Abstract
Background
Approximately 10% of all newborns require resuscitation at birth. Training healthcare providers in standardised formal neonatal resuscitation training (SFNRT) programmes may improve neonatal outcomes. Substantial healthcare resources are expended on SFNRT.
Objectives
To determine whether SFNRT programmes reduce neonatal mortality and morbidity, improve acquisition and retention of knowledge and skills, or change teamwork and resuscitation behaviour.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, PREMEDLINE, EMBASE, CINAHL, Web of Science and the Oxford Database of Perinatal Trials, ongoing trials and conference proceedings in April 2014 and updated in March 2015.
Selection criteria
Randomised or quasi‐randomised trials including cluster‐randomised trials, comparing a SFNRT with no SFNRT, additions to SFNRT or types of SFNRT, and reporting at least one of our specified outcomes.
Data collection and analysis
Two authors extracted data independently and performed statistical analyses including typical risk ratio (RR), risk difference (RD), mean difference (MD), and number needed to treat for an additional beneficial outcome (NNTB) or an additional harmful outcome (NNTH) (all with 95% confidence intervals (CI)). We analysed cluster‐randomised trials using the generic inverse variance and the approximate analysis methods.
Main results
We identified two community‐based and three manikin‐based trials that assessed the effect of SFNRT compared with no SFNRT. Very low quality evidence from one study suggested improvement in acquisition of knowledge (RR 5.96, 95% CI 3.60 to 9.87) and skills (RR 170, 95% CI 10.8 to 2711) and retention of knowledge (RR 3.60, 95% CI 2.43 to 5.35) and the other study suggested improvement in resuscitation and behavioural scores.
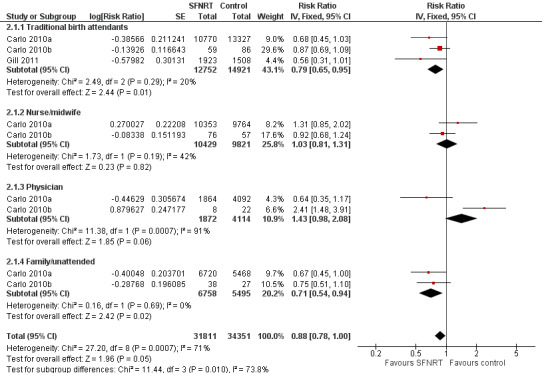
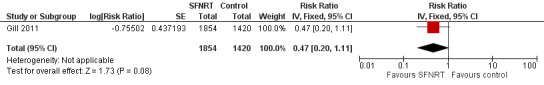
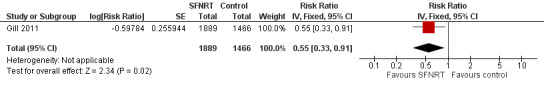
We identified three community‐based cluster‐randomised trials in developing countries comparing SFNRT with basic resuscitation training (Early Newborn Care). In this setting, there was moderate quality evidence that SFNRT decreased early neonatal mortality (typical RR 0.88, 95% CI 0.78 to 1.00; 3 studies, 66,162 neonates) and when analysed by the approximate analysis method (typical RR 0.85, 95% CI 0.75 to 0.96; RD ‐0.0044, 95% CI ‐0.0082 to ‐0.0006; NNTB 227, 95% CI 122 to 1667). Low quality evidence from one trial showed that SFNRT may decrease 28‐day mortality (typical RR 0.55, 95% CI 0.33 to 0.91) but the effect on late neonatal mortality was more uncertain (typical RR 0.47, 95% CI 0.20 to 1.11). None of our a priori defined neonatal morbidities were reported. We did not identify any randomised studies in the developed world.
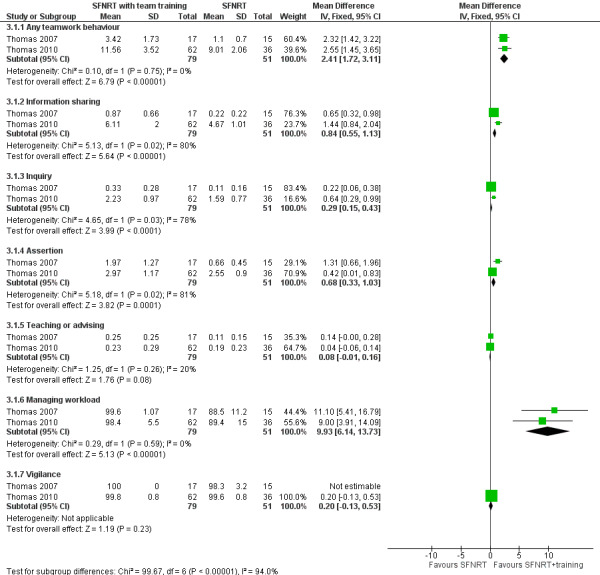
We identified two trials that compared SFNRT with team training to SFNRT. Teamwork training of physician trainees with simulation may increase any teamwork behaviour (assessed by frequency) (MD 2.41, 95% CI 1.72 to 3.11) and decrease resuscitation duration (MD ‐149.54, 95% CI ‐214.73 to ‐84.34) but may lead to little or no difference in Neonatal Resuscitation Program (NRP) scores (MD 1.40, 95% CI ‐2.02 to 4.82; 98 participants, low quality evidence).
We identified two trials that compared SFNRT with booster courses to SFNRT. It is uncertain whether booster courses improve retention of resuscitation knowledge (84 participants, very low quality evidence) but may improve procedural and behavioural skills (40 participants, very low quality evidence).
We identified two trials on decision support tools, one on a cognitive aid that did not change resuscitation scores and the other on an electronic decision support tool that improved the frequency of correct decision making on positive pressure ventilation, cardiac compressions and frequency of fraction of inspired oxygen (FiO2) adjustments (97 participants, very low quality evidence).
Authors' conclusions
SFNRT compared to basic newborn care or basic newborn resuscitation, in developing countries, results in a reduction of early neonatal and 28‐day mortality. Randomised trials of SFNRT should report on neonatal morbidity including hypoxic ischaemic encephalopathy and neurodevelopmental outcomes. Innovative educational methods that enhance knowledge and skills and teamwork behaviour should be evaluated.
Plain language summary
Newborn resuscitation training programmes for improving the health and survival of newborns
Review question: Does training healthcare providers in standardised formal neonatal resuscitation training (SFNRT) programmes reduce neonatal mortality and morbidity, improve acquisition and retention of knowledge and skills or change teamwork and resuscitation behaviour?
Background: One in 10 newborns need some resuscitation (first aid given when breathing or a heartbeat is not detected) at birth. There are many different newborn resuscitation programmes but the effectiveness of these programmes in decreasing deaths or brain injury due to lack of oxygen has not been reviewed.
Study characteristics: We searched for studies that evaluated the effectiveness of newborn resuscitation programmes in April 2014 and updated in March 2015 and found five community‐based studies (187,080 deliveries) and nine mannequin‐based studies (626 newborns).
Results and quality of the evidence: Moderate quality evidence from three studies suggested that training in newborn resuscitation probably decreases newborn deaths in the first seven days after birth. Low quality evidence from one study suggested that newborn resuscitation training may decrease newborn deaths in the first 28 days after birth. All three studies were performed in low‐income settings and their findings may have limited applicability to high‐income settings. We also found that teaching teamwork in addition to resuscitation training may improve team behaviour and decrease time for resuscitation (two studies, low quality evidence) but the effect on performance on resuscitation was uncertain. It is uncertain whether resuscitation programmes increase learners' knowledge and skills immediately and knowledge at six months because the quality of evidence was very low. Similarly, whether boosters to neonatal resuscitation help in retaining knowledge or performing resuscitation appropriately remain uncertain (the quality of evidence was very low). Also, whether visual or electronic aids for helping making decisions during resuscitation, improve resuscitation performance was uncertain (one study did not show effect but one electronic decision support tool with prompts improved resuscitation performance) (low quality evidence). We strongly encourage future studies to report outcomes related to long‐term health, such as brain injury due to lack of oxygen, fits and long‐term brain development. Effective methods to enhance teamwork behaviour, learning and retention of resuscitation knowledge and skills are needed.
Summary of findings
Background
Description of the condition
Many newborn infants require resuscitation to improve immediate postnatal adaptation. It is estimated that approximately 10% of all newborns require some assistance to begin breathing and less than 1% require extensive resuscitation (ILCOR 2006). Approximately four million newborn infants died worldwide in the neonatal period in 2000, with almost half of these deaths occurring in the first day (Lawn 2005). The vast majority of these neonatal deaths (98%) occurred in the developing world, where asphyxia accounted for approximately one‐quarter of all the deaths (Lawn 2005).
Although early neonatal depression is common, it may not be frequently predicted prior to birth. The need for resuscitation may be anticipated only in around 50% of cases (Chance 1987). Therefore, the presence of personnel adequately prepared to perform resuscitation is an important first step in newborn resuscitation. However, there can be significant variation in the presence of skilled personnel at newborn resuscitation. In South Asia and sub‐Saharan Africa, only about one‐third of women deliver in the presence of a skilled birth attendant (Knippenberg 2005). In the developed world, debate continues around the area of planned home births. One meta‐analysis found that there is a three‐fold increase in neonatal mortality in planned home deliveries. Some of this increase has been attributed to inadequate training of birth attendants in newborn resuscitation (Wax 2010).
In the past, there has been great variation in neonatal resuscitation practices, but this was addressed with the introduction of standardised, formal, neonatal resuscitation training programmes. One such programme is the NRP (Neonatal Resuscitation Program), which was introduced in 1987 in the US and is now taught in over 140 countries worldwide. There are now over 24,000 NRP instructors and over two million people trained in NRP in the US.
Description of the intervention
Numerous neonatal resuscitation programmes exist. These include the NRP, NLS (Neonatal Life Support) and ENLS (European Neonatal Life Support). In the developing world, resuscitation programmes often form one part of an overall newborn care intervention package (Narayanan 2004). The International Liaison Committee on Resuscitation (ILCOR) presents scientific statements, addresses consensus on cardiopulmonary resuscitation science statements and prepares treatment recommendations for resuscitation including the newborn infant (ILCOR 2006). These statements are frequently updated based on the most recent evidence available. Consensus has been reached on a number of key areas of newborn resuscitation. Recommendations have included the avoidance of routine intrapartum oropharyngeal or nasopharyngeal suctioning for infants with meconium‐stained amniotic fluid (Vain 2004), and avoidance of routine intratracheal suctioning of the vigorous meconium‐stained infant (Wiswell 2000). Routine suctioning of the vigorous newborn is not required (Estol 1992). The key to successful neonatal resuscitation is establishment of adequate ventilation and most newborns can be adequately ventilated with a bag and appropriate‐sized face mask (AHA 2000). There are a number of areas where insufficient evidence remains. The optimum pressure, inflation time and flow required to establish an effective functional residual capacity have not been determined. The optimum ventilation device is yet to be determined. Breakdown in teamwork and communication resulting in suboptimal resuscitation has not been addressed adequately in neonatal resuscitation programmes to date but ILCOR guidelines recommend the adoption of simulation, briefing and debriefing techniques (ILCOR 2006).
While neonatal resuscitation training programmes may differ in their content and format, they generally include knowledge‐ and skill‐based components taught over a half‐ or full‐day course. A standardised programme is defined as a training programme that addressed the following elements of newborn resuscitation: preparation for resuscitation, providing warmth and drying the baby, clearing the airway if necessary, stimulating the baby, assessing the baby's breathing and providing effective assisted ventilation if breathing was inadequate. A standardised training course need not include chest compressions, medication administration or advanced airway management such as intubation. We included all programmes irrespective of whether they offered certification or not after successfully completing the programme. We defined a formal training course as a planned teaching and learning experience in a formal setting (often an educational or work‐place environment), that follows a specified, newborn resuscitation curriculum followed by participant assessment. In the majority of newborn resuscitation programmes, participants are evaluated on their performance in a written examination (generally a multiple choice question format) followed by a skills evaluation. It is necessary to pass both written and skills evaluations to achieve provider status. The NRP recommends re‐certification every two years and the NLS every four years.
Methods of teaching include didactic sessions, skills sessions, scenarios and, more recently, the introduction of simulation‐based training. The purpose of simulation is to try to create the clinical scenario in a controlled environment that replicates the patient care environment and offers audio, visual and tactile cues to the participants.
How the intervention might work
The purpose of neonatal resuscitation education is to transfer resuscitation knowledge and skills to birth attendants and decrease neonatal mortality and morbidity. Therefore, every resuscitation education programme should be rigorously evaluated to verify that the programme is both valid and effective. Three types of studies can be examined to determine the effectiveness of resuscitation training programmes. Studies evaluating neonatal mortality and morbidity, including hypoxic ischaemic encephalopathy and long‐term neurodevelopmental follow‐up, provide the most direct evidence. Studies evaluating changes in resuscitation behaviour among birth attendants and those that evaluate acquisition and retention of knowledge and skills after resuscitation training may provide indirect evidence for the effectiveness of neonatal resuscitation programmes.
Why it is important to do this review
Substantial healthcare resources are expended on standardised formal neonatal resuscitation training (SFNRT) programmes, and thus it is important that they be proven effective. The primary objective of our review is to determine the effectiveness of standardised, formal, neonatal resuscitation training (SFNRT) programmes in reducing neonatal mortality and morbidity.
Objectives
To determine whether SFNRT programmes reduce neonatal mortality and morbidity, improve acquisition and retention of knowledge and skills, or change teamwork and resuscitation behaviour.
Methods
Criteria for considering studies for this review
Types of studies
Studies that were randomised or quasi‐randomised at the level of the individual or a cluster of individuals.
Types of participants
Healthcare professionals caring for newborn infants in a healthcare facility or home care setting; including physicians, nurses, midwives, traditional birth attendants, paramedics and respiratory therapists.
Types of interventions
Training of healthcare professionals in neonatal resuscitation using a defined programmatic approach, including, but not limited to, the NRP of the American Academy of Pediatrics. These neonatal resuscitation training programmes can be based on the following:
didactic courses (lecture, video‐based or online) only;
skills‐based courses (hands on training and interactive);
simulation based where the programme uses simulation to mimic clinical scenarios.
The essential elements of a resuscitation programme should include teaching resuscitation skills (preparation for resuscitation, providing warmth and drying the baby, clearing the airway if necessary, stimulating the baby, assessing the baby's breathing and providing effective assisted ventilation if the breathing is inadequate, but does not require the participant to perform chest compressions, administer medications or perform advanced airway management (e.g. endotracheal intubation). The programme should test the acquired knowledge and skills content by instructors who are certified with a national or international body that oversees resuscitation training. Resuscitation programmes may include content in addition to the essential elements described above (such as behavioural training or boosters), use any instructional format (e.g. didactics, simulation) and may include single or multiple sessions. Didactic courses may use lecture formats or video‐based training without a practical skills‐based approach. A skills‐based approach involves teaching in interactive sessions using mannequins or other equipment, or both. Simulation‐based programmes use simulation of real‐life scenarios using low‐fidelity or high‐fidelity mannequins or be virtual or computer based. We also included resuscitation programmes that integrate didactics, interactive components and simulation.
Planned comparisons
Any SFNRT programme versus no resuscitation training.
Any SFNRT programme versus basic newborn care that may include some resuscitation training (e.g. essential newborn care or mouth‐to‐mouth breathing).
Additions to a formal course such as SFNRT (e.g. teamwork behaviour, boosters) versus SFNRT alone.
Types of outcome measures
Primary outcomes
-
Neonatal mortality defined as death in the first 28 days after birth in neonates who were randomised including those requiring resuscitation. Subgroup categories for neonatal mortality were:
early neonatal mortality: death in the first seven days after birth;
late neonatal mortality: death between eight and 28 days after birth;
neonatal mortality in the first 28 days after birth.*
-
Neonatal morbidity defined as:
hypoxic ischaemic encephalopathy ‐ moderate‐to‐severe encephalopathy defined using a combination of clinical and biochemical parameters. This was defined as: in infants greater than 36 weeks' gestational age, either cord or arterial pH less than 7 or base deficit greater than 16 within the first hour of life or if there is no blood gas or cord or arterial pH 7 to 7.15 and base deficit 10 to 16, then additional criteria of history of an acute perinatal event and Apgar less than 5 at 10 minutes or need for mechanical ventilation at 10 minutes of age (Shankaran 2005);
low Apgar scores defined as a 10‐minute Apgar score less than 5;
seizures: electroencephalographically confirmed seizure within 72 hours of birth;
hypothermia (defined as a temperature less than 36 °C) on admission to the neonatal unit (de Almeida 2014); admission to the neonatal unit in randomised infants including those requiring resuscitation;
meconium aspiration syndrome ‐ defined as respiratory distress in an infant born through meconium‐stained amniotic fluid whose symptoms cannot be otherwise explained (Cleary 1998);
neurodevelopmental outcome at 18 to 24 months as assessed by a validated scoring tool.
Secondary outcomes
Change in healthcare professional and resuscitation team behaviour (measured by frequency or duration of six team behaviours: inquiry, information sharing, assertion, teaching and advising, workload management and vigilance) and decrease in resuscitation duration (Thomas 2007).*
Knowledge acquisition and retention (measured by written test immediately after the resuscitation training programme, six months or one year after resuscitation training programme) (Bell 2008).
Skill acquisition and retention (measured by skill appraisal immediately after resuscitation training programme, six months or one year after resuscitation training programme) (Bell 2008).
Mortality during initial hospitalisation.
*post‐hoc analyses.
Search methods for identification of studies
We performed our search for relevant articles using the Cochrane Neonatal Review Group's (CNRG) search strategy without language restriction in April 2014 and updated in March 2015. We searched:
the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, 2015, Issue 1);
electronic journal reference databases: MEDLINE (1966 to March 2015) and PREMEDLINE, EMBASE (1980 to March 2015), CINAHL (1982 to March 2015), Web of Science (1975 to April 2014) and the Oxford Database of Perinatal Trials;
ongoing trials at the following web sites: www.clinicaltrials.gov, www.controlled‐trials.com, and the World Health Organization (WHO) International Clinical Trials Platform (ICTRP) at www.who.int/ctrp/en.
abstracts of conferences ‐ proceedings of Pediatric Academic Societies (American Pediatric Society, Society for Pediatric Research and European Society for Paediatric Research (ESPR)) (PAS electronic version from 2000 to March 2015 and ESPR handsearch from 2000 to March 2015);
reference lists of identified clinical trials and in the authors' personal files.
In addition, we contacted authors who published in the field of neonatal resuscitation to identify relevant articles.
Search strategy for MEDLINE and PREMEDLINE
We adapted this strategy to suit CENTRAL, EMBASE and CINAHL.
explode 'resuscitation' [all subheadings in MIME, MJME]
training
teaching
NRP
Neonatal Resuscitation Program
Simulation
# 1 OR # 2 OR # 3 OR # 4 OR # 5 OR # 6
explode 'infant ‐ newborn' [all subheadings in MIME, MJME]
Neonat*
Newborn*
# 7 or # 8 or # 9
# 7 and # 11
Data collection and analysis
We employed the standard methods of the CNRG (neonatal.cochrane.org.en/index.html).
Selection of studies
The search identified randomised and quasi‐randomised trials. Review authors independently assessed the titles and the abstracts of studies identified by the search strategy for eligibility to be included in the review. Where this could not be done reliably, we obtained the full‐text version for assessment. We resolve differences by discussion. Where any queries arose or where additional data were required, we contacted the relevant study authors.
Data extraction and management
We used a data extraction form specifically designed for the study. Two review authors independently extracted, assessed and coded all data for each included study.
Assessment of risk of bias in included studies
We used the standardised review methods of the CNRG to assess the methodological quality of the studies. Review authors independently assessed the quality of the included studies using the standard criteria developed by The Cochrane Collaboration and the CNRG. We assessed the risk of bias for cluster‐randomised trials (Section 16.3.2) and for individual randomised trials (Table 8.5a) as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). In addition to risk of bias, we assessed quality of evidence using the GRADE method as evidence of high, moderate, low and very low quality based on imprecision, inconsistency, indirectness and publication bias (Higgins 2011).
For cluster‐randomised trials, we assessed recruitment bias, baseline imbalance, loss of clusters or individuals from the cluster, whether analysed taking clustering into account (unit of analysis error) and contamination between clusters.
For individual randomised trials, we independently assessed the quality and risk of bias of the potential studies based on the following six domains.
-
Selection bias
Method of sequence generation: selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence.
Concealment of allocation: selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment. In cluster‐randomised trials, all clusters are randomised at once and hence allocation concealment is usually not an issue. Baseline imbalance among clusters may be an issue.
Performance bias: due to knowledge of the allocated interventions by participants and personnel during the study.
Detection bias: due to knowledge of the allocated interventions by outcome assessors
Attrition bias: due to amount, nature or handling of incomplete outcome data
Reporting bias: due to selective outcome reporting.
Any other sources of bias or important concerns not addressed in the previous domains.
We resolved all discrepancies by discussion and consensus.
Measures of treatment effect
We reported dichotomous data using risk ratio (RR) and risk difference (RD) with 95% confidence intervals (CI). If there was a statistically significant reduction in RD, we calculated the number needed to treat for an additional beneficial outcome (NNTB) or additional harmful outcome (NNTH) and associated 95% CI. We reported MD with 95% CI for continuous outcomes.
Unit of analysis issues
In cluster‐randomised trials, we reported whether the sample size was estimated based on the intracluster correlation coefficient (ICC) and whether the trial had been analysed at the level of the cluster (the unit of randomisation) or the individual.
Assessment of heterogeneity
We assessed heterogeneity of treatment effects between trials using the I2 statistic to check the appropriateness of pooling data and performing meta‐analysis. We deferred meta‐analysis if heterogeneity was high (greater than 75%).
Data synthesis
We performed statistical analysis according to the recommendations of the CNRG and used the statistical package Review Manager 5 (RevMan 2011). Planned analyses for the subgroups were performed as defined under the Criteria for considering studies for this review. We used the fixed‐effect model for meta‐analysis.
Analysis of cluster‐randomised trials was performed as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). In cluster‐randomised trials that were analysed appropriately at the cluster level using the ICC, we used the summary estimate to generate natural log of the RR and standard error of the log RR, entered in Review Manager 5 and meta‐analysed using the generic inverse variance method. In cluster‐randomised trials that were not analysed at the cluster level, where the ICC was available, we calculated the design effect using the ICC and adjusted the sample size for analyses. If the ICC was not available, we used an assumed ICC from similar trials (used ICC from Carlo 2010a for Gill 2011) or performed approximate analysis as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When ICC could not be assumed due to variability in the study design or outcome, we summarised the results without meta‐analysis.
Subgroup analysis and investigation of heterogeneity
Planned subgroup analyses
Geographical location.
Developed world versus developing world.
A developed country is defined as a sovereign state that has a developed economy and advanced technological infrastructure. The criteria for evaluating the degree of economic development are gross domestic product (GDP), the per capita income and general standard of living (IMF 2012).
Type of programme.
-
Any neonatal resuscitation programme versus another neonatal resuscitation programme:
didactic programmes versus skill‐based programmes;
simulation programme versus didactic programmes;
simulation programme versus skill‐based programmes.
-
-
Type of participants.
Based on providers from different healthcare settings (e.g. hospital, clinic or community‐based healthcare providers).
Results
Description of studies
Results of the search
Our search strategy yielded 17,906 articles and 792 non‐duplicate articles were screened (Figure 1). Two review authors (ED and MP) independently reviewed the titles and abstracts of all potential articles. We identified 43 potential studies for inclusion. After reviewing the full‐text articles, 14 studies were eligible for inclusion in this review. The details of each of these studies are reported in the Characteristics of included studies table.
1.
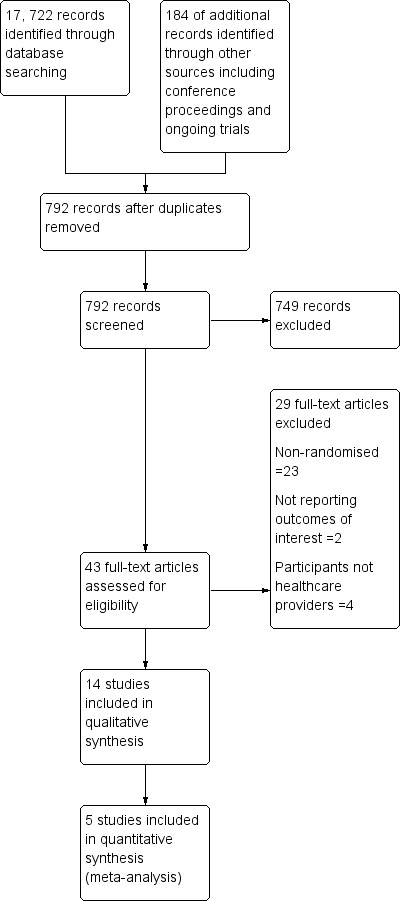
PRISMA flow diagram.
Included studies
Fourteen studies addressed the effects of formal neonatal resuscitation training programmes and met our inclusion criteria (Dunn 1992; Kaczorowski 1998; Thomas 2007; Opiyo 2008; Bould 2009; Carlo 2010a; Carlo 2010b; Thomas 2010; Gill 2011; Lee 2012; Xu 2014; Bender 2014; Rubio‐Gurung 2014; Fuerch 2015). Five were community‐based cluster‐randomised trials (Opiyo 2008; Carlo 2010a; Carlo 2010b; Gill 2011; Xu 2014), and nine were randomised controlled trials addressing aspects of knowledge and skills retention and changes in team behaviour (Dunn 1992; Kaczorowski 1998; Thomas 2007; Bould 2009; Thomas 2010; Lee 2012; Bender 2014; Rubio‐Gurung 2014; Fuerch 2015).
Randomised studies evaluating neonatal mortality
Carlo 2010a was a cluster‐randomised study that addressed the effects of NRP on neonatal mortality in a global network of Women's and Children's Health Research (First Breath Study Group). Prior to the implementation of the NRP, the Early Newborn Care (ENC), which is a basic newborn care intervention recommended by the WHO, was administered. The contents of the NRP course included in‐depth, hands‐on training in basic resuscitation knowledge and skills, including initial steps in resuscitation and bag‐and‐mask ventilation, but did not include training in chest compressions, endotracheal intubation or administration of medications. This trial involved 62,366 neonates born at or above 1500 g in body weight, in six countries (Zambia, India, Democratic Republic of Congo, Argentina, Guatemala and Pakistan) from March 2005 to February 2007. Randomised clusters were geographically distinct rural communities with at least 300 births a year. Eighty‐eight clusters were randomised to NRP intervention or no intervention in five countries (Argentina was not included), 43 clusters in the NRP group and 45 in the control group. The primary outcome was neonatal mortality from all causes in the first seven days after birth.
Carlo 2010b was a report of neonates who were born at less than 1500 g in body weight over the same time period in the same five countries as Carlo 2010a. The design and methodology were the same as Carlo 2010a but both studies were independently analysed and reported. In 1096 very low birthweight (VLBW) infants, 88 clusters of geographically distinct rural communities with at least 300 births a year were randomised to NRP intervention (43 clusters) or no intervention (45 clusters) in five countries (Argentina was not included). The primary outcome was neonatal mortality from all causes in the first seven days after birth.
Matendo 2011 reported the Democratic Republic of Congo component of the global network of Women's and Children's Health Research (First Breath Study Group) and was a subset of the Carlo 2010a study. The design and methodology were the same as Carlo 2010a. There were 6293 newborns enrolled in 12 geographically distinct rural communities. Twelve clusters were randomised, six clusters to the NRP group and six to the control group. The primary outcome was neonatal mortality from all causes in the first seven days of life. The data from this study were a subset of Carlo 2010a and hence not separately included in the meta‐analysis.
Gill 2011 performed a cluster‐randomised trial in the Lufwanyama District of Zambia involving traditional birth attendants who had been trained in basic obstetric and newborn care (including mouth‐to‐mouth assisted breathing) and clean delivery techniques, and used clean delivery kits for every delivery. A total of 3437 live births were enrolled and randomised to 60 intervention and 67 control clusters. Clusters were defined by the number of births delivered by a traditional birth attendant. The intervention was a modified version of the NRP coupled with single‐dose amoxicillin and referral of infants to a health centre compared with no intervention. The primary outcome was neonatal mortality in the first 28 days after birth.
Goudar 2012 reported the Indian component of the global network of Women's and Children's Health Research (First Breath Study Group) and was a subset of the Carlo 2010a study. The design and methodology were the same as Carlo 2010a and this was the largest site participating in the global network of Women's and Children's Health Research and the methodology of the trial was as per the First Breath Study Group. There were 12,904 newborns enrolled. Twenty‐six clusters were randomised to NRP intervention or control with 13 clusters each in the intervention and the control groups. Clusters were geographically distinct rural communities with at least 300 births per year. The primary outcome was neonatal mortality from all causes in the first seven days after birth. The data from this study were a subset of Carlo 2010a and hence not separately entered into the meta‐analysis.
Opiyo 2008 was a community‐based randomised controlled trial to determine if a simple one‐day newborn resuscitation training (NRT) improves health worker resuscitation practices in a public hospital setting in Kenya. Health workers were randomised to receive early training with NRT (28 health workers) or late training (the control group, 55 health workers). The training was adapted locally from the resuscitation programme recommended by the UK resuscitation council. The primary outcome was the proportion of appropriate initial resuscitation steps and the secondary outcomes were frequency of inappropriate practices and resuscitation mortality in the delivery room. Data were collected on 97 resuscitation episodes in the intervention group and 115 resuscitation episodes in the control group over seven weeks after early training.
Xu 2014 was a community‐based cluster‐randomised trial from eight counties (two provinces) that evaluated an intervention package promoting effective neonatal resuscitation training at county level hospitals across China. The study was conducted in Shandong and Heilongjiang, two eastern provinces of China. The intervention group consisted of 11 hospitals and 97 healthcare providers and the control group consisted of 11 hospitals and 87 healthcare providers. The intervention package was the neonatal resuscitation programme based on ILCOR guidelines that includes the initial steps of resuscitation, physiology, positive pressure ventilation (PPV), intubation, cardiac compressions (CC) and medication administration. The outcomes reported were incidence of birth asphyxia defined as Apgar scores of 7 or less at five minutes, asphyxia‐related deaths in the delivery room and healthcare providers' knowledge and self confidence that were evaluated by questionnaires.
Fuerch 2015 was a randomised controlled study of 65 participants (18 residents, one fellow, seven attending physicians, two respiratory therapists and 37 nurses) who were randomised to an electronic decision support tool (which gives auditory and visual prompts) or to no tool. Thirty participants were randomised to the control group and 35 to the intervention group. Primary outcomes were the percentage of time a participant appropriately decided to perform PPV or CC and the frequency of fraction of inspired oxygen (FiO2) adjustment. The study was conducted at Center for Advanced Pediatric and Perinatal Education (CAPE) at Lucille Packard Children's Hospital at Stanford.
Randomised studies evaluating acquisition and retention of knowledge and skills or behaviour
Dunn 1992 performed a cluster‐randomised trial of 20 institutions in Ontario, Canada and each institution contributed 10 participants. Cluster randomisation by institution was performed to avoid potential cross‐contamination between control and experimental subjects. The experimental group was pre‐tested, received a full‐day neonatal resuscitation programme, and were then post‐tested immediately after the intervention and again at six months. The testing involved a 50‐item multiple choice questionnaire for (knowledge), observer checklist (skills) and a 5‐point scale for the subject's perception of competence. The control group were tested at the initial visit and again at six months, with no teaching in between.
Kaczorowski 1998 compared the effectiveness of two booster strategies to improve retention of skills and knowledge in neonatal resuscitation. Family practice residents were randomly allocated to one of three groups: video, hands on or control. Residents in the two experimental groups (video and hands on) received a 'booster' three to five months after the NRP course and all participants completed the follow‐up test six to eight months after taking the course. The main outcome measures consisted of the NRP written examination and the performance checklists. A total of 44 residents completed the study (video, 13 residents; hands on, 14 residents; control, 17 residents).
Thomas 2007 randomised interns to receive NRP with team training or standard NRP, then video recorded simulated resuscitations at the end of a one‐day‐long course. Outcomes were assessed by observers blinded to the intervention allocation and included the frequency or duration of team behaviours namely inquiry, information sharing, assertion, teaching and advising, workload management and vigilance.
Bould 2009 recruited 32 anaesthesia trainees who had completed NRP previously and stratified by time elapsed since taking an NRP course and randomised to the use of a poster (cognitive aid) or not during a resuscitation scenario. Primary outcome was a validated 15‐point checklist for resuscitation technical score and the secondary outcome was Anaesthetists' Non‐Technical Skills (ANTS) scale of behavioural scores. The study was conducted at St. Michael's hospital and the University of Toronto, Canada.
In a follow‐up study, Thomas 2010 evaluated whether interns who received a two‐hour teamwork training intervention with the NRP compared to standard NRP demonstrated more teamwork and higher quality of resuscitation. A randomised trial was performed in which half of the participants in the team training arm practiced NRP skills by using high‐fidelity simulators; the remaining practiced with low‐fidelity simulators, as did control participants. Blinded, trained observers viewed video recordings of high‐fidelity simulated resuscitations for teamwork and resuscitation quality.
Lee 2012 was a randomised study of neonatal resuscitation simulation combined with an educational session versus standard didactics in second to fourth year emergency medicine residents. Twenty‐seven residents were enrolled of which 12 participants were randomised to the intervention group. The outcomes reported were neonatal resuscitation scores and confidence in neonatal resuscitation (evaluated by questionnaire).
Bender 2014 was a single‐centre randomised controlled trial of 50 residents from neonatal intensive care unit (NICU) and non‐NICU programmes that evaluated the impact of simulation booster seven to 10 months after NRP. Individual resident's resuscitation performance (procedural skills and team behaviour) were assessed 15 to 18 months after NRP training.
Rubio‐Gurung 2014 was a cluster‐randomised trial of in situ high‐fidelity simulation of neonatal resuscitation in 12 maternity hospitals in France. A random sample of 10 professionals in each unit was presented with two standardised scenarios played on a neonatal high‐fidelity simulator (four‐hour simulation training session delivered in situ for multidisciplinary groups of six professionals). All maternity hospitals were evaluated three months after the intervention and the outcomes reported were resuscitation technical scores, team scores, number of hazardous events and frequency of achieving heart rate greater than 90 beats per minute at three minutes and greater than 130 beats per minute at five minutes.
Excluded studies
We excluded 29 studies that evaluated neonatal resuscitation programmes mainly because they were for non‐randomised studies (see Characteristics of excluded studies table).
Non‐randomised studies evaluating neonatal outcomes
Ten non‐randomised studies addressed outcomes in a pre‐ and post‐intervention study design. Duran 2008a identified an improvement in Apgar scores and a reduction in hospital stay in neonates with perinatal asphyxia in Turkey, following implementation of the NRP. Patel 2001 and Patel 2002 identified an improvement in Apgar scores in term and VLBW infants in the state of Illinois, USA, following the introduction of the NRP. Deorari 2001 evaluated the impact of NRP on the incidence, management and outcome of birth asphyxia in 14 teaching hospitals in India. Chomba 2008 was a pre‐post intervention study evaluating the efficacy of ENC training that included neonatal resuscitation in Zambia. Boo 2009 identified an improvement in national perinatal and neonatal mortality in Malaysia during the eight years following implementation of the NRP compared to a historical five‐year period before the intervention. Carlo 2010c was a non‐randomised study of NRP performed in seven Zambian districts. Three studies assessed the efficacy of the Helping Babies Breathe (HBB) initiative in a non‐randomised study design (Ashish 2012; Goudar 2013; Msemo 2013).
Non‐randomised studies evaluating acquisition and retention of knowledge and skills
We excluded 13 non‐randomised studies from countries including Canada, Turkey, Italy, Sudan and Iraq that evaluated knowledge and skills acquisition following participation in a resuscitation training programme. Five studies used a pre‐post intervention design (Ergenekon 2000; Skidmore 2001; Trevisanuto 2005;Trevisanuto 2007; Duran 2008b). Two studies assessed paediatric advanced life support (López‐Herce 1999; Durojaiye 2002). Nadler 2011 investigated the role of debriefing as a tool to improve outcome of NRP in a non‐randomised evaluation. Singhal 2001 evaluated whether healthcare personnel used the NRP guidelines in the resuscitation of newborn babies using an interactive voice response system following a resuscitation. One study evaluated practical skills retention seven months following HBB (Ersdal 2013). Mathai 2015 was a non‐randomised manikin study that determined the effectiveness of training of healthcare personnel in use of the self inflating bag or the T‐piece resuscitator. Tan 2014 was a non‐randomised study on quality of CCs in resuscitation trained neonatal staff. Walker 2014 was a non‐randomised study of hospital‐based implementation trial of PRONTO (Programa de Rescate Obstetrico y Neonatal: Tratamiento optimo y Oportuno), a simulation‐based obstetric and neonatal emergency training programme in Mexico and reported on knowledge, self efficacy and teamwork scores.
Studies that evaluated the standardised formal neonatal resuscitation training in students who were not healthcare providers
Cavaleiro 2009, Curran 2015, and Deindl 2015 evaluated medical students and Hubballi 2014 evaluated auxiliary nursing midwife students in resuscitation training programmes.
Other excluded studies
Finan 2012 compared high‐fidelity versus low‐fidelity scenarios in NRP‐trained individuals and was not an evaluation of the NRP programme. Senarath 2007 was a community‐based cluster‐randomised trial but did not report any of our pre‐specified outcomes.
Other studies
Two studies were presented as abstracts in conferences and we are awaiting data from the investigators and classification (Campbell 2014; Yamada 2015). We also identified one ongoing study (Bang 2014).
Risk of bias in included studies
Detailed study specific risk of bias assessment is provided in the 'Risk of bias' section of the Characteristics of included studies table.
Allocation
In the community‐based NRP intervention studies that were cluster‐randomised, bias due to knowledge of the type of cluster before participant recruitment to the cluster could not be assessed. Allocation concealment was not relevant to the community‐based studies that were cluster‐randomised. Most of the manikin‐based studies reported adequate randomisation and allocation concealment (Kaczorowski 1998; Thomas 2007; Bould 2009; Thomas 2010; Lee 2012; Bender 2014).
Blinding
All the community‐based studies (Carlo 2010a; Carlo 2010b; Gill 2011; Goudar 2013; Xu 2014), and two manikin studies (Dunn 1992; Rubio‐Gurung 2014), were cluster‐randomised and hence blinding to minimise performance bias was not possible. Blinding of data entry to decrease detection bias was not clearly described in community‐based studies. Manikin studies by Thomas 2007 and Thomas 2010 specified the blinding of the detectors to the group assignment. Overall, methods to minimise performance and detection bias were not clearly described.
Incomplete outcome data
Overall follow‐up was excellent (greater than 95%) in the community‐based studies (Carlo 2010a; Carlo 2010b; Gill 2011). Thomas 2007 reported 80% follow‐up as few video recordings needed to be discarded and Bender 2014 reported a 13% attrition rate. In other studies, the follow‐up was more than 85% and hence attrition bias in these studies was minimal.
Selective reporting
All the community‐ and manikin‐based studies reported the pre‐specified outcomes.
Other potential sources of bias
Three cluster‐randomised trials noted unit of analysis error at the individual level (Dunn 1992; Xu 2014; Rubio‐Gurung 2014). There were no other potential sources of bias in the included studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Standardised formal neonatal resuscitation programme (SFNRT) compared with no SFNRT.
| Standardised formal neonatal resuscitation programme (SFNRT) compared with no SFNRT | ||||||
|
Patient or population: birth attendants Settings: hospitals in Canada Intervention: SFNRT Comparison: no SFNRT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No SFNRT | SFNRT | |||||
|
Knowledge acquisition (Immediately after SFNRT) |
Population at risk | RR 5.96 (3.60 to 9.87) | 166 participants (1 study) |
⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of serious risk of bias (high risk of selection bias, unit of analysis error and serious imprecision (evidence available from a single small study)) | |
| 153 per 1000 | 911 per 1000 (551 to 1510) |
|||||
|
Skills Acquisition (Immediately after SFNRT) |
Population at risk | RR 170.93 (10.78 to 2710.85) | 166 participants (1 study) |
⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of serious risk of bias (high risk of selection bias, unit of analysis error and serious imprecision (evidence available from a single small study)) | |
| 0 per 1000 | Not estimable | |||||
|
Knowledge retention (6 months after SFNRT) |
Population at risk | RR 3.60 (2.43 to 5.35) | 166 participants (1 study) |
⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of serious risk of bias (high risk of selection bias, unit of analysis error and serious imprecision (evidence available from a single small study)) | |
| 235 per 1000 | 846 per 1000 (571 to 1257) |
|||||
|
Skills retention (6 months after SFNRT) |
Population at risk | RR not estimable as there were no events in the control or the intervention groups | 166 participants (1 study) |
⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of serious risk of bias (high risk of selection bias, unit of analysis error and serious imprecision (evidence available from a single small study)) | |
| 0 per 1000 | Not estimable | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; SFNRT: standardised formal neonatal resuscitation programme. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Summary of findings 2. Standardised formal neonatal resuscitation training (SFNRT) programme compared with basic resuscitation training for reduction in neonatal mortality.
| Standardised formal neonatal resuscitation training (SFNRT) programme compared with basic resuscitation training for reduction in neonatal mortality | ||||||
|
Patient or population: Neonates delivered stratified by healthcare professionals involved in attending deliveries Settings: healthcare facility or home setting in low‐income settings of the developing world Intervention: SFNRT Comparison: basic resuscitation training | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Basic resuscitation training | SFNRT | |||||
|
Early neonatal mortality (mortality in the first 7 days of life) |
Low‐risk population | RR 0.88 (0.78 to 1.00) | 66,162 neonates (3 studies) |
⊕⊕⊕⊝ moderate | The quality of evidence was downgraded 1 level because of absence of blinding of intervention and inconsistencies across studies | |
| 21 per 1000 | 18 per 1000 (16 to 21) |
|||||
| Medium‐risk population | ||||||
| 30.5 per 1000 | 27 per 1000 (24 to 30.5) |
|||||
| High‐risk population | ||||||
| 645 per 1000 VLBW infants | 568 per 1000 VLBW infants (503 to 645) |
|||||
| Early neonatal mortality ‐ traditional birth attendants | Low‐risk population | RR 0.79 (0.65 to 0.95) | 27,673 neonates (3 studies) |
⊕⊕⊕⊝ moderate | The quality of evidence was downgraded 1 level because the participants were not blinded for the intervention | |
| 22 per 1000 | 17 per 1000 (14 to 21) |
|||||
| Medium‐risk population | ||||||
| 31 per 1000 | 18 per 1000 (95% CI 24 to 29) | |||||
| High‐risk population | ||||||
| 721 per 1000 | 570 per 1000 (469 to 685) |
|||||
| Early neonatal mortality ‐ nurse/midwife | Low‐risk population | RR 1.03 (0.81 to 1.31) | 20,250 neonates (2 studies) |
⊕⊕⊕⊝ moderate | The quality of evidence was downgraded 1 level because the participants were not blinded for the intervention | |
| 18 per 1000 | 19 per 1000 (15 to 24) |
|||||
| High‐risk population | ||||||
| 632 per 1000 | 651 per 1000 (512 to 828) |
|||||
| Early neonatal mortality ‐ physician | Low‐risk population | RR 1.43 (0.98 to 2.08) | 5986 neonates (2 studies) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because the participants were not blinded for the intervention and inconsistencies among studies | |
| 20 per 1000 | 29 per 1000 (19.6 to 42) |
|||||
| High‐risk population | ||||||
| 365 per 1000 VLBW infants | 522 per 1000 VLBW infants (358 to 759) |
|||||
| Early neonatal mortality ‐ family/unattended | Low‐risk population | RR 0.71 (0.54 to 0.94) | 12,253 neonates (2 studies) |
⊕⊕⊕⊝ moderate | The quality of evidence was downgraded 1 level because the participants were not blinded for the intervention | |
| 25 per 1000 | 18 per 1000 (13.5 to 24) |
|||||
| High‐risk population | ||||||
| 667 per 1000 VLBW infants | 474 per 1000 VLBW infants (360 to 627) |
|||||
|
Late neonatal mortality (mortality at > 7 days up to 28 days of life) |
At‐risk population | RR 0.47 (0.20 to 1.11) | 3274 neonates (1 study) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because the participants were not blinded for the intervention, the intervention also included administration of single dose of antibiotic if clinical concern of infection and facilitated referral to healthcare facility. The evidence was available from only 1 study | |
| 9 per 1000 | 4 per 1000 (1.8 to 10) |
|||||
| Neonatal mortality at 28 days | At‐risk population | RR 0.55 (0.33 to 0.91) | 3355 neonates (1 study) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because the participants were not blinded for the intervention, the intervention also included administration of single dose of antibiotic if clinical concern of infection and facilitated referral to healthcare facility. The evidence was available from only 1 study | |
| 40 per 1000 | 22 per 1000 (13.2 to 36) |
|||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; SFNRT: standardised formal neonatal resuscitation training; VLBW: very low birthweight. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Summary of findings 3. Standardised formal neonatal resuscitation training (SFNRT) programme with team training compared with SFNRT for improving teamwork behaviour.
| Standardised formal neonatal resuscitation training (SFNRT) programme with team training compared with SFNRT for improving teamwork behaviour | ||||||
|
Patient or population: healthcare professionals involved in attending deliveries Settings: mannequin based study in an educational setting Intervention: SFNRT with team training Comparison: SFNRT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| SFNRT | SFNRT with team training | |||||
| Teamwork behaviour ‐ any teamwork behaviour | The mean team behaviour ranged across control groups from 1.1 to 9.01 behaviours/minute | The mean team behaviour ranged across intervention groups from 3.42 to 11.56 behaviours/minute | MD 2.41 (1.72 to 3.11) | 130 participants (2 studies) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because of serious imprecision (evidence was available from only 2 studies from a single institution) and serious risk of bias (unclear allocation concealment and high risk for attrition bias in 1 study) |
| NRP performance scores | The mean NRP performance score in the control group was 71.5 | The mean NRP performance score in the intervention group was 72.9 | MD 1.40 (‐2.02 to 4.82) | 98 participants (1 study) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because of serious imprecision (evidence was available from only 2 studies from a single institution) and serious risk of bias (unclear allocation concealment and high risk for attrition bias in 1 study) |
| Resuscitation duration | The mean resuscitation duration ranged across control groups from 609 to 634 seconds |
The mean resuscitation duration ranged across intervention groups from 465 to 479 seconds | MD ‐149.54 (‐214.73 to ‐84.34) | 130 participants (2 studies) |
⊕⊕⊝⊝ low | The quality of evidence was downgraded 2 levels because of serious imprecision (evidence was available from only 2 studies from a single institution) and serious risk of bias (unclear allocation concealment and high risk for attrition bias in 1 study) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; NRP: Neonatal Resuscitation Program; SFNRT: standardised formal neonatal resuscitation training. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Summary of findings 4. Standardised formal neonatal resuscitation training (SFNRT) programme with boosters compared with SFNRT for knowledge and skills retention.
| Standardised formal neonatal resuscitation training (SFNRT) programme with boosters compared with SFNRT for knowledge and skills retention | ||||||
|
Patient or population: healthcare professionals involved in attending deliveries Settings: educational setting at University of Toronto Intervention: SFNRT with boosters Comparison: SFNRT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| SFNRT | SFNRT with boosters | |||||
| Knowledge retention ‐ hands on booster on NRP test scores | The mean score in the control group was 187 | The mean score in the intervention group was 194 | MD 7 (‐2.87 to 16.87) |
31 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
| Knowledge retention ‐ video booster on NRP test scores | The mean score in the control group was 187 | The mean score in the intervention group was 191 | MD 4 (‐9.72 to 17.72) |
30 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
| Knowledge retention ‐ any booster on NRP scores | The mean score in the control group was 187 | The mean score in the intervention group was 192.5 | MD 5.50 (‐4.37 to 15.37) | 44 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
|
Skills retention ‐ hands on booster on performance scores |
The mean score in the control group was 76 | The mean score in the intervention group was 81 | MD 5 (‐3.18 to 13.18) | 31 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
| Skills retention ‐ video booster on performance scores | The mean score in the control group was 76 | The mean score in the intervention group was 82 | MD 6 (‐1.16 to 13.16) | 30 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
| Skills retention ‐ any booster on performance scores | The mean score in the control group was 76 | The mean score in the intervention group was 81.48 | MD 5.48 (‐1.07 to 12.03) | 44 participants (1 study) | ⊕⊝⊝⊝ very low | The quality of evidence was downgraded 3 levels because of very serious imprecision (evidence was available from only 1 study with small sample size) and serious risk of bias (unclear concealment of allocation, absence of blinding of participants and poor follow‐up) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; NRP: Neonatal Resuscitation Program; SFNRT: standardised formal neonatal resuscitation training. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1. Standardised formal neonatal resuscitation training programme versus no resuscitation training (Comparison 1)
We identified seven trials that compared SFNRT with no SFNRT (Dunn 1992; Opiyo 2008; Bould 2009; Lee 2012; Xu 2014; Rubio‐Gurung 2014; Fuerch 2015). Two studies were community‐based studies (Opiyo 2008; Xu 2014), four were manikin‐based studies in an educational setting (Dunn 1992; Bould 2009; Lee 2012; Fuerch 2015), and one was an in situ simulation‐based SFNRT in the hospital setting (Rubio‐Gurung 2014).
Primary outcomes
Opiyo 2008 reported "overall mortality rates in all the resuscitation episodes" (18/65 with SFNRT versus 9/25 with no SFNRT, P value = 0.77), the meaning of which was unclear. We are awaiting data on neonatal mortality from the investigators.
Xu 2014 reported on incidence of asphyxia (defined as Apgar scores of 7 or less at five minutes) (7.5/1000 live births with SFNRT versus 7.8/1000 live births with no SFNRT) and mortality rate from asphyxia (16/100,000 with SFNRT versus 24.2/100,000 with no SFNRT). However, asphyxia in this study was not defined as per our definitions pre‐specified in our protocol and hence we did not include the data.
Secondary outcomes
Knowledge and skills acquisition (Outcomes 1.1 and 1.2)
One cluster‐randomised trial reported knowledge and skills acquisition in 166 participants after randomisation to SFNRT or no SFNRT (Dunn 1992). The proportion of participants who scored more than 80% on an evaluation of their knowledge of neonatal resuscitation by means of a multiple choice examination increased after training from 36% to 91%, compared to 15% in the controls (RR 5.96, 95% CI 3.60 to 9.87) (Figure 2). None of the participants scored 100% on the skills pre‐test (using structured evaluation of a mock code involving a manikin) but 100% of the experimental group did so in the post‐test (RR 170.93, 95% CI 10.78 to 2710.85) (Figure 3). However, this cluster‐randomised trial was analysed at the level of the individual and we used the design effect to adjust sample size (164 participants) using the ICC from the trial by Carlo 2010a. We rated the quality of evidence very low because of unit of analysis error and evidence was available from one single study.
2.
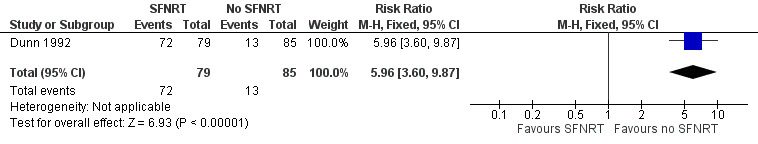
Forest plot of comparison: 1 Standardised formal neonatal resuscitation training (SFNRT) versus no resuscitation training, outcome: 1.1 Knowledge acquisition.
3.
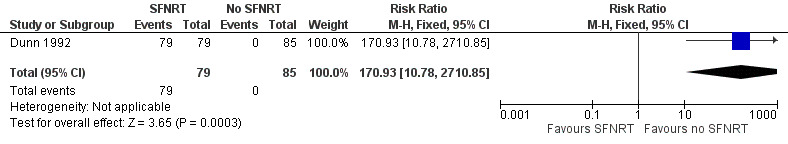
Forest plot of comparison: 1 Standardised formal neonatal resuscitation training (SFNRT) versus no resuscitation training, outcome: 1.2 Skills acquisition.
Bould 2009 randomised 32 anaesthesia residents to a cognitive aid (poster) during a resuscitation scenario and reported no differences when the intervention group was compared to controls in resuscitation technical scores (median 20.3, interquartile range (IQR) 18.3 to 21.3, range 15.0 to 24.3 with intervention versus median 18.2, IQR 15 to 20.5, range 10.7 to 25.3 with control) or ANTS scores (median 10.2, IQR 9.5 to 11, range 7.2 to 13.7 with intervention versus median 9.3, IQR 7.8 to 10.3, range 5.3 to 14 with control).
Lee 2012 reported on neonatal resuscitation scores (60.65, 95% CI 53.1 to 68.3 with intervention versus 66.69, 95% CI 61.2 to 78.2 with control). The intervention group performed 2.31 critical actions overall more than the control group and time to achieve warming (P value = 0.0002), drying (P value < 0.0001), tactile stimulation (P value = 0.002) and placing a cap on the baby (P value < 0.0001). We are awaiting more data from the investigators to be included in the meta‐analysis.
Xu 2014 reported on healthcare providers' knowledge that was evaluated by questionnaires (mean ± standard deviation (SD); 9.2 ± 1.2 with intervention versus 8.4 ± 1.5 with control, P value < 0.001).
Rubio‐Gurung 2014 reported on median technical scores (scenario one: mean 24.4, range 18.7 to 26.6 with intervention versus mean 17.4, range 15.6 to 19.5 with control, P value = 0.01; scenario two: mean 22.7, range 21.3 to 25, P value = 0.004), median team scores (mean 31.1, range 20.8 to 36.8 with intervention versus mean 19.9, range 13.3 to 25 with control, P value < 0.001). We are awaiting more data from the investigators to be included in the meta‐analysis.
Fuerch 2015 randomised 65 participants to an electronic decision support tool with prompts. PPV was performed correctly more frequently (94% to 95% with intervention versus 55% to 80% with control, P value < 0.0001) and CC were performed correctly more frequently (82% to 93% with intervention versus 71% to 81% with control, P value < 0.0001) and FiO2 was adjusted three times more frequently in the intervention group compared to controls.
Knowledge and skills retention (Outcome 1.3)
One cluster‐randomised trial reported knowledge and skills retention in 166 participants, six months after they had been randomised to SFNRT or no SFNRT (Dunn 1992). Eighty‐five per cent of the intervention group and 23% of controls passed the knowledge multiple choice test with a score of 80% or more (RR 3.60, 95% CI 2.43 to 5.35) (Figure 4). None of the participants in either group passed the skills test (mock code) at six months after the SFNRT (RR could not be estimated). However, this cluster‐randomised trial was analysed at the level of the individual and we used the design effect to adjust sample size (164 participants) using the ICC from the trial by Carlo 2010a. We rated the quality of evidence very low because of unit of analysis error and evidence available from one single study.
4.
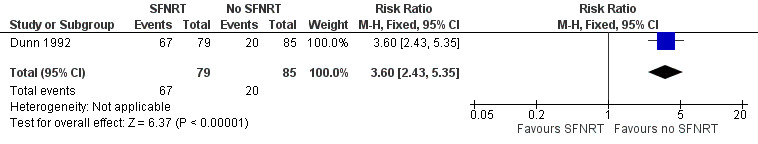
Forest plot of comparison: 1 Standardised formal neonatal resuscitation training (SFNRT) versus no resuscitation training, outcome: 1.3 Knowledge retention.
2. Standardised formal neonatal resuscitation training programme versus basic resuscitation training (Comparison 2)
We identified three community‐based cluster‐randomised trials, all performed in developing countries, which compared SFNRT with basic resuscitation training and reported on the primary outcomes (Carlo 2010a; Carlo 2010b; Gill 2011).
Primary outcomes
Early neonatal mortality (Outcome 2.1)
The estimated RR showed a reduction in early neonatal mortality (typical RR 0.88, 95% CI 0.78 to 1.00; data from three cluster‐randomised trials in 66,162 neonates) (Figure 5). We downgraded the quality of evidence from high to moderate quality, as the participants were not blinded to the intervention and due to inconsistency in the direction of the effects across studies (heterogeneity, I2 = 71%). Carlo 2010a and Carlo 2010b did not show a decrease in neonatal mortality, whereas the study by Gill 2011 that included only traditional birth attendants showed a significant decrease in mortality in the intervention group.
5.
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) versus basic newborn care, outcome: 2.1 Early neonatal mortality.
Subgroups by types of healthcare professionals
Traditional birth attendants
The estimated RR showed a reduction in early neonatal mortality (typical RR 0.79, 95% CI 0.65 to 0.95; data from three cluster‐randomised trials in 27,673 neonates). We downgraded the quality of evidence from high to moderate quality, as the participants were not blinded to the intervention. There was no heterogeneity (I2 = 20%). All three studies were conducted in the developing world and show that SFNRT of traditional birth attendants decreased early neonatal mortality.
Nurse/midwife
There was no change in the estimated RR for early neonatal mortality (RR 1.03, 95% CI 0.81 to 1.31; data from two cluster‐randomised trials in 20,250 neonates). We downgraded the quality of evidence from high to moderate quality, as the participants were not blinded to the intervention. Heterogeneity was low (I2 = 42%). Both the studies were performed in the developed world and did not show a decrease in early neonatal mortality.
Physician
Two cluster‐randomised trials compared the effects of standardised resuscitation training programme versus basic resuscitation training on early neonatal mortality in deliveries performed by physicians in 5986 neonates. Heterogeneity was high (I2 = 91%) and hence meta‐analysis was deferred. We downgraded the quality of evidence to low, as the participants were not blinded to the intervention and due to the inconsistent effects across studies. In the study by Carlo 2010a, which analysed neonates weighing 1500 g or greater, the RR was 0.64 (95% CI 0.35 to 1.17). Carlo 2010b, which analysed neonates weighing less than 1500 g, reported an increase in early neonatal mortality in physician attended deliveries (RR 2.41, 95% CI 1.48 to 3.91). The pooled RR for mortality was 1.43 (95% CI 0.98 to 2.08).
Family/unattended
The estimated RR suggested a decrease in early neonatal mortality (typical RR 0.71, 95% CI 0.54 to 0.94; data from two cluster‐randomised trials in 12,253 neonates). We downgraded the quality of evidence from high to moderate quality, as the participants were not blinded to the intervention. There was no heterogeneity (I2 = 0%). Carlo 2010a reported an RR of 0.67 (95% CI 0.45 to 1.00) and Carlo 2010b reported an RR of 0.75 (95% CI 0.51 to 1.10).
Data were not available for planned subgroup analyses by geographical location or type of resuscitation programme. All studies were performed in the developing world.
Early neonatal mortality by approximate analyses: we followed the Cochrane Handbook for Systematic Reviews of Interventions for approximate analysis of cluster‐randomised trials using 'effective sample sizes' because the ICCs of all the trials were not available (Higgins 2011). In the approximate analysis method, the sample sizes of the trials is reduced to effective sample sizes by the design effect. The design effect is in turn determined by the mean cluster size and the ICC. The second method of the approximate analysis is by inflating the standard errors of the effect estimate by multiplying with the square root of the design effect. The meta‐analysis is then performed in Review Manager 5 using the inflated variances and the generic inverse‐variance method. The approximate analysis method is generally regarded as being less accurate. Using the approximate analysis method, SFNRT programmes decreased early neonatal mortality (RR 0.85, 95% CI 0.75 to 0.96). The RD was ‐0.0044 (95% CI ‐0.0082 to ‐0.0006), which implies an NNTB of 227 (95% CI 122 to 1667). For every 227 deliveries occurring in a setting where healthcare workers were trained in a standardised formal neonatal resuscitation programme, there was one fewer neonatal death.
Late neonatal mortality (Outcome 2.2)
One cluster‐randomised trial reported no difference in the risk of late neonatal mortality in 3274 neonates (RR 0.47, 95% CI 0.20 to 1.11) (Figure 6). We downgraded the quality of evidence to low, as the participants were not blinded to the intervention and evidence was from only one study.
6.
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) versus basic newborn care, outcome: 2.2 Late neonatal mortality.
Neonatal mortality at 28 days (Outcome 2.3)
One cluster‐randomised trial reported a significant decrease in neonatal mortality in 3355 neonates after NRP (RR 0.55, 95% CI 0.33 to 0.91) (Figure 7). We downgraded the quality of evidence to low, as the participants were not blinded for the intervention and evidence was from only one study. This was a post‐hoc analysis that was not specified in the protocol.
7.
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) versus basic newborn care; outcome: 2.3 Neonatal mortality at 28 days.
Secondary outcomes
Changes in resuscitation behaviour
Three cluster‐randomised trials that enrolled 29,664 neonates reported resuscitation behaviour related to the use of bag and mask ventilation by healthcare providers. Heterogeneity was high (I2 = 95%) and meta‐analysis was deferred. We downgraded the quality of evidence to low, as the participants were not blinded to the intervention and due to the inconsistency of effects across studies. Two studies reported a significant increase in the use of bag mask ventilation (RR 1.18, 95% CI 1.04 to 1.33, Carlo 2010a; RR 29.50, 95% CI 9.39 to 92.65, Gill 2011). Carlo 2010b reported the RR for bag and mask resuscitation (RR 0.85, 95% CI 0.63 to 1.15).
Outcomes not reported: none of the included studies reported neonatal outcomes of hypoxic ischaemic encephalopathy, low Apgar scores (less than 5) at 10 minutes, seizure, hypothermia, admission to the neonatal unit, meconium aspiration syndrome, long‐term neurodevelopmental outcome at two years or mortality during initial hospitalisation.
3. Standardised formal neonatal resuscitation training programme with team training versus standardised formal neonatal resuscitation training programme (Comparison 3)
We identified two trials that compared SFNRT with team training to SFNRT (Thomas 2007; Thomas 2010).
Primary outcomes
Neither study reported on primary outcomes.
Secondary outcomes
Teamwork behaviour (Outcome 3.1)
Two randomised trials reported on teamwork behaviour in 130 participants, after completing teamwork training with SFNRT compared to SFNRT with no teamwork training (Thomas 2007; Thomas 2010). The teamwork behaviours, information sharing, inquiry, assertion, teaching and advising, managing workload and vigilance, were assessed by observations of the frequency or duration. Inquiry, information sharing, assertion, teaching and advising were measured as rates (number of behaviours in one minute), whereas workload management and vigilance were measured as a percentage of simulation time.
Teamwork training increased the frequency of any teamwork behaviour (MD 2.41 behaviours/minute, 95% CI 1.72 to 3.11). Heterogeneity was low (I2 = 0%) (Figure 8). Components of teamwork behaviour that increased after teamwork training were information sharing (MD 0.84 behaviours/minute, 95% CI 0.55 to 1.13), inquiry (MD 0.29 behaviours/minute, 95% CI 0.15 to 0.43) and managing workload (MD 9.93% of simulation time, 95% CI 6.14 to 13.73). There was no significant increase after teamwork training in teamwork behaviour related to teaching or advising (MD 0.08 behaviours/minute, 95% CI ‐0.01 to 0.16), assertion (MD 0.68 behaviours/minute, 95% CI 0.33 to 1.03) and vigilance (MD 0.20% of simulation time, 95% CI ‐0.13 to 0.53). We downgraded the quality of evidence to low as evidence was from only two studies from a single institution, unclear allocation concealment and imprecision of the estimate with wide CIs.
8.
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, outcome: 3.1 Teamwork behaviour.
Neonatal Resuscitation Program performance scores (Outcome 3.2)
One randomised trial found no difference in NRP performance scores in 98 participants after teamwork training with SFNRT compared to SFNRT with no teamwork training (estimated MD 1.40, 95% CI ‐2.02 to 4.82) (Figure 9). We downgraded the quality of evidence to low as evidence was from only one study from a single institution, unclear allocation concealment and imprecision of the estimate with wide CIs.
9.
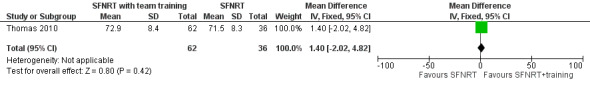
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, outcome: 3.2 Neonatal Resuscitation Program performance scores.
Resuscitation duration (Outcome 3.3)
Two randomised trials reported on resuscitation duration in 130 participants after teamwork training with SFNRT compared to SFNRT with no teamwork training (estimated MD ‐149.54 seconds, 95% CI ‐214.73 to ‐84.34) (Figure 10). We downgraded the quality of evidence to low as the evidence was from only one study from a single institution, unclear allocation concealment and imprecision of the estimate with wide CIs. This analysis was a post hoc analysis but was considered an important parameter in resuscitation.
10.
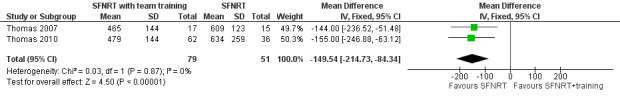
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, outcome: 3.3 Resuscitation duration.
4. Standardised formal neonatal resuscitation training programme with boosters versus standardised formal neonatal resuscitation training programme (Comparison 4)
We identified two trials that compared SFNRT with booster courses to SFNRT (Kaczorowski 1998; Bender 2014).
Primary outcomes
Neither study reported on primary outcomes.
Secondary outcomes
Knowledge retention (Outcome 4.1)
One trial reported the effect of 'hands on' and video boosters on knowledge retention in 187 participants (Kaczorowski 1998). There were no differences in knowledge retention after hands on booster (MD 7.00, 95% CI ‐2.87 to 16.87), video booster (MD 4.00, 95% CI ‐9.72 to 17.72) or any booster (MD 5.50, 95% CI ‐4.37 to 15.37) (Figure 11). We downgraded the quality of evidence to very low as evidence was from only one study and due to a high risk of selection, performance and attrition biases.
11.
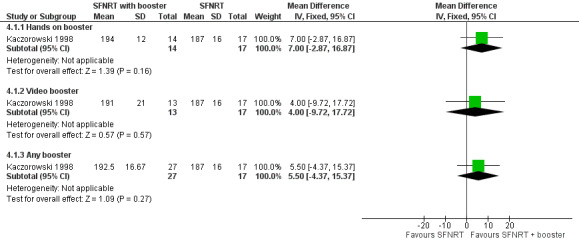
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) with boosters versus SFNRT, outcome: 4.1 Knowledge retention.
Skills retention (Outcome 4.2)
One trial reported the effect of 'hands on' and video boosters on skills retention in 187 participants (Kaczorowski 1998). There were no significant differences in skills retention after 'hands on' booster (MD 5.00, 95% CI ‐3.18 to 13.18), video booster (MD 6.00, 95% CI ‐1.16 to 13.16) or any booster (MD 5.48, 95% CI ‐1.07 to 12.03) (Figure 12). We downgraded the quality of evidence to very low as evidence was from only one study and due to a high risk of selection, performance and attrition biases.
12.
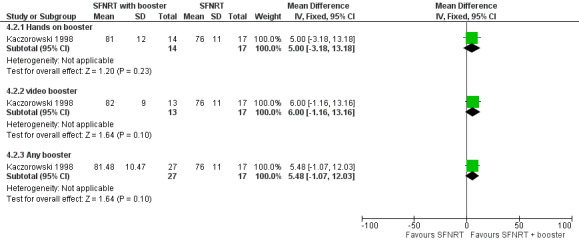
Forest plot of comparison: Standardised formal neonatal resuscitation training (SFNRT) with boosters versus SFNRT, outcome: 4.2 Skills retention.
Bender 2014 compared a simulation booster seven to 10 months after NRP and participants were assessed 15 months after NRP. There were no differences in knowledge scores between the intervention and control groups (70% with intervention versus 68.1% with control, P value = 0.57) but there was an improvement in procedural skills (sum of 107 procedural elements; 71.6 with intervention versus 64.4 with control, P value = 0.02) and behaviour (sum of 25 elements; 18.8 with intervention versus 16.2 with control, P value = 0.02). We are awaiting more data from the investigator to include in the meta‐analysis.
We could not perform a number of the planned subgroup analyses. We found no studies comparing outcomes in the developing versus the developed world or one type of programme versus another type of resuscitation programme (didactic, hands on or simulation based).
Discussion
Summary of main results
We identified 14 studies that addressed the effectiveness of standardised, formal, neonatal resuscitation training programmes, which are included in this review. Five studies were community‐based, cluster‐randomised trials performed in developing countries (Opiyo 2008; Carlo 2010a; Carlo 2010b; Gill 2011; Xu 2014), which reported neonatal mortality and data were available from three studies for meta‐analysis (Carlo 2010a; Carlo 2010b; Gill 2011). Participants in all these studies had baseline training in WHO ENC or equivalent (basic obstetric and neonatal care in Gill 2011), prior to enrolment. Moderate quality evidence from three trials that enrolled 66,162 neonates showed that intervention with SFNRT decreased early neonatal mortality (typical RR 0.88, 95% CI 0.78 to 1.00) and when analysed by the approximate analysis method (typical RR 0.85, 95% CI 0.75 to 0.96; typical RD ‐0.0044, 95% CI ‐0.0082 to ‐0.0006; NNTB 227, 95% CI 122 to 1667). A NNTB of 227 indicates that the SFNRT trained healthcare provider needs to attend 227 deliveries to reduce early neonatal mortality by one. Subgroup analyses revealed decreased early neonatal mortality for resuscitations attended by traditional birth attendants (typical RR 0.79, 95% CI 0.65 to 0.95; moderate quality evidence), and family/unattended deliveries (typical RR 0.71, 95% CI 0.54 to 0.94; moderate quality evidence) but not for nurse/midwife (typical RR 1.03, 95% CI 0.81 to 1.31; moderate quality evidence). SFNRT did not decrease late neonatal mortality (RR 0.47, 95% CI 0.20 to 1.11; one study, 3274 neonates; low quality evidence). In a post‐hoc analysis, neonatal mortality in the first 28 days of life was decreased (RR 0.55, 95% CI 0.33 to 0.91; one study, 3355 neonates; low quality evidence). None of our a priori defined neonatal morbidity outcomes of neonatal encephalopathy or neonatal seizures, 10‐minute Apgar scores, hypothermia, meconium aspiration or neurodevelopmental follow‐up were reported. One a posteriori outcome of 'mortality during initial hospitalisation' was also not reported. There were no studies comparing types of SFNRT courses (didactic, hands on or simulation based) to each other. A number of the other planned subgroup analyses could not be performed.
Nine randomised controlled trials using simulation and manikins addressed aspects of knowledge and skills acquisition and retention and changes in teamwork behaviour and the use of decision support tools in developed countries (Dunn 1992; Kaczorowski 1998; Thomas 2007; Bould 2009; Thomas 2010; Lee 2012; Bender 2014; Rubio‐Gurung 2014; Fuerch 2015). Low quality evidence from two studies that enrolled 130 participants suggested that teamwork training as adjunct to SFNRT increased any teamwork behaviour (MD 2.41 behaviours/minute, 95% CI 1.72 to 3.11) (Thomas 2007; Thomas 2010). Teamwork training did not influence NRP scores (MD 1.40, 95% CI ‐2.02 to 4.82; one study, 98 participants; low quality evidence) but decreased resuscitation duration (MD ‐149.54 seconds, 95% CI ‐214.73 to ‐84.34; two studies, 130 participants; low quality evidence). Very low quality evidence from one trial did not find any differences on knowledge retention after hands on booster (MD 7.00, 95% CI ‐2.87 to 16.87), video booster (MD 4.00, 95% CI ‐9.72 to 17.72) or any booster (MD 5.50, 95% CI ‐4.37 to 15.37) (Kaczorowski 1998). In the same study, skills retention also did not change after hands on booster (MD 5.00, 95% CI ‐3.18 to 13.18), video booster (MD 6.00, 95% CI ‐1.16 to 13.16) or any booster (MD 5.48, 95% CI ‐1.07 to 12.03; one study; very low quality evidence). Bender 2014 addressed the effects of simulation booster and found no change in knowledge but improvement in procedural skills (71.6 with intervention versus 64.4 with control, P value = 0.02) and behaviour (a sum of 25 elements; 18.8 with intervention versus 16.2 with control, P value = 0.02). Two studies addressed the use of decision support tools during resuscitation (Bould 2009; Fuerch 2015). A cognitive aid in the form of a poster did not improve resuscitation technical scores or ANTS behavioural scores but an electronic decision support tool with audible and visual prompts improved correct performance of positive pressure ventilation and cardiac compressions and FiO2 adjustments.
Simulation training in neonatal resuscitation may enhance knowledge acquisition and retention, but it remains to be seen if this will translate into an improved outcome for patients in the clinical setting. We found no such studies. It is unlikely that randomised trials reporting clinically relevant outcomes (e.g. mortality) utilising simulation training versus other teaching modalities will be performed. Therefore, simulation training will need to be assessed utilising clear, unambiguous, valid procedural metrics to determine clinician's level of competency and also permit documentation of progress and proficiency over time.
Overall completeness and applicability of evidence
Data from three community‐based, cluster‐randomised trials included in this review suggest that SFNRT intervention results in a reduction in early neonatal mortality in the developing world, where birth attendants were already trained in basic newborn care. These well‐designed, large community‐based studies provide moderate quality evidence supporting the efficacy of NRT programmes in improving neonatal outcomes. The greatest reduction in mortality was seen in the community where births were attended by SFNRT‐trained traditional birth attendants. However, all three studies were from the developing world, where baseline neonatal mortality rates are high and these findings may not be appropriate to extrapolate to the developed world. Cluster‐randomised trials of SFNRT in the developed world may not be feasible, where neonatal mortality is already low, where resuscitation training programmes are considered the standard of care and required for accreditation of training. We rated studies evaluating teamwork training and knowledge and skills low to very low quality evidence and they need to be investigated further.
Quality of the evidence
We downgraded the SFNRT intervention in the three community‐based programmes reporting neonatal mortality one level because of lack of blinding of participants to the intervention and present moderate quality evidence. We observed high heterogeneity among the studies for physician‐attended deliveries and change in resuscitation behaviour. The reasons for this high heterogeneity may be due to the differences in the neonatal population and the higher clinical risk in physician attended deliveries. Gill 2011 enrolled all neonates irrespective of birthweight, Carlo 2010b analysed only VLBW infants and Carlo 2010a included neonates born at greater than 1500 g. Enrolment of neonates with varying birthweights may be associated with varying risk that can partially contribute to this heterogeneity. High heterogeneity was also observed in the assessment of resuscitation behaviour of bag and mask ventilation, which could be attributed to the risk status of enrolled neonates or the varying skills of the trained birth attendants. All the three community‐based trials ensured good follow‐up data with loss to follow‐up less than 5%. We downgraded evidence from two studies that evaluated teamwork training as an adjunct to SFNRT by one level to low because both studies did not report allocation concealment and one study had high risk of attrition bias (Thomas 2007; Thomas 2010). Components of teamwork behaviour, namely information sharing, inquiry and assertion, showed high heterogeneity, which is hard to explain considering the homogeneity of the physician trainees enrolled in these studies. We downgraded evidence from one study that evaluated knowledge and skills retention to very low because of unclear allocation concealment, absence of blinding to intervention and high risk for attrition bias (Kaczorowski 1998).
Potential biases in the review process
We strove to decrease biases in the review process. Two authors performed the literature search using an inclusive search strategy and combined their results. Our search strategy identified randomised controlled trials reporting neonatal outcomes only from developing countries and not from the developed world. In the identified trials, we obtained additional data from the authors that facilitated the analyses (Thomas 2007; Carlo 2010a; Gill 2011), and are awaiting data from three trials (Opiyo 2008; Lee 2012; Bender 2014). Data from one study were not obtainable (Dunn 1992). Our deviations from the protocol were inclusion of 28‐day mortality, mortality during initial hospitalisation and resuscitation duration as outcomes and inclusion of GRADE methodology for assessing quality of evidence. Our deviations from the protocol were unlikely to introduce bias in the review process.
Agreements and disagreements with other studies or reviews
There are five previous published systematic reviews addressing resuscitation training and outcomes (Jabbour 1996; Meaney 2010; Opiyo 2010; Lee 2011; Mileder 2014), three of which addressed newborn resuscitation (Opiyo 2010; Lee 2011; Mileder 2014). The review by Lee 2011 included both observational studies (20 participants), quasi‐randomised (two participants) and randomised trials (two participants) relating to newborn resuscitation and found that neonatal resuscitation training in healthcare facilities reduced term intrapartum deaths (typical RR 0.70, 95% CI 0.59 to 0.84). Mileder 2014 reviewed simulation‐based neonatal and infant resuscitation teaching and identified 13 randomised controlled trials with 832 participants. However, due to distinct differences in research objectives and varying outcome assessment, the authors chose not to conduct a meta‐analysis. Eligible trials showed that simulation‐based resuscitation education can enhance trainees' cognitive, technical and behavioural skills as well as self confidence. Jabbour 1996 included all life support courses, including adult, paediatric and newborn resuscitation courses, and found a reduction in mortality after resuscitation training (odds ratio (OR) 0.28, 95% CI 0.22 to 0.37). This review was published in 1996 when there were no randomised controlled trials of SFNRT and no separate estimate of treatment effect for newborn resuscitation was provided. Meaney 2010 performed a systematic review of resuscitation training in developing countries that included neonatal resuscitation training along with paediatric and adult age groups. The review included a number of observational studies and data were not synthesised by meta‐analysis. Opiyo 2010 reviewed 'in service' training including neonatal resuscitation and found only two studies that are discussed in this review (Senarath 2007; Opiyo 2008).
Authors' conclusions
Implications for practice.
Standardised, formal, neonatal resuscitation training (SFNRT) of birth attendants, in addition to basic newborn care, results in reduction in early neonatal mortality (less than seven days after birth, moderate quality evidence) and mortality in the first 28 days after birth (low quality evidence) in developing countries. An SFNRT‐trained healthcare provider has to attend 227 deliveries to reduce early neonatal mortality by one. However, lack of blinding of participants to cluster allocation and all studies performed in the developing world, precludes generalisability of these findings. Teamwork training in addition to SFNRT in physician trainees during simulation improved teamwork behaviour and decreased resuscitation duration in the short term (low quality evidence). Boosters did not influence knowledge and skills retention (very low quality evidence).
Implications for research.
Community‐based evaluation of SFNRT in randomised trials have not been performed in the developed world; their cost‐effectiveness in such a setting is still unproven. In the developed world, it is inconceivable that SFNRT will be compared to no SFNRT, but further investigation in educational methods that facilitate acquisition and retention of knowledge and skills related to newborn resuscitation is essential to improve training and neonatal outcomes. Randomised comparisons of different SFNRT programmes (e.g. simulation versus didactic or skills‐based SFNRT) are feasible and may help to identify the most optimal method for training healthcare providers. Future studies evaluating SFNRT in developing countries should report on newborn morbidity outcomes including hypoxic ischaemic encephalopathy, low Apgar scores (less than 5) at 10 minutes, seizure, hypothermia, admission to the neonatal unit, meconium aspiration syndrome, long‐term neurodevelopmental outcome at 18 to 24 months and mortality during hospitalisation. Improvement in team behaviour and resuscitation duration after SFNRT needs to be confirmed in healthcare providers other than physician trainees, in the real‐life setting and in the long term.
Acknowledgements
We thank and acknowledge the willingness of Dr. Carlo, Dr. Gill, Dr. Bould and Dr. Thomas in sharing data from their studies that made the meta‐analysis possible.
Appendices
Appendix 1. Search strategy in Pubmed
Search strategy for Pubmed retrieved 1372 articles
(neon*[Text Word] OR newborn*[Text Word]) OR "Infant, Newborn"[Mesh] AND ("Resuscitation"[Mesh] ) AND ((training[Text Word] OR program[Text Word] OR teaching[Text Word] OR simulation[Text Word])) OR ((neonatal resuscitation program[Text Word] OR NRP[Text Word]))
Data and analyses
Comparison 1. Standardised formal neonatal resuscitation training (SFNRT) versus no SFNRT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Knowledge acquisition | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.96 [3.60, 9.87] |
| 2 Skills acquisition | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 170.93 [10.78, 2710.85] |
| 3 Knowledge retention | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.60 [2.43, 5.35] |
| 4 Skills retention | 1 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
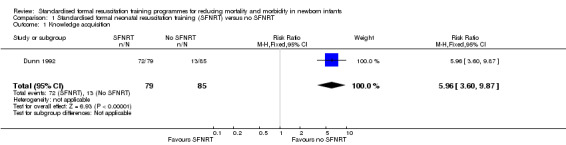
Comparison 1 Standardised formal neonatal resuscitation training (SFNRT) versus no SFNRT, Outcome 1 Knowledge acquisition.
1.2. Analysis.
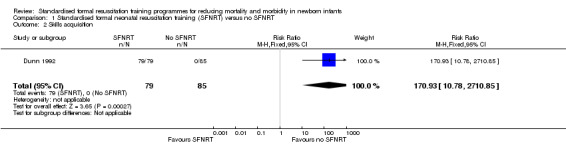
Comparison 1 Standardised formal neonatal resuscitation training (SFNRT) versus no SFNRT, Outcome 2 Skills acquisition.
1.3. Analysis.
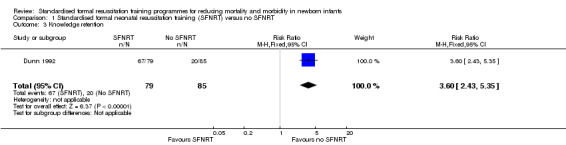
Comparison 1 Standardised formal neonatal resuscitation training (SFNRT) versus no SFNRT, Outcome 3 Knowledge retention.
1.4. Analysis.
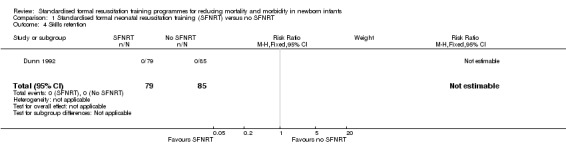
Comparison 1 Standardised formal neonatal resuscitation training (SFNRT) versus no SFNRT, Outcome 4 Skills retention.
Comparison 2. Standardised formal neonatal resuscitation training (SFNRT) versus basic resuscitation training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Early neonatal mortality | 3 | 66162 | Risk Ratio (Fixed, 95% CI) | 0.88 [0.78, 1.00] |
| 1.1 Traditional birth attendants | 3 | 27673 | Risk Ratio (Fixed, 95% CI) | 0.79 [0.65, 0.95] |
| 1.2 Nurse/midwife | 2 | 20250 | Risk Ratio (Fixed, 95% CI) | 1.03 [0.81, 1.31] |
| 1.3 Physician | 2 | 5986 | Risk Ratio (Fixed, 95% CI) | 1.43 [0.98, 2.08] |
| 1.4 Family/unattended | 2 | 12253 | Risk Ratio (Fixed, 95% CI) | 0.71 [0.54, 0.94] |
| 2 Late neonatal mortality | 1 | 3274 | Risk Ratio (Fixed, 95% CI) | 0.47 [0.20, 1.11] |
| 3 Neonatal mortality at 28 days | 1 | 3355 | Risk Ratio (Fixed, 95% CI) | 0.55 [0.33, 0.91] |
2.1. Analysis.
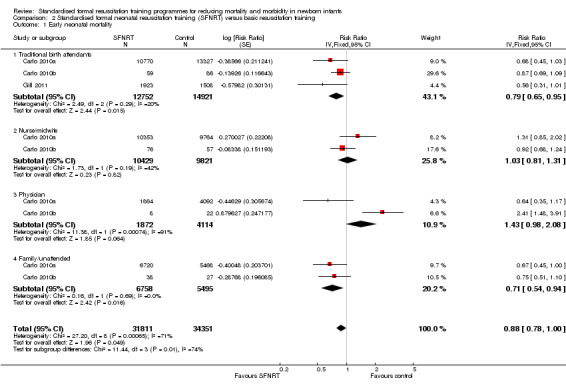
Comparison 2 Standardised formal neonatal resuscitation training (SFNRT) versus basic resuscitation training, Outcome 1 Early neonatal mortality.
2.2. Analysis.
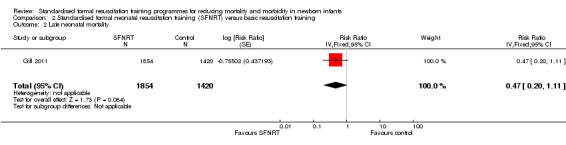
Comparison 2 Standardised formal neonatal resuscitation training (SFNRT) versus basic resuscitation training, Outcome 2 Late neonatal mortality.
2.3. Analysis.
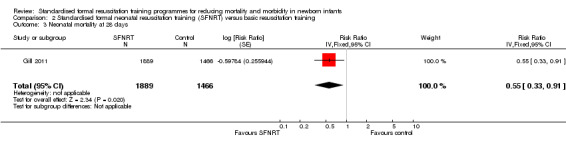
Comparison 2 Standardised formal neonatal resuscitation training (SFNRT) versus basic resuscitation training, Outcome 3 Neonatal mortality at 28 days.
Comparison 3. Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Teamwork behaviour | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Any teamwork behaviour | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 2.41 [1.72, 3.11] |
| 1.2 Information sharing | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 0.84 [0.55, 1.13] |
| 1.3 Inquiry | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 0.29 [0.15, 0.43] |
| 1.4 Assertion | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 0.68 [0.33, 1.03] |
| 1.5 Teaching or advising | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.01, 0.16] |
| 1.6 Managing workload | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 9.93 [6.14, 13.73] |
| 1.7 Vigilance | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.13, 0.53] |
| 2 Neonatal resuscitation training performance scores | 1 | 98 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [‐2.02, 4.82] |
| 3 Resuscitation duration (seconds) | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐149.54 [‐214.73, ‐84.34] |
3.1. Analysis.
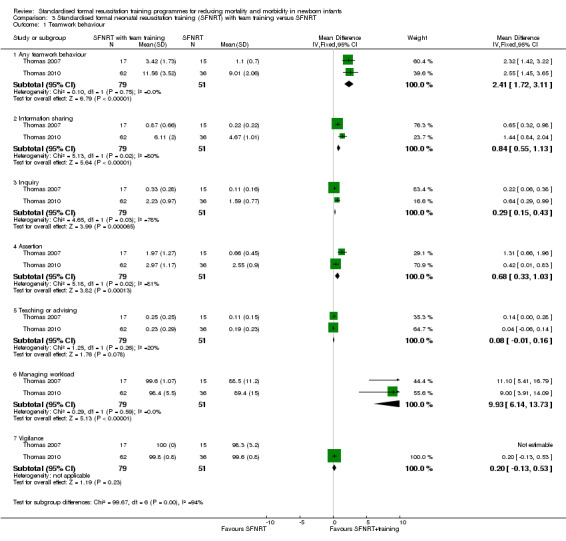
Comparison 3 Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, Outcome 1 Teamwork behaviour.
3.2. Analysis.
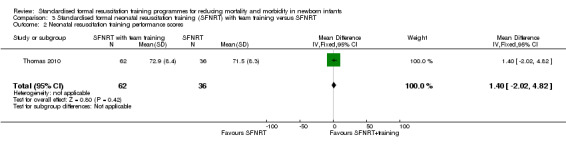
Comparison 3 Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, Outcome 2 Neonatal resuscitation training performance scores.
3.3. Analysis.
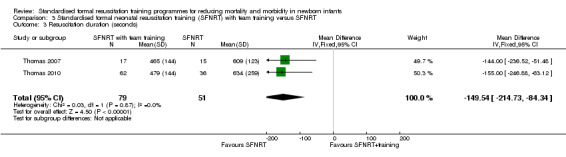
Comparison 3 Standardised formal neonatal resuscitation training (SFNRT) with team training versus SFNRT, Outcome 3 Resuscitation duration (seconds).
Comparison 4. Standardised formal neonatal resuscitation training (SFNRT) boosters versus SFNRT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Knowledge retention | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Hands on booster | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 7.00 [‐2.87, 16.87] |
| 1.2 Video booster | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐9.72, 17.72] |
| 1.3 Any booster | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 5.5 [‐4.37, 15.37] |
| 2 Skills retention | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Hands on booster | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 5.0 [‐3.18, 13.18] |
| 2.2 video booster | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 6.0 [‐1.16, 13.16] |
| 2.3 Any booster | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 5.48 [‐1.07, 12.03] |
4.1. Analysis.
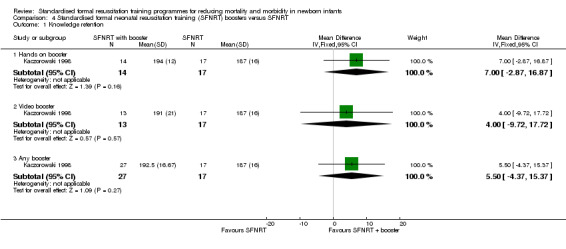
Comparison 4 Standardised formal neonatal resuscitation training (SFNRT) boosters versus SFNRT, Outcome 1 Knowledge retention.
4.2. Analysis.
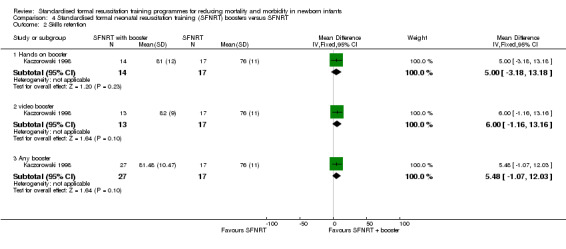
Comparison 4 Standardised formal neonatal resuscitation training (SFNRT) boosters versus SFNRT, Outcome 2 Skills retention.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bender 2014.
| Methods | Randomised controlled trial of the impact of immersive simulation in similar trainee populations' resuscitation knowledge, procedural skill and teamwork behaviour | |
| Participants | 50 residents from NICU and non‐NICU programmes | |
| Interventions | Booster simulation 7‐10 months after NRP | |
| Outcomes | Procedural skill and teamwork behaviour instruments were validated. Individual resident's resuscitation performance was assessed at 15‐18 months. 3 reviewers rated videos | |
| Notes | Single‐centre study from Rhode Island hospital, Providence, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated a priori assignment |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of intervention and control groups not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not clear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13.8% attrition noted |
| Selective reporting (reporting bias) | Low risk | Not noted |
| Other bias | Low risk | None noted |
Bould 2009.
| Methods | Randomised control study | |
| Participants | 32 anaesthesia trainees who had completed NRP previously | |
| Interventions | Trainees were stratified by time elapsed since taking an NRP course and randomised to the use of a poster (cognitive aid) or not during a resuscitation scenario | |
| Outcomes | Primary outcome was a validated 15‐point checklist for technical score for resuscitation and the secondary outcome was the ANTS scale of behavioural scores | |
| Notes | Study conducted at St. Michael's hospital and the University of Toronto | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specifically stated |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelope but transparency of the envelope not specified |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible because the intervention was the cognitive aid |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The assessors did not know if the cognitive aid was used or not by the appropriate placement of the cognitive aid |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None noted |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Unclear risk | None noted |
Carlo 2010a.
| Methods | Cluster‐randomised trial | |
| Participants | Birth attendants from 6 countries (Argentina, Democratic Republic of Congo, Guatemala, India, Pakistan, Zambia), which included traditional birth attendants, nurses, midwives and physicians | |
| Interventions | A modified version of the NRP was provided in a cluster‐randomised design (after Early Newborn Care). NRP course consisted of in‐depth, hands on training in basic knowledge and skills of resuscitation, including initial steps, bag‐and‐mask ventilation but did not include training in chest compressions, endotracheal intubation or administration of medications | |
| Outcomes | Early neonatal mortality was defined as rate of death from all causes in the first 7 days after birth. Secondary outcomes included death attributable to birth asphyxia (defined as failure to initiate or sustain normal breathing at birth, as assessed by the birth attendant), overall stillbirth rate and fresh stillbirth rate (defined as absence of maceration), perinatal death rate, death in first 24 hours after birth, 1‐ and 5‐minute Apgar (dichotomised as < 4 or ≥ 4), use of resuscitation techniques, neurological outcome at 7 days as assessed by examination | |
| Notes | Large NICHD sponsored study by the Global Network for Women's and Children's Research (First Breath Study Group) in neonates born at or above 1500 g. ICC was requested and obtained from the author (ICC = 0.002) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomisation method not stated. Not sure if recruitment to the clusters would be different if the type of cluster already known |
| Allocation concealment (selection bias) | Low risk | Not relevant as the randomisation occurred at the cluster level and occurred at 1 time point |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Not applicable |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Trained birth attendants collected data but not clear if blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data was available for 99.2% of all births |
| Selective reporting (reporting bias) | Low risk | All specified outcomes were reported |
| Other bias | Low risk | No loss of clusters were reported, analyses was appropriate taking clustering into account and clusters were similar with no baseline imbalance |
Carlo 2010b.
| Methods | Cluster‐randomised trial | |
| Participants | Birth attendants from 6 countries (Argentina, Democratic Republic of Congo, Guatemala, India, Pakistan, Zambia), which included traditional birth attendants, nurses, midwives and physicians | |
| Interventions | A modified version of the NRP was provided in a cluster‐randomised design (after Early Newborn Care). NRP course consisted of in‐depth, hands on training in basic knowledge and skills of resuscitation, including initial steps, bag‐and‐mask ventilation but did not include training in chest compressions, endotracheal intubation or administration of medication | |
| Outcomes | Early neonatal mortality was defined as rate of death from all causes in the first 7 days after birth. Secondary outcomes included death attributable to birth asphyxia (defined as failure to initiate or sustain normal breathing at birth, as assessed by the birth attendant), overall stillbirth rate and fresh stillbirth rate (defined as absence of maceration), perinatal death rate, death in first 24 hours after birth, 1‐ and 5‐minute Apgar (dichotomised as < 4 or ≥ 4), use of resuscitation techniques, neurological outcome at 7 days as assessed by examination developed by Ellis | |
| Notes | Report of VLBW infants. ICC was requested and obtained from the author (ICC = 0.002) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomisation method not stated. Not sure if recruitment to the clusters would be different if the type of cluster already known |
| Allocation concealment (selection bias) | Low risk | Not relevant as the randomisation occurred at the cluster level and at 1 time point |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Not applicable |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Trained birth attendants collected data but not clear if blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data was available for 99.2% of all births |
| Selective reporting (reporting bias) | Low risk | All specified outcomes were reported |
| Other bias | Low risk | No loss of clusters was reported, analyses were appropriate taking clustering into account and clusters were similar with no baseline imbalance |
Dunn 1992.
| Methods | Cluster‐randomised trial, where hospitals were randomised to NRP or no intervention | |
| Participants | Neonatal nurses | |
| Interventions | Neonatal resuscitation training course based on didactics and demonstration followed by revisit after 6 months. The initial workshop was offered over an 8‐hour day. Resuscitation skills were demonstrated, practiced and evaluated on a Simulaids CPR Premie Manikin. The control group received no NRP training | |
| Outcomes | A 50‐item multiple choice examination for assessing knowledge, a performance checklist for evaluating skills and a Likert‐type 5‐point rating scales for measuring participant's perception of their competence | |
| Notes | First randomised controlled trial on NRP intervention. Although cluster‐randomised, analysis was done at the individual level. Not included in meta‐analysis in this review as ICC was not known | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomisation method not stated clearly although stratification done. Not sure if recruitment to the clusters would be different if the type of cluster already known |
| Allocation concealment (selection bias) | Unclear risk | Not relevant as the randomisation occurs at the cluster level and at 1 time point |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Intervention could not be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessors aware of group status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 87% participated at 6 months |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Other bias | High risk | No loss of clusters was reported, clusters were similar with no baseline imbalance. Although cluster‐randomised, analyses were not performed at the cluster level |
Fuerch 2015.
| Methods | Randomised controlled study | |
| Participants | 65 participants were recruited into the study: 18 residents, 1 fellow, 7 attending physicians, 2 respiratory therapists and 37 nurses | |
| Interventions | Participants were randomised to an electronic decision support tool (which gives auditory and visual prompts) or to none. 30 participants were in the control group and 35 were in the intervention group | |
| Outcomes | Primary outcomes were: the percentage of time a participant appropriately decided to perform PPV or CC and frequency of FiO2 adjustment | |
| Notes | The study was conducted at the Center for Advanced Pediatric and Perinatal Education (CAPE) at Lucille Packard Children's Hospital at Stanford | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not explicitly stated |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible as the decision tool was visible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not clear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None noted |
| Selective reporting (reporting bias) | Low risk | None noted |
| Other bias | Low risk | Noted |
Gill 2011.
| Methods | Cluster‐randomised trial | |
| Participants | Traditional birth attendants in Lufwanyama district of Zambia | |
| Interventions | Modified version of NRP. All participants were trained in drying the infant, suctioning the mouth and nose and optimally positioning the airway. The intervention arm were trained to stimulate babies by gently rubbing their back or feet, and to provide PPV with a reusable resuscitator mask. Intervention birth attendants were also trained to recognise cardinal symptoms and signs of infection, and, if present, to administer oral amoxicillin and transfer to a hospital setting. They also received a laminated reference card summarising the neonatal resuscitation protocol and the trigger conditions for antibiotics with facilitated referral | |
| Outcomes | The primary outcome was the proportion of liveborn infants who died in the first 28 days after birth. Other outcomes included proportion of stillbirths, early neonatal death (< 1 week), late neonatal mortality from day 8 to 28 | |
| Notes | ICC was not available and hence ICC of 0.002 from the Carlo 2010a; Carlo 2010b study was used in the meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Public ceremony where birth attendant took a slip from a box to determine group assignment |
| Allocation concealment (selection bias) | Low risk | Not relevant as this was a cluster‐randomised trial and all randomisation occurred at 1 time point |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Possibility of overlap across rural areas |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Independently reviewed by 3 Boston neonatologists unaware of group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 98.3% contributed valid data |
| Selective reporting (reporting bias) | Low risk | All specified outcomes reported |
| Other bias | Low risk | No loss of clusters were reported, analyses was appropriate taking clustering into account and clusters were similar with no baseline imbalance |
Kaczorowski 1998.
| Methods | Randomised trial of 2 booster strategies designed to improve retention of skills and knowledge in neonatal resuscitation | |
| Participants | Family practice residents from a single institution | |
| Interventions | Boosters (video or 'hands on') vs. control. The video group reviewed a video of the NRP and were given the opportunity for unsupervised self directed mannequin practice 3‐5 months following original NRP training. The 'hands on' group received a 2‐hour supervised hands on mannequin practice 3‐5 months following original NRP. The control group received no booster sessions | |
| Outcomes | NRP written examination and observer assessment by checklists 6‐8 months following the original NRP course | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not clearly stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | 5 NRP instructors who were blinded to participants group membership |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 75% completed the study |
| Selective reporting (reporting bias) | Low risk | Not noted |
| Other bias | Unclear risk | Not noted |
Lee 2012.
| Methods | Randomised study | |
| Participants | Emergency medicine residents in their 2nd to 4th year | |
| Interventions | Neonatal resuscitation simulation scenario combined with an educational session vs. standard didactics | |
| Outcomes | Questionnaire regarding confidence in neonatal resuscitation and neonatal resuscitation scores | |
| Notes | 27 residents enrolled, 12 participants randomised to the intervention group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated assignment |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of intervention and control groups not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not explicitly stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants analysed |
| Selective reporting (reporting bias) | Low risk | Not noted |
| Other bias | Low risk | None noted |
Opiyo 2008.
| Methods | Randomised controlled trial to determine if a simple 1‐day NRT alters health worker resuscitation practices in a public hospital setting in Kenya | |
| Participants | Health workers receiving early training with NRT (28 workers) or late training (the control group, 55 workers) | |
| Interventions | The training was adapted locally from the resuscitation programme recommended by the UK Resuscitation Council | |
| Outcomes | The primary outcome was the proportion of appropriate initial resuscitation steps with the frequency of inappropriate practices and resuscitation mortality in the delivery room as secondary outcomes. Data were collected on 97 (intervention) and 115 (control) resuscitation episodes over 7 weeks after early training | |
| Notes | Controlled‐Trials.com ISRCTN92218092 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not specified |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded to the intervention or control group |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28 of the 32 providers in the intervention group and 55 of the 58 in the control group were observed |
| Selective reporting (reporting bias) | Unclear risk | Not clear |
| Other bias | Low risk | None noted |
Rubio‐Gurung 2014.
| Methods | A cluster‐randomised trial of maternity hospitals in France. The investigators aimed to determine whether in situ high‐fidelity simulation training (for ∼ 80% of the delivery room staff) improved neonatal resuscitation performed in the delivery room | |
| Participants | 12 maternity hospitals in France. A random sample of 10 professionals in each unit was presented with 2 standardised scenarios played on a neonatal high‐fidelity simulator | |
| Interventions | The 12 maternity hospitals were randomly assigned to receive the intervention (a 4‐hour simulation training session delivered in situ for multidisciplinary groups of 6 professionals) or not receive it. All maternity hospitals were evaluated again at 3 months after the intervention | |
| Outcomes | After intervention, the videos of resuscitation performance was assessed by 2 neonatologists and assigned a technical score. The frequency of achieving a heart rate > 90 beats/minute and number of hazardous events were also assessed | |
| Notes | In situ simulation study in France belonging to the AURORE perinatal network using mannequins | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed opaque envelopes randomised by an individual not involved in the study (? cluster‐randomised) |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not applicable |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | 2 blinded neonatologists performed the assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data reported |
| Selective reporting (reporting bias) | Unclear risk | All specified outcomes were reported |
| Other bias | High risk | Analyses was made at the participant level although the randomisation was performed at the maternity hospital level |
Thomas 2007.
| Methods | Randomised controlled trial | |
| Participants | Interns (paediatric, combined paediatric and internal medicine, family medicine and obstetrics and gynaecology) | |
| Interventions | Standard NRP compared to NRP with team training. The team training consisted of a 2.5‐hour session comprised of lectures, low‐fidelity simulation, short video clips and a question and answer period. They also received prompting during the NRP skills station to engage in team behaviours | |
| Outcomes | Teamwork behaviour consisting of inquiry, information sharing, assertion, evaluation of plans, workload management and vigilance | |
| Notes | Data acquired from the author for meta‐analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Not clear |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Performed on 2 separate floors. Instructors who interacted with the control group did not receive the teamwork curriculum |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Video recordings reviewed by independent assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 recordings were excluded due to technical issues. 80% follow‐up rate |
| Selective reporting (reporting bias) | Unclear risk | Not noted |
| Other bias | Low risk | Not noted |
Thomas 2010.
| Methods | Randomised trial | |
| Participants | Interns were non‐NRP certified admitted during the years 2007 and 2008 | |
| Interventions | 2‐hour teamwork training intervention with low‐fidelity, high‐fidelity NRP. Control participants practised low‐fidelity NRP without team training | |
| Outcomes | Teamwork behaviour: teamwork event rate, workload management and vigilance NRP performance: performance scores and duration of resuscitation |
|
| Notes | Data acquired from the author for meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Not clear |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding was not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Video recordings reviewed by assessors unaware of status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 90.7% follow‐up at 6 months |
| Selective reporting (reporting bias) | Low risk | Not noted |
| Other bias | Low risk | Not noted |
Xu 2014.
| Methods | Community‐based cluster‐randomised trial that evaluated an intervention package promoting effective neonatal resuscitation training at county level hospitals across China | |
| Participants | The study was conducted in Shandong and Heilongjiang, 2 eastern provinces of China. 8 counties (4 from each province) were randomly selected to participate in the study. Of those 8 counties, 2 counties from each province were randomly assigned to the intervention group. Intervention group: 11 hospitals and 97 healthcare providers and the control group consisted of 11 hospitals and 87 healthcare providers | |
| Interventions | The intervention package was implemented across 4 counties and the neonatal resuscitation programme was based on ILCOR guidelines that included the initial steps of resuscitation, physiology, PPV, intubation, CC and medication administration | |
| Outcomes | Incidence of birth asphyxia defined as Apgar scores ≤ 7 at 5 minutes, asphyxia‐related deaths in the delivery room and healthcare providers' knowledge and self confidence by questionnaires | |
| Notes | The definition of asphyxia in this study was different from our a priori definition | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not applicable |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcome assessment not clear |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition noted |
| Selective reporting (reporting bias) | Unclear risk | All specified outcomes were reported |
| Other bias | Unclear risk | No loss of clusters were reported and clusters were similar with no baseline imbalance but unit of analysis error noted |
ANTS: Anaesthetists' Non‐Technical Skills; CC: cardiac compression; CPR: cardiopulmonary resuscitation; FiO2: fraction of inspired oxygen; ICC: intracluster coefficient; ILCOR: International Liaison Committee on Resuscitation; NICHD: National Institute of Child Health and Human Development; NICU: neonatal intensive care unit; NRP: Neonatal Resuscitation Program; NRT: newborn resuscitation training; PPV: positive pressure ventilation; VLBW: very low birthweight.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ashish 2012 | Protocol for a pre‐post intervention study of Help Babies Breathe in Nepal |
| Boo 2009 | Observational and not a randomised study |
| Carlo 2010c | Not a randomised study. Pre‐post intervention study design |
| Cavaleiro 2009 | Participants were medical students and not healthcare providers |
| Chomba 2008 | Not a randomised study. WHO newborn care training that included neonatal resuscitation but was a pre‐ and post‐intervention study |
| Curran 2015 | Participants were medical students and not healthcare providers |
| Deindl 2015 | Not a randomised study and participants were 4th year medical students and not healthcare providers |
| Deorari 2001 | Not a randomised study. Pre‐ and post‐intervention study performed in 14 teaching hospitals in India |
| Duran 2008a | Not a randomised study. Assessed the impact of NRP in Turkey before and after NRP training |
| Duran 2008b | Not a randomised study. Pre‐ and post‐intervention study of retention of knowledge and skills related to NRP among paediatric trainees |
| Durojaiye 2002 | Not a randomised study. Pre‐ and post‐intervention study of the effect of a 1‐day paediatric life‐support course on the knowledge of paediatric trainees |
| Ergenekon 2000 | Not a randomised study. Pre‐ and post‐intervention study of trainees |
| Ersdal 2013 | Not a randomised trial. A 7‐month follow‐up of practical skills retention following course in Helping Babies Breathe |
| Finan 2012 | Comparison of high‐fidelity with low‐fidelity simulation on the impact of a neonatal resuscitation programme |
| Goudar 2013 | Not a randomised trial. A pre‐ and post‐intervention type study of Helping Babies Breathe |
| Hubballi 2014 | The participants are auxiliary nurse midwife students and not healthcare providers |
| López‐Herce 1999 | Not a randomised study. A pre‐ and post‐intervention study of participants evaluation of the course |
| Mathai 2015 | Not a randomised study. A prospective, comparative, observational study to determine the ease and effectiveness of training of healthcare personnel in use of the self inflating bag or the T‐piece resuscitator using infant training manikins |
| Msemo 2013 | Not a randomised trial. A pre‐ and post‐intervention study of Helping Babies Breathe |
| Nadler 2011 | Not a randomised study. Assessed the usefulness of video debriefings on teamwork in newborn resuscitation |
| Patel 2001 | Not a randomised study. Retrospective time cohort evaluation for changes in Apgar scores pre and post intervention with NRP |
| Patel 2002 | Not a randomised study. Retrospective evaluation in Apgar scores pre and post introduction of NRP |
| Senarath 2007 | A community‐based cluster‐randomised trial that did not report our pre‐specified outcomes |
| Singhal 2001 | Not a randomised study. Assessment of telephonic questionnaire on newborn resuscitation |
| Skidmore 2001 | Not a randomised study. Pre and post intervention and 6‐month retention of knowledge and skills study among birth room healthcare professionals |
| Tan 2014 | A non‐randomised study on quality of cardiac compressions in resuscitation trained neonatal staff |
| Trevisanuto 2005 | Not a randomised study. Questionnaire of knowledge related to NRP immediately and 6 months after NRP in paediatric residents |
| Trevisanuto 2007 | Not a randomised study. Questionnaire of knowledge related to NRP before and immediately after NRP, comparing cities in Italy and Sudan |
| Walker 2014 | A non‐randomised study with pair‐matched hospital‐based implementation trial of PRONTO (Programa de Rescate Obstetrico y Neonatal: Tratamiento optimo y Oportuno), a highly‐realistic, low‐tech simulation‐based obstetric and neonatal emergency training programme |
NRP: Neonatal Resuscitation Program; WHO: World Health Organization.
Characteristics of studies awaiting assessment [ordered by study ID]
Campbell 2014.
| Methods | Randomised study |
| Participants | Neonatal teams consisting of respiratory therapists, neonatal nurse and senior paediatric residents |
| Interventions | Video‐debriefing after simulated neonatal resuscitation |
| Outcomes | NRP scores and time to intubation. Attitudes and beliefs of participants regarding use of video debriefing and team behavioural skills |
| Notes | Data on the study and methodology requested from the investigators |
Yamada 2015.
| Methods | Randomised, prospective, cross‐over study evaluating the use of SCTs in decreasing errors during simulated neonatal resuscitation |
| Participants | 13 participants were recruited |
| Interventions | Participants performed as lead resuscitator in 2 simulated neonatal resuscitations. 2 confederates were trained to use or not use SCTs based on randomisation. Participants led 1 scenario in which confederates used non‐standard communication, and a second in which confederates used SCTs. Order of scenarios and communication methods were randomised. An NRP instructor blinded to group assignment reviewed each videotaped resuscitation |
| Outcomes | Primary outcome measures were: calculated per cent error rate, time to initiation of positive pressure ventilation and time to initiation of chest compressions |
| Notes | Data on the study and methodology requested from the investigators |
NRP: Neonatal Resuscitation Program; SCT: standardised communication technique.
Characteristics of ongoing studies [ordered by study ID]
Bang 2014.
| Trial name or title | Implementation and evaluation of the Helping Babies Breathe curriculum in 3 resource‐limited settings |
| Methods | 2‐year prospective pre‐post study to evaluate if a facility‐based training package, including HBB and essential newborn care, will reduce all perinatal mortality (fresh stillbirth or neonatal death prior to 7 days) among the Global Network's Maternal Neonatal Health Registry births > 1500 g in the study clusters served by the facilities. Will also evaluate the effectiveness of the HBB training programme changing on facility‐based perinatal mortality and resuscitation practices |
| Participants | 71 health facilities serving 52 geographically defined study clusters in Belgaum and Nagpur, India, and Eldoret, Kenya, and 30,000 women will be included |
| Interventions | HBB, a simulation‐training programme for babies wherever they are born, was developed for use in low‐to‐middle income countries. The intervention will be HBB training of facility birth attendants |
| Outcomes | Primary outcome data will be collected by staff not involved in the HBB intervention. Additional data on resuscitations, resuscitation debriefings, death audits, quality monitoring and improvement will be collected. HBB training will include training of master trainers, facility level birth attendants, and quality monitoring and improvement activities. This study will evaluate the effect of a HBB/ENC training and quality monitoring and improvement package on perinatal mortality using a large multicentre design and approach in 71 resource‐limited health facilities, leveraging an existing birth registry to provide neonatal outcomes through to day 7 |
| Starting date | |
| Contact information | |
| Notes | Trial registration ClinicalTrials.gov Identifier: NCT01681017 |
ENC: Early Newborn Care; HBB: Helping Babies Breathe.
Differences between protocol and review
Changes from protocol to review included the following post‐hoc analyses.
Inclusion of 28‐day mortality, mortality during initial hospitalisation and resuscitation duration as outcomes.
Inclusion of GRADE methodology in the Methods section for assessing quality of evidence.
Objectives in the protocol were split into primary objectives emphasising mortality and morbidity outcomes and secondary objectives focused on knowledge and skills acquisition and retention.
We modified our comparisons by adding, any SFNRT versus basic newborn care that may include some resuscitation training and additions to a formal course such as SFNRT (e.g. teamwork behaviour, boosters) versus SFNRT alone.
We deleted the following comparisons, didactic versus skill‐based programmes, simulation programme versus didactic programmes and simulation programme versus skill‐based programmes.
Contributions of authors
ED wrote the protocol and the review, identified articles for inclusion, extracted data, checked data with MP and collated comments from co‐authors.
MP assisted in writing the protocol and the review, identified articles for inclusion, extracted data, checked data with ED, entered the data in Review Manager 5 and analysed the data.
ACR commented and critiqued the review and comments were incorporated in the review.
KJB assisted in selection of studies for inclusion in the review, commented and critiqued the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Health Research Board, Ireland.
Dr. Dempsey received salary support to undertake this review
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA.
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN275201100016C
Declarations of interest
The authors have nothing to disclose.
New
References
References to studies included in this review
Bender 2014 {published data only}
- Bender J, Kennally K, Shields R, Overly F. Does simulation booster impact retention of resuscitation procedural skills and teamwork?. Journal of Perinatology 2014;34(9):664‐8. [DOI: 10.1038/jp.2014.72; PUBMED: 24762413] [DOI] [PubMed] [Google Scholar]
Bould 2009 {published data only}
- Bould MD, Hayter MA, Campbell DM, Chandra DB, Joo HS, Naik VN. Cognitive aid for neonatal resuscitation: a prospective single‐blinded randomized controlled trial. British Journal of Anaesthesia 2009;103(4):570‐5. [DOI] [PubMed] [Google Scholar]
Carlo 2010a {published data only}
- Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al for the First Breath Study Group. Newborn‐care training and perinatal mortality in developing countries. New England Journal of Medicine 2010;362(7):614‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goudar SS, Dhaded SM, McClure EM, Derman RJ, Patil VD, Mahantshetti NS, et al. ENC training reduces perinatal mortality in Karnataka, India. Journal of Maternal‐Fetal & Neonatal Medicine 2012;25(6):568‐74. [DOI] [PubMed] [Google Scholar]
- Matendo R, Engmann C, Ditekemena J, Gado J, Tshefu A, Kinoshita R, et al. Reduced perinatal mortality following enhanced training of birth attendants in the Democratic Republic of Congo: a time‐dependent effect. Biomed Central Medicine 2011;9:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlo 2010b {published data only}
- Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al for the First Breath Study Group. High mortality rates for very low birth weight infants in developing countries despite training. Pediatrics 2010;126(5):e1072‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunn 1992 {published data only}
- Dunn S, Niday P, Watters NE, McGrath P, Alcock D. The provision and evaluation of a neonatal resuscitation program. Journal of Continuing Education in Nursing 1992;23(3):118‐26. [DOI] [PubMed] [Google Scholar]
Fuerch 2015 {published data only}
- Fuerch JH, Yamada NK, Coelho PR, Lee HC, Halamek LP. Impact of a novel decision support tool on adherence to Neonatal Resuscitation Program algorithm. Resuscitation 2015;88:52‐6. [DOI] [PubMed] [Google Scholar]
Gill 2011 {published data only}
- Gill CJ, Phiri‐Mazala G, Guerina NG, Kasimba J, Mulenga C, MacLeod WB, et al. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): randomised controlled study. BMJ 2011;342:d346. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaczorowski 1998 {published data only}
- Kaczorowski J, Levitt C, Hammond M, Outerbridge E, Grad R, Rothman A, et al. Retention of neonatal resuscitation skills and knowledge: a randomized controlled trial. Family Medicine 1998;30(10):705‐11. [PubMed] [Google Scholar]
Lee 2012 {published data only}
- Lee M, Brown L, Bender J, Machan J, Overly F. A medical simulation‐based educational intervention for emergency medicine residents in neonatal resuscitation. Academic Emergency Medicine 2012;19:577‐85. [DOI] [PubMed] [Google Scholar]
Opiyo 2008 {published data only}
- Opiyo N, Were F, Govedi F, Fegan G, Wasunna A, English M. Effect of newborn resuscitation training on health worker practices in Pumwani Hospital, Kenya. PLoS One 2008;3(2):e1599. [DOI: 10.1371/journal.pone.0001599] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rubio‐Gurung 2014 {published data only}
- Rubio‐Gurung S, Putet G, Touzet S, Gauthier‐Moulinier H, Jordan I, Beissel A, et al. In situ simulation training for neonatal resuscitation: an RCT. Pediatrics 2014;134(3):e790‐7. [PUBMED: 25092937] [DOI] [PubMed] [Google Scholar]
Thomas 2007 {published data only}
- Thomas EJ, Taggart B, Crandell S, Lasky RE, Williams AL, Love LJ, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. Journal of Perinatology 2007;27(7):409‐14. [DOI] [PubMed] [Google Scholar]
Thomas 2010 {published data only}
- Thomas EJ, Williams AL, Reichman EF, Lasky RE, Crandell S, Taggart WR. Team training in the neonatal resuscitation program for interns: teamwork and quality of resuscitations. Pediatrics 2010;125(3):539‐46. [DOI] [PubMed] [Google Scholar]
Xu 2014 {published data only}
- Xu T, Wang H, Gong L, Ye H, Yu R, Wang D, et al. The impact of an intervention package promoting effective neonatal resuscitation training in rural China. Resuscitation 2014;85(2):253‐9. [AN: 2014062624 ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ashish 2012 {published data only}
- Ashish KC, Målqvist M, Wrammert J, Verma S, Aryal DR, Clark R, et al. Implementing a simplified neonatal resuscitation protocol‐helping babies breathe at birth (HBB) ‐ at a tertiary level hospital in Nepal for an increased perinatal survival. Biomed Central Pediatrics 2012;12:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boo 2009 {published data only}
- Boo NY. Neonatal resuscitation programme in Malaysia: an eight‐year experience. Singapore Medical Journal 2009;50(2):152‐9. [PubMed] [Google Scholar]
Carlo 2010c {published data only}
- Carlo WA, McClure EM, Chomba E, Chakraborty H, Hartwell T, Harris H, et al. Newborn care training of midwives and neonatal and perinatal mortality rates in a developing country. Pediatrics 2010;126(5):e1064‐71. [DOI] [PubMed] [Google Scholar]
Cavaleiro 2009 {published data only}
- Cavaleiro A, Guimaraes H, Calheiros F. Training neonatal skills with simulators?. Acta Paediatrica 2009;98(4):636‐9. [DOI] [PubMed] [Google Scholar]
Chomba 2008 {published data only}
- Chomba E, McClure EM, Wright LL, Carlo WA, Chakraborty H, Harris H. Effect of WHO newborn care training on neonatal mortality by education. Ambulatory Pediatrics 2008;8(5):300‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Curran 2015 {published data only}
- Curran V, Fleet L, White S, Bessell C, Deshpandey A, Drover A, et al. A randomized controlled study of manikin simulator fidelity on neonatal resuscitation program learning outcomes. Advances in Health Sciences Education: Theory and Practice 2015;20(1):205‐18. [DOI: 10.1007/s10459-014-9522-8; PUBMED: 24916954] [DOI] [PubMed] [Google Scholar]
Deindl 2015 {published data only}
- Deindl P, Schwindt J, Berger A, Schmolzer GM. An instructional video enhanced bag‐mask ventilation quality during simulated newborn resuscitation. Acta Paediatrica, International Journal of Paediatrics 2015;104(1):e20‐6. [AN: 2015643641 ] [DOI] [PubMed] [Google Scholar]
Deorari 2001 {published data only}
- Deorari AK, Paul VK, Singh M, Vidyasagar D. Impact of education and training on neonatal resuscitation practices in 14 teaching hospitals in India. Annals of Tropical Paediatrics 2001;21(1):29‐33. [PubMed] [Google Scholar]
Duran 2008a {published data only}
- Duran R, Aladag N, Vatansever U, Sut N, Acunas B. The impact of Neonatal Resuscitation Program courses on mortality and morbidity of newborn infants with perinatal asphyxia. Brain & Development 2008;30(1):43‐6. [DOI] [PubMed] [Google Scholar]
Duran 2008b {published data only}
- Duran R, Aladag N, Vatansever U, Kucukugurluoglu Y, Sut N, Acunas B. Proficiency and knowledge gained and retained by pediatric residents after neonatal resuscitation course. Pediatrics International 2008;50(5):644‐7. [DOI] [PubMed] [Google Scholar]
Durojaiye 2002 {published data only}
- Durojaiye L, O'Meara M. Improvement in resuscitation knowledge after a one‐day paediatric life‐support course. Journal of Paediatrics and Child Health 2002;38(3):241‐5. [DOI] [PubMed] [Google Scholar]
Ergenekon 2000 {published data only}
- Ergenekon E, Koc E, Atalay Y, Soysal S. Neonatal resuscitation course experience in Turkey. Resuscitation 2000;45(3):225‐7. [DOI] [PubMed] [Google Scholar]
Ersdal 2013 {published data only}
- Ersdal HL, Vossius C, Bayo E, Mduma E, Perlman J, Lippert A, et al. A one‐day "Helping Babies Breathe" course improves simulated performance but not clinical management of neonates. Resuscitation 2013;84(10):1422‐7. [DOI] [PubMed] [Google Scholar]
Finan 2012 {published data only}
- Finan E, Bismilla Z, Whyte H, LeBlanc V, McNamara P. High‐fidelity simulator technology may not be superior to traditional low‐fidelity equipment for neonatal resuscitation training. Journal of Perinatology 2012;32(4):287‐92. [DOI] [PubMed] [Google Scholar]
Goudar 2013 {published data only}
- Goudar SS, Somannavar MS, Clark R, Lockyer JM, Revankar AP, Fidler HM, et al. Stillbirth and newborn mortality in India after helping babies breathe training. Pediatrics 2013;131(2):e344‐52. [DOI] [PubMed] [Google Scholar]
Hubballi 2014 {published data only}
- Hubballi JG, Sumitra LA, Raddi SA. Randomized control trial to evaluate the effectiveness of Helping Babies Breathe Programme on knowledge and skills regarding neonatal resuscitation among auxiliary nurse midwives students. International Journal of Nursing Education 2014;6(1):146‐51. [DOI: ] [Google Scholar]
López‐Herce 1999 {published data only}
- López‐Herce J, Carrillo A, Rodriguez A, Calvo C, Delgado MA, Tormo C. Paediatric life support instructors courses in Spain. Spanish Paediatric and Neonatal Resuscitation Group. Resuscitation 1999;41(2):205‐9. [PubMed] [Google Scholar]
Mathai 2015 {published data only}
- Mathai SS, Adhikari KM, Rajeev A. Comparison of training in neonatal resuscitation using self inflating bag and T‐piece resuscitator. Medical Journal Armed Forces India 2015;71(1):19‐23. [AN: 2014707774 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Msemo 2013 {published data only}
- Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics 2013;131(2):e353‐60. [DOI] [PubMed] [Google Scholar]
Nadler 2011 {published data only}
- Nadler I, Sanderson PM, Dyken CR, Davis PG, Liley HG. Presenting video recordings of newborn resuscitations in debriefings for teamwork training. British Medical Journal Quality & Safety 2011;20(2):163‐9. [DOI] [PubMed] [Google Scholar]
Patel 2001 {published data only}
- Patel D, Piotrowski ZH, Nelson MR, Sabich R. Effect of a statewide neonatal resuscitation training program on Apgar scores among high‐risk neonates in Illinois. Pediatrics 2001;107(4):648‐55. [DOI] [PubMed] [Google Scholar]
Patel 2002 {published data only}
- Patel D, Piotrowski ZH. Positive changes among very low birth weight infant Apgar scores that are associated with the Neonatal Resuscitation Program in Illinois. Journal of Perinatology 2002;22(5):386‐90. [DOI] [PubMed] [Google Scholar]
Senarath 2007 {published data only}
- Senarath U, Fernando DN, Rodrigo I. Effect of training for care providers on practice of essential newborn care in hospitals in Sri Lanka. Journal of Obstetric Gynecologic & Neonatal Nursing 2007;36:531‐41. [DOI] [PubMed] [Google Scholar]
Singhal 2001 {published data only}
- Singhal N, McMillan DD, Yee WH, Akierman AR, Yee YJ. Evaluation of the effectiveness of the standardized neonatal resuscitation program. Journal of Perinatology 2001;21(6):388‐92. [DOI] [PubMed] [Google Scholar]
Skidmore 2001 {published data only}
- Skidmore MB, Urquhart H. Retention of skills in neonatal resuscitation. Paediatrics & Child Health 2001;6(1):31‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tan 2014 {published data only}
- Tan S, Batey N, Sharkey D. Cardiac compression quality deteriorates with increasing compression rate during preterm resuscitation simulations: a new preterm simulation trainer. Archives of Disease in Childhood 2014;99:A71. [AN: 71666433 ] [Google Scholar]
Trevisanuto 2005 {published data only}
- Trevisanuto D, Ferrarese P, Cavicchioli P, Fasson A, Zanardo V, Zacchello F. Knowledge gained by pediatric residents after neonatal resuscitation program courses. Paediatric Anaesthesia 2005;15(11):944‐7. [DOI] [PubMed] [Google Scholar]
Trevisanuto 2007 {published data only}
- Trevisanuto D, Ibrahim SA, Doglioni N, Salvadori S, Ferrarese P, Zanardo V. Neonatal resuscitation courses for pediatric residents: comparison between Khartoum (Sudan) and Padova (Italy). Paediatric Anaesthesia 2007;17(1):28‐31. [DOI] [PubMed] [Google Scholar]
Walker 2014 {published data only}
- Walker D, Cohen S, Fritz J, Olvera M, Lamadrid‐Figueroa H, Cowan JG, et al. Team training in obstetric and neonatal emergencies using highly realistic simulation in Mexico: impact on process indicators. BMC Pregnancy and Childbirth 2014;14(1):367. [AN 2015808130] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Campbell 2014 {published data only}
- Campbell DM, Finan E. Impact of video‐debriefing following simulated neonatal resuscitation in inter‐professional teams. Paediatrics and Child Health (Canada) 2014;19:e88. [AN: 71621217] [Google Scholar]
Yamada 2015 {published data only}
- Yamada NK, Fuerch JH, Halamek LP. Impact of standardized communication techniques on errors during simulated neonatal resuscitation. Journal of Investigative Medicine 2015;66:99‐100. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Bang 2014 {published data only}
- Bang A, Bellad R, Gisore P, Hibberd P, Patel A, Goudar S, et al. Implementation and evaluation of the Helping Babies Breathe curriculum in three resource limited settings: does Helping Babies Breathe save lives? A study protocol. BMC Pregnancy and Childbirth 2014;14(1):116. [AN: 2014284423] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
AHA 2000
- American Heart Association and International Liaison Committee on Resuscitation. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Part 11: neonatal resuscitation. Circulation 2000;102(8 Suppl):I343‐57. [PubMed] [Google Scholar]
Bell 2008
- Bell DS, Harless CE, Higa JK, Bjork EL, Bjork RA, Bazargan M, et al. Knowledge retention after an online tutorial: a randomized educational experiment among resident physicians. Journal of General Internal Medicine 2008;23(8):1164‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chance 1987
- Chance GW, Hanvey L. Neonatal resuscitation in Canadian hospitals. Canadian Medical Association Journal 1987;136(6):601‐6. [PMC free article] [PubMed] [Google Scholar]
Cleary 1998
- Cleary GM, Wiswell TE. Meconium‐stained amniotic fluid and the meconium aspiration syndrome. An update. Pediatric Clinics of North America 1998;45(3):511‐29. [DOI] [PubMed] [Google Scholar]
de Almeida 2014
- Almeida M, Guinsburg R, Sancho G, Rosa I, Lamy Z, Martinez F, et al. Hypothermia and early neonatal mortality in preterm infants. Journal of Pediatrics 2014;164(2):271‐5. [DOI] [PubMed] [Google Scholar]
Estol 1992
- Estol PC, Piriz H, Basalo S, Simini F, Grela C. Oro‐naso‐pharyngeal suction at birth: effects on respiratory adaptation of normal term vaginally born infants. Journal of Perinatal Medicine 1992;20(4):297‐305. [DOI] [PubMed] [Google Scholar]
Goudar 2012
- Goudar SS, Dhaded SM, McClure EM, Derman RJ, Patil VD, Mahantshetti NS, et al. ENC training reduces perinatal mortality in Karnataka, India. Journal of Maternal‐Fetal & Neonatal Medicine 2012;25(6):568‐74. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
ILCOR 2006
- International Liaison Committee on Resuscitation. The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics 2006;117(5):e978‐88. [DOI] [PubMed] [Google Scholar]
IMF 2012
- International Monetary Fund. Gross domestic product, current prices & gross domestic product based on purchasing‐power‐parity (PPP) valuation of country GD. World Economic Outlook Database. April 2012.
Jabbour 1996
- Jabbour M, Osmond MH, Klassen TP. Life support courses: are they effective?. Annals of Emergency Medicine 1996;28(6):690‐8. [DOI] [PubMed] [Google Scholar]
Knippenberg 2005
- Knippenberg R, Lawn JE, Darmstadt GL, Begkoyian G, Fogstad H, Walelign N, et al for the Lancet Neonatal Survival Steering Team. Systematic scaling up of neonatal care in countries. Lancet 2005;365(9464):1087‐98. [DOI] [PubMed] [Google Scholar]
Lawn 2005
- Lawn J, Cousens S, Zupan J. 4 million neonatal deaths: when? where? why?. Lancet 2005;365:891‐900. [DOI] [PubMed] [Google Scholar]
Lee 2011
- Lee AC, Cousens S, Wall SN, Niermeyer S, Darmstadt GL, Carlo WA, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta‐analysis and Delphi estimation of mortality effect. Biomed Central Public Health 2011;11(Suppl 3):S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Matendo 2011
- Matendo R, Engmann C, Ditekemena J, Gado J, Tshefu A, Kinoshita R, et al. Reduced perinatal mortality following enhanced training of birth attendants in the Democratic Republic of Congo: a time‐dependent effect. Biomed Central Medicine 2011;9:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meaney 2010
- Meaney PA, Topjian AA, Chandler HK, Botha M, Soar J, Berg RA, et al. Resuscitation training in developing countries: a systematic review. Resuscitation 2010;81(11):1462‐72. [DOI] [PubMed] [Google Scholar]
Mileder 2014
- Mileder LP, Urlesberger B, Szyld EG, Roehr CC, Schmölzer GM. Simulation‐based neonatal and infant resuscitation teaching: a systematic review of randomized controlled trials. Klinische Pädiatrie 2014;226(5):259‐67. [DOI: 10.1055/s-0034-1372621; PUBMED: 25153910] [DOI] [PubMed] [Google Scholar]
Narayanan 2004
- Narayanan I, Rose M, Cordero D, Faillace S, Sanghvian T. The Components of Essential Newborn Care. Published by Basics Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development. Arlington, Virginia. 2004.
Opiyo 2010
- Opiyo N, English M. In‐service training for health professionals to improve care of the seriously ill newborn or child in low and middle‐income countries (Review). Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD007071.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Shankaran 2005
- Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole‐body hypothermia for neonates with hypoxic‐ischemic encephalopathy. New England Journal of Medicine 2005;353(15):1574‐84. [DOI] [PubMed] [Google Scholar]
Vain 2004
- Vain NE, Szyld EG, Prudent LM, Wiswell TE, Aguilar AM, Vivas NI. Oropharyngeal and nasopharyngeal suctioning of meconium‐stained neonates before delivery of their shoulders: multicentre, randomised controlled trial. Lancet 2004;364(9434):597‐602. [DOI] [PubMed] [Google Scholar]
Wax 2010
- Wax JR, Lucas FL, Lamont M, Pinette MG, Cartin A, Blackstone J. Maternal and newborn outcomes in planned home birth vs planned hospital births: a meta‐analysis. American Journal of Obstetrics and Gynecology 2010;203(3):243.e1‐8. [DOI] [PubMed] [Google Scholar]
Wiswell 2000
- Wiswell TE, Gannon CM, Jacob J, Goldsmith L, Szyld E, Weiss K, et al. Delivery room management of the apparently vigorous meconium‐stained neonate: results of the multicenter, international collaborative trial. Pediatrics 2000;105(1 Pt 1):1‐7. [DOI] [PubMed] [Google Scholar]


