Abstract
This study investigated the factors that are associated with sleep disturbances among Chinese athletes. Sleep quality and associated factors were assessed by the Athlete Sleep Screening Questionnaire (ASSQ, n = 394, aged 18–32 years, 47.6% female). Sleep difficulty score (SDS) and level of sleep problem (none, mild, moderate, or severe) were used to classify participants' sleep quality. Categorical variables were analyzed by Chi-square or fisher's exact tests. An ordinal logistic regression analysis was used to explore factors with poor sleep (SDS ≥8).
Approximately 14.2% of participants had moderate to severe sleep problem (SDS ≥8). Fifty-nine percent of the athletes reported sleep disturbance during travel, while 43.3% experienced daytime dysfunction when travelling for competition. No significant difference was found in the SDS category between gender, sports level and events. Athletes with evening chronotype were more likely to report worse sleep than athletes with morning and intermediate chronotype (OR, 2.25; 95%CI, 1.44–3.52; p < 0.001). For each additional year of age, there was an increase of odds ratio for poor sleep quality (OR, 1.15; 95%CI, 1.04–1.26; p = 0.004), while each additional year of training reduced the odds ratio (OR, 0.95; 95%CI, 0.91–0.99; p = 0.044). To improve sleep health in athletes, chronotype, travel-related issues, age and years of training should be taken into consideration.
Keywords: Athlete, Sleep quality, Sleep health, Questionnaire
Highlights
-
•
Sleep problems in athletes have been noticed in recent years. By using the clinically validated questionnaire (ASSQ) in Chinese athletes, we found that 14.2% of Chinese athletes had sleep disturbance.
-
•
By using a multivariate ordinal logistic regression model, we were able to detect chronotype, travel-related issues, age and years of training were important influencing factors on poor sleep quality in Chinese athletes.
-
•
The novel findings observed in this study shed new light on the current sleep health and possible factors affecting sleep disturbances of Chinese athletes and provide a new perspective for Chinese athletes to optimize their sleep strategies that improve sleep quality.
Abbreviations
- ASSQ
Athlete Sleep Screening Questionnaire
- PSQ
Pittsburgh Sleep Quality Index
- SDS
Sleep Difficulty Score
- SE
Standard Error
- CI.L
Lower Limit of 95% Confidence Interval
- CI.U
Upper Limit of 95% Confidence Interval
Introduction
Athletic performance has been shown to be related to sleep quality.1 Sleep deficiency is defined as the insufficient duration of sleep time from the optimal sleep time for health, performance and well-being.2 On average athletes sleep for 6.7 h even though the optimal time is found to be on average 8.3 h.3 The International Olympic Committee recognizes that sleep deficiency and sleep disturbances seriously affect athletes' sleep health and may impair athletes' aerobic capacity,4 sprint capacity,5 neurocognitive function,6 and other indicators that affect athletic performance. Therefore, there is an expert consensus to implement routine assessment, identification, and interventions for athletes' sleep health.7 However, there is not enough evidence to draw a global consensus as to how the sleep health of athletes should be improved.8
Growing evidence has shown that elite athletes have sleep difficulties before important competitions,9,10,11 during intense training12 and after long-distance travel,13 and that fatigue and anxiety caused by the poor sleep has a direct impact on training14 and competition.15 Training schedules,10,16 increased levels of pre-competition arousal,17 and delayed sleep time due to the use of electronic devices before bedtime18 are usually the main factors affecting athletes' sleep.18
Studies have shown that19 different ethnical groups of athletes have different sleep characteristics. For Chinese athletes, there is a lack of data to support the development of sleep strategies for the specified group. According to Mo Yi,20 15.5% of 782 professional Chinese adult athletes had sleep disorders defined by Pittsburgh Sleep Quality Index (PSQI) global score. However, PSQI without athlete-related questions. There was also a lack of standardised data for athletes, and the results were not validated in the athlete population.8 Athletes sleep screening questionnaire (ASSQ) is the athlete-specific sleep questionnaire,21 can be used as an initial clinical tool to assess the sleep disturbance of the athlete population.22 Recently, Tan et al.23 found that 19.5% of 343 Chinese athletes had sleep disturbances by the ASSQ, but the purpose of the study was to assess the validity and reliability of the Chinese version of the ASSQ, and its participants consisted mostly of youth athletes. Information related to sleep characteristics and demographic data were not presented in the study. Thus, the purpose of this study was to use the ASSQ to monitor sleep characteristics among Chinese athletes. Specifically, we aimed to: (1) describe the sleep quality of Chinese athletes via an online survey of the ASSQ, (2) investigate the factors which are associated with the severity of sleep difficulty.
Materials and methods
Participants
The study was a cross-sectional design with a convenience sample. The inclusion criteria were Chinese athletes aged 18–35 years, who have a national athlete grade certificate issued by the General Administration of Sports of China. The athlete grades or sports levels included in this study were Master athletes, national-level athletes, and second-level athletes. According to the General Administration of Sports of China,24 Master athletes participated in Olympics, world championships, Asian championships, and national games in adults. The national level athletes are qualified to participate in comprehensive games and championships hosted by national sports bureaus and have reached the finals. The second-level athletes are qualified to participate in comprehensive games and championships hosted by provincial and municipal sports bureaus and have reached the finals. The highest sports level was considered for this study for each of the athletes. We also categorized athletes into sport-types according to the event group theory.25 Sports were divided into two major types based on similar competitive characteristics and training requirements, consisting of the skill-dominance category and physical-dominance category. The skill-dominance sports consisted of five groups: 1) Performance difficulty aesthetics sports (gymnastics, artistic gymnastics, aerobics, and martial arts); 2) Combat confrontational sports (wrestling, boxing, fencing and taekwondo); 3) Net confrontational sports (tennis, table tennis, badminton, and volleyball); 4) Same field confrontation sports (soccer, basketball, handball, and rugby); and 5) Performance accuracy sports (archery and shooting). The physical-dominance sports consisted of three groups: 1) Fast power sports (powerlifting, jumping, and throwing); 2) Sprinting sports (sprints, short-distance hurdles, and short-distance swimming); and 3) Endurance sports (marathon, rowing, and long distances running). There were no athletes from the performance-accuracy sports in this study, thus this classification was omitted. In addition, based on the form of competition, sports were classified as team sports and individual sports. Sports type information was also collected from athletes in this study.
Study design
We collected data by sleep questionnaire (ASSQ) as described by Bender et al.22 Sport events, sport type, sport level, years of training, phase of the season, and sociodemographic information were gathered from Chinese athletes through commercial online survey platforms (i.e., WenJuanWang and WeChat) from May 20 to June 30, 2021. The collected questionnaire was proofread by a researcher to remove outliers such as less than 1 year of training experience, younger than 18 years and older than 35 years of age. Athletes who did not report their sports events and phase of the season were also been excluded.
The study was performed according to the Declaration of Helsinki and was approved by the ethics committee of Shanghai Jiao Tong University, China (H2021138I). The questionnaire was anonymous and produced de-identified data. Informed consent was obtained from each participant before the beginning of the survey. The participants were volunteers without a monetary incentive, and they were informed about the use of their information.
Athlete Sleep Screening Questionnaire (ASSQ)
The Athlete Sleep Screening Questionnaire (ASSQ) was developed by Samuels et al. and Bender et al.21,22 as a sleep screening tool to assess sleep disturbances and daytime dysfunction based on the types and severity of the sleep difficulties(none, mild, moderate, or severe). The questionnaire was clinically validated in athletes and factors such as total sleep time, satisfaction with sleep, and presence of insomnia symptoms questions were set to obtain a “Sleep Difficulty Score” (SDS). The ASSQ has been incorporated into the International Olympic Committee's Mental Health Task Force as a secondary screening tool for athletes' mental health and is used to screen and intervene in the sleep problems of outstanding athletes.7 The ASSQ is the only clinically validated sleep screening questionnaire for athletes consisting of 16 items, Bender et al.22 have shown that the ASSQ has good reliability and validity among the athlete population. Tan et al.23 have examined the reliability and validity of the Chinese version of the ASSQ questionnaire using exploratory factor analysis and confirmatory factor analysis, which used the PSQI sleep questionnaire as the validity tool. They found a moderate agreement between the Chinese version of the ASSQ and the Chinese version of the PSQI for sleep screening among Chinese athletes, which could be applied to the daily sleep monitoring and screening of Chinese athletes (Cronbach's α = 0.696, Cohen's κ = 0.543). In addition, we have performed a cross-cultural adaptation process to assure equivalence between the original source and the Chinese target version of the ASSQ (see supplementary file 1). The Chinese version of ASSQ has demonstrated good reliability by internal consistency (Cronbach's α = 0.82) and test re-test reliability (r = 0.92).
The overall questionnaire consists of three sections: sleep difficulty score (SDS), modifier items, and other items. Of these sections, the SDS is the key component of the ASSQ based on 5 items (sleep quantity, sleep quality, sleep latency, sleep disturbance and use of sleep medicine), with a higher total score indicative of a higher level of sleep difficulty.22 The modifier items consisted of factors of sleep breathing disorders, travel, and chronotype (morning and intermediate type or evening type). These factors were not included in the SDS by the ASSQ developers because of their low prevalence in athletes and the negative impact on the psychometric properties of the ASSQ. Nevertheless, these factors have clinical implications and were significant for the diagnosis of the case, thus these were included as a secondary scoring system in ASSQ. The other items consisted of three questions on nap frequency, caffeine intake and the use of electronics before bedtime, which are not included in the SDS but are there to provide sleep optimization strategies.
SDS scoring
The sleep difficulty score (see supplementary file 1) consisted of the following 5 items: (1) During the recent past, how many hours of actual sleep did you get at night? (This may be different than the number of hours you spent in bed.); (2) How satisfied/dissatisfied are you with the quality of your sleep?; (3) During the recent past, how long does it usually take for you to fall asleep each night?; (4) How often do you have trouble staying asleep?; and (5) During the recent past, how often have you taken medicine to help you sleep (prescribed or over-the-counter)? Based on the answers to these questions, athletes who reported more sleep hours, satisfying sleep quality, no trouble falling asleep, and not taking sleep medicine, had low SDS scores. The Sleep Difficulty Score (SDS) was calculated on an 18-point scale and used to classify athletes into 4 different sleep difficulty categories: none (SDS: 0–4), mild (SDS: 5–7), moderate (SDS: 8–10), and severe (SDS: 11–17), these categories have resulted in a diagnostic sensitivity of 93% and specificity of 81%.22
Chronotype scoring
The ASSQ also has a secondary sub-scale related to chronotype. The classification of chronotype was derived from the total score (15-point scale) of the four items: (1) Considering only your own “feeling best” rhythm, at what time would you get up if you were entirely free to plan your day; (2) Considering your own “feeling best” rhythm, at what time would you go to bed if you were entirely free to plan your evening; (3) How alert do you feel during the first half-hour after having awakened; and (4) Do you consider yourself to be a morning type person or an evening type person? Added together with these four items, those below 5 are classified as evening chronotype, whereas scores above 5 were classified as morning and intermediate chronotype.22 Athletes classified as evening type were more likely to report later wake times, not being alert during the first half-hour after having awakened, going to sleep later, and self-reported as more likely to be an evening type.
Other items
Questions about sleep-disordered breathing were also considered in the ASSQ. If athletes answered “yes” to either of the two questions (loud snoring or apnea during sleep), then they were identified as potentially having sleep-disordered breathing. Furthermore, questions about sleep disturbances and performance issues during travel are included in the ASSQ. Study athletes have answered the following questions: (1) “When you are travelling for your sport, do you experience sleep disturbance?” and (2) When you are travelling for your sport, do you experience daytime dysfunction (feeling generally unwell or having poor performance)? Furthermore, questions on nap frequency, caffeine intake, and the use of electronics before bedtime were only used to provide strategies to optimize sleep in athletes and were not included in the ASSQ scoring system and classification system.
Statistical analyses
Based on the work of Bender et al.,22 we have calculated our obtained sample of 394 individuals who filled out the questionnaire from 7 different sport categories with a response rate of 73.37%. Therefore, we have performed post hoc power calculations using G∗Power software (Version 3.1, University of Dusseldorf, Germany) and found our sample is sufficient to have power of 0.89, producing a two-sided 95% confidence interval with a width equal to 0.075 when the sample proportion is 0.25. The Shapiro–Wilk test was used to check the normality of data distribution. If data were not normally distributed, they were analyzed by the non-parametric analysis method. Descriptive statistics were used to present the continuous data as the mean and confidence interval for the mean (95%CI) and categorical data as numbers (n) and proportions (%). Mann-Whitney test was used to compare sleep difficulty score (SDS) between gender, sport categories (physical dominance vs. skill dominance), sport-type group (individual sports vs. team sport), and phase of the season (pre-season vs. off-season). Kruskal-Wallis tests were used to compare the SDS between sport level and sport categories. A cross-table Chi-squared (ꭓ2) or Fisher's exact test were used where appropriate to assess the SDS category differences of gender, different sports type, phase of the season and sports level, and Cramer's V for estimation of effect size (small, medium or large).26,27
In addition, to explore factors associated with the severity of sleep difficulty, variables showing a significant correlation in the Chi-squared or Fisher's exact test were used to perform in a multivariate ordinal logistic regression model. The demographic variables such as age, BMI and training years were used as covariates for the model. The proportional-odds assumptions were evaluated for each model using the parallel line test. Odds ratios (OR) are given with 95%CIs. Statistical significance was set at 0.05. All analyses were performed using IBM SPSS Statistics 24.0 for Windows (SPSS, Inc., Chicago, IL, USA).
Results
Of the final analytical sample (n = 394),187 (47.6%) were male athletes and 207 (52.4%) were female athletes. Table 1 summarized the demographic information and sleep characteristics of the study participants. The age range of this study participants was 18–32 years, and the mean BMI was 22.0 (95%CI, 21.8–22.3). Fifty-nine percent of the participants were from individual sports and 47.6% were at the national level. Fifty-four percent of the participants were in the off-season and 45.8% were in the pre-season. Male athletes had higher BMI than female athletes (p = 0.001). There were no differences in age, BMI, and years of training by sport type. The age of master athletes was older than other levels of athletes, respectively (p < 0.001), and have more years of training than the national level and second level of athletes (p < 0.001). Twenty-four percent of the participants were from the same field confrontation sports, 19.2% were from the netting confrontational sports, 17.2% were from the combat confrontational sports, 14.4% were from the performance difficulty aesthetics sports, 14.2% were from sprinting sports, 5.8% were from endurance sports, 4.8% were from the fast power sports. Age, BMI and training years did not differ by sport categories (p > 0.05).
Table 1.
Participants' demographics and sleep characteristics.
| Total |
Gender |
Sports Type |
Sports Category |
Sports Level |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Team Sports |
Individual Sports |
Physical-dominance category |
Skill-dominance category |
Masters athletes |
National athletes |
Second-level athletes |
||
| Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95% CI) | Mean (95% CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | |
| Age | 21.2 (21.0–21.4) | 21.3 (21.0–21.6) | 21.1 (21.0–21.4) | 21.3 (21.0–21.6) | 21.2 (20.9–21.4) | 21.1 (20.9–21.4) | 21.5 (21.0–22.0) | 22.6 (22.1–23.2) ∗∗∗ | 20.7 (20.5–20.9) | 21.0 (20.6–21.4) |
| Body Mass Index (BMI, kg/m2) | 22.0 (21.8–22.3) | 22.9 (22.5–23.3) ∗∗∗ | 21.2 (20.9–21.5) | 22.2 (21.8–22.6) | 21.9 (21.5–22.2) | 22.1 (21.8–22.4) | 21.9 (21.3–22.4) | 22.4 (21.9–22.9) | 21.9 (21.5–22.3) | 21.9 (21.5–22.4) |
| Training Experience (yrs.) | 9.7 (9.3–10.1) | 9.4 (8.7–10.0) | 10.0 (9.5–10.6) | 9.4 (8.7–10.0) | 10.0 (9.4–10.5) | 9.8 (9.4–10.3) | 9.3 (8.5–10.2) | 12.3 (11.3–13.2) ∗∗∗ | 10.1 (9.5–10.6) | 7.2 (6.6–7.9) |
|
Sleep Difficulty Score (SDS) |
5.3 (5.1–5.5) |
5.2 (4.8–5.5) |
5.5 (5.2–5.8) |
5.2 (5.0–5.7) |
5.3 (5.0–5.6) |
5.3 (5.1–4.9) |
5.3 (4.9–5.7) |
5.5 (5.0–5.9) |
5.2 (4.9–5.5) |
5.3 (4.9–5.7) |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Nocturnal Sleep Duration | ||||||||||
| 5–6 h | 29 (7.4) | 13 (7.0) | 16 (7.7) | 7 (4.3) ∗ | 22 (9.6) | 4 (4.1) | 25 (8.4) | 7 (8.0) | 15 (8.0) | 7 (5.9) |
| 6–7 h | 134 (34.0) | 68 (36.4) | 66 (31.9) | 53 (32.3) | 81 (35.2) | 35 (36.1) | 99 (33.3) | 28 (31.8) | 63 (33.5) | 43 (36.4) |
| 7–8 h | 165 (41.9) | 75 (40.1) | 90 (43.5) | 66 (40.2) | 99 (43.0) | 43 (44.3) | 122 (41.1) | 38 (43.2) | 76 (40.4) | 51 (43.2) |
| 8–9 h | 52 (13.2) | 22 (11.8) | 30 (14.5) | 30 (18.3) | 22 (9.6) | 13 (13.4) | 39 (13.1) | 11 (12.5) | 31 (16.5) | 10 (8.5) |
| More than 9 h | 14 (3.6) | 9 (4.8) | 5 (2.4) | 8 (4.9) | 6 (2.6) | 2 (2.1) | 12 (4.0) | 4 (4.5) | 3 (1.6) | 7 (5.9) |
| Sleep Satisfaction | ||||||||||
| Very Satisfied | 39 (9.9) | 23 (12.3) | 16 (7.7) | 20 (12.2) | 19 (8.3) | 10 (10.3) | 29 (9.8) | 6 (6.8) | 19 (10.1) | 14 (11.9) |
| Somewhat satisfied | 192 (48.7) | 95 (50.8) | 97 (46.9) | 72 (43.9) | 120 (52.2) | 41 (42.3) | 151 (50.8) | 46 (52.3) | 91 (48.4) | 55 (46.6) |
| Neither satisfied nor dissatisfied | 119 (30.2) | 51 (27.3) | 68 (32.9 | 51 (31.1) | 68 (29.6) | 33 (34.0) | 86 (29.0) | 28 (31.8) | 56 (29.8) | 35 (29.7) |
| Somewhat dissatisfied | 33 (8.4) | 12 (6.4) | 21 (10.1) | 14 (8.5) | 19 (8.3) | 12 (12.4) | 21 (7.1) | 5 (5.7) | 17 (9.0) | 11 (9.3) |
| Very dissatisfied | 11 (2.8) | 6 (3.2) | 5 (2.4) | 7 (4.3) | 4 (1.7) | 1 (1.0) | 10 (3.4) | 3 (3.4) | 5 (2.7) | 3 (2.5) |
| Time to Fall Asleep | ||||||||||
| 15 min or less | 192 (48.7) | 99 (52.9) | 93 (44.9 | 67 (40.9) | 125 (54.3) | 53 (54.6) | 139 (46.8) | 41 (46.6) | 95 (50.5) | 56 (47.5) |
| 16–30 min | 147 (37.3) | 59 (31.6) | 88 (42.5) | 65 (39.6) | 82 (35.7) | 33 (34.0) | 114 (38.4) | 31 (35.2) | 73 (38.8) | 43 (36.4) |
| 31–60 min | 43 (10.9) | 22 (11.8) | 21 (10.1) | 27 (16.5) ∗ | 16 (7.0) | 9 (9.3) | 34 (11.4) | 12 (13.6) | 15 (8.0) | 16 (13.6) |
| Longer than 60 min | 12 (3.0) | 7 (3.7) | 5 (2.4) | 5 (3.0) | 7 (3.0) | 2 (2.1) | 10 (3.4) | 4 (4.5) | 5 (2.7) | 3 (2.5) |
| Having Trouble Staying Asleep | ||||||||||
| None | 116 (29.4) | 64 (34.2) | 52 (25.1) | 47 (28.7) | 69 (30.0) | 22 (22.7) | 94 (31.6) | 22 (25.0) | 56 (29.8) | 38 (32.2) |
| 1 or 2 times per week | 231 (58.6) | 106 (56.7) | 125 (60.4) | 99 (60.4) | 132 (57.4) | 61 (62.9) | 170 (57.2) | 53 (60.2) | 112 (59.6) | 66 (55.9) |
| 3 or 4 times per week | 41 (10.4) | 14 (7.5) | 27 (13.0) | 14 (8.5) | 27 (11.7) | 14 (14.4) | 27 (9.1) | 12 (13.6) | 17 (9.0) | 12 (10.2) |
| 5–7 days per week | 6 (1.5) | 3 (1.6) | 3 (1.4) | 4 (2.4) | 2 (0.9) | 0 (0.0) | 6 (2.0) | 1 (1.1) | 3 (1.6) | 2 (1.7) |
| Chronotype | ||||||||||
| Morning and Intermediate Type | 290 (73.6) | 145 (77.5) | 145 (70.0) | 124 (75.6) | 166 (72.2) | 69 (71.1) | 221 (74.4) | 66 (75.0) | 140 (74.5) | 84 (71.2) |
| Evening Type | 104 (26.4) | 42 (22.5) | 62 (30.0) | 40 (24.4) | 64 (27.8) | 28 (28.9) | 76 (25.6) | 22 (25.0) | 48 (25.5) | 34 (28.8) |
Abbreviation: (95%CI mean lower bound to upper bound), ∗∗∗, p < 0.001, ∗, p < 0.05.
Athletes in individual sports reported less total sleep time than team sports athletes (9.6% vs. 4.3%, p < 0.05). In contrast, compared with individual sport athletes, team sport athletes tended to report more time to fall asleep (16.5% vs. 7.0%, p < 0.05).
Sleep difficulty score (SDS) and sleep problem category
The SDS mean score was 5.3, with no significant difference between male and female athletes (p > 0.05). No sex differences were found in SDS across sport type, sport categories, phase of seasons, and sport levels either (p > 0.05). In addition, there were no significant differences in SDS by sport type and sport categories. Similarly, there were no significant differences in SDS across phases of the season and sports level (p > 0.05).
Among all athletes, 37.7% were categorized in the category of no clinical sleep problem, 48.1% were in the mild clinical sleep problem category, 11.4% were in the category of moderate clinical sleep problem, and 2.8% were in the category of severe clinical sleep problem (Table 2). No significant difference was found in sex, sport type, sport level, phase of the season and sleep-disordered breathing between different SDS categories, respectively (p > 0.05). However, athletes with sleep disturbances when travelling were categorized with a higher percentage of moderate to severe sleep difficulty problems than athletes who did not have sleep difficulties (p < 0.001). There were significant differences in SDS categories proportions between athletes who had performance issues and athletes without performance issues when travelling. Athletes with performance issues during travel had a higher proportion in the moderate and severe sleep problem category (p < 0.001).
Table 2.
SDS categories by gender, sports type, sports level, phase of the season, sports category, chronotype, sleep disturbance when travelling, performance issue when travelling and sleep-disordered breathing.
| None |
Mild |
Moderate |
Severe |
p-value (Cramer's V) |
|||||
|---|---|---|---|---|---|---|---|---|---|
|
n |
% |
n |
% |
n |
% |
n |
% |
||
| All Athletes | 149 | 37.8% | 189 | 48.0% | 45 | 11.4% | 11 | 2.8% | |
| Gender | 0.79 (0.05) | ||||||||
| Male | 74 | 18.8% | 87 | 22.1% | 22 | 5.6% | 4 | 1.0% | |
| Female | 75 | 19.0% | 102 | 25.9% | 23 | 5.8% | 7 | 1.8% | |
| Sports Type | 0.40 (0.09) | ||||||||
| Team sports | 65 | 16.5% | 74 | 18.8% | 18 | 4.6% | 7 | 1.8% | |
| Individual sports | 84 | 21.3% | 115 | 29.9% | 27 | 6.9% | 4 | 1.0% | |
| Sports Level | 0.54 (0.08) | ||||||||
| Master athletes | 33 | 8.4% | 40 | 10.2% | 12 | 3.0% | 3 | 0.8% | |
| National level of athletes | 74 | 18.8% | 93 | 23.6% | 15 | 3.8% | 6 | 1.5% | |
| Second-level athletes | 42 | 10.7% | 56 | 14.2% | 18 | 4.6% | 2 | 0.5% | |
| Phase of Season | 0.75 (0.06) | ||||||||
| Pre-season | 71 | 18.0% | 87 | 22.1% | 18 | 4.6% | 4 | 1.0% | |
| Off-season | 78 | 19.8% | 102 | 25.9% | 27 | 6.9% | 7 | 1.8% | |
| Chronotype | < 0.001 (0.24) | ||||||||
| Morning and Intermediate type | 119 | 30.2% | 140 | 35.5% | 29 | 7.4% | 2 | 0.5% | |
| Evening-type | 30 | 7.6% | 49 | 12.4% | 16 | 4.1% | 9 | 2.3% | |
| Sleep disturbance when travelling | < 0.001 (0.26) | ||||||||
| Have sleep disturbance | 65 | 16.5% | 122 | 31.0% | 37 | 9.4% | 8 | 2.0% | |
| No sleep disturbance | 84 | 21.3% | 68 | 17.0% | 8 | 2.0% | 3 | 0.8% | |
| Performance issue when travelling | < 0.001 (0.27) | ||||||||
| Have performance issue | 43 | 10.9% | 98 | 24.9% | 28 | 7.1% | 2 | 0.5% | |
| No performance issue | 106 | 26.9% | 91 | 23.1% | 17 | 4.3% | 9 | 2.3% | |
| Sleep-disordered breathing | 0.90 (0.04) | ||||||||
| Have sleep-disordered breathing | 36 | 9.1% | 49 | 12.4% | 10 | 2.5% | 2 | 0.5% | |
| No sleep-disordered breathing | 113 | 28.7% | 141 | 35.5% | 35 | 8.9% | 9 | 2.3% | |
Abbreviation: SDS, Sleep Difficulty Score.
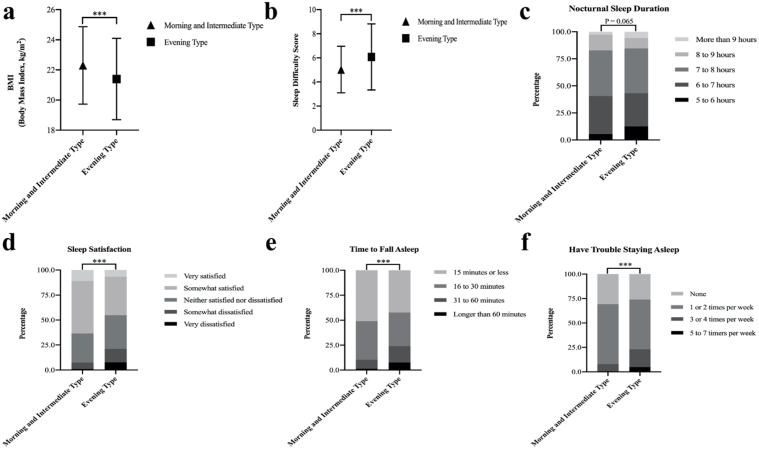
Chronotype
According to the secondary score system of the ASSQ, 73.6% of athletes were categorized into morning and intermediate types, and 26.4% were categorized into evening type. As shown in Fig. 1, there was a lower body mass index and higher sleep difficulty score in evening type athletes than athletes in the morning and intermediate types. In addition, evening type athletes tended to have less sleep duration than morning and intermediate type athletes (p = 0.065). Similarly, evening type athletes had worse subjective sleep satisfaction, longer time to fall asleep, and more frequency of having trouble falling asleep than morning and intermediate type athletes (All p < 0.001).
Fig. 1.
(a–f) Participant's demographic information and sleep characteristic by chronotype: body mass index (a); sleep difficulty score (b), nocturnal sleep duration (c), sleep satisfaction (d), time to fall asleep (e) and have trouble staying asleep (f). The line with symbol depicts means ± SD. ∗∗∗p < 0.001 for body mass index, sleep difficulty score, sleep satisfaction, time to fall asleep and have trouble staying asleep.
Associations of factors with SDS
Table 3 is a summary of the multiple ordinal logistic regression of the associate factors with the severity of sleep difficulty (SDS ≥8). The results showed that for each additional year of age of athletes, there was an increase in the odds ratio for poor sleep quality (OR, 1.15; 95%CI, 1.04–1.26; p = 0.004). However, increasing each additional year of training decreased of odds ratio for poor sleep quality (OR, 0.95; 95%CI, 0.91–0.99; p = 0.044). Chronotype was also an influential factor affecting the degree of sleep difficulty, with evening type athletes having a higher risk of moderate to severe sleep difficulty compared to morning and intermediate type athletes (OR, 2.25; 95%CI, 1.44–3.52; p < 0.001).
Table 3.
Association among demographic factors, chronotype with moderate to severe sleep problem as assessed by ASSQ.
| Variables | OR | SE | 95%CI | p-value |
|---|---|---|---|---|
| Age | 1.15 | 0.04 | 1.043–1.258 | 0.004 |
| Body mass index, kg/m2 | 1.05 | 0.04 | 0.979–1.131 | 0.169 |
| Training years | 0.95 | 0.03 | 0.905–0.998 | 0.044 |
| Chronotype | ||||
| Evening type vs. Morning and Intermediate type | 2.25 | 0.23 | 1.439–3.522 | < 0.001 |
Abbreviations: ASSQ, Athlete Sleep Screening Questionnaire; CI, confidence interval; OR, odds ratio. Note: Estimates represent the log odds that SDS ≥8 (indicative of a moderate to severe sleep problem).
Discussion
In this study, nearly four hundred athletes from 15 different sports provided reports on their demographic information and sleep quality. Overall, 14.2% of Chinese athletes had poor sleep health.
Our findings show a slightly lower proportion of sleep disturbances than in existing studies22,28 using the ASSQ as a measurement tool to monitor sleep in the athlete population. Biggins et al. yielded similar findings to the current study after conducting ASSQ in 58 Irish elite international athletes, 16% of the athletes required further assessment due to SDS classification, their sample size was too small and the types of sports involved were mostly team sports (64%), which may affect their results.17 Bender et al.22 found that nearly 25.1% of 199 Canadian National Team athletes in 23 different sports events had clinically significant sleep problems using the ASSQ. However, these studies did not report detailed information on such as the ethnicity of the participating athletes, their questionnaires were focused on the North American region and the findings may have been limited to that region's athlete population.28 Huskey et al. used the ASSQ to survey 1033 collegiate athletes from four universities, three-ethnicity groups (whites, blacks, and other underrepresented ethnicities) within the Pacific Athletic Conference (PAC-12) on sleep problems,19 and found that black athletes had worse sleep quality than the other two ethnicities. This suggests that there may be racial differences in sleep characteristics among athletes of different ethnicities. However, the Asian athletes in the study were not able to form a separate group due to the small sample size. A recent study from China found that after administering the ASSQ to 343 Chinese professional athletes, 67 (19.5%) athletes had clinical sleep problems categorized as moderate or severe sleep problem category, which is slightly different from the results of the present study (14.2%). This may be related to the intense training and closed management of their sports teams.23
In the present study, there were no significant differences found in the SDS or SDS categories by gender, sports type and sports events. These results were contradicted by the previous study,29 where Hrozanova et al. found that female endurance athletes preferred to report poorer subjective sleep quality than male athletes. The possible reason for this difference was the fluctuations of female hormones and the side effects of the menstrual cycle.29 However, information about female athletes’ menstrual cycle was not collected in this study and therefore cannot be interpreted. Besides, Rabin et al. found that there was no difference in SDS between various sports among American collegiate athletes,28 which is consistent with our result. This result may suggest that the ASSQ questionnaire can be used to assess the sleep disturbance of athletes in different sports with generalization.28
Several studies have found that sleep disturbance has many adverse effects on athletic performance such as longer reaction times,15 less accuracy,30 slower sprint times,31 and reduced endurance performance levels,32 respectively. The present study found that the sleep disturbances and having an influence on performance when travelling for their sport, which showed significant associations with poorer sleep quality. Compared to the general population, athletes have a higher risk of poor sleep health due to the frequent travel.33 Moods such as nervousness and anxiety resulting from travel and competition may cause insomnia and nightmares in athletes during sleep, which can reduce the total sleep time and sleep efficiency,34, 35, 36 which would ultimately affect sleep quality.
Athletes who reported evening chronotype had significantly more frequent sleep disturbances than those with a morning type or intermediate type.37 Our study found athletes with evening chronotype were more likely to be poorer sleepers. Similar findings were found by Bender et al. with evening chronotype athletes.22 In addition, Bender et al. found that misalignment of sleep times with circadian preference could contribute to poorer sleep quality in elite athletes.38 Some have proposed that chronotype affects ratings of perceived exertion and fatigue scores and athletic performance,39 as well as the quality of sleep after training and competition.39 Together with previous studies, our results provide a rationale for coaches and team physicians to pay attention to the chronotype of the athletes. Possible sleep interventions and treatments to improve sleep quality by regulating their time schedules for evening-type athletes are awaited.
This study had a few limitations. First, the current study only considered basic sports-related information such as sports level and training years, without including other possible factors that also affect athletes' sleep, such as the frequency of training per week, and mood into the study, which may lead to a partial interpretation. In addition, as a subjectively reported tool, the ASSQ may be prone to some recall bias. In contrast, using actigraphy as an objective measure is ideal for monitoring sleep, but the device is expensive, requires high compliance of participants, and demands more resource support. Overall, further research should be made including larger sample size of Chinese athletes to improve the athlete's sleep evaluation system and develop personalized sleep recommendations.
Conclusion
In this study, age, chronotype, training years, travel-related issues are possible factors that influence the severity of sleep difficulties among the Chinese athlete's population. It is important to provide sleep education and intervention to athletes to improve their sleep quality during training and competition.
Submission statement
This article has not been published previously (except in the form of an abstract or as part of a published lecture or academic thesis), is not under consideration for publication elsewhere, has been approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and, if accepted, it will not be published elsewhere, including electronically in the same form, in English, or any other language, without the written consent of the copyright holder.
Authors’ contributions
B.Z developed the idea of the manuscript, drafted the paper plan, conducted data analysis, and prepared the manuscript. A.B and T.X helped with data analysis and manuscript revision. S.C drafted the paper plan, conducted manuscript preparation, review and revision. Cheng has full responsibility of the integrity of the study. X. W and S.L reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Ethics approval statement
The study was performed following the Declaration of Helsinki and was approved by the ethics committee of the Shanghai Jiao Tong University, China (H2021138I). The participants were volunteers, without a monetary incentive and were informed about the use of their information. Informed consent from each participant was obtained.
Funding
This study was funded by the start-up plan for young scholar fund (Grant AF4150043) and the Shanghai Jiao Tong University Zhiyuan Foundation (CP2014013) at Shanghai Jiao Tong University.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank the athletes who participated in the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.smhs.2022.02.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gupta L., Morgan K., Gilchrist S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2017;47(7):1317–1333. doi: 10.1007/s40279-016-0650-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chattu V.K., Manzar M., Kumary S., et al. The global problem of insufficient sleep and its serious public health implications. Healthcare. 2019;7(1):1. doi: 10.3390/healthcare7010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sargent C., Lastella M., Halson S.L., et al. How much sleep does an elite athlete need? Int J Sports Physiol Perform. 2021;1(aop):1–12. doi: 10.1123/ijspp.2020-0896. [DOI] [PubMed] [Google Scholar]
- 4.Azboy O., Kaygisiz Z. Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiol Hung. 2009;96(1):29–36. doi: 10.1556/APhysiol.96.2009.1.3. [DOI] [PubMed] [Google Scholar]
- 5.Skein M., Duffield R., Edge J., et al. Intermittent-sprint performance and muscle glycogen after 30 h of sleep deprivation. Med Sci Sports Exerc. 2011;43(7):1301–1311. doi: 10.1249/MSS.0b013e31820abc5a. [DOI] [PubMed] [Google Scholar]
- 6.Hurdiel R., Van Dongen H.P., Aron C., et al. Sleep restriction and degraded reaction-time performance in Figaro solo sailing races. J Sports Sci. 2014;32(2):172–174. doi: 10.1080/02640414.2013.815359. [DOI] [PubMed] [Google Scholar]
- 7.Gouttebarge V., Bindra A., Blauwet C., et al. International olympic committee (IOC) sport mental health assessment tool 1 (SMHAT-1) and sport mental health recognition tool 1 (SMHRT-1): towards better support of athletes' mental health. Br J Sports Med. 2021;55(1):30–37. doi: 10.1136/bjsports-2020-102411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh N.P., Halson S.L., Sargent C., et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2020;55:356–368. doi: 10.1136/bjsports-2020-102025. [DOI] [PubMed] [Google Scholar]
- 9.Erlacher D., Ehrlenspiel F., Adegbesan O.A., et al. Sleep habits in German athletes before important competitions or games. J Sports Sci. 2011;29(8):859–866. doi: 10.1080/02640414.2011.565782. [DOI] [PubMed] [Google Scholar]
- 10.Lastella M., Roach G.D., Halson S.L., et al. Sleep/wake behaviour of endurance cyclists before and during competition. J Sports Sci. 2015;33(3):293–299. doi: 10.1080/02640414.2014.942690. [DOI] [PubMed] [Google Scholar]
- 11.Biggins M., Purtill H., Fowler P., et al. Sleep, health, and well-being in elite athletes from different sports, before, during, and after international competition. Physician Sportsmed. 2020:1–9. doi: 10.1080/00913847.2020.1850149. [DOI] [PubMed] [Google Scholar]
- 12.Nédélec M., Halson S., Abaidia A.-E., et al. Stress, sleep and recovery in elite soccer: a critical review of the literature. Sports Med. 2015;45(10):1387–1400. doi: 10.1007/s40279-015-0358-z. [DOI] [PubMed] [Google Scholar]
- 13.Lastella M., Roach G.D., Sargent C. Travel fatigue and sleep/wake behaviors of professional soccer players during international competition. Sleep Health. 2019;5(2):141–147. doi: 10.1016/j.sleh.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Reyner L., Horne J.A. Sleep restriction and serving accuracy in performance tennis players, and effects of caffeine. Physiol Behav. 2013;120:93–96. doi: 10.1016/j.physbeh.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Mah C.D., Mah K.E., Kezirian E.J., et al. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34(7):943–950. doi: 10.5665/SLEEP.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fullagar H., Skorski S., Duffield R., et al. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161–186. doi: 10.1007/s40279-014-0260-0. [DOI] [PubMed] [Google Scholar]
- 17.Biggins M., Purtill H., Fowler P., et al. Sleep in elite multi-sport athletes: implications for athlete health and wellbeing. Phys Ther Sport. 2019;39:136–142. doi: 10.1016/j.ptsp.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Romyn G., Robey E., Dimmock J.A., et al. Sleep, anxiety and electronic device use by athletes in the training and competition environments. Eur J Sport Sci. 2016;16(3):301–308. doi: 10.1080/17461391.2015.1023221. [DOI] [PubMed] [Google Scholar]
- 19.Huskey A., Kim K., Emert S., et al. 315 athlete sleep and mental health: differences by gender, race, and ethnicity. Sleep. 2021;44(Supplement_2):A125–A126. [Google Scholar]
- 20.Mo Y. Analysis of factors associated with sleep disorders in professional athletes. Primary Care Med Forum. 2016;20(14-1314/R):4350–4351. doi: 10.19435/j.1672-1721.2016.31.011. [DOI] [Google Scholar]
- 21.Samuels C., James L., Lawson D., et al. The Athlete Sleep Screening Questionnaire: a new tool for assessing and managing sleep in elite athletes. Br J Sports Med. 2015;418 doi: 10.1136/bjsports-2014-094332. [DOI] [PubMed] [Google Scholar]
- 22.Bender A.M., Lawson D., Werthner P., et al. The clinical validation of the athlete sleep screening questionnaire: an instrument to identify athletes that need further sleep assessment. Sports medicine - open. 2018;4(1):23. doi: 10.1186/s40798-018-0140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan Chenhao AY., Lu Jiaojiao, Qiu Jun. Revision and validation of the Chinese version of the athlete sleeping screening ques- tionnaire. Sport Sci Res. 2021;3(42):1006–1207. [Google Scholar]
- 24.GAoSo China. Technical grade standards for athletes in each event. http://www.sport.gov.cn/n4/n207/n209/c23399926/content.html
- 25.Maijiu T. Establishment and scientific value of event group training theory. China Sports Coaches. 2016;24(3):4. doi: 10.1186/s40798-018-0140-510.3969/j.issn.1006-8732.2016.03.002. [DOI] [Google Scholar]
- 26.McHugh M.L. The chi-square test of independence. Biochem Med. 2013;23(2):143–149. doi: 10.11613/bm.2013.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim H.-Y. Statistical notes for clinical researchers: chi-squared test and Fisher's exact test. Restorative dentistry & endodontics. 2017;42(2):152–155. doi: 10.5395/rde.2017.42.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rabin J.M., Mehra R., Chen E., et al. Assessment of sleep health in collegiate athletes using the Athlete Sleep Screening Questionnaire. J Clin Sleep Med. 2020;16(8):1349–1356. doi: 10.5664/jcsm.8532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hrozanova M., Klöckner C.A., Sandbakk Ø., et al. Sex differences in sleep and influence of the menstrual cycle on women's sleep in junior endurance athletes. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0253376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duffield R., Murphy A., Kellett A., et al. Recovery from repeated on-court tennis sessions: combining cold-water immersion, compression, and sleep recovery interventions. Int J Sports Physiol Perform. 2014;9(2):273. doi: 10.1123/ijspp.2012-0359. [DOI] [PubMed] [Google Scholar]
- 31.Skein M., Duffield R., Minett G., et al. The effect of overnight sleep deprivation after competitive rugby league matches on postmatch physiological and perceptual recovery. Int J Sports Physiol Perform. 2013;8(5):556. doi: 10.1123/ijspp.8.5.556. [DOI] [PubMed] [Google Scholar]
- 32.Thun E., Bjorvatn B., Flo E., et al. Sleep, circadian rhythms, and athletic performance. Sleep Med Rev. 2015;23:1–9. doi: 10.1016/j.smrv.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Simpson N., Gibbs E., Matheson G. Optimizing sleep to maximize performance: implications and recommendations for elite athletes. Scand J Med Sci Sports. 2017;27(3):266–274. doi: 10.1111/sms.12703. [DOI] [PubMed] [Google Scholar]
- 34.Erlacher D., Ehrlenspiel F., Schredl M. Frequency of nightmares and gender significantly predict distressing dreams of German athletes before competitions or games. J Psychol. 2011;145(4):331–342. doi: 10.1080/00223980.2011.574166. [DOI] [PubMed] [Google Scholar]
- 35.Schaal K., Tafflet M., Nassif H., et al. Psychological balance in high level athletes: gender-based differences and sport-specific patterns. PLoS One. 2011;6(5) doi: 10.1371/journal.pone.0019007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kashani M., Eliasson A., Vernalis M. Perceived stress correlates with disturbed sleep: a link connecting stress and cardiovascular disease. Stress. 2012;15(1):45–51. doi: 10.3109/10253890.2011.578266. [DOI] [PubMed] [Google Scholar]
- 37.Litwic-Kaminska K., Kotysko M. Sleep quality of student athletes and non-athletes-the role of chronotype, stress and life satisfaction. Sleep Science. 2020;13(4):249. doi: 10.5935/1984-0063.20190153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bender A.M., Van Dongen H.P.A., Samuels C.H. Sleep quality and chronotype differences between elite athletes and non-athlete controls. Clocks Sleep. 2019;1(1):3–12. doi: 10.3390/clockssleep1010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vitale J.A., Bonato M., Galasso L., et al. Sleep quality and high intensity interval training at two different times of day: a crossover study on the influence of the chronotype in male collegiate soccer players. Chronobiol Int. 2017;34(2):260–268. doi: 10.1080/07420528.2016.1256301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.