Abstract
Objective
To determine the effectiveness of community-based rehabilitation interventions which incorporate outdoor mobility on physical activity, endurance, outdoor mobility and falls-related self-efficacy in older adults.
Design
MEDLINE, Embase, CINAHL, PEDro and OpenGrey were searched systematically from inception to June 2021 for randomised controlled trials (RCTs) of community-based rehabilitation incorporating outdoor mobility on physical activity, endurance, outdoor mobility and/or falls-related self-efficacy in older adults. Duplicate screening, selection, extraction and appraisal were completed. Results were reported descriptively and with random-effects meta-analyses stratified by population (proactive [community-dwelling], reactive [illness/injury]).
Results
A total of 29 RCTs with 7,076 participants were identified (66% high bias for at least one domain). The outdoor mobility component was predominantly a walking programme with behaviour change. Rehabilitation for reactive populations increased physical activity (seven RCTs, 587 participants. Hedge’s g 1.32, 95% CI: 0.31, 2.32), endurance (four RCTs, 392 participants. Hedges g 0.24; 95% CI: 0.04, 0.44) and outdoor mobility (two RCTs with 663 participants. Go out as much as wanted, likelihood of a journey) at intervention end versus usual care. Where reported, effects were preserved at follow-up. One RCT indicated a benefit of rehabilitation for proactive populations on moderate-to-vigorous activity and outdoor mobility. No effect was noted for falls-related self-efficacy, or other outcomes following rehabilitation for proactive populations.
Conclusion
Reactive rehabilitation for older adults may include walking programmes with behaviour change techniques. Future research should address the potential benefit of a walking programme for proactive populations and address mobility-related anxiety as a barrier to outdoor mobility for both proactive and reactive populations.
Keywords: outdoor mobility, rehabilitation, physical activity, walking, social, older people, systematic review
Key Points
The proportion of older adults who are mobile outdoors is low, and this declines with illness/injury.
Loss of outdoor mobility is associated with poor health and social care outcomes.
Rehabilitation with outdoor mobility increased activity, outdoor mobility and endurance for older adults with illness/injury.
Rehabilitation for older adults with illness/injury should include walking programmes with behaviour change techniques.
Evidence was less certain for rehabilitation incorporating outdoor mobility for proactive populations of older adults.
Introduction
Older adults experience a gradual decline in functional capacity which often manifest in functional limitations including mobility limitations [1]. A reduction in outdoor mobility is associated with social withdrawal [2], higher disability in activities of daily living (ADL) [3], transition to care home [4] and mortality [5]. Despite this, between 10.3% (USA) [6] and 15.4% (Finland) [7] of community-dwelling older adults are not mobile outdoors. This decreases further following surgical and non-surgical hospitalisation [8].
Poor rates of outdoor mobility may be due to several influencing factors at both an environmental and individual level [9, 10]. Outdoor mobility is more physically, psychologically and cognitively challenging than mobilising in the controlled environment of a person’s own home. There are uneven surfaces, steps and obstructed walkways which present a challenge for strength, balance and coordination [9]. Navigating outdoor environments on foot or by transport requires confidence and self-efficacy [11], as well as the cognitive ability to adapt to ever-changing spaces [12]. As such, outdoor mobility is negatively affected by physical, psychological or cognitive impairment [9, 13].
Optimising outdoor mobility has the potential to preserve and/or improve the quality of life of older adults through increased opportunities for physical activity promoting independence [14] while negating the risks of comorbid disease and illness [3], and social isolation/loneliness [2]. Further, quality of life may be improved among carers of older adults by reducing the need to adapt to increased dependency [15]. As such, several randomised controlled trials (RCTs) of rehabilitation for community-dwelling older adults [16, 17] as well as rehabilitation for community-dwelling older adults with illness or injury [18, 19] include an outdoor mobility component. These components vary from supervised walking programmes [20] to mobility related goal setting [21] and their role in intervention effectiveness is not well understood.
Therefore, this review sought to determine the effectiveness of community-based rehabilitation interventions which incorporate outdoor mobility on physical activity, endurance, outdoor mobility and falls-related self-efficacy in older adults.
Methods
We reported this review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [22]. The protocol is registered on the International Register for Systematic Reviews (PROSPERO ID: CRD4202164082) [23].
Eligibility
We included definitive RCTs of community-based (any setting other than inpatient) rehabilitation interventions which incorporated an outdoor mobility component, and which sought to improve physical activity, endurance, outdoor mobility and/or falls-related self-efficacy against any comparator among adults aged 65 years or older. We defined rehabilitation using the World Health Organisation (WHO) definition as ‘a set of interventions designed to optimise functioning and reduce disability in individuals with health conditions in interaction with their environment’ [24]. We considered outdoor mobility components ranging from supervised outdoor walking to outdoor mobility goal setting. We excluded RCTs delivered exclusively in care homes.
Search
We searched five electronic databases: MEDLINE, Embase, CINAHL, PEDro and OpenGrey from database inception to 14 June 2021. We used published terms for the population (older adults) [25–28], the intervention (outdoor mobility) [25, 29], setting [25, 29] and study design (RCTs) [29, 30] (Supplementary File 1). Searches were limited to human and English language.
Selection
We completed title and abstract and full-text screening in duplicate in Covidence [31]. Conflicts were resolved by consensus. We screened reference lists of eligible RCTs. We contacted three authors to determine eligibility.
Quality assessment
We assessed quality in duplicate using the Cochrane Risk of Bias Tool considering bias in selection, performance, detection, attrition and reporting [32].
Extraction
We extracted data in duplicate onto a template adapted from the taxonomy to classify and describe fall-prevention interventions [33] including author, year, location, sample size, eligibility, intervention, comparator, longest follow-up and outcome—measure of central tendency and dispersion for physical activity, endurance, outdoor mobility and/or falls-related self-efficacy at intervention end and final follow-up. Where outcomes were reported as medians and ranges they were converted to means and standard deviations [34]. Where dispersion was presented as 95% confidence intervals they were converted first to standard errors allowing subsequent conversion to standard deviations (standard error x √sample size = standard deviation) [35]. Conflicts were resolved by consensus.
Synthesis
Analyses were completed in Stata v16 [36]. We used random-effects meta-analyses to calculate effects sizes (Hedge’s g (continuous) and Log-Odds Ratios (categorical)). Analyses were stratified by target population—proactive (community-dwelling) or reactive (illness/injury). We interpreted an effect size of 0.2 as small, 0.5 moderate and 0.8 as large [35]. We used I2 to assess heterogeneity considering 0–40% as unimportant, 30–60% as moderate, 50–90% as substantial and 75–100% as considerable [35]. We reported results not included in meta-analyses (as measures of dispersion/central tendency not provided and/or only 1 RCT for a given outcome) descriptively.
We used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) criteria to determine the confidence in effect estimates for each outcome [37]. GRADE downgrades RCTs based on risk of bias, inconsistency, imprecision, indirectness and publication bias. Conflicts were resolved by consensus [37].
Results
Selection
We identified 9,775 studies following deduplication. In total 9,694 were excluded on title and abstract screening and a further 47 on full-text screening. We included 33 articles for 28 RCTs in this review i.e. 10 articles reflected five RCTs (Figure 1).
Figure 1.
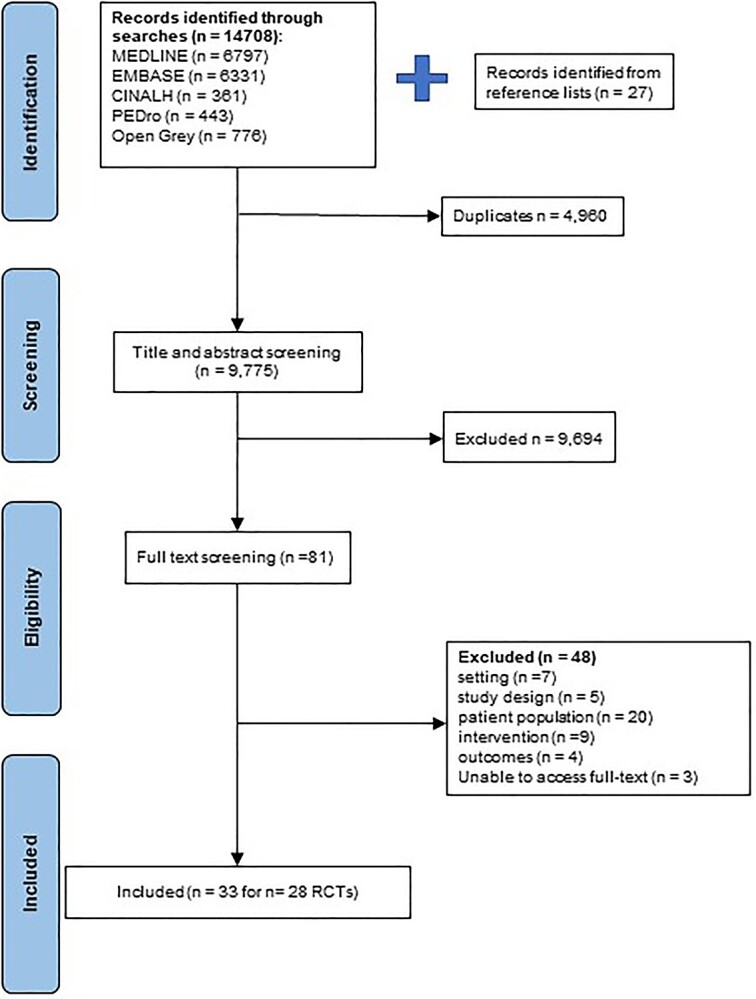
Study selection.
Quality assessment
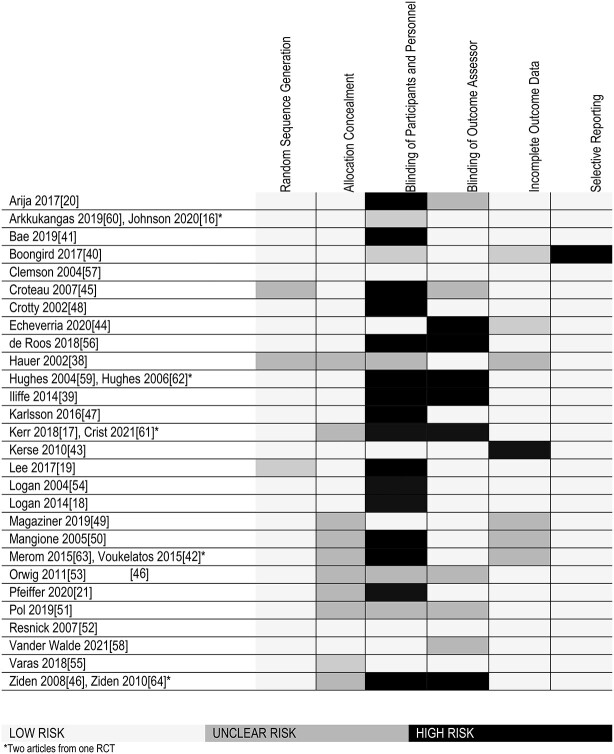
We present results of the quality assessment in Table 1. The most common reasons for high bias assignment were performance bias (n = 16) and detection bias (n = 7).
Table 1.
Risk of bias
|
Characteristics of RCTs
Characteristics of the 29 RCTs are available in Table 2. In total 7,076 older adults took part in the RCTs with sample sizes ranging from 28 [38] to 1,256 [39] participants. A total of 10 RCTs targeted proactive (community-dwelling) populations [16, 17, 20, 39–45]. Reactive populations included older adults with a specific condition: hip fracture (n = 10) [21, 38, 46–53], stroke (n = 2) [18, 54], chronic obstructive pulmonary disease (COPD) (n = 2) [55, 56], falls risk (n = 1) [57], depressive symptoms (n = 1) [17], cancer (n = 1) [58], osteoarthritis (n = 1) [59] or hypertension (n = 1) [19].
Table 2.
Characteristics of randomised controlled trials
| Author/year | Location | Sample size I:C |
Recruitment | Population | Intervention setting |
Comparator | Relevant outcome/s† | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Arija 2017 [20] | Spain | 260:104 | Primary care | Inclusion: primary care catchment, mean age >65 years Exclusion: episode of ischemic heart disease less than 6 months previously, acute episode of arthritis that would limit the ability to walk, lung or heart disease causing dyspnoea |
Community | Usual care | International Physical Activity Questionnaire, short version | 9 months |
| Arkkukangas 2019 [60] and Tuvemo Johnson 2021 [16]* |
Sweden | 61:58:56 | Patients who requested walking aids/home care from health centres or municipality | Inclusion: ≥75 years, able to walk independently and understand written and oral information in Swedish, mean age >80 years Exclusion: scoring <25 on the Mini Mental State Examination, ongoing regular physiotherapy, terminal care |
Home and healthcare centres | Otago exercise program | Falls Efficacy Scale (Swedish version) The Frandin/Grimby Activity Scale |
12 weeks, 12 months and 24 months |
| Bae 2019 [41] | Japan | 41:42 | The National Centre for Geriatrics and Gerontology Study of Geriatric Syndromes | Inclusion: mild cognitive impairment, normal general cognitive function, no evidence of functional dependency, no dementia, mean age >65 Exclusion: <65 years, certification of needing care from the long-term care insurance, disability in activities of daily living, history of Parkinson’s or Alzheimer’s disease, depression, contraindication of exercise by GP, pacemaker, connection to this research, frequent 1–10 km trips outdoors, currently employed, no mild cognitive impairment, missing data |
Community | Oral care and nutrition education | Time spent in moderate-to-vigorous physical activity Step count Going outdoors, number of times/day |
N/A |
| Boongird 2017 [40] | Thailand | 219:220 | N/A | Inclusion: mild to moderate balance dysfunction, mean age >65 Exclusion: moderate to severe cognitive problems, neurological conditions influencing gait and mobility, acute arthritis, unstable or terminal illness that would preclude the planned exercises, not Thai speaking, participating in regular strengthening exercise |
Primary care clinics | Falls prevention education | Thai fall efficacy scale | 3, 6, 9 and 12 months |
| Clemson 2004 [57] | Australia | 157:153 | Promotional material, health referrals, advertisements, mailing lists, department of veteran’s affairs, football clubs, community organisations | Inclusion: fallen in the previous year, consider themselves at risk of falling, conversational English, mean age >70 years Exclusion: cognitive problems associated with dementia, homebound, unable to independently leave home |
Predetermined community venue | Two social visits from an occupational therapist | Modified Falls-Efficacy Scale Physical Activity Scale for the Elderly |
N/A |
| Croteau 2007 [45] | USA | 95:84 | Health, educational, and social programmes in the community | Inclusion: able to ambulate independently, able to walk at velocity and/or with appropriate gait patterns necessary to permit adequate pedometer readings, wears appropriate clothing, physician approval, mean age >70 years | Community | Wait-list controls instructed to continue with their usual activity | Daily step counts | 12 weeks, 24 weeks |
| Crotty 2002 [48] |
Australia | 34:32 | Acute hospital | Inclusion: hip fracture, medically stable, physical and mental capacity, expected home discharge Exclusion: inadequate social support, no telephone, outside catchment, mean age >80 years |
Home | Routine care | Falls Efficacy Scale | 4 months |
| de Roos 2018 [56] | The Netherlands | 26:26 | Primary general care practices and hospital | Inclusion: Clinically stable COPD (GOLD Stage II COPD—≤50% FEV1 < 80%), score of ≥2 on Medical Research Council Dyspnoea Scale, mean age >70 years Exclusion: Exercise-restricting, non-COPD related complaints (e.g. severe cardiac or MSK issues) |
Primary physiotherapy care centre and home | Usual care | Daily physical activity (minutes per day) 6-min Walk test |
10 weeks |
| Echeverria 2020 [44] | Spain | 27:28 | Internal Medicine and Neurology services of University Hospital of Araba | Inclusion: ≥70 years, scored ≥20 on the Mini Mental State Examination, able to walk at least 4 m independently, mean age >80 years Exclusion: Chronic kidney disease, severe dementia, autoimmune neuromuscular disease, acute myocardial infarction, bone fracture in the last 3 months, refusal to sign informed consent |
Hospital and home | Short-term program | 6-min walk test Time in moderate-vigorous physical activity steps per day |
24 weeks |
| Hauer 2002 [38] |
Germany | 15:13 | Inpatient rehabilitation | Inclusion: hip fracture, ≥75 years, female, mean age >80 years Exclusion: severe cognitive/cardiovascular/musculoskeletal disease, acute neurological impairment, unstable chronic/terminal illness, major depression |
Outpatient geriatric rehabilitation unit | Seated activities | Physical activity questionnaire for elderly people | 3 months |
| Hughes 2004 [59] Hughes 2006 [62]* |
USA | 80:70 | Newsletter, announcements in the local media, presentations to local senior groups | Inclusion: clinical presence of lower extremity joint osteoarthritis, mean age >70 years Exclusion: <60 years, participating in an aerobic exercise programme, have had uncomplicated hip or knee surgery within the previous 6 months or complicated surgery within the past year, have received steroid injections in either knee or hip within the previous 3 months; a diagnosis of rheumatoid arthritis, moderate to severe cognitive impairment; severe, limiting cardiovascular disease, active thrombophlebitis, recent pulmonary embolus, acute systemic illness, poorly controlled diabetes, people with other health conditions precluding exercise. |
Senior centres, senior housing residences | ‘The Arthritis Helpbook’, a list of community exercise programmes, self-care materials and handouts | 6-min walk test Maintenance of Physical Activity (minutes per week) |
2, 6, 9, and 12 months |
| Iliffe 2014 [39] | UK | 411:387:458 | General practices, mailed invitations, telephone contact | Inclusion: commitment to participate for the duration of the study, availability of suitable community venue, ≥65 years, able to walk independently indoors and outdoors, physically able to take part in a group exercise class, eligible to participate in the trial, mean age >70 years Exclusion: significant cognitive impairment, three or more self-reported falls in the previous year, resting blood pressure >180/100 mmHg, tachycardia >100 bpm, uncontrolled hypertension as considered by GP, drop in blood pressure during exercise, psychiatric conditions preventing participation in an exercise class, uncontrolled medical problems, conditions requiring a specialist exercise program, unable to maintain a seated upright position, unable to move independently indoors, not living independently, receiving long-term physiotherapy, already in an exercise program. |
Home | Free to participate in any other exercise as they normally would | Proportion meeting target of ≥150 min of moderate-vigorous physical activity per week (Community Health Activities Model Program for Seniors scale) Physical Activity Scale for the Elderly Falls-related self-efficacy |
6, 12, 18 and 24 months |
| Karlsson 2016 [47] | Sweden | 107:98 | Geriatric ward | Inclusion: hip fracture, ≥70 years, living in the municipality of Umeå, lives in ordinary housing or residential care facilities, dementia and cognitive impairments were included, mean age >80 years Exclusion: pathological fractures and those whose hip fracture occurred in hospital |
Home | Conventional geriatric care and rehabilitation | Walking ability indoors and outdoors | 3 and 12 months |
| Kerr 2018 [17] and Crist 2021 [61]* | USA | 151:156 and 150:155 |
Flyers, presentations, participant testimonials from previous sites, encouragement from site staff and peers | Inclusion: >65 years, timed up and go <30 s, able to walk 20 m without assistance, no falls in previous 12 months that resulted in hospitalisation, able to talk over the phone, no plans to move in the next 12 months, completion of post-consent comprehension test, mean age >80 years Exclusion: dementia or cognitive impairment |
Continuing Care Retirement Communities | Education on successful ageing and four general health calls |
Physical activity (minutes of moderate-vigorous per day) Time spent in four mutually exclusive domains further from home (GPS) |
3, 6, 9 and 12 months |
| Kerse 2010 [43] | New Zealand | 97:96 | Invitation from primary care practitioner | Inclusion: ≥75 years, community dwelling, able to communicate in English, complete assessments, no severe dementia or unstable medical conditions preventing participation in physical activity, mean age >80 years Exclusion: dementia/cognitive impairment, living in residential care, terminal illness, unable to communicate in English, unstable medical condition |
Home | Social visits | Auckland Heart Study Physical Activity Questionnaire | 6 and 12 months |
| Lee 2007 [19] | Taiwan | 102:100 | Eligible individuals identified and contacted from healthcare database | Inclusion: resident in local township, mild to moderate hypertension (resting systolic blood pressure between 140 mmHg and 179 mmHg), mean age >70 years Exclusion: Unable to walk regularly, high blood pressure |
Community, home and/or telephone | Usual care | Self-Efficacy for Exercise Scale | 6 months |
| Logan 2004 [54] | UK | 86:82 | GP registers | Inclusion: clinical diagnosis of stroke in the last 36 months, mean age >70 years | Home | Routine care and transport leaflets | Outdoor mobility satisfaction Number of journeys made outside the house |
4 and 10 months |
| Logan 2014 [18] | UK | 287:281 | General practices, primary care therapy teams, community stroke teams, outpatient clinics | Inclusion: stroke at least 6 weeks previously, wished to get out of the house more often, mean age >70 years Exclusion: not able to comply with the protocol and therapy programme, being in active rehabilitation |
Home | Verbal advice, packs of local travel information | Number of journeys made outside the house Satisfaction with outdoor mobility |
6 months, 12 months |
| Magaziner 2019 [49] | USA | 105:105 | Clinic/health centres | Inclusion: hip fracture, community dwelling, ambulatory prefracture, <300 m in 6-min walk test at randomisation, mean age >80 years Exclusion: medically unstable, pathological fracture, low potential to benefit, practical impediments to participation |
Home | Seated activities and TENS | 6-min walk test | 4 months |
| Mangione 2005 [50] | USA | 13:17:11 | Physiotherapy practice | Inclusion: hip fracture, ≥65 years, living at home, discharged from physiotherapy, able to travel for assessment, mean age >75 years Exclusion: MMSE<20, unstable angina, uncompensated congestive heart failure, metabolic conditions that limit training, residual hemiplegia, Parkinsons Disease, life expectancy of <6 months, nursing home dwelling |
Home | Routine care and written materials | 6-min walk test | 3 months |
| Orwig 2011 [53] |
USA | 91:89 | Acute hospital | Inclusion: hip fracture, ≥65 years, female, community dwelling, ambulatory unaided prefracture, mean age >80 years Exclusion: <20 MMSE, pathological fracture, cardiovascular/neurologic/respiratory diseases/conditions which increased risk of falls limiting exercising home alone, bone disease, metastatic cancer, cirrhosis, end-stage renal disease, hardware in contralateral hip |
Home | Routine care | Yale Physical Activity Scale | 2,6, and 12 months |
| Pfeiffer 2020 [21] |
Germany | 57:58 | Inpatient rehabilitation | Inclusion: hip fracture, community-dwelling, positively screened for fear of falling, mean age >80 years Exclusion: cognitive impairment, severe communication deficiencies |
Inpatient rehabilitation and home | Routine care | Short Falls Efficacy Scale Daily walking duration |
3 months |
| Pol 2019 [51] |
Netherlands | 87:76:77 | Nursing and community care facilities | Inclusion: hip fracture, ≥65 years, living alone, MMSE ≥15 Exclusion: MMSE <15, terminal illness, awaiting nursing home placement, mean age >80 years |
Home, nursing and community care facilities | Routine care | Falls Efficacy Scale International | 1, 4 and 6 months |
| Resnick 2007 [52] |
USA | 51:54:52:51 | Acute hospital | Inclusion: hip fracture, ≥65 years, female, community dwelling, clearance from surgeon, mean age ≥80 years Exclusion: MMSE <20, medical problems that increase falls risk when exercising home alone, walking unaided prefracture, pathological fracture |
Home | Routine care | Self-efficacy for walking/exercise scale The Yale Physical Activity Survey |
2, 6 and 12 months |
| VanderWalde 2021 [58] | USA | 27:27 | Dept of Radiation Oncology at the West Cancer Center and Research Institute | Inclusion: ≥65 years, English speaking, stage 0–3 breast cancer, exercise less than 120 min per week, scheduled to receive either whole breast or regional radiotherapy with curative intent, mean age >65 years Exclusion: those who exercise ≥120 min per week, too unhealthy to walk safely |
Home | Standard fractionated radiotherapy | 1 month | |
| Varas 2018 [55] | Spain | 21:19 | Hospital at Universidad Autonoma de Madrid | Inclusion: COPD diagnosis, no exacerbation 4 weeks prior to the study, exertional dyspnoea, habitual low physical activity level (<30 min of moderate intensity exercise per day) mean age >65 years Exclusion: difficulty walking, CVD (except high BP), participated in a PR programme in the 12 months prior |
Community | Exercise education, pedometer with general recommendations to walk more every day | Exercise capacity—Endurance Shuttle test Physical activity (average number of steps/day) |
10 weeks, 3 and. 12 months |
| Voukelatos 2015 [42] and Merom 2015 [63]* | Australia | 191:194 145:170 |
Newspaper advertisements, personal and professional referrals, sampling from Australian electoral roll | Inclusion: ≥65 years, inactive (<120 min exercise per week), able to walk at least 50 m, able to communicate in English, walk unaided or with manual assistance for 50 m, mean age >70 years Exclusion: neurological conditions limiting participation or cognitive impairment |
Home | Health education | Falls Efficacy Scale-International Incidental and Planned Exercise Questionnaire |
2 months and 12 months |
| Ziden 2008 [46] and Ziden 2010 [64]* | Sweden | 48:54 | Community-dwelling patients with hip fracture in the central or western parts of Goteborg | Inclusion: hip fracture, ≥65 years, able to speak and understand Swedish, mean age >80 years Exclusion: severe medical illness with expected survival of <1 year, severe drug or alcohol abuse, mental illness, or severe cognitive impairment |
Home | Conventional Care | Falls efficacy Scale, Swedish version | 1, 6 and 12 months |
I: Intervention C: Control COPD: Chronic Pulmonary Disease
*Two articles for one RCT
†Relevant to current systematic review
RCTs compared interventions with usual care (n = 15) [16, 19–21, 39, 45–48, 51–54, 56, 58], education (n = 8) [17, 18, 40–42, 50, 55, 59] and sham active controls including seated activities [38] or seated activities and transcutaneous electrical stimulation [49]. One RCT compared a short duration intervention with a longer duration intervention [44]. All included RCTs captured physical activity (objective/self-report), endurance, outdoor mobility and/or falls-related self-efficacy as a primary/secondary outcome measure (Table 2).
Interventions
Detailed descriptors of interventions are available in Table 3. Interventions were home-based (n = 14) [18, 21, 41–43, 46–50, 52–54, 58], community-based (n = 6) [17, 19, 20, 38, 42, 57] or included both home and community components (n = 8) [16, 39, 40, 44, 45, 51, 56, 59]. Intervention durations ranged from 3 weeks [46] to 48 weeks [42], with longest follow-up ranging from 1 month [58] to 24 months [39, 60].
Table 3.
Intervention descriptors
| Author year |
Supervised/ unsupervised |
Type | Duration | Frequency | Intensity | Psychological | Environment/ assistive technology |
Knowledge | Outdoor |
|---|---|---|---|---|---|---|---|---|---|
| Arija 2017 [20] | supervised | socio-cultural activities and walking itineraries (average 5 km circuits) accompanied and monitored by healthcare professionals | 9 months | 2 walking sessions per week, socio-cultural activities once per month |
120 min/week walking (396 METs min/week) | no | no | walking itineraries | outdoor sociocultural activities, walks encouraged in and around the city |
| Arkkukangas 2019 [60], Tuvemo Johnson 2021 [16]* | supervised | a: Otago exercise programme and walking programme b: Otago exercise programme, walking programme, and motivational interviewing |
12 weeks | a and b: exercise three times per week b: motivational interviewing five sessions |
a and b: exercise 30 min | b: motivational interviewing | ankle weight | exercise manual with pictures and description of each exercise | walks encouraged in between exercise days |
| Bae 2019 [41] | supervised | four to five participants and two staff per group. Stretching, physical cognitive and social activities tailored to preference and available community resources near their residence. | 24 weeks | twice weekly | 90 min | social activities; group based | accelerometer | no | outdoor activity of choice e.g. walking, visiting temple, shopping |
| Boongird 2017 [40] | unsupervised following 1 h demonstration; telephone progress monitoring | modified Otago program and a walking plan | 12 weeks | exercise six times weekly; twice weekly walking | 20 min exercises; 30 min walking | weekly planners | video disc recorder | fall prevention education, exercise manual | walks encouraged 2 x 30 min weekly |
| Clemson 2004 [57] | supervised | 12 participants in each group. Lower limb balance and strengthening, community mobility and discrete skills. One session included a community mastery experience during which community mobility and discrete skills e.g. negotiating grass or curb ramps were practiced. | 7 weeks | once weekly | 120 min | group based. Reflections and sharing accomplishments, action planning, weekly homework | no | coping with visual loss and regular screening, medication management, environmental and behavioural home safety, community safety | community mobility session |
| Croteau 2007 [45] | supervised and unsupervised | intervention consisting of pedometer usage, counselling, and self-monitoring | 24 weeks (12 week intervention, 12 week maintenance) | monthly group sessions, daily walking | Individually tailored - step count 5% greater than participants baseline | counselling, goal setting, identifying strategies to increase step count | pedometer | step calendar, list of sample strategies to increase physical activity | list of walking strategies included outdoor mobility (e.g. talking dog for walks, walking with a friend) |
| Crotty 2002 [48] | supervised | gait, balance, functional tasks, general physical activity | individually tailored | individually tailored | individually tailored | goal setting | home risk assessment, modifications, mobility aids |
no | author confirmed outdoor mobility training included |
| de Roos 2018 [56] | supervised and unsupervised | incremental treadmill walking, cycling and extremity resistance exercise, education sessions, instructions to walk | 10 weeks | two times per week | 10 min incremental treadmill walking, cycling and resistance exercise Self-paced walking programme |
no | no | instructions on exercise compliance and the importance staying active | ≥30 min walking 1 day per week |
| Echeverria 2020 [44] | Supervised (hospital group session) and unsupervised (individual home program) | SGB: 6 weeks at hospital +18 weeks at home LGB: 12 weeks at hospital +12 weeks at home Group = strength, power, balance, walking Individual = Otago Program e.g. balance, strength, walks |
24 weeks | Hospital: 2 x 1 h per week Home: walk 15–60 min daily |
Strength training: weeks 1–3 40–50% 1RM, weeks 4 onwards 60–70% 1RM |
No | No | No | home component included 7 days of walking recommendations aimed at perform outdoor walking without assistance. |
| Hauer 2002 [38] | supervised | gait, balance and functional training, strength/resistance, general physical activity. | 3 months | 145 min 3 days/week |
70–0% max workload | no | no | no | author confirmed outdoor mobility training included |
|
Hughes 2004 [59] Hughes 2006 [62]* |
supervised | Fit and strong intervention: flexibility exercises, resistance training, walking, group discussion and education | 8 weeks | 90 min sessions, three times per week |
Individually tailored | goal setting and systematic feedback on progress made, identify strategies for self-efficacy adherence | no | Performance records shared with participants. Exercise log, The Arthritis helpbook, and health education. | outdoor walking |
| Iliffe 2014 [39] | supervised and unsupervised | a: Otago exercise and walking programme b: community centre postural stability instructor led exercise programme, Otago home exercise, and walking programme |
24 weeks | a: three times per week; and at least twice weekly walking b: one group exercise class, twice weekly home exercise; and at least twice weekly walking |
a: 30 min home exercise; walking 30 min at moderate pace b: 1 h group exercise, 30 min home exercise, walking 30 min moderate pace |
coping strategies to reduce risk of complications from a long lie after a fall. | a: ankle cuff weights | a and b: instruction booklet | walks encouraged 2 x 30 min weekly |
| Karlsson 2016 [47] | supervised | comprehensive geriatric assessment, gait, balance and functional training, strength/resistance, general physical activity, monitoring -pain, wound care, medication, nutrition. Intervention specified walking ability indoors and outdoors. | 10 weeks | initially daily home visits | na | no | home risk assessment, modifications, assistive devices |
no | walking indoors and outdoors with physiotherapist |
|
Kerr 2018 [17] Crist 2021 [61]* |
supervised and unsupervised | group walks led by staff and peer leaders from 6 weeks to 6 months, led by peer-leaders alone from 6 to 12 months. Goal setting for step count to achieve during group walks and independently. | 12 months | all participants encouraged to achieve a 3,000 step increase from baseline in first 12 weeks and maintain this for remainder of study. | four counselling phone calls in first 8 weeks to identify barriers and set goals. Goals achieved celebrated in group sessions. Progress charts of steps taken every two weeks for first 6 months. Weekly step logs. | pedometers | step counts for common locations around their area, and walking maps for their local community. Nine group education sessions led by research staff and peer-leaders for information e.g. local activity classes, safe walking tips, barriers and benefits of PA, goal setting, social support, disease specific recommendations. | encouraged to walk around community | |
| Kerse 2010 [43] | supervised and unsupervised | Otago exercise programme, progressive resistance training, progressive balance training, and walking programme | 6 months | three times per week; six visits in first 2 months, seventh at month, eighth at month 6 | walking 30 min; 60 min visits | calendars to record physical activity; functional goal setting; encouraged to identify a social companion for exercise | no | no | regular walking 3 x weekly and functional goal setting e.g. prune the roses |
| Lee 2007 [19] | supervised | Community-based walking intervention underpinned by self-efficacy theory delivered by a public health nurse | 6 months | individually tailored (median = 6) | NA | discuss ideas for overcoming perceived barriers, verbal encouragement; recognise interpretations of physiological and emotional responses to walking, identify performance accomplishments | pedometer | advise about regular walking and a walking log, shared practical information about pleasant walking routes and others experiences of success | community-based walking |
| Logan 2004 [54] | supervised | assessment of barriers to outdoor mobility, mobility goal setting and tailored interventions to achieve goals | up to 3 months | seven times | tailored | advice, encouragement, mobility goal setting, overcoming fear/apprehension by e.g. supervised mobility | walking aids, adaptations as needed | leaflets describing local mobility services, information on e.g. resuming driving, alternatives to cars and buses | intervention based on mobility goals e.g. getting public transport |
| Logan 2014 [18] | supervised | additional rehabilitation, exercise, practical activities, psychological interventions to improve confidence and targeted information; a treatment manual | 4 months | according to participants preference, maximum 12 visits | Individually tailored | goal planning, checklist of benefits and barriers of going outside, motivational and confidence-building strategies | Walking aids, referrals for additional equipment as needed | example of skills needed for outdoor mobility, case vignettes of treatment plans, personalised pack of local travel information | intervention based on mobility goals (e.g. long walk of >100 m), included a protocol for a first outing walking and practicing outdoor mobility |
| Magaziner 2019 [49] | supervised | gait, balance and functional training, strength/resistance, endurance | 4 months | 60 min every other day | Strength:3x8 repetitions at eight repetition max Endurance: 50% heart rate max or 3–5/10 perceived exertion | no | no | no | intervention specified outdoor ambulation (if able) on flat surface or up and down steps |
| Mangione 2005 [50] | supervised | group 1: strength/resistance, group 2: endurance | 3 months | 30–40 min x2/week month 1 and 2, then x1/week month 3 | Strength: eight repetition max Endurance: 65-75% heart rate max or 3–5/10 perceived exertion | no | no | no | intervention specified outdoor and indoor walking included in endurance training |
| Orwig 2011 [53] | supervised x3/week month 1 and 2, x2/week month 3 and 4, x1/1-2 weeks for remainder |
strength/resistance, endurance, flexibility, cognitive behavioural interventions | 12 months | strength x2/week 30 min aerobic x3/week |
Strength: 3 × 10 repetitions x 11 exercises TheraBand at individual level | motivational phone calls | no | no | author confirmed aerobic activity incorporated outdoor walking |
| Pfeiffer 2020 [21] | supervised (eight sessions) and unsupervised | cognitive behavioural interventions, gait, balance, and functional training, strength/resistance | 3 months | 30–60min ≥2/week | NA | no | home risk assessment, modifications | written exercise programme with photos and instructions or recorded instructions with music player, exercise diary | intervention targeting mobility-based goals example specifies travelling by bus using a wheeled walker |
| Pol 2019 [51] | supervised and unsupervised |
cognitive behavioural interventions, gait, balance and functional training | 3 months | 60 min/week coaching, on discharge: four phone calls over 10 weeks | NA | no | home risk assessment, modifications | information and education sessions on importance of physical activity | specified monitoring of outdoor physical activity; appendix describes case addressing poor outdoor mobility in goal setting |
| Resnick 2007 [52] | supervised | strength/resistance, endurance, flexibility | 12 months | Strength: x2/week Aerobic: 30 min x3/week |
NA | goal setting, group 2 + 3: verbal encouragement, removal of unpleasant sensations, cueing | no | group 2 + 3 booklet on exercise benefits after hip fracture | author confirmed aerobic activity incorporated outdoor walking |
| Vander Walde 2021 [58] | unsupervised | walking programme | tailored | from 3 days to 5 days/week | from 15 min to 30 min | walking diary | no | exercise workbook; information of exercise to improve fatigue during radiotherapy | encouraged 150 min walking per week |
| Varas 2018 [55] | supervised and unsupervised | exercise training and plan to increase physical activity level | 8 weeks | walking 5 days a week | walking for 30–60 min (incremental cycles of 15–20 min) at individualised predetermined speeds | weekly phone calls for encouragement, objective setting, analyse reasons of noncompliance | pedometer | activity diary to note gait and steps per day | walking programme |
| Voukelatos 2015 [42] Merom 2015 [63] * | unsupervised | walking programme: stage 1 -12 weeks focused on frequency and duration, stage 2 -12 weeks focused on intensity, and stage 3 -24 weeks of maintenance | 12 weeks | 3 times per week | 30 min | seven telephone coaching sessions at weeks 1, 3, 6, 12, 16, 24, and 36 walking diary |
encouraged to use a pedometer | walking manual sent by post at 0, 12 and 24 weeks with guidance for each stage | progressive walking intervention undertaken at participants preferred location |
| Ziden 2008 [46],2010 [64]* | supervised and unsupervised | general physical activity, cognitive behavioural interventions, involvement of family in discharge planning. Physiotherapy intervention focused on improving outdoor mobility. | 3 weeks | individually tailored | individually tailored | goal setting and motivation | no | no | physiotherapy intervention focussed on outdoor mobility |
*two articles from one RCT
Most RCTs included a walking programme as their outdoor mobility component including unsupervised walking programmes (n = 10) [16, 17, 38–40, 43, 44, 46, 47, 58], supervised walking programmes (n = 10) [18–20, 48–50, 52, 53, 56, 59] or a ‘community mastery’ session where negotiating grass, curbs and ramps were practiced (n = 1) [57]. The prescribed frequency ranged from walking as one option for exercise [38, 41] to 2- [20, 39, 50, 56], 3- [43, 52, 53, 59], 4- [49], 5- [55, 58] and 7-day walking per week [44]. The frequency was not specified for five RCTs [17, 40, 46, 47, 61].
Most contained one or more behaviour change components including action planning (n = 1) [57], tailored goal setting for outcomes (n =n = 6) [17, 21, 46–48, 54] or behaviours e.g. increasing activity (n = 4) [18, 40, 45, 51], behavioural contracts (n = 2) [16, 51], self-monitoring of behaviour (n = 10) [16, 19, 21, 39, 42, 43, 45, 55, 58, 59], feedback on behaviour (n = 8) [19, 21, 40, 41, 44, 47, 51, 59], monitoring outcomes of behaviour without feedback (n = 3) [40, 42, 48], prompts/cues e.g. at home visits/telephone follow-up (n = 8) [39, 42, 43, 46, 47, 52–55] and/or social support through group activities (n = 5) [17, 20, 41, 57, 59] or to enable mobility e.g. exercise/transport companion (n = 5) [19, 21, 43, 47, 54]. Five RCTs included instructions on how to perform the programme [17, 21, 39, 42, 54], while two RCTs provided information on health consequences [51, 57]. Five RCTs provided pedometers [17, 19, 42, 45, 55] and one walking aids [54]. One RCT restructured the physical environment to enable mobility by extending crosswalk times adding cues at intersections, clearing bridges and cutting back foliage [17].
Synthesis
Meta-analyses were completed for physical activity (total, moderate-vigorous), outdoor mobility, endurance and falls-related self-efficacy. Forest plots for all meta-analyses are available in Supplementary File 2. GRADE criteria are available in Table 4. Results from RCTs not included in meta-analyses are available in Supplementary File 3.
Table 4.
Outcomes in the proactive and reactive population according to grading of recommendations assessment, development and evaluation (GRADE)
| Proactive population | |||
|---|---|---|---|
| Outcomes | Hedge’s g (CI) | Number of participants (studies) | Quality of evidence (GRADE) |
| physical activity, intervention end |
0.13 (−0.04, 0.30) | 1,704 (5) | ⊕ ⊕ ⊝⊝ac Low |
| physical activity, 12- month follow-up |
0.00 (−0.12, 0.12) | 756 (2) | ⊕ ⊕ ⊕⊝d Moderate |
| falls-related self-efficacy intervention end | −0.03 (−0.11, 0.05) | 1,816 (3) | ⊕ ⊕ ⊕⊝e Moderate |
| falls-related self-efficacy 24-month follow-up |
0.63 (−0.16, 1.43) | 681 (2) | ⊕⊝⊝⊝abd Very low |
| Reactive population | |||
| Outcomes | Hedge’s g (CI) | Number of participants (studies) | Quality of evidence (GRADE) |
| physical activity, intervention end |
1.32 (0.31, 2.32) | 587 (7) | ⊕ ⊕ ⊝⊝af Low |
| physical activity, 12- month follow-up |
0.62 (0.44, 0.80) | 449 (5) | ⊕ ⊕ ⊝⊝af Low |
| endurance, intervention end | 0.24 (0.04, 0.44) | 392 (4) | ⊕ ⊕ ⊕⊝g Moderate |
| falls-related self-efficacy intervention end | 0.27 (−0.18, 0.71) | 429 (4) | ⊕⊝⊝⊝abg Very low |
| able to mobilise outdoor, intervention end* | 0.90 (−1.03, 2.82) | 285 (2) | ⊕⊝⊝⊝abg Very low |
| able to mobilise outdoor, final follow-up* |
0.18 (−0.38, 0.75) | 253 (2) | ⊕⊝⊝⊝abg Very low |
| satisfied with outdoor mobility, intervention end* | 0.66 (−0.28, 1.60) | 663 (2) | ⊕⊝⊝⊝abi Very low |
| satisfied with outdoor mobility, final follow-up* |
0.46 (−0.27, 1.19) | 600 (2) | ⊕⊝⊝⊝abi Very low |
*Log Odds Ratio (CI)
aInconsistency, I2 > 45%
bImprecision
cRisk of Bias: random sequence generation, allocation concealment, blinding of outcome assessor, blinding of participants and personnel
dRisk of Bias: blinding of outcome assessor, blinding of participants and personnel
eRisk of Bias: blinding of outcome assessor, allocation concealment, blinding of participants and personnel
fRisk of Bias: random sequence generation, allocation concealment, incomplete outcome data, blinding of outcome assessor, blinding of participants and personnel
gRisk of Bias: allocation concealment, blinding of outcome assessor, blinding of participants and personnel
iRisk of Bias: blinding of participants and personnel
CI: confidence interval.
GRADE Working Group grades of evidence
High quality ⊕ ⊕ ⊕⊕: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality ⊕ ⊕ ⊕⊝: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality ⊕ ⊕ ⊝⊝: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality ⊕⊝⊝⊝: We are very uncertain about the estimate.
Physical activity
There was no effect of rehabilitation interventions for proactive populations which incorporated outdoor mobility on total physical activity at intervention end (five RCTs with 1,704 participants. Hedge’s g 0.13, 95% CI: −0.04, 0.30. I2 = 69.69. GRADE: Low) [20, 39, 42, 45, 60] or 12-month follow-up (two RCTs with 756 participants. Hedge’s g 0.00, 95% CI: −0.12, 0.12. I2 = 0.00. GRADE: Moderate) [16, 39]. The findings are in keeping with two RCTs not included in the meta-analysis for intervention end [41, 44] and follow-up [44]. Four RCTs evaluated the effectiveness of rehabilitation interventions for proactive populations incorporating outdoor mobility on minutes spent in moderate-vigorous physical activity with inconsistent evidence for an effect [17, 39, 41, 44].
There was a large effect of rehabilitation interventions for reactive populations which incorporated outdoor mobility on total physical activity at intervention end (seven RCTs with 587 participants. Hedge’s g 1.32, 95% CI: 0.31, 2.32. I2 = 96.31. GRADE: Low) [21, 38, 43, 55, 56, 58, 59] and 12-month follow-up (five RCTs with 449 participants. Hedge’s g 0.62, 95% CI: 0.44, 0.80. I2 = 0.00. GRADE: Low) [38, 43, 52, 55, 59]. The finding is in keeping with two RCTs not included in the meta-analysis for intervention end [53] and follow-up [19, 53]. In contrast, Clemson et al. reported no difference in the change in physical activity as measured by the Physical Activity Scale for the Elderly from baseline to follow-up for intervention (mean difference (standard deviation (SD)): −13.48 (42.25)) versus control (mean change (SD): −4.40 (36.25)) (P = 0.06) [57]. No RCT targeting reactive populations evaluated moderate-vigorous physical activity.
Endurance
Echeverria et al. investigated the effect of rehabilitation interventions for proactive populations which incorporated outdoor mobility on walking endurance. They noted an increase in 6-min walk test distance for both intervention groups at intervention end (mean metres(m) (SD): short-term group baseline 324 m (135) intervention end 372 m (118); long-term group baseline 321 m (117) intervention end 383 m (110)) [44]. No difference in 6-min walk test distance was noted between intervention end and 24-week follow-up [44].
Rehabilitation interventions for reactive populations which incorporated outdoor mobility had a small effect on walking endurance at intervention end (four RCTs with 392 participants. Hedges g 0.24; 95% CI: 0.04, 0.44, I2 = 0.00. GRADE: Moderate) [49, 50]. The finding is in keeping with one RCT not included in the meta-analysis for intervention end and follow-up [55]. In contrast, Hughes et al. [62] noted no between-group difference in 6-min walk test distance at 12-month follow-up (mean metres (SD): intervention 1281.53(502.93), control 1106.53(484.10)).
Outdoor mobility
Crist et al. [61] assessed the effect of a 12-month rehabilitation intervention for a proactive population incorporating outdoor mobility on the time spent walking (as a proportion of total time) in four mutually exclusive domains—home, campus, neighbourhood and beyond neighbourhood. Baseline mean (standard deviation) total walking time in minutes/day was 83.8 (45.4) for the intervention and 72.7(48.0) for the control group [61]. The intervention group increased daily walking from baseline to 3 months by 21.48 min/day (95% confidence interval (CI) 12.0, 31.0), while the control group saw no change in walk time (data not provided) [61]. The intervention increase was observed for non-home domains at 3 months (linear regression coefficient = 11.48, 95% CI: 1.7, 21.3), which was sustained over 12 months [61]. In contrast, Bae et al. [41] noted no between-group difference in the change in number of times participants went outdoors per day at the end of their 24-week intervention (P = 0.18).
Two RCTs showed a moderate effect which failed to reach statistical significance of rehabilitation interventions for reactive populations which incorporated outdoor mobility on satisfaction with outdoor mobility at intervention end (two RCTs with 663 participants. Log Odds-Ratio 0.69, 95% CI: −0.18, 1.57. I2 = 81.44. GRADE: Very low) and 10–12-month follow-up (two RCTs with 600 participants. Log Odds-Ratio 0.48, 95% CI: −0.22, 1.18. I2 = 70.41. GRADE: Very low) [18, 54]. Two RCTs showed a large effect which failed to reach statistical significance of rehabilitation interventions for reactive populations which incorporated outdoor mobility on ability to mobilise outdoors at intervention end (two RCTs with 285 participants. Log Odds-Ratio 0.90, 95% CI: −1.03, 2.82. I2 = 91.42. GRADE: Very low) and a small effect which failed to reach statistical significance at 12-month follow-up (2 RCTs with 253 participants. Log Odds-Ratio 0.18, 95% CI: −0.38, 0.75. I2 = 8.04. GRADE: Very low) [46, 47].
Logan et al. [54] 2004 noted a higher proportion of participants got out of the house as much as they wanted for the intervention when compared with the control group at 4-month (rate ratio 1.72, 95% CI 1.25 to 2.37) and 10-month follow-up (rate ratio 1.74, 95% CI 1.24 to 2.44) (baseline count(%): intervention 24(28), control 32(39)). Similar effects were noted for Logan 2014 where the intervention group were more likely to make a journey outdoors than the control group at 6-month (rate ratio 1.42, 95% CI 1.14 to 1.67) and 12-month follow-up (rate ratio 1.76, 95% CI 1.36 to 1.95) (baseline count(%) for getting out of house as much as wanted: intervention 18(6.3), control 20(7.1)) [18].
Falls-related self-efficacy
There was no effect of rehabilitation interventions for proactive populations which incorporated outdoor mobility on falls-related self-efficacy at intervention end (three RCTs with 1,816 participants. Hedge’s g − 0.03 95% CI: −0.11, 0.05. I2 = 0.00. GRADE: Moderate) [39, 42, 60] Two rehabilitation interventions had a moderate effect but it failed to reach statistical significance at 24-month follow-up (two RCTs with 681 participants. Hedge’s g 0.63 95% CI: −0.16, 1.43. I2 = 96.66. GRADE: Very low) [16, 39]. The findings are in keeping with two RCTs not included in the meta-analysis for intervention end [63] and follow-up [40].
There was a small effect which failed to reach statistical significance of rehabilitation intervention for reactive populations which incorporated outdoor mobility on falls-related self-efficacy at intervention end (four RCTs with 429 participants. Hedge’s g 0.27 95% CI: −0.18, 0.71. I2 = 84.50. GRADE: Very low) [21, 46, 48, 52]. The absence of an effect is in keeping with two RCTs not included in the meta-analysis [51, 57]. Two RCTs reported conflicting evidence for an effect on falls-related self-efficacy at follow-up [51, 64].
Discussion
Summary of evidence
We identified 33 articles for 28 RCTs. Rehabilitation interventions for reactive populations which incorporated an outdoor mobility component improved physical activity, outdoor mobility and endurance at intervention end and final follow-up compared with usual care. No effect was noted for rehabilitation interventions for proactive populations which incorporated an outdoor mobility component on total physical activity, or endurance or falls-related self-efficacy. The confidence in effect estimates from meta-analysis ranged from moderate to very low due to concerns with risk of bias, inconsistency and imprecision. Evidence from one RCT indicated a potential benefit of rehabilitation interventions for proactive populations which incorporated an outdoor mobility component on minutes spent in moderate to vigorous activity at intervention end, and outdoor mobility at intervention end and follow-up, versus control.
Interpretation
Rehabilitation interventions for reactive populations which incorporate outdoor mobility saw a large effect on physical activity at intervention end with a moderate effect sustained at 12-month follow-up. The quality of the evidence was low indicating further research is required to replicate the results. All interventions which saw a beneficial effect on outcomes compared with control groups (88%) included a walking programme. Walking was recently reported as older adults preferred exercise [9]. The structure of programmes varied across RCTs from unsupervised to supervised, and with target frequencies of optional [38, 41] to 7-days a week [44]. The interventions by Kerse and Varas incorporated explicit prescription of walking 3–5 days per week for 30-min and demonstrated large effects on physical activity at the end of the intervention and 12-month follow-up [43, 55]. The review results suggest a walking programme may be a key component of community-rehabilitation with a dose–response relationship.
Walking programmes may also be beneficial for rehabilitation programmes for proactive populations. For proactive populations, Crist et al. [61] noted an increase in the time the intervention group spent walking outside their home on completion of a walking programme compared with the control group which was sustained at 12-months. The walking programme included walking maps for the local area and targeted change at the individual, interpersonal and community levels with both individual and group walks prescribed [61]. Arija et al. [20] saw a beneficial effect of their intervention on physical activity at intervention end versus control. Their intervention group received walking itineraries and attended a monthly sociocultural activity including visits to museums and libraries, cultural exhibitions, tourist attractions and dance lessons [20]. These RCTs suggest a possible interaction between walking programme and social intervention components on physical activity and outdoor mobility outcomes adding weight to the potential benefit of integrated care for community-dwelling older adults [65].
Most RCTs identified by the current review operationalised their outdoor mobility intervention component as a walking programme, with few including assistive devices or transport. For the RCTs by Logan et al. [18, 54], the intervention targeted a broader definition of outdoor mobility which included walking, use of assistive devices (walking aids, mobility scooters), resuming driving and taking a taxi or public transport. Participants were supported by up to seven [54] or 12 [18] sessions with an occupational therapist to build confidence during practice of outdoor mobility. From the meta-analyses in the current review, Logan’s interventions may lead to greater satisfaction with outdoor mobility at intervention end and 12-month follow-up, but the confidence interval did not exclude the potential for a small loss in satisfaction and the quality of the evidence was graded as very low indicating uncertainty in the estimate. Further, compared with the control group, participants in the intervention groups took more outdoor journeys [54] and were more likely to make an outdoor journey [18] at intervention end and 10–12-month follow-up. These interventions were evaluated among older adults post-stroke who may face different physical, psychological and cognitive barriers to outdoor mobility compared with other patient groups [66]. Similar interventions in different target groups are warranted to determine their effectiveness in supporting older adults to achieve the World Health Organisation’s definition of functional ability as ‘all the health-related attributes that enable people to be and to do what they have reason to value’ [67].
For the current review, most interventions incorporated a behaviour change technique. Evidence from an umbrella review suggests that behaviour change techniques are effective at improving physical activity among community-dwelling older adults [68]. This also applies to rehabilitation interventions for reactive populations where behaviour change techniques were more effective at improving real-world walking habits after stroke than exercise alone [69]. However, for the current review no intervention included a component explicitly targeting anxiety related to outdoor mobility or fear of falling. This might explain why there was no effect of interventions on falls-related self-efficacy for either proactive or reactive populations. Given that fear of falling is negatively associated with outdoor mobility behaviour [13, 63] future RCTs should include an intervention component to explicitly target improvements in falls-related self-efficacy [70, 71].
Limitations
First, we searched five electronic databases; however, we excluded protocols, pilot/feasibility RCTs, non-randomized trials, which may have underestimated the extent of relevant evidence. Second, we excluded conference proceedings and those not published in English which may have introduced publication bias. Third, we included community-based RCTs of older adults irrespective of target population. We also employed a broad definition of ‘outdoor mobility’ ranging from supervised outdoor walking to goal setting. We employed random-effects meta-analysis to account for expected variation between populations and interventions and stratified meta-analyses by proactive/reactive populations. Despite this, we noted heterogeneity for some analyses which contributed to the very low to moderate grading of recommendations limiting the generalisability of the review findings. We did not explore this heterogeneity further e.g. by different types of interventions or outcome measures due to the small number of RCTs in each meta-analysis [35].
Conclusions
Rehabilitation interventions for reactive populations which incorporated an outdoor mobility component led to sustained improvements in physical activity, outdoor mobility and endurance among older adults. In most RCTs the outdoor mobility component comprised a walking programme and was accompanied by behaviour change techniques. These intervention components may be considered for community-based reactive rehabilitation for older adults who wish to increase their outdoor mobility. The quality of the evidence ranged from very low to moderate and should be replicated in future research. Future research should also seek to confirm/refute the benefit of a walking programme for proactive populations observed in RCTs not incorporated in meta-analysis of the current review. Further, no improvements in falls-related self-efficacy were noted across RCTs which may relate to the absence of intervention components directly addressing mobility-related anxiety. This should also be addressed by future research.
Supplementary Material
Contributor Information
Olyvia Geohagen, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Lydia Hamer, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Alexandra Lowton, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Stefanny Guerra, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Rhian Milton-Cole, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Pippa Ellery, Cornwall Partnership NHS Foundation Trust, UK.
Finbarr C Martin, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Sallie E Lamb, Institute of Health Research, University of Exeter, UK.
Catherine Sackley, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK; Faculty of Medicine and Health Sciences, University of Nottingham, UK.
Katie J Sheehan, Department of Population Health Sciences, School of Population and Environmental Sciences, Kings College London, UK.
Declaration of Conflicts of Interest
K.S. received funding from the NIHR Research for Patient Benefit, the Chartered Society of Physiotherapy Charitable Trust and UKRI Future Leaders Fellowship for hip fracture health services research. K.S. is current Lead of the International Fragility Fracture Network’s Hip Fracture Recovery Research Special Interest Group. C.S. received funding from the National Institutes of Health Research and Dunhill Medical Trust for research not related to this study.
Declaration of Sources of Funding
None.
References
- 1. Tuna HD, et al. Effect of age and physical activity level on functional fitness in older adults. European Review of Aging and Physical Activity 2009; 6: 99–106. [Google Scholar]
- 2. Mollenkopf H, Marcellini F, Ruoppila I, Flaschenträger P, Gagliardi C, Spazzafumo L. Outdoor mobility and social relationships of elderly people. Arch Gerontol Geriatr 1997; 24: 295–310. [DOI] [PubMed] [Google Scholar]
- 3. Jacobs JM, Cohen A, Hammerman-Rozenberg R, Azoulay D, Maaravi Y, Stessman J. Going outdoors daily predicts long-term functional and health benefits among ambulatory older people. J Aging Health 2008; 20: 259–72. [DOI] [PubMed] [Google Scholar]
- 4. Hajek A, Brettschneider C, Lange Cet al. Longitudinal predictors of institutionalization in old age. PLoS One 2015; 10: e0144203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Inoue K, Shona T, Matsumoto M. Absence of outdoor activity and mortality risk in older adults living at home. J Aging Phys Act 2006; 14: 203–11. [DOI] [PubMed] [Google Scholar]
- 6. Ganguli M, Fox A, Gilby J, Belle S. Characteristics of rural homebound older adults: a community-based study. J Am Geriatr Soc 1996; 44: 363–70. [DOI] [PubMed] [Google Scholar]
- 7. Eronen J, von Bonsdorff MB, Törmäkangas Tet al. Barriers to outdoor physical activity and unmet physical activity need in older adults. Prev Med 2014; 67: 106–11. [DOI] [PubMed] [Google Scholar]
- 8. Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med 2009; 150: 372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smith AR, Chen C, Clarke P, Gallagher NA. Trajectories of outdoor mobility in vulnerable community-dwelling elderly: the role of individual and environmental factors. J Aging Health 2016; 28: 796–811. [DOI] [PubMed] [Google Scholar]
- 10. Rantanen T. Promoting mobility in older people. J Prev Med Public Health 2013; 46: S50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bergland A, Thorsen K, Loland N. The relationship between coping, self-esteem and health on outdoor walking ability among older adults in Norway. Ageing & Society 2010; 30: 949–63. [Google Scholar]
- 12. De Silva NA, Gregory MA, Venkateshan SS, Verschoor CP, Kuspinar A. Examining the association between life-space mobility and cognitive function in older adults: a systematic review. J Aging Res 2019; 2019: 3923574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rantakokko M, Mänty M, Iwarsson Set al. Fear of moving outdoors and development of outdoor walking difficulty in older people. J Am Geriatr Soc 2009; 57: 634–40. [DOI] [PubMed] [Google Scholar]
- 14. Portegijs E, Keskinen KE, Eronen J, Saajanaho M, Rantakokko M, Rantanen T. Older Adults' physical activity and the relevance of distances to Neighborhood destinations and barriers to outdoor mobility. Front Public Health 2020; 8: 335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Saletti-Cuesta L, Tutton E, Langstaff D, Willett K. Understanding informal carers' experiences of caring for older people with a hip fracture: a systematic review of qualitative studies. Disabil Rehabil 2018; 40: 740–50. [DOI] [PubMed] [Google Scholar]
- 16. Tuvemo Johnson S, Anens E, Johansson AC, Hellström K. The Otago exercise program with or without motivational interviewing for community-dwelling older adults: a 12-month follow-up of a randomized. Controlled Trial J Appl Gerontol 2021; 40: 289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kerr J, Rosenberg D, Millstein RAet al. Cluster randomized controlled trial of a multilevel physical activity intervention for older adults. Int J Behav Nutr Phys Act 2018; 15: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Logan PA, Armstrong S, Avery TJet al. Rehabilitation aimed at improving outdoor mobility for people after stroke: a multicentre randomised controlled study (the getting out of the house study). Health Technol Assess 2014; 18p. vii-viii: 1–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee LL, Arthur A, Avis M. Evaluating a community-based walking intervention for hypertensive older people in Taiwan: a randomized controlled trial. Prev Med 2007; 44: 160–6. [DOI] [PubMed] [Google Scholar]
- 20. Arija V, Villalobos F, Pedret Ret al. Effectiveness of a physical activity program on cardiovascular disease risk in adult primary health-care users: the "pas-a-pas" community intervention trial. BMC Public Health 2017; 17: 576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pfeiffer K, Kampe K, Klenk Jet al. Effects of an intervention to reduce fear of falling and increase physical activity during hip and pelvic fracture rehabilitation. Age Ageing 2020; 49: 771–8. [DOI] [PubMed] [Google Scholar]
- 22. Liberati A, Altman DG, Tetzlaff Jet al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. International Register of Systematic Reviews (PROSPERO). https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=264082 (13 December 2021, date last accessed).
- 24. World Health Organisation . Rehabilitation in Health Systems. http://apps.who.int/iris/bitstream/handle/10665/254506/9789241549974-eng.pdf;jsessionid=18DF8F518ED956AA5FF9D8772E365298?sequence=1 (13 December 2021, date last accessed).
- 25. Crotty M, Unroe K, Cameron IDet al. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev 2010; 1: CD007624. [DOI] [PubMed] [Google Scholar]
- 26. Young C, Hall AM, Gonçalves-Bradley DCet al. Home or foster home care versus institutional long-term care for functionally dependent older people. Cochrane Database Syst Rev 2017; 2017: CD009844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Noone C, McSharry J, Smalle Met al. Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database Syst Rev 2020; 2020: CD013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Garrison SR, Kolber MR, Korownyk CSet al. Blood pressure targets for hypertension in older adults. Cochrane Database Syst Rev 2017; 2017: CD011575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barclay RE, Stevenson TJ, Poluha Wet al. Interventions for improving community ambulation in individuals with stroke. Cochrane Database Syst Rev 2015; 3: CD010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Smith TO, Gilbert AW, Sreekanta Aet al. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database Syst Rev 2020; 2: CD010569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org. [Accessed on 13/12/2021]. [Google Scholar]
- 32. Higgins JP, Altman DG, Gotzsche PCet al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lamb SE, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011; 12: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Higgins JPT, et al. , Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). www.training.cochrane.org/handbook (13 December 2021, date last accessed).
- 36. StataCorp . Stata Statistical Software: Release 16 S. LLC, Editor, 2019; College Station, TX.
- 37. Guyatt G, Oxman AD, Akl EAet al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64: 383–94. [DOI] [PubMed] [Google Scholar]
- 38. Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing 2002; 31: 49–57. [DOI] [PubMed] [Google Scholar]
- 39. Iliffe S, Kendrick D, Morris Ret al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess 2014; 18vii-xxvii: 1–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Boongird C, Keesukphan P, Phiphadthakusolkul S, Rattanasiri SA. Effects of a simple home-based exercise program on fall prevention in older adults: a 12-month primary care setting, randomized controlled trial. Geriatr Gerontol Int 2017; 17: 2157–63. [DOI] [PubMed] [Google Scholar]
- 41. Bae S, Lee S, Lee Set al. The effect of a multicomponent intervention to promote community activity on cognitive function in older adults with mild cognitive impairment: a randomized controlled trial. Complement Ther Med 2019; 42: 164–9. [DOI] [PubMed] [Google Scholar]
- 42. Voukelatos A, Merom D, Sherrington C, Rissel C, Cumming RG, Lord SR. The impact of a home-based walking programme on falls in older people: the easy steps randomised controlled trial. Age Ageing 2015; 44: 377–83. [DOI] [PubMed] [Google Scholar]
- 43. Kerse N, Hayman KJ, Moyes SAet al. Home-based activity program for older people with depressive symptoms: DeLLITE–a randomized controlled trial. Ann Fam Med 2010; 8: 214–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Echeverria I, Amasene M, Urquiza Met al. Multicomponent physical exercise in older adults after hospitalization: a randomized controlled trial comparing short- vs. long-term group-based interventions. Int J Environ Res Public Health 2020; 17: 666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Croteau KA, Richeson NE, Farmer BC, Jones DB. Effect of a pedometer-based intervention on daily step counts of community-dwelling older adults. Res Q Exerc Sport 2007; 78: 401–6. [DOI] [PubMed] [Google Scholar]
- 46. Ziden L, Frandin K, Kreuter M. Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. Clin Rehabil 2008; 22: 1019–33. [DOI] [PubMed] [Google Scholar]
- 47. Karlsson A, Berggren M, Gustafson Y, Olofsson B, Lindelöf N, Stenvall M. Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial. J Am Med Dir Assoc 2016; 17: 464.e9–15. [DOI] [PubMed] [Google Scholar]
- 48. Crotty M, Whitehead CH, Gray S, Finucane PM. Early discharge and home rehabilitation after hip fracture achieves functional improvements: a randomized controlled trial. Clin Rehabil 2002; 16: 406–13. [DOI] [PubMed] [Google Scholar]
- 49. Magaziner J, Mangione KK, Orwig Det al. Effect of a multicomponent home-based physical therapy intervention on ambulation after hip fracture in older adults: the CAP randomized clinical trial. JAMA 2019; 322: 946–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mangione KK, Craik RL, Tomlinson SS, Palombaro KM. Can elderly patients who have had a hip fracture perform moderate- to high-intensity exercise at home? Phys Ther 2005; 85: 727–39. [PubMed] [Google Scholar]
- 51. Pol MC, Riet G, Hartingsveldt M, Kröse B, Buurman BM. Effectiveness of sensor monitoring in a rehabilitation programme for older patients after hip fracture: a three-arm stepped wedge randomised trial. Age Ageing 2019; 48: 650–7. [DOI] [PubMed] [Google Scholar]
- 52. Resnick B, OrwigD Y-YJet al. Testing the effectiveness of the exercise plus programin older women post-hip fracture. Ann Behav Med 2007; 34: 67–76. [DOI] [PubMed] [Google Scholar]
- 53. Orwig DL, Hochberg M, Yu-Yahiro Jet al. Delivery and outcomes of a yearlong home exercise program after hip fracture: a randomized controlled trial. Arch Intern Med 2011; 171: 323–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Logan PA, Gladman JRF, Avery A, Walker MF, Dyas J, Groom L. Randomised controlled trial of an occupational therapy intervention to increase outdoor mobility after stroke. BMJ 2004; 329: 1372–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Varas AB, Córdoba S, Rodríguez-Andonaegui I, Rueda MR, García-Juez S, Vilaró J. Effectiveness of a community-based exercise training programme to increase physical activity level in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Physiother Res Int 2018; 23: e1740. [DOI] [PubMed] [Google Scholar]
- 56. Roos P, Lucas C, Strijbos JH, Trijffel E. Effectiveness of a combined exercise training and home-based walking programme on physical activity compared with standard medical care in moderate COPD: a randomised controlled trial. Physiotherapy 2018; 104: 116–21. [DOI] [PubMed] [Google Scholar]
- 57. Clemson L, Cumming RG, Kendig H, Swann M, Heard R, Taylor K. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc 2004; 52: 1487–94. [DOI] [PubMed] [Google Scholar]
- 58. VanderWalde NA, Martin MY, Kocak Met al. Randomized phase II study of a home-based walking intervention for radiation-related fatigue among older patients with breast cancer. J Geriatr Oncol 2021; 12: 227–34. [DOI] [PubMed] [Google Scholar]
- 59. Hughes SL, Seymour RB, Campbell R, Pollak N, Huber G, Sharma L. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist 2004; 44: 217–28. [DOI] [PubMed] [Google Scholar]
- 60. Arkkukangas M, Johnson ST, Hellström K, Anens E, Tonkonogi M, Larsson U. Fall prevention exercises with or without behavior change support for community-dwelling older adults: a two-year follow-up of a randomized controlled trial. J Aging Phys Act 2019; 28: 34–41. [DOI] [PubMed] [Google Scholar]
- 61. Crist K, Jankowska MM, Schipperijn Jet al. Change in GPS assessed walking locations following a cluster-randomized controlled physical activity trial in older adults, results from the MIPARC trial. Health Place 2021; 69: 102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hughes SL, Seymour RB, Campbell RTet al. Long-term impact of fit and strong! On older adults with osteoarthritis. Gerontologist 2006; 46: 801–14. [DOI] [PubMed] [Google Scholar]
- 63. Merom D, Gebel K, Fahey Pet al. Neighborhood walkability, fear and risk of falling and response to walking promotion: the easy steps to health 12-month randomized controlled trial. Prev Med Rep 2015; 2: 704–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ziden L, Kreuter M, Frandin K. Long-term effects of home rehabilitation after hip fracture - 1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disabil Rehabil 2010; 32: 18–32. [DOI] [PubMed] [Google Scholar]
- 65. Goodwin N. Understanding integrated care. Int J Integr Care 2016; 16: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Daniela Kahlert NE. Out-of-home mobility and social participation of older people: a photo-based ambulatory assessment study. Journal of Population Ageing 2020; 13: 547–60. [Google Scholar]
- 67. World Health Organisation . World Report on Ageing and Health. https://apps.who.int/iris/handle/10665/186463 (13 December 2021, date last accessed).
- 68. Zubala A, MacGillivray S, Frost Het al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLoS One 2017; 12: e0180902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Stretton CM, Mudge S, Kayes NM, McPherson KM. Interventions to improve real-world walking after stroke: a systematic review and meta-analysis. Clin Rehabil 2017; 31: 310–8. [DOI] [PubMed] [Google Scholar]
- 70. Kruisbrink M, Crutzen R, Kempen GIJMet al. Disentangling interventions to reduce fear of falling in communitydwelling older people: a systematic review and meta-analysis of intervention components. Disabil Rehabil 2021; 1–11. [DOI] [PubMed] [Google Scholar]
- 71. Weber M, Schnorr T, Morat M, Morat T, Donath L. Effects of mind-body interventions involving meditative movements on quality of life, depressive symptoms, fear of falling nd sleep quality in older adults: a systematic review with meta-analysis. Int J Environ Res Public Health 2020; 17: 6556. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


