Abstract
Previous studies have shown that Taijiquan and Qigong exercise can effectively reduce depression and anxiety in healthy and clinical populations. At present, only a few reviews have elaborated on the premise of different types of interventions, and there is still a lack of studies that systematically summarize the clinical evidence of patients with substance use disorders. The purpose of this meta-analysis was to assess the impact of the Taijiquan and Qigong exercise on the mood of individuals with substance use disorders (SUD); Articles were searched in Pubmed, Embase, Cochrane Library, Web of Science, and CNKI from their inception to the May 24, 2021. All randomized controlled trials (RCT) using Taijiquan and Qigong intervention were included. With the Review Manager software to determine the effect (standardized mean difference, SMD), subgroup analysis was conducted to intervention type, exercise time, and exercise duration. Nine studies totaling 823 participants were included in the study. Overall results indicated that Taijiquan and Qigong exercise had significant benefits in reducing depression (SMD = −0.35, 95% CI: −0.53 to −0.18, Z = 4.00, p < 0.01) and anxiety (SMD = −0.31, 95% CI: −0.50 to −0.11, Z = 3.06, p < 0.01) symptoms in SUD. When depression and anxiety were examined separately, subgroup analysis demonstrated that Taijiquan intervention (SMD = −0.45, 95% CI: −0.71 to −0.19, Z = 3.39, p < 0.01) and Qigong intervention (SMD = −0.28, 95% CI −0.51 to −0.04, Z = 2.33, p = 0.02),30–60 min exercise time (SMD = −0.41, 95% CI: −0.61 to −0.20, Z = 3.82, p < 0.01) and duration of 9–12 weeks (SMD = −0.57, 95% CI: −1.10 to −0.04, Z = 2.10, p = 0.04) more than 12 weeks (SMD = −0.28, 95% CI: −0.50 to −0.07, Z = 2.59, p = 0.01) could effectively alleviate the symptoms of depression. Meanwhile, Qigong intervention (SMD = −0.31, 95% CI: −0.52 to −0.10, Z = 2.85, p < 0.01), 30–60 min exercise time (SMD = −0.29, 95% CI: −0.53 to −0.04, Z = 2.28, p = 0.02), more than 60 min exercise time (SMD = −0.54, 95% CI: −1.06 to −0.02, Z = 2.05, p = 0.04), and duration of less than 9 weeks (SMD = −0.35, 95% CI: −0.68 to −0.02, Z = 2.07, p = 0.04) had positive effects on alleviating anxiety symptoms with SUD. Taijiquan and Qigong exercise could reduce levels of anxiety and depression in those with SUD. Considering the small number of included studies, more reliable RCTs are needed on this topic.
Keywords: Depression, Anxiety, Substance abuse disorder, Exercise, Taijiquan, Qigong
Introduction
Substance abuse is a global problem that encompasses the misuse of alcohol, tobacco, heroin, and synthetic drugs. According to the World Health Organization, in 2016, approximately 275 million people worldwide used drugs at least once, accounting for 5.6% of the world's population in the age range of 15–64 years.1 In 2017, about 585,000 people died from drug abuse.2 Numerous studies have shown that drug-dependent people generally suffer from affective disturbances. Drug abuse can cause chronic illness3; long-term abuse may also lead to symptoms such as anxiety, depression, insomnia, and impaired social functioning.4, 5, 6, 7, 8 Opioid dependence is one of the most severe types of drug dependency.9 Currently, the treatment of drug dependency relies on drug replacement therapy, in which either methadone or buprenorphine is used to treat opioid addiction.10,11 However, methadone or buprenorphine use is a risk factor for addiction, and overuse of either substances may lead to serious health and social problems.12,13 There is currently no effective way to manage the toxic effects of drugs, including those of synthetic drugs.14 Increasing physical activity levels has been shown to improve mental health by reducing the risk of depression,15, 16, 17 anxiety, and other stress-related disorders.18,19 Physical exercise has recently been used to treat mental illness,20 such as anorexia nervosa,21 bulimia, and alcohol and substance abuse disorders.22 Exercise may be a complementary approach to pharmacological and psychological interventions because it is non-discriminatory.23 Exercise and movement may aid smoking cessation, enhancing mood, reducing negative affect, and decreasing the severity of withdrawal symptoms.24, 25, 26
Qigong and Taijiquan are two of the most popular traditional Chinese exercise and martial arts modalities, respectively, known as mind-body exercise therapy. Qigong is older than Taijiquan and is considered a kind of “medical” movement in the field of Chinese medicine.27 Recently, both modalities have attracted research attention due to their efficacy in treating mental diseases, mood disorders, and other secondary diseases. Both modalities represent mind-body exercises, helping achieve physical and mental health harmony through body movements, regular breathing, and adjustments of the mind. Taijiquan and Qigong exercise can effectively relieve depression and anxiety symptoms among drug abusers.28,29 Previous studies have shown promising effects of Taijiquan or Qigong practice on improving depression and anxiety in otherwise healthy adults,30 young people with major depressive disorder,31 obese women,32 cancer patients,33 and chronic obstructive pulmonary disease patients.34,35 However, previous studies have used both modalities at varied frequencies and over different periods; therefore, their effects on the levels of anxiety, depression, and overall mood in patients with substance use disorders (SUD) remain unclear. The present meta-analysis aimed to clarify the impact of these exercise modalities on the mood of patients with SUD, accounting for the differences in exercise type, and session and practice duration.
Materials and methods
Search strategy
The literature search was conducted in PUBMED, Web of Science, EMBASE, Cochrane Library, and China National Knowledge Infrastructure databases, covering the period from database inception to the May 24, 2021. There were no restrictions on the publication date or language. Databases were searched using the following terms: Tai Ji, Tai Chi, Tai Ji Quan, Taijiquan, T'ai Chi, Tai Chi Chuan, Qigong, Qi Gong, Qi-gong, Chi Kung, Chi Chung, Qi-training, Qigong Massage, Health Qigong, Meditation, Meditative Movement, Liuzijue, Wuqinxi, Yijinjing, Baduanjin, Traditional Exercise, Chinese Traditional Exercise, Substance-Related Disorders, Alcohol, Tobacco, Nicotine, Heroin, Morphine, Marijuana, Cannabis, Opioid, Cocaine, Methamphetamine, Drug Abuse, Drug Addiction, Drug Dependence, Drug Use Disorder, Substance Use, Substance Abuse, Depression, Anxiety, Mental Health, Mental Problem, Psychological Health, and Psychological Problem. Chinese translations of these terms were used for Chinese database searches. A complete record of search strings is provided in the supplementary file. We manually searched the reference lists of all included studies and relevant reviews to identify any additional potentially relevant studies. If an article was incomplete or its full text was unavailable, we contacted the corresponding author by email to obtain detailed information. For literature tracing, based on the retrieved literature or related references listed in the review, we used Baidu Scholar and Google Scholar to search for them retrospectively.
Eligibility criteria
Only randomized clinical trials (RCT) of interventions for depression and anxiety in individuals aged ≥18 years and diagnosed with SUD were included. Reviews, comments, conference abstracts, and book chapters were excluded.
To be included in the meta-analysis, a study must have included both an experimental group that received Taijiquan or Qigong exercise, and a control condition that included hospital routine care, no treatment, or other types of intervention (e.g., medication).
The main outcomes were depression and anxiety symptoms. Outcome measures included the Hamilton Anxiety Scale, Beck Depression Inventory, Profile of Mood States, State-Trait Anxiety Inventory, Hamilton Rating Scale for Depression, Self-Rating Anxiety Scale, Hospital Anxiety and Depression Scale, Symptom Checklist-90, and Self-Rating Depression Scale scores.
Study selection and data extraction
Two reviewers (Zhang and Yang, respectively) extracted and cross-checked trial data. The decision to include a study was made primarily based on its title and abstract; in cases where title and abstract were insufficient to determine study eligibility, full-text reading was performed. Inconsistencies were resolved by a third independent reviewer and group discussion, as required (Ma). We extracted data on the following variables: publication year, first author name, study design (e.g., intervention model, practice time, persistence time, and outcome measurements), and participant characteristics (e.g. age, sex, and sample size). Risk of bias evaluation details are presented in Table 1.
Table 1.
Characteristics of included studies.
| Study name | Location (Language) | Substance | Sample Size (Attrition Rate) | Sample size (Mean age ±SD) | Intervention Program |
Training |
Outcome measures | ||
|---|---|---|---|---|---|---|---|---|---|
| Frequency (Week) | Time (Min) | Duration (Week) | |||||||
| Li et al. (2002)37 | Guangzhou, China (English) |
Heroin | 86,0% | E:n = 34 (33.3 ± 6.5) C 1:n = 26 (31.9 ± 5.9) C 2:n = 26 (31.7 ± 6.1) |
E = Pangu Qigong C1 = Medication C2 = No treatment |
7 | 120–150 | 1 week +3 days |
HAS |
| Li et al. (2013)38 | Yunnan, China (English) |
Heroin | 70,53% | E: n = 36 (30.7 ± 6.3) C:n= 34 (30.7 ± 6.3) |
E = Taijiquan C = Treatment as usual |
14 | 60 | 24 weeks | HRSD |
| Zhu et al. (2018)39 | Shanghai, China (English) |
Amphetamine-drugs | 80,39% | E:n = 40 (33.74 ± 7.1) C:n = 40 (37.76 ± 9.85) |
E = 24−posture Taijiquan routine C = the 9th Guang Bo Ti Cao |
1–3 months =5 4–6 months =3 |
60 | 24 weeks | SDS |
| Oh et al. (2016)40 | Jeungpyeong, Korea (English) | Alcohol | 50,24% | E:n = 25 (45.4 ± 7.8) C:n = 25 (48.1 ± 11.5) |
E = 24−posture Taijiquan routine C = Hospital−rehabilitation program |
3 | 50 | 8 weeks | BDI |
| Geng et al. (2016)41 | Shanghai, China (Chinese) |
Amphetamine-drugs | 60,5% | E:n = 30 (34 ± 7) C:n = 30 (37.76 ± 9.85) |
E = Yang−style Taijiquan C = the 9th Guang Bo Ti Cao |
5 | 45 | 12 weeks | SCL-90 |
| Huang et al. (2015)42 | Guangdong, China (Chinese) |
Heroin | 100,13% | E:n = 50 (35.26 ± 12.22) C:n = 50 (35.21 ± 12.12) |
E = Qigong (Baduanjin) +Medication C = Medication |
14 | 30 | 20 weeks | SAS |
| Zhang et al. (2020)43 |
Heze, China (English) |
Amphetamine-drugs |
76,5% |
E:n = 38 (41.08 ± 9.94) C:n = 38 (39.11 ± 8.90) |
E = 24−posture Taijiquan routine C = the 9th Guang Bo Ti Cao |
5 |
80 |
24 weeks |
BDI |
| David et al. (2013)44 | Bedford, USA (English) | Cocaine | 101,17% | E:n = 51 (36.0 ± 9.4) C:n = 50 (40.4 ± 11.9) |
E = Qigong C = Sham Qigong |
2–3 | 15 | 2 weeks | BDI STAIT |
| Fu et al. (2016)45 | Anhui, China (Chinese) | Amphetamine-drugs | 200,0% | E:n = 100 (28.3 ± 7.83) C:n = 100 (27.99 ± 8.17) |
E = Qigong (Wuqinxi) C = No treatment |
7 | 30 | 20 weeks | SAS SDS |
1 E-experiment group; C-control group; HAS-Hamilton Anxiety Scales; BDI-Beck Depression Inventory; STAIT-Trait Anxiety Inventory; POMS-Profile of Mood States; HRSD-Hamilton Rating Scale for Depression; SCL−90-Symptom Checklist 90; SAS-Self−Rating Anxiety Scale; SDS Self-Rating Depression Scale.
Study quality assessment
Two authors (Zhang and Yang) evaluated the risk of bias in each study using a tool provided by the Cochrane Collaboration.36 We evaluated seven key domains: allocation concealment, sequence generation, blinding of participants and personnel, incomplete outcome data, blinding of outcome assessment, selective outcome reporting, and other sources of bias. The risk of bias was classified as low, unclear, or high for each included study. Discrepancies in assessments were resolved by a third party.
Study analysis method
The Review Manager (version: 5.4.1, Cochrane, UK) was used for statistical analysis. For continuous outcomes, we calculated the standardized mean difference (SMD) and 95% confidence intervals (95% CI). The I2 statistic was used to assess heterogeneity; fixed- and random-effects models were used to evaluate studies with low (I2 < 50%) and high (I2 ≥ 50%) heterogeneity, respectively. The p-values of < 0.05 indicated statistically significant findings. Subgroup analyses were performed to minimize the impact of heterogeneity on the reported estimates. The included studies varied in terms of exercise type, time, and duration, which were the factors considered in subgroup analysis. The variables of interest were: (a) intervention type (two groups): Taijiquan and Qigong; (b) exercise time (three groups): less than 30 min, 30–60 min, and more than 60 min; and (c) exercise duration (three groups): shorter than 9 weeks, 9–12 weeks, and more than 12 weeks.
Results
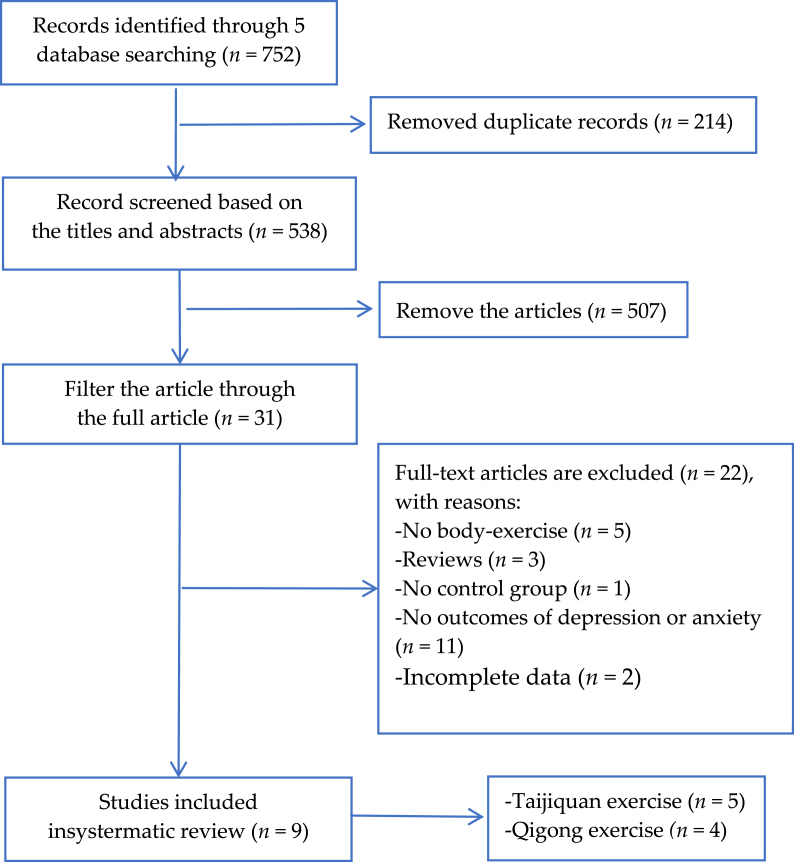
A total of 752 articles were identified. In preliminary screening, we excluded 721 studies based on their title and abstract for reasons including duplications (n = 214) and irrelevance (n = 507). The remaining 31 articles were further screened by reading the full text. Twenty-two studies were removed owing to no body-exercise (n = 5), reviews (n = 3), no control group (n = 1), no outcomes of depression or anxiety (n = 11), incomplete data (n = 2). Finally, the meta-analysis included five and four studies on Taijiquan and Qigong exercises, respectively (Fig. 1).
Fig. 1.
Flow of study selection.
Study characteristics
Selected studies are shown in Table 1. Our systematic review included nine articles.37, 38, 39, 40, 41, 42, 43, 44, 45 Table 1 presents the characteristics of the included studies. These studies used Taijiquan or Qigong exercise modalities as an intervention in the experimental groups, and “hospital routine care”, “no treatment”, and “other types of intervention” in the control groups. Of all included studies, six were published in English37, 38, 39, 40,43,44 and three were published in Chinese.41,42,45 In addition, one study was performed in the United States,44 one was performed in Korea,40 and seven were performed in China.37, 38, 39,41, 42, 43,45 The included participants were dependent on heroin, methamphetamine, amphetamine-type stimulant, K powder, ecstasy, and synthetic drugs. The sample sizes ranged from 50 to 200 participants, with a total of 823 participants (404 and 419 participants in the Taijiquan and Qigong, and control groups, respectively). Four studies included only female participants38, 39, 40, 41,45 and one study included only male participants.37
Selected studies included three styles of Taijiquan. Three of the included articles involved the style of 24-posture,39,40,43 one used the Yang style,41 and one did not specify the exercise style used. Among the studies involving Qigong, one used Pangu Qigong,37 created by Chinese Qigong experts and considered easy to learn and practice; one study used the Baduanjin style,42 one used the Wuqinxi style,45 and one study did not specify the style used.44 One trial compared the effect of Qigong versus that of no treatment and that of medication.37 Intervention duration ranged from 10 days to 24 weeks. All studies examined the effects of Taijiquan and Qigong exercise immediately after the intervention, but few studies reported follow-up outcomes. Seven studies measured depression-related variables,37, 38, 39, 40, 41,43, 44, 45, and five studies measured anxiety-related variables.37,41,42,44,45 The anxiety scales used included the Spielberger State-Trait Anxiety Inventory-State, Hamilton Anxiety Scale, Self-rating Anxiety Scale, and Symptom Checklist-90. Depression scales used included the Hamilton Rating Scale for Depression, Center for Epidemiological Studies Depression Scale, Self-rating Depression Scale, and Symptom Checklist-90.
Methodological quality assessment
Methodological details of the included studies are shown in Table 2. Most included articles failed to report the process of sequence generation and allocation of concealment and were thus classified as “unclear” in the risk of bias domain. Six articles described study drop-outs, and the dropout rate was within reasonable limits (Table 1). Blinding of instructors and participants is impossible in this type of exercise intervention. Therefore, the risk of bias was judged as low for group allocation and result blinding. All studies reported their randomization protocols, including four studies that used random sequence generation processes,37,39,40,45 two studies that used the order of admission to hospital,37,45 and two studies that used digital random tables and computer randomization.39,40 All studies described interventions used in the control group, but only three articles accounted for blinding.39,43,44 One article failed to report the reason for participant loss to follow-up and withdrawal.43,44 Overall, the quality of the included studies was relatively high.
Table 2.
Quality assessment of the included articles.
| Study name | Random sequence generation |
Allocation concealment | Blinding of Participants and personnel | Blinding of outcome assessments |
Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Li et al.(2002)37 | High | Unclear | Unclear | Low | Low | Low | Unclear |
| Li et al.(2013)38 | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Zhu et al.(2018)39 | Low | Low | Low | Unclear | Low | Low | Unclear |
| Oh et al.(2016)40 | Low | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Geng et al.(2016)41 | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Huang et al.(2015)42 | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Zhang et al.(2020)43 | Unclear | Low | Low | Low | Low | Low | Unclear |
| David et al.(2013)44 | Low | Low | Low | Low | Low | Low | Unclear |
| Fu et al.(2016)45 | High | Unclear | Unclear | Unclear | Low | Low | Unclear |
Meta-analysis of outcome indicators
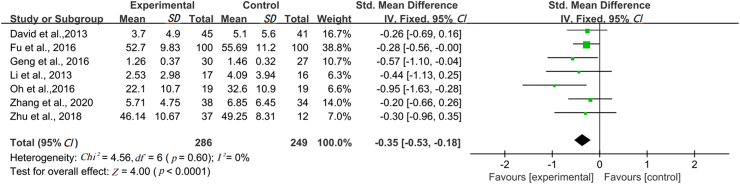
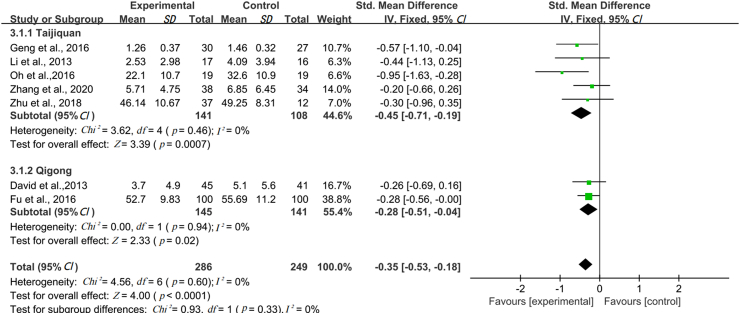
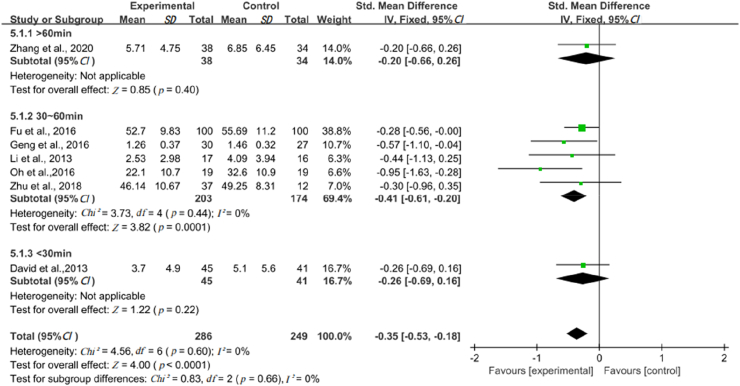
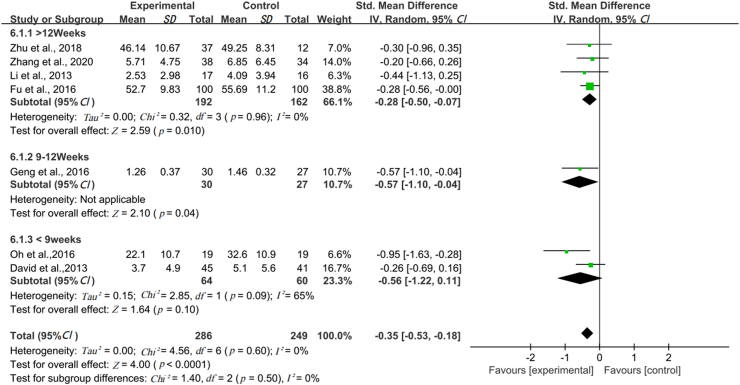
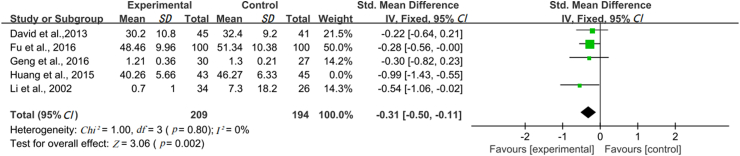
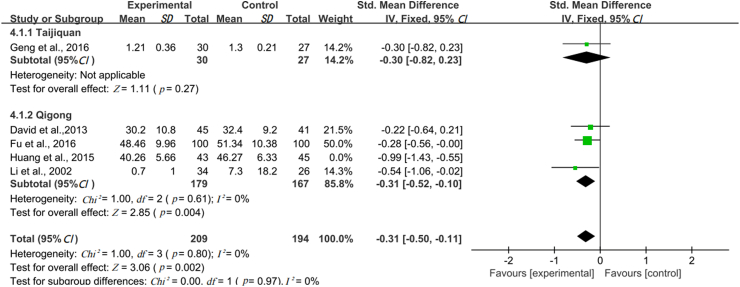
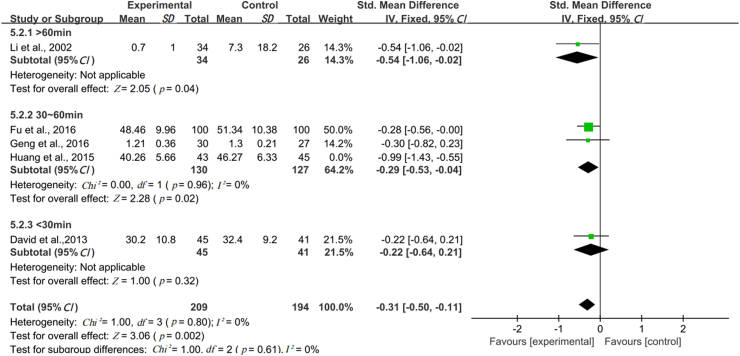
Seven studies (n = 535) were included in the meta-analysis of the impact of Taijiquan and Qigong exercise on depression in SUD patients. Heterogeneity was low (I2 = 0%, p < 0.05) and the fixed-effects model was used for analysis, revealing that, compared with the control intervention, Taijiquan and Qigong exercise practice may alleviate depressive symptoms of SUD patients (SMD = −0.35, 95% CI: −0.53 to −0.18, Z = 4.00, p < 0.01; Fig. 2). A subgroup analysis was conducted to further explore the relationship between moderating variables and depression in drug users, confirming that Taijiquan and Qigong exercises can alleviate depressive symptoms in this group (SMD = −0.45, 95% CI: −0.71 to −0.19, Z = 3.39, p < 0.01, I2 = 0%, and SMD = −0.28, 95% CI −0.51 to −0.04, Z = 2.33, p = 0.02, I2 = 0%, respectively) (Fig. 2, Fig. 3). In addition, 30–60 min of exercise (SMD = −0.41, 95% CI: −0.61 to −0.20, Z = 3.82, p < 0.01; Fig. 4) was more effective at reducing depressive symptoms than the other factors tested. In addition, 9–12 weeks (SMD = −0.57, 95% CI: −1.10 to −0.04, Z = 2.10, p = 0.04) and more than 12 weeks (SMD = −0.28, 95% CI: −0.50 to −0.07, Z = 2.59, p = 0.01) of exercise alleviated symptoms of depression. However, subgroup analysis of two studies with exercise duration of less than 9 weeks revealed high heterogeneity (I2 = 65%); thus, the random-effects model was used for meta-analysis, which revealed some non-significant effects (SMD = −0.56, 95% CI: −1.22 to −0.11, Z = 1.64, p = 0.1; Fig. 5).
Fig. 2.
The forest plot about the effect of Taijiquan and Qigong exercise on depression.
Fig. 3.
The forest plot about the effect of intervention type on depression.
Fig. 4.
The forest plot about the effect of exercise time on depression.
Fig. 5.
The forest plot about the effect of exercise duration on depression.
We included 5 (n = 491) studies in the meta-analysis of the impact of Taijiquan and Qigong exercise on anxiety in SUD patients were as follows. After the heterogeneity test, (I2 = 54%, p = 0.001). It suggests that the 5 groups of data selected in this study have high heterogeneity and heterogeneity lookup is necessary. Through sensitivity analysis of the 5 groups of data, the article written by Huang et al.42 affected heterogeneity after removing the study, which showed that the remaining 4 groups of data (I2 = 0%, p = 0.80) and Effect Size relative risk (RR) could be subjected to meta-analysis with fixed effects. The results showed that compared with the control group, the intervention of Taijiquan and Qigong exercise practice could significantly alleviate anxiety symptoms among SUD patients (SMD = −0.31, 95% CI: −0.50 to −0.11, Z = 3.06, p = 0.002; Fig. 6).
Fig. 6.
The forest plot about the effect of Taijiquan and Qigong exercise on anxiety.
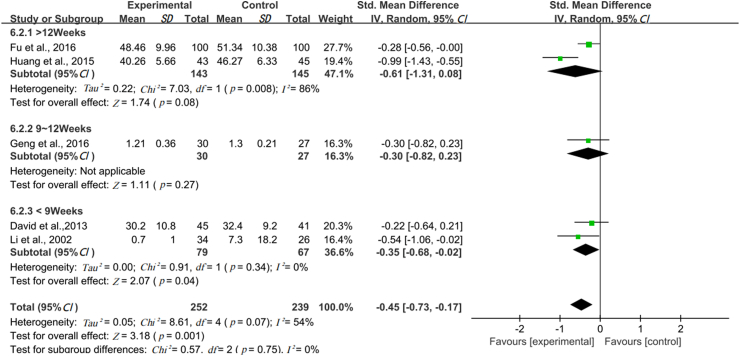
Subgroup analyses were performed based on exercise types. Heterogeneity among the four studies on Qigong exercise was high (I2 = 64%, p = 0.04) suggesting between the data selected in this study. The heterogeneity is statistically significant and requires a heterogeneous lookup. Sensitivity analysis of four literature found that the article written by Huang et al.42 had a great impact on heterogeneity, removed again for heterogeneity test analysis, and the results show the remaining 3 articles There was no heterogeneity (I2 = 0%, p = 0.61), and Effect Size RR could be subjected to meta-analysis with fixed effects (SMD = −0.31, 95% CI: −0.52 to −0.10) and were statistically significant (Z = 2.85, p = 0.004). Subgroup analysis showed that the practice of Qigong exercise can significantly alleviate symptoms of anxiety among SUD patients. In the subgroup analysis of Tai Chi exercise intervention events, since there is only one study on the intervention of anxiety, there is no statistical significance (Fig. 7). About the effect of exercise time on anxiety, 3 groups of data involving exercise 30–60 min, tested for heterogeneity, (I2 = 73%, p = 0.04), suggesting between the data selected in this study. The heterogeneity is statistically significant and requires a heterogeneous lookup. Another heterogeneity test after removing the article of Huang et al.42 showed no heterogeneity between the remaining 2 articles (I2 = 0%, p = 0.96) fixed-effects model (SMD = −0.29, 95% CI: −0.53 to −0.04) and were statistically significant (Z = 2.28, p = 0.02). The results showed more than 60 min exercise time (SMD = −0.54, 95% CI: −1.06 to −0.02, Z = 2.05, p = 0.04) and 30–60 min exercise time (SMD = −0.29, 95% CI: −0.53 to −0.04, Z = 2.28, p = 0.02) were more effective than the other factors tested (Fig. 8). In the 2 articles on the effect of exercise duration on the duration of anxiety for more than 12 weeks, after the heterogeneity test, (I2 = 86%, p = 0.008), indicating that the heterogeneity between the two studies is high, So when choosing random-effects for meta-analysis. The results showed a duration of longer than 12 weeks that are not statistically significant (SMD = −0.61, 95% CI: −1.31 to −0.08, Z = 1.74, p = 0.08). In addition, about the effect of exercise duration on anxiety the duration of shorter than 9 weeks (SMD = −0.35, 95% CI: −0.68 to −0.02, Z = 2.07, p = 0.04), could reduce anxiety symptoms, which were more effective than the other factors tested (Fig. 9).
Fig. 7.
The forest plot about the effect of intervention type on anxiety.
Fig. 8.
The forest plot about the effect of exercise time on anxiety.
Fig. 9.
The forest plot about the effect of exercise duration on anxiety.
Discussion
This meta-analysis aimed to summarize the existing evidence on the impact of Taijiquan and Qigong exercise on the levels of depression and anxiety in SUD patients. The present findings suggest that Taijiquan and Qigong exercise modalities may alleviate depression and anxiety symptoms. Given the safety of these modalities, clinicians may prescribe Taijiquan and Qigong exercise to support treatment for depression and anxiety in SUD patients. The present findings are consistent with those of previous systematic reviews on the effects of Taijiquan and Qigong exercise on the levels of anxiety in SUD patients.46 Overall, Taijiquan and Qigong exercise reduced depression (SMD = −0.35, 95% CI: −0.53 to −0.18, Z = 4.00, p < 0.01) and anxiety (SMD = −0.45, 95% CI: −0.50 to −0.11, Z = 3.06, p < 0.01) levels in SUD patients. Meanwhile, there may be significant heterogeneity in the research of Huang et al.42 compared with the effect size of other studies, they proved to have a great impact on SUD anxiety, Through the analysis of this study, from the event intervention aspect, it was found that the intervention (Qigong + Medication) for SUD patients was different from other studies. Subgroup analysis revealed that Taijiquan and Qigong, 30–60 min exercise time had significant benefits in anxiety symptoms in SUD patients. In addition, exercise duration of more than 9 weeks improved depression symptoms and that of less than 9 weeks improved depression symptoms; these findings are inconsistent with those of some individual studies. Further RCTs on Taijiquan and Qigong in the treatment of anxiety and depression are required to elucidate the underlying mechanisms. Studies that showed the impact of less than 9 weeks of exercise practice on anxiety levels all involved Qigong exercise, suggesting the suitability of this intervention in the short term. Meanwhile, the impact of Taijiquan exercise on anxiety symptoms of SUD patients remains unclear due to the limited number of studies available, suggesting a need for further research.
Substance dependence involves complex mechanisms, including the brain's adaptation to exogenous opioids,47,48 which act on the same receptors as endogenous neurotransmitters such as endorphins and dopamine.49 Endorphins and dopamine are key signaling molecules in the brain's reward circuits, associated with habit and long-term memory formation.50 Studies have reported that exercise improves the mood of drug-dependent individuals mainly by regulating norepinephrine (NE) and glucocorticoid pathways. The sympathetic nervous system and hypothalamic-pituitary-adrenal (HPA) system are both activated in response to stress.51 The adrenal medulla secretes a large amount of NE, increasing NE levels in the ventral tegmental area and nucleus accumbens.52 Elevated NE levels increase CRF secretion in the hypothalamus, activate HPA, and increase corticosterone (CORT) production. CORT crosses the blood-brain barrier and enters the brain,53,54 increasing the levels of serotonin (5-HT) and its metabolite 5-hydroxyindoleacetic acid in the frontal cortex, nucleus accumbens, hypothalamus, and CA. In general, 5-HT acts in synergy with NE. These changes affect the limbic system.55
Moderate-intensity exercise affects the HPA activation–CORT-mediated pathway. The relative reduction in the rate of NE synthesis and activation of the sympathetic nervous system can be achieved through stress management techniques.56 Liu et al.51 used a 12-week Taijiquan training intervention, showing it may increase the physiological adaptability and modulate the reactivity of the sympathetic nervous system, helping reduce the fluctuation of stress-related hormones and levels of depression and anxiety. Taijiquan is characterized by continuous slow movement,57 deep breathing, and mental concentration. Qigong involves Qi and Yi to help achieve inner balance. It consists of meditation, relaxation, guided imagery, deep tranquility, and breathing exercises. Taijiquan and Qigong are both moderate-intensity exercise modalities. The smooth rhythmic motions of Taijiquan and Qigong exercise are usually experienced as relatively pleasurable.58,59 Several studies have assessed the effects of Taijiquan and Qigong on psychological responses, such as depression, stress, and life satisfaction.60, 61, 62, 63 The effects of these modalities may be mediated by moderate rhythmic movement, which increases the parasympathetic tone.39 In addition, both modalities help patients achieve relaxation, and reconnect with their mind, body, and spirit, making them more mindful and internally focused.64 Finally, practicing Taijiquan and Qigong exercises in a group can promote social interaction in interpersonal relationships, providing social support, and benefiting patients’ physical and mental health.63
Cognitive behavioral therapy and other non-drug therapies, such as exercise, acupuncture, and psychotherapy, have become important complementary modalities in treating SUD patients. Although exercise is a low-risk and low-cost intervention, further research is needed to develop evidence-based exercise prescriptions in this patient group.
Our study has several strengths. Relatively few relevant studies have been published, precluding subgroup analysis. However, we examined the impact of the type of intervention, exercise session time, and practice duration on the outcomes of interest. Our review methods were systematic and described in detail. We used extensive search strategies with no constraints on publication date or language. Furthermore, study eligibility criteria were clearly defined, and only RCTs were included in this review. At least two independent reviewers were responsible for study selection, quality assessment, and data extraction.
This study has some limitations. First, only nine studies were included (five on Taijiquan and four on Qigong) and the overall sample size was small. Second, outcomes were difficult to measure; therefore, the presented results should be approached with caution. Moreover, different levels of exercise intensity may differently affect hormonal regulation and the resulting mood; however, exercise intensity was not reported in the examined studies.
Conclusions
Our meta-analysis revealed that Taijiquan and Qigong exercise may improve depression and anxiety symptoms in patients with SUD. In addition, this meta-analysis showed that Qigong exercise duration of less than 9 weeks may reduce anxiety levels in SUD patients. The present findings may provide a foundation for future research and clinical applications. However, the number of studies included was small. Future studies are required to validate the present findings.
Submission statement
All authors have read and agreed to the content of the manuscript, which is not yet published and is not considered for publication elsewhere.
Authors’ contributions
M.X. conceived of and designed the review; M.X., P.Z., Y.Q., L.Z., Z.J. performed the searches and conducted the meta-analysis; all authors analyzed the data including screening of studies, quality assessment, data extraction; P.Z. and M.X. wrote the paper with all authors contributing to the drafting and finalization of the manuscript.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgement
This research was funded by Sichuan Social Science Fund, grant number SC21ZW003.
References
- 1.UNODC. World . Vol. 1. United Nations Office on Drugs and Crime (UNODC); New York: 2018. (Drug Report -Executive Summary—Conclusions and Policy Implications). [Google Scholar]
- 2.UNODC. World . Vol. 1. United Nations Office on Drugs and Crime (UNODC); New York: 2019. (Drug Report -Executive Summary—Conclusions and Policy Implications). [Google Scholar]
- 3.Zhang Y., Lu C., Zhang J., et al. Gender differences in abusers of amphetamine-type stimulants and ketamine in southwestern China. Addict Behav. 2013;38(1):1424–1430. doi: 10.1016/j.addbeh.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 4.Anglin M.D., Burke C., Perrochet B., Stamper E., Dawud-Noursi S. History of the methamphetamine problem. J Psychoactive Drugs. 2000;32(2):137–141. doi: 10.1080/02791072.2000.10400221. [DOI] [PubMed] [Google Scholar]
- 5.Homer B.D., Solomon T.M., Moeller R.W., Mascia A., DeRaleau L., Halkitis P.N. Methamphetamine abuse and impairment of social functioning: a review of the underlying neurophysiological causes and behavioral implications. Psychol Bull. 2008;134(2):301–310. doi: 10.1037/0033-2909.134.2.301. [DOI] [PubMed] [Google Scholar]
- 6.Beadell N.C., Thompson E.M., Delashaw J.B., Cetas J.S. The deleterious effects of methamphetamine use on initial presentation and clinical outcomes in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2012;117(4):781–786. doi: 10.3171/2012.7.JNS12396. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J.B., Dickow A., Horner K., et al. Abuse and violence history of men and women in treatment for methamphetamine dependence. Am J Addict. 2003;12(5):377–385. [PubMed] [Google Scholar]
- 8.Pocuca N., Young J.W., MacQueen D.A., et al. Sustained attention and vigilance deficits associated with HIV and a history of methamphetamine dependence. Drug Alcohol Depend. 2020;215:108245. doi: 10.1016/j.drugalcdep.2020.108245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krupitsky E., Zvartau E., Woody G. Use of naltrexone to treat opioid addiction in a country in which methadone and buprenorphine are not available. Curr Psychiatry Rep. 2010;12(5):448–453. doi: 10.1007/s11920-010-0135-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deng Q., Tang Q., Schottenfeld R.S., Hao W., Chawarski M.C. Drug use in rural China: a preliminary investigation in Hunan Province. Addiction. 2012;107(3):610–613. doi: 10.1111/j.1360-0443.2011.03648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joseph H., Stancliff S., Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med. 2000;67(5-6):347–364. [PubMed] [Google Scholar]
- 12.Huhn A.S., Strain E.C., Tompkins D.A., Dunn K.E. A hidden aspect of the U.S. opioid crisis: Rise in first-time treatment admissions for older adults with opioid use disorder. Drug Alcohol Depend. 2018;193:142–147. doi: 10.1016/j.drugalcdep.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen S., Dietze P., Lee N., Dunlop A., Taylor D. Concurrent buprenorphine and benzodiazepines use and self-reported opioid toxicity in opioid substitution treatment. Addiction. 2007;102(4):616–622. doi: 10.1111/j.1360-0443.2006.01731.x. [DOI] [PubMed] [Google Scholar]
- 14.Rawson R.A. Current research on the epidemiology, medical and psychiatric effects, and treatment of methamphetamine use. J Food Drug Anal. 2013;21(4):S77–S81. doi: 10.1016/j.jfda.2013.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuch F.B., Vancampfort D., Firth J., et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am J Psychiatr. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- 16.Harvey S.B., Øverland S., Hatch S.L., Wessely S., Mykletun A., Hotopf M. Exercise and the Prevention of Depression: Results of the HUNT Cohort Study. Am J Psychiatr. 2018;175(1):28–36. doi: 10.1176/appi.ajp.2017.16111223. [DOI] [PubMed] [Google Scholar]
- 17.Vieira J., Porcu M., Rocha P. The regular physical exercises practice as complementary therapy to the treatment of depressed women. Jornal Brasileiro De Psiquiatria [in Portuguese] 2007;56(1):23–28. doi: 10.1590/S0047-20852007000100007. [DOI] [Google Scholar]
- 18.McDowell C.P., Dishman R.K., Vancampfort D., et al. Physical activity and generalized anxiety disorder: results from The Irish Longitudinal Study on Ageing (TILDA) Int J Epidemiol. 2018;47(5):1443–1453. doi: 10.1093/ije/dyy141. [DOI] [PubMed] [Google Scholar]
- 19.LeardMann C.A., Kelton M.L., Smith B., et al. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126(3):371–383. doi: 10.1177/003335491112600311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torales J., Almirón M., Gonzalez I., et al. Physical exercise as an adjuvant treatment of mental disorders. A narrative review. Anales de la Facultad de Ciencias Médicas (Asunción) [in Spanish] 2018;51(3):27–32. doi: 10.18004/anales/2018.051(03)27-032. [DOI] [Google Scholar]
- 21.Bassøe H.H. Anorexia/bulimia nervosa: the development of anorexia nervosa and of mental symptoms. Treatment and the outcome of the disease. Acta Psychiatr Scand Suppl. 1990;361:7–13. doi: 10.1111/j.1600-0447.1990.tb11076.x. [DOI] [PubMed] [Google Scholar]
- 22.Zschucke E., Heinz A., Ströhle A. Exercise and physical activity in the therapy of substance use disorders. Sci World J. 2012;2012:901741. doi: 10.1100/2012/901741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hallgren M., Vancampfort D., Giesen E.S., Lundin A., Stubbs B. Exercise as treatment for alcohol use disorders: systematic review and meta-analysis. Br J Sports Med. 2017;51(14):1058–1064. doi: 10.1136/bjsports-2016-096814. [DOI] [PubMed] [Google Scholar]
- 24.Bock B.C., Marcus B.H., King T.K., Borrelli B., Roberts M.R. Exercise effects on withdrawal and mood among women attempting smoking cessation. Addict Behav. 1999;24(3):399–410. doi: 10.1016/s0306-4603(98)00088-4. [DOI] [PubMed] [Google Scholar]
- 25.Scully D., Kremer J., Meade M.M., Graham R., Dudgeon K. Physical exercise and psychological well being: a critical review. Br J Sports Med. 1998;32(2):111–120. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ussher M.H., Taylor A.H., West R., McEwen A. Does exercise aid smoking cessation? A systematic review. Addiction. 2000;95(2):199–208. doi: 10.1046/j.1360-0443.2000.9521996.x. [DOI] [PubMed] [Google Scholar]
- 27.LG X. Heilongjiang Science and Technology Publisher; Harbin: 1990. Chinese Medical Qigong. [Google Scholar]
- 28.Zhu D., Xu D., Dai G., Wang F., Xu X., Zhou D. Beneficial effects of Tai Chi for amphetamine-type stimulant dependence: a pilot study. Am J Drug Alcohol Abuse. 2016;42(4):469–478. doi: 10.3109/00952990.2016.1153646. [DOI] [PubMed] [Google Scholar]
- 29.Wang D., Wang Y., Wang Y., Li R., Zhou C. Impact of physical exercise on substance use disorders: a meta-analysis. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0110728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang C.W., Chan C.H., Ho R.T., Chan J.S., Ng S.M., Chan C.L. Managing stress and anxiety through qigong exercise in healthy adults: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med. 2014;14:8. doi: 10.1186/1472-6882-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giles A., Nasstasia Y., Baker A., et al. Exercise as Treatment for Youth With Major Depression: The Healthy Body Healthy Mind Feasibility Study. J Psychiatr Pract. 2020;26(6):444–460. doi: 10.1097/PRA.0000000000000516. [DOI] [PubMed] [Google Scholar]
- 32.McCain N.L., Gray D.P., Elswick R.K., et al. A randomized clinical trial of alternative stress management interventions in persons with HIV infection. J Consult Clin Psychol. 2008;76(3):431–441. doi: 10.1037/0022-006X.76.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeng Y., Luo T., Xie H., Huang M., Cheng A.S. Health benefits of qigong or tai chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med. 2014;22(1):173–186. doi: 10.1016/j.ctim.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 34.Yeh G.Y., Roberts D.H., Wayne P.M., Davids R.B., Quilty M.T., Phillips R.S. Tai Chi Exercise for Patients With Chronic Obstructive Pulmonary Disease: A Pilot Study. Respir care. 2010;55(11):1475–1482. [PMC free article] [PubMed] [Google Scholar]
- 35.Wu J.J., Zhang Y.X., Du W.S., et al. Effect of Qigong on self-rating depression and anxiety scale scores of COPD patients: A meta-analysis. Medicine (Baltimore) 2019;98(22) doi: 10.1097/MD.0000000000015776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins J.P.T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. http://www.cochrane-handbook.org [updated March 2011] [Google Scholar]
- 37.Li M., Chen K., Mo Z. Use of qigong therapy in the detoxification of heroin addicts. Altern Ther Health Med. 2002;8(1):50–59. [PubMed] [Google Scholar]
- 38.Li D.X., Zhuang X.Y., Zhang Y.P., et al. Effects of Tai Chi on the protracted abstinence syndrome: a time trial analysis. Am J Chin Med. 2013;41(1):43–57. doi: 10.1142/S0192415X13500043. [DOI] [PubMed] [Google Scholar]
- 39.Zhu D., Dai G., Xu D., et al. Long-Term Effects of Tai Chi Intervention on Sleep and Mental Health of Female Individuals With Dependence on Amphetamine-Type Stimulants. Front Psychol. 2018;9:1476. doi: 10.3389/fpsyg.2018.01476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oh C.U., Kim N.C. Effects of T'ai Chi on Serotonin, Nicotine Dependency, Depression, and Anger in Hospitalized Alcohol-Dependent Patients. J Altern Complement Med. 2016;22(12):957–963. doi: 10.1089/acm.2016.0246. [DOI] [PubMed] [Google Scholar]
- 41.Geng J., Zhu D., Xu D. Rehabilitation effect of Taiji rehabilitation exercise on compulsory isolation of female drug abusers. Chin J Sports Med [in Chinese] 2016;35(11):1048–1051. doi: 10.16038/j.1000-6710.2016.11.011. [DOI] [Google Scholar]
- 42.Huang X., Wu S., Xu H. Clinical observation of modified Ba Duan Jin combined with methadone in improving anxiety symptoms of heroin addicts. Shenzhen J Integrated Tradit Chin West Med. [in Chinese] 2015;25(13):98–99. doi: 10.16458/j.cnki.1007-0893.2015.13.052. [DOI] [Google Scholar]
- 43.Zhang Z., Zhu D. Effect of Taijiquan exercise on rehabilitation of male amphetamine-type addicts. Evid Based Complement Alternat Med. 2020;2020:8886562. doi: 10.1155/2020/8886562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smelson D., Chen K.W., Ziedonis D., et al. A pilot study of Qigong for reducing cocaine craving early in recovery. J Altern Complement Med. 2013;19(2):97–101. doi: 10.1089/acm.2012.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fu G., Huang S., Tang C., Liu Y., Gao Y., et al. Effect of Wuqinxi on emotion in patients abstaining from drug. J Anhui Univ Chin Med. [in Chinese] 2016;35(05):26–29. doi: 10.3969/j.issn.2095-7246.2016.05.008. [DOI] [Google Scholar]
- 46.Liu F., Cui J., Liu X., Chen K.W., Chen X., Li R. The effect of tai chi and Qigong exercise on depression and anxiety of individuals with substance use disorders: a systematic review and meta-analysis. BMC Complement Med Ther. 2020;20(1):161. doi: 10.1186/s12906-020-02967-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Belcheva M.M., Ho M.T., Ignatova E.G., et al. Buprenorphine differentially alters opioid receptor adaptation in rat brain regions. J Pharmacol Exp Ther. 1996;277(3):1322–1327. [PMC free article] [PubMed] [Google Scholar]
- 48.Swain J.E., Ho S.S. Opioids and maternal brain-behavior adaptation. Neuropsychopharmacology. 2021;46(1):265–266. doi: 10.1038/s41386-020-00858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martin J.A., Campbell A., Killip T., et al. QT interval screening in methadone maintenance treatment: report of a SAMHSA expert panel [published correction appears in J Addict Dis. J Addict Dis. 2012 Jan;31(1):91. doi: 10.1080/10550887.2011.610710. Haigney, Mark C P [added]]. J Addict Dis. 2011;30(4):283-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leshner A.I. Addiction is a brain disease, and it matters. Science. 1997;278(5335):45–47. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- 51.Liu Y.P., Yuan M.Z., H C., et al. Effect of 12–week taichi on catecholamines and angiotensin–II in young people. Journal of Fujian Normal University (Natural Science Edition) [in Chinese] 2015;31(5):115–119. [Google Scholar]
- 52.Shaham Y., Erb S., Stewart J. Stress-induced relapse to heroin and cocaine seeking in rats: a review. Brain Res Brain Res Rev. 2000;33(1):13–33. doi: 10.1016/s0165-0173(00)00024-2. [DOI] [PubMed] [Google Scholar]
- 53.Sairanen M., O'Leary OF, Knuuttila J.E., Castrén E. Chronic antidepressant treatment selectively increases expression of plasticity-related proteins in the hippocampus and medial prefrontal cortex of the rat. Neuroscience. 2007;144(1):368–374. doi: 10.1016/j.neuroscience.2006.08.069. [DOI] [PubMed] [Google Scholar]
- 54.Lapmanee S., Charoenphandhu J., Teerapornpuntakit J., Krishnamra N., Charoenphandhu N. Agomelatine, venlafaxine, and running exercise effectively prevent anxiety- and depression-like behaviors and memory impairment in restraint stressed rats. PLoS One. 2017;12(11):e0187671. doi: 10.1371/journal.pone.0187671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Müller C.P., Homberg J.R. The role of serotonin in drug use and addiction. Behav Brain Res. 2015;277:146–192. doi: 10.1016/j.bbr.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 56.Fink G. Academic Press; 2000. Encyclopedia of stress. [Google Scholar]
- 57.Zou L., Han J., Li C., et al. Effects of Tai Chi on lower limb proprioception in adults aged over 55: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100(6):1102–1113. doi: 10.1016/j.apmr.2018.07.425. [DOI] [PubMed] [Google Scholar]
- 58.Pa J., Goodson W., Bloch A., King A.C., Yaffe K., Barnes D.E. Effect of exercise and cognitive activity on self-reported sleep quality in community-dwelling older adults with cognitive complaints: a randomized controlled trial. J Am Geriatr Soc. 2014;62(12):2319–2326. doi: 10.1111/jgs.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim T.H., Pascual-Leone J., Johnson J., Tamim H. The mental-attention Tai Chi effect with older adults. BMC Psychol. 2016;4(1):29. doi: 10.1186/s40359-016-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang C., Collet J.P., Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 61.Gillespie L.D., Robertson M.C., Gillespie W.J., et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 62.Garber C.E., Blissmer B., Deschenes M.R., et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 63.Wang F., Man J.K., Lee E.K., et al. The effects of qigong on anxiety, depression, and psychological well-being: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2013;2013:152738. doi: 10.1155/2013/152738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Breslin K.T., Reed M.R., Malone S.B. An holistic approach to substance abuse treatment. J Psychoactive Drugs. 2003;35(2):247–251. doi: 10.1080/02791072.2003.10400006. [DOI] [PubMed] [Google Scholar]