Abstract
Since the outbreak of the coronavirus disease 2019 (COVID-19), there have been heightened levels of fear worldwide. The steadily increasing number of COVID-19 cases in Nigeria as reported by the Nigerian center for Disease Control has led to different behavioral responses influenced by perceived threat and efficacy. This study aimed to understand the levels of perceived threat and efficacy to COVID-19 in Nigeria across various demographic groups using the Extended Parallel Process Model. This was a cross-sectional study conducted across all states in Nigeria, between May and June 2020. The majority of respondents were recruited via social media, with a smaller fraction interviewed face to face due to Government restrictions on movement in some states. Based on findings, respondents had high exposure to COVID-19 messages on social media (85%), followed by television (67%), radio (54%), and the Nigeria center for Disease Control short message services (52%). High exposure to COVID-19 messages across all media platforms was significantly associated with perceived severity, response efficacy, and self-efficacy (p< 0.01). Also, with an increase in age, there was a corresponding increase in the perceived susceptibility to COVID-19. As the level of education increased, respondents' perceived severity, susceptibility, self-efficacy, and response efficacy to COVID-19 increased. A chi-square test between demographic variables and intermediate outcome variables (danger or fear control process) showed a significant association with age, gender, highest educational level, and employment type. From the findings, the majority of respondents were less likely to practice the recommended protective behaviors as COVID-19 was not perceived as a threat. The proportion of the Nigerian population willing to take up recommended preventive behaviors were just 15%. Developing messages with an appropriate balance between threat and efficacy to target different audiences would likely encourage the adoption and practice of recommended COVID-19 preventive behaviors.
Keywords: Risk perception, COVID-19, Extended parallel process model, Centre for Communication and Social Impact
Introduction
In December 2019, Wuhan, Hubei province of China recorded an outbreak of pneumonia cases of unknown cause. These pneumonia cases were subsequently identified as the novel coronavirus disease (COVID-19) [1,12]; which later spread globally. According to the World Health Organization (WHO), over twenty-six million people worldwide have been infected with COVID-19, with over eight hundred thousand fatalities globally as of 7th of September 2020 [28]. (WHO Coronavirus Disease (COVID-19) Dashboard, 2020). The Nigerian Federal Ministry of Health confirmed the first case of COVID-19 in Ogun State, South-West Nigeria, on 7th February 2020. Over a period of seven months, Nigeria had recorded over fifty-five thousand confirmed cases with over a thousand fatalities [16].
COVID-19 has been documented to spread mainly from person to person through infected respiratory droplets. Globally, the most effective way of reducing the spread of the virus is through regular washing of hands with soap and water, maintaining a physical distance of at least two meters, proper hygiene, and the wearing of a face mask [5,7,14,30]. In addition, precautionary measures such as nationwide lockdown were initiated by countries like Nigeria to forestall unnecessary movement thereby limiting the spread of COVID-19.
Recently published studies have highlighted the impact of the perception of threat to COVID-19 on psychological and behavioral responses ([4], p. 19; [19,27]). The psychological responses, especially anxiety and fear have been documented to lead to reluctant adoption of COVID-19 preventive behavior [19]. Behavioral response to risk communication campaigns during pandemics is often determined by people's perceived level of threat and efficacy. In the early phase of the COVID-19 pandemic in Nigeria, risk communication messages were disseminated across various media platforms such as radio, television, prints, social media, and short message service (SMS) to inform Nigerians about the associated risks and mode of prevention for COVID-19. Understanding the level of perceived threat and efficacy to COVID-19 would support the development of effective risk communication messages.
The Extended Parallel Process Model (EPPM) has been used to assess the levels of perceived threat and efficacy with respect to adherence to preventive health behaviors [3,15]. As far as the authors know, this is the first study applying the EPPM to understand COVID-19 behavioral response. This study is aimed at assessing the level of threat and efficacy across various demographic groups.
Theoretical framework
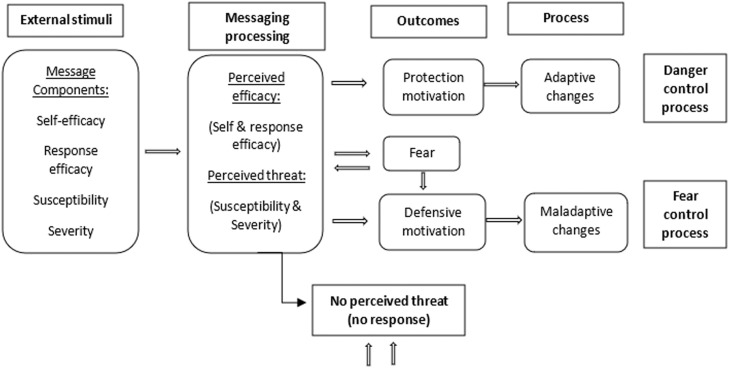
This paper draws on the Extended Parallel Process Model which was introduced by Witte [29]. It emphasizes the role of threat and efficacy as key elements required for a behavior change. The model is used to explain how individuals process and respond to fear appeal messages targeted at promoting protective health behaviors [2]. According to Carey & Sarma [6], the EPPM was developed as a framework to understand complex psychological processes triggered in response to threat messages. Since its introduction, the model has been applied extensively in health communication research [22].
The EPPM describes how the ‘combination of rational considerations and emotional reactions determine behavioral decisions’ (Health Communication Capacity Collaborative, 2014:1). As shown in Fig. 1 , the construct of threat has two subcomponents: severity (perception of the seriousness of the threat) and susceptibility (perceived probability of experiencing a threat). Efficacy also has two subcomponents: response efficacy (perceived effectiveness of alternate responses to threat) and self-efficacy (belief about one's ability to perform a behavior) [8,29].
Fig. 1.
The Extended Parallel Process Model. Adopted from [22].
The EPPM has been used successfully to understand messaging around various preventive health programs, including building confidence in the use of vaccines [2,24], early breast cancer diagnosis [31], reduction of substance use, smoking prevention program [8,9], improvement of treatment uptake for HIV/AIDS [15], and willingness of employees to work during an influenza pandemic [26].
Methods
This was a cross-sectional study conducted across the 36 states in Nigeria, including the Federal Capital Territory. Data collection took place between May 19 and June 5, 2020. During this period, the Federal Government instituted a nationwide lockdown, however, in some of the study states the lockdown was partial. Data was collected through an online questionnaire and face to face interviews in states where lockdown was partial. The survey tool was deployed using Microsoft forms through social media platforms (Instagram, Twitter, Facebook, WhatsApp). Face to face interviewers adhered to COVID-19 preventive measures while administering the questionnaire. Convenience and snowball sampling approaches were used to recruit respondents. Participation was voluntary and only respondents aged 18 and above were eligible to participate in the study.
Survey instrument
The data collection instrument included questions on demographics, media consumption habits, perceived threat (perceived severity and susceptibility), and perceived efficacy (self and response efficacy). This survey tool was designed and administered in English. The questionnaire was designed based on existing questionnaires from peer-reviewed studies [13,20] using the EPPM framework. The Cronbach's alpha coefficient was 0.6 and 0.88 for threat and efficacy variables, respectively, this alpha value is similar to that found in other studies [10,25].
Demographic information collected included state of residence, gender, age, marital status, highest level of education attained, and primary employment. The level of exposure to COVID-19 messages was assessed by measuring the frequency of getting information from television, radio, social media, and text messages from the Nigeria center for Disease Control (NCDC). Responses were categorized into high (4 to 7 times a week) or low (0 to 3 times a week).
The perceived threat was measured with three scaled items. Questions were asked about the participant's perceived severity (1 item) and susceptibility (2 items) to COVID-19. A sample item for perceived severity included, “I believe that COVID-19 is a serious threat to public health” and for perceived susceptibility, “I am at risk of getting infected with COVID-19″.
Perceived efficacy was measured with eight scaled items. Questions were asked to assess the respondent's self-efficacy (4 items) and response efficacy (4 items) to practice COVID-19 preventive measures such as handwashing, maintaining physical distance, and practicing respiratory hygiene. Examples of questions asked to assess response efficacy include: “Washing hands frequently with soap and water is effective in preventing COVID-19 infection”; while to assess self-efficacy, “I can wash my hands with soap and water frequently”.
Responses to the perceived threat and efficacy questions were measured on a five-point Likert scale (strongly agree, agree, neutral, disagree, strongly disagree). None of the items were reverse coded.
Extended parallel process model variable constructs
The EPPM constructs were derived from the threat and efficacy component of the model. The threat construct was developed as a sum of participants’ responses to perceived susceptibility and severity questions. The efficacy construct was developed by summing responses to self-efficacy and response efficacy questions. Based on the two EPPM key components, four categories were derived: low threat/low efficacy (LT/LE), low threat/high efficacy (LT/HE), high threat/low efficacy (HT/LE), and high threat/high efficacy (HT/HE).
The benchmark was set at the 75th percentile, values at the 75th percentile and above were high for perceived threat and efficacy. Audiences in HT/HE were considered to be in the danger control domain, while those in LT/LE were categorized in fear control. The EPPM assumes that audiences in danger control are likely to adhere to recommended preventive behaviors, while audiences in fear control will reject recommended behaviors.
Statistical analysis
Descriptive, bivariate, and multivariate analyses were performed using STATA version 14.2. Frequencies and percentages were used to describe the study population as well as the level of exposure to messages on COVID-19 across various media. A Chi-square test was used to assess the association between selected demographic variables within danger and fear control domains. A logistic regression model was constructed to estimate the effect of demographic variables and exposure to COVID-19 messages on threat and efficacy.
Results
In total, 5132 respondents participated in the study, with a mean age of 33 years (the mean age according to the NDHS 2018 is 29 years). Eighty-three percent of respondents (83%) had tertiary education (NDHS 2018 reported 10%); 53% were single (NDHS 2018 reported 31%), and 37% were fully employed (NDHS 2018 reported 65%). Overall, respondents had very high exposure to COVID-19 messages across various platforms with social media having the highest (85%), followed by television (67%), radio (54%), and NCDC SMS (52%).
Descriptive analysis of the level of exposure to COVID-19 messages on radio, television, social media, and text messages from NCDC across different demographics is shown in Table 1 .
Table 1.
Media consumption habits across demographic variables.
| Demographic variables | Radio N(%) |
Television N(%) |
Social media N(%) |
NCDC text message N(%) |
||||
|---|---|---|---|---|---|---|---|---|
| Low | High | Low | High | Low | High | Low | High | |
| Age | ||||||||
| 18–28 | 1017 (51.16) | 917 (48.84) | 772 (38.83) | 1216 (61.17) | 271 (13.63) | 1717 (86.37) | 937 (47.13) | 1051 (52.87) |
| 29–39 | 917 (47.89) | 998 (52.11) | 592 (30.91) | 1323 (69.09) | 236 (12.32) | 1697 (87.68) | 955 (49.87) | 960 (50.13) |
| 40–50 | 322 (36.10) | 570 (63.9) | 229 (25.67) | 663 (74.33) | 167 (18.72) | 725 (81.28) | 406 (45.52) | 486 (54.48) |
| 51+ | 113 (33.93) | 220 (66.07) | 90 (27.03) | 243 (72.97) | 89 (26.73) | 244 (73.27) | 153 (45.95) | 180 (54.05) |
| Gender | ||||||||
| Male | 1150 (43.84) | 1473 (56.16 | 881 (33.59) | 1742 (66.41) | 371 (14.14) | 2252 (85.86) | 1269 (48.38) | 1354 (51.62) |
| Female | 1219 (48.59) | 1290 (51.41) | 802 (31.96) | 1707 (68.04) | 392 (15.62) | 2117 (84.38) | 1182 (47.11) | 1327 (52.89) |
| Marital status | ||||||||
| Single | 1379 (50.55) | 1349 (49.95) | 1031 (37.79) | 1697 (62.21) | 356 (13.05) | 2372 (86.95) | 1321 (48.42) | 1407 (51.58) |
| Married | 990 (41.18) | 1414 (58.82) | 652 (27.12) | 1752 (72.88) | 407 (16.93) | 1997 (83.07) | 1130 (47) | 1274 (53) |
| Highest educational level | ||||||||
| None | 22 (24.72) | 67 (75.28) | 73 (82.02) | 16 (17.98) | 76 (85.39) | 13 (14.61) | 67 (75.28) | 22 (24.72) |
| Primary | 13 (29.55) | 31 (70.45) | 31 (70.45) | 13 (29.55) | 40 (90.91) | 4 (9.09) | 33 (75) | 11 (25) |
| Secondary | 314 (44.04) | 399 (55.96) | 290 (40.67) | 423 (59.33) | 203 (28.47) | 510 (71.53) | 332 (46.56) | 381 (53.44) |
| Tertiary | 2020 (47.13) | 2266 (52.87) | 1289 (30.07) | 2997 (69.93) | 444 (10.36) | 3842 (89.64) | 2019 (47.11) | 2267 (52.89) |
| Employment status | ||||||||
| Artisans/daily paid workers | 127 (42.27) | 172 (57.53) | 136 45.48 | 163 (54.52) | 112 (37.46) | 187 (62.54) | 174 (58.19) | 125 (41.81) |
| Business/shop owners | 402 (43.55) | 521 (56.45) | 287 (31.09) | 636 (68.91) | 183 (19.83) | 740 (80.17) | 445 (48.21) | 478 (51.79) |
| Fully employed | 924 (48.05) | 999 (51.95) | 562 (29.23) | 1361 (70.77) | 195 (10.14) | 1728 (89.86) | 926 (48.15) | 997 (51.85) |
| Student/Corpers | 464 (48.43) | 494 (51.97) | 324 (33.82) | 634 (66.18) | 95 (9.92) | 863 (90.08) | 435 (45.41) | 523 (54.59) |
| Unemployed | 452 (43.93) | 577 (56.07) | 374 (36.35) | 655 (63.65) | 178 (17.30) | 851 (82.70) | 471 (45.77) | 558 (54.23) |
| Geopolitical zones | ||||||||
| North-Central | 619 (50.37) | 610 (49.63) | 314 (25.55) | 915 (74.45) | 178 (14.48) | 1051 (85.52) | 601 (48.9) | 628 (51.1) |
| North-East | 376 (54.1) | 319 (45.9) | 274 (39.42) | 421 (60.58) | 138 (19.86) | 557 (80.14) | 344 (49.5) | 351 (50.5) |
| North-West | 215 (34.24) | 413 (65.76) | 215 (34.24) | 413 (65.76) | 125 (19.9) | 503 (80.1) | 280 (44.6) | 348 (55.4) |
| South-East | 189 (33.63) | 373 (66.37) | 186 (33.10) | 376 (66.9) | 82 (14.59) | 480 (85.41) | 270(48.04) | 292 (51.96) |
| South-South | 316 (43.11) | 417 (56.89) | 241 (32.88) | 492 (67.12) | 98 (13.37) | 635 (86.63) | 340 (46.38) | 393 (53.62) |
| South-West | 654 (50.89) | 631 (49.11) | 453 (35.25) | 832 (64.75) | 42 (11.05) | 1143 (88.95) | 616 (47.94) | 669 (52.06) |
Table 2 below presents the result of the chi-square test between demographic variables and the danger/fear control process. There was significant association between danger/fear control and demographic variables except marital status.
Table 2.
Percentage of the audience in danger or fear control by demographic variables.
| Demographic variables | Danger control (%) | Fear control (%) | Pearson chi² test |
|---|---|---|---|
| Age | |||
| 18–28 | 17.83 | 82.17 | 0.001 |
| 29–39 | 21.87 | 78.13 | |
| 40–50 | 25.00 | 75.00 | |
| 51+ | 22.47 | 77.53 | |
| Gender | |||
| Male | 21.99 | 78.01 | 0.000 |
| Female | 19.61 | 80.39 | |
| Marital status | |||
| Single | 18.43 | 81.57 | 0.071 |
| Married | 23.71 | 76.29 | |
| Highest educational level | |||
| None | 3.70 | 96.30 | 0.000 |
| Primary | 4.65 | 95.35 | |
| Secondary | 19.89 | 80.11 | |
| Tertiary | 21.67 | 78.33 | |
| Employment types | |||
| Artisans/daily paid workers | 14.17 | 85.83 | 0.004 |
| Business/shop owners | 17.69 | 82.31 | |
| Fully employed | 23.12 | 76.88 | |
| Student/Corpers | 21.62 | 78.38 | |
| Unemployed | 21.02 | 78.98 |
Regression analysis of the EPPM categories and demographic variables with the beta coefficients and significant levels is shown in Table 3 . The results revealed that as age increases, the perceived susceptibility to COVID-19 increased. Also, as the level of education increased, respondents’ perceived severity, susceptibility, response efficacy, and self-efficacy on COVID-19 increased. High exposure to COVID-19 messages across all media platforms was significantly associated with perceived severity, response efficacy, and self-efficacy, however, NCDC SMS had no significant association with respondent's perceived susceptibility to COVID-19.
Table 3.
Regression with demographic variables and EPPM components.
| Demographic variables | Total N (%) | EPPM framework components |
|||
|---|---|---|---|---|---|
| Perceived susceptibility | Perceived severity | Response Efficacy | Self-efficacy | ||
| Age | |||||
| 18–28 | 1988 (39%) | 0.000 | 0.000 | 0.000 | 0.000 |
| 29–39 | 1915 (37%) | 0.022 | −0.021 | 0.048** | 0.052** |
| 40–50 | 892 (17%) | 0.040* | −0.025 | 0.033 | 0.058** |
| 51+ | 333 (6%) | 0.067*** | −0.008 | 0.033* | 0.032* |
| Gender | |||||
| Female | 2509 (49%) | 0.000 | 0.000 | 0.000 | 0.000 |
| Male | 2623 (51%) | 0.014 | 0.029* | −0.018 | −0.024 |
| Marital status | |||||
| Single | 2728 (53%) | 0.000 | 0.000 | 0.000 | 0.000 |
| Married | 2404 (47%) | 0.016 | 0.064*** | 0.018 | 0.027 |
| Highest educational level | |||||
| None | 89 (2%) | 0.000 | 0.000 | 0.000 | 0.000 |
| Primary | 44 (1%) | 0.042* | 0.021 | 0.020 | 0.009 |
| Secondary | 713 (14%) | 0.277*** | 0.168*** | 0.240*** | 0.242*** |
| Tertiary | 4286 (83%) | 0.359*** | 0.111** | 0.315*** | 0.359*** |
| Employment status | |||||
| Artisans/daily paid workers | 299 (6%) | 0.000 | 0.000 | 0.000 | 0.000 |
| Business/shop owners | 923 (18%) | 0.014 | −0.032 | 0.038 | 0.105*** |
| Fully employed | 1923 (37%) | 0.078* | −0.022 | 0.118*** | 0.161*** |
| Student/Corpers | 958 (19%) | 0.039 | 0.023 | 0.063* | 0.118*** |
| Unemployed | 1029 (20%) | 0.052* | 0.006 | 0.074** | 0.125*** |
| Geopolitical zone | |||||
| North Central | 1, 229 (24%) | 0.000 | 0.000 | 0.000 | 0.000 |
| North-East | 695 (14%) | −0.040* | 0.044** | −0.032* | −0.063*** |
| North-West | 628 (12%) | −0.042** | 0.068*** | −0.005 | 0.017 |
| South-East | 562 (11%) | −0.000 | 0.014 | −0.008 | 0.020 |
| South-South | 733 (14%) | −0.007 | −0.054*** | −0.023 | −0.013 |
| South-West | 1, 285 (25%) | 0.005 | −0.076*** | 0.009 | 0.033* |
| Exposure to COVID-19 messages across media platforms | |||||
| Radio | |||||
| Low | 2369 (46%) | 0.000 | 0.000 | 0.000 | 0.000 |
| High | 2763 (54%) | 0.044** | 0.110*** | 0.040** | 0.049*** |
| TV | |||||
| Low | 1683 (33%) | 0.000 | 0.000 | 0.000 | 0.000 |
| High | 3449 (67%) | 0.083*** | 0.076*** | 0.095*** | 0.084*** |
| Social media | |||||
| Low | 763 (15%) | 0.000 | 0.000 | 0.000 | 0.000 |
| High | 4369 (85%) | 0.061*** | 0.047** | 0.091*** | 0.099*** |
| NCDC messages | |||||
| Low | 2451 (48%) | 0.000 | 0.000 | 0.000 | 0.000 |
| High | 2681 (52%) | 0.016 | 0.052*** | 0.055*** | 0.061*** |
P > 0.01*** P> 0.05** P>0.1*.
Table 4 below shows the disaggregation of audiences into fear control and danger control categories, a total of 15% of respondents were engaging in danger control (HTHE) processes, and 59% were engaging in fear control (LTLE) processes. Respondents in the danger control category are more likely to take protective action to avoid or reduce the threat of COVID-19, while those in the fear control category do not feel at risk and are unlikely to take preventive steps.
Table 4.
Audience categorization on the Extended Parallel Process Model framework.
| High efficacy: Belief in the effectiveness of COVID-19 preventive solutions and confidence to practice them | Low Efficacy: Doubts about the effectiveness of COVID-19 solutions and lack of confidence to practice them | |
|---|---|---|
| High Threat: The belief that the threat is harmful and that one is at risk of getting infected with COVID-19 | 15% (self-protective behaviors) | 13% (denial or rejection of protective behaviors) |
| Low Threat: The belief that the threat is trivial and that one is not at-risk | 13% (know what to do but are not really motivated to do much) | 59% (People do not feel at risk and do not know what to do about it) |
Discussion
Findings from this study revealed that exposure to COVID-19 messages differed across various media platforms, with more respondents getting information from social media and television, other studies have also shown these two media channels to be the highest source of knowledge on COVID-19 in Nigeria [17,21]. Also, the main source of information was social media and television, and this was consistent across all age groups. However, social media was regarded as the least reliable source of information when compared with TV, radio, and NCDC SMS.
Threat components: perceived susceptibility and perceived severity differed across groups. Notably, the perceived susceptibility of COVID-19 was higher among older people, showing that older people feel they are more likely to be affected by COVID-19. These findings are however in contrast with a study conducted among health care workers in Pakistan, which showed that age had no significant effect on attitude towards COVID-19 [23].
From this study, more than half of respondents were in the fear control domain (59%), indicating that the majority did not perceive COVID-19 as a threat and therefore were less likely to practice the recommended protective behaviors such as hand washing, maintaining physical distance and wearing a face mask. Audiences in the danger control domain (15%) were however more likely to adopt the COVID-19 protective behaviors.
There were differences in perceived threat and efficacy responses across demographic profiles. First, regarding age, more of the younger people (18–28years) were within the fear control domain when compared to those aged 50 years and above. This may be attributed to the fact that prior messages on COVID-19 were focused on older people as ‘at risk’ group to COVID-19, which perhaps makes them more likely to adopt the protective behaviors as a lifesaving instinct, inadvertently making younger people feel less at risk of being infected with the virus.
Also, 96.3% of respondents with no education were in the fear control domain and, as level of education increased, respondents’ perceived severity, susceptibility, response efficacy and self-efficacy on COVID 19 also increased. Regarding the employment category, 85.8% of artisans/daily paid workers were mostly in the fear control category. These findings are similar to a study carried out by [23] where members of different occupation groups were also found to respond differently to the COVID-19 pandemic, however, this study was among health care workers.
The economic effects of the COVID-19 lockdown in Nigeria [11,18], especially on those in the non-formal sector may have shaped their perception of COVID-19. Practices such as maintaining physical distance, regular handwashing, and wearing a face mask seemed less practicable among this target audience. Artisans and daily-paid workers may not have access to constant water supply and find it difficult to maintain physical distancing due to the nature of their jobs. However, fully employed persons have access to systems and structures that support adherence to protective measures.
Limitation
The study was carried out during strict lockdown measures in some states, hence most respondents were reached online. However, in a few states, face to face interviews was possible as lockdown measures were relaxed. This might have a potential for selection bias against an audience that lacks access to social media or the internet.
This study utilized an observational study approach, and as such associations were only examined, as one cannot draw causal inferences.
Conclusion
This study focused on understanding the potential response to COVID-19 protective behaviors as influenced by elements of threat and efficacy. Based on the findings, we can conclude the following:
First, social media serves as a common source of information though considered unreliable by the study participants when compared with other sources, and this might be attributed to the unverifiable nature of information shared across social media. Second, levels of threat and efficacy varied across different demographic groups, and only 15% of the respondents interviewed were in the high threat -high efficacy domain. This means that very few respondents were likely to take up protective behaviors.
To develop and disseminate a more effective risk communication campaign, consideration should be given to placing an appropriate balance between threat and efficacy elements. Also, messages should address the diverse demographic population while ensuring the balance between threat and efficacy.
Future research assessing the impact of the risk communication campaign on behavioral outcomes based on the key protective behaviors of handwashing, the practice of respiratory hygiene, and maintaining physical distancing, should be considered using the EPPM theoretical framework.
Declaration of Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported, in part, by the Bill & Melinda Gates Foundation [017044]. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript that might arise from this submission.
Editor: Dr. B Gyampoh
References
- 1.Ahmed M.A., Jouhar R., Ahmed N., Adnan S., Aftab M., Zafar M.S., Khurshid Z. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) Outbreak. Int. J. Environ Res. Public Health. 2020;17(8):2821. doi: 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnett D.J., Errett N.A., Rutkow L. A threat- and efficacy-based framework to understand confidence in vaccines among the public health workforce. Vaccines (Basel) 2013;1(2):77–87. doi: 10.3390/vaccines1020077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett D.J., Thompson C.B., Semon N.L., Errett N.A., Harrison K.L., Anderson M.K., Ferrell J.L., Freiheit J.M., Hudson R., McKee M., Mejia-Echeverry A., Spitzer J., Balicer R.D., Links J.M., Storey J.D. EPPM and Willingness to respond: the role of risk and efficacy communication in strengthening public health emergency response systems. Health Commun. 2014;29(6):598–609. doi: 10.1080/10410236.2013.785474. [DOI] [PubMed] [Google Scholar]
- 4.Bhuiyan A.K.M.I., Sakib N., Pakpour A.H., Griffiths M.D., Mamun M.A. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int. J. Ment. Health Addict. 2020 doi: 10.1007/s11469-020-00307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carey R.N., Sarma K.M. Threat appeals in health communication: messages that elicit fear and enhance perceived efficacy positively impact on young male drivers. BMC Public Health. 2016;16(1):645. doi: 10.1186/s12889-016-3227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC Coronavirus Disease 2019 (COVID-19) Centers for Disease Control and Prevention. 2020 https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html [Google Scholar]
- 8.Choi H.J., Krieger J.L., Hecht M.L. Reconceptualizing efficacy in substance use prevention research: refusal response efficacy and drug resistance self-efficacy in adolescent substance use. Health Commun. 2013;28(1):40–52. doi: 10.1080/10410236.2012.720245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gharlipour Z., Hazavehei S.M.M., Moeini B., Nazari M., Beigi A.M., Tavassoli E., Heydarabadi A.B., Reisi M., Barkati H. The effect of preventive educational program in cigarette smoking: extended Parallel Process Model. J. Educ. Health Promot. 2015;4:7. doi: 10.4103/2277-9531.151875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jahangiry, L., Bakhtari, F., Sohrabi, Z., Reihani, P., Samei, S., Ponnet, K., & Montazeri, A. (2020). Risk perception related to COVID-19 among the Iranian general population: an application of the extended parallel process model [Preprint]. In Review. 10.21203/rs.3.rs-33493/v2 [DOI] [PMC free article] [PubMed]
- 11.Kanu I.A. COVID-19 and the economy: an african perspective. J. African Stud. Sustainable Development. 2020;3(2) https://acjol.org/index.php/jassd/article/view/jassd_v3n2_3 Article 2. [Google Scholar]
- 12.Khurshid Z., Asiri F.Y.I., Al Wadaani H. Human saliva: non-invasive fluid for detecting novel coronavirus (2019-nCoV) Int. J. Environ. Res. Public Health. 2020;17(7) doi: 10.3390/ijerph17072225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li X. Media exposure, perceived efficacy, and protective behaviors in a public health emergency. Int. J. Commun. 2018;12(0):20. [Google Scholar]
- 14.Liu J., Liao X., Qian S., Yuan J., Wang F., Liu Y., Wang Z., Wang F.-.S., Liu L., Zhang Z. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerging Infect. Dis. 2020;26(6):1320–1323. doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muthusamy N., Levine T.R., Weber R. Scaring the already scared: some problems with HIV/AIDS fear appeals in Namibia. J. Commun. 2009;59(2):317–344. doi: 10.1111/j.1460-2466.2009.01418.x. [DOI] [Google Scholar]
- 16.NCDC Coronavirus COVID-19 Microsite. (n.d.). Retrieved 27 August 2020, from https://covid19.ncdc.gov.ng/
- 17.Olapegba P.O., Iorfa S.K., Kolawole S.O., Oguntayo R., Gandi J.C., Ottu I.F.A., Ayandele O. Survey data of COVID-19-related knowledge, risk perceptions, and precautionary behavior among Nigerians. Data Brief. 2020;30 doi: 10.1016/j.dib.2020.105685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozili P.K. COVID-19 pandemic and economic crisis: the nigerian experience and structural causes (SSRN Scholarly Paper ID 3567419) Social Sci. Res. Network. 2020 doi: 10.2139/ssrn.3567419. [DOI] [Google Scholar]
- 19.Pakpour A.H., Griffiths M.D., Lin C.-.Y. Assessing psychological response to the COVID-19: the fear of COVID-19 scale and the COVID stress scales. Int. J. Ment. Health Addict. 2020 doi: 10.1007/s11469-020-00334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Popova L. The extended parallel process model: illuminating the gaps in research. Health Educ. Behav. 2012;39(4):455–473. doi: 10.1177/1090198111418108. [DOI] [PubMed] [Google Scholar]
- 21.Reuben R.C., Danladi M.M.A., Saleh D.A., Ejembi P.E. Knowledge, attitudes, and practices towards COVID-19: an epidemiological survey in north-central Nigeria. J. Community Health. 2020 doi: 10.1007/s10900-020-00881-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rintamaki L.S., Yang Z.J. Advancing the extended parallel process model through the inclusion of response cost measures. J. Health Commun. 2014;19(7):759–774. doi: 10.1080/10810730.2013.864722. [DOI] [PubMed] [Google Scholar]
- 23.Saqlain M., Munir M.M., Rehman S.U., Gulzar A., Naz S., Ahmed Z., Tahir A.H., Mashhood M. Knowledge, attitude, practice, and perceived barriers among healthcare workers regarding COVID-19: a cross-sectional survey from Pakistan. J. Hosp. Infect. 2020;105(3):419–423. doi: 10.1016/j.jhin.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scherr C.L., Jensen J.D., Christy K. Dispositional pandemic worry and the health belief model: promoting vaccination during pandemic events. J Public Health (Bangkok) 2017;39(4):e242–e250. doi: 10.1093/pubmed/fdw101. [DOI] [PubMed] [Google Scholar]
- 25.Shirahmadi S., Seyedzadeh-Sabounchi S., Khazaei S., Bashirian S., Miresmæili A.F., Bayat Z., Houshmand B., Semyari H., Barati M., Jenabi E., Heidarian F., Zareian S., Kheirandish M., Dadae N. Fear control and danger control amid COVID-19 dental crisis: application of the extended parallel process model. PLoS ONE. 2020;15(8) doi: 10.1371/journal.pone.0237490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Von Gottberg C., Krumm S., Porzsolt F., Kilian R. The analysis of factors affecting municipal employees’ willingness to report to work during an influenza pandemic by means of the extended parallel process model (EPPM) BMC Public Health. 2016;16(1):26. doi: 10.1186/s12889-015-2663-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO Coronavirus Disease (COVID-19) Dashboard. (n.d.). Retrieved 27 August 2020, from https://covid19.who.int
- 29.Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun. Monogr. 1992;59(4):329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]
- 30.Zarocostas J. How to fight an infodemic. Lancet North Am. Ed. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zonouzy V.T., Niknami S., Ghofranipour F., Montazeri A. An educational intervention based on the extended parallel process model to improve attitude, behavioral intention, and early breast cancer diagnosis: a randomized trial. Int. J. Women's Health. 2018 doi: 10.2147/IJWH.S182146. Dove Press. [DOI] [PMC free article] [PubMed] [Google Scholar]