Abstract
In the lungs, fibrosis is a growing clinical problem that results in shortness of breath and can end up in respiratory failure. Even though the main fibrotic disease affecting the lung is idiopathic pulmonary fibrosis (IPF), which affects the interstitial space, there are many fibrotic events that have high and dangerous consequences for the lungs. Asthma, chronic obstructive pulmonary disease (COPD), excessive allergies, clearance of infection or COVID-19, all are frequent diseases that show lung fibrosis. In this review, we describe the different kinds of fibrosis and analyse the main types of cells involved—myofibroblasts and other cells, like macrophages—and review the main fibrotic mechanisms. Finally, we analyse present treatments for fibrosis in the lungs and highlight potential targets for anti-fibrotic therapies.
Keywords: pulmonary fibrosis, myofibroblast, macrophages, secretome, EMT, endoMT, TGF-β
1. What Is Lung Fibrosis?
The adult lung is one of the few organs that comes in direct contact with the outside environment. In that sense, the single layer of respiratory epithelial cells that lines the airways is constantly exposed to potentially toxic agents and pathogens and therefore is in constant communication with the mucosal immune system. For that reason, it must be able to respond quickly and effectively to repair cellular damage. The interaction between the epithelium and the other cell types in the lungs is thus crucial, and when dysregulated, produces pathological processes in a wide range of respiratory conditions, including fibrosis.
Lung fibrosis can be defined as the aberrant activation and differentiation of lung fibroblasts to myofibroblasts, persistent alveolar injury, exuberant extracellular matrix (ECM) deposition, and incomplete repair that over time can lead to progressive loss of respiratory function and death. According to the World Health Organization (WHO), the top-three causes of death worldwide in descending order are associated with cardiovascular, respiratory, and neonatal conditions (https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 9 December 2020)). Lower respiratory diseases rank fourth. As defined by the U.S. Centers for Disease Control and Prevention (CDC) and the WHO, chronic lower respiratory disease (CLRD) encompasses four major diseases: chronic obstructive pulmonary disease (COPD), chronic bronchitis, emphysema, and asthma [1,2]. Three of these are involved in the appearance of fibrosis in the lungs although the cell subsets and the mechanisms involved in the development of fibrotic events may differ. In that sense, asthma, COPD, and idiopathic pulmonary fibrosis (IPF) are categorised as severe multifactorial lung diseases that have the common feature of lung remodelling in morphologically distinct compartments, notably the large or small airways and parenchyma [3]. Likewise, innate and adaptive immune cells are fundamental for protection. Understanding the complex composition of cells—not only differentiated myofibroblasts but also fibroblasts, endothelial and epithelial cells, and innate and adaptive immune cells—and extracellular matrix (ECM) components such as collagen and fibronectin is important for understanding the different fibrotic events that can occur. Among the different cells, we emphasize the role of macrophages, as they have been shown to activate myofibroblasts, the main source of the extracellular matrix in fibrotic diseases.
2. Myofibroblasts in the Lung
The respiratory tract is a complex organ, that can be differentiated into upper and lower airways. The upper respiratory tract includes the nose and nasal passages, pharynx, and larynx. The lower respiratory tract comprises the trachea, bronchi, and bronchioles, the conducting airways where respiration occurs. They include respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. The respiratory system is not only formed by epithelial cells but is also lined with cells from the circulatory system, resident lung cells (including immune cells) and mesenchymal cells. These are all connected thanks to the ECM.
In this scenario, myofibroblasts play an important role during tissue repair. They show an increased contractibility, hence their role in closing open wounds. However, they are the main source of ECM components, and when dysregulated, they secrete excessive amounts of ECM proteins, which alters the normal structure of the respiratory airways, eventually disrupting normal lung physiology [4].
Myofibroblasts were first described in ultrastructural examinations of rat wounds [5]. In the first description, Gabbiani et al. characterized the presence of modified fibroblasts in the granulation tissue of wounds [6]. They are large cells with ruffled membranes, and they exhibit cytoplasmic stress fibres, such as those found in contractile smooth muscle cells, along with peripheral focal adhesions [4].
The origin of these myofibroblasts is still a matter of debate, meaning that its identification would be a step toward understanding of the mechanisms responsible for fibrosis, which may lead to the discovery of new therapeutic targets for different fibrotic processes in the lung.
The contribution of resident mesenchymal populations has been broadly accepted [7,8]; moreover, immune cells, especially resident macrophages, play a major role in the activation and differentiation of myofibroblasts, which is extensively described in this review. Moreover, signals produced in response to inflammation or mechanical stresses can also trigger processes involved in the epithelial–mesenchymal transition (EMT) and endothelial–mesenchymal transition (EndoMT). Finally, we cannot forget the contribution from other cellular populations, like pericytes or fibrocytes, or the inherent biochemical and physical properties of the ECM componentsFinally, although the activation or differentiation into myofibroblasts may represent the final stage in remodelling, some authors have raised the possibility that myofibroblasts may represent a functional population.
The main cell types that both differentiate into, or activate, myofibroblasts in the lung are described in the next sections, which focus not only on their involvement in myofibroblast activation but also on the importance of these cells per se in different fibrotic processes that in lung disease.
2.1. Epithelial Cells
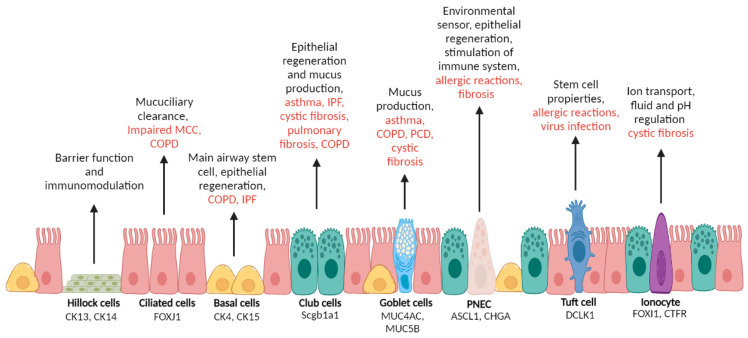
Single-cell RNA sequencing (scRNA-seq) has changed the information we have about the layer of different cells that covers the surface of the airways [9,10]. Although not the focus of this review, we summarize here and in Figure 1 the main cells found in the respiratory epithelium. Although some authors doubt that epithelial cells serve as progenitors of myofibroblasts, we believe there is enough evidence to claim that the epithelial-to-mesenchymal transition (EMT) explains myofibroblast differentiation. Moreover, there is considerable evidence showing that cells of epithelial origin contribute to fibrotic lesions and other respiratory diseases. Four main cells—basal, club, goblet and ciliated—line the conduction airways.
Figure 1.
Schematic representation of epithelial cells lining the airways. Cell names are shown in bold together with the main expressed cell markers. The figure also shows the principal known cell role and in red their related respiratory diseases. This figure was created with Biorender (www.biorender.com (accessed on 1 May 2022)).
Basal cells are the progenitors of the airway epithelium. They can self-renew after injury and differentiate into other important cell types: club, goblet, and ciliated; pulmonary ionocytes; pulmonary neuroendocrine cells (PNECs); and tuft cells [11,12,13]. They have a cuboidal shape and they are attached to the basement membrane. In the human lung, they express cytokeratin 5 and 14 as well as many other markers [12,13]. Basal cell expansion is a common feature of epithelial remodelling in IPF and other chronic lung diseases.
Club cells were previously known as Clara cells, a term that the scientific community should have avoided as it reflects their discovery by a Nazi military doctor. These cells have a dome shape and are the main cell type in respiratory bronchioles [14]. Club cells are commonly characterized by the expression of Scgb1a1 [15], and like basal cells, also behave as stem cells and aid in epithelial repair [16]. The dysregulation of club cells contributes to many respiratory conditions, including asthma, IPF, cystic fibrosis, pulmonary fibrosis or COPD [17,18].
Goblet cells are present in airway lining and secrete a gel-forming mucus [19]. Together with ciliated cells, they facilitate effective mucus clearance by expressing mucins, mainly MUC5AC and MUC5B. Increased mucus production by Goblet cells is a typical feature of many respiratory diseases, including asthma, COPD, primary cilia dyskinesia (PCD) or cystic fibrosis (CF) [9,20].
Ciliated cells are columnar cells that are found throughout the airways. They play a pivotal role in airway homeostasis and together with the airway mucus mediate the critical mucociliary clearance (MCC) of inhaled particles and pathogens [21]. Chronic lung disorders are characterised by impaired MCC. For example, it has been shown that smoking shortens the size of the cilia. COPD patients also show a significant decrease in the number of ciliated cells [22,23,24].
Basal, club, goblet and ciliated cells are the main ones in the lining of the conducting airways and the most involved in the EMT, which produces myofibroblasts. Apart from these, other epithelial cells are also present in the airways but in a very low proportion. However, they include PNECs, which behave as stem cells [22] and have been involved in inducing the proliferation and migration of fibroblasts [25] or other minority cells, such as tuft cells, ionocytes or Hillock cells (see Figure 1).
The main known function of PNECs is to serve as a key element in the crosstalk between the immune and the nervous systems [14]. They sense airway activity and secrete neuropeptides (serotonin, calcitonin gene-related peptide) to stimulate immune responses [26,27]. Tuft cells have been described in both the gastrointestinal tract [28] nose, trachea, and proximal airways, but their role in the lungs is less clear, so evidence implicating them in respiratory disease is limited [29,30]; however, it has been suggested that they decrease the effects produced by an airway allergic reaction. Rane et al. also demonstrated that they develop in the lung after a severe influenza injury [31]. Pulmonary ionocytes express CF transmembrane conductance regulator (CFTR) and forkhead box I1 (FOXI1) [32,33], and because of that there is a hope that they could be used to develop a CF treatment [29]. Finally, there is not much information about hillock cells; in fact, it is not apparent that they are present along the whole respiratory tract. They were first described by Montoro et al., as a different kind of club cell that express keratin 13 [32]. They are normally found in groups that form structures that resemble small hills, hence their name. Their function is not clear, but it is known that they have a particularly high turnover rate [29] and express high levels of Ki67 [9].
Alveolar type I and II cells: Pulmonary alveolar type I (AT1) cells cover the great majority of the alveolar surface. They are essential for alveolar regeneration and are in charge of the air–blood barrier function. However, it is definitively the AT2 population that is more involved in fibrosis, especially IPF. In that sense, there are numerous studies showing that AT2 injury or malfunction triggers IPF. As a consequence, fibroblast proliferation increases as it does paracrine signalling to myofibroblasts, the production of other pro-fibrotic factors, and the development of fibrotic processes [25], leading to the progressive loss of lung function [26,27]. Moreover, constant damage to these cells produces impaired repair function. In that sense, AT2 cells in fibrotic lesions soon become hypertrophic and hyperplastic [28].
2.2. Endothelial Cells
The main process by which endothelial cells differentiate into myofibroblasts is via endothelial–mesenchymal transition (EndoMT). This process shares many characteristics with the EMT, and in fact has been described as a different kind of EMT. The EndoMT is characterised by the loss of typical endothelial markers such as CD31/PECAM-1 (platelet EC adhesion molecule-1), Tie1, Tie2, VE-cadherin and von Willebrand Factor (vWF); and the expression of mesenchymal markers such as such as α-SMA, N-cadherin and vimentin [29]. Recently, Kovacic et al. [30] reviewed the signalling pathways controlling EndoMT and found that transforming growth factor beta (TGF-β) was one of the main ones.
Apart from this, endothelial cells also contribute to fibrosis by producing profibrotic molecules as well as chemokines and cytokines that recruit immune cells that contribute to inflammation of the fibrotic foci. In the lung, pulmonary capillary endothelial cells, through EndoMT, may serve as a source of fibroblasts in pulmonary fibrosis [31].
2.3. Resident Mesenchymal Cells: Fibroblasts
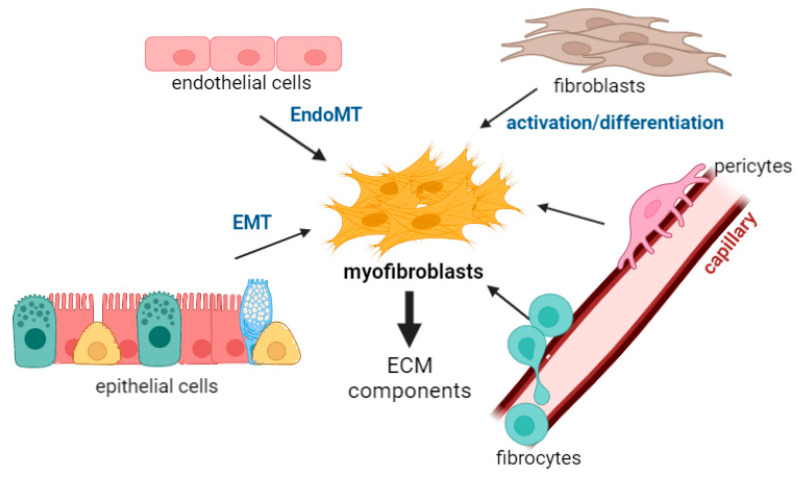
Fibroblasts play a major role in the process of fibrosis in the lungs as they are responsible for the production and homeostasis of the ECM. Therefore, they modify the composition and the properties of the ECM and, very importantly, differentiate into myofibroblasts, one of the main cell types associated with the development of fibrotic tissue [32]. Fibroblasts are regulated by different molecules: they can be influenced by ECM components and other molecules present in the matrix, such as receptors, cytokines, chemokines, and growth factors. Among these, TGF-β, is the main cytokine that stimulates fibroblasts to produce ECM constituents (see part 4). However, molecules such as interferon-gamma (IFN-γ) or tumour necrosis factor (TNF) [33,34,35,36,37,38] also act as fibroblast inhibitors. As shown in Figure 2 and part 4, fibroblasts are one of the major sources of myofibroblasts under pathological conditions when ECM turnover is altered and fibrosis is found in the bronchi and bronchioles [33,39,40,41,42].
Figure 2.
The diagram shows the proposed origin of myofibroblasts: (i) The main myofibroblasts progenitor after injury of different tissues seems to be locally residing fibroblasts, which differentiate into myofibroblasts. (ii) Epithelial and endothelial cells undergo transdifferentiation to form myofibroblasts by epithelial–mesenchymal transition (EMT) or endothelial–mesenchymal transition (EndoMT). (iii) bone marrow-derived precursor cells such as fibrocytes may also differentiate to form myofibroblasts. (iv) pericytes can also differentiate to myofibroblasts. In a normal repair process, excess myofibroblasts undergo regulated apoptosis, but in fibrosis, uncontrolled proliferation of myofibroblasts, along with excess deposition of the ECM, results in structural remodelling that leads to scar lesions, loss of alveolar function, and respiratory failure. This figure was created with BioRender (www.biorender.com (accessed on 1 May 2022)).
2.4. Bone Marrow/Derived Precursors: Fibrocytes
Fibrocytes have also been observed in human fibrotic lung disease. They are spindle-shaped mesenchymal progenitor cells that were first described by Bucala et al. [43]. They express markers such as Col-1 and CD45 [44] and have been described in fibrotic disorders not only in the lung but also in other organs. These cells respond to signals and transmigrate to damaged sites where they differentiate into myofibroblasts [45]. It has been proposed that this happens through factors such as interleukin-31 or stem cell factor (SCF) [46]. In vitro, TGF-β stimulated fibrocytes in monolayers that then differentiate into cells expressing α-SMA and causing contraction of collagen gels [47].
Apart from this role in differentiation, they also produce ECM components, such as collagen I and III, vimentin and fibronectin [48]. Another mechanism by which fibrocytes may indirectly influence fibroblastic behaviour in resident cells is by the release of exosomes [4]. Finally, fibrocytes are thought to activate fibroblasts or inherently participate in inflammation, which of course, leads to ECM remodelling and fibrosis [49,50].
Fibrocytes have been described in patients with IPF, specifically in the fibrotic lesions [51]. Moreover, there is an increase of the concentration of fibrocytes in IPF patients, which has been shown to be a sign of poor prognosis [52].
It is important to note that, as Byrne et al. stated, it is not very clear whether fibrocytes represent a distinct, fibroblast-precursor lineage or are (as is more likely) a subset of monocyte-derived macrophages, which again underlining the extent of macrophage plasticity [53].
2.5. Perivascular Stromal Origin: Pericytes
Lung pericytes are mesenchymal-derived cells in the basement membrane of capillaries that have been shown to add structural support to small vessels, as well as control vascular tone. They also produce molecules that promote angiogenesis and components of the ECM [54]. In fact, the loss of pericytes in the alveolar capillaries has been associated with lung fibrosis. Lung pericytes are also capable of responding to danger signals and amplifying the inflammatory response through the elaboration of cytokines and adhesion molecules [4].
The first paper describing pericyte involvement in myofibroblasts differentiation was by Göritz et al. [55], in which they described pericyte function in wound healing in the central nervous system. In the lung, Hung et al. [56] used the bleomycin model to demonstrate that pericytes are present in fibrotic lesions.
3. Role of Macrophages in Myofibroblasts Differentiation and Activation
If there is one immune population that is important to highlight in the different processes of fibrosis in the lungs, it is macrophages. To start with, they are versatile cells that exhibit a high degree of plasticity. When the lung is injured, macrophages are pushed towards a pro-inflammatory phenotype that promotes differentiation and activation of myofibroblasts. Macrophages are the main innate immune cells in the healthy lung and have many functions: immune surveillance, cellular debris removal, microbe clearance, inflammation resolution, and repair [57]. In addition, they localize close to myofibroblasts, which are considered the major ECM source during fibrosis [58]. Moreover, an elevated expression of macrophage-derived molecules has been found in fibrotic lungs [59].
As will be described in Table 1, macrophages secrete many different molecules important for the development of fibrosis. Moreover, as we have learned so far, myofibroblasts are thought to come from many different progenitor cells. Macrophage–myofibroblast transition (MMT) is a recent term that describes the mechanism by which macrophages derived from bone marrow-derived monocytes transform into myofibroblasts, contributing to fibrosis [60]. This has been described mainly in kidney fibrosis [60,61] but also very recently in the lung [62]. The molecular mechanism that controls the MMT is still unknown, but the idea of this differentiation opens a new avenue that could bring valid targets and provide insight into the development of novel antifibrotic therapies.
Table 1.
Macrophages derived secretory proteins and fibrosis in the lungs: the macrophage secretome.
| Secretome Molecules | Macrophage Type | Study Subject | Role in Fibrosis | Reference |
|---|---|---|---|---|
| KC | Monocyte-derived AMs | LPS stimulation | Increase proliferation of ECM components | [69,77] |
| type IV collagenase | AMs | BLM-induced fibrosis mice model | Abnormal collagen degradation | [78,79] |
| MMP-1 | lung macrophages | IPF, COVID-19 | Role in IPF presently unknown. Present in early fibrotic processes in COVID-19 patients | [26,80] |
| MMP-2 | lung macrophages | IPF | Effect on fibrocytes: Tissue migration and homing | [81] |
| MMP-3 | AMs | IPF patients, lung | Induction of epithelial-mesenchymal transition through activation of β-catenin signaling | [82] |
| MMP-7 | lung macrophages | IPF, COVID-19 | Effect on AEC2 cells. Present in early fibrotic processes in COVID-19 patients | [26,80] |
| MMP-8 | lung macrophages | IPF patients, lung | Effect on fibrocytes: Tissue migration and homing. Initiation of collagen destruction and remodelling | [81,83,84] |
| MMP9 | AMs IMs |
BLM-induced fibrosis mice model IPF patients, lung |
Degradation and remodeling of extracellular matrix components | [78,84,85] |
| MMP-12 | macrophages | LPS stimulation | Effect on TGF-β1 signaling pathway activation | [86,87] |
| MMP-13 | Monocyte-derived macrophages e. | Lung fibrosis | Cleaves fibrillar collagens. Specific role largely unknown. | [76,87,88] |
| Periostin | lung macrophages | IPF, COVID-19 | Present in early fibrotic processes in COVID-19 patients | [80] |
| TIMP1 | IMs | IPF patients, lung | Promotes the fibrotic response | [89] |
| MT1-MMP | macrophages | IAV sensing | ECM remodelling through collagenase activity | [90] |
| CCL18 | AMs | Pulmonary fibrosis | Increases collagen production | [91] |
| IFNβ | AMs | IAV sensing | Not specified | [92] |
| IFNγ, | M1 macrophages macrophage |
Lung injury | Macrophage polarization | [93] |
| TGF-β1 | M2 macrophages, AM | Lung fibrosis, BLM-induced fibrosis mice model, COPD patients | Differentiation of fibroblasts into myofibroblasts. EMT transition through the TGF-Smad2 signalling pathway | [76,94,95] |
| TNFα | AM, M1 macrophages | COPD patients, enhanced lung injury, BLM-induced fibrosis mice model | Initiates inflammation and enhaces lung injury. Induces M1 macrophages to produce proinflammatory cytokines | [76,94,96] |
| PDGF | primary macrophages | inflammatory process, Lung injury, lung fibrosis | Promotes de fibrotic process | [76,97] |
| VEGF | primary macrophages | inflammatory process, Lung injury | Promotes blood vessel development and cellular proliferation | [76,98] |
| IGF-1 | primary macrophages | inflammatory process, Lung injury | Promotes blood vessel development and cellular proliferation | [76] |
| amphiregulin | primary macrophages, AM | inflammatory process, LPS stimulation, Lung injury |
Contributes to immune regulation, Protects lung tissues. Counteracts epithelial damage. Enhances EGFR signalling and proliferative responses. | [99,100,101] |
| CCL2 | macrophages | BLM-induced fibrosis mice model, IPF patients, BALF | Cellular recruitment to the lung. Enhancement of cytokine and collagen production. | [102,103] |
| CCL24 | macrophages | BLM-induced fibrosis mice model. IPF patients, BALF |
Not specified. | [102,103] |
| arginase 1 | Monocyte-derived macrophages | Lung fibrosis | Effect on collagen synthesis | [76,104] |
| IL-4 | M2 macrophages | Lung fibrosis | ||
| IL-6 | AM, M1 macrophages | Viral infection, enhanced lung injury | Promotes macrophages recruitment to the lung | [76,105] |
| IL-8 | AM | COPD patients | Promotes neutrophil recrutiment | [94] |
| IL-10 | M2 macrophages | Lung fibrosis | Induces reprogramming of macrophages to the M2 phenotype. Enhances tissue repair and promotes matrix synthesis. | [76] |
| IL-12 | M1 macrophages | Lung injury | Not specified | [93] |
| IL-1β | IMs, AMs | Uninjured lung, IPF patients, lung | Triggers the activation, proliferation and transdifferentiation of epithelia cells and resident fibroblasts into myofibroblasts. Stimulates the secretion of neutrophil-attracting CXC chemokines. | [101] |
| IL-18 | AMs | IPF patients, lung | Not specified | [106] |
Abbreviations: TNF-α: Tumour necrosis factor-α; IFN-γ: Interferon-γ; LPS: Lipopolysaccharide; IL: interleukin; PDGF: platelet-derived growth factor; VEGF: vascular endothelial growth factor; IGF-1: insulin-like growth factor 1; KC: keratinocyte chemokine; MMP: Metalloproteinase; TIMP-1: Metalloproteinase Inhibitor-1; TGF-β1: Transforming growth factor 1; IPF: Idiopathic pulmonary fibrosis; COPD: Chronic obstructive pulmonary disease; BLM: Bleomicin; BALF: Bronchoalveolar lavage fluid; AM: Alveolar macrophage; IM: Interstitial macrophage; IAV: Influenza A virus; EMT: Epithelial to mesenchymal transition; ECM: Extracellular matrix.
There are two major macrophage subsets: alveolar macrophage (AM), and interstitial macrophage (IM). A potential third subset found in airway lumen, airway macrophages, has also been proposed and may be discovered in airways diseases such as asthma [63] or in allergic-airway mice models [64]. In that sense, Tamò et al. suggested that lung stem cells could contribute to the appearance of a new subpopulation of macrophages after fibrosis in the lungs or a repetitive injury [65].
In a healthy lung, AMs are present in larger numbers than IMs (up to eight-fold) in digested murine lungs according to Gibbing et al. [66]. Even though both types present bona fide macrophages markers, (e.g., CD64 or F4/80, CD68, Lamp1, Lysozyme 2 or CD36) [67], they also express different markers, as was very well summarized in a recent review by Shi et al. Apart from this difference in surface markers, both kinds of macrophage are also be differentiated by key transcription factors although AM macrophages have been studied more in this regard [57,66].
AMs are in the airway space, usually close to the alveolar epithelium, facing the external environment [53]. AMs are long-lived cells and under homeostatic conditional or after cell depletion, their repopulation occurs by in situ proliferation rather than by replenishment from bone marrow [68]. However, after infection or an inflammatory insult, AMs are rapidly depleted and republish by monocyte-derived AMS [69,70,71]. The work of Misharin’s group, which performed scRNA-seq to compare eight normal human lungs to eight severely fibrotic lungs, showed that AMs show greater heterogeneity in fibrotic foci [72].
Conversely, IMs reside in the lung parenchyma [53], and their functions are less studied and therefore less well understood [57]. However, their location is ideal for influencing all fibrotic processes compared to AMs. In fact, different mice studies have highlighted the importance of IMs in pulmonary fibrosis in models of radiation-induced pulmonary fibrosis [73] and airway allergic inflammation.
Apart from this difference in AMs and IMs, lung macrophage populations have been classified according to their activation status between M1 and M2. The two M1/M2 macrophages “entities” have been very much used to classify these monocyte-derived macrophages, especially in other organs such as the intestine In the lungs, however, the macrophage population is so heterogenous that it is almost impossible to classify them according to this very strict pair [74]. This is rather controversial as even though some authors doubt about the utility of describing macrophages as M1 or M2 in the context of pulmonary fibrosis [53], others have extensively described how regulators of M2 polarization contribute to fibrotic progression [75]. For example, Cheng et al. recently wrote that promoting the apoptosis of M2 macrophages or inhibiting their polarization may be beneficial for treating pulmonary fibrosis [76].
3.1. Macrophage-Derived Secretory Proteins and Fibrosis in the Lungs: The Macrophage Secretome
In any case, macrophages are without doubt major drivers of fibrosis and are often found close to the myofibroblasts that produce components of the ECM. They produce different chemokines and cytokines, including matrix metalloproteases, as well as pro-fibrotic soluble mediators involved in the proliferation of fibroblasts, conversion to myofibroblasts, and recruitment of other immune cells to the injury site. We have summarised the different secretory proteins produced by macrophages, in Table 1.
3.2. Other Immune Cells
Apart from macrophages, other immune cell populations have been implicated in fibrosis and in contributing to the fibrotic microenvironment. Neutrophils, for example, behave as friends or foes in an immune response in the lung, yet numerous articles show the implication of neutrophils in IPF. For example, bad prognosis in IPF patients is associated with an increased number of neutrophils [107], and CXCL8, an important chemokine produced by neutrophils, is also increased during fibrosis [108]. Recently, neutrophil extracellular traps (NETs) have attracted attention as they are meant to be present in Interstitial Lung Disease (ILD) [109]. The role of neutrophils and other immune cells are not discussed here as we are focused on the processes of myofibroblast differentiation. Nevertheless, we recommended a recent review from Desai et al. in which they describe the role of immune cells in IPF very well [110].
4. Signaling Pathways in Fibrosis
It is clear then that fibrosis can be described as an imbalance between matrix deposition and matrix degradation, which in turn produces tissue remodelling. Understanding the main signal transduction pathways that govern the differentiation and maintenance of myofibroblasts in fibrotic diseases is therefore of paramount importance for develop anti-fibrotic therapies [111].
The TGF-β signalling: TGF-β regulates varied functions, such as stem cell pluripotency, development, proliferation, differentiation and immune responses. It is one of the most potent factors for inducing myofibroblast differentiation, and has been shown to be produced by AM and AT2 cells [112,113].
Apart from its role in myofibroblast differentiation, TGF-β participates in the induction of many molecules that participate in ECM remodelling, such as matrix metalloproteinases, integrins [114] and in the production suppression of anti-fibrotic molecules such as hepatocyte growth factor and prostaglandin E2 [115,116]. Furthermore, TGF-β inhibits alveolar epithelial cell growth and repair.
An increase in TGF-β levels is seen in many diseases, as well as in most pulmonary diseases such as asthma [117,118], fibrosis and cancer. For example, TGF-β1 expression has been found in small airway epithelial cells among smokers and patients with COPD [119].
The best characterized intracellular effectors of the TGF-β superfamily proteins are the Smads, a group of eight structurally related proteins with homologues that have been identified in both vertebrates and invertebrates [120]. However, recent evidence suggests that TGF-β-independent mechanisms may also contribute to Smad activation in certain cell types. For example, in epithelial cells, it has been suggested that a viral infection activate Smads in a TGF-β-independent manner [121]. The significance of TGF-β-independent Smad signaling in lung fibrosis is not clear yet.
The Wnt/β-catenin signalling: The Wnt–β-catenin system is an evolutionary conserved signalling pathway that is of particular importance for morphogenesis and cell organization during embryogenesis. The system is usually suppressed in adulthood; however, it can be re-activated by organ injury and regeneration [122]. Wnt–β-catenin signalling has been extensively implicated in the differentiation of mesenchymal stem cells and progression of fibrotic diseases [123,124], specifically in the lungs. Hou et al. showed that M2 macrophages can promote myofibroblast differentiation by activating the Wnt–β-catenin signalling pathway [125]. More recently, Cao et al. showed the critical involvement of this pathway in the regulation of myofibroblast differentiation and its importance in pulmonary fibrosis [126].
Many studies have emphasized a key role for canonical Wnt signalling in fibrogenesis of the heart and kidneys, and several fibrotic disorders of the skin [127,128,129]. In the lungs, there is aberrant pathway activation in IPF [123]. Its inhibition has also been related to the development of pulmonary fibrosis [130].
YAP and TAZ signalling: YAP and TAZ are two major molecules in the hippo pathway and have been studied for their role in stem cell fate, organ size control, cancer and very recently mechanobiology [131,132,133,134]. When dysregulated, this pathway is implicated in many diseases, as Cai et al. recently reviewed [135].
There is also increasing evidence of f this pathway’s important role in myofibroblast activation [111]. For example, TAZ upregulation has been seen in fibroblasts from IPF patients, and this increase was related to differentiation to myofibroblast phenotypes [136].
Furthermore, in respiratory fibrotic processes, a study by Liu et al. found that YAP and TAZ were increased in the fibroblasts of IPF patients, whereas their nuclear localization was largely absent in normal lungs [136]. Furthermore, as Gokey et al., recently wrote, many studies have elucidated the upstream and downstream effects of YAP/TAZ in lung fibrosis [137].
We believed that it was important to summarise these three very complex signalling pathways briefly to understand the therapeutically efforts that are currently made to treat lung fibrosis. In that sense it is important to note two different aspects: these pathways are regulated by a very controlled cytosolic/nuclear shuffle that produces the activation of its transcription activators. Second, TGF-β, Wnt, and YAP and TAZ work in concert, instead of in isolation. The final output of these pathways is, of course, the activation and maintenance of the myofibroblast phenotype [111].
5. Therapeutic Targets in Lung Tissue Remodelling and Fibrosis
Pulmonary remodelling is the most intractable feature of respiratory diseases because of damage to the structure of the airways and parenchyma, which leads to impaired airflow and gas exchange. Different drugs have been approved for the treatment of diseases (e.g., asthma, COPD, and IPF) that involve pulmonary remodelling, including. However, these treatments do not usually target the molecules that contribute to remodelling. Therefore, drugs that prevent or reverse these events are of potential interest.
5.1. Pirfenidone and Nintedanib
In 2014, the U.S. Food and Drug Administration approved pirfenidone and nintedanib, two drugs that proved to be effective in the delay of IPF [138,139]. For example, nintedanib slowed the progression of lung fibrosis and improved lung function in clinical trials [140].
The principal action of pirfenidone is the alteration of the TGF-β pathway, which decreases Smad3, p38 and Akt phosphorylation [141,142]. This inhibition was shown to suppress fibroblast proliferation and collagen production. In addition, pirfenidone also inhibited the production of pro-inflammatory cytokines (TNFα, IL-1, IL-6) and promoted the production of anti-inflammatory cytokines such as IL-10 [143].
On the other hand, nintedanib is a small-molecule tyrosine kinase inhibitor that targets fibroblast migration and proliferation, thereby inhibiting important downstream signaling pathways such as the vascular endothelial growth factor receptor (VEGFR) and the fibroblast growth factor receptor (FGFR).
Due to different mechanisms of action, both pirfenidone and nintedanib can be used in combination. A clinical trial [141] investigated the safety and tolerability of both drugs as a primary end-point. It enrolled 53 IPF patients under combination therapy and compared them to 51 IPF patients treated with nintedanib alone. The adverse effect frequency was similar in the two groups, except for nausea and vomiting which were greater in the combination group. Moreover, the combination treatment was related to a trend in the reduction of forced vital capacity (FVC) [141]. In another study, 89 IPF patients were treated with nintedanib in addition to a pre-existing pirfenidone treatment, but this study did not bring new signals to the known safety profile of either therapy alone [142]. Although the available data are promising for tolerability and safety, more randomized controlled clinical trials should be conducted in large cohorts.
It is important to note that these drugs do not represent a cure, as their benefits are limited to delaying parenchymal remodelling rather than inhibiting or reversing it. For this reason, the search for new therapeutic targets is still a clinical necessity.
5.2. Novel Therapies
The activation of multiple pathways that lead to myofibroblast proliferation, migration and differentiation have been identified as possible molecular targets for early clinical trials (Table 2).
Table 2.
Current clinical trials in idiopathic pulmonary fibrosis (IPF).
| Therapy | Mechanism of Action | Clinical Trial Identifier | Status | Observations | Ref. |
|---|---|---|---|---|---|
| Fresolimumab | Antibody to neutralize TGFβ | NCT00125385 | Phase I completed | - | |
| Lebrikizumab | Anti-IL-13 and IL-14 antibody | NCT01872689 | Phase II completed | [147] | |
| Tralokinumab | Anti-IL-13 antibody | NCT01629667 | Phase II terminated (lack of efficacy) | The study was stopped due to lack of efficacy | [146] |
| NCT02036580 | Phase II completed | Early termination due to lack of efficacy | - | ||
| Pamrevlumab (FG-3019) | Anti-CTGF antibody | NCT01890265 | Phase II completed | Preliminary report shows overall safety and marginally favorable outcome in some patients | [149] |
| NCT03955146 | Phase III recruiting | - | |||
| BG00011 (STX-100) | Anti-integrin antibody | NCT01371305 | Phase II completed | This trial was terminated due to safety concerns | - |
| Simtuzumab | Anti-LOX antibody | NCT01769196 | Phase II terminated | The study recommended early termination due to lack of efficacy | [151] |
| PRM-151 | Recombinant human pentraxin 2 (also known as serum amyloid P) | NCT01254409 | Phase I | A preliminary report showed overall safety and a marginally favorable outcome in some patients | [157] |
| NCT02550873 | Phase II completed | Decreased pulmonary function decline and stability in 6MWD over 24 weeks | [160] | ||
| NCT04594707 | Phase III recruiting | ||||
| PBI-4050 | GPR84 antagonist/GPR40 agonist | NCT02538536 | Phase II completed | PBI-4050 alone or in combination with nintedanib or pirfenidone showed no safety concerns | [159] |
Abbreviations: FVC: forced vital capacity; IL: interleukin; LOX: lysyl oxidase; PDGF: platelet-derived growth factor; TGF-β1: Transforming growth factor 1; IPF: Idiopathic pulmonary fibrosis; 6MWD: 6-min walk distance.
5.2.1. Inhibition of Pro-Fibrotic Molecules
In a recent review, Györfi et al. extensively revised the possible strategies for targeting the pro-fibrotic cytokine TGF-β, which, as highlighted above, plays a main role in lung tissue remodeling in pulmonary fibrosis [144]. Apart from pirfenidone, other compounds have been used to suppress parenchyma remodeling by targeting TGF-β. A Phase I, open-label, non-randomized, multicenter study (ClinicalTrials.gov Identifier: NCT00125385) was performed to investigate the tolerability, safety and pharmacokinetics of Fresolimumab (GC1008), a recombinant human monoclonal antibody that inhibits all three TGF-β isoforms [143,144]. However, as far as we are aware, results of this study have never been published.
Many previous studies have described the important role that interleukins play in the pathogenesis of lung fibrosis. IL-13 and IL-14 are key cytokines in many signaling pathways related to lung remodeling [145]. Several monoclonal antibodies targeting IL-13 (tralokinumab) or IL-13 and IL-14 (lebrikizumab) have failed to show efficacy in treating IPF [146,147]. Recently, a study of an IL-11 neutralizing antibody was conducted, and although results were promising, it was only used in vitro or in IPF mice models [148].
Connective tissue growth factor (CTGF, also known as CCN2) is involved in lung remodeling and also mediates TGF-β activation. Pamrevlumab (FG-3019) is a monoclonal antibody against CTGF, and successfully attenuated the progression of IPF in a phase II study [149]. A phase III clinical trial is currently underway (ClinicalTrials.gov Identifier: NCT03955146).
5.2.2. Drugs Targeting ECM Proteins Directly
Several recent novel treatments to inhibit lung fibrosis have been developed that target factors such as ECM proteins that are downstream of TGF-β.
For example, integrins play a central role in ECM adhesion and are involved in fibrosis. Partial inhibition of integrin avβ6 blocks development of pulmonary fibrosis without affecting inflammation [150]. Along that line, a phase II trial (ClinicalTrials.gov Identifier: NCT01371305c) studied the safety and tolerability of a humanized monoclonal antibody (BG00011) against this integrin. However, this trial was terminated due to safety concerns.
Another example is Simtuzumab, a monoclonal antibody against Lysyl oxidase-like-2 LOLX2. This enzyme catalyzes the cross-linking of collagen fibers and elastin [151], and elevated levels of LOXL2 are found in IPF [152]. PXS-5120A, a small molecule inhibitor of LOXL2, has been shown to reduce collagen production although this study was conducted on a bleomycin mouse model [153].
5.2.3. Other Targets
Pentraxin (PTX)-2 has been shown to reduce fibrosis by inhibiting differentiation into profibrotic fibrocytes and TGF-β-producing macrophages [154,155]. Low PTX-2 levels have been observed in patients with IPF [156] and a recombinant human PTX-2 analog (PRM-151) has been shown to ameliorate fibrosis in bleomycin- and TGF-β-overexpressing animal models. In humans, a phase II study demonstrated significant improvement in lung function and stability over 24 weeks with an acceptable safety profile compared to a placebo [157] (ClinicalTrials.gov Identifier: NCT02550873). There is at the moment an ongoing phase III clinical trial (ClinicalTrials.gov Identifier: NCT04594707).
Finally, clinical trials have also been conducted with PBI-4050 (ClinicalTrials.gov Identifier: NCT02538536), an analog of a medium-chain fatty acid that shows an affinity for G-protein receptors that target and inhibit multiple pathways including TGF-β [158]. PBI-4050 alone or in combination with nintedanib gave good results, as the stability of the FVC between baseline and week 12 looked encouraging [159]. Further studies with PBI-4050 in combination with nintedanib or alone are being considered.
Fibrosis and pulmonary remodeling may be treated with multiple drugs in combination, and further studies are needed to identify and better understand the role and therapeutic potential of key molecules in lung fibrosis.
6. Final Remarks
Fibrotic phenomena in some lung disorders can be found in isolation or be the pathophysiological basis of devastating diseases such as IPF. Lung myofibroblast likely originate from multiple sources in lung-resident cells. Their relative contributions vary depending not only on the type of injury, but also on the environmental risk factors (cigarette smoking being the most consistent) and normal biological processes such as aging. Both are also related to the differentiation of fibroblasts into myofibroblasts.
Currently, only two drugs are approved to treat IPF, so knowledge of the molecular pathways involved in these complex processes will allow different targets in the same patient to be attacked, as it is being done for other respiratory diseases, such as pulmonary arterial hypertension and cystic fibrosis.
Acknowledgments
Figures were created with BioRender.com. The authors want to acknowledge Julio Cortijo and Juan Viña for helping with funding.
Author Contributions
E.O.-Z., J.S.-C., P.M. and I.R. wrote the original draft manuscript. All authors critically reviewed the manuscript and edited the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
J.S-C acknowledge funding from the Institute of Health Carlos III (COV20/01209), Ministry of Science and Innovation of Spain. P.M and I.R acknowledge funding from the grants PID2020-114871RB-I00 (JC), European Regional Development Fund (FEDER), and Instituto de Salud Carlos III, PI20/01363 (JM), CIBERES (CB06/06/0027) the Spanish Government, and research grants from the Regional Government Prometeo 2017/023/UV (JC), from “Generalitat Valenciana”. The funding entities did not contribute to the study design or data collection, analysis, or interpretation, or to the writing of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vestbo J., Hurd S.S., Agustí A.G., Jones P.W., Vogelmeier C., Anzueto A., Barnes P.J., Fabbri L.M., Martinez F.J., Nishimura M., et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD Executive Summary. Am. J. Respir. Crit. Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 2.Postma D.S., Kerstjens H.A.M. Characteristics of Airway Hyperresponsiveness in Asthma and Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 1998;158:S187–S192. doi: 10.1164/ajrccm.158.supplement_2.13tac170. [DOI] [PubMed] [Google Scholar]
- 3.Liu G., Philp A.M., Corte T., Travis M.A., Schilter H., Hansbro N.G., Burns C.J., Eapen M.S., Sohal S.S., Burgess J.K., et al. Therapeutic targets in lung tissue remodelling and fibrosis. Pharmacol. Ther. 2021;225:107839. doi: 10.1016/j.pharmthera.2021.107839. [DOI] [PubMed] [Google Scholar]
- 4.Hung C. Origin of Myofibroblasts in Lung Fibrosis. Curr. Tissue Microenviron. Rep. 2020;1:155–162. doi: 10.1007/s43152-020-00022-9. [DOI] [Google Scholar]
- 5.Hinz B., Phan S.H., Thannickal V.J., Galli A., Bochaton-Piallat M.L., Gabbiani G. The Myofibroblast. Am. J. Pathol. 2007;170:1807–1816. doi: 10.2353/ajpath.2007.070112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases: The myofibroblast. J. Pathol. 2003;200:500–503. doi: 10.1002/path.1427. [DOI] [PubMed] [Google Scholar]
- 7.Hinz B., Phan S.H., Thannickal V.J., Prunotto M., Desmoulière A., Varga J., De Wever O., Mareel M.M., Gabbiani G. Recent Developments in Myofibroblast Biology. Am. J. Pathol. 2012;180:1340–1355. doi: 10.1016/j.ajpath.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coen M., Gabbiani G., Bochaton-Piallat M.L. Myofibroblast-Mediated Adventitial Remodeling: An Underestimated Player in Arterial Pathology. Arterioscler. Thromb. Vasc. Biol. 2011;31:2391–2396. doi: 10.1161/ATVBAHA.111.231548. [DOI] [PubMed] [Google Scholar]
- 9.Braga F.A.V., Kar G., Berg M., Carpaij O.A., Polanski K., Simon L.M., Brouwer S., Gomes T., Hesse L., Jiang J., et al. A cellular census of human lungs identifies novel cell states in health and in asthma. Nat. Med. 2019;25:1153–1163. doi: 10.1038/s41591-019-0468-5. [DOI] [PubMed] [Google Scholar]
- 10.Goldfarbmuren K.C., Jackson N.D., Sajuthi S.P., Dyjack N., Li K.S., Rios C.L., Plender E.G., Montgomery M.T., Everman J.L., Bratcher P.E., et al. Dissecting the cellular specificity of smoking effects and reconstructing lineages in the human airway epithelium. Nat. Commun. 2020;11:2485. doi: 10.1038/s41467-020-16239-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hong K.U., Reynolds S.D., Watkins S., Fuchs E., Stripp B.R. Basal Cells Are a Multipotent Progenitor Capable of Renewing the Bronchial Epithelium. Am. J. Pathol. 2004;164:577–588. doi: 10.1016/S0002-9440(10)63147-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rock J.R., Onaitis M.W., Rawlins E.L., Lu Y., Clark C.P., Xue Y., Randell S.H., Hogan B.L.M. Basal cells as stem cells of the mouse trachea and human airway epithelium. Proc. Natl. Acad. Sci. USA. 2009;106:12771–12775. doi: 10.1073/pnas.0906850106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis J.D., Wypych T.P. Cellular and functional heterogeneity of the airway epithelium. Mucosal Immunol. 2021;14:978–990. doi: 10.1038/s41385-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boers J.E., Ambergen A.W., Thunnissen F.B.J.M. Number and Proliferation of Clara Cells in Normal Human Airway Epithelium. Am. J. Respir. Crit. Care Med. 1999;159:1585–1591. doi: 10.1164/ajrccm.159.5.9806044. [DOI] [PubMed] [Google Scholar]
- 15.Guo M., Du Y., Gokey J.J., Ray S., Bell S.M., Adam M., Sudha P., Perl A.K., Deshmukh H., Potter S.S., et al. Single cell RNA analysis identifies cellular heterogeneity and adaptive responses of the lung at birth. [(accessed on 27 April 2022)];Nat. Commun. 2019 10:37. doi: 10.1038/s41467-018-07770-1. Available online: http://www.nature.com/articles/s41467-018-07770-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basil M.C., Katzen J., Engler A.E., Guo M., Herriges M.J., Kathiriya J.J., Windmueller R., Ysasi A.B., Zacharias W.J., Chapman H.A., et al. The Cellular and Physiological Basis for Lung Repair and Regeneration: Past, Present, and Future. Cell Stem Cell. 2020;26:482–502. doi: 10.1016/j.stem.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rokicki W., Rokicki M., Wojtacha J., Dżeljijli A. The role and importance of club cells (Clara cells) in the pathogenesis of some respiratory diseases. Pol. J. Cardio-Thorac. Surg. 2016;1:26–30. doi: 10.5114/kitp.2016.58961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zuo W.L., Shenoy S.A., Li S., O’Beirne S.L., Strulovici-Barel Y., Leopold P.L., Wang G., Staudt M.R., Walters M.S., Mason C., et al. Ontogeny and Biology of Human Small Airway Epithelial Club Cells. Am. J. Respir. Crit. Care Med. 2018;198:1375–1388. doi: 10.1164/rccm.201710-2107OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reid A.T., Veerati P.C., Gosens R., Bartlett N.W., Wark P.A., Grainge C.L., Stick S.M., Kicic A., Moheimani F., Hansbro P.M., et al. Persistent induction of goblet cell differentiation in the airways: Therapeutic approaches. Pharmacol. Ther. 2018;185:155–169. doi: 10.1016/j.pharmthera.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Whitsett J.A., Kalin T.V., Xu Y., Kalinichenko V.V. Building and Regenerating the Lung Cell by Cell. Physiol. Rev. 2019;99:513–554. doi: 10.1152/physrev.00001.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tilley A.E., Walters M.S., Shaykhiev R., Crystal R.G. Cilia Dysfunction in Lung Disease. Annu. Rev. Physiol. 2015;77:379–406. doi: 10.1146/annurev-physiol-021014-071931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouadah Y., Rojas E.R., Riordan D.P., Capostagno S., Kuo C.S., Krasnow M.A. Rare Pulmonary Neuroendocrine Cells Are Stem Cells Regulated by Rb, p53, and Notch. Cell. 2019;179:403–416.e23. doi: 10.1016/j.cell.2019.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hewitt R.J., Lloyd C.M. Regulation of immune responses by the airway epithelial cell landscape. Nat. Rev. Immunol. 2021;21:347–362. doi: 10.1038/s41577-020-00477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Branchfield K., Nantie L., Verheyden J.M., Sui P., Wienhold M.D., Sun X. Pulmonary neuroendocrine cells function as airway sensors to control lung immune response. Science. 2016;351:707–710. doi: 10.1126/science.aad7969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noble P.W., Barkauskas C.E., Jiang D. Pulmonary fibrosis: Patterns and perpetrators. J. Clin. Investig. 2012;122:2756–2762. doi: 10.1172/JCI60323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Selman M., Pardo A. The leading role of epithelial cells in the pathogenesis of idiopathic pulmonary fibrosis. Cell Signal. 2020;66:109482. doi: 10.1016/j.cellsig.2019.109482. [DOI] [PubMed] [Google Scholar]
- 27.Parimon T., Yao C., Stripp B.R., Noble P.W., Chen P. Alveolar Epithelial Type II Cells as Drivers of Lung Fibrosis in Idiopathic Pulmonary Fibrosis. Int. J. Mol. Sci. 2020;21:2269. doi: 10.3390/ijms21072269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kulkarni T., de Andrade J., Zhou Y., Luckhardt T., Thannickal V.J. Alveolar epithelial disintegrity in pulmonary fibrosis. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2016;311:L185–L191. doi: 10.1152/ajplung.00115.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma J., Sanchez-Duffhues G., Goumans M.J., ten Dijke P. TGF-β-Induced Endothelial to Mesenchymal Transition in Disease and Tissue Engineering. Front. Cell Dev. Biol. 2020;8:260. doi: 10.3389/fcell.2020.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovacic J.C., Dimmeler S., Harvey R.P., Finkel T., Aikawa E., Krenning G., Baker A.H. Endothelial to Mesenchymal Transition in Cardiovascular Disease. J. Am. Coll. Cardiol. 2019;73:190–209. doi: 10.1016/j.jacc.2018.09.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nataraj D., Ernst A., Kalluri R. Idiopathic Pulmonary Fibrosis Is Associated with Endothelial to Mesenchymal Transition. Am. J. Respir. Cell Mol. Biol. 2010;43:129–130. doi: 10.1165/rcmb.2010-0044ED. [DOI] [PubMed] [Google Scholar]
- 32.Dees C., Chakraborty D., Distler J.H.W. Cellular and molecular mechanisms in fibrosis. Exp. Dermatol. 2021;30:121–131. doi: 10.1111/exd.14193. [DOI] [PubMed] [Google Scholar]
- 33.Zandvoort A., Postma D.S., Jonker M.R., Noordhoek J.A., Vos J.T.W.M., van der Geld Y.M., Timens W. Altered expression of the Smad signalling pathway: Implications for COPD pathogenesis. Eur. Respir. J. 2006;28:533–541. doi: 10.1183/09031936.06.00078405. [DOI] [PubMed] [Google Scholar]
- 34.Roberts A.B., McCune B.K., Sporn M.B. TGF-β: Regulation of extracellular matrix. Kidney Int. 1992;41:557–559. doi: 10.1038/ki.1992.81. [DOI] [PubMed] [Google Scholar]
- 35.Schiller M., Javelaud D., Mauviel A. TGF-β-induced SMAD signaling and gene regulation: Consequences for extracellular matrix remodeling and wound healing. J. Dermatol. Sci. 2004;35:83–92. doi: 10.1016/j.jdermsci.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 36.Morty R.E., Konigshoff M., Eickelberg O. Transforming Growth Factor- Signaling across Ages: From Distorted Lung Development to Chronic Obstructive Pulmonary Disease. Proc. Am. Thorac. Soc. 2009;6:607–613. doi: 10.1513/pats.200908-087RM. [DOI] [PubMed] [Google Scholar]
- 37.Sugiura H., Ichikawa T., Liu X., Kobayashi T., Wang X.Q., Kawasaki S., Togo S., Kamio K., Mao L., Ann Y., et al. N-acetyl-l-cysteine inhibits TGF-β1-induced profibrotic responses in fibroblasts. Pulm. Pharmacol. Ther. 2009;22:487–491. doi: 10.1016/j.pupt.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 38.Araya J., Nishimura S.L. Fibrogenic Reactions in Lung Disease. Annu. Rev. Pathol. Mech. Dis. 2010;5:77–98. doi: 10.1146/annurev.pathol.4.110807.092217. [DOI] [PubMed] [Google Scholar]
- 39.Parameswaran K., Willems-Widyastuti A., Alagappan V.K.T., Radford K., Kranenburg A.R., Sharma H.S. Role of Extracellular Matrix and Its Regulators in Human Airway Smooth Muscle Biology. Cell Biochem. Biophys. 2006;44:139–146. doi: 10.1385/CBB:44:1:139. [DOI] [PubMed] [Google Scholar]
- 40.Kranenburg A.R., Willems-Widyastuti A., Mooi W.J., Sterk P.J., Alagappan V.K.T., de Boer W.I., Sharma H.S. Enhanced Bronchial Expression of Extracellular Matrix Proteins in Chronic Obstructive Pulmonary Disease. Am. J. Clin. Pathol. 2006;126:725–735. doi: 10.1309/JC477FAEL1YKV54W. [DOI] [PubMed] [Google Scholar]
- 41.Lagente V., Manoury B., Nénan S., Le Quément C., Martin-Chouly C., Boichot E. Role of matrix metalloproteinases in the development of airway inflammation and remodeling. Braz. J. Med. Biol. Res. 2005;38:1521–1530. doi: 10.1590/S0100-879X2005001000009. [DOI] [PubMed] [Google Scholar]
- 42.Li H., Cui D., Ma N., Lu L., Gao Y., Cui X., Wang D. The effect of extracellular matrix remodeling on airflow obstruction in a rat model of chronic obstructive pulmonary disease. Zhonghua Jie He He Hu Xi Za Zhi Zhonghua Jiehe He Huxi Zazhi Chin. J. Tuberc. Respir. Dis. 2002;25:403–407. [PubMed] [Google Scholar]
- 43.Bucala R. Fibrocytes at 20 Years. Mol. Med. Camb. Mass. 2015;21:S3–S5. doi: 10.2119/molmed.2015.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keeley E.C., Schutt R.C., Marinescu M.A., Burdick M.D., Strieter R.M., Mehrad B. Circulating fibrocytes as predictors of adverse events in unstable angina. Transl. Res. 2016;172:73–83.e1. doi: 10.1016/j.trsl.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moore B.B., Kolb M. Fibrocytes and progression of fibrotic lung disease. Ready for showtime? Am. J. Respir. Crit. Care Med. 2014;190:1338–1339. doi: 10.1164/rccm.201411-2013ED. [DOI] [PubMed] [Google Scholar]
- 46.Dolgachev V.A., Ullenbruch M.R., Lukacs N.W., Phan S.H. Role of Stem Cell Factor and Bone Marrow-Derived Fibroblasts in Airway Remodeling. Am. J. Pathol. 2009;174:390–400. doi: 10.2353/ajpath.2009.080513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Borie R., Quesnel C., Phin S., Debray M.P., Marchal-Somme J., Tiev K., Bonay M., Fabre A., Soler P., Dehoux M., et al. Detection of Alveolar Fibrocytes in Idiopathic Pulmonary Fibrosis and Systemic Sclerosis. PLoS ONE. 2013;8:e53736. doi: 10.1371/journal.pone.0053736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kleaveland K.R., Velikoff M., Yang J., Agarwal M., Rippe R.A., Moore B.B., Kim K.K. Fibrocytes Are Not an Essential Source of Type I Collagen during Lung Fibrosis. J. Immunol. 2014;193:5229–5239. doi: 10.4049/jimmunol.1400753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heukels P., van Hulst J.A.C., van Nimwegen M., Boorsma C.E., Melgert B.N., van den Toorn L.M., Boomars K.A.T., Wijsenbeek M., Hoogsteden H., von der Thusen J., et al. Fibrocytes are increased in lung and peripheral blood of patients with idiopathic pulmonary fibrosis. Respir. Res. 2018;19:90. doi: 10.1186/s12931-018-0798-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maharaj S.S., Baroke E., Gauldie J., Kolb M.R.J. Fibrocytes in chronic lung disease—Facts and controversies. Pulm. Pharmacol. Ther. 2012;25:263–267. doi: 10.1016/j.pupt.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 51.Andersson-Sjöland A., de Alba C.G., Nihlberg K., Becerril C., Ramírez R., Pardo A., Westergren-Thorsson G., Selman M. Fibrocytes are a potential source of lung fibroblasts in idiopathic pulmonary fibrosis. Int. J. Biochem. Cell Biol. 2008;40:2129–2140. doi: 10.1016/j.biocel.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 52.Moeller A., Gilpin S.E., Ask K., Cox G., Cook D., Gauldie J., Margetts P.J., Farkas L., Dobranowski J., Boylan C., et al. Circulating Fibrocytes Are an Indicator of Poor Prognosis in Idiopathic Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2009;179:588–594. doi: 10.1164/rccm.200810-1534OC. [DOI] [PubMed] [Google Scholar]
- 53.Byrne A.J., Maher T.M., Lloyd C.M. Pulmonary Macrophages: A New Therapeutic Pathway in Fibrosing Lung Disease? Trends Mol. Med. 2016;22:303–316. doi: 10.1016/j.molmed.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 54.Yuan K., Shamskhou E.A., Orcholski M.E., Nathan A., Reddy S., Honda H., Mani V., Zeng Y., Ozen M.O., Wang L., et al. Loss of Endothelium-Derived Wnt5a Is Associated with Reduced Pericyte Recruitment and Small Vessel Loss in Pulmonary Arterial Hypertension. Circulation. 2019;139:1710–1724. doi: 10.1161/CIRCULATIONAHA.118.037642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Göritz C., Dias D.O., Tomilin N., Barbacid M., Shupliakov O., Frisén J. A Pericyte Origin of Spinal Cord Scar Tissue. Science. 2011;333:238–242. doi: 10.1126/science.1203165. [DOI] [PubMed] [Google Scholar]
- 56.Hung C., Linn G., Chow Y.H., Kobayashi A., Mittelsteadt K., Altemeier W.A., Gharib S.A., Schnapp L.M., Duffield J.S. Role of Lung Pericytes and Resident Fibroblasts in the Pathogenesis of Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2013;188:820–830. doi: 10.1164/rccm.201212-2297OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shi L., Jiang Q., Bushkin Y., Subbian S., Tyagi S. Biphasic Dynamics of Macrophage Immunometabolism during Mycobacterium tuberculosis Infection. mBio. 2019;10:e02550-18. doi: 10.1128/mBio.02550-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Laskin D.L. Macrophages and Inflammatory Mediators in Chemical Toxicity: A Battle of Forces. Chem. Res. Toxicol. 2009;22:1376–1385. doi: 10.1021/tx900086v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schupp J.C., Binder H., Jäger B., Cillis G., Zissel G., Müller-Quernheim J., Prasse A. Macrophage Activation in Acute Exacerbation of Idiopathic Pulmonary Fibrosis. PLoS ONE. 2015;10:e0116775. doi: 10.1371/journal.pone.0116775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang S., Meng X.-M., Ng Y.-Y., Ma F.Y., Zhou S., Zhang Y., Yang C., Huang X.-R., Xiao J., Wang Y.-Y., et al. TGF-β/Smad3 signalling regulates the transition of bone marrow-derived macrophages into myofibroblasts during tissue fibrosis. Oncotarget. 2016;7:8809–8822. doi: 10.18632/oncotarget.6604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Y.-Y., Jiang H., Pan J., Huang X.-R., Wang Y.-C., Huang H.-F., To K.-F., Nikolic-Paterson D.J., Lan H.-Y., Chen J.-H. Macrophage-to-Myofibroblast Transition Contributes to Interstitial Fibrosis in Chronic Renal Allograft Injury. J. Am. Soc. Nephrol. 2017;28:2053–2067. doi: 10.1681/ASN.2016050573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang F., Chang Y., Zhang C., Xiong Y., Wang X., Ma X., Wang Z., Li H., Shimosawa T., Pei L., et al. UUO induces lung fibrosis with macrophage-myofibroblast transition in rats. Int. Immunopharmacol. 2021;93:107396. doi: 10.1016/j.intimp.2021.107396. [DOI] [PubMed] [Google Scholar]
- 63.van der Veen T.A., de Groot L.E.S., Melgert B.N. The different faces of the macrophage in asthma. Curr. Opin. Pulm. Med. 2020;26:62–68. doi: 10.1097/MCP.0000000000000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ogger P.P., Byrne A.J. Macrophage metabolic reprogramming during chronic lung disease. Mucosal Immunol. 2021;14:282–295. doi: 10.1038/s41385-020-00356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tamò L., Simillion C., Hibaoui Y., Feki A., Gugger M., Prasse A., Jäger B., Goldmann T., Geiser T., Gazdhar A. Gene Network Analysis of Interstitial Macrophages after Treatment with Induced Pluripotent Stem Cells Secretome (iPSC-cm) in the Bleomycin Injured Rat Lung. Stem Cell Rev. Rep. 2018;14:412–424. doi: 10.1007/s12015-017-9790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gibbings S.L., Thomas S.M., Atif S.M., McCubbrey A.L., Desch A.N., Danhorn T., Leach S.M., Bratton D.L., Henson P.M., Janssen W.J., et al. Three Unique Interstitial Macrophages in the Murine Lung at Steady State. Am. J. Respir. Cell Mol. Biol. 2017;57:66–76. doi: 10.1165/rcmb.2016-0361OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.The Immunological Genome Consortium. Gautier E.L., Shay T., Miller J., Greter M., Jakubzick C., Ivanov S., Helft J., Chow A., Elpek K.G., et al. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat. Immunol. 2012;13:1118–1128. doi: 10.1038/ni.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hashimoto D., Chow A., Noizat C., Teo P., Beasley M.B., Leboeuf M., Becker C.D., See P., Price J., Lucas D., et al. Tissue-Resident Macrophages Self-Maintain Locally throughout Adult Life with Minimal Contribution from Circulating Monocytes. Immunity. 2013;38:792–804. doi: 10.1016/j.immuni.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mould K.J., Barthel L., Mohning M.P., Thomas S.M., McCubbrey A.L., Danhorn T., Leach S.M., Fingerlin T.E., O’Connor B.P., Reisz J.A., et al. Cell Origin Dictates Programming of Resident Versus Recruited Macrophages during Acute Lung Injury. Am. J. Respir. Cell Mol. Biol. 2017;57:294–306. doi: 10.1165/rcmb.2017-0061OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Machiels B., Dourcy M., Xiao X., Javaux J., Mesnil C., Sabatel C., Desmecht D., Lallemand F., Martinive P., Hammad H., et al. A gammaherpesvirus provides protection against allergic asthma by inducing the replacement of resident alveolar macrophages with regulatory monocytes. Nat. Immunol. 2017;18:1310–1320. doi: 10.1038/ni.3857. [DOI] [PubMed] [Google Scholar]
- 71.Cole S.L., Ho L.P. Contribution of innate immune cells to pathogenesis of severe influenza virus infection. Clin. Sci. 2017;131:269–283. doi: 10.1042/CS20160484. [DOI] [PubMed] [Google Scholar]
- 72.Misharin A.V., Morales-Nebreda L., Reyfman P.A., Cuda C.M., Walter J.M., McQuattie-Pimentel A.C., Chen C.-I., Anekalla K.R., Joshi N., Williams K.J.N., et al. Monocyte-derived alveolar macrophages drive lung fibrosis and persist in the lung over the life span. J. Exp. Med. 2017;214:2387–2404. doi: 10.1084/jem.20162152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murray L.A., Rosada R., Moreira A.P., Joshi A., Kramer M.S., Hesson D.P., Argentieri R.L., Mathai S., Gulati I., Herzog E.L., et al. Serum amyloid P therapeutically attenuates murine bleomycin-induced pulmonary fibrosis via its effects on macrophages. PLoS ONE. 2010;5:e9683. doi: 10.1371/journal.pone.0009683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ogawa T., Shichino S., Ueha S., Matsushima K. Macrophages in lung fibrosis. Int. Immunol. 2021;33:665–671. doi: 10.1093/intimm/dxab040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yao Y., Wang Y., Zhang Z., He L., Zhu J., Zhang M., He X., Cheng Z., Ao Q., Cao Y., et al. Chop Deficiency Protects Mice Against Bleomycin-Induced Pulmonary Fibrosis by Attenuating M2 Macrophage Production. Mol. Ther. J. Am. Soc. Gene Ther. 2016;24:915–925. doi: 10.1038/mt.2016.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cheng P., Li S., Chen H. Macrophages in Lung Injury, Repair, and Fibrosis. Cells. 2021;10:436. doi: 10.3390/cells10020436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schauer I.G., Ressler S.J., Rowley D.R. Keratinocyte-derived chemokine induces prostate epithelial hyperplasia and reactive stroma in a novel transgenic mouse model: KC/IL-8 Induces Prostate Epithelial Hyperplasia. Prostate. 2009;69:373–384. doi: 10.1002/pros.20886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shi T., Denney L., An H., Ho L.P., Zheng Y. Alveolar and lung interstitial macrophages: Definitions, functions, and roles in lung fibrosis. J. Leukoc. Biol. 2021;110:107–114. doi: 10.1002/JLB.3RU0720-418R. [DOI] [PubMed] [Google Scholar]
- 79.Gadek J.E., Kelman J.A., Fells G., Weinberger S.E., Horwitz A.L., Reynolds H.Y., Fulmer J.D., Crystal R.G. Collagenase in the Lower Respiratory Tract of Patients with Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 1979;301:737–742. doi: 10.1056/NEJM197910043011401. [DOI] [PubMed] [Google Scholar]
- 80.Safont B., Tarraso J., Rodriguez-Borja E., Fernández-Fabrellas E., Sancho-Chust J.N., Molina V., Lopez-Ramirez C., Lope-Martinez A., Cabanes L., Andreu A.L., et al. Lung Function, Radiological Findings and Biomarkers of Fibrogenesis in a Cohort of COVID-19 Patients Six Months after Hospital Discharge. Arch. Bronconeumol. 2022;58:142–149. doi: 10.1016/j.arbres.2021.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.García-de-Alba C., Becerril C., Ruiz V., González Y., Reyes S., García-Alvarez J., Selman M., Pardo A. Expression of Matrix Metalloproteases by Fibrocytes: Possible Role in Migration and Homing. Am. J. Respir. Crit. Care Med. 2010;182:1144–1152. doi: 10.1164/rccm.201001-0028OC. [DOI] [PubMed] [Google Scholar]
- 82.Yamashita C.M., Dolgonos L., Zemans R.L., Young S.K., Robertson J., Briones N., Suzuki T., Campbell M.N., Gauldie J., Radisky D.C., et al. Matrix metalloproteinase 3 is a mediator of pulmonary fibrosis. Am. J. Pathol. 2011;179:1733–1745. doi: 10.1016/j.ajpath.2011.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Craig V.J., Polverino F., Laucho-Contreras M.E., Shi Y., Liu Y., Osorio J.C., Tesfaigzi Y., Pinto-Plata V., Gochuico B.R., Rosas I.O., et al. Mononuclear phagocytes and airway epithelial cells: Novel sources of matrix metalloproteinase-8 (MMP-8) in patients with idiopathic pulmonary fibrosis. PLoS ONE. 2014;9:e97485. doi: 10.1371/journal.pone.0097485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Henry M.T., McMahon K., Mackarel A.J., Prikk K., Sorsa T., Maisi P., Sepper R., FitzGerald M., O’Connor C. Matrix metalloproteinases and tissue inhibitor of metalloproteinase-1 in sarcoidosis and IPF. Eur. Respir. J. 2002;20:1220–1227. doi: 10.1183/09031936.02.00022302. [DOI] [PubMed] [Google Scholar]
- 85.Lemjabbar H., Gosset P., Lechapt-Zalcman E., Franco-Montoya M.L., Wallaert B., Harf A., Lafuma C. Overexpression of alveolar macrophage gelatinase B (MMP-9) in patients with idiopathic pulmonary fibrosis: Effects of steroid and immunosuppressive treatment. Am. J. Respir. Cell Mol. Biol. 1999;20:903–913. doi: 10.1165/ajrcmb.20.5.3260. [DOI] [PubMed] [Google Scholar]
- 86.Huang W.-C., Sala-Newby G.B., Susana A., Johnson J.L., Newby A.C. Classical macrophage activation up-regulates several matrix metalloproteinases through mitogen activated protein kinases and nuclear factor-κB. PLoS ONE. 2012;7:e42507. doi: 10.1371/journal.pone.0042507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pardo A., Cabrera S., Maldonado M., Selman M. Role of matrix metalloproteinases in the pathogenesis of idiopathic pulmonary fibrosis. Respir. Res. 2016;17:23. doi: 10.1186/s12931-016-0343-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nkyimbeng T., Ruppert C., Shiomi T., Dahal B., Lang G., Seeger W., Okada Y., D’Armiento J., Günther A. Pivotal Role of Matrix Metalloproteinase 13 in Extracellular Matrix Turnover in Idiopathic Pulmonary Fibrosis. PLoS ONE. 2013;8:e73279. doi: 10.1371/journal.pone.0073279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dancer R.C.A., Wood A.M., Thickett D.R. Metalloproteinases in idiopathic pulmonary fibrosis. Eur. Respir. J. 2011;38:1461–1467. doi: 10.1183/09031936.00024711. [DOI] [PubMed] [Google Scholar]
- 90.Talmi-Frank D., Altboum Z., Solomonov I., Udi Y., Jaitin D.A., Klepfish M., David E., Zhuravlev A., Keren-Shaul H., Winter D., et al. Extracellular Matrix Proteolysis by MT1-MMP Contributes to Influenza-Related Tissue Damage and Mortality. Cell Host Microbe. 2016;20:458–470. doi: 10.1016/j.chom.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 91.Prasse A., Pechkovsky D.V., Toews G.B., Jungraithmayr W., Kollert F., Goldmann T., Vollmer E., Müller-Quernheim J., Zissel G. A vicious circle of alveolar macrophages and fibroblasts perpetuates pulmonary fibrosis via CCL18. Am. J. Respir. Crit. Care Med. 2006;173:781–792. doi: 10.1164/rccm.200509-1518OC. [DOI] [PubMed] [Google Scholar]
- 92.Jaworska J., Coulombe F., Downey J., Tzelepis F., Shalaby K., Tattoli I., Berube J., Rousseau S., Martin J.G., Girardin S.E., et al. NLRX1 prevents mitochondrial induced apoptosis and enhances macrophage antiviral immunity by interacting with influenza virus PB1-F2 protein. Proc. Natl. Acad. Sci. USA. 2014;111:E2110–E2119. doi: 10.1073/pnas.1322118111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wojtan P., Mierzejewski M., Osińska I., Domagała-Kulawik J. Macrophage polarization in interstitial lung diseases. Cent. Eur. J. Immunol. 2016;2:159–164. doi: 10.5114/ceji.2016.60990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ni L., Dong C. Roles of Myeloid and Lymphoid Cells in the Pathogenesis of Chronic Obstructive Pulmonary Disease. [(accessed on 12 April 2022)];Front. Immunol. 2018 9:1431. doi: 10.3389/fimmu.2018.01431. Available online: https://www.frontiersin.org/article/10.3389/fimmu.2018.01431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhu L., Fu X., Chen X., Han X., Dong P. M2 macrophages induce EMT through the TGF-β/Smad2 signaling pathway. Cell Biol. Int. 2017;41:960–968. doi: 10.1002/cbin.10788. [DOI] [PubMed] [Google Scholar]
- 96.Pulmonary Macrophages: Key Players in the Innate Defence of the Airways—PubMed. [(accessed on 13 April 2022)]; Available online: https://pubmed.ncbi.nlm.nih.gov/26286722/
- 97.Shimokado K., Raines E.W., Madtes D.K., Barrett T.B., Benditt E.P., Ross R. A significant part of macrophage-derived growth factor consists of at least two forms of PDGF. Cell. 1985;43:277–286. doi: 10.1016/0092-8674(85)90033-9. [DOI] [PubMed] [Google Scholar]
- 98.Berse B., Brown L.F., Van de Water L., Dvorak H.F., Senger D.R. Vascular permeability factor (vascular endothelial growth factor) gene is expressed differentially in normal tissues, macrophages, and tumors. Mol. Biol. Cell. 1992;3:211–220. doi: 10.1091/mbc.3.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zaiss D.M.W., Gause W.C., Osborne L.C., Artis D. Emerging functions of amphiregulin in orchestrating immunity, inflammation, and tissue repair. [(accessed on 13 April 2022)];Immunity. 2015 42:216–226. doi: 10.1016/j.immuni.2015.01.020. Available online: https://pubmed.ncbi.nlm.nih.gov/25692699/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Xu Y., Meng C., Liu G., Yang D., Fu L., Zhang M., Zhang Z., Xia H., Yao S., Zhang S. Classically Activated Macrophages Protect against Lipopolysaccharide-Induced Acute Lung Injury by Expressing Amphiregulin in Mice. Anesthesiology. 2016;124:1086–1099. doi: 10.1097/ALN.0000000000001026. [DOI] [PubMed] [Google Scholar]
- 101.Allard B., Panariti A., Martin J.G. Alveolar Macrophages in the Resolution of Inflammation, Tissue Repair, and Tolerance to Infection. Front. Immunol. 2018;9:1777. doi: 10.3389/fimmu.2018.01777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Baran C.P., Opalek J.M., McMaken S., Newland C.A., O’Brien J.M., Hunter M.G., Bringardner B.D., Monick M.M., Brigstock D.R., Stromberg P.C., et al. Important roles for macrophage colony-stimulating factor, CC chemokine ligand 2, and mononuclear phagocytes in the pathogenesis of pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2007;176:78–89. doi: 10.1164/rccm.200609-1279OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lee J., Arisi I., Puxeddu E., Mramba L.K., Amicosante M., Swaisgood C.M., Pallante M., Brantly M.L., Sköld C.M., Saltini C. Bronchoalveolar lavage (BAL) cells in idiopathic pulmonary fibrosis express a complex pro-inflammatory, pro-repair, angiogenic activation pattern, likely associated with macrophage iron accumulation. PLoS ONE. 2018;13:e0194803. doi: 10.1371/journal.pone.0194803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Minutti C.M., Knipper J.A., Allen J.E., Zaiss D.M.W. Tissue-specific contribution of macrophages to wound healing. Semin. Cell Dev. Biol. 2017;61:3–11. doi: 10.1016/j.semcdb.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 105.Pyle C.J., Uwadiae F.I., Swieboda D.P., Harker J.A. Early IL-6 signalling promotes IL-27 dependent maturation of regulatory T cells in the lungs and resolution of viral immunopathology. PLoS Pathog. 2017;13:e1006640. doi: 10.1371/journal.ppat.1006640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sayan M., Mossman B.T. The NLRP3 inflammasome in pathogenic particle and fibre-associated lung inflammation and diseases. Part. Fibre Toxicol. 2015;13:51. doi: 10.1186/s12989-016-0162-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kinder B.W., Brown K.K., Schwarz M.I., Ix J.H., Kervitsky A., King T.E. Baseline BAL Neutrophilia Predicts Early Mortality in Idiopathic Pulmonary Fibrosis. Chest. 2008;133:226–232. doi: 10.1378/chest.07-1948. [DOI] [PubMed] [Google Scholar]
- 108.Xaubet A., Agustí C., Luburich P., Barberá J.A., Carrión M., Ayuso M.C., Roca J., Rodriguez-Roisin R. Interleukin-8 expression in bronchoalveolar lavage cells in the evaluation of alveolitis in idiopathic pulmonary fibrosis. Respir. Med. 1998;92:338–344. doi: 10.1016/S0954-6111(98)90118-4. [DOI] [PubMed] [Google Scholar]
- 109.Chrysanthopoulou A., Mitroulis I., Apostolidou E., Arelaki S., Mikroulis D., Konstantinidis T., Sivridis E., Koffa M., Giatromanolaki A., Boumpas D.T., et al. Neutrophil extracellular traps promote differentiation and function of fibroblasts: NETs induce fibrosis via differentiation of fibroblasts. J. Pathol. 2014;233:294–307. doi: 10.1002/path.4359. [DOI] [PubMed] [Google Scholar]
- 110.Desai O., Winkler J., Minasyan M., Herzog E.L. The Role of Immune and Inflammatory Cells in Idiopathic Pulmonary Fibrosis. Front. Med. 2018;5:43. doi: 10.3389/fmed.2018.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Piersma B., Bank R.A., Boersema M. Signaling in Fibrosis: TGF-β, WNT, and YAP/TAZ Converge. [(accessed on 2 May 2022)];Front. Med. 2015 2:59. doi: 10.3389/fmed.2015.00059. Available online: http://journal.frontiersin.org/Article/10.3389/fmed.2015.00059/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Coker R.K. Localisation of transforming growth factor beta1 and beta3 mRNA transcripts in normal and fibrotic human lung. Thorax. 2001;56:549–556. doi: 10.1136/thorax.56.7.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Broekelmann T.J., Limper A.H., Colby T.V., McDonald J.A. Transforming growth factor beta 1 is present at sites of extracellular matrix gene expression in human pulmonary fibrosis. Proc. Natl. Acad. Sci. USA. 1991;88:6642–6646. doi: 10.1073/pnas.88.15.6642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Saito A., Horie M., Nagase T. TGF-β Signaling in Lung Health and Disease. Int. J. Mol. Sci. 2018;19:2460. doi: 10.3390/ijms19082460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Garrison G., Huang S.K., Okunishi K., Scott J.P., Kumar Penke L.R., Scruggs A.M., Penke L.R.K., Scruggs A.M., Peters-Golden M. Reversal of Myofibroblast Differentiation by Prostaglandin E2. Am. J. Respir. Cell Mol. Biol. 2013;48:550–558. doi: 10.1165/rcmb.2012-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bauman K.A., Wettlaufer S.H., Okunishi K., Vannella K.M., Stoolman J.S., Huang S.K., Courey A.J., White E.S., Hogaboam C.M., Simon R.H., et al. The antifibrotic effects of plasminogen activation occur via prostaglandin E2 synthesis in humans and mice. J. Clin. Investig. 2010;120:1950–1960. doi: 10.1172/JCI38369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Redington A.E., Madden J., Frew A.J., Djukanovic R., Roche W.R., Holgate S.T., Howarth P.H. Transforming Growth Factor- β 1 in Asthma: Measurement in Bronchoalveolar Lavage Fluid. Am. J. Respir. Crit. Care Med. 1997;156:642–647. doi: 10.1164/ajrccm.156.2.9605065. [DOI] [PubMed] [Google Scholar]
- 118.Vignola A.M., Chanez P., Chiappara G., Merendino A., Pace E., Rizzo A., La Rocca A.M., Bellia V., Bonsignore G., Bousquet J. Transforming Growth Factor- β Expression in Mucosal Biopsies in Asthma and Chronic Bronchitis. Am. J. Respir. Crit. Care Med. 1997;156:591–599. doi: 10.1164/ajrccm.156.2.9609066. [DOI] [PubMed] [Google Scholar]
- 119.Takizawa H., Tanaka M., Takami K., Ohtoshi T., Ito K., Satoh M., Okada Y., Yamasawa F., Nakahara K., Umeda A. Increased Expression of Transforming Growth Factor- β 1 in Small Airway Epithelium from Tobacco Smokers and Patients with Chronic Obstructive Pulmonary Disease (COPD) Am. J. Respir. Crit. Care Med. 2001;163:1476–1483. doi: 10.1164/ajrccm.163.6.9908135. [DOI] [PubMed] [Google Scholar]
- 120.Hanna A., Humeres C., Frangogiannis N.G. The role of Smad signaling cascades in cardiac fibrosis. Cell Signal. 2021;77:109826. doi: 10.1016/j.cellsig.2020.109826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gowripalan A., Abbott C.R., McKenzie C., Chan W.S., Karupiah G., Levy L., Newsome T.P. Cell-to-cell spread of vaccinia virus is promoted by TGF-β-independent Smad4 signalling. [(accessed on 25 May 2022)];Cell. Microbiol. 2020 22:e13206. doi: 10.1111/cmi.13206. Available online: https://onlinelibrary.wiley.com/doi/10.1111/cmi.13206. [DOI] [PubMed] [Google Scholar]
- 122.Schunk S.J., Floege J., Fliser D., Speer T. WNT–β-catenin signalling—A versatile player in kidney injury and repair. Nat. Rev. Nephrol. 2021;17:172–184. doi: 10.1038/s41581-020-00343-w. [DOI] [PubMed] [Google Scholar]
- 123.Chilosi M., Poletti V., Zamò A., Lestani M., Montagna L., Piccoli P., Pedron S., Bertaso M., Scarpa A., Murer B., et al. Aberrant Wnt/β-Catenin Pathway Activation in Idiopathic Pulmonary Fibrosis. Am. J. Pathol. 2003;162:1495–1502. doi: 10.1016/S0002-9440(10)64282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kühl S.J., Kühl M. On the role of Wnt/β-catenin signaling in stem cells. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2013;1830:2297–2306. doi: 10.1016/j.bbagen.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 125.Hou J., Shi J., Chen L., Lv Z., Chen X., Cao H., Xiang Z., Han X. M2 macrophages promote myofibroblast differentiation of LR-MSCs and are associated with pulmonary fibrogenesis. Cell Commun. Signal. CCS. 2018;16:89. doi: 10.1186/s12964-018-0300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cao H., Wang C., Chen X., Hou J., Xiang Z., Shen Y., Han X. Inhibition of Wnt/β-catenin signaling suppresses myofibroblast differentiation of lung resident mesenchymal stem cells and pulmonary fibrosis. Sci. Rep. 2018;8:13644. doi: 10.1038/s41598-018-28968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Duan J., Gherghe C., Liu D., Hamlett E., Srikantha L., Rodgers L., Regan J.N., Rojas M., Willis M., Leask A., et al. Wnt1/βcatenin injury response activates the epicardium and cardiac fibroblasts to promote cardiac repair: Wnt1/βcatenin injury response regulates cardiac repair. EMBO J. 2012;31:429–442. doi: 10.1038/emboj.2011.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.He W., Dai C., Li Y., Zeng G., Monga S.P., Liu Y. Wnt/β-Catenin Signaling Promotes Renal Interstitial Fibrosis. J. Am. Soc. Nephrol. 2009;20:765–776. doi: 10.1681/ASN.2008060566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wei J., Fang F., Lam A.P., Sargent J.L., Hamburg E., Hinchcliff M.E., Gottardi C.J., Atit R., Whitfield M.L., Varga J. Wnt/β-catenin signaling is hyperactivated in systemic sclerosis and induces Smad-dependent fibrotic responses in mesenchymal cells. Arthritis Rheum. 2012;64:2734–2745. doi: 10.1002/art.34424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Henderson W.R., Chi E.Y., Ye X., Nguyen C., Tien Y.-T., Zhou B., Borok Z., Knight D.A., Kahn M. Inhibition of Wnt/β-catenin/CREB binding protein (CBP) signaling reverses pulmonary fibrosis. Proc. Natl. Acad. Sci. USA. 2010;107:14309–14314. doi: 10.1073/pnas.1001520107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Huang J., Wu S., Barrera J., Matthews K., Pan D. The Hippo Signaling Pathway Coordinately Regulates Cell Proliferation and Apoptosis by Inactivating Yorkie, the Drosophila Homolog of YAP. Cell. 2005;122:421–434. doi: 10.1016/j.cell.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 132.Camargo F.D., Gokhale S., Johnnidis J.B., Fu D., Bell G.W., Jaenisch R., Brummelkamp T.R. YAP1 Increases Organ Size and Expands Undifferentiated Progenitor Cells. Curr. Biol. 2007;17:2054–2060. doi: 10.1016/j.cub.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 133.Piccolo S., Dupont S., Cordenonsi M. The Biology of YAP/TAZ: Hippo Signaling and Beyond. Physiol. Rev. 2014;94:1287–1312. doi: 10.1152/physrev.00005.2014. [DOI] [PubMed] [Google Scholar]
- 134.Panciera T., Azzolin L., Cordenonsi M., Piccolo S. Mechanobiology of YAP and TAZ in physiology and disease. Nat. Rev. Mol. Cell Biol. 2017;18:758–770. doi: 10.1038/nrm.2017.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cai X., Wang K.-C., Meng Z. Mechanoregulation of YAP and TAZ in Cellular Homeostasis and Disease Progression. Front. Cell Dev. Biol. 2021;9:673599. doi: 10.3389/fcell.2021.673599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Noguchi S., Saito A., Mikami Y., Urushiyama H., Horie M., Matsuzaki H., Takeshima H., Makita K., Miyashita N., Mitani A., et al. TAZ contributes to pulmonary fibrosis by activating profibrotic functions of lung fibroblasts. Sci. Rep. 2017;7:42595. doi: 10.1038/srep42595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gokey J.J., Patel S.D., Kropski J.A. The Role of Hippo/YAP Signaling in Alveolar Repair and Pulmonary Fibrosis. Front. Med. 2021;8:752316. doi: 10.3389/fmed.2021.752316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Richeldi L., du Bois R.M., Raghu G., Azuma A., Brown K.K., Costabel U., Cottin V., Flaherty K.R., Hansell D.M., Inoue Y., et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014;370:2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 139.King T.E., Jr., Bradford W.Z., Castro-Bernardini S., Fagan E.A., Glaspole I., Glassberg M.K., Gorina E., Hopkins P.M., Kardatzke D., Lancaster L., et al. A Phase 3 Trial of Pirfenidone in Patients with Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2014;370:2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 140.Wollin L., Wex E., Pautsch A., Schnapp G., Hostettler K.E., Stowasser S., Kolb M. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015;45:1434–1445. doi: 10.1183/09031936.00174914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Togami K., Kanehira Y., Tada H. Possible involvement of pirfenidone metabolites in the antifibrotic action of a therapy for idiopathic pulmonary fibrosis. Biol. Pharm. Bull. 2013;36:1525–1527. doi: 10.1248/bpb.b13-00452. [DOI] [PubMed] [Google Scholar]
- 142.Conte E., Gili E., Fagone E., Fruciano M., Iemmolo M., Vancheri C. Effect of pirfenidone on proliferation, TGF-β-induced myofibroblast differentiation and fibrogenic activity of primary human lung fibroblasts. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2014;58:13–19. doi: 10.1016/j.ejps.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 143.Bizargity P., Liu K., Wang L., Hancock W.W., Visner G.A. Inhibitory effects of pirfenidone on dendritic cells and lung allograft rejection. Transplantation. 2012;94:114–122. doi: 10.1097/TP.0b013e3182584879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Györfi A.H., Matei A.E., Distler J.H.W. Targeting TGF-β signaling for the treatment of fibrosis. Matrix Biol. 2018;68–69:8–27. doi: 10.1016/j.matbio.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 145.Belperio J.A., Dy M., Burdick M.D., Xue Y.Y., Li K., Elias J.A., Keane M.P. Interaction of IL-13 and C10 in the pathogenesis of bleomycin-induced pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 2002;27:419–427. doi: 10.1165/rcmb.2002-0009OC. [DOI] [PubMed] [Google Scholar]
- 146.Parker J.M., Glaspole I.N., Lancaster L.H., Haddad T.J., She D., Roseti S.L., Fiening J.P., Grant E.P., Kell C.M., Flaherty K.R. A Phase 2 Randomized Controlled Study of Tralokinumab in Subjects with Idiopathic Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2018;197:94–103. doi: 10.1164/rccm.201704-0784OC. [DOI] [PubMed] [Google Scholar]
- 147.Maher T.M., Costabel U., Glassberg M.K., Kondoh Y., Ogura T., Scholand M.B., Kardatzke D., Howard M., Olsson J., Neighbors M., et al. Phase 2 trial to assess lebrikizumab in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2021;57:1902442. doi: 10.1183/13993003.02442-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ng B., Dong J., D’Agostino G., Viswanathan S., Widjaja A.A., Lim W.-W., Ko N.S.J., Tan J., Chothani S.P., Huang B., et al. Interleukin-11 is a therapeutic target in idiopathic pulmonary fibrosis. Sci. Transl. Med. 2019;11:eaaw1237. doi: 10.1126/scitranslmed.aaw1237. [DOI] [PubMed] [Google Scholar]
- 149.Richeldi L., Pérez E.R.F., Costabel U., Albera C., Lederer D.J., Flaherty K.R., Ettinger N., Perez R., Scholand M.B., Goldin J., et al. Pamrevlumab, an anti-connective tissue growth factor therapy, for idiopathic pulmonary fibrosis (PRAISE): A phase 2, randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 2020;8:25–33. doi: 10.1016/S2213-2600(19)30262-0. [DOI] [PubMed] [Google Scholar]
- 150.Horan G.S., Wood S., Ona V., Li D.J., Lukashev M.E., Weinreb P.H., Simon K.J., Hahm K., Allaire N.E., Rinaldi N.J., et al. Partial Inhibition of Integrin αvβ6 Prevents Pulmonary Fibrosis without Exacerbating Inflammation. Am J. Respir. Crit. Care Med. 2008;177:56–65. doi: 10.1164/rccm.200706-805OC. [DOI] [PubMed] [Google Scholar]
- 151.Kim Y.M., Kim E.C., Kim Y. The human lysyl oxidase-like 2 protein functions as an amine oxidase toward collagen and elastin. Mol. Biol. Rep. 2011;38:145–149. doi: 10.1007/s11033-010-0088-0. [DOI] [PubMed] [Google Scholar]
- 152.Chien J.W., Richards T.J., Gibson K.F., Zhang Y., Lindell K.O., Shao L., Lyman S.K., Adamkewicz J.I., Smith V., Kaminski N., et al. Serum lysyl oxidase-like 2 levels and idiopathic pulmonary fibrosis disease progression. Eur. Respir. J. 2014;43:1430–1438. doi: 10.1183/09031936.00141013. [DOI] [PubMed] [Google Scholar]
- 153.Findlay A.D., Foot J.S., Buson A., Deodhar M., Jarnicki A.G., Hansbro P.M., Liu G., Schilter H., Turner C.I., Zhou W. Identification and Optimization of Mechanism-Based Fluoroallylamine Inhibitors of Lysyl Oxidase-like 2/3. J. Med. Chem. 2019;62:9874–9889. doi: 10.1021/acs.jmedchem.9b01283. [DOI] [PubMed] [Google Scholar]
- 154.Pilling D., Buckley C.D., Salmon M., Gomer R.H. Inhibition of Fibrocyte Differentiation by Serum Amyloid P. J. Immunol. 2003;171:5537–5546. doi: 10.4049/jimmunol.171.10.5537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Pilling D., Roife D., Wang M., Ronkainen S.D., Crawford J.R., Travis E.L., Gomer R.H. Reduction of Bleomycin-Induced Pulmonary Fibrosis by Serum Amyloid P. J. Immunol. 2007;179:4035–4044. doi: 10.4049/jimmunol.179.6.4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Dillingh M.R., van den Blink B., Moerland M., van Dongen M.G.J., Levi M., Kleinjan A., Wijsenbeek M.S., Lupher Jr M.R., Harper D.M., Getsy J.A., et al. Recombinant human serum amyloid P in healthy volunteers and patients with pulmonary fibrosis. Pulm. Pharmacol. Ther. 2013;26:672–676. doi: 10.1016/j.pupt.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 157.van den Blink B., Dillingh M.R., Ginns L.C., Morrison L.D., Moerland M., Wijsenbeek M., Trehu E.G., Bartholmai B., Burggraaf J. Recombinant human pentraxin-2 therapy in patients with idiopathic pulmonary fibrosis: Safety, pharmacokinetics and exploratory efficacy. Eur. Respir. J. 2016;47:889–897. doi: 10.1183/13993003.00850-2015. [DOI] [PubMed] [Google Scholar]
- 158.Gagnon L., Leduc M., Thibodeau J.-F., Zhang M.-Z., Grouix B., Sarra-Bournet F., Gagnon W., Hince K., Tremblay M., Geerts L., et al. A Newly Discovered Antifibrotic Pathway Regulated by Two Fatty Acid Receptors. Am. J. Pathol. 2018;188:1132–1148. doi: 10.1016/j.ajpath.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 159.Khalil N., Manganas H., Ryerson C.J., Shapera S., Cantin A.M., Hernandez P., Turcotte E.E., Parker J.M., Moran J.E., Albert G.R., et al. Phase 2 clinical trial of PBI-4050 in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2019;53:1800663. doi: 10.1183/13993003.00663-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Raghu G., van den Blink B., Hamblin M.J., Brown A.W., Golden J.A., Ho L.A., Wijsenbeek M.S., Vasakova M., Pesci A., Antin-Ozerkis D.E., et al. Effect of Recombinant Human Pentraxin 2 vs. Placebo on Change in Forced Vital Capacity in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Clinical Trial. JAMA. 2018;319:2299–2307. doi: 10.1001/jama.2018.6129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.