Abstract
Cancer is characterized by increased oxidative stress, an imbalance between reactive oxygen species (ROS) and antioxidants. Enhanced ROS accumulation, as a result of metabolic disturbances and signaling aberrations, can promote carcinogenesis and malignant progression by inducing gene mutations and activating pro-oncogenic signaling, providing a possible rationale for targeting oxidative stress in cancer treatment. While numerous antioxidants have demonstrated therapeutic potential, their clinical efficacy in cancer remains unproven. Here, we review the rationale for, and recent advances in, pre-clinical and clinical research on antioxidant therapy in cancer, including targeting ROS with nonenzymatic antioxidants, such as NRF2 activators, vitamins, N-acetylcysteine and GSH esters, or targeting ROS with enzymatic antioxidants, such as NOX inhibitors and SOD mimics. In addition, we will offer insights into prospective therapeutic options for improving the effectiveness of antioxidant therapy, which may expand its applications in clinical cancer treatment.
Keywords: reactive oxygen species, oxidative stress, antioxidants, cancer therapy
1. Introduction
Redox homeostasis is essential for biological function and its disturbance leads to profound pathophysiological consequences in cells, which emphasize the balance between the relative abundance of reactive oxygen species (ROS) and antioxidants [1,2,3]. However, cells may generate excessive ROS as an unavoidable result of alterations in metabolic signaling pathways [4,5]. Oxidative stress arises when ROS are excessively produced, while antioxidants are relatively insufficient. The ROS levels are tightly regulated by antioxidant systems, including enzymatic antioxidant and nonenzymatic antioxidant systems. To accommodate oxidative stress, cells modify metabolic and genetic reprogramming, thereby leading to increased production of NADPH, glutathione (GSH, l-γ-glutamyl-l-cysteinyl-glycine), superoxide dismutases (SODs) and thioredoxins (TRXs), returning ROS to homeostatic levels [6,7,8].
When the high ROS level exceeds non-toxic doses, ROS may cause oxidative damage to macromolecules, such as nucleic acids, proteins, lipids and glucose, resulting in fragmentation of enzymes and structural proteins, membrane damage, gene mutations and even pro-oncogenic signaling activation [9,10]. Increased oxidative stress can initiate tumor development and contribute to tumor progression by directly oxidizing macromolecules or oxidative stress-caused aberrant redox signaling [11], demonstrating that high ROS levels may increase the risk of cancer when antioxidant systems are insufficient to protect cells from oxidative stress. Since oxidative stress plays an important role in carcinogenesis and cancer progression [2,12,13], it is an attractive idea to use antioxidants for the treatment of cancer. Numerous antioxidants were developed in the past few decades. They can be classified as nonenzymatic antioxidants, such as NF-E2 p45-related factor 2 (NRF2) activators [14], vitamins [15], N-acetylcysteine (NAC) and GSH esters [16,17], and enzymatic antioxidants, such as NADPH oxidase (NOX) inhibitors [18] and SOD mimics [19]. Some of them have shown potential to act as anticancer drugs and multiple antioxidant therapeutic strategies were explored in pre-clinical and clinical research [20].
In this review, we will summarize redox homeostasis mechanisms and the relationship between oxidative stress and cancer, providing a detailed description of the rationale for, and recent advances in, antioxidant therapy in cancer. In addition, we also highlight several kinds of antioxidant drugs in pre-clinical and clinical trials, discussing the promise and limitations of antioxidant therapeutic strategies in cancer.
2. Redox Homeostasis: The Biological Basis for Antioxidant Therapy
ROS are a class of highly reactive free radicals, such as hydroxyl radical (•OH), the superoxide radical (O2•−) and hydrogen peroxide (H2O2) [21,22]. The high intracellular ROS level-induced oxidative stress leads to the upregulation of antioxidant capacity to maintain redox homeostasis by metabolic rerouting or activation of genetic programs [23,24]. Disruption of redox homeostasis contributes to multiple human diseases, including cancer, and resetting redox homeostasis with antioxidants is a promising strategy to prevent tumorigenesis or inhibit cancer progression. It is well known that redox homeostasis is balanced by the equilibrium of ROS generation and ROS elimination. Therefore, we first describe the underlying mechanisms that regulate the cellular redox homeostasis (Figure 1).
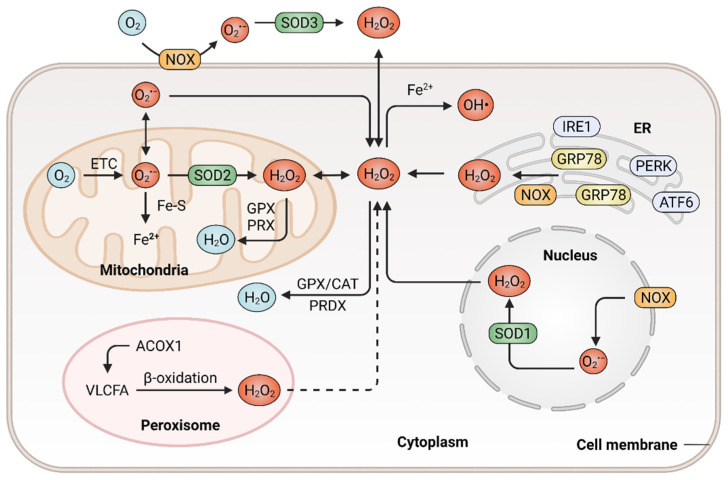
Figure 1.
Generation and elimination of ROS in mammalian cells. ROS are generated extracellularly by NADPH oxidase (NOX) or intracellularly in different subcellular compartments, including endoplasmic reticulum (ER), peroxisome, nucleus as well as the mitochondrial electron transport chain (ETC). Antioxidant systems include the peroxiredoxin (PRDX), the glutathione peroxidase (GPX) and catalase (CAT) in the cytosol or mitochondria, which hydrolyze H2O2 to H2O.
2.1. Mechanisms in ROS Generation
ROS are prominently generated by transmembrane NOXs and other various oxidases from the mitochondrial electron transport chain (ETC) [25], endoplasmic reticulum (ER) [26] and peroxisomes [27], in response to intracellular signaling and extracellular stimuli. The mitochondrion functions as a highly dynamic organelle and an essential endogenous enzymatic source of ROS, which generates ROS through ETC, a series of electron transfer complexes located on the mitochondrial inner membrane [28,29]. The production of mitochondrial ROS is associated with the metabolism of glucose, fatty acids and amino acids (via glycolysis, β-oxidation and oxidative deamination, respectively), which provide precursors for tricarboxylic acid (TCA) cycle to produce metabolic substrates that enter the ETC [30,31]. In the mitochondrial ETC, ROS generation is probably due to the leak of electrons from complex I, II and III. During this process, oxygen is reduced with a single electron and thus generating O2•−, which can be dismutated to H2O2 [32,33]. The rate of ROS generation from the mitochondrial ETC is predominantly dependent on the concentration of the one-electron donor and the reaction rate between the donor and oxygen. The primary function of NOXs is to produce ROS, which is triggered by a variety of factors and reported to be associated with tumor development [34]. The NOX family consists of seven members, namely NOX1, NOX2, NOX3, NOX4, NOX5, DUOX1 and DUOX2 [35]. They catalyze the conversion of oxygen to O2•− by transferring electrons to molecular oxygen in various subcellular compartments, such as the nucleus [36]. NOXs-derived ROS might activate the downstream secondary oxidase systems, such as xanthine oxidase and uncoupled endothelial nitric oxide synthase, further aggravating oxidative stress and accelerating the development of cancer [37]. ER is a protein-folding factory, which plays an important role in normal physiology [38,39]. The oxidizing site in ER supports the proper conformation and post-translational modifications of nascent proteins [40]. In response to the aggregation of unfolded or misfolded proteins within ER, glucose-regulated protein 78 (GRP78) dissociates from ER stress receptors, such as activating transcription factor 6 (ATF6), pancreatic ER kinase (PKR)-like ER kinase (PERK) and inositol-requiring enzyme 1 (IRE1), leading to ER stress and eventually resulting in ROS accumulation [41,42,43]. In addition, the release of calcium from the ER and depolarization of the mitochondrial inner membrane can stimulate the production of mitochondrial ROS and mediate excessive oxidative stress [44,45]. As multifunctional dynamic organelles, peroxisomes exist in almost all eukaryotic cells and play essential roles in redox homeostasis [46,47]. The name of peroxisomes derives from their function in the metabolism of H2O2 [27]. Peroxisomal respiration accounts for approximately 20% of total oxygen consumption and produces up to 35% of total H2O2 by peroxisomal oxidases in certain mammalian cells [48]. For instance, peroxisomal oxidase acyl-CoA oxidase 1 (ACOX1), the rate-limiting enzyme in fatty acid β-oxidation, can oxidize very long-chain fatty acid (VLCFA) and lead to H2O2 production in peroxisomes. In addition, a gain-of-function mutation in ACOX1 may further enhance the ROS levels [49]. Besides, the ACOX1-induction of ROS production was demonstrated to be involved in oxidative DNA damage and the progression of hepatocellular carcinoma (HCC) [50]. Ultraviolet (UV) radiation is also an important factor that contributes to ROS generation and subsequent carcinogenesis [51]. Cells exhibit an increased production of ROS when exposed to UV radiation. UV-induced transition-type mutations at dipyrimidine sites frequently occur in the RAS oncogene and p53 tumor suppressor gene [52]. In addition, a wide range of biological phenomena, such as inflammatory and oxidative modifications of macromolecules, were reported to participate in UV-induced skin carcinogenesis and the progression of glioblastoma [53,54].
2.2. ROS Elimination with Enzymatic or Nonenzymatic Antioxidant System
Increased accumulation of ROS can be eliminated by various enzymatic antioxidant systems including SODs [55], GSH peroxidases (GPXs) [56], peroxiredoxins (PRDXs) [57], paraoxonase (PONs) and catalase (CAT) [58]. Additionally, ROS can also be eliminated by nonenzymatic antioxidant systems, such as GSH [59] and TRXs [60]. The antioxidant systems counteract ROS-mediated damage to maintain ROS homeostasis, enabling tumor cell survival [20].
The enzymatic antioxidant system mainly consists of SODs, PRDXs, CAT, PONs and GPXs. Under oxidative stress, these antioxidant enzymes are upregulated or activated to prevent oxidative damage. SODs catalyze the conversion of O2•− into molecular oxygen and H2O2, thus controlling the levels of ROS and limiting their potential toxicity [61]. Since SOD1 was firstly discovered in 1969, all of the three members in the SOD family were biochemically and molecularly characterized in mammalian cells, including Cu/Zn-SOD (SOD1), Mn-SOD (SOD2) and EC-SOD (SOD3) [62]. SOD1 and SOD2 localize in cytosol, the mitochondrial inter membrane space, the nucleus and the mitochondrial matrix, while SOD3 is secreted into the extracellular space [63,64,65]. The SOD family constitutes the first line of defense against ROS. The O2•− is dismutated by SODs to form H2O2, which can be decomposed into O2 and H2O by CAT or GPXs [66]. Several enzymes, such as glutathione reductase and glucose-6-phosphate dehydrogenase, function as secondary antioxidant enzymes that enable GPX to function with cofactors (NADPH, GSH and glucose 6-phosphate) but not to act on ROS directly [67,68]. PON2 is one member of the PON family that consists of three members, namely PON1, PON2 and PON3. PON2 is a membrane-associated protein that is located in the plasma membrane, mitochondria and ER [69]. It was reported that PON2 protects against oxidative stress, both in vivo and in vitro [70,71]. For instance, PON2 binds with high affinity to coenzyme Q10 and protects against mitochondrial dysfunction when localized to the mitochondria, while PON2 deficiency results in mitochondrial oxidative stress [72].
Nonenzymatic antioxidants are non-catalytic small molecules that can quench ROS and reduce oxidative stress [73]. The most abundant nonenzymatic antioxidant is GSH, a tripeptide composed of glutamate, cysteine and glycine. Its synthesis is regulated by glutaminases (GLS1 and GLS2), the cystine-glutamate antiporter xCT (SLC7A11), the GSH biosynthetic rate-limiting enzyme glutamate-cysteine ligase (GCL) and the GSH synthetase (GSS) [74,75]. GCL is a heterodimeric holoenzyme that is composed of catalytic (GCLC) and modifier (GCLM) subunits; the expression levels of GCLC and GCLM are highly associated with the drug sensitivity of cancer cells and patient survival [76]. Moreover, the silencing of SLC7A11, GCLC and GSS represses the proliferation of clear cell renal cell carcinoma by decreasing the cellular GSH levels. However, reduced levels of GSH were also observed in patients with breast or colon cancers, especially in the advanced stages of these diseases, indicating the essential role of GSH in cancer cell survival [77,78]. Another nonenzymatic antioxidant is the TRX system, which is composed of TRXs and NADPH-dependent thioredoxin reductase (TrxR), which participate in the removal of harmful and excessive H2O2 [79]. There are two kinds of TRXs in mammalian cells, known as cytosolic TRX1 and mitochondrial TRX2 [80]. TRXs directly donate electrons to thiol-dependent PRDXs to remove H2O2. Oxidized TRXs are then reduced by TrxR, with NADPH as a cofactor [81]. Moreover, the oxidized PRDXs can also be reduced by TRXs [57]. Given the important role of the TRX system in cellular redox homeostasis, disturbance in the TRXs’ metabolism is highly associated with the progression and chemoresistance of multiple tumors [82], thus making TRXs essential targets for anticancer therapy.
3. ROS Promote Carcinogenesis and Cancer Progression
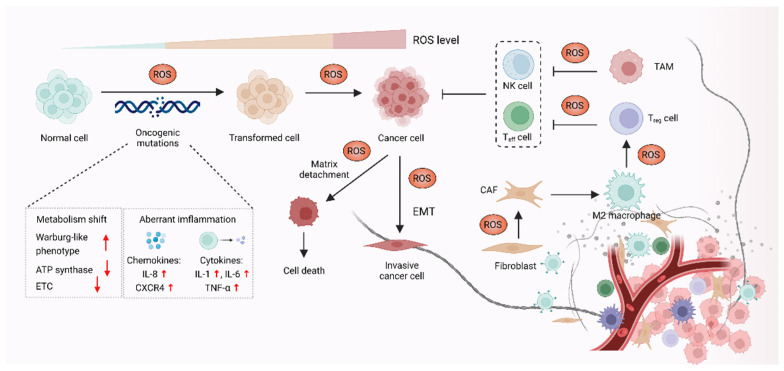
It was demonstrated that oxidative stress is involved in a wide range of pathologies including cancer, and increased production of ROS are common features of cancer cells. Although high ROS levels are cytotoxic and may exert anti-tumorigenic effects via oxidative damage and ROS-dependent death signaling, ROS play critical roles during tumorigenesis and cancer development. Here, we focus on the pro-tumorigenic role of ROS in malignant progression, which may be addressed with antioxidant therapy. The elevated levels of ROS from altered redox homeostasis contribute to the transformation of healthy cells into cancerous cells and enable their survival through two major mechanisms. The first is that ROS directly oxidize macromolecules, such as nucleic acids, proteins, lipids and glucose, resulting in gene mutation and aberrant inflammation [83]. The second mechanism involves oxidative stress-caused aberrant redox signaling. ROS, particularly H2O2 and O2•−, might function as signaling molecules to cause various signaling pathways to go awry and drive cancer progression [84,85] (Figure 2).
Figure 2.
ROS promote carcinogenesis and malignant progression. In the process of carcinogenesis, ROS can contribute to DNA damage, which results in aberrant inflammation and metabolism, leading to oncogenic mutations and cell hyperproliferation. ROS can also act as signaling molecules to enable cancer cells’ survival and cancer progression via epithelial-to-mesenchymal transition (EMT). In addition, ROS might affect stromal cells, such as cancer-associated fibroblasts (CAFs), regulatory T (Treg) cells, effector T (Teff) cells and NK cells in the tumor microenvironment (TME) to promote cancer progression.
3.1. ROS-Mediated Oncogenic Mutations Promote Carcinogenesis
The elevated ROS level functions as a contributor to the malignant transformation of normal cells by inducing mutations in nuclear DNA (nDNA) or mitochondrial DNA (mtDNA), as well as by causing oxidative damage to biomolecules [86,87,88]. Excessive ROS are highly associated with both nDNA and mtDNA mutations, which were reported to result in aberrant inflammation and metabolism, thus promoting malignant transformation [89]. Overproduction of ROS causes nDNA mutation and genetic instability, which further activate multiple oncogenes and lead to abnormal metabolic activity and decreased antioxidant capacity. These events eventually promote the production of ROS in a positive feedback manner [90,91]. Increased ROS was demonstrated to promote chronic inflammation, one of the major causes of cancer, through inducing chemokines such as IL-8 and CXCR4, as well as inflammatory cytokines including IL-1, IL-6 and TNF-α [92,93]. In the context of cancer initiation, mtDNA is also an essential target of ROS, as mtDNA mutation was linked to carcinogenesis [94,95]. Each mitochondrion carries a few dozen mtDNA copies. Increased ROS-induced somatic mutations in mtDNA affect the function of ETC and the ATP synthase, which might promote a Warburg-like phenotype shift towards glycolysis. The metabolic shift can shape cell behavior and participate in oncogenic transformation in multiple types of cancer, such as colorectal cancer, lung cancer, gastric cancer, liver cancer and head and neck cancer [96].
3.2. ROS Function as Signaling Molecules to Drive Cancer Progression
In addition to supporting carcinogenesis, ROS were also demonstrated to sustain and accelerate cancer progression via epithelial-to-mesenchymal transition (EMT), which is involved in reprogramming the tumor microenvironment (TME) [97,98]. The TME is affected by ROS through regulating the function of T cells, tumor-associated macrophages (TAMs) and cancer-associated fibroblasts (CAFs) in TME [99]. The TAMs and CAFs promote cell proliferation, angiogenesis, immunosuppression and invasion, thus enabling cancer progression via the reciprocal crosstalk between cancer cells and the TME [100]. Moreover, regulatory T (Treg) cells and cytotoxic CD8+ T cells in TME can suppress effective tumor immunity and contribute to cancer progression, which is associated with poor response to immunotherapy [101,102]. In terms of the role of ROS in TME, H2O2 is thought to function as signaling molecules, which might cause metabolic changes in CAFs, such as altered glucose uptake and mitochondrial activity [103,104]. ROS also contribute to cancer progression by triggering the immunosuppressive properties of TAMs. For instance, mitochondrial ROS activate MAPK/ERK activity, which contributes to the secretion of TNF-α and subsequently promotes cancer invasion [105]. Furthermore, it was also demonstrated that O2•− can suppress T cell-mediated inflammation, thus promoting TAM-mediated immunosuppression and leading to tumor development [106].
4. Antioxidant Therapeutic Strategies in Cancer
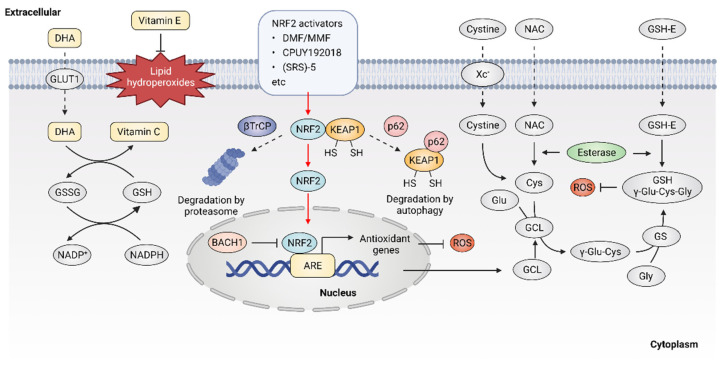
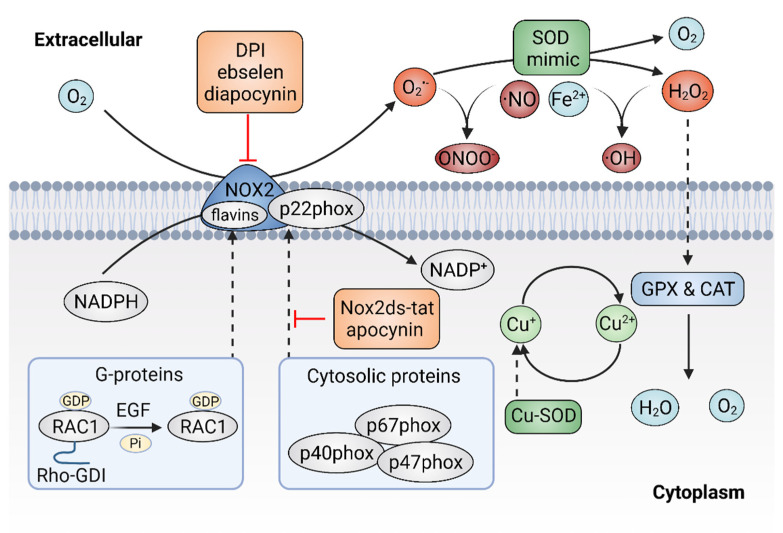
Given the important role of ROS in cancer, it follows that modulating ROS levels is a promising anticancer strategy. This may suppress ROS-induced carcinogenesis and cancer progression by inducing oxidative damage and ROS-dependent cell death [1,89]. Therefore, multiple antioxidants and weak pro-oxidants were explored in pre-clinical research and clinical evaluations. Cancer cells can produce excessive ROS through the above-mentioned mechanisms and increased formation of ROS are common features of cancer cells, which makes them more susceptible to a further increase in ROS than normal cells. Therefore, pro-oxidants may function as anticancer agents. For example, it was reported that exogeneous H2O2 can dramatically reduce the survival of MCF-7 cells with PRDX1 knockout, showing the potential of pro-oxidants to promote ROS-mediated cell death [107]. In addition, weak pro-oxidants may also function as important contributors to antioxidant therapy by boosting internal antioxidant capacity. However, treatment with weak pro-oxidants in cancer therapy still needs further investigation. Here, we focus on the antioxidant therapeutic strategies using antioxidants. Overall, antioxidant therapeutic strategies in cancer can be classified as targeting ROS with nonenzymatic antioxidants, including NRF2 activators [108], vitamins [109,110] (Figure 3) or targeting ROS with enzymatic antioxidants, including NOX inhibitors [18,111], SOD mimics [112], NAC and GSH esters (Figure 4) (Table 1) [113,114].
Figure 3.
Targeting ROS with nonenzymatic antioxidants. Dehydroascorbic acid (DHA), the oxidized form of vitamin C, is taken up by cells through glucose transporter 1 (GLUT1) and then reduced to vitamin C. Vitamin E is located in cell membranes and defends against lipid hydroperoxides. NRF2 activators may disrupt the KEAP1-NRF2 interaction, leading to the activation of NRF2 downstream antioxidant genes. Glutathione (GSH) is synthesized from cysteine, glutamate and glycine. Exogenous N-Acetyl cysteine (NAC) and GSH esters (GSH-E) supplementation promote GSH production and defense against excessive ROS.
Figure 4.
Targeting ROS with enzymatic antioxidants. The inhibitors of plasma membrane NADPH oxidase 2 (NOX2) can prevent the production of superoxide (O2•−) and superoxide dismutase (SOD) mimics might dismutate O2•− to hydrogen peroxide (H2O2).
Table 1.
Anticancer antioxidants in clinical trials.
| Antioxidants | Cancer Types | Trial Status | Trial ID |
|---|---|---|---|
| NRF2 activators | |||
| Sulforaphane | Lung cancer | Phase 2 | NCT03232138 |
| Breast cancer | Phase 2 | NCT00982319 | |
| Prostate cancer | Phase 2 | NCT01228084 | |
| Colon cancer | NA | NCT01344330 | |
| HNSCC | Early Phase 1 | NCT03182959 | |
| Resveratrol | Colon cancer | Phase 1 | NCT00256334 |
| Colorectal cancer | Phase 1 | NCT00920803 | |
| Neuroendocrine tumor | NA | NCT01476592 | |
| Breast cancer | NA | NCT03482401 | |
| Multiple myeloma | Phase 2 | NCT00920556 | |
| Quercetin | Prostate cancer | Phase 1 | NCT01912820 |
| Colorectal cancer | NA | NCT00003365 | |
| Pancreatic cancer/NSCLC | Phase 2/3 | NCT02195232 | |
| Curcumin | Breast cancer | Phase 2 | NCT01042938 |
| Colorectal cancer | Phase 2 | NCT02439385 | |
| Prostate cancer | NA | NCT03211104 | |
| Head and neck cancer | Early Phase 1 | NCT01160302 | |
| Pancreatic cancer | Phase 2 | NCT00192842 | |
| Bardoxolone-methyl (CDDO-Me, RTA402) |
Solid tumors/Lymphoid malignancies | Phase 1 | NCT00529438 |
| Pancreatic cancer | Phase 1 | NCT00529113 | |
| Solid tumors/ Lymphoid malignancies | Phase 1 | NCT00508807 | |
| RTA-408 (omaveloxolone) |
NSCLC | Phase 1 | NCT02029729 |
| Breast cancer | Phase 2 | NCT02142959 | |
| Melanoma | Phase 1/2 | NCT02259231 | |
| Dimethyl fumarate | Multiple sclerosis | Phase 3 | NCT02430532 |
| Lymphocytic leukemia | Phase 1 | NCT02784834 | |
| Glioblastoma | Phase 1 | NCT02337426 | |
| Oltipraz | Lung cancer | Phase 1 | NCT00006457 |
| SOD mimics | |||
| GC4419 | Head and neck cancer | Phase 2 | NCT04529850 |
| Pancreatic cancer | Phase 1/2 | NCT03340974 | |
| Squamous cell carcinoma | Phase 1 | NCT01921426 | |
| Head and neck cancer | Phase 2 | NCT02508389 | |
| Metalloporphyrins | Lung cancer | Phase 3 | NCT00054795 |
| NOX inhibitors | |||
| Ebselen (SPI-1005) | Cancer | Phase 1 | NCT01452607 |
| Lung cancer, Head and neck cancer | Phase 2 | NCT01451853 | |
| GSH-related antioxidants | |||
| NAC | Breast cancer | Phase 1 | NCT01878695 |
| Gastric cancer | NA | NCT03238404 | |
| Ovarian cancer | NA | NCT03491033 | |
| Head and neck cancer | Phase 2 | NCT02123511 | |
| Gastrointestinal neoplasms | Phase 2 | NCT00196885 | |
| Bladder cancer | NA | NCT02756637 | |
| Lung cancer | Phase 2 | NCT00691132 | |
| Colorectal cancer | NA | NCT01325909 | |
| NOV-002 | Breast cancer | Phase 2 | NCT00499122 |
| Ovarian cancer | Phase 2 | NCT00345540 | |
| NSCLC | Phase 3 | NCT00347412 | |
| Leukemia | Phase 2 | NCT00960726 | |
| Reduced GSH | Breast cancer | Phase 2 | NCT00266331 |
| Vitamins | |||
| Vitamin C | Ovarian cancer | Phase 2 | NCT00284427 |
| Pancreatic cancer | Phase 1 | NCT00954525 | |
| Prostatic neoplasms | Phase 2 | NCT01080352 | |
| Ovarian cancer | Phase 2 | NCT00284427 | |
| Advanced cancer | Phase 1/2 | NCT01050621 | |
| Solid cancers | Phase 1 | NCT00441207 | |
| NSCLC | Phase 1/2 | NCT02655913 | |
| Head and Neck Cancer | NA | NCT03531190 | |
| Skin cancer | NA | NCT01032031 | |
| Liver cancer | Phase 1/2 | NCT01754987 | |
| Vitamin E | Prostate cancer | Phase 3 | NCT00006392 |
| Colorectal cancer | Phase 1 | NCT00905918 | |
| Head and neck neoplasms | Phase 2 | NCT02397486 | |
| Skin neoplasms | NA | NCT02248584 | |
| Pancreatic neoplasms | Phase 1 | NCT00985777 | |
| Breast cancer | Phase 2 | NCT00022204 |
NA: Not Applicable; HNSCC, head and neck squamous cell carcinoma; NSCLC, Non-small cell lung cancer.
4.1. Targeting ROS with Nonenzymatic Antioxidants
The transcription factor NRF2 was considered as a master regulator of various homeostatic genes that defend against cellular stress, including oxidative stress [115]. Upon exposure to oxidative stress, the transcription factor NRF2 is released from its principal negative regulator Kelch-like ECH-associated protein 1 (KEAP1) and translocates to the nucleus, where NRF2 binds to antioxidant response element (ARE) and promotes the expression of antioxidant genes [116]. High expression of NRF2 was observed in various oxidative stress-related diseases including cancer, especially in NRF2-activated malignant tumors. NRF2 activators were considered as potential agents to prevent carcinogenesis or reverse cancer progression [117]. Five categories of NRF2 activator were developed, the underlying action mechanisms of which include: (1) modification on sensor cysteines of KEAP1, leading to the dissociation between NRF2 and KEAP1 [118,119]; (2) direct disruption of the KEAP1-NRF2 interaction [120]; (3) disruption of the interaction between NRF2 and β-transducin repeat-containing protein (βTrCP), which targets NRF2 for proteasome degradation [121]; (4) sequestration of KEAP1 into autophagosomes by p62 [122]; (5) upregulation of NRF2 protein levels by de novo synthesis that cannot be degraded by KEAP1 [123]; (6) inhibition of the NRF2 transcriptional repressor BTB domain and CNC homolog 1 (BACH1) [124].
The current development of NRF2 activators is mainly based on modifying sensor cysteines of KEAP1 and disrupting the KEAP1-NRF2 interaction. For instance, fumaric acid esters are oral analogs of fumarate that represent a group of NRF2 activators that work by modifying sensor cysteines of KEAP1, among which dimethyl fumarate (DMF) is the most successful example [125]. It was reported that DMF can alkylate Cys151 of KEAP1, leading to the dissociation of NRF2 and KEAP1 [126]. DMF metabolite monomethyl fumarate (MMF) was also demonstrated to react with KEAP1 through Cys151, thereby stabilizing and activating NRF2 [127]. DMF and its major metabolite MMF can reduce inflammatory responses and exhibit a favorable tolerability profile in clinical trials, showing promise for cancer treatment [128]. In addition, compounds that show improved bioavailability compared with MMF, through improving the release rate, were synthesized, such as TFM735, which is reported to activate NRF2 via the Cys151 in KEAP1, leading to the inhibition of IL-6 and IL-17 from peripheral blood mononuclear cells [129]. In addition, nitro fatty acids (NO2-FAs), such as nitro linoleic acid and nitro-oleic acid, are endogenous signaling mediators that react with Cys273 and Cys288 in KEAP1 through nitro alkylation, resulting in the activation of NRF2 and being implicated in anti-inflammatory activities [130]. Recently, the non-covalent NRF2 activators were developed, which directly disrupt the KEAP1–NRF2 protein–protein interaction via a cysteine-independent binding mechanism [131]. For instance, the bis-carboxylic acid compound CPUY192018 is a high-affinity KEAP1 ligand, which promotes the release of NRF2 from KEAP1 and enhances the expression of NRF2-target genes [132]. The sulfonamide-containing compounds were reported to inhibit the KEAP1–NRF2 interaction and enhance the expression of NAD(P)H: quinone oxidoreductase (NQO1), which reduces lung inflammation in animal models [133]. The naphthalene bis-sulfonamide was also reported to promote the expression of NRF2-target NQO1 and protect against dextran sulfate sodium (DSS)-induced colitis [134]. In addition to the above-mentioned compounds, (SRS)-5 and benzene-disulfonamides were also demonstrated to function as potent non-covalent NRF2 activators that disrupt the interaction between KEAP1 and NRF2 [135,136]. Altogether, these compounds are high-affinity ligands for KEAP1 and can directly block the KEAP1–NRF2 interface, thereby activating NRF2 downstream antioxidant genes and protecting cells from oxidative stress. Although current drugs mainly target KEAP1, it is noted that NRF2 might bind to ARE sequences in a KEAP1-independent manner, possibly involving the regulation of transcriptional repressor BACH1 [137]. Therefore, compounds that inhibit the binding of BACH1 to ARE-driven genes, such as HMOX1, were also developed [124]. Presently, more NRF2 activators eliciting beneficial effects are arising. However, treatment with NRF2 activators may inactivate drug-induced oxidative stress that normally would result in cell death. Therefore, it is necessary to monitor their clinical efficacy, given that the activation of NRF2 may contribute to the development of chemoresistance [138,139]. Taken together, NRF2 activators have shown potential for cancer therapy, but further investigations are also needed to demonstrate their clinical efficacy, especially in combination with chemotherapeutic drugs.
NAC is currently one of the most studied antioxidant agents that can be quickly absorbed via the anion exchange membrane and deacetylate to produce cysteine, thus replenishing GSH [140]. NAC can reduce cysteine conjugates and is used therapeutically for many human diseases, including cancers [141]. However, NAC was also reported to increase melanoma cell metastasis in NOD-SCID-Il2rg−/− (NSG) mice [142]. GSH esters, the derivatives of GSH, were developed for GSH supplementation, since GSH cannot be effectively transported into cells and exogenously administered GSH is rapidly cleared in plasma. Ester derivatives of GSH, such as monoethyl (GSH-MEE), diethyl (GSH-DEE), monomethyl (GSH-OMe) and isopropyl esters have shown high efficiency in increasing cellular GSH level [143]. In addition, compared with oral administration, subcutaneous or intraperitoneal injection of GSH esters is more effective in elevating GSH levels in various tissues [144]. However, although the efficacy of GSH esters to alleviate oxidative stress in cells and animal models was demonstrated, clinical trials with GSH ester are still needed.
As the most widely used dietary antioxidants, L-ascorbic acid (vitamin C) and α- tocopherol (vitamin E) are of great interest in cancer therapy [145]. Vitamin C is a type of water-soluble vitamin that cannot be synthesized endogenously in the human body, but can only be provided by dietary supplement, making it an essential nutritional component [146]. Dehydroascorbic acid (DHA), the oxidized form of vitamin C, is absorbed from the renal tubules by renal epithelial cells and functions as a reductant and an enzyme cofactor [147]. It was described that high dose vitamin C shows promising antitumor efficacy in patients with advanced cancer [15,148,149,150]. However, the role of vitamin C in cancer treatment is still controversial, as half of the studies indicate that vitamin C has no significant effect on the incidence and mortality of cancer [151,152,153]. Vitamin E is lipid soluble and mainly localizes to the plasma membrane, where it functions as a ROS scavenger through reacting with free radicals, thus defending against oxidative stress [154]. It was reported that vitamin E only has low toxicity and causes no obvious side effects at high dose intake [155]. However, several animal studies showed that vitamin E supplements might promote carcinogenesis and cancer progression [156]. Overall, the controversial effect of antioxidants on cancer raises significant concerns regarding antioxidant supplements. Therefore, novel strategies are warranted to resolve the double-edged effect of supplemental antioxidants, including vitamin C and vitamin E.
4.2. Targeting ROS with Enzymatic Antioxidants
As mentioned above, the NOX family is a major source of ROS and excessive activation of NOXs can contribute to oxidative stress. Thus, agents that would efficaciously target NOXs to scavenge ROS might hold significant promise for cancer therapy [157]. There are two types of NOXs inhibitors, including peptidic inhibitors and small-molecule inhibitors, both of which are based on the mechanism of inhibiting NOX enzyme activity or suppressing the assembly of the NOX2 enzyme [158]. Small peptide inhibitors of NOX complexes have shown therapeutic potential. The first peptidic inhibitor is Nox2ds-tat ([H]-R-K-K-R-R-Q-R-R-R-C-S-T-R-I-R-R-Q-L-[NH2], also known as gp91ds-tat). Nox2ds-tat was reported to inhibit the assembly of NOX2, a complex that consists of six subunits: the Nox2 subunit (also known as gp91phox); p22phox, and four cytosolic components; p47phox (organizer subunit); p67phox (activator subunit); p40phox, and the small Rho-family GTP binding protein Rac1 or Rac2 [159,160]. Nox2ds-tat selectively blocks NOX2 activity through interrupting the Nox2–p47phox interaction [161]. The inhibitory effects of Nox2ds-tat were demonstrated both in vitro and in vivo. For instance, Nox2ds-tat was reported to inhibit the production of angiotensin II-induced O2•− [162]. Moreover, administration of Nox2ds-tat by subcutaneous infusion significantly attenuated the production of vascular O2•− and subsequent vascular inflammation in angiotensin II-infused rat model [34,163]. In summary, the viability of Nox2ds peptide as a NOX2 inhibitor was demonstrated, which is important for suppressing NOX2 activity and preventing excessive ROS production.
Currently, multiple small-molecule global inhibitors that inhibit NOXs or flavoproteins in general, were synthesized, including diphenyleneiodonium (DPI), ebselen and diapocynin [164]. Among them, DPI is the first identified and commonly used potential inhibitor of NOXs, which inhibits the production of ROS by forming adducts with FAD, potentially contributing to the reduction of ROS and showing anticancer properties in colon cancer cells [165]. However, as a nonselective inhibitor, DPI might target other flavin-dependent enzymes, such as xanthine oxidase and nitric oxide synthase. Ebselen and diapocynin are described as NOX inhibitors but were also previously found to display unrelated effects [166]. Unlike DPI, apocynin specifically prevents the activation of NOX2 by inhibiting the translocation of p47phox, thereby repressing the production of O2− in vitro and exhibiting anti-inflammatory activity in vivo [167]. In addition, other specific NOX inhibitors, were also identified via cellular and membrane assays [168]. For instance, fulvene-5, one of the fulvene derivatives that have a chemical similarity to DPI, could inhibit NOX2 and NOX4 in vitro, as well as block the growth of endothelial cell-derived neoplasia in mice [169]. However, despite the great efforts made by researchers, few NOXS inhibitors have yet reached clinical trials. It remains challenging to identify compounds that target NOX specifically and show a profound impact in alleviating cancer. Much more work is still needed to develop NOX inhibitors for the treatment of oxidative-stress-associated disorders, including cancer.
SOD is a metalloprotein that can efficiently eliminate O2•− with a dismutation mechanism. SOD was developed as a drug known as orgotein, to defend against oxidative stress in mammalian cells [170]. The anti-inflammatory property of orgotein was demonstrated through preclinical and clinical studies [171]. It was also reported that orgotein can effectively prevent or reduce the side effects of radiation therapy in bladder cancer patients [172]. In addition, several types of SOD mimics were synthesized, such as metalloporphyrins, Mn (II) polyamines, Mn (III) salens, Mn (III) corroles and Mn (IV) biliverdins [173,174,175]. Although the rate constants are much lower than the enzymes, SOD mimics appear to be effective in extracellular fluids where the antioxidant enzymes are absent or at deficient concentrations [176]. Moreover, some SOD mimics may act as pro-oxidants rather than antioxidants, thereby activating rather than mimicking SOD [177].
Metalloporphyrins have emerged as the most studied SOD mimics, such as Mn porphyrins. Various Mn porphyrin compounds, including MnTM-2-pYp5+, MnTE-2-pYp5+ and MnTDE-2-ImP5+, have shown high SOD activity that dismutates O2•− to H2O2 [178]. The protective and therapeutic potential of Mn porphyrins were demonstrated in animal models of diseases, including cancers. To date, more porphyrins or porphyrin-based SOD mimics were synthesized with the establishment of the structure–activity relationships between SOD and metal-site redox ability [19]. The Mn (II)-containing penta-aza macrocyclic manganese compound GC4419 (known as avasopasem manganese, AVA) was reported to enhance tumor-killing activity when synergized with radiation in head and neck cancer [179]. In addition, GC4419 can enhance the toxicity of high-dose vitamin C in a H₂O₂-dependent manner, promoting radiation-induced cancer cell killing [180]. Furthermore, GC4419 also exhibits therapeutic potential in the inflammation animal model [181]. Unlike GC4419, the Mn (III)- containing salen complexes, such as EUK-8, EUK-134 and EUK-189, are not specific and have dismutation activity on both O2•− and H2O2, showing protective effects for various types of cancer [182].
In summary, multiple antioxidant therapeutic strategies were developed for cancer treatment, which can be classified into two different categories of groups according to their targets: enzymatic antioxidants and nonenzymatic antioxidants, both of which have shown potential to act as antioxidant drugs in pre-clinical and clinical research.
5. Perspectives and Conclusions
Because oxidative stress is a well-documented phenomenon in cancer, it is rational that antioxidants can significantly reduce cancer incidence and progression. Although multiple antioxidant therapeutic strategies were explored and some of them are undergoing clinical trial, their efficacy remains unsatisfied. The factors that impede the anticancer activity of antioxidants include: (1) most studies use pharmacological but not dietary doses based on in vitro studies, however, antioxidants may be affected by complex, in vivo conditions; (2) antioxidants might be distributed unevenly in different tissues, and probably cannot function due to the low bioavailability and bio-accessibility in some specific organ; (3) some antioxidants exhibit antioxidant or pro-oxidant properties depending on their concentration and the pressure of oxygen. These factors determine the distinct consequences of the supplementary antioxidants. Moreover, most chemotherapeutic drugs generate high levels of ROS and result in oxidative stress. Treatment with antioxidants in cancer patients might, therefore, lead to an antagonistic effect on chemotherapeutic drug-induced cell death.
As discussed above, multiple antioxidants failed to demonstrate efficacy in clinical practice. Given that most antioxidant capacity is attributed to endogenously antioxidant enzymes or antioxidants, we propose that treatment with weak pro-oxidants to boost antioxidant activity might be a promising way for cancer patients, although the underlying biological rationale warrants further investigation and long-term follow-up of interventions are needed. An improved understanding of these mechanisms will facilitate the development of novel therapeutic agents, which might be effective in the prevention and treatment of cancer.
Acknowledgments
The authors acknowledge BioRender (www.biorender.com, accessed on 7 May 2022). Figures in this review were created with the BioRender platform.
Author Contributions
Conceptualization, C.H. and J.X.; writing—original draft preparation, M.L.; writing—review and editing, L.Z., Z.H., B.L. and E.C.N.; supervision, C.H. and J.X.; funding acquisition, C.H. and J.X. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by grants from the National Natural Science Foundation of China (81790251, 52007087, 82103168 and 82073246), the Natural Science Foundation of Zhejiang Province, China (LY22C110001), the Natural Science Foundation of Ningbo City, China (202003N4116), the Fund from the Educational Commission of Zhejiang Province, China (Y202044047), and the Fundamental Research Funds for the Provincial Universities of Zhejiang (SJLZ2022001).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Forman H.J., Zhang H. Targeting oxidative stress in disease: Promise and limitations of antioxidant therapy. Nat. Rev. Drug Discov. 2021;20:689–709. doi: 10.1038/s41573-021-00233-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayes J.D., Dinkova-Kostova A.T., Tew K.D. Oxidative Stress in Cancer. Cancer Cell. 2020;38:167–197. doi: 10.1016/j.ccell.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peng L., Jiang J., Chen H.N., Zhou L., Huang Z., Qin S., Jin P., Luo M., Li B., Shi J., et al. Redox-sensitive cyclophilin A elicits chemoresistance through realigning cellular oxidative status in colorectal cancer. Cell Rep. 2021;37:110069. doi: 10.1016/j.celrep.2021.110069. [DOI] [PubMed] [Google Scholar]
- 4.Wang K., Jiang J., Lei Y., Zhou S., Wei Y., Huang C. Targeting Metabolic-Redox Circuits for Cancer Therapy. Trends Biochem. Sci. 2019;44:401–414. doi: 10.1016/j.tibs.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Liang D., Minikes A.M., Jiang X. Ferroptosis at the intersection of lipid metabolism and cellular signaling. Mol. Cell. 2022 doi: 10.1016/j.molcel.2022.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Virag L., Jaen R.I., Regdon Z., Bosca L., Prieto P. Self-defense of macrophages against oxidative injury: Fighting for their own survival. Redox Biol. 2019;26:101261. doi: 10.1016/j.redox.2019.101261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caserta S., Ghezzi P. Release of redox enzymes and micro-RNAs in extracellular vesicles, during infection and inflammation. Free Radic. Biol. Med. 2021;169:248–257. doi: 10.1016/j.freeradbiomed.2021.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Chavez Z., Vazquez C., Mejia-Tlachi M., Marquez-Duenas C., Manning-Cela R., Encalada R., Rodriguez-Enriquez S., Michels P.A.M., Moreno-Sanchez R., Saavedra E. Gamma-glutamylcysteine synthetase and tryparedoxin 1 exert high control on the antioxidant system in Trypanosoma cruzi contributing to drug resistance and infectivity. Redox Biol. 2019;26:101231. doi: 10.1016/j.redox.2019.101231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaiswing L., St Clair W.H., St Clair D.K. Redox Paradox: A Novel Approach to Therapeutics-Resistant Cancer. Antioxid. Redox Signal. 2018;29:1237–1272. doi: 10.1089/ars.2017.7485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Urso L., Cavallari I., Sharova E., Ciccarese F., Pasello G., Ciminale V. Metabolic rewiring and redox alterations in malignant pleural mesothelioma. Br. J. Cancer. 2020;122:52–61. doi: 10.1038/s41416-019-0661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canli O., Nicolas A.M., Gupta J., Finkelmeier F., Goncharova O., Pesic M., Neumann T., Horst D., Lower M., Sahin U., et al. Myeloid Cell-Derived Reactive Oxygen Species Induce Epithelial Mutagenesis. Cancer Cell. 2017;32:869–883.e865. doi: 10.1016/j.ccell.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Luo M., Huang Z., Yang X., Chen Y., Jiang J., Zhang L., Zhou L., Qin S., Jin P., Fu S., et al. PHLDB2 Mediates Cetuximab Resistance via Interacting With EGFR in Latent Metastasis of Colorectal Cancer. Cell Mol. Gastroenterol. Hepatol. 2022;13:1223–1242. doi: 10.1016/j.jcmgh.2021.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klaunig J.E. Oxidative Stress and Cancer. Curr. Pharm. Des. 2018;24:4771–4778. doi: 10.2174/1381612825666190215121712. [DOI] [PubMed] [Google Scholar]
- 14.Rojo de la Vega M., Chapman E., Zhang D.D. NRF2 and the Hallmarks of Cancer. Cancer Cell. 2018;34:21–43. doi: 10.1016/j.ccell.2018.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ngo B., Van Riper J.M., Cantley L.C., Yun J. Targeting cancer vulnerabilities with high-dose vitamin C. Nat. Rev. Cancer. 2019;19:271–282. doi: 10.1038/s41568-019-0135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li P., Wu M., Wang J., Sui Y., Liu S., Shi D. NAC selectively inhibit cancer telomerase activity: A higher redox homeostasis threshold exists in cancer cells. Redox Biol. 2016;8:91–97. doi: 10.1016/j.redox.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saidu N.E.B., Kavian N., Leroy K., Jacob C., Nicco C., Batteux F., Alexandre J. Dimethyl fumarate, a two-edged drug: Current status and future directions. Med. Res. Rev. 2019;39:1923–1952. doi: 10.1002/med.21567. [DOI] [PubMed] [Google Scholar]
- 18.Augsburger F., Filippova A., Rasti D., Seredenina T., Lam M., Maghzal G., Mahiout Z., Jansen-Durr P., Knaus U.G., Doroshow J., et al. Pharmacological characterization of the seven human NOX isoforms and their inhibitors. Redox Biol. 2019;26:101272. doi: 10.1016/j.redox.2019.101272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batinic-Haberle I., Tome M.E. Thiol regulation by Mn porphyrins, commonly known as SOD mimics. Redox Biol. 2019;25:101139. doi: 10.1016/j.redox.2019.101139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris I.S., DeNicola G.M. The Complex Interplay between Antioxidants and ROS in Cancer. Trends Cell Biol. 2020;30:440–451. doi: 10.1016/j.tcb.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Sies H., Jones D.P. Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Nat. Rev. Mol. Cell Biol. 2020;21:363–383. doi: 10.1038/s41580-020-0230-3. [DOI] [PubMed] [Google Scholar]
- 22.Sies H., Belousov V.V., Chandel N.S., Davies M.J., Jones D.P., Mann G.E., Murphy M.P., Yamamoto M., Winterbourn C. Defining roles of specific reactive oxygen species (ROS) in cell biology and physiology. Nat. Rev. Mol. Cell Biol. 2022:1–17. doi: 10.1038/s41580-022-00456-z. [DOI] [PubMed] [Google Scholar]
- 23.Galan-Cobo A., Sitthideatphaiboon P., Qu X., Poteete A., Pisegna M.A., Tong P., Chen P.H., Boroughs L.K., Rodriguez M.L.M., Zhang W., et al. LKB1 and KEAP1/NRF2 Pathways Cooperatively Promote Metabolic Reprogramming with Enhanced Glutamine Dependence in KRAS-Mutant Lung Adenocarcinoma. Cancer Res. 2019;79:3251–3267. doi: 10.1158/0008-5472.CAN-18-3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J., Lu Q., Cai J., Wang Y., Lai X., Qiu Y., Huang Y., Ke Q., Zhang Y., Guan Y., et al. Nestin regulates cellular redox homeostasis in lung cancer through the Keap1-Nrf2 feedback loop. Nat. Commun. 2019;10:5043. doi: 10.1038/s41467-019-12925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schofield J.H., Schafer Z.T. Mitochondrial Reactive Oxygen Species and Mitophagy: A Complex and Nuanced Relationship. Antioxid. Redox Signal. 2021;34:517–530. doi: 10.1089/ars.2020.8058. [DOI] [PubMed] [Google Scholar]
- 26.Cantoni O., Zito E., Fiorani M., Guidarelli A. Arsenite impinges on endoplasmic reticulum-mitochondria crosstalk to elicit mitochondrial ROS formation and downstream toxicity. Semin. Cancer Biol. 2021;76:132–138. doi: 10.1016/j.semcancer.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 27.He A., Dean J.M., Lodhi I.J. Peroxisomes as cellular adaptors to metabolic and environmental stress. Trends Cell Biol. 2021;31:656–670. doi: 10.1016/j.tcb.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nolfi-Donegan D., Braganza A., Shiva S. Mitochondrial electron transport chain: Oxidative phosphorylation, oxidant production, and methods of measurement. Redox Biol. 2020;37:101674. doi: 10.1016/j.redox.2020.101674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raimondi V., Ciccarese F., Ciminale V. Oncogenic pathways and the electron transport chain: A dangeROS liaison. Br. J. Cancer. 2020;122:168–181. doi: 10.1038/s41416-019-0651-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dambrova M., Zuurbier C.J., Borutaite V., Liepinsh E., Makrecka-Kuka M. Energy substrate metabolism and mitochondrial oxidative stress in cardiac ischemia/reperfusion injury. Free Radic. Biol. Med. 2021;165:24–37. doi: 10.1016/j.freeradbiomed.2021.01.036. [DOI] [PubMed] [Google Scholar]
- 31.Flockhart M., Nilsson L.C., Tais S., Ekblom B., Apro W., Larsen F.J. Excessive exercise training causes mitochondrial functional impairment and decreases glucose tolerance in healthy volunteers. Cell Metab. 2021;33:957–970.e956. doi: 10.1016/j.cmet.2021.02.017. [DOI] [PubMed] [Google Scholar]
- 32.Stefanatos R., Sanz A. The role of mitochondrial ROS in the aging brain. FEBS Lett. 2018;592:743–758. doi: 10.1002/1873-3468.12902. [DOI] [PubMed] [Google Scholar]
- 33.Marin R., Chiarello D.I., Abad C., Rojas D., Toledo F., Sobrevia L. Oxidative stress and mitochondrial dysfunction in early-onset and late-onset preeclampsia. Biochim. Biophys. Acta Mol. Basis Dis. 2020;1866:165961. doi: 10.1016/j.bbadis.2020.165961. [DOI] [PubMed] [Google Scholar]
- 34.Bedard K., Krause K.H. The NOX family of ROS-generating NADPH oxidases: Physiology and pathophysiology. Physiol. Rev. 2007;87:245–313. doi: 10.1152/physrev.00044.2005. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Y., Murugesan P., Huang K., Cai H. NADPH oxidases and oxidase crosstalk in cardiovascular diseases: Novel therapeutic targets. Nat. Rev. Cardiol. 2020;17:170–194. doi: 10.1038/s41569-019-0260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Magnani F., Mattevi A. Structure and mechanisms of ROS generation by NADPH oxidases. Curr. Opin. Struct. Biol. 2019;59:91–97. doi: 10.1016/j.sbi.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Dang P.M., Rolas L., El-Benna J. The Dual Role of Reactive Oxygen Species-Generating Nicotinamide Adenine Dinucleotide Phosphate Oxidases in Gastrointestinal Inflammation and Therapeutic Perspectives. Antioxid. Redox Signal. 2020;33:354–373. doi: 10.1089/ars.2020.8018. [DOI] [PubMed] [Google Scholar]
- 38.Sitia R., Braakman I. Quality control in the endoplasmic reticulum protein factory. Nature. 2003;426:891–894. doi: 10.1038/nature02262. [DOI] [PubMed] [Google Scholar]
- 39.Wadgaonkar P., Chen F. Connections between endoplasmic reticulum stress-associated unfolded protein response, mitochondria, and autophagy in arsenic-induced carcinogenesis. Semin. Cancer Biol. 2021;76:258–266. doi: 10.1016/j.semcancer.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bibli S.I., Fleming I. Oxidative Post-Translational Modifications: A Focus on Cysteine S-Sulfhydration and the Regulation of Endothelial Fitness. Antioxid. Redox Signal. 2021;35:1494–1514. doi: 10.1089/ars.2021.0162. [DOI] [PubMed] [Google Scholar]
- 41.Samanta S., Yang S., Debnath B., Xue D., Kuang Y., Ramkumar K., Lee A.S., Ljungman M., Neamati N. The Hydroxyquinoline Analogue YUM70 Inhibits GRP78 to Induce ER Stress-Mediated Apoptosis in Pancreatic Cancer. Cancer Res. 2021;81:1883–1895. doi: 10.1158/0008-5472.CAN-20-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ren J., Bi Y., Sowers J.R., Hetz C., Zhang Y. Endoplasmic reticulum stress and unfolded protein response in cardiovascular diseases. Nat. Rev. Cardiol. 2021;18:499–521. doi: 10.1038/s41569-021-00511-w. [DOI] [PubMed] [Google Scholar]
- 43.Bhattarai K.R., Chaudhary M., Kim H.R., Chae H.J. Endoplasmic Reticulum (ER) Stress Response Failure in Diseases. Trends Cell Biol. 2020;30:672–675. doi: 10.1016/j.tcb.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 44.Wong C.O., Karagas N.E., Jung J., Wang Q., Rousseau M.A., Chao Y., Insolera R., Soppina P., Collins C.A., Zhou Y., et al. Regulation of longevity by depolarization-induced activation of PLC-beta-IP3R signaling in neurons. Proc. Natl. Acad. Sci. USA. 2021;118:e2004253118. doi: 10.1073/pnas.2004253118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Booth D.M., Varnai P., Joseph S.K., Hajnoczky G. Oxidative bursts of single mitochondria mediate retrograde signaling toward the ER. Mol. Cell. 2021;81:3866–3876.e3862. doi: 10.1016/j.molcel.2021.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fransen M., Lismont C. Redox Signaling from and to Peroxisomes: Progress, Challenges, and Prospects. Antioxid. Redox Signal. 2019;30:95–112. doi: 10.1089/ars.2018.7515. [DOI] [PubMed] [Google Scholar]
- 47.Sargsyan Y., Thoms S. Staying in Healthy Contact: How Peroxisomes Interact with Other Cell Organelles. Trends Mol. Med. 2020;26:201–214. doi: 10.1016/j.molmed.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 48.Ivashchenko O., Van Veldhoven P.P., Brees C., Ho Y.S., Terlecky S.R., Fransen M. Intraperoxisomal redox balance in mammalian cells: Oxidative stress and interorganellar cross-talk. Mol. Biol. Cell. 2011;22:1440–1451. doi: 10.1091/mbc.e10-11-0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chung H.L., Wangler M.F., Marcogliese P.C., Jo J., Ravenscroft T.A., Zuo Z., Duraine L., Sadeghzadeh S., Li-Kroeger D., Schmidt R.E., et al. Loss- or Gain-of-Function Mutations in ACOX1 Cause Axonal Loss via Different Mechanisms. Neuron. 2020;106:589–606.e586. doi: 10.1016/j.neuron.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen X.F., Tian M.X., Sun R.Q., Zhang M.L., Zhou L.S., Jin L., Chen L.L., Zhou W.J., Duan K.L., Chen Y.J., et al. SIRT5 inhibits peroxisomal ACOX1 to prevent oxidative damage and is downregulated in liver cancer. EMBO Rep. 2018;19:e45124. doi: 10.15252/embr.201745124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Emanuelli M., Sartini D., Molinelli E., Campagna R., Pozzi V., Salvolini E., Simonetti O., Campanati A., Offidani A. The Double-Edged Sword of Oxidative Stress in Skin Damage and Melanoma: From Physiopathology to Therapeutical Approaches. Antioxidants. 2022;11:612. doi: 10.3390/antiox11040612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nishigori C., Hattori Y., Toyokuni S. Role of reactive oxygen species in skin carcinogenesis. Antioxid. Redox Signal. 2004;6:561–570. doi: 10.1089/152308604773934314. [DOI] [PubMed] [Google Scholar]
- 53.Allouche J., Rachmin I., Adhikari K., Pardo L.M., Lee J.H., McConnell A.M., Kato S., Fan S., Kawakami A., Suita Y., et al. NNT mediates redox-dependent pigmentation via a UVB- and MITF-independent mechanism. Cell. 2021;184:4268–4283.e4220. doi: 10.1016/j.cell.2021.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kesanakurti D., Maddirela D., Banasavadi-Siddegowda Y.K., Lai T.H., Qamri Z., Jacob N.K., Sampath D., Mohanam S., Kaur B., Puduvalli V.K. A novel interaction of PAK4 with PPARgamma to regulate Nox1 and radiation-induced epithelial-to-mesenchymal transition in glioma. Oncogene. 2017;36:5309–5320. doi: 10.1038/onc.2016.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Y., Branicky R., Noe A., Hekimi S. Superoxide dismutases: Dual roles in controlling ROS damage and regulating ROS signaling. J. Cell Biol. 2018;217:1915–1928. doi: 10.1083/jcb.201708007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shui S., Zhao Z., Wang H., Conrad M., Liu G. Non-enzymatic lipid peroxidation initiated by photodynamic therapy drives a distinct ferroptosis-like cell death pathway. Redox Biol. 2021;45:102056. doi: 10.1016/j.redox.2021.102056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bolduc J., Koruza K., Luo T., Malo Pueyo J., Vo T.N., Ezerina D., Messens J. Peroxiredoxins wear many hats: Factors that fashion their peroxide sensing personalities. Redox Biol. 2021;42:101959. doi: 10.1016/j.redox.2021.101959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Patgiri A., Skinner O.S., Miyazaki Y., Schleifer G., Marutani E., Shah H., Sharma R., Goodman R.P., To T.L., Robert Bao X., et al. An engineered enzyme that targets circulating lactate to alleviate intracellular NADH:NAD(+) imbalance. Nat. Biotechnol. 2020;38:309–313. doi: 10.1038/s41587-019-0377-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ogiwara H., Takahashi K., Sasaki M., Kuroda T., Yoshida H., Watanabe R., Maruyama A., Makinoshima H., Chiwaki F., Sasaki H., et al. Targeting the Vulnerability of Glutathione Metabolism in ARID1A-Deficient Cancers. Cancer Cell. 2019;35:177–190.e178. doi: 10.1016/j.ccell.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 60.Zhang J., Li X., Han X., Liu R., Fang J. Targeting the Thioredoxin System for Cancer Therapy. Trends Pharmacol. Sci. 2017;38:794–808. doi: 10.1016/j.tips.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 61.Costa T.J., Barros P.R., Arce C., Santos J.D., da Silva-Neto J., Egea G., Dantas A.P., Tostes R.C., Jimenez-Altayo F. The homeostatic role of hydrogen peroxide, superoxide anion and nitric oxide in the vasculature. Free Radic. Biol. Med. 2021;162:615–635. doi: 10.1016/j.freeradbiomed.2020.11.021. [DOI] [PubMed] [Google Scholar]
- 62.Reddi A.R., Culotta V.C. SOD1 integrates signals from oxygen and glucose to repress respiration. Cell. 2013;152:224–235. doi: 10.1016/j.cell.2012.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Montllor-Albalate C., Colin A.E., Chandrasekharan B., Bolaji N., Andersen J.L., Wayne Outten F., Reddi A.R. Extra-mitochondrial Cu/Zn superoxide dismutase (Sod1) is dispensable for protection against oxidative stress but mediates peroxide signaling in Saccharomyces cerevisiae. Redox Biol. 2019;21:101064. doi: 10.1016/j.redox.2018.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang M., Cobine P.A., Molik S., Naranuntarat A., Lill R., Winge D.R., Culotta V.C. The effects of mitochondrial iron homeostasis on cofactor specificity of superoxide dismutase 2. EMBO J. 2006;25:1775–1783. doi: 10.1038/sj.emboj.7601064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mohammedi K., Bellili-Munoz N., Marklund S.L., Driss F., Le Nagard H., Patente T.A., Fumeron F., Roussel R., Hadjadj S., Marre M., et al. Plasma extracellular superoxide dismutase concentration, allelic variations in the SOD3 gene and risk of myocardial infarction and all-cause mortality in people with type 1 and type 2 diabetes. Cardiovasc. Diabetol. 2015;14:845. doi: 10.1186/s12933-014-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dong S., Dong Y., Liu B., Liu J., Liu S., Zhao Z., Li W., Tian B., Zhao R., He F., et al. Guiding Transition Metal-Doped Hollow Cerium Tandem Nanozymes with Elaborately Regulated Multi-Enzymatic Activities for Intensive Chemodynamic Therapy. Adv. Mater. 2022;34:e2107054. doi: 10.1002/adma.202107054. [DOI] [PubMed] [Google Scholar]
- 67.Robbins M.E., Cho H.Y., Hansen J.M., Luchsinger J.R., Locy M.L., Velten M., Kleeberger S.R., Rogers L.K., Tipple T.E. Glutathione reductase deficiency alters lung development and hyperoxic responses in neonatal mice. Redox Biol. 2021;38:101797. doi: 10.1016/j.redox.2020.101797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Luzzatto L., Arese P. Favism and Glucose-6-Phosphate Dehydrogenase Deficiency. N. Engl. J. Med. 2018;378:60–71. doi: 10.1056/NEJMra1708111. [DOI] [PubMed] [Google Scholar]
- 69.Harel M., Aharoni A., Gaidukov L., Brumshtein B., Khersonsky O., Meged R., Dvir H., Ravelli R.B., McCarthy A., Toker L., et al. Structure and evolution of the serum paraoxonase family of detoxifying and anti-atherosclerotic enzymes. Nat. Struct. Mol. Biol. 2004;11:412–419. doi: 10.1038/nsmb767. [DOI] [PubMed] [Google Scholar]
- 70.Fumarola S., Cecati M., Sartini D., Ferretti G., Milanese G., Galosi A.B., Pozzi V., Campagna R., Morresi C., Emanuelli M., et al. Bladder Cancer Chemosensitivity is Affected by Paraoxonase-2 Expression. Antioxidants. 2020;9:175. doi: 10.3390/antiox9020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Campagna R., Bacchetti T., Salvolini E., Pozzi V., Molinelli E., Brisigotti V., Sartini D., Campanati A., Ferretti G., Offidani A., et al. Paraoxonase-2 Silencing Enhances Sensitivity of A375 Melanoma Cells to Treatment with Cisplatin. Antioxidants. 2020;9:1238. doi: 10.3390/antiox9121238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Devarajan A., Bourquard N., Hama S., Navab M., Grijalva V.R., Morvardi S., Clarke C.F., Vergnes L., Reue K., Teiber J.F., et al. Paraoxonase 2 deficiency alters mitochondrial function and exacerbates the development of atherosclerosis. Antioxid. Redox Signal. 2011;14:341–351. doi: 10.1089/ars.2010.3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Guan T., Song J., Wang Y., Guo L., Yuan L., Zhao Y., Gao Y., Lin L., Wang Y., Wei J. Expression and characterization of recombinant bifunctional enzymes with glutathione peroxidase and superoxide dismutase activities. Free Radic. Biol. Med. 2017;110:188–195. doi: 10.1016/j.freeradbiomed.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 74.Cao L., Wu G., Zhu J., Tan Z., Shi D., Wu X., Tang M., Li Z., Hu Y., Zhang S., et al. Genotoxic stress-triggered beta-catenin/JDP2/PRMT5 complex facilitates reestablishing glutathione homeostasis. Nat. Commun. 2019;10:3761. doi: 10.1038/s41467-019-11696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Floros K.V., Cai J., Jacob S., Kurupi R., Fairchild C.K., Shende M., Coon C.M., Powell K.M., Belvin B.R., Hu B., et al. MYCN-Amplified Neuroblastoma Is Addicted to Iron and Vulnerable to Inhibition of the System Xc-/Glutathione Axis. Cancer Res. 2021;81:1896–1908. doi: 10.1158/0008-5472.CAN-20-1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schaupp C.M., Botta D., White C.C., Scoville D.K., Srinouanprachanh S., Bammler T.K., MacDonald J., Kavanagh T.J. Persistence of improved glucose homeostasis in Gclm null mice with age and cadmium treatment. Redox Biol. 2022;49:102213. doi: 10.1016/j.redox.2021.102213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kelly-Aubert M., Trudel S., Fritsch J., Nguyen-Khoa T., Baudouin-Legros M., Moriceau S., Jeanson L., Djouadi F., Matar C., Conti M., et al. GSH monoethyl ester rescues mitochondrial defects in cystic fibrosis models. Hum. Mol. Genet. 2011;20:2745–2759. doi: 10.1093/hmg/ddr173. [DOI] [PubMed] [Google Scholar]
- 78.Navarro J., Obrador E., Carretero J., Petschen I., Avino J., Perez P., Estrela J.M. Changes in glutathione status and the antioxidant system in blood and in cancer cells associate with tumour growth in vivo. Free Radic. Biol. Med. 1999;26:410–418. doi: 10.1016/S0891-5849(98)00213-5. [DOI] [PubMed] [Google Scholar]
- 79.McCarver A.C., Lessner D.J. Molecular characterization of the thioredoxin system from Methanosarcina acetivorans. FEBS J. 2014;281:4598–4611. doi: 10.1111/febs.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hanschmann E.M., Petry S.F., Eitner S., Maresch C.C., Lingwal N., Lillig C.H., Linn T. Paracrine regulation and improvement of beta-cell function by thioredoxin. Redox Biol. 2020;34:101570. doi: 10.1016/j.redox.2020.101570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Peskin A.V., Meotti F.C., Kean K.M., Gobl C., Peixoto A.S., Pace P.E., Horne C.R., Heath S.G., Crowther J.M., Dobson R.C.J., et al. Modifying the resolving cysteine affects the structure and hydrogen peroxide reactivity of peroxiredoxin 2. J. Biol. Chem. 2021;296:100494. doi: 10.1016/j.jbc.2021.100494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perez-Jimenez R., Li J., Kosuri P., Sanchez-Romero I., Wiita A.P., Rodriguez-Larrea D., Chueca A., Holmgren A., Miranda-Vizuete A., Becker K., et al. Diversity of chemical mechanisms in thioredoxin catalysis revealed by single-molecule force spectroscopy. Nat. Struct. Mol. Biol. 2009;16:890–896. doi: 10.1038/nsmb.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhong H., Yin H. Role of lipid peroxidation derived 4-hydroxynonenal (4-HNE) in cancer: Focusing on mitochondria. Redox Biol. 2015;4:193–199. doi: 10.1016/j.redox.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ye Z.W., Zhang J., Townsend D.M., Tew K.D. Oxidative stress, redox regulation and diseases of cellular differentiation. Biochim. Biophys. Acta. 2015;1850:1607–1621. doi: 10.1016/j.bbagen.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Parascandolo A., Laukkanen M.O. Carcinogenesis and Reactive Oxygen Species Signaling: Interaction of the NADPH Oxidase NOX1-5 and Superoxide Dismutase 1–3 Signal Transduction Pathways. Antioxid. Redox Signal. 2019;30:443–486. doi: 10.1089/ars.2017.7268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Srinivas U.S., Tan B.W.Q., Vellayappan B.A., Jeyasekharan A.D. ROS and the DNA damage response in cancer. Redox Biol. 2019;25:101084. doi: 10.1016/j.redox.2018.101084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lood C., Blanco L.P., Purmalek M.M., Carmona-Rivera C., De Ravin S.S., Smith C.K., Malech H.L., Ledbetter J.A., Elkon K.B., Kaplan M.J. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat. Med. 2016;22:146–153. doi: 10.1038/nm.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ishikawa K., Takenaga K., Akimoto M., Koshikawa N., Yamaguchi A., Imanishi H., Nakada K., Honma Y., Hayashi J. ROS-generating mitochondrial DNA mutations can regulate tumor cell metastasis. Science. 2008;320:661–664. doi: 10.1126/science.1156906. [DOI] [PubMed] [Google Scholar]
- 89.Poprac P., Jomova K., Simunkova M., Kollar V., Rhodes C.J., Valko M. Targeting Free Radicals in Oxidative Stress-Related Human Diseases. Trends Pharmacol. Sci. 2017;38:592–607. doi: 10.1016/j.tips.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 90.Moloney J.N., Cotter T.G. ROS signalling in the biology of cancer. Semin. Cell Dev. Biol. 2018;80:50–64. doi: 10.1016/j.semcdb.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 91.Niedernhofer L.J., Gurkar A.U., Wang Y., Vijg J., Hoeijmakers J.H.J., Robbins P.D. Nuclear Genomic Instability and Aging. Annu. Rev. Biochem. 2018;87:295–322. doi: 10.1146/annurev-biochem-062917-012239. [DOI] [PubMed] [Google Scholar]
- 92.Blaser H., Dostert C., Mak T.W., Brenner D. TNF and ROS Crosstalk in Inflammation. Trends Cell Biol. 2016;26:249–261. doi: 10.1016/j.tcb.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 93.Gupta S.C., Hevia D., Patchva S., Park B., Koh W., Aggarwal B.B. Upsides and downsides of reactive oxygen species for cancer: The roles of reactive oxygen species in tumorigenesis, prevention, and therapy. Antioxid. Redox Signal. 2012;16:1295–1322. doi: 10.1089/ars.2011.4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhao M., Wang Y., Li L., Liu S., Wang C., Yuan Y., Yang G., Chen Y., Cheng J., Lu Y., et al. Mitochondrial ROS promote mitochondrial dysfunction and inflammation in ischemic acute kidney injury by disrupting TFAM-mediated mtDNA maintenance. Theranostics. 2021;11:1845–1863. doi: 10.7150/thno.50905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kopinski P.K., Singh L.N., Zhang S., Lott M.T., Wallace D.C. Mitochondrial DNA variation and cancer. Nat. Rev. Cancer. 2021;21:431–445. doi: 10.1038/s41568-021-00358-w. [DOI] [PubMed] [Google Scholar]
- 96.Sabharwal S.S., Schumacker P.T. Mitochondrial ROS in cancer: Initiators, amplifiers or an Achilles’ heel? Nat. Rev. Cancer. 2014;14:709–721. doi: 10.1038/nrc3803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Koelwyn G.J., Quail D.F., Zhang X., White R.M., Jones L.W. Exercise-dependent regulation of the tumour microenvironment. Nat. Rev. Cancer. 2017;17:620–632. doi: 10.1038/nrc.2017.78. [DOI] [PubMed] [Google Scholar]
- 98.Kubli S.P., Bassi C., Roux C., Wakeham A., Gobl C., Zhou W., Jafari S.M., Snow B., Jones L., Palomero L., et al. AhR controls redox homeostasis and shapes the tumor microenvironment in BRCA1-associated breast cancer. Proc. Natl. Acad. Sci. USA. 2019;116:3604–3613. doi: 10.1073/pnas.1815126116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Weinberg F., Ramnath N., Nagrath D. Reactive Oxygen Species in the Tumor Microenvironment: An Overview. Cancers. 2019;11:1191. doi: 10.3390/cancers11081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Casey S.C., Amedei A., Aquilano K., Azmi A.S., Benencia F., Bhakta D., Bilsland A.E., Boosani C.S., Chen S., Ciriolo M.R., et al. Cancer prevention and therapy through the modulation of the tumor microenvironment. Semin. Cancer Biol. 2015;35:S199–S223. doi: 10.1016/j.semcancer.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Krejcik J., Casneuf T., Nijhof I.S., Verbist B., Bald J., Plesner T., Syed K., Liu K., van de Donk N.W., Weiss B.M., et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128:384–394. doi: 10.1182/blood-2015-12-687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.La Fleur L., Botling J., He F., Pelicano C., Zhou C., He C., Palano G., Mezheyeuski A., Micke P., Ravetch J.V., et al. Targeting MARCO and IL37R on Immunosuppressive Macrophages in Lung Cancer Blocks Regulatory T Cells and Supports Cytotoxic Lymphocyte Function. Cancer Res. 2021;81:956–967. doi: 10.1158/0008-5472.CAN-20-1885. [DOI] [PubMed] [Google Scholar]
- 103.Druzhkova I.N., Shirmanova M.V., Lukina M.M., Dudenkova V.V., Mishina N.M., Zagaynova E.V. The metabolic interaction of cancer cells and fibroblasts—coupling between NAD(P)H and FAD, intracellular pH and hydrogen peroxide. Cell Cycle. 2016;15:1257–1266. doi: 10.1080/15384101.2016.1160974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhu J., Thompson C.B. Metabolic regulation of cell growth and proliferation. Nat. Rev. Mol. Cell Biol. 2019;20:436–450. doi: 10.1038/s41580-019-0123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kastl L., Sauer S., Beissbarth T., Becker M., Krammer P., Gulow K. TNF-a stimulation enhances ROS-dependent cell migration via NF-?B activation in liver cells. Free Radic. Biol. Med. 2014;75((Suppl. S1)):S32. doi: 10.1016/j.freeradbiomed.2014.10.765. [DOI] [PubMed] [Google Scholar]
- 106.Li G., Liu D., Kimchi E.T., Kaifi J.T., Qi X., Manjunath Y., Liu X., Deering T., Avella D.M., Fox T., et al. Nanoliposome C6-Ceramide Increases the Anti-tumor Immune Response and Slows Growth of Liver Tumors in Mice. Gastroenterology. 2018;154:1024–1036.e1029. doi: 10.1053/j.gastro.2017.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bajor M., Zych A.O., Graczyk-Jarzynka A., Muchowicz A., Firczuk M., Trzeciak L., Gaj P., Domagala A., Siernicka M., Zagozdzon A., et al. Targeting peroxiredoxin 1 impairs growth of breast cancer cells and potently sensitises these cells to prooxidant agents. Br. J. Cancer. 2018;119:873–884. doi: 10.1038/s41416-018-0263-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schmidlin C.J., Shakya A., Dodson M., Chapman E., Zhang D.D. The intricacies of NRF2 regulation in cancer. Semin. Cancer Biol. 2021;76:110–119. doi: 10.1016/j.semcancer.2021.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Young M.R.I., Xiong Y. Influence of vitamin D on cancer risk and treatment: Why the variability? Trends Cancer Res. 2018;13:43–53. [PMC free article] [PubMed] [Google Scholar]
- 110.Bakalova R., Zhelev Z., Miller T., Aoki I., Higashi T. New potential biomarker for stratification of patients for pharmacological vitamin C in adjuvant settings of cancer therapy. Redox Biol. 2020;28:101357. doi: 10.1016/j.redox.2019.101357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liang S., Ma H.Y., Zhong Z., Dhar D., Liu X., Xu J., Koyama Y., Nishio T., Karin D., Karin G., et al. NADPH Oxidase 1 in Liver Macrophages Promotes Inflammation and Tumor Development in Mice. Gastroenterology. 2019;156:1156–1172.e1156. doi: 10.1053/j.gastro.2018.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Batinic-Haberle I., Tovmasyan A., Spasojevic I. Mn Porphyrin-Based Redox-Active Drugs: Differential Effects as Cancer Therapeutics and Protectors of Normal Tissue Against Oxidative Injury. Antioxid. Redox Signal. 2018;29:1691–1724. doi: 10.1089/ars.2017.7453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wu Z.Y., Kim H.J., Lee J.W., Chung I.Y., Kim J.S., Lee S.B., Son B.H., Eom J.S., Kim S.B., Gong G.Y., et al. Breast Cancer Recurrence in the Nipple-Areola Complex After Nipple-Sparing Mastectomy With Immediate Breast Reconstruction for Invasive Breast Cancer. JAMA Surg. 2019;154:1030–1037. doi: 10.1001/jamasurg.2019.2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wu J.H., Batist G. Glutathione and glutathione analogues; therapeutic potentials. Biochim. Biophys. Acta. 2013;1830:3350–3353. doi: 10.1016/j.bbagen.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 115.Yamamoto M., Kensler T.W., Motohashi H. The KEAP1-NRF2 System: A Thiol-Based Sensor-Effector Apparatus for Maintaining Redox Homeostasis. Physiol. Rev. 2018;98:1169–1203. doi: 10.1152/physrev.00023.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dodson M., Castro-Portuguez R., Zhang D.D. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107. doi: 10.1016/j.redox.2019.101107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mills E.L., Ryan D.G., Prag H.A., Dikovskaya D., Menon D., Zaslona Z., Jedrychowski M.P., Costa A.S.H., Higgins M., Hams E., et al. Itaconate is an anti-inflammatory metabolite that activates Nrf2 via alkylation of KEAP1. Nature. 2018;556:113–117. doi: 10.1038/nature25986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Eggler A.L., Liu G., Pezzuto J.M., van Breemen R.B., Mesecar A.D. Modifying specific cysteines of the electrophile-sensing human Keap1 protein is insufficient to disrupt binding to the Nrf2 domain Neh2. Proc. Natl. Acad. Sci. USA. 2005;102:10070–10075. doi: 10.1073/pnas.0502402102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shin J.W., Chun K.S., Kim D.H., Kim S.J., Kim S.H., Cho N.C., Na H.K., Surh Y.J. Curcumin induces stabilization of Nrf2 protein through Keap1 cysteine modification. Biochem. Pharmacol. 2020;173:113820. doi: 10.1016/j.bcp.2020.113820. [DOI] [PubMed] [Google Scholar]
- 120.Kerr F., Sofola-Adesakin O., Ivanov D.K., Gatliff J., Gomez Perez-Nievas B., Bertrand H.C., Martinez P., Callard R., Snoeren I., Cocheme H.M., et al. Direct Keap1-Nrf2 disruption as a potential therapeutic target for Alzheimer’s disease. PLoS Genet. 2017;13:e1006593. doi: 10.1371/journal.pgen.1006593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chowdhry S., Zhang Y., McMahon M., Sutherland C., Cuadrado A., Hayes J.D. Nrf2 is controlled by two distinct beta-TrCP recognition motifs in its Neh6 domain, one of which can be modulated by GSK-3 activity. Oncogene. 2013;32:3765–3781. doi: 10.1038/onc.2012.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Komatsu M., Kurokawa H., Waguri S., Taguchi K., Kobayashi A., Ichimura Y., Sou Y.S., Ueno I., Sakamoto A., Tong K.I., et al. The selective autophagy substrate p62 activates the stress responsive transcription factor Nrf2 through inactivation of Keap1. Nat. Cell Biol. 2010;12:213–223. doi: 10.1038/ncb2021. [DOI] [PubMed] [Google Scholar]
- 123.Covas G., Marinho H.S., Cyrne L., Antunes F. Activation of Nrf2 by H2O2: De novo synthesis versus nuclear translocation. Methods Enzymol. 2013;528:157–171. doi: 10.1016/B978-0-12-405881-1.00009-4. [DOI] [PubMed] [Google Scholar]
- 124.Casares L., Unciti-Broceta J.D., Prados M.E., Caprioglio D., Mattoteia D., Higgins M., Apendino G., Dinkova-Kostova A.T., Munoz E., de la Vega L. Isomeric O-methyl cannabidiolquinones with dual BACH1/NRF2 activity. Redox Biol. 2020;37:101689. doi: 10.1016/j.redox.2020.101689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mrowietz U., Morrison P.J., Suhrkamp I., Kumanova M., Clement B. The Pharmacokinetics of Fumaric Acid Esters Reveal Their In Vivo Effects. Trends Pharmacol. Sci. 2018;39:1–12. doi: 10.1016/j.tips.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 126.Belcher J.D., Chen C., Nguyen J., Zhang P., Abdulla F., Nguyen P., Killeen T., Xu P., O’Sullivan G., Nath K.A., et al. Control of Oxidative Stress and Inflammation in Sickle Cell Disease with the Nrf2 Activator Dimethyl Fumarate. Antioxid. Redox Signal. 2017;26:748–762. doi: 10.1089/ars.2015.6571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ahuja M., Ammal Kaidery N., Yang L., Calingasan N., Smirnova N., Gaisin A., Gaisina I.N., Gazaryan I., Hushpulian D.M., Kaddour-Djebbar I., et al. Distinct Nrf2 Signaling Mechanisms of Fumaric Acid Esters and Their Role in Neuroprotection against 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Induced Experimental Parkinson’s-Like Disease. J. Neurosci. 2016;36:6332–6351. doi: 10.1523/JNEUROSCI.0426-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Galloway D.A., Williams J.B., Moore C.S. Effects of fumarates on inflammatory human astrocyte responses and oligodendrocyte differentiation. Ann. Clin. Transl. Neurol. 2017;4:381–391. doi: 10.1002/acn3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Higashi C., Kawaji A., Tsuda N., Hayashi M., Saito R., Yagishita Y., Suzuki T., Uruno A., Nakamura M., Nakao K., et al. The novel Nrf2 inducer TFM-735 ameliorates experimental autoimmune encephalomyelitis in mice. Eur. J. Pharmacol. 2017;802:76–84. doi: 10.1016/j.ejphar.2017.02.044. [DOI] [PubMed] [Google Scholar]
- 130.Delmastro-Greenwood M., Hughan K.S., Vitturi D.A., Salvatore S.R., Grimes G., Potti G., Shiva S., Schopfer F.J., Gladwin M.T., Freeman B.A., et al. Nitrite and nitrate-dependent generation of anti-inflammatory fatty acid nitroalkenes. Free Radic. Biol. Med. 2015;89:333–341. doi: 10.1016/j.freeradbiomed.2015.07.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cuadrado A., Rojo A.I., Wells G., Hayes J.D., Cousin S.P., Rumsey W.L., Attucks O.C., Franklin S., Levonen A.L., Kensler T.W., et al. Therapeutic targeting of the NRF2 and KEAP1 partnership in chronic diseases. Nat. Rev. Drug Discov. 2019;18:295–317. doi: 10.1038/s41573-018-0008-x. [DOI] [PubMed] [Google Scholar]
- 132.Lu M.C., Zhao J., Liu Y.T., Liu T., Tao M.M., You Q.D., Jiang Z.Y. CPUY192018, a potent inhibitor of the Keap1-Nrf2 protein-protein interaction, alleviates renal inflammation in mice by restricting oxidative stress and NF-kappaB activation. Redox Biol. 2019;26:101266. doi: 10.1016/j.redox.2019.101266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moi P., Chan K., Asunis I., Cao A., Kan Y.W. Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the beta-globin locus control region. Proc. Natl. Acad. Sci. USA. 1994;91:9926–9930. doi: 10.1073/pnas.91.21.9926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lu M.C., Ji J.A., Jiang Y.L., Chen Z.Y., Yuan Z.W., You Q.D., Jiang Z.Y. An inhibitor of the Keap1-Nrf2 protein-protein interaction protects NCM460 colonic cells and alleviates experimental colitis. Sci. Rep. 2016;6:26585. doi: 10.1038/srep26585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hu L., Magesh S., Chen L., Wang L., Lewis T.A., Chen Y., Khodier C., Inoyama D., Beamer L.J., Emge T.J., et al. Discovery of a small-molecule inhibitor and cellular probe of Keap1-Nrf2 protein-protein interaction. Bioorg. Med. Chem. Lett. 2013;23:3039–3043. doi: 10.1016/j.bmcl.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Marcotte D., Zeng W., Hus J.C., McKenzie A., Hession C., Jin P., Bergeron C., Lugovskoy A., Enyedy I., Cuervo H., et al. Small molecules inhibit the interaction of Nrf2 and the Keap1 Kelch domain through a non-covalent mechanism. Bioorg. Med. Chem. 2013;21:4011–4019. doi: 10.1016/j.bmc.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 137.Lignitto L., LeBoeuf S.E., Homer H., Jiang S., Askenazi M., Karakousi T.R., Pass H.I., Bhutkar A.J., Tsirigos A., Ueberheide B., et al. Nrf2 Activation Promotes Lung Cancer Metastasis by Inhibiting the Degradation of Bach1. Cell. 2019;178:316–329e.318. doi: 10.1016/j.cell.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tossetta G., Fantone S., Montanari E., Marzioni D., Goteri G. Role of NRF2 in Ovarian Cancer. Antioxidants. 2022;11:663. doi: 10.3390/antiox11040663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Barrera G., Cucci M.A., Grattarola M., Dianzani C., Muzio G., Pizzimenti S. Control of Oxidative Stress in Cancer Chemoresistance: Spotlight on Nrf2 Role. Antioxidants. 2021;10:510. doi: 10.3390/antiox10040510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Pedre B., Barayeu U., Ezerina D., Dick T.P. The mechanism of action of N-acetylcysteine (NAC): The emerging role of H2S and sulfane sulfur species. Pharmacol. Ther. 2021;228:107916. doi: 10.1016/j.pharmthera.2021.107916. [DOI] [PubMed] [Google Scholar]
- 141.Pilewskie M., Morrow M. Axillary Nodal Management Following Neoadjuvant Chemotherapy: A Review. JAMA Oncol. 2017;3:549–555. doi: 10.1001/jamaoncol.2016.4163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Piskounova E., Agathocleous M., Murphy M.M., Hu Z., Huddlestun S.E., Zhao Z., Leitch A.M., Johnson T.M., DeBerardinis R.J., Morrison S.J. Oxidative stress inhibits distant metastasis by human melanoma cells. Nature. 2015;527:186–191. doi: 10.1038/nature15726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cacciatore I., Cornacchia C., Pinnen F., Mollica A., Di Stefano A. Prodrug approach for increasing cellular glutathione levels. Molecules. 2010;15:1242–1264. doi: 10.3390/molecules15031242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Puri R.N., Meister A. Transport of glutathione, as gamma-glutamylcysteinylglycyl ester, into liver and kidney. Proc. Natl. Acad. Sci. USA. 1983;80:5258–5260. doi: 10.1073/pnas.80.17.5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gomes-Neto J.C., Round J.L. Gut microbiota: A new way to take your vitamins. Nat. Rev. Gastroenterol. Hepatol. 2018;15:521–522. doi: 10.1038/s41575-018-0044-3. [DOI] [PubMed] [Google Scholar]
- 146.Said H.M., Nexo E. Gastrointestinal Handling of Water-Soluble Vitamins. Compr. Physiol. 2018;8:1291–1311. doi: 10.1002/cphy.c170054. [DOI] [PubMed] [Google Scholar]
- 147.Cossey L.N., Rahim F., Larsen C.P. Oxalate nephropathy and intravenous vitamin C. Am. J. Kidney Dis. 2013;61:1032–1035. doi: 10.1053/j.ajkd.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 148.Mikirova N., Casciari J., Rogers A., Taylor P. Effect of high-dose intravenous vitamin C on inflammation in cancer patients. J. Transl. Med. 2012;10:189. doi: 10.1186/1479-5876-10-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yun J., Mullarky E., Lu C., Bosch K.N., Kavalier A., Rivera K., Roper J., Chio I.I., Giannopoulou E.G., Rago C., et al. Vitamin C selectively kills KRAS and BRAF mutant colorectal cancer cells by targeting GAPDH. Science. 2015;350:1391–1396. doi: 10.1126/science.aaa5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Harris H.R., Orsini N., Wolk A. Vitamin C and survival among women with breast cancer: A meta-analysis. Eur. J. Cancer. 2014;50:1223–1231. doi: 10.1016/j.ejca.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 151.Carr A.C., Cook J. Intravenous Vitamin C for Cancer Therapy—Identifying the Current Gaps in Our Knowledge. Front. Physiol. 2018;9:1182. doi: 10.3389/fphys.2018.01182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Creagan E.T., Moertel C.G., O’Fallon J.R., Schutt A.J., O’Connell M.J., Rubin J., Frytak S. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N. Engl. J. Med. 1979;301:687–690. doi: 10.1056/NEJM197909273011303. [DOI] [PubMed] [Google Scholar]
- 153.Moertel C.G., Fleming T.R., Creagan E.T., Rubin J., O’Connell M.J., Ames M.M. High-dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomized double-blind comparison. N. Engl. J. Med. 1985;312:137–141. doi: 10.1056/NEJM198501173120301. [DOI] [PubMed] [Google Scholar]
- 154.Niki E. Role of vitamin E as a lipid-soluble peroxyl radical scavenger: In vitro and in vivo evidence. Free Radic. Biol. Med. 2014;66:3–12. doi: 10.1016/j.freeradbiomed.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 155.Sauberlich H.E. Pharmacology of vitamin C. Annu. Rev. Nutr. 1994;14:371–391. doi: 10.1146/annurev.nu.14.070194.002103. [DOI] [PubMed] [Google Scholar]
- 156.Yang C.S., Suh N., Kong A.N. Does vitamin E prevent or promote cancer? Cancer Prev. Res. 2012;5:701–705. doi: 10.1158/1940-6207.CAPR-12-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Konate M.M., Antony S., Doroshow J.H. Inhibiting the Activity of NADPH Oxidase in Cancer. Antioxid. Redox Signal. 2020;33:435–454. doi: 10.1089/ars.2020.8046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Cifuentes-Pagano M.E., Meijles D.N., Pagano P.J. Nox Inhibitors & Therapies: Rational Design of Peptidic and Small Molecule Inhibitors. Curr. Pharm. Des. 2015;21:6023–6035. doi: 10.2174/1381612821666151029112013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cifuentes-Pagano E., Csanyi G., Pagano P.J. NADPH oxidase inhibitors: A decade of discovery from Nox2ds to HTS. Cell Mol. Life Sci. 2012;69:2315–2325. doi: 10.1007/s00018-012-1009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Altenhofer S., Radermacher K.A., Kleikers P.W., Wingler K., Schmidt H.H. Evolution of NADPH Oxidase Inhibitors: Selectivity and Mechanisms for Target Engagement. Antioxid. Redox Signal. 2015;23:406–427. doi: 10.1089/ars.2013.5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.DiStasi M.R., Mund J.A., Bohlen H.G., Miller S.J., Ingram D.A., Dalsing M.C., Unthank J.L. Impaired compensation to femoral artery ligation in diet-induced obese mice is primarily mediated via suppression of collateral growth by Nox2 and p47phox. Am. J. Physiol. Heart Circ. Physiol. 2015;309:H1207–H1217. doi: 10.1152/ajpheart.00180.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Krotz F., Sohn H.Y., Gloe T., Zahler S., Riexinger T., Schiele T.M., Becker B.F., Theisen K., Klauss V., Pohl U. NAD(P)H oxidase-dependent platelet superoxide anion release increases platelet recruitment. Blood. 2002;100:917–924. doi: 10.1182/blood.V100.3.917. [DOI] [PubMed] [Google Scholar]
- 163.Ebrahimian T., Li M.W., Lemarie C.A., Simeone S.M., Pagano P.J., Gaestel M., Paradis P., Wassmann S., Schiffrin E.L. Mitogen-activated protein kinase-activated protein kinase 2 in angiotensin II-induced inflammation and hypertension: Regulation of oxidative stress. Hypertension. 2011;57:245–254. doi: 10.1161/HYPERTENSIONAHA.110.159889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hou L., Zhang L., Hong J.S., Zhang D., Zhao J., Wang Q. Nicotinamide Adenine Dinucleotide Phosphate Oxidase and Neurodegenerative Diseases: Mechanisms and Therapy. Antioxid. Redox Signal. 2020;33:374–393. doi: 10.1089/ars.2019.8014. [DOI] [PubMed] [Google Scholar]
- 165.Doroshow J.H., Gaur S., Markel S., Lu J., van Balgooy J., Synold T.W., Xi B., Wu X., Juhasz A. Effects of iodonium-class flavin dehydrogenase inhibitors on growth, reactive oxygen production, cell cycle progression, NADPH oxidase 1 levels, and gene expression in human colon cancer cells and xenografts. Free Radic. Biol. Med. 2013;57:162–175. doi: 10.1016/j.freeradbiomed.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Schroder K. NADPH oxidases: Current aspects and tools. Redox Biol. 2020;34:101512. doi: 10.1016/j.redox.2020.101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Mora-Pale M., Kwon S.J., Linhardt R.J., Dordick J.S. Trimer hydroxylated quinone derived from apocynin targets cysteine residues of p47phox preventing the activation of human vascular NADPH oxidase. Free Radic. Biol. Med. 2012;52:962–969. doi: 10.1016/j.freeradbiomed.2011.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Murley J.S., Arbiser J.L., Weichselbaum R.R., Grdina D.J. ROS modifiers and NOX4 affect the expression of the survivin-associated radio-adaptive response. Free Radic. Biol. Med. 2018;123:39–52. doi: 10.1016/j.freeradbiomed.2018.04.547. [DOI] [PubMed] [Google Scholar]
- 169.Bhandarkar S.S., Jaconi M., Fried L.E., Bonner M.Y., Lefkove B., Govindarajan B., Perry B.N., Parhar R., Mackelfresh J., Sohn A., et al. Fulvene-5 potently inhibits NADPH oxidase 4 and blocks the growth of endothelial tumors in mice. J. Clin. Investig. 2009;119:2359–2365. doi: 10.1172/JCI33877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Cao F., Zhang L., You Y., Zheng L., Ren J., Qu X. An Enzyme-Mimicking Single-Atom Catalyst as an Efficient Multiple Reactive Oxygen and Nitrogen Species Scavenger for Sepsis Management. Angew. Chem. Int. Ed. Engl. 2020;59:5108–5115. doi: 10.1002/anie.201912182. [DOI] [PubMed] [Google Scholar]
- 171.Carillon J., Rouanet J.M., Cristol J.P., Brion R. Superoxide dismutase administration, a potential therapy against oxidative stress related diseases: Several routes of supplementation and proposal of an original mechanism of action. Pharm. Res. 2013;30:2718–2728. doi: 10.1007/s11095-013-1113-5. [DOI] [PubMed] [Google Scholar]
- 172.Johnke R.M., Sattler J.A., Allison R.R. Radioprotective agents for radiation therapy: Future trends. Future Oncol. 2014;10:2345–2357. doi: 10.2217/fon.14.175. [DOI] [PubMed] [Google Scholar]
- 173.Weitner T., Kos I., Sheng H., Tovmasyan A., Reboucas J.S., Fan P., Warner D.S., Vujaskovic Z., Batinic-Haberle I., Spasojevic I. Comprehensive pharmacokinetic studies and oral bioavailability of two Mn porphyrin-based SOD mimics, MnTE-2-PyP5+ and MnTnHex-2-PyP5+ Free Radic. Biol. Med. 2013;58:73–80. doi: 10.1016/j.freeradbiomed.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tovmasyan A., Reboucas J.S., Benov L. Simple biological systems for assessing the activity of superoxide dismutase mimics. Antioxid. Redox Signal. 2014;20:2416–2436. doi: 10.1089/ars.2013.5576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bonetta R. Potential Therapeutic Applications of MnSODs and SOD-Mimetics. Chemistry. 2018;24:5032–5041. doi: 10.1002/chem.201704561. [DOI] [PubMed] [Google Scholar]
- 176.Sherlock L.G., Trumpie A., Hernandez-Lagunas L., McKenna S., Fisher S., Bowler R., Wright C.J., Delaney C., Nozik-Grayck E. Redistribution of Extracellular Superoxide Dismutase Causes Neonatal Pulmonary Vascular Remodeling and PH but Protects Against Experimental Bronchopulmonary Dysplasia. Antioxidants. 2018;7:42. doi: 10.3390/antiox7030042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chatterjee A., Zhu Y., Tong Q., Kosmacek E.A., Lichter E.Z., Oberley-Deegan R.E. The Addition of Manganese Porphyrins during Radiation Inhibits Prostate Cancer Growth and Simultaneously Protects Normal Prostate Tissue from Radiation Damage. Antioxidants. 2018;7:21. doi: 10.3390/antiox7010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Batinic-Haberle I., Tovmasyan A., Roberts E.R., Vujaskovic Z., Leong K.W., Spasojevic I. SOD therapeutics: Latest insights into their structure-activity relationships and impact on the cellular redox-based signaling pathways. Antioxid. Redox Signal. 2014;20:2372–2415. doi: 10.1089/ars.2012.5147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sishc B.J., Ding L., Nam T.K., Heer C.D., Rodman S.N., Schoenfeld J.D., Fath M.A., Saha D., Pulliam C.F., Langen B., et al. Avasopasem manganese synergizes with hypofractionated radiation to ablate tumors through the generation of hydrogen peroxide. Sci. Transl. Med. 2021;13:eabb3768. doi: 10.1126/scitranslmed.abb3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Heer C.D., Davis A.B., Riffe D.B., Wagner B.A., Falls K.C., Allen B.G., Buettner G.R., Beardsley R.A., Riley D.P., Spitz D.R. Superoxide Dismutase Mimetic GC4419 Enhances the Oxidation of Pharmacological Ascorbate and Its Anticancer Effects in an H(2)O(2)-Dependent Manner. Antioxidants. 2018;7:18. doi: 10.3390/antiox7010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.El-Mahdy M.A., Alzarie Y.A., Hemann C., Badary O.A., Nofal S., Zweier J.L. The novel SOD mimetic GC4419 increases cancer cell killing with sensitization to ionizing radiation while protecting normal cells. Free Radic. Biol. Med. 2020;160:630–642. doi: 10.1016/j.freeradbiomed.2020.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Asadi Z., Mandegani Z., Asadi M., Pakiari A.H., Salarhaji M., Manassir M., Karbalaei-Heidari H.R., Rastegari B., Sedaghat M. Substituted effect on some water-soluble Mn(II) salen complexes: DNA binding, cytotoxicity, molecular docking, DFT studies and theoretical IR & UV studies. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2019;206:278–294. doi: 10.1016/j.saa.2018.08.020. [DOI] [PubMed] [Google Scholar]