Abstract
Background
Informal primary caregivers provide crucial supports to loved ones experiencing serious mental illnesses with profound outcomes for the caregivers themselves. A comprehensive understanding of how different serious mental illnesses change the caregiving experience may provide important insight into the ways in which caregivers can be better supported in their role. The aim of this review was to synthesize the comparative literature examining caregiver burden and psychological functioning (anxiety, depression, distress, and psychological wellbeing) between caregivers of people with schizophrenia spectrum disorders and bipolar disorder.
Methods
Studies were included if they compared caregivers across both diagnostic groups and used measures assessing either caregiver burden or psychological functioning of caregivers. Databases searched up until 11th of January 2022 included: Medline COMPLETE, Embase, PsycINFO and CINAHL. Reference list scans and grey literature searches across government, organisational and dissertation databases were also conducted.
Results
Twenty-eight studies comprising 6166 caregivers were included. Fourteen studies suggested that caregiving burden was comparable across both groups. The effects of caring on caregiver mental health and stress were comparable across both groups. However, methodological limitations were noted, including a reliance on cross-sectional studies, multiple and sometimes competing definitions of caregiving burden, variable sample sizes, and variation in measures used.
Conclusion and implications
The experience of providing care is multidimensional and complex. Symptoms and functional difficulties experienced by people being cared for may affect caregivers more so than diagnosis. Caregivers play a vital role in helping people with serious mental illness. Supporting caregivers by reducing their burden and improving their psychological functioning may help them to continue to provide support, and cope with, the challenges of providing care.
Keywords: Caregiver, Caregiver burden, Bipolar disorder, Schizophrenia Spectrum disorders, Mental health
Introduction
Serious mental illnesses (SMI), such as schizophrenia spectrum disorders and bipolar disorder, incur significant functional impairments [1, 2], increase the likelihood of disability [3, 4], and shorten life expectancies [5]. The severity and chronicity of SMI results in associated care costs of $56.7 billion to the Australian healthcare system [6]. Personal costs associated with supporting individuals with SMI are often experienced by informal primary caregivers (hereafter referred to as ‘caregivers’), who are family members, spouses, friends, or close others who provide primary support [7]. Caregivers assist with emotional support, daily living, finances, behavioural management, liaising with professionals, and functional recovery [8]. The global move away from institutionalization and greater reliance on caregiver supports has resulted in better outcomes for individuals with SMI in terms of symptomatology and quality of life [9]. However, the increasing reliance on caregivers, whose role has an approximate annual economic value of $13.2 billion in the Australian mental health system [10], has profound impacts on caregivers themselves. These impacts have often been considered with relation to caregivers of those with medical conditions such as cancer or dementia [11–13]. However, increasing focus has been placed upon caregivers of those with SMI, and several outcomes of caring have been investigated, with caregiving duties negatively associated with caregiver physical health [14], financial burden [15], rates of employment [9] and quality of life [16, 17].
Caregiver burden, or the difficulties experienced in providing care, is one outcome frequently examined [18]. There exist several conceptualisations of caregiver burden, however the most common terms are objective and subjective burden [19]. Objective burden represents observable and verifiable disruptions from providing care, whereas subjective burden represents personal feelings of burden [20]. As caregiver burden encompasses several difficulties of providing care, the psychological functioning of caregivers has also been considered.
Psychological functioning, or the ability of individuals to achieve their aspirations in their external environment [21], includes mental health difficulties caregivers may experience, like anxiety, depression and caregiver distress. Anxiety and depression are typically assessed by symptoms such as worried thoughts, feelings of worthlessness, diminished interest in daily activities, and disruptions to sleep and energy [22]. Caregiver distress represents emotional suffering, characterised as loss, hopelessness or restlessness, in response to specific stressors that affect caregivers [23, 24]. Psychological wellbeing, a component of psychological functioning, is a concept that has seldom been considered in caregivers. It can be divided into hedonic and eudaimonic wellbeing. Hedonic wellbeing represents feelings of short-term happiness and positive emotions [25], whereas eudaimonic wellbeing refers to one’s life purpose and self-acceptance [26]. Given the vital role of caregivers, considering their psychological functioning from this multidimensional perspective can inform the available supports caregivers require while caring for loved ones with SMI.
Most research of SMI has involved examinations of caregiver burden and psychological functioning for caregivers of those with schizophrenia spectrum disorders, and more specifically, chronic schizophrenia [16]. This is understandable, given schizophrenia spectrum disorders are defined by significantly impactful positive symptoms, such as hallucinations and delusions, alongside significantly impactful and often persistent negative symptoms, including social withdrawal [22]. Individuals with these disorders are at greater risk of poorer outcomes, including early mortality in comparison to the general population [27]. Caregivers of those with schizophrenia have reported high subjective burden [28], and the severity of positive psychotic symptoms has been associated with significant objective burden relating to financial demands, increase in family conflicts and mental health difficulties [29], and decreases in life satisfaction [8]. However, focusing on caregivers of those with chronic schizophrenia limits the generalisability of findings for caregivers of those with other diagnoses of SMI and at earlier stages of caregiving. SMI diagnoses may be associated with differential experiences of caregiving due to differences in symptoms and associated impacts, whereas the stage of diagnosis may reflect differences in the caregiver’s adjustment and appraisal of their loved one’s illness. By understanding whether differential outcomes exist, the treatments and supports for caregivers can be specified to reflect the circumstances of their caring role. In doing so, this may benefit caregivers more so than a generalized approach to caregiver supports. Additionally, the focus on negative caregiver outcomes means there has been lesser focus on the psychological wellbeing of caregivers. This field of literature is growing [30, 31]. However, further research is necessary in considering the potential for positive growth and improved wellbeing in association with providing care. These factors may help reduce the level of burden and mental health difficulties reported by caregivers.
A growing number of studies have compared how different SMIs affect caregiving, particularly for caregivers of those with bipolar disorder [32–34]. Bipolar disorder contrasts from schizophrenia spectrum disorders as it is characterized by symptoms that reflect significant shifts an individual’s energy, mood and activity [22]. All-cause mortality rates, representing death by any cause, in populations diagnosed with bipolar disorder is double the rate found within the general population [35]. While bipolar disorder presents with differing symptoms to schizophrenia, the rates of mortality between both disorders have been found to be similar [36]. Caregivers of those with bipolar disorder report severe burden and heightened anxiety, depression and distress during their caregiving experience [37, 38]. The literature for caregivers of those with bipolar disorder presents with similar limitations to that of the literature for caregivers of those with schizophrenia – primarily, the focus on chronic presentations and relative paucity of psychological wellbeing literature. Despite these limitations, the burden and mental health difficulties that caregivers for those with bipolar disorder experience has often been likened to that of caregivers for those with schizophrenia [39, 40]. These disorders, however, present with differential illness trajectories and symptom profiles [22]. It is possible that caregivers may encounter unique challenges given these diagnostic differences, and several studies have moved to compare whether caregiving outcomes are influenced by diagnosis.
To date, there has been no comprehensive review of these comparative studies to determine whether a clear indicator of how diagnosis may influence caregiving outcomes exists. Prior systematic reviews have examined the impact of schizophrenia [8, 41] and bipolar disorder [42, 43] on caregiver outcomes separately, and others have examined the multidimensional impact of SMI as a broad categorization on family members [44, 45]. None have directly examined the comparative literature to determine whether specific disorder characteristics differentiate caregiver experiences. This review will contribute to the understanding of how disorder characteristics are associated with caregiving, which can help determine optimal support options in facilitating caregiver wellbeing and allowing caregivers to continue providing essential supports.
The aim of this systematic review was to address this gap in the literature and determine whether different diagnostic groups influence the outcomes of caregiving on caregivers. Specifically, we wanted to determine whether caregivers of individuals with schizophrenia spectrum disorders differ from caregivers of individuals with bipolar disorder with respect to:
-
(i)
caregiver burden
-
(ii)
mental health outcomes, encompassing anxiety, depression, and caregiver distress
-
(iii)
psychological wellbeing
Method
Protocol
The review protocol was registered and is accessible on The International Prospective Register of Systematic Reviews (PROSPERO; Protocol ID CRD42019120815).
Inclusion and exclusion criteria
Studies were included in the review if they met the following criteria:
Published from January 1st, 1900 to January 11th, 2022;
Presented quantitative data comparing caregiving outcomes between caregivers of individuals with schizophrenia spectrum disorders and bipolar disorder;
Included samples of caregivers as per criteria specified by Pollak and Perlick [7]. That is, family members satisfying three of the following criteria, or non-family members satisfying two of the following criteria: i) is a spouse (or equivalent), parent, sibling, or close other; ii) has the most frequent contact with the individual; iii) helps to support the individual financially; iv) has most frequently been a collateral in the individual’s treatment, and v) is contacted by treatment staff in case of emergency;
- Included a measure of caregiver burden or psychological functioning (mental health outcomes of caring or psychological wellbeing):
To ensure saturation of literature, numerous study design types were considered, including observational studies, prospective and retrospective cohort studies, case-control, cross-sectional, and descriptive studies. Baseline data from randomised controlled trials (RCT) comparing caregiving burden or psychological functioning were also considered.
Exclusion criteria
Studies were excluded if they only contained qualitative data and/or were not in English.
Identification and selection of studies
Comprehensive literature searches were conducted across electronic databases including MEDLINE Complete, Embase, PsycINFO and CINAHL. Terms and synonyms related to the caring role (i.e., caregiver, carer, support, caring), caring outcomes (i.e., burden, distress), individuals who may be caregivers (i.e., family, parent, sibling, relatives, spouses, partners, grandparents, children, guardian), bipolar disorder (i.e., bipolar I, bipolar II, mania, bipolar affective disorder, manic episode, manic depression), and schizophrenia spectrum disorders (i.e., schizophrenia, psychosis, psychotic, schizophreniform, schizoaffective, delusional disorder) were used (a full electronic search strategy is available upon request). Medical subject headings and controlled vocabularies were applied across all databases. An initial search was conducted on 1st of July 2019 and a final updated search on January 11th, 2022. Authors of articles were contacted where further information was required. Searches for unpublished or non-commercial documents (grey literature) with quantitative data were conducted across the Australian Bureau of Statistics, Australian Institute of Family Studies, Australia Institute of Health and Wellbeing, Analysis and Policy Observatory, Carers Australia, Deakin Library Catalogue (Dissertations), PsycEXTRA, TROVE and Web of Science (Dissertations). Variations of the primary search strategy were implemented depending on the search functionalities of each database. Consistency across databases was maintained by using the search terms focused on “caregivers”, “bipolar disorder” and “schizophrenia”.
Study selection
All search results were examined using Covidence Systematic Review Management tool [46]. Two authors (GK & AJ) independently conducted duplicate screening. Title and abstracts of each article were independently screened to determine full-text eligibility. All reasons for excluding articles were noted. Full-text screening of included articles was again independently conducted by GK & AJ. To ensure literature saturation, the reference list of all articles included in the final systematic review were scanned for additional studies.
Data extraction
Authors (GJK and AJ) conducted independent data extraction for all studies included. A data extraction template was developed based on the Cochrane Consumers and Communication Data Extraction Template for Included Studies [47]. Data on study characteristics were extracted, including author and date of publication, location and setting of study, reported conflict of interests, study design, statistical methods for analysis, sample size, inclusion and exclusion criteria, psychometric properties of outcome measures, key findings, and limitations. Baseline caregiver characteristics including gender, caregiver age, employment and marital status, relationship to individual and level of education were obtained.
Evaluation of methodological quality and risk of bias
Risk of bias was assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [48] and recommendations from the Joanna Briggs Institute [49]. Authors (GJK & AJ) independently assessed all included studies in the final review. Disputes regarding the methodological quality of articles were resolved via author discussion.
Synthesis of results
Narrative synthesis was used to summarise and explain key findings both within and between studies included. Aggregate data and key findings were summarised in tables to include study and sample characteristics, measures used, and key results. The conduct of this review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA [50];) and the Synthesis without Meta-Analysis in Systematic Reviews guidelines (SWiM [51];).
Results
Literature search strategy
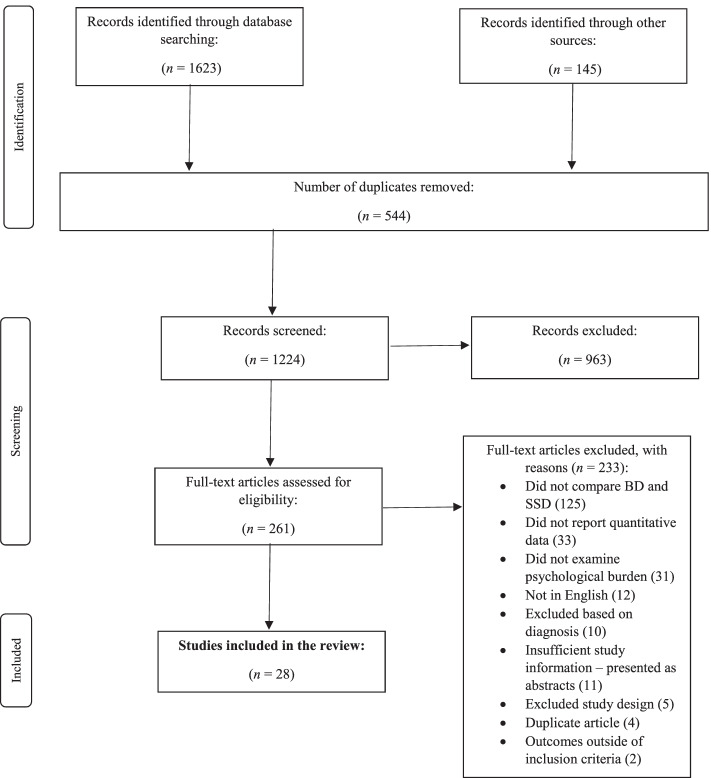
The literature search processes are summarised in Fig. 1. Twenty-eight studies met criteria for full-text inclusion.
Fig. 1.
Flow Diagram of The Study Selection Process
Study characteristics
Twenty-five (89.3%) studies were cross-sectional (see Table 1). Recruitment sites included psychiatric hospitals (50%, n = 14), university teaching settings (17.8%, n = 5), outpatient mental health settings (28.6%, n = 8), a transit home (3.6%, n = 1), and an unspecified source (3.6%, n = 1). Studies were conducted in Asia (57.1%, n = 16), Africa (17.9%, n = 5), the Americas (10.7%, n = 3), Europe (10.7%, n = 3), and the Middle East (3.6%, n = 1).
Table 1.
Summary of twenty-eight studies included in this review
| Study ID and Authors | Country & Setting | Study Design | Caregiving domains measured | t-test, p and Cohen’s d derived from M(SD) of SSD and BD comparisons | Key Findings |
|---|---|---|---|---|---|
| 1. Blanthorn-Hazell et al. [52] | Germany, Spain & UK, community mental health | Cross-sectional | Burden | t(240) = 0.30, p = .764, d = 0.04 | - Caring for those with either SCZ or BD with agitation confers substantial and similar burden. |
| 2. Chadda et al. [53] | India, psychiatric outpatient clinic | Prospective cohort | Burden | t(198) = 0.78, p = .437, d = 0.11 | - Both caregiver groups experienced similar levels of burden, with no significant differences between caregiving groups. |
| 3. Chakrabarti and Gill [54] | India, psychiatric hospital | Cross-sectional | Burden | t(56) = 3.42, p < .01, d = 0.88 | - Total burden scores were significantly greater for caregivers of those with SCZ than BD. |
| 4. Chakrabarti et al. [55] | India | Cross-sectional/ psychometric validation | Distress | Information not available | - There were no differences in distress between caregivers of those with SCZ and BD. |
| 5. Chang et al. [56] | Taiwan, four hospitals | Cross-sectional | Burden, Depression, Anxiety |
No total burden score available Depression Total Score t(298) = 0.98, p = .326, d = 0.12 Anxiety Total Score t(298) = 0.72, p = .470, d = 0.09 |
- There were no significant differences in burden experienced between both caregiver groups. - No significant differences between groups on measures of depression and anxiety. |
| 6. Chien et al. [57] | Hong Kong & China, two psychiatric outpatient clinics | Cross-sectional/ psychometric validation | Burden | t(128) = 0.40, p = .690, d = 0.11 | - Level of family burden was not statistically significant between caregiver groups. |
| 7. Fekih-Romdhane et al. [58] | Tunisia, psychiatric hospital | Cross-sectional | Burden | t(43) = 1.99, p = .053, d = 0.61 | - No significant differences in burden experienced between caregivers based on diagnosis. |
| 8. Grover et al. [59] | India, tertiary-care teaching hospital | Cross-sectional | Burden, Distress |
Total Burden score t(138) = 2.92, p < .01, d = 0.49 Distress comparison data not available |
- Overall negative caregiving experience was higher in SCZ group compared to BD. - Positive personal caregiver experience was significantly higher in caregivers of those with SCZ compared to BD. - No significant differences between caregivers on measure of psychological distress. |
| 9. Grover et al. [60] | India, psychiatry outpatient clinic | Cross-sectional | Burden | Information not available |
- Caregivers of those with SCZ had significantly higher moderate to severe objective burden compared to caregivers of those with BD. - Caregivers of those with BD has significantly higher subjective burden compared to caregivers of those with SCZ. |
| 10. Grover et al. [61] | India, psychiatry hospital | Cross-sectional | Burden |
Objective Burden Score t(98) = 1.63, p = .107, d = 0.33 Subjective Burden Score t(98) = 3.67, p < .001, d = 0.74 |
- Caregivers in SCZ group had significantly higher objective burden, subjective burden, and disruption to routines. |
| 11. Grover et al. [62] | India, 14 national mental health centres | Cross-sectional | Distress | t(1049) = 1.28, p = .200, d = 0.09 | - Caregivers of those with SCZ had significantly higher distress compared to caregivers of individuals with BD. |
| 12. Ak et al. [63] | Turkey, inpatient psychiatric unit | Cross-sectional | Burden | Information not available | - Caregiving burden was high across both groups, but no statistical difference was found. |
| 13. Nehra et al. [64] | India, hospital | Cross-sectional | Burden |
Total Objective Burden Score t(98) = 0.97, p = .334, d = 0.19 |
- All differences were non-significant between the two groups. |
| 14. Ramírez et al. [65] | Colombia, Mood Disorders and Psychosis Clinic | Randomized-controlled trial | Burden | Information not available | - When comparing scores between the BD and schizophrenia groups, no statistically significant differences were found. |
| 15. Rodrigo et al. [66] | Sri Lanka, psychiatric hospital unit | Prospective cohort and cross-sectional | Burden, Depression | Information not available | - No significant differences between groups based on individual diagnosis were found on measures of burden and depression. |
| 16. Roychaudhuri et al. [67] | Nigeria, psychiatric teaching hospital | Cross-sectional | Burden |
Total Objective Burden Score t(52) = 0.73, p = .467, d = 0.20 Subjective Positive Appraisal t(52) = 1.65, p = .104, d = 0.45 Subjective Negative Appraisal t(52) = 2.23, p < .05, d = 0.62 |
- Statistically significant differences between caregivers of those with SSD and BD were only observed in subjective negative burden domain. |
| 17. Sharma et al. [68] | Nepal, psychiatric inpatient unit | Cross-sectional |
Burden, Depression, Anxiety |
Burden Total Score t(98) = 0.48, p = .632, d = 0.09 Depression Total Score t(98) = 0.57, p = .572, d = 0.11 Anxiety Total Score t(52) = 0.67, p = .504, d = 0.13 |
- There were no statistically significant differences on burden, depression and anxiety based on individual diagnosis alone. - Spouses of individuals with SCZ had significantly higher stress levels than spouses of individuals with BD. |
| 18. Singh and Prajapati [69] | Nepal, transit home | Cross-sectional | Burden | Information not available | - Moderate caregiving burden was statistically higher in caregivers of those with SCZ compared to caregivers of those with BD. |
| 19. Vasudeva et al. [70] | India, tertiary care hospital | Cross-sectional | Burden | t(101) = 2.15, p < .05, d = 0.42 | - Both caregiver groups experience considerable burden, but global burden in caregivers of those with SCZ was significantly higher than in BD group. |
| 20. Webb et al. [71] | USA, hospital inpatient and outpatient programs | Cross-sectional | Burden, Psychological wellbeing |
Total Burden Score t(82) = 1.45, p = .151, d = 0.33 Total Wellbeing Score t(82) = 1.97, p = .052, d = 0.17 |
- No significant differences related to diagnosis of individual were found. |
| 21. Zendjidjian et al. [72] | France, psychiatric hospital unit | Cross-sectional | Mental Health |
Mental Health Composite Score t(359) = 2.23, p < .05, d = 0.24 |
- Caregivers of individuals with SCZ reported significantly lower mental health outcome scores compared to caregivers of those with BD. |
| 22. Zhou et al. [73] | China, nine psychiatric units | Cross-sectional |
Burden, Depression, Anxiety |
Information not available | - Caregivers of those with BD reported greater burden, regarding violent and suicidal behaviours from individuals, compared to caregivers of those with SCZ. |
| 23. Abdeta and Desalegn [74] | Ethiopia, university hospital | Cross-sectional | Presence of common mental disorders | Information not available | - No significant differences were noted in the percentage of caregivers presenting with common mental disorders (anxiety and depression). |
| 24. Cohen et al. [75] | Brazil, outpatient teaching hospital | Cross-sectional | Mental health, Depression, Psychological outcomes |
Mental Health Composite score t(123) = 0.97, p = 0.332, d = 0.17 Psychological Outcomes score t(123) = 1.02, p = 0.311, d = 0.18 Total Depression score t(123) = 2.92, p < 0.01, d = 0.52 |
- Caregivers of individuals with SCZ had significantly higher depressive symptoms compared to caregivers of those BD. - No significant differences were observed on the mental health and psychological outcome scores between caregiver groups. |
| 25. Ukpong and Ibigbami [76] | Nigeria, outpatient psychiatric clinics | Cross-sectional | Burden, Depression, Anxiety, Psychological outcomes |
Total Burden score t(198) = 5.19, p > 0.001, d = 0.73 Total Anxiety score t(198) = − 0.17, p = 0.867, d = 0.02 Total Depression score t(198) = 3.25, p < 0.001, d = 0.46 Total Psychological outcomes score t(198) = 2.62, p < 0.01, d = 0.37 |
- Burden was significantly higher in caregivers of individuals with SCZ compared to caregivers of those with BD. - Caregivers did not significantly differ in anxiety experienced. - Caregivers of those with BD reported significantly higher depression scores than caregivers of those with SCZ. - Caregivers of those with SCZ reported significantly lower psychological outcome scores compared to caregivers of those with BD. |
| 26. Udoh et al. [77] | Nigeria, neuropsychiatric hospital | Cross-sectional | Burden, Psychological Distress |
Burden Total Score t(128) = 2.39, p < 0.05, d = 0.45 Psychological Distress Total Score t(128) = 0.48, p = 0.63, d = 0.08 |
- No significant differences in caregiver burden were reported between caregivers of individuals with SCZ or BD. - Caregivers of individuals with SCZ reported higher levels of psychological distress compared to caregivers of those with BD. |
| 27. Asl et al. [78] | Iran, university psychiatric institute | Descriptive analytical | Burden, Depression, Anxiety, Psychological distress |
Total Burden Score t(298) = 0.45, p = 0.65, d = 0.05 Depression, Anxiety and Stress Composite Score t(298) = 0.02, p = 0.99, d < 0.01 |
- No significant differences in caregiver burden were observed between caregivers of individuals with SCZ or BD. - No significant differences in depression, anxiety or distress were observed between caregivers of individuals with SCZ or BD. |
| 28. Khatoon et al. [79] | India, psychiatric hospital | Cross-sectional | Burden |
Total Objective Burden Score t(58) = 2.06, p < 0.05, d = 0.53 |
- Caregivers of those with SCZ presented with significantly higher caregiver burden on subscales of total objective burden, subjective burden, financial burden, disruption to family activities, disruption to family leisure and disruption to family interaction. - There were no significant differences in caregiver burden observed between caregivers of individuals with SCZ or BD on the clinician-rated objective burden subscale, and burden subscales on effects on physical and mental health. |
SSD schizophrenia spectrum disorder, SCZ schizophrenia, BD bipolar disorder, M mean, SD standard deviation
Sample characteristics
Across 27 studies, data were presented for 6166 caregivers (see Table 2), with one study omitting caregiver sample size [65]. Sample sizes in studies ranged from 40 caregivers to 1403 caregivers, and nine studies (32.1%) included samples of under 100 caregivers. Across 6166 caregivers, 32.7% (n = 2018) were caregivers of individuals with bipolar disorder, 47.9% (n = 2955) were caregivers of individuals with schizophrenia spectrum disorders and 19.4% (n = 1193) were caregivers of individuals with other mental health conditions. Based on data from 21 studies, 48.6% (n = 2997) of caregivers were female. Reporting of caregiver relationships to cared-for individuals varied, but available data indicated 32.3% (n = 1993) of caregivers were parents, 24.4% (n = 1507) were partners, 12.4% (n = 766) were siblings, 4.3% (n = 265) were children, and 11.9% (n = 732) had other relationships. Data on characteristics related to employment varied; eight studies did not report employment characteristics. Across 20 studies, 56.5% (n = 2662) of caregivers held either part- or full-time employment, and 10.7% (n = 503) were unemployed. Twenty studies indicated that 58.8% (n = 3623) of caregivers were married or in a relationship, 8.2% (n = 503) of caregivers were single, 2.3% (n = 139) of caregivers were divorced or widowed, and 0.2% (n = 13) were listed as “Other”. Employment data on the remaining 55.0% of caregivers, and marital status data on the remaining 30.5% of caregivers, in the overall review sample were not presented.
Table 2.
Sample characteristics across twenty-eight studies included in this review
| Study ID and Authors | n (%) of Caregivers (SSD, BD & Other Groups) | Age M(SD) | n (%) female | ||
|---|---|---|---|---|---|
| SSD n(%) | BD n(%) | Other n(%) | |||
| 1. Blanthorn-Hazell et al. [52] | 138(46.0%) | 159(54.0%) | N/A | Total N: 44.8(13.1) | Total N = 214(72.0%) |
| 2. Chadda et al. [53] | 100(50.0%) | 100(50.0%) | N/A | 75.0% between 25 and 50 years of age |
SSD = 51(51.0%) BD = 42(42.0%) |
| 3. Chakrabarti and Gill [54] | 20(34.5%) | 38(65.5%) | N/A |
SSD = 48.7(10.7) BD = 39.2(9.3) |
SSD = 12(60.0%) BD = 17(45.0%) Total N = 29(50.0%) |
| 4. Chakrabarti et al. [55] | 20(50.0%) | 20(50.0%) | N/A |
SSD = 44.7(13.1) BD = 41.7(12.9) Total N = 43.2(13.1) |
SSD = 8(40.0%) BD = 9(45.0%) Total N = 17(42.5%) |
| 5. Chang et al. [56] | 215(46.8%) | 85(18.5%) | MDD: 159 (34.6%) |
SSD = 55.0(13.5) BD = 51.4(12.6) MDD = 52.1(13.8) |
SSD = 118(55.0%) BD = 43(51.0%) MDD = 74(47.0%) Total N = 235(51.2%) |
| 6. Chien et al. [57] | 168(64.1%) | 12(4.6%) | Dep: 48 (18.3%) | Total N = 42.6(10.8) | Total N = 158(60.3%) |
| 7. Fekih-Romdhane et al. [58] | 20(38.5%) | 25(48.1%) | SCZAF: 7 (13.5%) | Total N = 48.4(13.1) | Total N = 41(78.8%) |
| 8. Grover et al. [59] | 70(50.0%) | 70(50.0%) | N/A |
SSD = 49.9(11.8) BD = 42.6(13.8) |
SSD = 21(33.3%) BD = 40(57.2%) Total N = 61(43.6%) |
| 9. Grover et al. [60] | 65(53.3%) | 57(46.7%) | N/A | Total N = 47.1(13.7) | Total N = 47(38.5%) |
| 10. Grover et al. [61] | 50(50.0%) | 50(50.0%) | N/A |
SSD = 50.3(14.9) BD = 45.0(13.2) |
SSD = 15(30.0%) BD = 26(52.0%) Total N = 41(41.0%) |
| 11. Grover et al. [62] | 707(50.4%) | 344(24.5%) | Dep: 352 (25.1%) | Total N = 44.6(12.5) | Total N = 620(44.2%) |
| 12. Ak et al. [63] | 40(50.0%) | 40(50.0%) | N/A | Not reported |
SSD = 30(75.0%) BD = 25(62.5%) Total N = 55(68.8%) |
| 13. Nehra et al. [64] | 50(50.0%) | 50(50.0%) | N/A |
SSD = 43.50(9.8) BD = 40.1(11.4) |
SSD = 23(46.0%) BD = 23(46.0%) Total N = 44(44.0%) |
| 14. Ramírez et al. [65] | Not specified | Not specified | N/A | Not reported | Not reported |
| 15. Rodrigo et al. [66] | 65(81.3%) | 15(18.7%) | N/A | Total N = 57.7(13.3) | Total N = 44(55.0%) |
| 16. Roychaudhuri et al. [67] | 30(55.5%) | 24(44.4%) | N/A |
Reported as n(%): < 35 years = 24 (44.4%) > 35 years = 30 (55.6%) |
Total N = 20(37.0%) |
| 17. Sharma et al. [68] | 50(50.0%) | 50(50.0%) | N/A | Total N = 43(12.0) |
SSD = 23(46.0%) BD = 18(36.0%) Total N = 41(41.0%) |
| 18. Singh and Prajapati [69] | 40(50.0%) | 40(50.0%) | N/A |
SSD Carer females = 58.3(9.5) BD Carer females = 0.0(16.7) |
SSD = 30(75.0%) BD = 20(50.0%) Total N = 50(62.5%) |
| 19. Vasudeva et al. [70] | 52(50.5%) | 51(49.5%) | N/A |
SSD = 48.3(11.7) BD = 47.4(12.0) |
SSD = 20(38.5%) BD = 23(45.1%) Total N = 43(41.8%) |
| 20. Webb et al. [71] | 59(70.2%) | 25(29.8%) | N/A | Total N = 56.0(13.6) | Total N = 66(78.0%) |
| 21. Zendjidjian et al. [72] | 246(51.5%) | 115(24%) | Dep: 117(24.5%) | BD & MDD Total = 52.2(15.5) | Total N = 135(58.2%) |
| 22. Zhou et al. [73] | 243(54.9%) | 200(45.2%) | N/A |
SSD = 47.7(13.7) BD = 44.4(13.6) |
SSD = 107(44.0%) BD = 102(51.0%) Total N = 209(47.2%) |
| 23. Abdeta and Desalegn [74] | 80(37.2%) | 60(27.9%) |
Dep: 50(23.3%) Anx: 25(11.6%) |
Total N = 35(1.62) | Total N = 120(55.8%) |
| 24. Cohen et al. [75] | 63(50.4%) | 62(49.6%) | N/A |
SSD = 51.28(12.65) BD = 40.55(15.17) |
SSD = 52(84.1%) BD = 43(69.4%) |
| 25. Ukpong and Ibigbami [76] | 100(50%) | 100(50%) | N/A |
SSD = 56.13(12.99) BD = 43.03(13.06) |
SSD = 63(63%) BD = 52(52%) |
| 26. Udoh et al. [77] | 84(20.2%) | 46(11.1%) |
Dep: 104(25.1%) SUD: 92(22.2%) Others: 89(21.4%) |
15–29 years = 181 (43.6%) 30–44 years = 154 (37.1%) 45–59 years = 63(15.2%) Above 60 years = 17(4.1%) |
Total female = 236(56.9%) |
| 27. Asl et al. [78] | 150(33.33%) | 150(33.33%) | ASD: 150(33.33%) |
SSD = 42.22(1.28) BD = 48.41(1.37) |
SSD = 81(54%) BD = 87(58%) |
| 28. Khatoon et al. [79] | 30(50.0%) | 30(50.0%) | N/A |
20–30 years = 16(26.6%) 30–40 years = 34(56.6%) 40–50 years = 10(16.6%) |
Not reported |
SSD Schizophrenia Spectrum Disorders, BD Bipolar Disorder, SCZAF Schizoaffective Disorder, Dep Depression, Anx Anxiety, SUD Substance Use Disorders, ASD Autism Spectrum Disorder, M Mean, SD Standard Deviation, N/n Number of participants
Study quality
All studies implemented established measures of caregiver burden and psychological impacts but presented inconsistent detail in their psychometric properties. Caregivers were recruited mostly from psychiatric hospital departments and mental health clinical settings, decreasing the likelihood of sample representativeness for caregivers in the general community. Six studies [52, 66, 69, 74, 77, 78] did not stipulate what diagnostic framework was used to determine diagnosis of individuals. Only four studies [63, 65, 70, 76] used diagnostic assessments to confirm diagnoses of cared-for individuals. Cultural diversity in samples of caregivers was captured given the broad diversity of countries included.
In appraising studies, eleven were of “Higher” quality [52, 54, 56–58, 72, 73, 75, 76], 16 were of “Moderate” quality [53, 55, 59–65, 67–71, 78, 79], and three were of “Lower” quality due to unclear inclusion criteria [66, 74, 77].
Measurement of caregiver burden and psychological functioning
Measures used to assess caregiver burden and psychological functioning are presented in Table 3. Caregiver burden was assessed using 11 different measures across 23 studies. The Family Burden Interview Schedule [FBIS; 80] was most commonly used across eight studies [57, 60, 61, 64, 67, 69, 76, 79]. There were six measures of objective and/or subjective burden in 18 studies (61.5%), two measures of stress-appraisal coping in four studies (15.4%), two measures of general family burden in two studies (7.7%) and one measure of caregiver strain in two studies (7.7%).
Table 3.
Measures used across twenty-eight studies to assess caregiver burden and psychological functioning
| Name of measure | How construct is defined | How construct is assessed by measure | Studies used in |
|---|---|---|---|
| Burden | |||
| Involvement Evaluation Questionnaire (IEQ [80];) | Stress-appraisal-coping model | 29-items across four factors: tension, supervision, worrying and urging. A total score represents overall burden. | 1, 9, 10 |
| Burden Assessment Schedule (BAS [81];) | Objective and subjective burden | 40-items across nine factors: spouse (caregiver related), physical & mental health of caregivers, external support, caregiver’s routine, support of individual, taking responsibility, other relations, individual’s behaviour, and caregiver strategy. A total score represents overall burden. | 2, 3, 19 |
| Caregiving Burden Inventory (CBI [82];) | Burden defined through the five factors assessed | 24-items across five factors: time-dependent; developmental; physical; social and emotional. | 5 |
| Family Burden Interview Schedule (FBIS [83];) | Objective burden with a subjective burden question included. |
24-items across six factors: financial burden, disruption of family routine, disruption of family leisure, disruption of family interactions, effect on physical health and mental health of relatives. One additional item assessing subjective burden. Two total scores representing objective and subjective burden. Clinician-rated. |
6, 9, 10, 13, 16, 18, 25, 28 |
| Subjective Well-being Inventory (SUBI [84];) | Subjective burden | Two sets of items assessing positive and negative assessments of well-being and subjective burden. Two total scores for positive and negative sets. | 16 |
| Zarit Burden Interview (ZBI [85];) | Subjective burden | 12-items assessing caregiver’s state of health, psychological and financial wellbeing, social life, and relationship with the individual. A total score represents overall subjective burden. | 7, 12, 26, 27 |
| Modified Caregiver Strain Index (MCSI [86];) | Caregiver strain | 13-items across six factors: social, psychological, physical, time, financial and employment. Higher scores indicate greater caregiver strain. | 15, 17 |
| Experience of Caregiving Inventory (ECI [87];) | Stress-appraisal-coping model | 66-items across ten factors: eight negative aspects of caregiving (difficult behaviours, negative symptoms, stigma, problems with services, effects on family, need for back-up, dependency, and loss) and two positive aspects of caregiving (positive personal experience and good aspects of relationship). Three total scores represent overall negative score, overall positive score, and global score. | 8 |
| Family Burden Schedule (adaptation of the Spanish adaptation of the Social Behaviour Assessment Schedule) (FBS [88];) | Objective burden, attribution level and subjective burden. | Number of items not specified. Assesses burden across three factors: objective burden evaluates change in daily functioning; level of attribution evaluates whether caregivers consider their problems related to the individual; subjective burden evaluates perception of stress related to subject’s behaviour. | 14 |
| Significant Other Scale (based on subscale of Family Evaluation Form) [89] | Objective burden | 37-item measure, with the study using a 13-item subscale described by the original measure authors as assessing objective burden. One total score representing overall burden. | 20 |
| Name of measure | How construct is defined | How construct is assessed by measure | Studies used in |
| Family Experience Inventory Schedule (FEIS [90];) | Family burden + Depression and anxiety | 28-items across five factors: violent behaviour, depression and anxiety symptoms and social isolation of the caregiver, disruption of caregiver routines, individual suicidality, and satisfaction with the quality-of-service provision. | 22 |
| Psychological Functioning | |||
| Distressing Symptom Rating Scale (DSRS [55];) | Caregiver distress | 44-items across 16 factors: depressive/negative, manic, socially disruptive, somatic, delusions/odd beliefs, hallucinations, cognitive, aggression, work, self-care, dependence, compliance, side effects, substance abuse, insight, poor rapport, and other. | 4 |
| Taiwanese Depression Questionnaire (TDQ [91];) | Presence and severity of depression | 18-items evaluating depressive symptoms over past week, calculated to obtain total depression score. | 5 |
| Beck Anxiety Inventory (BAI [92];) | Presence and severity of anxiety | 21-items summed to obtain total anxiety score. | 5, 17 |
| General Health Questionnaire (GHQ [93];) | Psychological morbidity/distress | 12-items summed up obtain total score assessing psychological distress/morbidity. | 8, 11, 26 |
| Center for Epidemiological Studies – Depression Scale (CES-D [94];) | Possibility of depression | 20-items with one total score representing overall depression. | 15 |
| Beck Depression Inventory (BDI [95];) | Presence and severity of depression | 21-items with one total score representing depression. | 17, 24 |
| National Center for Health Statistics General Wellbeing-Schedule (from the Medical History Questionnaire) [96] | Wellbeing | 22-items across six factors of caregiver wellbeing: anxiety, depression, general health, positive wellbeing, vitality, self-control. | 20 |
| Family Experience Inventory Schedule (FEIS [90];) | Family burden + Depression and anxiety | 28-items across five factors: violent behaviour, depression/anxiety symptoms and social isolation of the caregiver, disruption of caregiver routines, individual suicidality, and satisfaction with the quality-of-service provision. | 22 |
| Self-Reported Questionnaire-20 (SRQ-20 [97];) | Presence of common mental disorders (anxiety and depression) | 20-item screening tool with one total score designed to assess the presence of symptoms of common mental disorders, such as anxiety and depression. | 23 |
| Short Form-36 (SF-36 [98];) | Quality of life (including mental health outcomes) | 36-items across eight factors: physical functioning, social functioning, role-physical problems, role-emotional problems, mental health, vitality, bodily pain, and general health. Two component summary scores representing physical and mental overall score. | 21, 24 |
|
World Health Organization Quality of Life Instrument – BREF (WHOQOL-BREF [99];) |
Quality of life (including psychological outcomes domain) | 26-items divided into four domains: physical, psychological, social relationships and environment, along with two general questions of quality of life. Total scores range from 0 to 100 and the higher the value of scores, the higher quality of life. | 24, 25 |
| Hospital Anxiety and Depression Inventory (HADS [100];) | Anxiety and depression | 14-item measure of anxiety and depressive symptom severity. One total score is calculated with higher scores representing greater symptom severity. | 25 |
| Depression, Anxiety and Stress Scale (DASS [101];) | Depression, anxiety, and stress | 42-item measure of three 14-item subscales of depression, anxiety, and stress. Three total scores representing each domain are calculated measured from mild to severe severity. | 27 |
Psychological functioning was assessed using 13 measures across 14 studies. Nine measures were used to assessed anxiety, depression or both [90–92, 94, 95, 97, 100, 101], two assessed variations of caregiver distress [55, 93] and two measured quality of life (QoL) including a specific mental health or psychological outcomes domain [98, 99]. Psychological wellbeing [96] was directly assessed in one study [71], while one study [59] implemented the Experience of Caregiving Inventory (ECI [87];), a stress-appraisal-coping measure of caregiving burden that examines both the positive and negative experiences of providing care.
Comparison of caregiver burden
No significant differences
Fourteen (50%) studies comparing caregiver burden, comprising 2091 caregivers [52, 53, 56–58, 63–66, 68, 71, 77–79], showed no significant differences in caregiver burden between caregivers of individuals with bipolar disorder or schizophrenia spectrum disorders. Two studies [77, 78] presented data on caregivers of those with schizophrenia and bipolar disorder as part of a larger group; relevant data was extracted and t-tests were re-ran to determine differences in caregiving burden observed. Studies emphasized that despite the perceived episodic nature of bipolar disorders, greater chronicity and severity of symptoms across both diagnoses may confer similar burden [52, 53, 58, 63, 68, 78]. Caregiver characteristics were associated with burden across both groups, including lower level of education attained, being a spousal caregiver, and higher caregiver distress.
Significantly greater caregiver burden in schizophrenia spectrum disorders
Nine (32.1%) papers comprising 1217 caregivers demonstrated that caregiving burden was significantly greater in caregivers of individuals with schizophrenia spectrum disorders than in caregivers of individuals with bipolar disorders [59–61, 67, 69, 70, 76, 79]. Five studies noted significantly lower functioning in participants with schizophrenia as compared to participants with bipolar disorder, but this was inconsistently associated with heightened caregiver burden [54, 59–61, 70]. Other studies noted that individuals diagnosed with schizophrenia presented with more severe and longer duration of untreated illness compared to individuals diagnosed with bipolar disorders [54, 70, 79]. This was not uniform across studies, as Grover et al. [59] reported longer duration of treated illness for participants with bipolar disorder compared to individuals with schizophrenia (Bipolar Disorder, M = 160.06, SD = 97.50; Schizophrenia, M = 112.82, SD = 74.07, t = 3.24, p = .001). Individuals with bipolar disorder may experience more defined periods of well and ill-health compared to the persistent functional and symptomatic impacts of schizophrenia. However, this would not hold true for individuals with chronic and persistent bipolar disorder [54].
Several caregiver and illness characteristics were proposed as contributing to the greater burden experienced by caregivers of people with schizophrenia. Chakrabarti and Gill [54] noted that caregiver burden (Schizophrenia Spectrum Disorders, M = 71.95, SD = 14.09; Bipolar Disorders M = 61.42, SD = 9.26; t = 3.42, p < .01) was greater for caregivers of those with schizophrenia in all burden domains except for that pertaining to the relationships caregivers have with other family members or friends. While no discernable reason was reported for this lack of difference regarding other relationships, high burden was correlated with several coping strategies. Caregivers of individuals with schizophrenia were more likely to adopt avoidance, resignation and seeking spiritual help coping as opposed to caregivers of individuals with bipolar disorder. Grover et al. [61] noted that caregivers of those with schizophrenia believed their diagnosed loved ones had higher unmet healthcare needs than caregivers of those with bipolar disorder. These unmet needs included amelioration of psychotic symptoms, need for psychoeducation and relief of psychological distress. Caregivers with heightened burden also presented with higher levels of psychological distress. Vasudeva et al. [70] found that caregivers of those with schizophrenia had significantly higher total objective burden score (t = 2.15, p < .05, d = 0.42), higher burden in needs for external support (p < .05, d = 0.48), disruptions to caregivers’ routine (p < 0.01, d = 0.539), and higher scores in other relations (p < .05, d = 0.38). Whilst these differences were attributed to the ongoing functional and symptomatic impacts of schizophrenia, the study authors posited that caregivers of those with schizophrenia may have ongoing concerns about their loved one’s capacity to return to normal functioning, even when acute symptoms were treated.
Significantly greater caregiver burden in bipolar disorders
Two (7.7%) studies comprising 565 caregivers demonstrated that caregiving burden was significantly higher in caregivers of individuals with bipolar disorder compared to individuals with schizophrenia [60, 73]. Zhou et al. [73] demonstrated that caregiver perceptions of violent behaviour (B = 2.01, p < .001) and suicidal risk (B = 0.51, p < .05) were greater in caregivers of individuals with acute bipolar disorder compared to caregivers of those with acute schizophrenia spectrum disorders. The focus on acute presentations of illness may explain the outcomes obtained, but symptom severity comparison was not possible due to differences in symptom measures used. Grover et al. [60] noted that caregivers of those with bipolar disorder appraised their caregiving burden to be higher than caregivers of those with schizophrenia on the Involvement Evaluation Questionnaire (IEQ; t = 2.96, p < .01). While direct explanations were not provided, considerations of how caregiver characteristics influence caregiver burden was emphasized given its multidimensionality.
Comparison of psychological functioning
No significant difference in mental health outcomes
Eleven (39.3%) studies comprising 3246 caregivers demonstrated no significant differences in mental health outcomes for caregivers associated with caring for individuals with either schizophrenia spectrum disorders or bipolar disorders [55, 56, 59, 62, 66, 68, 73–76, 78]. One study [78] presented data on caregivers of those with schizophrenia and bipolar disorder as part of a larger group; relevant data was extracted and t-tests were re-ran to determine differences in mental health outcomes observed. The studies demonstrated that while caregivers experienced high levels of distress, depressive and anxious symptoms, diagnosis did not differentiate outcomes. Many studies noted the likelihood that both diagnoses confer similar distress to caregivers given their chronicity, symptom severity and functional impacts. Certain caregiver characteristics demonstrated mixed associations with poorer mental health outcomes, including caregiver substance use, lower caregiver educational status, heightened caregiver burden, caregivers experiencing illness themselves, and being a spousal caregiver.
Significant mental health outcomes in caregivers of those with schizophrenia spectrum disorders
Four studies (11%) comprising 933 caregivers demonstrated poorer mental health outcomes of caregivers of those with schizophrenia spectrum disorders compared to caregivers of those with bipolar disorder [72, 75–77]. One study [77] presented data on caregivers of those with schizophrenia and bipolar disorder as part of a larger group; relevant data was extracted and t-tests were re-ran to determine differences in mental health outcomes observed. Zendjidjian et al. [72] found that caregivers of those with schizophrenia reported significantly lower scores on the mental health domains of a quality-of-life measure, the Short Form-36 (SF-36 [98];). Whilst no direct reason was offered to explain these differences, this may be indicative of caregiving as multidimensional, and suggests that caregiver supports should be tailored to address the most-impaired domains within a caregiver’s experience. Cohen et al. [75] noted that caregivers of those with schizophrenia presented with higher depressive symptoms, attributing this to positive psychotic symptoms and stigma, which are more commonly associated with schizophrenia. Ukpong and Ibigbami [76] demonstrated that caregivers of those with schizophrenia had poorer mental health. Factors associated with poorer mental health across both caregiving groups included older caregiver age, longer duration of illness and caregiving, caregivers not being married, and increased caregiver burden, anxiety, and depression.
Significant mental health outcomes in caregivers of those with bipolar disorders
One study (3.8%) comprising 200 caregivers demonstrated poorer mental health outcomes in caregivers of those with bipolar disorder when compared to caregivers of individuals with schizophrenia [76]. The study demonstrated that caregivers of individuals with bipolar disorder presented with higher depressive symptoms than caregivers of those with schizophrenia. This finding was unexpected, and significant negative correlations were noted between caregiver depressive symptoms and all four domains of the QoL measure used, which assessed physical, psychological, social, and environmental QoL.
Comparison of psychological wellbeing
Only two studies, comprising 224 caregivers, examined outcomes pertaining to psychological wellbeing of caregiving [59, 71]. Webb et al. [71] assessed caregiver wellbeing but found no significant differences based on individual diagnosis. This may have been attributable to small sample size and reliance on chart diagnosis. However, older caregiver age and higher frequency of positive symptoms were significantly associated with greater well-being. While reasons for the latter were not explored, as caregivers age, they may be more accepting of their loved one’s illness or are better equipped to access social supports. Grover et al. [59] noted that caregivers of those with schizophrenia spectrum disorders reported higher positive personal caregiver experiences than caregivers of those with bipolar disorder (t(138) = 2.67, p < .001) on a measure of stress-appraisal coping. Positive appraisals were significantly correlated with negative care appraisals across both groups. Individuals diagnosed with bipolar disorder had longer illness and treatment duration, which may concurrently reduce their caregiver’s experience of role demands and positive aspects of caring.
Discussion
To our knowledge, this was the first systematic review that examined whether experiences of caregiver burden and psychological functioning differ for caregivers depending on whether they provide care to an individual diagnosed with a schizophrenia spectrum disorder or bipolar disorder. Previous systematic reviews have focused on examining the negative impacts of caregiving for these two groups separately [41–43] or have examined the broader categorization of SMI without specific diagnostic focus [44, 45].
The comparative outcomes of the caregiving experience
Caregiver burden
A primary finding amongst all studies, except for Singh and Prajapati [69], was that both groups experienced high levels of burden. This is unsurprising, yet consistent with literature noting high caregiver burden experienced by caregivers of those with SMI [37, 102]. Singh and Prajapati [69] attributed this exception to their sample of individuals diagnosed with bipolar disorder not being acutely unwell, but this contrasts the literature indicating that non-acute bipolar disorder still confers symptomatic and functional impacts to diagnosed individuals [103].
Within the 14 studies demonstrating no significant difference in caregiving burden experienced between both caregiver groups, the comparable symptomatic and functional impairments associated with both schizophrenia spectrum disorders, and bipolar disorders, were highlighted. However, individual symptom severity was only directly compared on the same measure in three studies [53, 58, 63], and while higher symptom severity significantly contributed to burden, burden did not differ between caregiver groups based on symptom severity. There were conflicting results on the influence of transdiagnostic symptoms, such as aggression and suicidality, contributing to comparable levels of caregiver burden [52] and to greater caregiver burden in bipolar disorder alone [73]. However, the latter focused on individuals with acute symptom presentations at recruitment. This may indicate that the combination of symptom severity and acuity were of higher relevance to caregiver burden then the diagnosis itself, given this is an isolated finding within the review. Across many studies, groups presented with similar degrees of chronicity [53, 58, 63, 64, 68]. Given both bipolar disorder and schizophrenia spectrum disorders are associated with disabling impacts [104], chronicity of illnesses could contribute to comparable caregiver burden. Whilst transdiagnostic features were not a primary focus, similarities in caregiver burden across groups may warrant an exploration of these features in the caregiver literature. This suggestion is raised given the growing perspective in psychiatric research that traditional psychiatric diagnoses may limit novel developments in clinical and research settings [105, 106]. Additionally, caregiver characteristics were noted as contributing to heightened burden across both groups, emphasizing that caregiving was not only influenced by the individual being cared for and their clinical characteristics.
The nine studies demonstrating higher caregiver burden in caregivers of those with schizophrenia compared to bipolar disorder demonstrate some consistencies. While group characteristics such as illness duration were mostly comparable, two studies noted that individuals with schizophrenia had higher duration of untreated illness [59, 70]. Even when individuals with bipolar disorder had longer illness duration, the significantly higher level of burden in caregivers of those with schizophrenia was attributed to the symptomatic and functional impacts schizophrenia can incur upon affected individuals [79]. The role of functional impairments in contributing to caregiver burden was possible given five studies noted lower functioning in individuals with schizophrenia; however, functioning was not a consistent correlation of, or contributor to, differential caregiver burden. Other potential caregiver characteristics differentiating caregiver burden were suggested, including the greater stigma around schizophrenia [56], appraisal of illness and functional expectations [59, 70], specific caregiving coping [54], unmet caregiver and individual needs [61] and cultural expectations of functioning [67]. Higher levels of caregiving burden for caregivers of those with bipolar disorder were considered with respect to acuity of symptoms [73] and limited clinician knowledge regarding caregiver burden in bipolar disorder [60]. However, few studies supported differentiation in caregiver burden based on diagnosis, contrasting previous literature emphasizing the association between burden, clinical, individual and caregiver characteristics [55, 107, 108].
The current review findings can be considered in a broader context of the literature examining caregivers of those with other medical conditions. Caregiving burden across numerous medical conditions, including cancer [109], dementia [12], neurological conditions [110, 111] and stroke [112], has been demonstrated as consistently high, and is often compared between these conditions. However, the influence of diagnosis alone on caregiving burden in these medical conditions is, similar to this review’s findings, mixed [11, 13, 109]. Emphasis has instead been placed upon the multidimensionality of caregiving burden as influenced by numerous factors. These have included symptom severity and behavioural disturbances across multiple forms of dementia [12, 113], presence of psychiatric symptoms of anxiety and depression across patients with stroke or neurological conditions [110–112], and caregiver factors including the amount of time and effort spent caregiving across caregivers of those with dementia, stroke or cancer [12, 109, 112]. This demonstrates that, for these more commonly researched medical conditions, caregiver burden is influenced by multiple factors that may be common amongst several diagnoses or may not be associated with diagnosis at all.
Considering the current results and the broader literature of caregiving burden in other conditions, these findings suggest that diagnosis alone may not determine caregiver burden experienced by caregivers, similar to a prior systematic review [44]. Instead, caregiving burden is a multidimensional concept, consisting of multiple domains influenced by numerous individual and caregiver factors. These findings suggest that when considering the various factors in the caregiving experience, diagnosis may not be as relevant as other transdiagnostic illness characteristics, or characteristics of the caregiver themselves. Whilst the focus on diagnosis is important given it reflects the widespread implementation in clinical and research settings of these defined psychopathologies, it is possible and worth exploring whether caregivers view diagnosis with the same significance. This is further reflected in the many concepts intermittently considered in this review and the papers within it that are distinct from diagnosis, including expressed emotion [114], caregiver physical health [115], coping strategies [32], quality of life [116] and social supports [17], amongst several others.
Conceptualization of caregiving burden
The lack of standardization for caregiver burden means that, despite relatively sound psychometric data, the diversity of measures and definitions limits consistency of how caregiver burden is assessed across studies. The wide variation in this relatively small sample of caregiving studies is reflective of the wider difficulties in operationalizing caregiving burden. A systematic review and meta-analysis of tools used to assess caregiving burden [117] noted that this multidimensionality meant any measure applied would be informed by the burden dimensions specifically examined, and considerations of the study design, including study location. Despite the review noting the Zarit Burden Interview as being the most commonly adopted and psychometrically sound measure of caregiver burden [117], it was only used four times [58, 63, 77, 78] in this current review. Comparatively, the Family Burden Interview Schedule (FBIS) was applied across eight studies in this review. This may reflect that many studies in this review were based in India, where the FBIS is well-validated [54, 60, 61]. The diversity in measures limits global generalizability of results and conclusions that can be drawn in comparing caregiver experiences.
Psychological functioning and mental health outcomes
Juxtaposing the findings around caregiving burden, consistency was noted across the 14 studies examining the mental health outcomes of caregiving – that being depression, anxiety, and psychological distress. As eleven studies demonstrated no significant differences in mental health outcomes of caring between caregiver groups based on individual diagnosis, this may reflect that these aspects of caregiving are better understood and operationalized in comparison to burden. Despite overlap in the mental health outcomes measured, anxiety, depression and distress are relatively distinct and well-defined concepts compared to burden, and the findings present more robustly. Most studies acknowledged that the mental health outcomes measured were similarly high for both caregiver groups [73, 74, 76, 78]. The lack of differentiation in mental health outcomes may reflect the similarly impactful nature of bipolar disorder and schizophrenia spectrum disorders to individuals and their caregivers [24, 118, 119]. Both individual and caregiver characteristics were considered, as spousal caregivers experienced greater distress compared to parental caregivers [68]. It is important to consider caregiver characteristics, as caregiving is influenced by factors beyond diagnosis, including poorer quality of life, older caregiver age, longer illness duration and stigma [75, 76].
Psychological wellbeing
The two studies in the current review that considered psychological wellbeing and the positive outcomes of care is indicative of the wider need to focus on this under-researched but developing area [30, 31, 120]. The two studies in this review were not consistent in their findings on psychological wellbeing, as one [71] found no difference between groups, while the other [59] noted that caregivers of those with schizophrenia reported higher positive, and paradoxically negative, caregiving experiences. This disparity in findings may reflect the difference in measures used to examine the positive outcomes of care between caregiver groups. Grover et al. [59] explored positive appraisals of care in the context of a stress-appraisal coping measure of burden, whilst Webb et al. [71] implemented a direct measure of psychological wellbeing to assess these positive outcomes. Differences were also noted in the factors that associated with these findings, which may suggest that given the differences in how positive outcomes of care were assessed, these findings were not measuring the same concept. Further research is warranted, as studies outside of this review have noted that positive personal characteristics may mediate the impacts of caring, and proactive resilience strategies may improve caregiver experiences [30, 31].
Methodological limitations of the current literature
A noteworthy strength of the literature within this review is its cross-cultural nature, with 18 countries identified across the review in both developed and developing nations. However, many studies did not consider whether cultural factors influenced differences in family structures and who may adopt a caregiving role, and whether that influenced differences in caregiving. Most studies were conducted in developing nations, where caregiving demands may be higher due to less developed mental health systems, cultural stigma towards mental illness or differences in cultural practices. This may bias the current review findings, and further research is needed to determine how caregivers in developed and developing nations differ in their caregiving experiences. Several important methodological limitations were identified. First, most studies were cross-sectional, limiting causal inferences. Attempts were made within studies to account for confounding variables, however which variables were considered was inconsistent across studies. Second, variation in frameworks and measures used to assess caregiver burden meant that comparison of results was challenging for this complex and multidimensional construct. This limitation raises concerns regarding conceptual overlap in measures, as some, such as the Family Experience Inventory Schedule, examined caregiving burden by including caregiver anxiety and depression. Additionally, while some studies included significantly large sample sizes ranging from 200 to 1403 caregivers [52, 56, 62, 72, 73], 32.1% of studies had sample sizes below 100 caregivers, limiting generalizability and strength of results. The lack of control groups in all studies except for Zendjidjian et al. [72] limits the extent to which the results can compare caregiving for those with SMI to the typical caregiving demands that arise from relationships irrespective of the presence of SMI or caregiving associated with other chronic health conditions. Finally, all studies, except for Zhou et al. [73], did not examine early stage or acute-phase bipolar disorder and schizophrenia spectrum disorders, omitting explorations of how caregivers at the early stages of illness adapt to their newfound caring role.
Strengths and limitations of the review
We implemented a comprehensive search strategy across major databases, and all potentially eligible studies were assessed for inclusion and methodological quality by two independent raters. However, there were limitations. First, studies were excluded if they were not written in English. Twelve papers were omitted from full-text analysis due to this limitation, and these studies took place in developed European nations such as Germany, Greece, Switzerland, and Turkey, alongside Japan and China. Scans of abstracts and listed authors indicated that these excluded studies were not reporting on the same cohorts as other papers in this review. This limits the review’s cultural representativeness; however, we did not aim to determine how cultural experiences influences caregiving. Second, while the data extraction template was based on established Cochrane standards [47], two quality appraisal tools were used to appraise article quality, which may compromise validity of the approach used. Thirdly, while the study authors have commented on the possible influence of transdiagnostic features compared to diagnoses, the current review’s deliberate focus on diagnosis limited an exploration of this influence. Fourthly, the current review did not examine quality of relationships between caregivers and their loved ones. While this was not a focus of the review and is often overlooked in caregiving literature, it was considered in some of the included studies [59, 66] and the quality of these relationships are important considerations within the wider familial and social context of any caregiver-patient dyad. Finally, the current review omitted qualitative studies, which represent an important and substantial area of the caregiver literature [32, 102].
Directions for future research
Future research would benefit from using longitudinal and real time assessment study designs, and employing consistently larger sample sizes and control groups, to assess changes in caregiving over time and accurately compare differential caregiving experiences. The diversity of conceptualizations and measures for caregiver burden limits comparability, and future research should move towards standardizing caregiving burden for conceptual clarity. Optimistically, current research is moving towards establishing commonality in defining caregiving burden [121]. This is sorely needed in the field to allow better comparability across studies. Given the focus on caregivers of those with chronic presentations of schizophrenia spectrum disorders and bipolar disorders, further research could compare caregiving experience at the early stages of illness. This may reveal differential outcomes of caregiving as caregivers are adapting to their newfound role [122]. The relative paucity of comparative research examining the positive experiences of care presents an opportunity to understand the resilience and personal strengths caregivers have. Finally, the growing interest in transdiagnostic features in psychiatric research [105, 106] presents an opportunity in the caregiver literature to go beyond examinations of caregiving in discrete diagnostic groups, and to think more broadly about the experience of caregiving as a whole.
Clinical implications
There are several clinical implications of these findings. Establishing a consistent definition for the various factors of caregiving that can be reliably assessed is important in aiding clinicians to accurately understand the caregiver role, and what supports caregivers may require. As caregiving is multidimensional, consideration of the evolving needs of caregivers would better inform supports, rather than focusing on how diagnoses affect caregivers. While there are inconsistent findings on whether diagnosis distinguishes experiences of care, it does suggest that both disorders confer significant burden and psychological impacts. Early implementation of caregiver supports, including peer and psychological support, respite, financial or relief services specifically focused on supporting caregivers of loved ones entering mental health care for the first time, may prevent longer-term negative impacts. Psychoeducation has been implemented across settings as a primary support for caregivers, and while modest benefits have been noted [123], further research is required to determine whether certain modalities, such as group or individual interventions, are most beneficial in supporting caregiver health and wellbeing. Finally, clinicians would benefit from being able to provide ongoing support for caregivers, as caregivers’ needs will likely change over time.
Conclusions
In this review we have considered whether the caregiving experience is comparable with respects to caregiving burden and psychological functioning for caregivers of those diagnosed with either schizophrenia spectrum disorder or bipolar disorder. Twenty-eight studies presented varying results regarding the similarities and differences of these two groups. Most papers suggested that individual diagnosis did not differentiate the caregiving experience. However, a lack of definitional and measurement consensus for caregiving burden means that comparison is difficult. Similarly, several methodological issues were noted which impacts the generalizability of results. We suggest that both caregiver groups experience significant burden and mental health outcomes. Future studies should aim to: (a) incorporate longitudinal and real time assessment study designs with larger samples examining various components of the caregiving role; (b) establish a standardized definition of burden; (c) assess the positive outcomes of caring; and (d) focus on diverse caregiving populations, including cross-cultural and early-stage caregivers, to determine how caregiver and individual factors influence the caring experience.
Acknowledgments
Not applicable.
Abbreviations
- SMI
Serious Mental Illnesses
- M
Mean
- SD
Standard Deviation
- QoL
Quality of Life
- BD
Bipolar Disorders
- SSD
Schizophrenia Spectrum Disorders
- SCZ
Schizophrenia
- IEQ
Involvement Evaluation Questionnaire
- BAS
Burden Assessment Schedule
- CBI
Caregiver Burden Inventory
- FBIS
Family Burden Interview Schedule
- SUBI
Subjective Wellbeing Inventory
- ZBI
Zarit Burden Interview
- MCSI
Modified Caregiver Strain Index
- ECI
Experience of Caregiving Inventory
- FBS
Family Burden Schedule
- FEIS
Family Experience Inventory Schedule
- DSRS
Distressing Symptom Rating Scale
- BAI
Beck Anxiety Inventory
- GHQ
General Health Questionnaire
- CES-D
Center for Epidemiological Studies – Depression Scale
- BDI
Beck Depression Inventory
- SRQ-20
Self-Reported Questionnaire-20
- SF-36
Short Form 36
- HADS
Hospital Anxiety and Depression Inventory
- DASS
Depression, Anxiety and Stress Scale
- WHOQOL-BREF
World Health Organization Quality of Life Instrument – Brief
- TDQ
Taiwanese Depression Questionnaire
Authors’ contributions
Extracted and analysed the data: GJK AJ. Wrote the first draft, contributed to the writing, and agree with manuscript results and conclusions: GJK KF LKB KAA SMC. The author(s) read and approved the final manuscript.
Funding
KA is supported by a NHMRC Career Development Fellowship (1141207). SC is supported by a NHMRC Senior Research Fellowship (1136344). No other funding sources are declared by the authors.
Availability of data and materials
Data, search strategies and appraisals of included studies are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no potential conflict of interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centorrino F, Mark TL, Talamo A, Oh K, Chang J. Health and economic burden of metabolic comorbidity among individuals with bipolar disorder. J Clin Psychopharmacol. 2009;29(6):595–600. doi: 10.1097/JCP.0b013e3181bef8a6. [DOI] [PubMed] [Google Scholar]
- 2.Rinaldi M, Killackey E, Smith J, Shepherd G, Singh SP, Craig T. First episode psychosis and employment: a review. Int Rev Psychiatry. 2010;22(2):148–162. doi: 10.3109/09540261003661825. [DOI] [PubMed] [Google Scholar]
- 3.Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102. doi: 10.1016/s0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 4.Morgan VA, McGrath JJ, Jablensky A, Badcock JC, Waterreus A, Bush R, et al. Psychosis prevalence and physical, metabolic and cognitive co-morbidity: data from the second Australian national survey of psychosis. Psychol Med. 2014;44(10):2163–2176. doi: 10.1017/S0033291713002973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viron MJ, Stern TA. The impact of serious mental illness on health and healthcare. Psychosomatics. 2010;51(6):458–465. doi: 10.1016/s0033-3182(10)70737-4. [DOI] [PubMed] [Google Scholar]
- 6.The Royal Australian & New Zealand College of Psychiatrists, Australian Health Policy Collaboration . Economic cost of serious mental illness and comorbidities in Australia and New Zealand. Melbourne: Royal Australian & New Zealand College of Psychiatrists; 2016. [Google Scholar]
- 7.Pollak CP, Perlick D. Sleep problems and institutionalization of the elderly. J Geriatr Psychiatry Neurol. 1991;4(4):204–210. doi: 10.1177/089198879100400405. [DOI] [PubMed] [Google Scholar]
- 8.Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics. 2008;26(2):149–162. doi: 10.2165/00019053-200826020-00005. [DOI] [PubMed] [Google Scholar]
- 9.Ran MS, Chui CH, Wong IY, Mao WJ, Lin FR, Liu B, et al. Family caregivers and outcome of people with schizophrenia in rural China: 14-year follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(4):513–520. doi: 10.1007/s00127-015-1169-0. [DOI] [PubMed] [Google Scholar]
- 10.Diminic S, Hielscher E, Lee Y, Harris M, Schess J, Kealton J. In: The economic value of informal mental health caring in Australia. Australia M, editor. MIND Australia; 2017. pp. 1–188. [Google Scholar]
- 11.Del-Pino-Casado R, Priego-Cubero E, Lopez-Martinez C, Orgeta V. Subjective caregiver burden and anxiety in informal caregivers: a systematic review and meta-analysis. PLoS One. 2021;16(3):e0247143. doi: 10.1371/journal.pone.0247143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiao CY, Wu HS, Hsiao CY. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev. 2015;62(3):340–350. doi: 10.1111/inr.12194. [DOI] [PubMed] [Google Scholar]
- 13.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1060. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- 14.Pinquart M, Sorensen S. Correlates of physical health of informal caregivers: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62(2):P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- 15.Tungpunkom P, Napa W, Chaniang S, Srikhachin P. Caregiving experiences of families living with persons with schizophrenia: a systematic review. JBI Database System Rev Implement Rep. 2013;11(8):415–564. doi: 10.11124/jbisrir-2013-881. [DOI] [Google Scholar]
- 16.Caqueo-Urizar A, Miranda-Castillo C, Lemos Giraldez S, Lee Maturana SL, Ramirez Perez M, Mascayano TF. An updated review on burden on caregivers of schizophrenia patients. Psicothema. 2014;26(2):235–243. doi: 10.7334/psicothema2013.86. [DOI] [PubMed] [Google Scholar]
- 17.Ribe JM, Salamero M, Perez-Testor C, Mercadal J, Aguilera C, Cleris M. Quality of life in family caregivers of schizophrenia patients in Spain: caregiver characteristics, caregiving burden, family functioning, and social and professional support. Int J Psychiatry Clin Pract. 2018;22(1):25–33. doi: 10.1080/13651501.2017.1360500. [DOI] [PubMed] [Google Scholar]
- 18.Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis. Br J Psychiatry. 2010;196(4):259–265. doi: 10.1192/bjp.bp.109.070466. [DOI] [PubMed] [Google Scholar]
- 19.Hoenig J, Hamilton MW. The schizophrenic patient in the community and his effect on the household. Int J Soc Psychiatry. 1966;12(3):165–176. doi: 10.1177/002076406601200301. [DOI] [PubMed] [Google Scholar]
- 20.Platt S. Measuring the burden of psychiatric illness on the family: an evaluation of some rating scales. Psychol Med. 1985;15(2):383–393. doi: 10.1017/s0033291700023680. [DOI] [PubMed] [Google Scholar]
- 21.Preedy VR, Watson RR. Psychological functioning. In: Preedy VR, Watson RR, editors. Handbook of disease burdens and quality of life measures. New York: Springer New York; 2010. p. 4300. [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- 23.Mitsonis C, Voussoura E, Dimopoulos N, Psarra V, Kararizou E, Latzouraki E, et al. Factors associated with caregiver psychological distress in chronic schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):331–337. doi: 10.1007/s00127-010-0325-9. [DOI] [PubMed] [Google Scholar]
- 24.Stanley S, Balakrishnan S, Ilangovan S. Psychological distress, perceived burden and quality of life in caregivers of persons with schizophrenia. J Ment Health. 2017;26(2):134–141. doi: 10.1080/09638237.2016.1276537. [DOI] [PubMed] [Google Scholar]
- 25.Marino VR, Haley WE, Roth DL. Beyond hedonia: a theoretical reframing of caregiver well-being. Translat Issues Psychol Sci. 2017;3(4):400–409. doi: 10.1037/tps0000134. [DOI] [Google Scholar]
- 26.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- 27.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 28.Flyckt L, Lothman A, Jorgensen L, Rylander A, Koernig T. Burden of informal care giving to patients with psychoses: a descriptive and methodological study. Int J Soc Psychiatry. 2013;59(2):137–146. doi: 10.1177/0020764011427239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ong HC, Ibrahim N, Wahab S. Psychological distress, perceived stigma, and coping among caregivers of patients with schizophrenia. Psychol Res Behav Manag. 2016;9:211–218. doi: 10.2147/PRBM.S112129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jansen JE, Lysaker PH, Harder S, Haahr UH, Lyse HG, Pedersen MB, et al. Positive and negative caregiver experiences in first-episode psychosis: emotional overinvolvement, wellbeing and metacognition. Psychol Psychother. 2014;87(3):298–310. doi: 10.1111/papt.12014. [DOI] [PubMed] [Google Scholar]
- 31.Wang A, Bai X, Lou T, Pang J, Tang S. Mitigating distress and promoting positive aspects of caring in caregivers of children and adolescents with schizophrenia: mediation effects of resilience, hope, and social support. Int J Ment Health Nurs. 2020;29(1):80–91. doi: 10.1111/inm.12651. [DOI] [PubMed] [Google Scholar]
- 32.Ganguly KK, Chadda RK, Singh TB. Caregiver burden and coping in schizophrenia and bipolar disorder: a qualitative study. Am J Psychiatric Rehabil. 2010;13(2):126–142. doi: 10.1080/15487761003757009. [DOI] [Google Scholar]
- 33.Goossens PJ, Van Wijngaarden B, Knoppert-van Der Klein EA, Van Achterberg T. Family caregiving in bipolar disorder: caregiver consequences, caregiver coping styles, and caregiver distress. Int J Soc Psychiatry. 2008;54(4):303–316. doi: 10.1177/0020764008090284. [DOI] [PubMed] [Google Scholar]
- 34.Vargas-Huicochea I, Berenzon S, Rascon ML, Ramos L. A bittersweet relationship: what does it mean to be the caregiver of a patient with bipolar disorder? Int J Soc Psychiatry. 2018;64(3):207–216. doi: 10.1177/0020764018758124. [DOI] [PubMed] [Google Scholar]
- 35.Hayes JF, Miles J, Walters K, King M, Osborn DP. A systematic review and meta-analysis of premature mortality in bipolar affective disorder. Acta Psychiatr Scand. 2015;131(6):417–425. doi: 10.1111/acps.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hayes JF, Marston L, Walters K, King MB, Osborn DPJ. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000-2014. Br J Psychiatry. 2017;211(3):175–181. doi: 10.1192/bjp.bp.117.202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Voort TY, Goossens PJ, van der Bijl JJ. Burden, coping and needs for support of caregivers for patients with a bipolar disorder: a systematic review. J Psychiatr Ment Health Nurs. 2007;14(7):679–687. doi: 10.1111/j.1365-2850.2007.01158.x. [DOI] [PubMed] [Google Scholar]
- 38.Perlick D, Rosenheck RR, Clarkin JF, Raue P, Sirey J. Impact of family burden and patient symptom status on clinical outcome in bipolar affective disorder. J Nerv Ment Dis. 2001;189(1):31–37. doi: 10.1097/00005053-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Perlick D, Rosenheck RA, Miklowitz DJ, Kaczynski R, Link B, Ketter T, et al. Caregiver burden and health in bipolar disorder: a cluster analytic approach. J Nerv Ment Dis. 2008;196(6):484–491. doi: 10.1097/NMD.0b013e3181773927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogilvie AD, Morant N, Goodwin GM. The burden on informal caregivers of people with bipolar disorder. Bipolar Disord. 2005;7(Suppl 1):25–32. doi: 10.1111/j.1399-5618.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 41.Millier A, Schmidt U, Angermeyer MC, Chauhan D, Murthy V, Toumi M, et al. Humanistic burden in schizophrenia: a literature review. J Psychiatr Res. 2014;54:85–93. doi: 10.1016/j.jpsychires.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 42.Beentjes TA, Goossens PJ, Poslawsky IE. Caregiver burden in bipolar hypomania and mania: a systematic review. Perspect Psychiatr Care. 2012;48(4):187–197. doi: 10.1111/j.1744-6163.2012.00328.x. [DOI] [PubMed] [Google Scholar]
- 43.Steele A, Maruyama N, Galynker I. Psychiatric symptoms in caregivers of patients with bipolar disorder: a review. J Affect Disord. 2010;121(1–2):10–21. doi: 10.1016/j.jad.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 44.Fekadu W, Mihiretu A, Craig TKJ, Fekadu A. Multidimensional impact of severe mental illness on family members: systematic review. BMJ Open. 2019;9(12):e032391. doi: 10.1136/bmjopen-2019-032391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yıldırım S. Caregiver burden in chronic mental illness: a systematic review. J Psychiatr Nurs. 2017. 10.14744/phd.2017.60783.
- 46.Covidence [Computer program] [Internet]. 2019 [cited Version accessed July 2019].
- 47.Ryan R, Synnot A, Prictor M, Hill S. Cochrane consumers and communication group data extraction template for included studies. Melbourne: La Trobe University; 2016. [Google Scholar]
- 48.U.S. Department of Health and Human Services . Quality assessment tool for observational cohort and cross-sectional studies. 2019. [Google Scholar]
- 49.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Joanna Briggs institute Reviewer's manual. The Joanna Briggs Institute; 2017. Chapter 5: systematic reviews of prevalence and incidence. [Google Scholar]
- 50.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blanthorn-Hazell S, Gracia A, Roberts J, Boldeanu A, Judge D. A survey of caregiver burden in those providing informal care for patients with schizophrenia or bipolar disorder with agitation: results from a European study. Ann General Psychiatry. 2018;17:8. doi: 10.1186/s12991-018-0178-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chadda RK, Singh TB, Ganguly KK. Caregiver burden and coping: a prospective study of relationship between burden and coping in caregivers of patients with schizophrenia and bipolar affective disorder. Soc Psychiatry Psychiatr Epidemiol. 2007;42(11):923–930. doi: 10.1007/s00127-007-0242-8. [DOI] [PubMed] [Google Scholar]
- 54.Chakrabarti S, Gill S. Coping and its correlates among caregivers of patients with bipolar disorder: a preliminary study. Bipolar Disord. 2002;4(1):50–60. doi: 10.1034/j.1399-5618.2002.01167.x. [DOI] [PubMed] [Google Scholar]
- 55.Chakrabarti S, Nehra R, Sharma S. Distress associated with symptoms of schizophrenia and bipolar disorder: the caregiver’s perspective. J Mental Health Hum Behav. 2003;8:39–50. [Google Scholar]
- 56.Chang CC, Yen CF, Jang FL, Su JA, Lin CY. Comparing affiliate stigma between family caregivers of people with different severe mental illness in Taiwan. J Nerv Ment Dis. 2017;205(7):542–549. doi: 10.1097/NMD.0000000000000671. [DOI] [PubMed] [Google Scholar]
- 57.Chien WT, Chan ZC, Chan SW. Testing the psychometric properties of a Chinese version of the level of expressed emotion scale. ScientificWorldJournal. 2014;2014:905950. doi: 10.1155/2014/905950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fekih-Romdhane F, Ben Ali S, Ghazouani N, Tira S, Cheour M. Burden in Tunisian family caregivers of older patients with schizophrenia Spectrum and bipolar disorders; associations with depression, anxiety, stress, and quality of life. Clin Gerontol. 2020;43(5):545–557. doi: 10.1080/07317115.2020.1728600. [DOI] [PubMed] [Google Scholar]
- 59.Grover S, Chakrabarti S, Aggarwal M, Avasthi A, Kulhara P, Sharma S, et al. Comparative study of the experience of caregiving in bipolar affective disorder and schizophrenia. Int J Soc Psychiatry. 2011;58(6):614–622. doi: 10.1177/0020764011419054. [DOI] [PubMed] [Google Scholar]
- 60.Grover S, Chakrabarti S, Ghormode D, Dutt A, Kate N, Kulhara P. Clinicians’ versus caregivers’ ratings of burden in patients with schizophrenia and bipolar disorder. Int J Soc Psychiatry. 2014;60(4):330–336. doi: 10.1177/0020764013488708. [DOI] [PubMed] [Google Scholar]
- 61.Grover S, Chakrabarti S, Ghormode D, Dutt A. A comparative study of caregivers’ perceptions of health-care needs and burden of patients with bipolar affective disorder and schizophrenia. Nord J Psychiatry. 2015;69(8):629–636. doi: 10.3109/08039488.2015.1033010. [DOI] [PubMed] [Google Scholar]
- 62.Grover S, Avasthi A, Singh A, Dan A, Neogi R, Kaur D, et al. Stigma experienced by caregivers of patients with severe mental disorders: a nationwide multicentric study. Int J Soc Psychiatry. 2017;63(5):407–417. doi: 10.1177/0020764017709484. [DOI] [PubMed] [Google Scholar]
- 63.Ak M, Yavuz KF, Lapsekili N, Turkcapar MH. Kronik Psikiyatrik Bozukluğu Bulunan Hastaların Ve Bakım Verenlerinin Bakım Yükü Açısından Değerlendirilmesi / Evaluation Of Burden in A Group of Patients That Have Chronic Psychiatric Disorders And Their Caregivers. Dusunen Adam: J Psychiatry Neurol Sci. 2012. 10.5350/dajpn2012250405.
- 64.Nehra R, Chakrabarti S, Kulhara P, Sharma R. Caregiver-coping in bipolar disorder and schizophrenia--a re-examination. Soc Psychiatry Psychiatr Epidemiol. 2005;40(4):329–336. doi: 10.1007/s00127-005-0884-3. [DOI] [PubMed] [Google Scholar]
- 65.Ramírez A, Palacio JD, Vargas C, Díaz-Zuluaga AM, Duica K, Agudelo Berruecos Y, et al. Expressed emotions, burden and family functioning in schizophrenic and bipolar I patients of a multimodal intervention programme: PRISMA. Rev Colombiana de Psiquiatría (English ed) 2017;46(1):2–11. doi: 10.1016/j.rcpeng.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 66.Rodrigo C, Fernando T, Rajapakse S, De Silva V, Hanwella R. Caregiver strain and symptoms of depression among principal caregivers of patients with schizophrenia and bipolar affective disorder in Sri Lanka. Int J Ment Health Syst. 2013;7(1):2. doi: 10.1186/1752-4458-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roychaudhuri J, Mondal D, Boral A, Bhattacharya D. Family burden among long term psychiatric patients. Indian J Psychiatry. 1995;37(2):81–85. [PMC free article] [PubMed] [Google Scholar]
- 68.Sharma R, Sharma SC, Pradhan SN. Assessing caregiver burden in caregivers of patients with schizophrenia and bipolar affective disorder in Kathmandu medical college. J Nepal Health Res Counc. 2018;15(3):258–263. doi: 10.3126/jnhrc.v15i3.18851. [DOI] [PubMed] [Google Scholar]
- 69.Singh PM, Prajapati A. Burden of schizophrenia on caregivers in Nepal. Nepal Med Coll J. 2013;15(2):140–143. [PubMed] [Google Scholar]
- 70.Vasudeva S, Sekhar CK, Rao PG. Caregivers burden of patients with schizophrenia and bipolar disorder: a sectional study. Indian J Psychol Med. 2013;35(4):352–357. doi: 10.4103/0253-7176.122224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Webb C, Pfeiffer M, Mueser KT, Gladis M, Mensch E, DeGirolamo J, et al. Burden and well-being of caregivers for the severely mentally ill: the role of coping style and social support. Schizophr Res. 1998;34(3):169–180. doi: 10.1016/s0920-9964(98)00089-9. [DOI] [PubMed] [Google Scholar]
- 72.Zendjidjian X, Richieri R, Adida M, Limousin S, Gaubert N, Parola N, et al. Quality of life among caregivers of individuals with affective disorders. J Affect Disord. 2012;136(3):660–665. doi: 10.1016/j.jad.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 73.Zhou Y, Rosenheck R, Mohamed S, Ou Y, Ning Y, He H. Comparison of burden among family members of patients diagnosed with schizophrenia and bipolar disorder in a large acute psychiatric hospital in China. BMC Psychiatry. 2016;16(1):283. doi: 10.1186/s12888-016-0962-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abdeta T, Desalegn D. Common mental disorders among informal primary caregivers of adults with mental illness during the coronavirus disease 2019 epidemic in eastern Ethiopia: a cross-sectional study. Front Psych. 2021:12. 10.3389/fpsyt.2021.676379. [DOI] [PMC free article] [PubMed]
- 75.Cohen M, Lima AFBS, Silva CPA, Miguel SRPS, Fleck MPA. Quality of life of family primary caregivers of individuals with bipolar disorder and schizophrenia in south of Brazil. Int J Soc Psychiatry. 2021:207640211006737. 10.1177/00207640211006737. [DOI] [PubMed]
- 76.Ukpong D, Ibigbami O. Correlates of quality of life in caregivers of patients with schizophrenia and bipolar affective disorder: a study from southwestern Nigeria. Turk Psikiyatri Dergisi. 2021;32(1):26–32. doi: 10.5080/u25125. [DOI] [PubMed] [Google Scholar]
- 77.Udoh EE, Omorere DE, Sunday O, Osasu OS, Amoo BA. Psychological distress and burden of care among family caregivers of patients with mental illness in a neuropsychiatric outpatient clinic in Nigeria. PLoS One. 2021;16(5):e0250309. doi: 10.1371/journal.pone.0250309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Asl MA, Shojaee A, Shariati B, Rasoolian M, Rashedi V. A comparative study on the burden of disease of schizophrenia, bipolar disorder type I, and autism Spectrum disorder on the family caregivers in Iran. Arch Rehabil. 2021;22(3):320–340. doi: 10.32598/RJ.22.3.3143.1. [DOI] [Google Scholar]
- 79.Khatoon K, Dhamija S, Gupta N, Padhi D, Kiran M, Chaudhury S. Pattern of burden on the family of patients with schizophrenia and bipolar disorder: a comparative study. Ind Psychiatry J. 2021;30(Suppl 1):S178–SS83. doi: 10.4103/0972-6748.328811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.van Wijngaarden B, Schene AH, Koeter M, Vazquez-Barquero JL, Knudsen HC, Lasalvia A, et al. Caregiving in schizophrenia: development, internal consistency and reliability of the involvement evaluation questionnaire--European version. EPSILON study 4. European psychiatric services: inputs linked to outcome domains and needs. Br J Psychiatry Suppl. 2000;39:s21–s27. doi: 10.1192/bjp.177.39.s21. [DOI] [PubMed] [Google Scholar]
- 81.Thara R, Padmavati R, Kumar S, Srinivasan L. Instrument to assess burden on caregivers of chronic mentally ill. Indian J Psychiatry. 1998;40(1):21–29. [PMC free article] [PubMed] [Google Scholar]
- 82.Chou KR, Jiann-Chyun L, Chu H. The reliability and validity of the Chinese version of the caregiver burden inventory. Nurs Res. 2002;51(5):324–331. doi: 10.1097/00006199-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 83.Pai S, Kapur RL. The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry. 1981;138:332–335. doi: 10.1192/bjp.138.4.332. [DOI] [PubMed] [Google Scholar]
- 84.Sell H. The subjective well-being inventory (SUBI) Int J Mental Health. 1994;23(3):89–102. doi: 10.1080/00207411.1994.11449289. [DOI] [Google Scholar]
- 85.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 86.Sullivan MT. The modified caregiver strain index (CSI) Urol Nurs. 2007;27:251–252. [PubMed] [Google Scholar]
- 87.Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the experience of caregiving inventory. Soc Psychiatry Psychiatr Epidemiol. 1996;31(3–4):137–148. doi: 10.1007/BF00785760. [DOI] [PubMed] [Google Scholar]
- 88.Reinares M, Vieta E, Colom F, Martínez-Arán A, Torrent C, Comes M, et al. Evaluación de la carga familiar: Una propuesta de escala autoaplicada derivada de la escala de desempeño psicosocial. Rev Psiquiatría Facultad Med Barcelona. 2004;31(1):7–13. [Google Scholar]
- 89.Herz MI, Endicott J, Spitzer RL. Brief versus standard hospitalization: the families. Am J Psychiatry. 1976;133(7):795–801. doi: 10.1176/ajp.133.7.795. [DOI] [PubMed] [Google Scholar]
- 90.Tessler R, Gamache G. Evaluating family experiences with severe mental illness. Cambridge: Health Services Research Institute Evaluation Center; 1993. [Google Scholar]
- 91.Lee Y, Yang M-J, Lai T-J, Chiu N-M, Chau T-T. Development of the Taiwanese depression questionnaire. Chang Gung Med J. 2000;23(11):688–694. [PubMed] [Google Scholar]
- 92.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 93.Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. 1979;9(1):139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 94.Radloff LS. The CES-D scale. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 95.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 96.Dupuy H. The psychological section on the current health and nutrition examination survey. In: Statistics NCoH, editor. Proc public health conference on records and statistics meeting jointly with the National Conference on health statistics. Washington, DC: National Center of Health Statistics; 1972. [Google Scholar]
- 97.Sartorius N, Janca A. Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol. 1996;31(2):55–69. doi: 10.1007/BF00801901. [DOI] [PubMed] [Google Scholar]
- 98.Ware J, The MOS. 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 99.World Health Organization Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 100.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 101.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 102.Shiraishi N, Reilly J. Positive and negative impacts of schizophrenia on family caregivers: a systematic review and qualitative meta-summary. Soc Psychiatry Psychiatr Epidemiol. 2019;54(3):277–290. doi: 10.1007/s00127-018-1617-8. [DOI] [PubMed] [Google Scholar]
- 103.Conus P, Macneil C, McGorry PD. Public health significance of bipolar disorder: implications for early intervention and prevention. Bipolar Disord. 2014;16(5):548–556. doi: 10.1111/bdi.12137. [DOI] [PubMed] [Google Scholar]
- 104.Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, et al. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am J Psychiatry. 2010;167(9):1116–1124. doi: 10.1176/appi.ajp.2010.09101406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dalgleish T, Black M, Johnston D, Bevan A. Transdiagnostic approaches to mental health problems: current status and future directions. J Consult Clin Psychol. 2020;88(3):179–195. doi: 10.1037/ccp0000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Newby JM, McKinnon A, Kuyken W, Gilbody S, Dalgleish T. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev. 2015;40:91–110. doi: 10.1016/j.cpr.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 107.Perlick D, Clarkin JF, Sirey J, Raue P, Greenfield S, Struening E, et al. Burden experienced by care-givers of persons with bipolar affective disorder. Br J Psychiatry. 1999;175:56–62. doi: 10.1192/bjp.175.1.56. [DOI] [PubMed] [Google Scholar]
- 108.Mueser KT, Webb C, Pfeiffer M, Gladis M, Levinson DF. Family burden of schizophrenia and bipolar disorder: perceptions of relatives and professionals. Psychiatr Serv. 1996;47(5):507–511. doi: 10.1176/ps.47.5.507. [DOI] [PubMed] [Google Scholar]
- 109.Ge L, Mordiffi SZ. Factors associated with higher caregiver burden among family caregivers of elderly Cancer patients: a systematic review. Cancer Nurs. 2017;40(6):471–478. doi: 10.1097/NCC.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 110.Figved N, Myhr KM, Larsen JP, Aarsland D. Caregiver burden in multiple sclerosis: the impact of neuropsychiatric symptoms. J Neurol Neurosurg Psychiatry. 2007;78(10):1097–1102. doi: 10.1136/jnnp.2006.104216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mosley PE, Moodie R, Dissanayaka N. Caregiver burden in Parkinson disease: a critical review of recent literature. J Geriatr Psychiatry Neurol. 2017;30(5):235–252. doi: 10.1177/0891988717720302. [DOI] [PubMed] [Google Scholar]
- 112.Rigby H, Gubitz G, Phillips S. A systematic review of caregiver burden following stroke. Int J Stroke. 2009;4(4):285–292. doi: 10.1111/j.1747-4949.2009.00289.x. [DOI] [PubMed] [Google Scholar]
- 113.Etters L, Goodall D, Harrison BE. Caregiver burden among dementia patient caregivers: a review of the literature. J Am Acad Nurse Pract. 2008;20(8):423–428. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 114.Cherry MG, Taylor PJ, Brown SL, Rigby JW, Sellwood W. Guilt, shame and expressed emotion in carers of people with long-term mental health difficulties: a systematic review. Psychiatry Res. 2017;249:139–151. doi: 10.1016/j.psychres.2016.12.056. [DOI] [PubMed] [Google Scholar]
- 115.Poon AWC, Curtis J, Ward P, Loneragan C, Lappin J. Physical and psychological health of carers of young people with first episode psychosis. Australas Psychiatry. 2018;26(2):184–188. doi: 10.1177/1039856217748250. [DOI] [PubMed] [Google Scholar]
- 116.Zeng Y, Zhou Y, Lin J. Perceived burden and quality of life in Chinese caregivers of people with serious mental illness: a comparison cross-sectional survey. Perspect Psychiatr Care. 2017;53(3):183–189. doi: 10.1111/ppc.12151. [DOI] [PubMed] [Google Scholar]
- 117.Whalen KJ, Buchholz SW. The reliability, validity and feasibility of tools used to screen for caregiver burden: a systematic review. JBI Libr Syst Rev. 2009;7(32):1373–1430. doi: 10.11124/01938924-200907320-00001. [DOI] [PubMed] [Google Scholar]
- 118.Perlick D, Rosenheck RA, Miklowitz DJ, Chessick C, Wolff N, Kaczynski R, et al. Prevalence and correlates of burden among caregivers of patients with bipolar disorder enrolled in the systematic treatment enhancement program for bipolar disorder. Bipolar Disord. 2007;9(3):262–273. doi: 10.1111/j.1399-5618.2007.00365.x. [DOI] [PubMed] [Google Scholar]
- 119.Raj E, Shiri S, Jangam K. Subjective burden, psychological distress, and perceived social support among caregivers of persons with schizophrenia. Indian J Soc Psychiatry. 2016;32(1). 10.4103/0971-9962.176767.
- 120.Bowman S, Alvarez-Jimenez M, Wade D, Howie L, McGorry P. The positive and negative experiences of caregiving for siblings of young people with first episode psychosis. Front Psychol. 2017;8:730. doi: 10.3389/fpsyg.2017.00730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tamizi Z, Fallahi-Khoshknab M, Dalvandi A, Mohammadi-Shahboulaghi F, Mohammadi E, Bakhshi E. Defining the concept of family caregiver burden in patients with schizophrenia: a systematic review protocol. Syst Rev. 2019;8(1):289. doi: 10.1186/s13643-019-1182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jansen JE, Gleeson J, Cotton S. Towards a better understanding of caregiver distress in early psychosis: a systematic review of the psychological factors involved. Clin Psychol Rev. 2015;35:56–66. doi: 10.1016/j.cpr.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 123.Sin J, Gillard S, Spain D, Cornelius V, Chen T, Henderson C. Effectiveness of psychoeducational interventions for family carers of people with psychosis: a systematic review and meta-analysis. Clin Psychol Rev. 2017;56:13–24. doi: 10.1016/j.cpr.2017.05.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data, search strategies and appraisals of included studies are available from the corresponding author upon request.