoracic pressures generated by coughing and sneezing were reported to be more excessive than most daily activities that patients are currently advised to avoid.10 Many patients rapidly lose muscle and bone mass during poststernotomy sedentary periods,11 increasing the risk of falls and prolonging recovery. Accordingly, a number of preliminary studies have demonstrated superior outcomes when beginning activity earlier after sternotomy.5,12,13,14,15
Despite advances in poststernotomy care, there are no accepted evidence-based recommendations to guide clinicians and CR professionals. This has resulted in the unsatisfactory situation of consensus opinion rather than empirical evidence guiding clinical care. To our knowledge, there are no good quality prospective trials that have assessed the effectiveness and safety of earlier initiation of CR exercise training after sternotomy for cardiac surgery.
The objective of this randomized clinical trial was to investigate the effectiveness and safety of CR exercise training started 2 weeks after sternotomy (early CR) compared with 6 weeks after sternotomy (usual-care CR). We hypothesized that early CR would be as effective and safe as usual-care CR.
Methods
Trial Design/Setting
The Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training (SCAR) study was a pragmatic, assessor-blind, noninferiority, parallel-group, randomized clinical trial, conducted in a real-world UK National Health Service outpatient CR service. The trial protocol is published in full elsewhere16 and in Supplement 1. The trial was approved by Edgbaston Research Ethics Committee and registered with ClinicalTrials.gov. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.17
Study Participants
Recruitment took place between June 12, 2017, and March 17, 2020. Patients who had coronary artery bypass graft and mitral/aortic valve replacement/repair and were recovering from median sternotomy at University Hospital, Coventry, UK, and Hospital of St Cross, Rugby, UK, were eligible. Inclusion criteria included age 18 to 90 years and the ability to provide written informed consent. Patient race and ethnicity data were not collected. Patients were excluded for the following reasons: serious compromising cardiac arrhythmias, neurologic disorders, significant comorbidities that would prevent full participation, and inability to enroll for the full duration the trial. Transport to and from the CR facility was offered to participants who had no other means of travel. Following sternotomy, patients were not permitted to drive in line with UK postsurgical Driving and Vehicle Licensing Agency restrictions.18
Randomization and Blinding
Participants were randomly assigned to early CR or usual-care CR, on a 1:1 basis, via block randomization. The random allocation sequence was generated by the trial statistician (P.K.K.) and implemented by an independent clinician. To ensure allocation concealment, randomization requests were submitted further to completion of all baseline assessments after surgery. Outcome assessors and cardiac surgeons were blind to group allocation. It was not possible for participants and CR professionals involved in the exercise training interventions to be blind to group allocation.
Interventions
Usual-Care CR
Locally produced written home exercise guidance was provided for 6 weeks preceding enrollment, recommending short bouts (5 minutes) of light-moderate–intensity walking, progressing in duration each week. Participants completed 8 weeks of twice-weekly, 1-hour, CR exercise training. In addition, a series of shoulder mobility exercises was recommended, with the advice to avoid pain and/or undue postexercise fatigue. At 6 weeks, usual-care CR adhered to UK standards (British Association for Cardiovascular Prevention and Rehabilitation/Association of Chartered Physiotherapists in Cardiac Rehabilitation).4,19 Briefly, a 15-minute warm-up with light cardiovascular and mobility exercises (<40% heart rate reserve) was followed by 20 to 40 minutes of moderate-intensity continuous cardiovascular exercise (eg, cycle ergometer, rowing ergometer, treadmill, walking track) at 40% to 70% heart rate reserve. After a 10-minute cooldown, functional muscular strength, flexibility, and proprioception exercises were undertaken (eg, resistance machines, free weights, multiplane functional exercises). Upper body exercises were performed carefully to avoid sternal and leg wound pain and complications. Exercise duration and workload were increased, as tolerated, based on heart rate and participant-reported rating of perceived exertion.
Early CR
Participants completed 8 weeks of twice-weekly, 1-hour, CR exercise training. There are no specific outpatient CR exercise prescription guidelines for patients who have undergone recent sternotomy (<6 weeks). In the first 2 to 3 weeks of early CR, participants followed an individualized exercise program dictated by their current level of fitness and postsurgery symptoms and limitations. Light shoulder and chest mobility and strength exercises were introduced when participants were able to perform them with minimal discomfort, with moderate-intensity cardiovascular interval training started in parallel. By weeks 2 to 3 of early CR, participants progressed toward achieving current UK standards as per usual-care CR.
Outcomes
Primary Outcome
Outcomes were measured at 3 time points: (1) baseline (inpatient postsurgery prerandomization), (2) after the 8-week CR program (approximately 10 weeks after surgery for early CR and 14 weeks after surgery for usual-care CR), and (3) 12 months after randomization.
The primary outcome was the change in 6-minute walk test (6MWT) distance from baseline to after rehabilitation. The 6MWT was conducted in accordance with guidelines.20 Participants walked, self-paced, along a 30-m walking track for 6 minutes. The primary outcome was calculated as the postrehabilitation measurement minus the baseline measurement so that a positive value corresponded to an improvement and a negative value to a deterioration.
Secondary Outcomes
To assess functional lower extremity muscular strength and power, the 5 Times Sit-to-Stand (5T-STS) Test was performed.21 Leg strength was further evaluated with isometric dynamometry using the PCE FB1k dynamometer (PCE Instruments); the force generated during a resisted leg extension was measured for both limbs, and the highest value was recorded.22 Digital handheld dynamometry using JAMAR Plus (Performance International Limited) was undertaken to measure hand grip strength in both limbs, adhering to the American Society of Hand Therapists recommendations.23 Participants were instructed to perform a maximal grip contraction for 2 to 5 seconds; the highest of 3 attempts was recorded.
Anxiety and depression were measured with the 7-item Generalized Anxiety Disorder (GAD-7) and 9-item Patient Health Questionnaire (PHQ-9), respectively.24 The Short-Form Survey (SF-12) was used to evaluate health-related quality of life, providing values for mental, physical, and total health.25
Compliance and adherence were evaluated by recording the number of CR sessions completed and reasons for dropout. To assess the safety of early CR, adverse and serious adverse events were defined a priori and monitored in line with the international principles of Good Clinical Practice.26 By convention, serious adverse events were recorded from randomization and classified as any untoward medical occurrence that resulted in death, was immediately life-threatening, required hospitalization or prolongation of existing hospitalization, or resulted in persistent or significant disability or incapacity.26
Sample Size
As described elsewhere,16 to achieve 90% power, 60 participants were required in each trial group to assess the noninferiority of early CR compared with usual-care CR, based on the mean difference of 6MWT changes from baseline to after rehabilitation (primary outcome). The noninferiority margin was 35 m, and the mean 6MWT changes for early and usual-care CR were assumed equal. Based on existing data,27 a common SD of 65 m was assumed. A target sample size of 140 participants (70 in each arm) was required to allow for 15% dropout. During the study, dropout rate was higher than expected (22% for early CR and 29% for usual-care CR); therefore, the sample size was revised to 170 participants. The trial was not powered to confirm the noninferiority of secondary outcomes.
Statistical Analysis
Statistical analyses were performed in R (R Foundation).28 To compare categorical baseline characteristics for early CR and usual-care CR, counts, percentages, and χ2 tests were used. Mean (SD), median (IQR), and Mann-Whitney U tests were used to compare baseline ordinal and continuous characteristics.
A t test (primary analysis) was used to compare mean 6MWT changes after rehabilitation with baseline measures (primary outcome) for early CR and usual-care CR. The 95% CI from the analysis was used to determine if early CR was noninferior to usual-care CR.27 Similarly, for each secondary outcome, a t test was used to compare the mean changes for early CR and usual-care CR. Noninferiority margins were not prespecified for secondary outcomes. Before using a t test, normality of outcome values in usual-care CR and early CR was assessed using a Shapiro-Wilk test and histogram. A post hoc analysis of covariance model, adjusting for the baseline 6MWT distance, was fitted to compare mean 6MWT distance changes after rehabilitation with baseline measures (primary outcome) for early CR and usual-care CR. To compare adverse and serious adverse events for early CR and usual-care CR, χ2 tests were used. Two-sided P values were computed and P ≤ .05 was considered statistically significant.
Preplanned secondary analysis was to fit a linear mixed model for each outcome with measurements taken at all assessment visits. However, after noting that measurements at each assessment visit were not approximately normally distributed, multiple imputation was preferred with chained equations using the multivariate imputation by chained equations (MICE) package29 in R because both assume values are missing at random. Three deceased participants (1 in early CR; 2 in usual-care CR) were not included in multiple imputation.
Secondary outcomes were derived by calculating the change after rehabilitation from baseline. Changes were approximately normally distributed and computed so that a positive change corresponded to an improvement and a negative change to a deterioration, except for 5T-STS, GAD-7, and PHQ-9, where the reverse occurs.
Results
Participant Characteristics
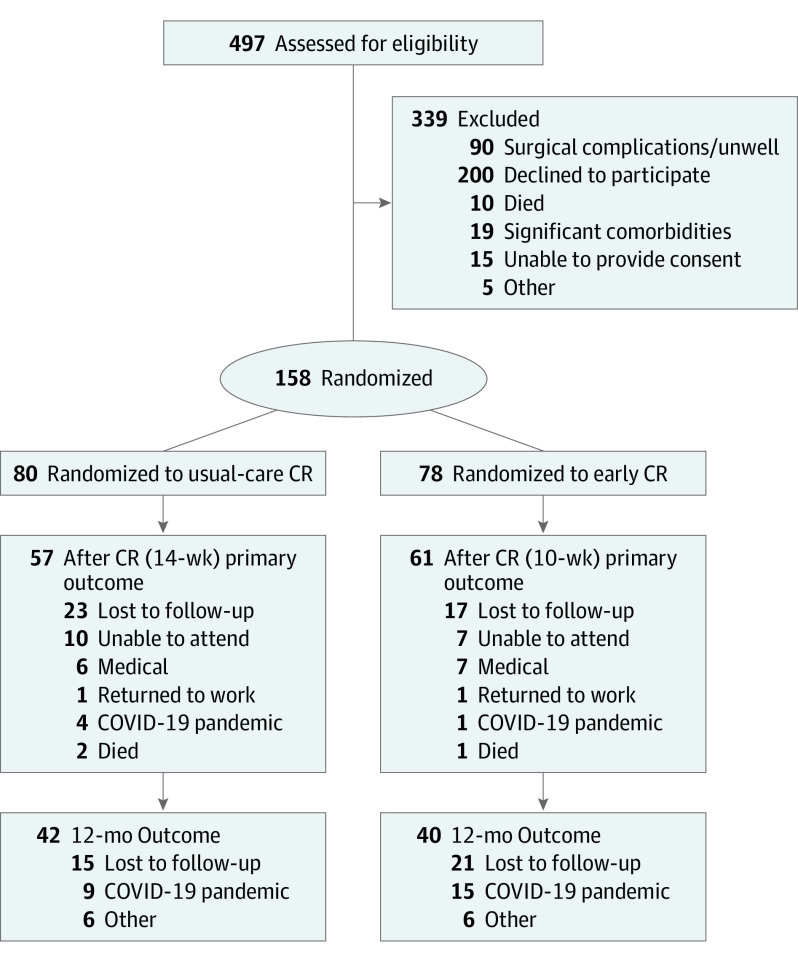
A total of 497 patients were screened and met the inclusion criteria at University Hospital Coventry and Warwickshire National Health Service trust between June 12, 2017, and January 9, 2020 (Figure 1). A total of 339 patients were excluded: 139 were ineligible owing to surgical complications, and 200 declined participation. In total, 158 participants (mean [SD] age, 63 [11.5] years, 133 male patients [84.2%]; 25 female patients [15.8%]) were randomly assigned to the intervention groups. Baseline characteristics for the usual-care CR group (80 [50.6%]) and early CR (78 [49.4%]) were balanced for demographics and comorbidities (Table 1); 118 patients (usual-care CR, 61 [51.7%]; early CR, 57 [48.3%]) were included in the primary analysis. Baseline characteristics were also similar between completers (n = 118) and participants lost to follow-up (n = 40) (eTable 1 in Supplement 2).
Figure 1. Consolidated Standards of Reporting Trials (CONSORT) Diagram.
CR indicates cardiac rehabilitation.
Table 1. Demographic and Clinical Characteristics.
| Characteristic/outcome | No. (%) | |
|---|---|---|
| Usual-care CR (n = 80) | Early CR (n = 78) | |
| Female gender | 9 (11.3) | 16 (20.5) |
| Male gender | 71 (88.8) | 62 (79.5) |
| Age at surgery, y | ||
| Mean (SD) | 64.0 (10.3) | 61.6 (12.6) |
| Median (IQR) | 66.0 (58.0-72.2) | 64.0 (56.0-70.0) |
| Body mass indexa | ||
| Mean (SD) | 28.6 (4.9) | 29.29 (5.7) |
| Median (IQR) | 27.7 (25.7-31.0) | 28.45 (25.1-32.7) |
| Surgery | ||
| Elective | 56 (70.0) | 49 (62.8) |
| Emergency | 24 (30.0) | 29 (37.2) |
| Procedure | ||
| CABG | 39 (48.7) | 32 (41.1) |
| AVR/MVR | 35 (43.8) | 39 (50) |
| CABG + AVR/MVR | 6 (7.5) | 7 (8.9) |
| Surgery to randomization, mean (SD), d | 5.39 (1.6) | 5.17 (1.6) |
| Previous CABG, yes | 1 (1.2) | 0 (0) |
| IHD, yes | 24 (30.0) | 14 (17.9) |
| Previous MI, yes | 10 (12.5) | 12 (15.4) |
| Other past conditions, yes | 13 (16.7) | 17 (21.2) |
| Hypertension, yes | 39 (48.8) | 32 (41.0) |
| Diabetes, yes | 12 (15.0) | 21 (26.9) |
| Family history, yes | 18 (22.5) | 12 (15.4) |
| HAD, yes | 3 (3.8) | 3 (3.8) |
| Smoking status | ||
| Nonsmoker | 71 (88.8) | 67 (85.9) |
| Smoker | 9 (11.2) | 11 (14.1) |
| Hypercholesterolemia, yes | 25 (31.2) | 24 (30.8) |
Abbreviations: AVR, aortic valve replacement; CABG, coronary artery bypass graft; CR, cardiac rehabilitation; HAD, Hospital Anxiety and Depression Score; IHD, ischemic heart disease; MI, myocardial infarction; MVR, mitral valve replacement.
Calculated as weight in kilograms divided by height in meters squared.
Primary Outcome
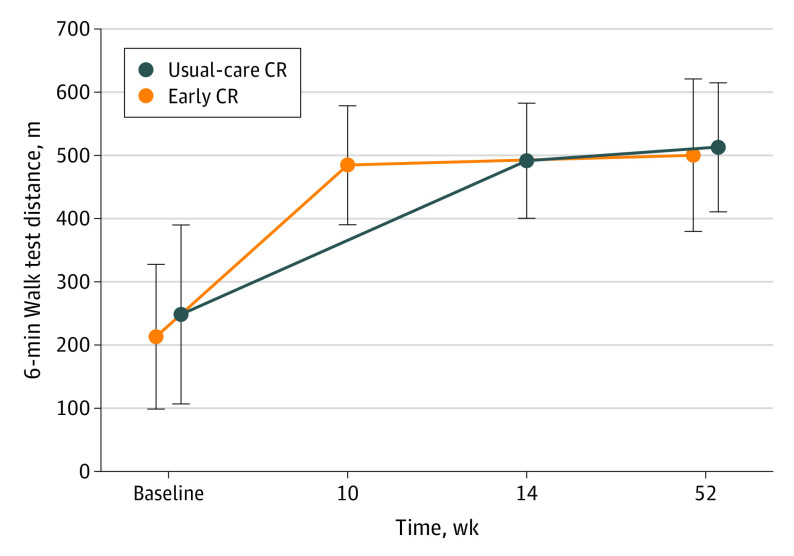
At baseline, the mean (SD) 6MWT distance for early CR (209.1 [117.6] m) was lower than that for usual-care CR (243.9 [144.2] m) (Figure 2). After rehabilitation, the mean 6MWT distance for early CR was similar to that of usual-care CR, showing a greater increase in 6MWT distance for early CR than for usual-care CR (275.0 [148.5] m vs 247.5 [146.6] m, respectively). Early CR was not inferior to usual-care CR (noninferiority margin, 35 m; difference in mean change for 6MWT, 28 m; 95% CI, −11 to 66; P = .16) (Figure 2, Table 2) and the improvement with early CR was achieved 4 weeks earlier in the recovery timeline. Post hoc analysis of covariance confirmed these findings (adjusted difference in mean change for 6MWT distance, 8 m; 95% CI, −20 to 36; P = .58).
Figure 2. Primary Outcome: Change in 6-Minute Walk Test Distance From Baseline to After Rehabilitation and 12 Months of Follow-up.
CR indicates cardiac rehabilitation.
Table 2. Summary of Results Comparing Changes From Baseline to After Rehabilitation.
| Outcome | Complete case analysis | Multiple imputation, difference in changes (early CR − usual-care CR)a | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Mean (SD) | Difference (early CR − usual-care CR) in changesa | Mean (95% CI) | P value | ||||||
| UCR | ECR | Usual-care CR | Early CR | Mean (95% CI) | P value | |||||
| Baseline | After CR | Baseline | After CR | |||||||
| 6MWT, m | 57 | 61 | 243.9 (144.2) | 491.4 (92.9)b | 209.1 (117.6) | 484.1 (95.9)b | 27.5 (−11.2 to 66.2) | .16 | 27.7 (−9.9 to 65.3) | .15 |
| 5T-STS | 55 | 58 | 19.27 (10.26) | 9.33 (2.45)b | 18.42 (9.50) | 9.07 (2.45)b | −0.58 (−3.84 to 2.67) | .72 | −0.57 (−3.56 to 2.42) | .71 |
| Leg strength, kg | 48 | 52 | 32.04 (13.17) | 37.26 (13.89)b | 33.72 (11.51) | 40.92 (13.71)b | 1.97 (−1.90 to 5.84) | .32 | 1.12 (−2.62 to 4.87) | .55 |
| Grip strength, kg | 56 | 59 | 32.48 (9.01) | 36.42 (9.27)b | 32.17 (8.93) | 35.01 (10.14)b | −1.10 (−3.16 to 0.96) | .29 | −0.98 (−3.02 to 1.07) | .35 |
| GAD-7 | 44 | 55 | 5.18 (5.24) | 1.55 (3.34)b | 5.95 (5.47) | 1.35 (2.23)b | 0.96 (−0.99 to 2.92) | .33 | 1.00 (−0.81 to 2.81) | .28 |
| PHQ-9 | 54 | 61 | 7.87 (5.64) | 2.22 (3.00)b | 8.39 (5.78) | 2.44 (3.05)b | 0.30 (−1.86 to 2.47) | .78 | 0.70 (−1.30 to 2.70) | .49 |
| SF-12 | ||||||||||
| Physical | 37 | 47 | 12.03 (3.08) | 16.38 (2.28)b | 11.51 (3.03) | 15.53 (2.39)b | −0.33 (−1.66 to 1.00) | .62 | −0.71 (−1.88 to 0.46) | .24 |
| Mental | 37 | 47 | 19.00 (4.55) | 22.30 (3.74)b | 17.74 (3.93) | 22.57 (3.00)b | 1.53 (−0.24 to 3.30) | .09 | 0.65 (−0.95 to 2.26) | .43 |
| SF-12 total | 37 | 47 | 31.03 (7.01) | 38.84 (5.26)b | 29.47 (6.28) | 38.09 (4.47)b | 0.81 (−1.84 to 3.46) | .55 | −0.39 (−2.73 to 1.95) | .75 |
Abbreviations: 5T-STS, 5 Times Sit-to-Stand Test; 6MWT, 6-minute walk test; CR, cardiac rehabilitation; ECR, early CR; GAD-7, Generalized Anxiety Disorder questionnaire; PHQ-9, Patient Health Questionnaire; SF-12, 12-Item Short-Form Survey; UCR, usual-care CR.
Positive and negative differences favor early CR and usual-care CR, respectively.
Improvement.
Secondary Outcomes
For both early CR and usual-care CR, there were improvements in all secondary outcomes from baseline to after rehabilitation (Table 2). Mean differences between groups for all secondary outcomes were not statistically significant, indicating the noninferiority of early CR. For leg strength, GAD-7, PHQ-9, and SF-12 mental and total, mean improvements for early CR were greater than those for usual-care CR (leg strength, 70.61 N vs 51.19 N; GAD-7, −4.6 vs −3.63; PHQ-9, −5.95 vs −5.65; SF-12 total, 8.62 vs 7.81; SF-12 mental, 4.83 vs 3.3), whereas for 5T-STS, grip strength, and SF-12 physical, mean improvements for usual-care CR were greater than those for early CR (5T-STS, 9.94 vs 9.35 seconds; grip strength, 42.95 N vs 27.85 N; SF-12 physical, 4.35 vs 4.02 points).
The COVID-19 pandemic substantially impeded collection of 12-month follow-up data. For all outcomes, complete case analysis of changes at 12 months from baseline did not show statistically significant differences between early CR and usual-care CR (eTable 2 in Supplement 2).
Adherence and Safety
Fifty-six of 83 participants (67.5%) in usual-care CR, and 58 of 78 participants (74.3%) in early CR completed at least 80% (13 of 16) of scheduled sessions. The mean (SD) number of sessions completed was 11 (5.6) in usual-care CR and 11 (5.4) in early CR. Reasons for dropout between randomization and the primary outcome time point for usual-care CR and early CR included returned to work (usual-care CR, 1 of 23 [4.3%]; early CR, 1 of 17 [5.9%]), medical (usual-care CR, 6 of 23 [26.1%]; early CR, 7 of 17 [41.2%]), unable to attend (usual-care CR, 10 of 23 [43.5%]; early CR, 7 of 17 [41.2%]), died (usual-care CR, 2 of 23 [8.7%]; early CR, 1 of 17 [5.9%]), and COVID-19 pandemic (usual-care CR, 4 of 23 [17.4%]; early CR, 1 of 17 [5.9%]).
There were 46 adverse events in usual-care CR and 58 in early CR (Table 3). Further, there were 14 serious adverse events in usual-care CR and 18 in early CR There was no difference between usual-care CR and early CR, in the likelihood of participants having at least 1 adverse event or serious adverse event (eTable 3 in Supplement 2). There were 4 sternal wound complications in early CR compared with only 1 in usual-care CR; however, all instances were identified and resolved before the commencement of exercise training.
Table 3. Adverse Events.
| Events | No. (%) | |
|---|---|---|
| Usual-care CR (n = 80) | Early CR (n = 78) | |
| Serious adverse events | ||
| Total | 14 (17.5) | 18 (23.1) |
| Death | 2 (2.5) | 1 (1.3) |
| Sternal instability | 1 (1.3) | 4 (5.1) |
| Sternal wound infection | 1 (1.3) | 0 (0) |
| Musculoskeletal pain | 1 (1.3) | 2 (2.6) |
| Transient ischemic attack | 1 (1.3) | 2 (2.6) |
| LRTI | 3 (3.8) | 2 (2.6) |
| Fluid overload | 2 (2.5) | 0 (0) |
| Anemia | 1 (1.3) | 1 (1.3) |
| Atrial fibrillation | 2 (2.5) | 1 (1.3) |
| Endocarditis | 0 (0) | 1 (1.3) |
| Acute kidney injury | 0 (0) | 1 (1.3) |
| Pulmonary embolism | 0 (0) | 1 (1.3) |
| Road traffic accident | 0 (0) | 1 (1.3) |
| Eye casualty | 0 (0) | 1 (1.3) |
| Adverse events | ||
| Total | 46 (57.5) | 58 (74.4) |
| Arrythmia | 14 (17.5) | 10 (12.8) |
| Superficial wound infection | 8 (10.0) | 10 (12.8) |
| LRTI | 4 (5.0) | 9 (11.5) |
| Pleural effusion | 5 (6.3) | 0 (0) |
| Excessive dyspnea | 1 (1.3) | 8 10.3) |
| Presyncope | 2 (2.5) | 2 (2.6) |
| Musculoskeletal pain | 3 (3.8) | 5 (6.4) |
| Fluid retention | 1 (1.3) | 2 (2.6) |
| Vertigo | 0 (0) | 1 (1.3) |
| Urinary tract infection | 2 (2.5) | 1 (1.3) |
| Hypertension >180/100 mm Hg | 1 (1.3) | 1 (1.3) |
| Hematuria | 1 (1.3) | 3 (3.8) |
| Leg wound bleed | 0 (0) | 1 (1.3) |
| Constipation | 0 (0) | 1 (1.3) |
| Osteoarthritis | 0 (0) | 1 (1.3) |
| Perirectal bleed | 0 (0) | 1 (1.3) |
| Deep venous thrombosis | 1 (1.3) | 0 (0) |
| Panic attack | 1 (1.3) | 0 (0) |
| Diarrhea | 0 (0) | 1 (1.3) |
| Cellulitis | 0 (0) | 1 (1.3) |
| Epilepsy | 1 (1.3) | 0 (0) |
Abbreviations: CR, cardiac rehabilitation; LRTI, lower respiratory tract infection.
Discussion
In this randomized clinical trial, starting CR exercise training as early as 2 weeks after sternotomy (early CR) was as effective as starting 6 weeks after sternotomy (usual-care CR). Effectiveness was demonstrated primarily by there being no difference between the 2 trial groups in the change in 6MWT distance from baseline to after rehabilitation. Importantly, the early CR group achieved the same improvement as the usual-care CR group up to 4 weeks earlier in their recovery. The safety of early CR, although not proven definitely, was underscored by there being no difference between the 2 trial groups in the likelihood of participants experiencing adverse or serious adverse events. Existing guidelines based on consensus opinion recommend abstinence from CR exercise training for 6 weeks after sternotomy. Data from the current trial lend support to starting as early as 2 weeks after sternotomy.
To our knowledge, the present study is the first prospective trial to test the effectiveness and safety of early initiation of poststernotomy CR. Our findings support previous observational studies.5,10,12,30 By starting as early as 2 weeks after sternotomy, the noninferiority design of our trial enabled us to assess if these previously reported benefits could be safely achieved up to 4 weeks earlier than current usual-care clinical practice. Gaining the physical and psychosocial benefits of rehabilitation up to 4 weeks earlier at no additional risk to recovery has significant implications for patients undergoing median sternotomy. Social function and economic productivity can be restored more quickly, leading to a substantial positive effect on quality of life.6 In addition, clinicians can now advocate earlier rehabilitation based on empirical evidence rather than consensus opinion. Providing a progressive individualized approach is taken, rehabilitation professionals can now feel assured in removing many of the unhelpful restrictions that may have previously hindered patients’ recovery.
In addition to the noninferiority of early CR in 6MWT distance, our trial also demonstrated equal improvement in all other clinical, physical, and quality of life outcomes. These findings indicate the holistic benefit of early CR. Further, long-term recovery was consistent between trial groups; over 12 months, 6MWT distance improved equally in both groups. It should be noted that our sample size at 12 months was affected considerably by the COVID-19 pandemic, preventing long-term follow-up in 35 participants.
Our findings confirm previous reports highlighting the potential benefits of relaxing restrictive sternal precautions postoperatively. The “Keep Your Move in the Tube” sternal guidance5 has been shown to improve outcomes,15,30,31 and a recent review concluded that controlled upper body activity, individualized progressive functional activity, and less restrictive precautions promoted better recovery.12 Despite these findings, many guidelines remain restrictive. Data from the current trial can inform new guidelines.
Although we have shown that sternotomy patients can participate in earlier CR, work is required to reassure patients that this is beneficial and safe. Of the 497 patients screened, 200 (40%) did not wish to take part. This low uptake could relate to fear of harm with earlier CR as well as disinterest in research during life-changing circumstances. Patients’ beliefs are directly influenced by the health care advice they receive.32 Therefore, dissemination of the lack of evidence supporting restrictive precautions in this population, to all surgical and health care professionals involved in sternotomy patient care, is essential. If surgical teams inform patients at the initial preoperative consultation, that early poststernotomy CR is in their best interest, it is likely that there would be fewer objections or concerns.
There were more serious adverse events in the early CR group, however, these related to prolongation of postsurgery hospitalization before starting CR rather than resulting from participation in exercise training. Although we also recorded more adverse events with early CR, we believe this can be attributed to more regular contact with this group in the early stages of recovery resulting in more opportunity for participants to discuss minor medical complaints that may otherwise have resolved without the intervention of a health care professional.
Limitations
This was a pragmatic trial in a real-world clinical setting; thus, results are clinically relevant to poststernotomy care and CR around the world. However, although participants were recruited from a wide geographic area and completed their CR at 1 of 2 facilities, this was essentially a single-center trial. Results may not be representative of the UK as a whole, and the population was primarily male (85%); although this is indicative of the cardiac surgery population.33 A considerable proportion of 12-month data was missing owing to the COVID-19 pandemic, meaning we have lower confidence in our findings at 12 months. Nevertheless, we did achieve appropriate statistical power to confirm the effectiveness of early CR compared with usual-care CR at our postrehabilitation primary outcome time point. Although we can, to some extent, confirm the safety of early CR compared with usual-care CR, the trial was not powered specifically for safety outcomes.
Conclusions
Results of this randomized clinical trial indicate that in cardiac surgery patients undergoing median sternotomy, supervised CR exercise training started as early as 2 weeks after sternotomy was as effective as starting at 6 weeks. The physical and psychosocial benefits of CR were achieved up to 4 weeks earlier, allowing a faster return to social functioning and economic productivity. Providing a progressive, individualized approach is taken, clinicians and rehabilitation professionals can initiate exercise training as early as 2 weeks after sternotomy.
Trial Protocol
eTable 1. Demographic and Clinical Characteristics of Completers vs Lost to Follow-up
eTable 2. Summary of Results for Complete Cases Analysis Comparing Changes at 12 Months From Baseline
eTable 3. Adverse Events in Early CR and Usual-Care CR
Data Sharing Statement
References
- 1.The Society for Cardiothoracic Surgery in Great Britain & Ireland . Second National Thoracic Surgery Activity & Outcomes Report. Henley-on-Thames; 2011. [Google Scholar]
- 2.Osnabrugge RL, Speir AM, Head SJ, et al. Prediction of costs and length of stay in coronary artery bypass grafting. Ann Thorac Surg. 2014;98(4):1286-1293. doi: 10.1016/j.athoracsur.2014.05.073 [DOI] [PubMed] [Google Scholar]
- 3.Jones J, Buckley J, Furze G, Sheppard G, eds Cardiovascular Prevention and Rehabilitation in Practice. 2nd ed. Wiley Blackwell; 2020. doi: 10.1002/9781119071006 [DOI] [Google Scholar]
- 4.British Association of Cardiovascular Prevention and Rehabilitation . BACPR standards and core components for cardiovascular disease prevention and rehabilitation 2017. 3rd ed. Accessed February 14, 2022. http://www.bacpr.com/resources/6A7_BACR_Standards_and_Core_Components_2017.pdf
- 5.Adams J, Lotshaw A, Exum E, et al. An alternative approach to prescribing sternal precautions after median sternotomy, “Keep Your Move in the Tube”. Proc (Bayl Univ Med Cent). 2016;29(1):97-100. doi: 10.1080/08998280.2016.11929379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fell J, Dale V, Doherty P. Does the timing of cardiac rehabilitation impact fitness outcomes? an observational analysis. Open Heart. 2016;3(1):e000369. doi: 10.1136/openhrt-2015-000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marzolini S, Blanchard C, Alter DA, Grace SL, Oh PI. Delays in referral and enrolment are associated with mitigated benefits of cardiac rehabilitation after coronary artery bypass surgery. Circ Cardiovasc Qual Outcomes. 2015;8(6):608-620. doi: 10.1161/CIRCOUTCOMES.115.001751 [DOI] [PubMed] [Google Scholar]
- 8.Eder B, Hofmann P, von Duvillard SP, et al. Early 4-week cardiac rehabilitation exercise training in elderly patients after heart surgery. J Cardiopulm Rehabil Prev. 2010;30(2):85-92. doi: 10.1097/HCR.0b013e3181be7e32 [DOI] [PubMed] [Google Scholar]
- 9.King KM, Parry M, Southern D, Faris P, Tsuyuki RT. Women’s Recovery from Sternotomy-Extension (WREST-E) study: examining long-term pain and discomfort following sternotomy and their predictors. Heart. 2008;94(4):493-497. doi: 10.1136/hrt.2007.117606 [DOI] [PubMed] [Google Scholar]
- 10.Adams J, Schmid J, Parker RD, et al. Comparison of force exerted on the sternum during a sneeze versus during low-, moderate-, and high-intensity bench press resistance exercise with and without the valsalva maneuver in healthy volunteers. Am J Cardiol. 2014;113(6):1045-1048. doi: 10.1016/j.amjcard.2013.11.064 [DOI] [PubMed] [Google Scholar]
- 11.Wall BT, Dirks ML, van Loon LJ. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12(4):898-906. doi: 10.1016/j.arr.2013.07.003 [DOI] [PubMed] [Google Scholar]
- 12.El-Ansary D, LaPier TK, Adams J, et al. An evidence-based perspective on movement and activity following median sternotomy. Phys Ther. 2019;99(12):1587-1601. doi: 10.1093/ptj/pzz126 [DOI] [PubMed] [Google Scholar]
- 13.Pack QR, Dudycha KJ, Roschen KP, Thomas RJ, Squires RW. Safety of early enrollment into outpatient cardiac rehabilitation after open heart surgery. Am J Cardiol. 2015;115(4):548-552. doi: 10.1016/j.amjcard.2014.11.040 [DOI] [PubMed] [Google Scholar]
- 14.Mungovan SF, Singh P, Gass GC, Smart NA, Hirschhorn AD. Effect of physical activity in the first 5 days after cardiac surgery. J Rehabil Med. 2017;49(1):71-77. doi: 10.2340/16501977-2165 [DOI] [PubMed] [Google Scholar]
- 15.Katijjahbe MA, Granger CL, Denehy L, et al. Standard restrictive sternal precautions and modified sternal precautions had similar effects in people after cardiac surgery via median sternotomy (SMART Trial): a randomised trial. J Physiother. 2018;64(2):97-106. doi: 10.1016/j.jphys.2018.02.013 [DOI] [PubMed] [Google Scholar]
- 16.Ennis S, Lobley G, Worrall S, et al. Early initiation of poststernotomy cardiac rehabilitation exercise training (SCAR): study protocol for a randomised controlled trial and economic evaluation. BMJ Open. 2018;8(3):e019748. doi: 10.1136/bmjopen-2017-019748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schulz KF, Altman DG, Moher D; CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vusirikala A, Backhouse M, Schimansky S. Improving driving advice provided to cardiology patients on discharge. BMJ Open Qual. 2018;7(1):e000162. doi: 10.1136/bmjoq-2017-000162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Association of Chartered Physiotherapists in Cardiac Rehabilitation . Standards for physical activity and exercise in the cardiac population. Accessed January 14, 2022. https://www.acpicr.com/data/Page_Downloads/ACPICRStandards.pdf
- 20.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories . ATS statement: guidelines for the 6-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-117. doi: 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 21.Bohannon RW. Test-retest reliability of the 5-repetition sit-to-stand test: a systematic review of the literature involving adults. J Strength Cond Res. 2011;25(11):3205-3207. doi: 10.1519/JSC.0b013e318234e59f [DOI] [PubMed] [Google Scholar]
- 22.Hansen EM, McCartney CN, Sweeney RS, Palimenio MR, Grindstaff TL. Hand-held dynamometer positioning impacts discomfort during quadriceps strength testing: a validity and reliability study. Int J Sports Phys Ther. 2015;10(1):62-68. [PMC free article] [PubMed] [Google Scholar]
- 23.Fess E. Grip strength. In: Casanova J, ed. Clinical Assessment Recommendations. 2nd ed. American Society of Hand Therapists; 1992:41-45. [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 25.Ware J Jr, Kosinski M, Keller SDA. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-233. doi: 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 26.International Council for Harmonisation . Integrated addendum to ICH E6 (R1): guideline for good clinical practice. Accessed January 14, 2022. https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf
- 27.Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res. 2005;40(2):577-591. doi: 10.1111/j.1475-6773.2005.0l374.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rizzo ML. Statistical Computing with R. 2nd ed. CRC Press; 2019. [Google Scholar]
- 29.van Buuren S, Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 30.Gach R, Triano S, Ogola GO, et al. “Keep Your Move in the Tube” safely increases discharge home following cardiac surgery. PM R. 2021;13(12):1321-1330. doi: 10.1002/pmrj.12562 [DOI] [PubMed] [Google Scholar]
- 31.Holloway C, Pathare N, Huta J, et al. The impact of a less-restrictive poststernotomy activity protocol compared with standard sternal precautions in patients following cardiac surgery. Phys Ther. 2020;100(7):1074-1083. doi: 10.1093/ptj/pzaa067 [DOI] [PubMed] [Google Scholar]
- 32.Salenger R, Morton-Bailey V, Grant M, Gregory A, Williams JB, Engelman DT. Cardiac-enhanced recovery after surgery: a guide to team building and successful implementation. Semin Thorac Cardiovasc Surg. 2020;32(2):187-196. doi: 10.1053/j.semtcvs.2020.02.029 [DOI] [PubMed] [Google Scholar]
- 33.Koch CG, Khandwala F, Nussmeier N, Blackstone EH. Gender profiling in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;126(6):2044-2051. doi: 10.1016/S0022-5223(03)00955-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Demographic and Clinical Characteristics of Completers vs Lost to Follow-up
eTable 2. Summary of Results for Complete Cases Analysis Comparing Changes at 12 Months From Baseline
eTable 3. Adverse Events in Early CR and Usual-Care CR
Data Sharing Statement