Abstract
Background: Bacteria produce volatile organic compounds (VOCs) during growth, which can be detected by colorimetric sensor arrays (CSAs). The SpecifAST® system (Specific Diagnostics) employs this technique to enable antibiotic susceptibility testing (AST) directly from blood cultures without prior subculture of isolates. The aim of this study was to compare the SpecifAST® AST results and analysis time to the VITEK®2 (bioMérieux) system. Methods: In a 12-month single site prospective study, remnants of clinical positive monomicrobial blood cultures were combined with a series of antibiotic concentrations. Volatile emission was monitored at 37 °C via CSAs. Minimal Inhibitory Concentrations (MICs) of seven antimicrobial agents for Enterobacterales, Staphylococcus, and Enterococcus spp. were compared to VITEK®2 AST results. MICs were interpreted according to EUCAST clinical breakpoints. Performance was assessed by calculating agreement and discrepancy rates. Results: In total, 96 positive blood cultures containing Enterobacterales, Staphylococcus, and Enterococcus spp. were tested (269 bug–drug combinations). The categorical agreement of the SpecifAST® system compared to the VITEK®2 system was 100% and 91% for Gram-negatives and Gram-positives, respectively. Errors among Gram-positives were from coagulase-negative staphylococci. Overall results were available in 3.1 h (±0.9 h) after growth detection without the need for subculture steps. Conclusion: The AST results based on VOC detection are promising and warrant further evaluation in studies with a larger sample of bacterial species and antimicrobials.
Keywords: direct antimicrobial susceptibility testing, blood cultures, phenotypic antimicrobial susceptibility testing, volatile organic compounds, rapid diagnostics
1. Introduction
Rapid antimicrobial susceptibility test (AST) results of bacteria causing bloodstream infections are essential to guide targeted antimicrobial therapy, as ineffective empirical treatment increases the risk for morbidity and mortality in bacteremia [1,2]. Phenotypic AST results are preferable given the poor correlation between genotypes and phenotypes, the high number of resistance genes, and the lack of information on Minimal Inhibitory Concentrations (MIC) for clinical decision-making [3,4]. Phenotypic AST is dependent on bacterial growth rate and the lag phase of microbial growth is one of the time-limiting factors [3]. Current AST results using automated growth-based systems (e.g., VITEK®2, bioMérieux, Inc., Durham, NC, USA and BD PHOENIXTM, Franklin Lakes, NJ, USA) often take at least two days after bacterial growth detection, partly due to the need for a subsequent subculture step, to standardize the initial inoculum size for reliable results [5,6,7,8,9]. AST results during a single working shift are not possible when a subculture step is required, like in current AST methods. Subcultures might be unnecessary when measuring viability indirectly, e.g., by volatile organic compound (VOC) detection for AST, thus potentially enabling AST results within a single working shift.
VOCs are small metabolites (<300 Da) produced during bacterial growth. Several functions of VOCs have been described involving the interaction between other physically separated micro-organisms, such as modulation of virulence or growth, by diffusing in water or air [10]. The group of VOCs is heterogeneous, involving different chemical classes such as alcohols, ketones, and benzenoids [11]. Various biosynthetic pathways are involved in the production of VOCs contributing to this high diversity. Some VOCs can be seen as common metabolites, produced by many different bacteria or bacterial groups, while other VOCs are specific to certain genera or even species [10]. Due to the unique fingerprint of VOCs in bacterial species, the differentiation between species is possible and has been studied using different detection methods, such as an electric nose, ion mobility spectrometry, and gas chromatography/mass spectrometry (GC/MS) [12,13,14,15,16]. Nevertheless, these techniques come with some challenges, such as the inability to identify and quantify VOCs (electric nose), the large, lab-based instruments (GC-MS), and high costs (GC-MS and ion mobility spectrometry) [17,18]. In contrast, colorimetric sensor array (CSA) is a technique that measures VOCs by a sensor with chemo responsive indicators, changing color when exposed to different VOCs. This results in a fast, inexpensive, portable, and simple to operate method [18,19]. Successful differentiation between bacterial species using CSA has been described [19,20]. Additionally, identification of different yeast species was described previously. with promising results [21]. Susceptibility testing based on VOC detection is not widely studied, but discrimination between susceptible and resistant Staphylococcus aureus and Escherichia coli strains (for oxacillin and ampicillin or gentamicin, respectively) have been described previously [22,23,24]. The SpecifAST® system (Specific Diagnostics, CA, USA), a prototype of the RevealASTTM system, measures VOCs of bacteria combined with a selection of antibacterial agents by CSA.
The aim of our study was to compare SpecifAST® AST results and the corresponding analysis time to the VITEK®2 AST system directly from clinical positive blood cultures with Enterobacterales, Staphylococcus, and Enterococcus spp.
2. Methods
In a 12-month single site prospective laboratory study, the SpecifAST® system was evaluated in comparison to the current standard practice, using remnant materials of positive blood cultures collected in routine clinical care.
2.1. Objectives
The primary objective of this study was to assess the performance of the SpecifAST® system compared to the VITEK®2 system. Performance was measured by the categorical agreement, defined as agreement for the same categorical interpretation (susceptible (S), susceptible increased exposure (I), or resistant (R)) based on MIC values, in accordance with the 2021 European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoints [25]. The analysis time in hours and number of Colony Forming Units per milliliter (CFU/mL) were measured as secondary objectives.
2.2. Sample Selection
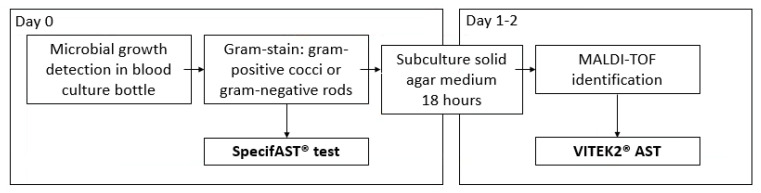
From May 2017 until June 2018, blood cultures were selected for SpecifAST® testing at the Medical Microbiology department of the Amsterdam University Medical Centers. Microbial growth in blood cultures was detected in the automated blood culture systems BACTEC™ FX (BACTEC; Becton Dickinson, Sparks, MD, USA) or BACT/ALERT®3 D (BacT/ALERT 3D; bioMérieux, Marcy, L’Étoile, France), followed by Gram-staining. Aerobic blood culture bottles containing Gram-negative rods or Gram-positive cocci were eligible for SpecifAST® testing (Figure 1, SpecifAST®, Specific Diagnostics, San Jose, CA, USA). One positive blood culture was randomly selected by the study staff, once or twice a day, due to limited capacity of the SpecifAST® system. Exclusion criteria were (1) positive blood cultures of the same patient enrolled in the past 30 days, to ensure enrolment of unique bacteremia episodes, or (2) polymicrobial blood cultures.
Figure 1.
Study procedures MALDI-TOF: matrix-assisted laser desorption-ionization/time-of-flight mass spectrometry.
2.3. Sample Preparation for SpecifAST® Testing
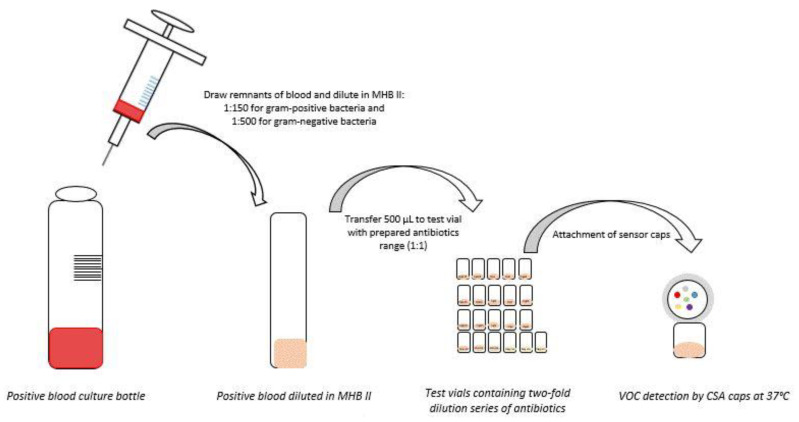
Blood cultures containing Gram-positive bacteria and Gram-negative bacteria were diluted 1:150 and 1:500, respectively, in cation adjusted Mueller Hinton II Broth (CA-MHB II). Samples were combined 1:1 with a range of antibiotics for SpecifAST® testing (Table 1, Figure 2). Enterobacterales spp. were tested for susceptibility to cefotaxime, ciprofloxacin, and meropenem; Enterococcus spp. were tested for susceptibility to vancomycin and ampicillin; and Staphylococcus spp. were tested for susceptibility to cefoxitin, oxacillin, and ampicillin (Table 1). The SpecifAST® software for VOC pattern analysis was trained for these three groups of (easily growing) bacterial species, which are also the most often identified in clinical blood cultures in our academic hospital. Each bug–drug combination was tested in triplicate, including a positive (no antibiotics) and negative control (no bacteria). Subcultures were performed to verify the number of CFU at the time of testing.
Table 1.
Combinations of micro-organisms and antimicrobial agents (bug–drug combinations) and corresponding antibiotic concentration ranges tested.
| Micro-Organism Group | Antimicrobial Agent | Specifast® Concentration Range | VITEK2® Concentration Range |
|---|---|---|---|
| Enterobacterales spp. | Ciprofloxacin Cefotaxime Meropenem |
0.25–4 μg/mL 0.25–64 μg/mL 0.25–16 μg/mL |
0.25–4 μg/mL 0.25–64 μg/mL 0.25–16 μg/mL |
| Staphylococcus spp. | Oxacillin + 2% NaCl a Vancomycin Cefoxitin |
0.25–4 μg/mL 0.5–32 μg/mL 6 μg/mL |
0.25–4 μg/mL 0.5–32 μg/mL 6 μg/mL |
| Enterococcus spp. | Ampicillin Vancomycin |
2–32 μg/mL 0.5–64 μg/mL |
2–32 μg/mL 0.5–32 μg/mL |
NaCl: Sodium chloride; a The first seven Staphylococcal blood cultures were tested with solely oxacillin, in the consecutive samples Oxacillin with two percent of sodium chloride was used.
Figure 2.
Sample preparation for SpecifAST® testing MHB II: Muller Hinton II Broth; CSA: Colorimetric sensor array; VOC: Volatile organic compounds.
2.4. SpecifAST® Testing
Colorimetric Sensor Array (CSA) caps (Specific Diagnostics) were used for detecting VOCs. Once the vials were inoculated with the bacterial suspension, a pre-assembled CSA cap was screwed on top of the vial. The cap contained six indicator spots which react to VOCs via color change in the presence of bacterial growth. The vials were inverted on a flat-bed scanner with the CSA caps facing the scanner. This assembly was incubated at 37 °C at 200 rpm, and VOC patterns were measured every 10 min. The total run time was 12 h, collecting a total of 72 images by the completion of the assay. An early (2018) version of Specific Diagnostics proprietary software was used to monitor the array of volatile-responsive sensors positioned in the headspace above each growing sample. Divergence of sensor responses in positive controls versus those with antibiotics were utilized to determine MICs.
2.5. Comparator Method
VITEK®2 (bioMérieux, Marcy, L’Étoile, France) AST was used as a comparator method (Figure 1). VITEK®2 AST cards N344, AST P567, and AST P586 were used for AST of Enterobacterales, Staphylococcus, and Enterococcus spp., respectively, based on matrix-assisted laser desorption-ionization/time-of-flight mass spectrometry (MALDI-TOF MS, Bruker Daltonics, BD, Bremen, Germany) results for bacterial identification after subculture on solid media.
2.6. Data Analysis
Positive blood cultures containing Enterobacterales, Staphylococcus, or Enterococcus spp. were eligible for analysis. Samples with errors leading to missing VITEK®2 or SpecifAST® test results were excluded from the analysis. MIC values were interpreted and compared in accordance with the EUCAST clinical breakpoints [25]. For all Staphylococcus spp., cefoxitin 6 mg/L breakpoint was used. In bug–drug combinations without categorical agreement, discrepancy rates were calculated: very major error (VME; falsely susceptible), major error (ME; falsely resistant), and minor error (mE; susceptible, increased exposure versus susceptible or resistant) [26]. Numbers and percentages of agreement and corresponding error rates were calculated using IBM® SPSS® Statistics 26.
2.7. Ethical Considerations
This study was exempted from medical ethical review and informed consent as anonymized leftover materials were used. Specimens were only used when patients had not indicated any objection for anonymized research use of specimens according to local regulations.
3. Results
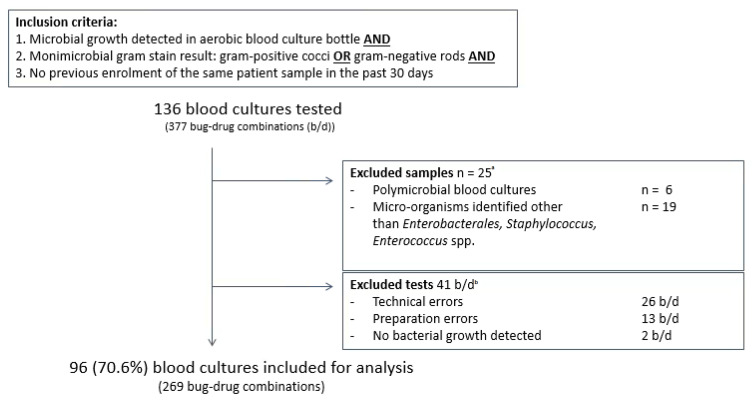
From May 2017 until June 2018, 136 aerobic positive clinical aerobic blood cultures containing Gram-positive cocci or Gram-negative rods were tested in the SpecifAST® and VITEK®2 system. Twenty-five samples were excluded for analysis due to polymicrobial growth (6) or non-eligible bacterial species such as Streptococcus spp. or Pseudomonas aeruginosa (19) (Figure 3; Supplemental Material Table S1). Another 15 blood cultures were excluded since tests results (44 bug/drug combinations) were not available due to errors: 13 preparation errors, 26 SpecifAST® technical errors, and 2 errors due to lack of bacterial growth in both SpecifAST® and VITEK®2 testing (Supplemental Material Table S2).
Figure 3.
Baseline figure in and excluded samples. Inclusion criteria were microbial growth detection in aerobic blood culture bottles and monomicrobial gram stain result with gram-positive cocci or gram-negative rods and no previous enrolment of the same patient in the past 30 days. Exclusion criteria were polymicrobial blood cultures, micro-organisms, other than Enterobacterales spp., Staphylococcus spp. or Enterococcus spp., and errors leading to missing data. Error details are provided in Supplementary Table S2. B/d: bug–drug combinations. a 25 blood culture samples and all corresponding b/d combinations (67) were excluded from analysis based on polymicrobial growth or micro-organism identification result. b In 15 blood culture samples, all b/d combinations were excluded from analysis due to errors or absence of microbial growth. In 2 blood culture samples, one or more b/d combinations were excluded from analysis due to errors or absence of microbial growth. In total, 41 b/d combinations were excluded.
A total of 96 positive blood cultures (269 bug–drug combinations) were included for analysis: 46 Enterobacterales spp. (47.9%), 40 Staphylococcus spp. (41.7%), and 10 Enterococcus spp. (10.4%). Eight different Enterobacterales spp., mostly Escherichia coli (n = 28, 60.9%), four different Staphylococcus spp. and two different Enterococcus spp., were identified (Table 2). No meropenem resistant Enterobacterales spp. or methicillin resistant Staphylococcus aureus were found (Table 3). One vancomycin resistant Enterococcus spp. was found. In four samples, species were identified as Extended Spectrum Beta Lactamase (ESBL) producing Enterobacterales.
Table 2.
Identified micro-organisms in included blood culture samples.
| Enterobacterales spp. | N = 46 |
|---|---|
| Citrobacter freundii | 1 (2.2%) |
| Klebsiella aerogenes | 1 (2.2%) |
| Escherichia coli | 28 (60.9%) |
| Klebsiella pneumoniae | 9 (19.6%) |
| Klebsiella variicola | 3 (6.5%) |
| Morganella morganii | 3 (6.5%) |
| Proteus mirabilis | 1 (2.2%) |
| Salmonella typhi | 1 (2.2%) |
| Enterococcus spp. | N = 10 |
| Enterococcus faecalis | 3 (30.0%) |
| Enterococcus faecium | 7 (70%) |
| Staphylococcus spp. | N = 40 |
| Staphylococcus aureus | 12 (30.0%) |
| Staphylococcus epidermidis | 13 (32.5%) |
| Staphylococcus hominis | 11 (27.5%) |
| Staphylococcus capitis | 4 (10.0%) |
Table 3.
Number and percentages of categorical and essential agreement between SpecifAST® and VITEK2® AST results, corresponding error rates and percentages, resistance rates, and time to test results per micro-organism group and antimicrobial agent.
| Antimicrobial Agent | Number of Clinical Blood Cultures Tested | Number of AB Tested (B/D) | CA | VME | ME | mE | R | TTR (h) SpecifAST Mean (SD) |
TTR (h) VITEK2 a Mean (SD) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Enterobacterales spp. | Cefotaxime | 45 (46.9%) | 45 (16.7%) | 45 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 7 (15.6%) | ||
| Ciprofloxacin | 44 (45.8%) | 44 (16.4%) | 44 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 9 (20.5%) | |||
| Meropenem | 45 (46.9%) | 45 (16.7%) | 45 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Total | 46 (47.9%) | 134 (49.8%) | 134 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 16 (11.9%) | 2.8 (0.6) | 9.8 (2.6) | |
| Staphylococcus spp. | Cefoxitin | 38 (39.6%) | 38 (14.1%) | 34 (89.4%) | 4 (25%) | 0 (0%) | n.a. | 16 (42.1%) | ||
| Oxacillin | 39 (40.6%) | 39 (14.5%) | 34 (87.1%) | 1 (7.1%) | 4 (16%) | 0 (0%) | 14 (35.9%) | |||
| Vancomycin | 39 (40.6%) | 39 (14.5%) | 37 (94.9%) | 0 (0%) | 2 (5.1%) | 0 (0%) | 0 (0%) | |||
| Total | 40 (41.7%) | 116 (43.1%) | 105 (90.5%) | 5 (16.7%) | 6 (7.0%) | 0 (0%) | 30 (25.9%) | 3.4 (1.1) | 11.5 (2.4) | |
| Enterococcus spp. | Ampicillin | 10 (10.4%) | 9 (3.3%) | 8 (88.9%) | 0 (0%) | 0 (0%) | 1 (11.1%) | 5 (55.6%) | ||
| Vancomycin | 10 (10.4%) | 10 (3.7%) | 10 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | |||
| Total | 10 (10.4%) | 19 (7.1%) | 18 (94.7%) | 0 (0%) | 0 (0%) | 1 (1.7%) | 6 (31.6%) | 3.2 (0.5) | 8.8 (1.6) | |
| Overall | 96 (100%) | 269 (100%) | 257 (95.5%) | 5 (9.6%) | 6 (2.8%) | 1 (0.4%) | 52 (19.3%) | 3.1 (0.9) | 10.5 (2.6) |
Data are n (%) unless otherwise indicated. a12 b/d combinations missing VITEK2® TTR. AB: antibiotics; CA: categorical agreement; VME: very major error (the number of false susceptible b/d in SpecifAST®, divided by the number of resistant b/d in VITEK2®); ME: major error (the number of false resistant b/d in SpecifAST®, divided by the number of susceptible b/d in VITEK2®); mE: minor error (number of intermediate versus resistant or susceptible b/d, divided by the total number of b/d tested); NA: not available; R: resistance; TTR: time to test result.
3.1. Primary Outcome SpecifAST® Performance
The overall categorical agreement between both AST methods for Enterobacterales spp. was 100% (134/134), as no discrepancies in interpretative results for ciprofloxacin, cefotaxime, and meropenem were found (Table 3). In Staphylococcus spp. the categorical agreement was lower: 90.5% (105/116), due to 5 very major errors (5/30, 16.7%) and 6 major errors (6/86, 7.0%). All five VME concerned Staphylococcus epidermidis, whereby four cefoxitin resistant strains (MIC 6 mg/L) and one oxacillin resistant strain (MIC > 2 mg/L) were reported as susceptible (MIC ≤ 0.25 mg/L) by SpecifAST® (Supplementary Material Table S3E,F). The six major errors concerned Staphylococcus aureus (2) and coagulase negative staphylococci, CoNS (4) with discrepancies in oxacillin and vancomycin susceptibilities (Supplementary Material Table S3D,E,G,H). In Enterococcus spp. the overall categorical agreement was 94.7% due to one minor error (1/19). The overall sensitivity and specificity of the SpecifAST method compared to the VITEK2 was 91% (95%-CI: 83.1–98.9) and 97% (95%-CI: 94.8–99.2), Supplementary Table S4.
3.2. Secondary Outcomes: Analysis Time and Number of CFU
The mean analysis time was 3.1 h (+/−0.9 h) by the SpecifAST® system compared to 10.5 h (2.6 +/−SD) by VITEK®2, which corresponds to a 70.5% reduction. A subculture step of 18–24 h was required prior VITEK® testing, while this was not needed prior to SpecifAST® testing. The time between bacterial growth detection in the automated blood culture systems and the initiation of the SpecifAST® tests varied between 2.5 h and 38.5 h. Blood cultures were used directly for SpecifAST® tests, without standardization of the inoculum, and the mean numbers of CFU per blood culture bottle were 108.80 ± 0.69 and 108.75 ± 0.45 for Gram-positives and Gram-negatives, respectively.
4. Discussion
The SpecifAST® AST results in our proof-of-principle laboratory study are promising for Enterobacterales spp., as full categorical agreement was found. Given the small number of ciprofloxacin and cefotaxime resistant strains, and the lack of meropenem resistant strains, further studies are required to establish the performance of detecting resistance.
The categorical agreement for Gram-positives was acceptable (≥90%), but the error rates were high. All very major errors found in this study included oxacillin or cefoxitin resistance in Staphylococcus epidermidis. Beta-lactam resistance (such as oxacillin and cefoxitin resistance) in CoNS is very common [27,28] and mostly mediated by alteration of the penicillin-binding-protein (PBP2a), encoded by the MecA gene [29]. Detection of beta-lactam resistance in CoNS is complex, even in current AST methods, as resistance can be expressed solely in a small proportion of cells (heterotypic phenotype) [30,31,32]. An essential difference between the SpecifAST® system and the VITEK®2 system is the use of a single or a few colonies from subcultures by the VITEK®2 system, while the SpecifAST® system directly uses positive blood cultures. It could be hypothesized that VOC detection in the entire bacterial population represents the main expressed beta-lactam phenotype in CoNS. Therefore, SpecifAST® results could hypothetically be more representative of the entire bacterial population present in the blood culture. For beta-lactam resistance detection in CoNS, further studies to assess whether AST of the entire bacterial population might be an advantage compared to AST of single colonies, which should include standard reference testing for beta-lactam resistance either by PBP2a culture colony test or MecA PCR [30].
Susceptibility testing based on VOCs as surrogates of viability is a new area of research. The correlation between VOCs and AST results in different combinations of bacteria and antibiotics may vary [3]. There are many factors that influence VOC levels, either directly, e.g., temperature or humidity (volatility), or indirectly, e.g., oxygen or the nutrient availability in a growth medium (bacterial metabolism) [10]. Further investigations should aim to standardize those factors to limited variability in results.
The time range between bacterial growth detection and SpecifAST® testing was broad due to the laboratory operating hours. The corresponding inoculum sizes for SpecifAST® testing also varied widely. It is notable that a high categorical agreement was found despite a wide range of CFUs in tested samples, as standardized inoculum sizes are required for most AST systems for reliable MIC values [33]. This might be due to the fact that SpecifAST® detects changes in bacterial metabolic products instead of bacterial growth. By facilitating non-standardized initial inoculum sizes and omitting prior subculture steps, SpecifAST® enables the rapid availability of test results, possibly facilitating same-day test results after bacterial growth detection. As we did not formally assess the correlation between inoculum size and AST results, the reliability of VOC-based AST without subculture steps should be assessed in future studies.
One of the limitations of this study was the comparison with the VITEK®2 system, instead of a reference method for AST, such as broth dilution [34,35]. The VITEK®2 system is our current clinical reference test like many clinical laboratories, which use less time-consuming and laborious phenotypic and genotypic AST tests [34,35]. Although the VITEK®2 system has proven to be a reliable AST method, it is possible that some of the discordant results were due to VITEK®2 errors. Further studies should therefore compare the SpecifAST® system to a reference method.
Second, only a limited number and type of bacterial species and antibiotics were included in this study. Only Enterobacterales, Staphylococcus, and Enterococcus spp. were eligible for testing with the SpecifAST® prototype. Future studies should assess AST results of other bacterial species and multiple antibiotics using the automated Reveal ASTTM system, which is an updated version of the SpecifAST® system that enables parallel identification and susceptibility testing for a panel of antibacterial agents. Polymicrobial blood cultures were excluded from our analysis and some concerns exist related to the use of polymicrobial specimens. First, it is known that bacterial species can affect VOC production of other species, which might play a role in polymicrobial specimens [36]. Second, direct positive blood culture testing provides a combined resistance phenotype of all bacteria present in polymicrobial specimens, which might not be clinically relevant. AST results in polymicrobial specimens varied when using another rapid system that enables AST without prior subcultures, the Accelerate Pheno™ system (Accelerate Diagnostics, Tucson, AZ) [37], based on fluorescence in-situ hybridization [38,39]. Follow-up studies should assess whether AST results are reliable in various polymicrobial specimens.
Finally, this study was performed in a setting with low AMR levels. To evaluate the SpecifAST® performance in detecting resistance, further studies in settings with higher AMR prevalence are required.
5. Conclusions
Measuring volatile organic compounds is a novelty for antimicrobial susceptibility testing. Our proof-of-principle results are promising, and further investigation is warranted to establish the reliability of results in multiple combinations of bacteria and antimicrobials.
Acknowledgments
We thank Janine van Baar, Esiyoma Odiete and Patrick Habermehl for performing SpecifAST® runs during their internship at our department.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11060705/s1, Table S1: Samples excluded based on isolated micro-organisms other than Enterobacterales spp., Staphylococcus spp. or Enterococcus spp.; Table S2: Specifications of errors occurred; Table S3: Minimal inhibitory concentrations of Enterobacterales, Staphylococcus and Enterococcus spp. and corresponding tested antimicrobials measured by SpecifAST® and VITEK®2; Table S4: Sensitivity and specificity of SpecifAST® method compared to VITEK®2.
Author Contributions
Conceptualization, C.E.V.; Formal analysis, S.D.K., and S.H.; Funding acquisition, C.E.V.; Investigation, S.D.K., S.H. and P.S.; Methodology, S.D.K., C.S., M.D.d.J. and C.E.V.; Project administration, S.D.K., S.H. and P.S.; Resources, P.S. and P.R.; Supervision, C.S., M.D.d.J. and C.E.V.; Writing–original draft, S.D.K.; Writing–review and editing, S.D.K., S.H., C.S., P.S., P.R., M.D.d.J. and C.E.V. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was exempted from medical ethical review and informed consent, as anonymized remnants of blood cultures collected for routine care were used. According to local regulations, specimens were only used when patients had not indicated any objection for anonymized research use of specimens.
Informed Consent Statement
Not applicable.
Data Availability Statement
The dataset is fully accessible under CC0 license on figshare via DOI: 10.6084/m9.figshare.12052782.
Conflicts of Interest
Currently unpaid advisor dr. Caroline Visser (CEV) for Specific Diagnostics and past unpaid advisor Bezoldigi. SpecifAST® instrument with associated consumables, support and service for the instrument were supplied by Specific Diagnostics (PS and PR).
Funding Statement
This study is funded by Amsterdam UMC (location Academic Medical Center) innovation impuls grant 2017-26. SpecifAST® instrument with associated consumables and service for the instrument were supplied by Specific Diagnostics.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kumar A., Ellis P., Arabi Y., Roberts D., Light B., Parrillo J.E., Dodek P., Wood G., Kumar A., Simon D., et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136:1237–1248. doi: 10.1378/chest.09-0087. [DOI] [PubMed] [Google Scholar]
- 2.Adhikari N.K., Fowler R.A., Bhagwanjee S., Rubenfeld G.D. Critical care and the global burden of critical illness in adults. Lancet. 2010;376:1339–1346. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Belkum A., Burnham C.D., Rossen J.W.A., Mallard F., Rochas O., Dunne W.M., Jr. Innovative and rapid antimicrobial susceptibility testing systems. Nat. Rev. Microbiol. 2020;18:299–311. doi: 10.1038/s41579-020-0327-x. [DOI] [PubMed] [Google Scholar]
- 4.Bard J.D., Lee F. Why Can’t We Just Use PCR? The Role of Genotypic versus Phenotypic Testing for Antimicrobial Resistance Testing. Clin. Microbiol. Newslett. 2018;40:87–95. doi: 10.1016/j.clinmicnews.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dubourg G., Lamy B., Ruimy R. Rapid phenotypic methods to improve the diagnosis of bacterial bloodstream infections: Meeting the challenge to reduce the time to result. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2018;24:935–943. doi: 10.1016/j.cmi.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 6.Machen A., Drake T., Wang Y.F. Same day identification and full panel antimicrobial susceptibility testing of bacteria from positive blood culture bottles made possible by a combined lysis-filtration method with MALDI-TOF VITEK mass spectrometry and the VITEK2 system. PLoS ONE. 2014;9:e87870. doi: 10.1371/journal.pone.0087870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romero-Gómez M.P., Gómez-Gil R., Paño-Pardo J.R., Mingorance J. Identification and susceptibility testing of microorganism by direct inoculation from positive blood culture bottles by combining MALDI-TOF and Vitek-2 Compact is rapid and effective. J. Infect. 2012;65:513–520. doi: 10.1016/j.jinf.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 8.Choi J., Jeong H.Y., Lee G.Y., Han S., Han S., Jin B., Lim T., Kim S., Kim D.Y., Kim H.C., et al. Direct, rapid antimicrobial susceptibility test from positive blood cultures based on microscopic imaging analysis. Sci. Rep. 2017;7:1148. doi: 10.1038/s41598-017-01278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Puttaswamy S., Gupta S.K., Regunath H., Smith L.P., Sengupta S. A Comprehensive Review of the Present and Future Antibiotic Susceptibility Testing (AST) Systems. Arch. Clin. Microbiol. 2018;9:83. doi: 10.4172/1989-8436.100083. [DOI] [Google Scholar]
- 10.Weisskopf L., Schulz S., Garbeva P. Microbial volatile organic compounds in intra-kingdom and inter-kingdom interactions. Nat. Rev. Microbiol. 2021;19:391–404. doi: 10.1038/s41579-020-00508-1. [DOI] [PubMed] [Google Scholar]
- 11.Schulz-Bohm K., Martín-Sánchez L., Garbeva P. Microbial Volatiles: Small Molecules with an Important Role in Intra- and Inter-Kingdom Interactions. Front. Microbiol. 2017;8:2484. doi: 10.3389/fmicb.2017.02484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ratiu I.A., Ligor T., Bocos-Bintintan V., Buszewski B. Mass spectrometric techniques for the analysis of volatile organic compounds emitted from bacteria. Bioanalysis. 2017;9:1069–1092. doi: 10.4155/bio-2017-0051. [DOI] [PubMed] [Google Scholar]
- 13.Steppert I., Schönfelder J., Schultz C., Kuhlmeier D. Rapid in vitro differentiation of bacteria by ion mobility spectrometry. Appl. Microbiol. Biotechnol. 2021;105:4297–4307. doi: 10.1007/s00253-021-11315-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunze-Szikszay N., Euler M., Kuhns M., Thieß M., Groß U., Quintel M., Perl T. Headspace analyses using multi-capillary column-ion mobility spectrometry allow rapid pathogen differentiation in hospital-acquired pneumonia relevant bacteria. BMC Microbiol. 2021;21:69. doi: 10.1186/s12866-021-02102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boots A.W., Smolinska A., van Berkel J.J., Fijten R.R., Stobberingh E.E., Boumans M.L., Moonen E.J., Wouters E.F., Dallinga J.W., Van Schooten F.J. Identification of microorganisms based on headspace analysis of volatile organic compounds by gas chromatography-mass spectrometry. J. Breath Res. 2014;8:027106. doi: 10.1088/1752-7155/8/2/027106. [DOI] [PubMed] [Google Scholar]
- 16.Guo L., Qiu Z., Wang Y., Yu K., Zheng X., Li Y., Liu M., Wang G., Guo N., Yang M., et al. Volatile Organic Compounds to Identify Infectious (Bacteria/Viruses) Diseases of the Central Nervous System: A Pilot Study. Eur. Neurol. 2021;84:325–332. doi: 10.1159/000507188. [DOI] [PubMed] [Google Scholar]
- 17.Maugeri G., Lychko I., Sobral R., Roque A.C.A. Identification and Antibiotic-Susceptibility Profiling of Infectious Bacterial Agents: A Review of Current and Future Trends. Biotechnol. J. 2019;14:e1700750. doi: 10.1002/biot.201700750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kangas M.J., Burks R.M., Atwater J., Lukowicz R.M., Williams P., Holmes A.E. Colorimetric Sensor Arrays for the Detection and Identification of Chemical Weapons and Explosives. Crit. Rev. Anal. Chem. 2017;47:138–153. doi: 10.1080/10408347.2016.1233805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim S.H., Mix S., Xu Z., Taba B., Budvytiene I., Berliner A.N., Queralto N., Churi Y.S., Huang R.S., Eiden M., et al. Colorimetric sensor array allows fast detection and simultaneous identification of sepsis-causing bacteria in spiked blood culture. J. Clin. Microbiol. 2014;52:592–598. doi: 10.1128/JCM.02377-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carey J.R., Suslick K.S., Hulkower K.I., Imlay J.A., Imlay K.R., Ingison C.K., Ponder J.B., Sen A., Wittrig A.E. Rapid identification of bacteria with a disposable colorimetric sensing array. J. Am. Chem. Soc. 2011;133:7571–7576. doi: 10.1021/ja201634d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shrestha N.K., Lim S.H., Wilson D.A., SalasVargas A.V., Churi Y.S., Rhodes P.A., Mazzone P.J., Procop G.W. The combined rapid detection and species-level identification of yeasts in simulated blood culture using a colorimetric sensor array. PLoS ONE. 2017;12:e0173130. doi: 10.1371/journal.pone.0173130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smart A., de Lacy Costello B., White P., Avison M., Batty C., Turner C., Persad R., Ratcliffe N. Sniffing out resistance—Rapid identification of urinary tract infection-causing bacteria and their antibiotic susceptibility using volatile metabolite profiles. J. Pharm. Biomed. Anal. 2019;167:59–65. doi: 10.1016/j.jpba.2019.01.044. [DOI] [PubMed] [Google Scholar]
- 23.Wiesner K., Jaremek M., Pohle R., von Sicard O., Stuetz E. Monitoring of Bacterial Growth and Rapid Evaluation of Antibiotic Susceptibility by Headspace Gas Analysis. Procedia Eng. 2014;87:332–335. doi: 10.1016/j.proeng.2014.11.750. [DOI] [Google Scholar]
- 24.Allardyce R.A., Hill A.L., Murdoch D.R. The rapid evaluation of bacterial growth and antibiotic susceptibility in blood cultures by selected ion flow tube mass spectrometry. Diagn. Microbiol. Infect. Dis. 2006;55:255–261. doi: 10.1016/j.diagmicrobio.2006.01.031. [DOI] [PubMed] [Google Scholar]
- 25.(EUCAST) E.C.o.A.S.T. Clinical Breakpoints-Breakpoints and Guidance. [(accessed on 5 July 2021)]. Available online: https://www.eucast.org/clinical_breakpoints/
- 26.Humphries R.M., Ambler J., Mitchell S.L., Castanheira M., Dingle T., Hindler J.A., Koeth L., Sei K. CLSI Methods Development and Standardization Working Group Best Practices for Evaluation of Antimicrobial Susceptibility Tests. J. Clin. Microbiol. 2018;56:e01934-17. doi: 10.1128/JCM.01934-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Archer G.L., Scott J. Conjugative transfer genes in staphylococcal isolates from the United States. Antimicrob. Agents Chemother. 1991;35:2500–2504. doi: 10.1128/AAC.35.12.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.York M.K., Gibbs L., Chehab F., Brooks G.F. Comparison of PCR detection of mecA with standard susceptibility testing methods to determine methicillin resistance in coagulase-negative staphylococci. J. Clin. Microbiol. 1996;34:249–253. doi: 10.1128/jcm.34.2.249-253.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morris C.P., Simner P.J. Tailoring Antimicrobial Susceptibility Testing to Individual Species of Coagulase-Negative Staphylococci: Next Up, Staphylococcus epidermidis. J. Clin. Microbiol. 2019;57:e01391-19. doi: 10.1128/JCM.01391-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naccache S.N., Callan K., Burnham C.A., Wallace M.A., Westblade L.F., Dien Bard J. Evaluation of Oxacillin and Cefoxitin Disk Diffusion and Microbroth Dilution Methods for Detecting mecA-Mediated β-Lactam Resistance in Contemporary Staphylococcus epidermidis Isolates. J. Clin. Microbiol. 2019;57:e00961-19. doi: 10.1128/JCM.00961-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Archer G.L., Climo M.W. Antimicrobial susceptibility of coagulase-negative staphylococci. Antimicrob. Agents Chemother. 1994;38:2231–2237. doi: 10.1128/AAC.38.10.2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dickinson T.M., Archer G.L. Phenotypic expression of oxacillin resistance in Staphylococcus epidermidis: Roles of mecA transcriptional regulation and resistant-subpopulation selection. Antimicrob. Agents Chemother. 2000;44:1616–1623. doi: 10.1128/AAC.44.6.1616-1623.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsik F.J. Antimicrobial Susceptibility Testing. In: Mahon C.R., Lehman D.C., Manuselis G., editors. Textbook of Diagnostic Microbiology. 4th ed. Saunders Elsevier; Maryland Heights, MO, USA: 2011. pp. 276–314. [Google Scholar]
- 34.Jorgensen J.H., Ferraro M.J. Antimicrobial susceptibility testing: A review of general principles and contemporary practices. Clin. Infect. Dis. 2009;49:1749–1755. doi: 10.1086/647952. [DOI] [PubMed] [Google Scholar]
- 35.M07-A11; Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, 10th ed.; Approved Standard. Clinical and Laboratory Standards Institute, Wayne, PA, USA: 2018
- 36.Schulz-Bohm K., Zweers H., de Boer W., Garbeva P. A fragrant neighborhood: Volatile mediated bacterial interactions in soil. Front. Microbiol. 2015;6:1212. doi: 10.3389/fmicb.2015.01212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robinson E.D., Stilwell A., Attai A.E., Donohue L.E., Shah M.D., Hill B.K., Elliott Z.S., Poulter M., Brewster F., Cox H.L., et al. Implementation of a Rapid Phenotypic Susceptibility Platform for Gram-Negative Bloodstream Infections with Paired Antimicrobial Stewardship Intervention: Is the Juice Worth the Squeeze? Clin. Infect. Dis. 2021;73:783–792. doi: 10.1093/cid/ciab126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Charnot-Katsikas A., Tesic V., Love N., Hill B., Bethel C., Boonlayangoor S., Beavis K.G. Use of the Accelerate Pheno System for Identification and Antimicrobial Susceptibility Testing of Pathogens in Positive Blood Cultures and Impact on Time to Results and Workflow. J. Clin. Microbiol. 2018;56:e01166-17. doi: 10.1128/JCM.01166-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marschal M., Bachmaier J., Autenrieth I., Oberhettinger P., Willmann M., Peter S. Evaluation of the Accelerate Pheno System for Fast Identification and Antimicrobial Susceptibility Testing from Positive Blood Cultures in Bloodstream Infections Caused by Gram-Negative Pathogens. J. Clin. Microbiol. 2017;55:2116–2126. doi: 10.1128/JCM.00181-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset is fully accessible under CC0 license on figshare via DOI: 10.6084/m9.figshare.12052782.