Abstract
Background and Objectives
Evidence regarding the safety and efficacy of messenger RNA (mRNA) vaccines in patients with myasthenia gravis (MG) after immunosuppressive therapies is scarce. Our aim is to determine whether the mRNA-1273 vaccine is safe and able to induce humoral and cellular responses in patients with MG.
Methods
We performed an observational, longitudinal, prospective study including 100 patients with MG of a referral center for MG in our country, conducted from April 2021 to November 2021 during the vaccination campaign. The mRNA-1273 vaccine was scheduled for all participants. Blood samples were collected before vaccination and 3 months after a second dose. Clinical changes in MG were measured using the MG activities of daily life score at baseline and 1 week after the first and second doses. A surveillance of all symptoms of coronavirus disease 2019 (COVID-19) was conducted throughout the study. Humoral and cellular immune responses after vaccination were assessed using a spike-antibody ELISA and interferon gamma release assay in plasma. The primary outcomes were clinically significant changes in MG symptoms after vaccination, adverse events (AEs), and seroconversion and T-cell immune response rates.
Results
Ninety-nine patients completed the full vaccination schedule, and 98 had 2 blood samples taken. A statistically significant worsening of symptoms was identified after the first and second doses of the mRNA-1273 vaccine, but this was not clinically relevant. Mild AEs occurred in 14 patients after the first dose and in 21 patients after the second dose. Eighty-seven patients developed a humoral response and 72 patients showed a T-cell response after vaccination. A combined therapy with prednisone and other immunosuppressive drugs correlated with a lower seroconversion ratio (OR = 5.97, 95% CI 1.46–24.09, p = 0.015) and a lower T-cell response ratio (OR = 2.83, 95% CI 1.13–7.13, p = 0.024).
Discussion
Our findings indicate that the mRNA vaccination against COVID-19 is safe in patients with MG and show no negative impact on the disease course. Patients achieved high humoral and cellular immune response levels.
Classification of Evidence
This study provides Class IV evidence that patients with MG receiving the mRNA-1273 vaccine did not show clinical worsening after vaccination and that most of the patients achieved high cellular or immune response levels.
Myasthenia gravis (MG) is a rare neuromuscular disease caused by autoantibodies against postsynaptic receptors in the neuromuscular junction, which leads to muscular weakness.1-4 The disease is characterized by the fluctuations of symptoms over time, but triggering factors such as infections, surgery, and drugs may induce exacerbations.5-7 Several immunosuppressive and immunomodulator drugs are commonly used for the treatment of the disease.8,9
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has prompted the development of effective and safe vaccines based on new messenger RNA (mRNA) technology. These vaccines not only produce high seroconversion rates but are also capable of inducing a T-cell immunologic response against SARS-CoV-2.10-13
The need for massive vaccination has reignited the debate about the vaccine's safety in patients with MG and its efficacy in patients with autoimmune disease taking immunosuppressive therapies.14-16 Moreover, in view of the hypothetical role of the SARS-CoV-2 infection as a triggering factor of a myasthenic exacerbation that could induce respiratory insufficiency in addition to the severe respiratory distress that COVID-19 may cause, it is of interest to prevent the coronavirus infection in this group of patients.6,17-19
In this study, we aimed to longitudinally investigate humoral and cellular responses to mRNA-1273 vaccine in patients with MG and assess the vaccine safety regarding MG worsening and side effects.
Methods
Study Design and Patients
In this prospective longitudinal study, we prospectively recruited 100 unvaccinated patients with MG scheduled for SARS-CoV-2 vaccination between April and May 2021. In accordance with the health authorities' recommendations at that moment, patients with significant comorbidities, including MG, were offered vaccination, except for patients with a confirmed COVID-19 infection in the previous 6 months who were not considered candidates to immunization then. We excluded patients who had presented significant clinical or therapeutic changes in the previous 6 months.
Demographics (sex and age), date of MG onset, Myasthenia Gravis Foundation of America (MGFA) score at onset, highest MGFA score to date, MGFA score at baseline visit, and presence of thymoma were obtained from clinical records. Active and former immunosuppressive treatments since MG onset were also collected from the clinical records. Patients taking prednisone alone were classified as receiving monotherapy, and patients on prednisone combined with another immunosuppressive drug (e.g., azathioprine, mycofenolate mofetil, cyclosporine, tacrolimus, or rituximab) were considered to be on combination therapy. Patients were considered drug-refractory as defined by Sanders et al.9 COVID-19 symptoms were monitored using a telematic system.
Vaccination Protocol and Immune Response Evaluation
The Moderna COVID-19 (mRNA-1273) vaccine (Moderna TX, Inc., Cambridge, MA) was administered in accordance with the protocol at our center, and the recommended schedules were followed. All participants received 2 doses separated by 28 days.
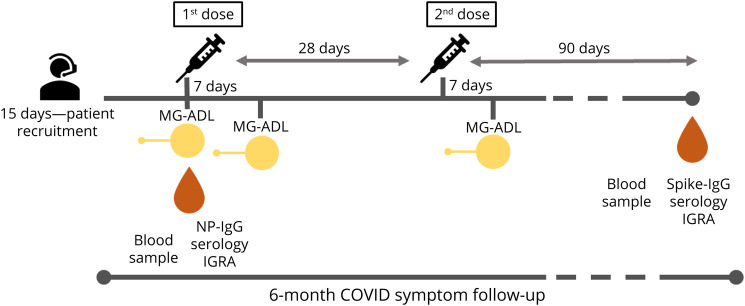
Blood samples were collected in serum and heparin tubes at baseline visit before the first vaccine dose and at 90 days after the second vaccine dose administration (Figure 1). Immunoglobulin G (IgG) positivity against nucleocapsid protein (NP) was detected in baseline blood samples using the SARS-CoV-2 NP-IgG ELISA kit in accordance with the manufacturer's instructions (MyBioSource, Inc., San Diego, CA, MBS398004), and a sample was considered positive when OD readings were greater than 0.2. A high-sensitive SARS-CoV-2 S1-IgG ELISA kit (MyBioSource, Inc., MBS398013) was used to detect spike-IgG in the 90 days after vaccination, following the manufacturer's instructions. A sample is considered positive if values were ≥5 IU/mL.
Figure 1. Study Concept.
Patients were prospectively recruited by telephone call over a period of 15 consecutive week days. The baseline MG-ADL score and a blood sample to assess NP-IgG serology and IGRA was obtained before the first dose was administered. Seven days after the first dose, a second MG-ADL score was obtained. The second dose of the vaccine was administered 28 days after the first dose, following the manufacturer's recommendations. A third MG-ADL score was administered a week after the second dose. For all 3 MG-ADL scores, patients were asked about symptoms in the previous 7 days to score each MG-ADL item. A second blood sample was obtained 90 days after the second dose, and IGRA and spike-IgG were determined. During a 6-month-follow-up, COVID-19 symptoms were telematically assessed in all patients. COVID-19 = coronavirus disease 2019; IgG = immunoglobulin G; IGRA = interferon gamma release assay; MG-ADL = myasthenia gravis activities of daily living score; NP-IgG serology = SARS-CoV-2 nucleocapsid protein antibodies serology; SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; spike-IgG serology = SARS-CoV-2 spike protein 1 IgG antibodies serology.
The cellular immune response was evaluated using an interferon gamma release assay (IGRA) method. A commercial kit (Quan-T-Cell SARS-CoV-2 EUROIMMUN, order no. ET 2606-3003. and Quan-T-Cell ELISA EUROIMMUN, order no. EQ 6841-9601) was used. According to the manufacturer's specifications, the EUROIMMUN recommends basing results on a borderline range. Positive results are considered those with >200 mIU/mL and negative results as those with <100 mIU/mL. Borderline results are those with levels between 100 and 200 mIU/mL, and indeterminate results are those with a nonvalid stimulation control. Finally, we grouped the participants as having either a T-cell IGRA positive or T-cell IGRA nonpositive result. Negative, borderline, and indeterminate results were included in the former group.
Clinical Changes in Myasthenia Gravis and Adverse Events
Clinical changes during the study were assessed using the validated myasthenia gravis activities of daily life (MG-ADL) score administered through telephone call. This is a quantitative, reliable, and simple-to-administer scale that reflects the severity of symptoms in MG and their effect on daily living activities.20
The MG-ADL score was obtained at 3 time points referred to MG symptoms occurring in the 7 days before the baseline visit, in the 7 days after the first dose administration, and in the 7 days after the second dose (Figure 1) in all patients. Changes in symptoms were considered clinically relevant when an increase in MG-ADL score of 3 points or more was observed.
All patients were instructed to contact the team if any symptoms of MG appeared or worsened within the first 2 months of the study. Adverse events (AEs) related to the vaccination were self-reported and collected from each patient in the 2 weeks after the first and second doses of the vaccine by telephone call or email. Severe AEs were those that resulted in hospitalization, disability, or a life-threatening event. To differentiate between generalized fatigue or other AEs and MG symptoms, patients who reported fatigue or flu-like symptoms for more than 72 hours were clinically assessed by neurologic examination. Patients were also instructed to contact the study team if COVID-19 symptoms and/or positive SARS-CoV-2 testing appeared during the study period and were telematically assessed.
Statistical Analysis
A descriptive statistics of the demographic variables, AEs, humoral and cellular immune responses, and statistical analyses were performed using IBM-SPSS Statistics v.21 software (IBM, Armonk, NY).
The time course of MG-ADL scores was explored using 1-way repeated measures analysis of variance. Greenhouse-Geisser correction was applied. We performed post hoc multiple comparisons by means of Bonferroni correction. Generalized linear models were used to study the effect of several variables on Spike-IgG and IGRA response. To discern between models, we considered plausibility of estimation and Akaike information criterion. We finally chose a Poisson log-linear model that included the following variables: sex, age, thymectomy, time of disease evolution, and the various types of immunosuppressive and immunomodulator treatment (prednisone, azathioprine, mycophenolate mofetil, cyclosporine, tacrolimus, periodic endovenous immunoglobulins, and periodic plasma exchange).
The Fisher exact test was used to compare the number of events between categorical groups of patients. The relative risk was also calculated to evaluate the risk of not developing a serologic or cellular immune response.
Standard Protocol Approvals, Registrations, and Patient Consents
The study was approved by the “Hospital de la Santa Creu i Sant Pau” ethics committee (IIBSP-COV-2021-26). All participants gave written informed consent to participate in the study.
Data Availability
Anonymized data not published within this article will be made available by request from any qualified investigator.
Results
Demographics and Baseline Characteristics of Patients With MG
From our registry of 378 patients with MG, 70 patients older than 80 years were already vaccinated when we started the study protocol. One patient was pregnant and did not meet vaccination criteria then, and 8 patients refused vaccination. One hundred patients were therefore finally included in the study.
Table 1 summarizes the baseline characteristics of these 100 patients. Blood samples were collected from all of them at the first time point and at the first and second MG-ADL. Ninety-nine patients completed the full vaccination protocol (see further). The remaining patient, who was on prednisone and azathioprine, was lost to follow-up after the first scheduled blood sample.
Table 1.
Baseline Characteristics, Medical History, and MG Treatments
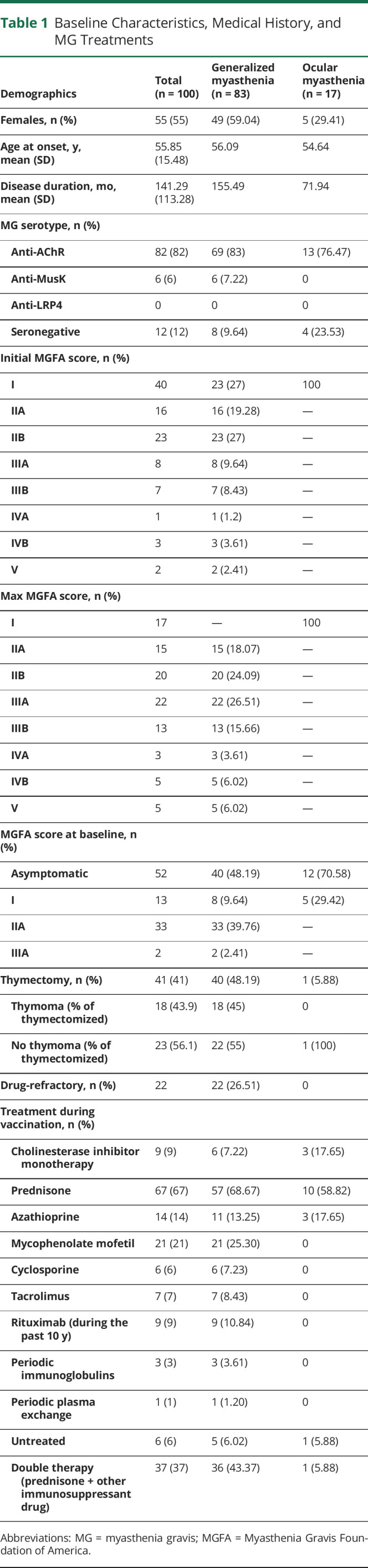
Four patients reported confirmed COVID-19 or PCR positive asymptomatic infection before the baseline visit. The mean time (SD) from infection to the first blood sample was 8.25 months (4.19). One patient reported close contact with a SARS-CoV-2–positive individual but did not develop symptoms.
Table 1 summarizes ongoing treatments in our cohort. Sixty-seven patients were on prednisone, 37 together with some type of concomitant immunosuppressive therapy: prednisone and mycophenolate in 20 patients; prednisone and azathioprine in 5; prednisone and cyclosporine in 6; and prednisone and tacrolimus in 2. Four further patients had been on prednisone and rituximab at some point in the last 10 years (September 2017, April 2018, May 2019, and November 2019). In addition, 1 patient on cyclosporine and prednisone at baseline received rituximab.
The mean prednisone dose (SD) was 12.6 mg daily (8.27). Nine patients were on high prednisone doses (daily doses greater than 20 mg). The mean doses of other immunosuppressant drugs were as follows: azathioprine, 110.71 mg/24 h (38.87); mycophenolate, 1,976 mg/24 h (109.11); cyclosporine, 166.67 mg/24 h (87.56); and tacrolimus, 4.14 mg/24 h (1.46).
One anti-MusK–positive female patient was undergoing rituximab treatment when the study started, with the most recent dose being administered in the month before immunization. This patient developed severe COVID-19 1 week after the first vaccine; she required ICU admission and mechanical ventilation but made a full recovery in 1 month. She did not receive the second dose of the vaccine in view of the recommendations of her infectious disease specialist. The remaining 8 patients on rituximab, treated between 2015 and 2019, received their second vaccine dose as scheduled, and none developed COVID-19.
Clinical Evaluation
The mean MG-ADL score (SD) at the beginning (n = 100) of the study was 2.34 (3.22). A week after the first dose (n = 100), it was 2.65 (3.52), and after the second dose, it was 2.72 (3.57) (n = 99). The effect of occasion was statistically significant (F = 5.074; p = 0.011). Further post hoc tests showed a statistically significant difference between the MG-ADL score at baseline and that after the first vaccine (p = 0.018) and between the MG-ADL score at baseline and that after the second dose (p = 0.046). However, no difference was observed between the first and second vaccine doses (p > 0.05). Nevertheless, the differences between baseline MG-ADL score and MG-ADL score after the first and second doses were less than 2 points.
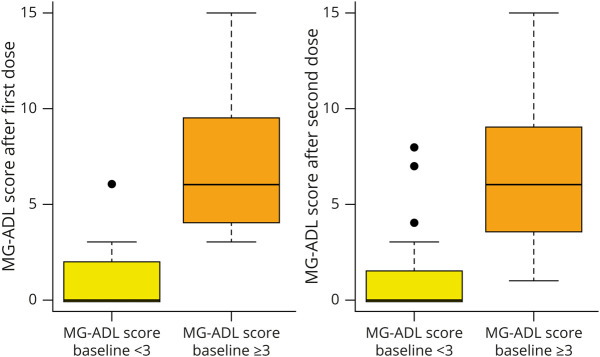
We observed an increase of 3 or more points in MG-ADL scores in 8 patients after the first vaccine dose and in 10 patients after the second vaccine dose. Five patients worsened after both doses, 3 with only the first dose and 5 with only the second one. In these cases, the mean worsening was 3.25 points after the first dose (2–7 range) and 3.9 points (2–7 range) after the second dose. Nonetheless, when we focused on baseline clinical characteristics, patients with an MG-ADL score greater than 3 points at baseline were prone to MG-ADL worsening after the first and second doses (Figure 2). In all but 1 patient, this worsening was self-limited—lasting less than 7 days—and mild, affecting ocular and limb items on the MG-ADL score, and they did not need any therapeutic interventions. So we did not considere those patients to have an MG exacerbation for the current analysis. The remaining case was a generalized MG patient with anti-AChR–positive antibodies MG-ADL 4 at baseline (diplopia 2 and ptosis 2) treated with 20 mg of prednisone every other day and pyridostigmine on demand. This patient experienced an MG exacerbation after the second dose of the vaccine with mild limb weakness together with moderate to severe worsening in ptosis and diplopia, reaching an MG-ADL score of 7 and requiring a modification of treatment comprising an increase in prednisone to 25 mg every other day and 6 pyridostigmine tablets. This worsening lasted for 4 months, and the number of pyridostigmine tablets was lowered to 1 tablet, achieving an MG-ADL 2 of ptosis and diplopia.
Figure 2. MG-ADL Score After Vaccination in Accordance With Baseline MG-ADL Score.
Boxplot representing the MG-ADL scores after the first and second doses. The vertical axis represents the MG-ADL score reported by the patients, from minimum to maximum. The horizontal axis represents the MG-ADL score at baseline less than 3 (yellow box) or equal to or greater than 3 (orange box). At both time points, patients with an MG-ADL at baseline of 3 points or more had a higher MG-ADL score after each dose, with higher ranges reflecting greater variability in that group. MG-ADL score = myasthenia gravis activities of daily living score.
No patients presented worsening of bulbar items of the MG-ADL score (dysarthria, swallowing, and dyspnea). Another patient who had an ocular phenotype and was asymptomatic at baseline (MG-ADL = 0) with 17.5 mg of prednisone every other day and 150 mg of azathioprine a day, presented with diplopia and ptosis, scoring 2 points in the MG-ADL 1 week after the last MG-ADL score was obtained. A change in therapy was required, with an increasing dose in prednisone until 30 mg per day. This worsening was excluded from the current analysis because it did not occur within the time limits of our study protocol.
Immune Response to the Vaccine
We assessed the immune response to vaccination in 98 patients. Four showed positive NP antibodies in baseline blood samples and spike-IgG seroconversion and IGRA positivity in their postvaccination blood sample.
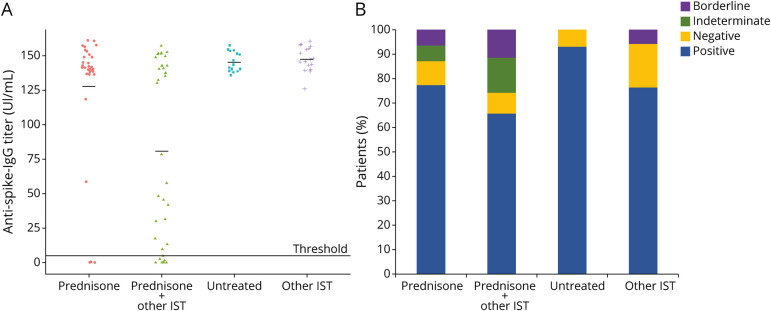
Eighty-seven of the 98 patients developed spike-IgG antibodies in the blood sample collected after vaccination (88.77%). The frequency of spike-IgG positivity in the different treatment groups is shown in Figure 3A. A statistically significant difference (the Fisher exact p = 0.015) was found between the percentage of seroconverted patients when they were grouped as taking either immunosuppressive monotherapy or combined therapy (prednisone and another immunosuppressant), with an OR = 5.97 (95% CI 1.46–24.09) of not seroconverting in this second group. None of the other variables analyzed were statistically significant in the generalized linear model.
Figure 3. Antispike-IgG Antibody titers and IGRA Positivity After Vaccinations According to Treatment Group.
(A) Antispike-IgG antibody titers in IU/mL is represented in the dot plot for each treatment group. The mean titer is represented by a black line for each group. Threshold line represents the 5 IU/mL cutoff for positivity. (B) Blue bars indicate the percentage of IGRA-positive patients. The percentage of IGRA-negative patients is indicated in yellow bars. Indeterminate IGRA are represented in green bars. IGRA resulting in borderline tests are represented in purple bars. IgG = immunoglobulin G; IGRA = interferon gamma release assay; IST = immunosuppressant therapy.
Of the nonimmunosuppressed patients, including patients on cholinesterase inhibitor monotherapy, 15/15 developed antispike antibodies after vaccination. No statistically significant differences were found (the Fisher exact p = 0.206) compared with those in patients on immunosuppressants (72/83 patients seroconverted).
Eight of the 98 patients had a negative IGRA result according to the manufacturer's recommendations. Eight other patients had a borderline result and 10 had an indeterminate result. Therefore, 72 of the 98 patients (73.47%) were IGRA positive. Figure 3B shows the frequency of IGRA results in each treatment group. The difference in the frequency of IGRA positive and IGRA nonpositive results between patients taking immunosuppressive monotherapy and those taking combined therapy was statistically significant. The Fisher exact test yielded a p value of 0.024 with an OR value of 2.83 (95% CI 1.13–7.13). None of the other variables included in the generalized linear model showed a statistically significant correlation (p > 0.05).
Fourteen of the 15 patients in the subgroup not on immunosuppressive therapy had a positive IGRA result after vaccination compared with 60/83 in the group of patients taking immunosuppressive therapy. This difference was not statistically significant (the Fisher exact p = 0.065).
Vaccination-Related AEs
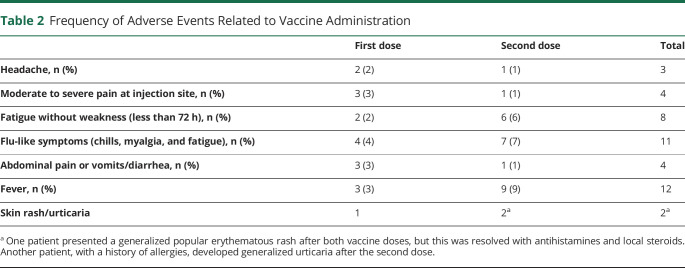
Fourteen patients reported AEs (14%) after the first dose, and 21 patients (21%) reported such events after the second dose. No statistically significant differences were found in the rates of reported AEs between patients on immunosuppressant therapy and patients not receiving immunosuppression after the first dose (the Fisher exact p = 0.687) and the second dose (the Fisher exact p = 0.301). Table 2 summarizes the main AEs and their frequency. No severe AEs were reported.
Table 2.
Frequency of Adverse Events Related to Vaccine Administration
Vaccine Efficacy Against Symptomatic COVID-19 After Vaccination
None of the 99 patients who received the full vaccination scheme developed symptomatic COVID-19 in the following 6 months.
Discussion
In this study, we prospectively studied a representative population of patients with MG after administration of the mRNA-based vaccine against COVID-19. Our results showed the participants did not develop clinically significant worsening of MG symptoms or severe side effects after vaccination. Moreover, patients achieved high rates of humoral and cellular immune responses, and none of those who completed the vaccination scheme had confirmed SARS-CoV-2 infection or suggestive symptoms during a high-incidence period in our country.
The use of vaccines in the autoimmune disease population has been a matter of debate for many years.21 Specifically in MG, vaccines have been considered a potential trigger of exacerbation, although scientific evidence is conflicting.15,22-24 Clinical case reports suggest that mRNA vaccines can lead to MG debut and moderate exacerbations25-27 and that COVID-19 may also lead to MG worsening.19 In our daily clinical practice, we observed that patients were concerned that the new mRNA vaccines could lead to clinical worsening of their illness, and this fear had an impact on their willingness to receive the vaccination against COVID-19.15,17,18 The findings from our study showed that the SARS-CoV-2 mRNA-1273 vaccine is safe in patients with MG. In our series, only 8% of patients had MG-ADL worsening ≥3 points after the first dose and only 10% after the second dose. No patients required hospitalization, and only 2 patients (2%) from among the whole cohort needed therapeutic intervention to control symptoms. Most of these patients had higher MG-ADL scores at baseline, probably reflecting poorer control of the disease and a greater predisposition to clinical fluctuations. Another finding of interest is that the patients experienced AEs less frequently than the healthy population studied in the mRNA-1273 clinical trial.11 We hypothesize that the effect of systemic corticosteroid therapy may have limited the development of systemic AEs.
In addition to safety issues, we aimed to elucidate the immunogenicity of this vaccine in autoimmune patients on immunosuppressive therapies. Preliminary mRNA 1273 studies observed seroconversion in 100% of participants,13 but patients under immunosuppression were excluded from the clinical trial. Several studies in patients receiving immunosuppressive drugs for various autoimmune diseases and in solid organ transplant recipients showed rates of seroconversion as low as 30% or less than those in seroconverted patients. This lack of efficacy seems to be more evident in patients on rituximab, fingolimod, or calcineurine inhibitors.28,29 For this reason, concerns have been raised in recent scientific literature about the lack of efficacy of the usual vaccination schemes in immunosuppressed patients.30 Specifically in neurologic disorders, a study performed in multiple sclerosis on different immunosuppressant treatment scheme patients assessing both humoral and cellular immune responses has been recently published.31 Our results showed a 100% seroconversion rate in untreated patients and a slightly lower rate (86.7%) in immunosuppressed patients. Although this lower rate, none of these patients developed COVID-19 symptoms during a 6-month follow-up in a period of high COVID-19 incidence in our country. In contrast with previous studies, our findings may be due to the use of fewer or lower doses of immunosuppressive drugs. Nevertheless, in agreement with other studies in highly immunosuppressed populations,28,29,31 a therapy combined with prednisone and another immunosuppressive drug resulted in an almost 6 times higher risk of not developing antibodies against spike protein.
Our study includes data about cellular T-cell response to mRNA-1273, another important immune trait that may constitute a long-lasting feature in the prevention of COVID-19. As shown in preliminary studies of the mRNA-1273 vaccine, many patients developed a T-cell response measured by quantifying cytokines and IF-gamma in serum after vaccination.13 In our study, 73.5% of our patients developed a T-cell response measured by IGRA. Patients on combined immunosuppressive therapy had nearly 3 times more risk of not achieving a T-cell immune response after vaccination than patients on monotherapy. Because of the difficulties in studying the vaccine efficacy in preventing COVID-19 infection in rare diseases such as MG, serologic and cell assays emerge as reliable surrogate biomarkers. These biomarkers may be useful to assess vaccine efficacy in rare autoimmune diseases.
The main limitation of our study is the lack of a proportional control group. Nevertheless, our cohort includes a group of patients with MG who were not taking immunosuppressive treatment and had a 100% rate of seroconversion and 93% of T-cell response measured by IGRA. A second limitation is the absence of a standardized method to assess the humoral and cellular responses to the COVID-19 vaccine. Several techniques are now available to measure antispike antibody titers and T-cell response based on different cytokines, limiting the external validity of our findings if the same methods are not applied. In addition, although we were unable to measure the complete immune response, the methods we used were sufficiently efficient to assess immune response for the purposes of this study.32 The main strength of this study is that it included a cohort of patients with MG taking a wide range of immunosuppressive therapies. Also this study gathered important information about the immune response after the COVID-19 vaccination protocol and adds new evidence to support the safety and efficacy of mRNA vaccines in patients with MG.
This study provides Class IV evidence that patients with MG receiving the mRNA-1273 vaccine did not show clinical worsening after vaccination and that most patients achieved high cellular or immune response levels.
Our results indicate that the mRNA-1273 vaccine does not cause significant AEs or relevant worsening in the clinical status of patients with MG. Despite receiving immunosuppressive therapy, the patients in this study achieved significant humoral and cellular immune responses, and none of those who completed the vaccination scheme developed COVID-19 during a period of high incidence. Taken together, these findings support the safety and efficacy of the mRNA-1273 vaccine in MG.
Acknowledgment
The authors are indebted to the patients for their encouragement to perform this study. The authors also thank the nurses Nuria Vidal, Concepción Escola, and Manuel Cabezas for their collaboration in collecting blood samples and technicians Carmen Martinez and Daniel Albert for managing laboratory samples. The authors also thank Dr Silvia Vidal for providing control blood samples. David Reyes-Leiva, Francesc Pla-Juncà, Ricard Rojas-García, Janina Turon-Sans, Luis Querol, Rodrigo Álvarez-Velasco, Montse Olivé, Isabel Illa, and Elena Cortés-Vicente are members of the European Reference Network for Neuromuscular Diseases (EURO-NMD). David Reyes-Leiva, Francesc Pla-Juncà, Ricard Rojas-García, Janina Turon-Sans, Luis Querol, Rodrigo Álvarez-Velasco, Montse Olivé, Isabel Illa, and Elena Cortés-Vicente work in a reference center for rare neuromuscular diseases (CSUR). David Reyes-Leiva, Francesc Pla-Juncà, Ricard Rojas-García, Janina Turon-Sans, Luis Querol, Rodrigo Álvarez-Velasco, Montse Olivé, Isabel Illa, and Elena Cortés-Vicente are members of XUECs (Networks of Specialized Centers of Excellence in Minority Health).
Glossary
- ADL
activities of daily life
- COVID-19
coronavirus disease 2019
- IgG
immunoglobulin G
- IGRA
interferon gamma release assay
- MG
myasthenia gravis
- MGFA
Myasthenia Gravis Foundation of America
- mRNA
messenger RNA
- NP
nucleocapsid protein
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
Appendix. Authors
Footnotes
See page e200010
Contributor Information
David Reyes-Leiva, Email: dreyes@santpau.cat.
Joaquín López-Contreras, Email: jlcontreras@santpau.cat.
Esther Moga, Email: mmoga@santpau.cat.
Francesc Pla-Juncà, Email: fpla@santpau.cat.
Elionor Lynton-Pons, Email: elynton@santpau.cat.
Ricardo Rojas-Garcia, Email: rrojas@santpau.cat.
Janina Turon-Sans, Email: jturon@santpau.cat.
Luis Querol, Email: lquerol@santpau.cat.
Montse Olive, Email: molivep@santpau.cat.
Rodrigo Álvarez-Velasco, Email: rodrigo.alvarez@salud.madrid.org.
Marta Caballero-Ávila, Email: mcaballeroa@santpau.cat.
Álvaro Carbayo, Email: acarbayo@santpau.cat.
Ana Vesperinas-Castro, Email: avesperinas@santpau.cat.
Pere Domingo, Email: pdomingo@santpau.cat.
Isabel Illa, Email: iilla@santpau.cat.
Eduard Gallardo, Email: egallardo@santpau.cat.
Elena Cortés-Vicente, Email: acarbayo@santpau.cat.
Study Funding
This work was funded by the “Instituto de Salud Carlos III” through project PI19/01774 (cofunded by the European Union ERDF), PI I. Illa and E. Gallardo; and the collaboration of “AMES” (Spanish Association of Myasthenia) and Cesce. The study was partially supported by the grant COV20/00070 from “Instituto de Salud Carlos III, Madrid, Spain” to Pere Domingo. E. Cortés-Vicente was supported by a “Juan Rodés” grant (JR19/00037) from the “Fondo de Investigación en Salud, Instituto de Salud Carlos III” and cofunded by the European Union (ERDF/ESF, “A way to make Europe”/“Investing in your future”), Ministry of Health (Spain).
Disclosure
The authors report no disclosures. Go to Neurology.org/NN for full disclosures.
References
- 1.Drachman DB, de Silva S, Ramsay D, Pestronk A. Humoral pathogenesis of myasthenia gravis. Ann NY Acad Sci. 1987;505:90-105. [DOI] [PubMed] [Google Scholar]
- 2.Hoch W, McConville J, Helms S, Newsom-Davis J, Melms A, Vincent A. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat Med. 2001;7(3):365-368. [DOI] [PubMed] [Google Scholar]
- 3.Querol L, Illa I. Myasthenia gravis and the neuromuscular junction: Curr Opin Neurol. 2013;26(5):459-465. [DOI] [PubMed] [Google Scholar]
- 4.Berrih-Aknin S, Souroujon MC. Cutting edge in myasthenia gravis. Autoimmun Rev. 2013;12(9):861-862. [DOI] [PubMed] [Google Scholar]
- 5.Thomas CE, Mayer SA, Gungor Y, et al. Myasthenic crisis: clinical features, mortality, complications, and risk factors for prolonged intubation. Neurology. 1997;48(5):1253-1260. [DOI] [PubMed] [Google Scholar]
- 6.Gilhus NE, Romi F, Hong Y, Skeie GO. Myasthenia gravis and infectious disease. J Neurol. 2018;265(6):1251-1258. [DOI] [PubMed] [Google Scholar]
- 7.Ramos-Fransi A, Rojas-García R, Segovia S, et al. Myasthenia gravis: descriptive analysis of life-threatening events in a recent nationwide registry. Eur J Neurol. 2015;22(7):1056-1061. [DOI] [PubMed] [Google Scholar]
- 8.Díaz-Manera J, Rojas García R, Illa I. Treatment strategies for myasthenia gravis: an update. Expert Opin Pharmacother. 2012;13(13):1873-1883. [DOI] [PubMed] [Google Scholar]
- 9.Sanders DB, Wolfe GI, Benatar M, et al. International consensus guidance for management of myasthenia gravis: executive summary. Neurology. 2016;87(4):419-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603-2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA vaccine against SARS-CoV-2—preliminary report. N Engl J Med. 2020;383(20):1920-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strijbos E, Huijbers MG, van Es IE, et al. A prospective, placebo controlled study on the humoral immune response to and safety of tetanus revaccination in myasthenia gravis. Vaccine. 2017;35(46):6290-6296. [DOI] [PubMed] [Google Scholar]
- 15.Auriel E, Regev K, Dori A, Karni A. Safety of influenza and H1N1 vaccinations in patients with myasthenia gravis, and patient compliance: short Reports. Muscle Nerve. 2011;43(6):893-894. [DOI] [PubMed] [Google Scholar]
- 16.Chung JY, Lee SJ, Shin B-S, Kang HG. Myasthenia gravis following human papillomavirus vaccination: a case report. BMC Neurol. 2018;18(1):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacob S, Muppidi S, Guidon A, et al. Guidance for the management of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19 pandemic. J Neurol Sci. 2020;412:116803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guidon AC, Amato AA. COVID-19 and neuromuscular disorders. Neurology. 2020;94(22):959-969. [DOI] [PubMed] [Google Scholar]
- 19.Muppidi S, Guptill JT, Jacob S, et al. COVID-19-associated risks and effects in myasthenia gravis (CARE-MG). Lancet Neurol. 2020;19(12):970-971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfe GI, Herbelin L, Nations SP, Foster B, Bryan WW, Barohn RJ. Myasthenia gravis activities of daily living profile. Neurology. 1999;52(7):1487-1487. [DOI] [PubMed] [Google Scholar]
- 21.Shoenfeld Y. Infections, vaccines and autoimmunity. Lupus. 2009;18(13):1127-1128. [DOI] [PubMed] [Google Scholar]
- 22.Zinman L, Thoma J, Kwong JC, Kopp A, Stukel TA, Juurlink DN. Safety of influenza vaccination in patients with myasthenia gravis: a population-based study: influenza vaccine in MG patients. Muscle Nerve. 2009;40(6):947-951. [DOI] [PubMed] [Google Scholar]
- 23.Ruan Z, Tang Y, Li C, et al. COVID-19 vaccination in patients with myasthenia gravis: a single-center case series. Vaccines (Basel). 2021;9(10):1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seok HY, Shin HY, Kim JK, et al. The impacts of influenza infection and vaccination on exacerbation of myasthenia gravis. J Clin Neurol. 2017;13(4):325-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tagliaferri AR, Narvaneni S, Azzam MH, Grist W. A case of COVID-19 vaccine causing a myasthenia gravis crisis. Cureus. 2021;13(6):e15581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaulen LD, Doubrovinskaia S, Mooshage C, et al. Neurological autoimmune diseases following vaccinations against SARS-CoV-2: a case series. Eur J Neurol. 2022;29(2):555-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chavez A, Pougnier C. A case of COVID-19 vaccine associated new diagnosis myasthenia gravis. J Prim Care Community Health. 2021;12:21501327211051932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner A, Jasinska J, Tomosel E, Zielinski CC, Wiedermann U. Absent antibody production following COVID19 vaccination with mRNA in patients under immunosuppressive treatments. Vaccine. 2021;39(51):7375-7378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall VG, Ferreira VH, Ierullo M, et al. Humoral and cellular immune response and safety of two-dose SARS-CoV-2 mRNA-1273 vaccine in solid organ transplant recipients. Am J Transplant. 2021;21(12):3980-3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Golding B, Lee Y, Golding H, Khurana S. Pause in immunosuppressive treatment results in improved immune response to SARS-CoV-2 vaccine in autoimmune patient: a case report. Ann Rheum Dis. 2021;80(10):1359-1361. [DOI] [PubMed] [Google Scholar]
- 31.Tortorella C, Aiello A, Gasperini C, et al. Humoral- and T-cell–specific immune responses to SARS-CoV-2 mRNA vaccination in patients with MS using different disease-modifying therapies. Neurology. 2022;98(5):e541-e554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel N, Bouchard J, Oliver MB, Badowski ME, Carreno JJ; Society of Infectious Diseases Pharmacists. Early clinical trial data and real-world assessment of COVID-19 vaccines: insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2021;41(10):837-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.