Abstract
Simple Summary
Radiotherapy is as an important part of esophageal cancer (EC) treatment. However, it often causes severe radiation-induced lymphopenia (RIL). The aim of the current study was to evaluate the influence of severe RIL on the outcomes of EC. A systematic review and meta-analysis including 17 studies was performed. Our meta-analysis found that severe RIL was associated with a lower pathologic complete response rate and inferior overall survival and progression-free survival of EC patients. The lymphocyte nadir was found during 4–6 weeks after the start of radiotherapy. A series of dosimetric factors and clinical factors associated with RIL were summarized. Our results provide important evidence for the clinical application of radiotherapy. Minimizing the dosimetric risk factors, especially in patients with clinical risk factors, might benefit their outcomes. Our results might also offer clues for the strategy of combining radiotherapy and immunotherapy in EC patients.
Abstract
The aim of the current study was to evaluate the influence of severe radiation-induced lymphopenia (RIL) on the outcomes of esophageal cancer (EC). A systematic review and meta-analysis was performed through the PRISMA guideline. Seventeen studies were included in the current systematic review, with eight included in the meta-analyses. Meta-analyses found that severe RIL was associated with lower pathologic complete response (pCR) rate (odds ratio (OR) = 0.44, 95% confidence interval (CI) = 0.30–0.66, I2 = 0%), inferior overall survival (OS) (hazard ratio (HR) = 1.50, 95% CI = 1.29–1.75, I2 = 6%), and worse progression-free survival (PFS) (HR = 1.70, 95% CI = 1.39–2.07, I2 = 0%) of EC patients. The lymphocyte nadir was found during 4–6 weeks after the start of radiotherapy. The leading dosimetric factors associated with severe RIL included larger PTV, higher dose to heart and body, and higher effective dose to the immune cells (EDIC). Clinical risk factors for RIL mainly comprised lower baseline ALC, higher tumor length and clinical stage, and distal EC. In conclusion, severe RIL might be associated with a lower pCR rate and worse OS and PFS of EC patients. Minimizing the dosimetric risk factors, especially in patients with clinical risk factors, might benefit their outcomes.
Keywords: esophageal cancer, radiation therapy, lymphopenia, pathologic complete response, survival outcomes, effective dose to the immune cells
1. Introduction
Esophageal cancer (EC) is one of the most aggressive malignancies, with morbidity and mortality ranked seventh and sixth worldwide, respectively [1]. Approximately half of EC patients have cancer that extends beyond the locoregional confines of the primary site [2]. The 5-year overall survival (OS) of all EC patients is only about 20% in the United States [3]. Radiotherapy plays an important role in the management of EC, which serves as neoadjuvant chemoradiotherapy (CRT), followed by surgery or definitive CRT [4]. However, it often causes treatment-associated toxicities, including effects on host immunity such as lymphopenia [5].
Radiotherapy may play a primary role in the incidence of treatment-related lymphopenia in cancer patients [5], since lymphocytes are so radiosensitive that even a fraction of 2 Gy can kill half of the irradiated lymphocytes [6]. Radiation-induced lymphopenia (RIL) affects all lymphocyte subsets (CD3+, CD4+, CD8+ T cells, B cells, and natural killer cells) [7]. A study revealed that total lymphocyte counts did not change after neoadjuvant chemotherapy in non-small-cell lung cancer, while steep declines were found after the initiation of thoracic radiotherapy [8]. There are also studies wherein both radiotherapy and concurrent CRT significantly decreased the mean absolute number of lymphocytes compared to pretreatment levels, but no differences were detected in the characteristics of the lymphopenia induced by the two treatments in cervical cancer [9,10]. A study evaluated the radiation-induced hematological toxicity in patients with solid malignant tumors, which showed that at the end of radiotherapy, the patients with EC had the second lowest lymphocyte counts among common solid tumors, only better than head and neck cancer [11].
Previous studies found that RIL was associated with poor prognosis in several types of cancers [12]. Through multivariate analysis, meta-analyses showed that RIL was linked to worse overall survival (OS) in cancers such as lung cancer, brain cancer, pancreatic cancer, and head and neck cancer [13,14]. There are plenty of studies that showed that RIL was associated with worse OS [15,16,17,18], worse progression-free survival (PFS) [16,17,19], worse DMFS [20,21], worse local relapse-free survival (LRFS) [17], and worse disease-specific survival (DSS) [20] of EC patients. Previous studies also observed that severe RIL was related to a lower pathologic complete response (pCR) rate [19,22].
There was a previous meta-analysis that found that RIL was associated with inferior OS of severe solid tumors [13]. This meta-analysis included three EC studies [16,20,23] and found that the individual adjusted hazard ratio (HR) estimated in these studies was consistently larger than 1, and pooled HR demonstrated a trend toward statistical significance (HR = 1.46, 95% confidence interval (CI) = 0.95–2.23). It should be noted that this study only analyzed the association between RIL and OS of EC patients, and we found that there were some related studies that were not included in this meta-analysis [15,17]. Therefore, we performed this more comprehensive systematic review and meta-analysis. Our systematic review seeks to determine whether RIL is associated with poorer outcomes in EC patients and to summarize the risk factors for severe RIL in EC patients. The results of our study might provide valuable information for radiotherapy strategy in EC patients.
2. Materials and Methods
2.1. Literature Search
The current systematic review was performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 guidelines [24]. The literature was searched on the following databases: PubMed, Embase, and Cochrane Library. The search was updated to 4 May 2022. Data S1 lists the searching strategy of the current study. Our systematic review was registered at Open science (https://osf.io/prereg/ (accessed on 10 May 2022)) with a registration number of 10.17605/OSF.IO/HK7QU.
2.2. Inclusion and Exclusion Criteria
The inclusion and exclusion criteria were designed based on the population, intervention, comparison, outcome, and study design (PICOS) model (Data S1). In detail, the target population was the EC patients who had radiotherapy as a part of their therapy strategy; the intervention was the EC patients with severe RIL; the comparison was the EC patients without severe RIL; the outcome was defined as the outcome data on the association between severe RIL and non-severe RIL, such as pCR and survival-related outcome data; and the study design type should be an observational study (either retrospective or prospective).
Included studies met the following criteria: (1) a cohort study which includes EC patients who had radiotherapy during their treatment; (2) recorded RIL information during or after radiotherapy; (3) contains RIL-related outcome data, such as pCR rate or survival outcome data.
The exclusion criteria of the current study were as follows: (1) a study with a cohort that has less than 10 patients, (2) written in a non-English language, (3) published before the year 2007.
2.3. Review Process and Data Extraction
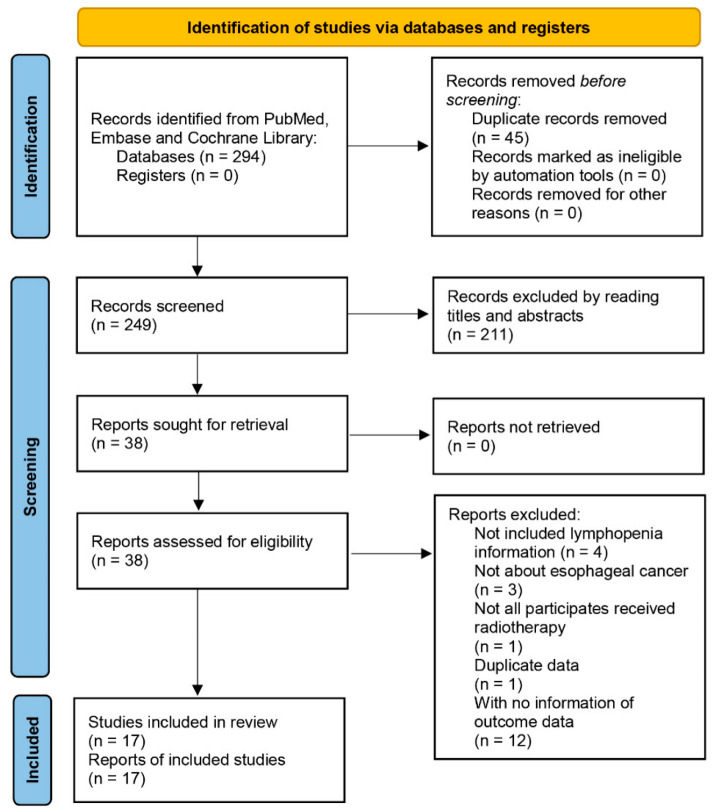
The review process was performed according to the PRISMA 2020 flow diagram for new systematic reviews, only including searches of databases and registers [24] (Figure 1). The identified records from different databases were first screened by removing the duplicates. Potential related studies were collected after reading the titles and abstracts, and further assessed by the inclusion and exclusion criteria described above.
Figure 1.
Flowchart of selection process in this systematic review. This is the PRISMA 2020 flow diagram for new systematic reviews, which only includes searches of databases and registers.
The following information from each included study was extracted: first author/publication year, region where the cohort was from, number of patients, tumor stage, age, histology, tumor location, median follow-up time, radiotherapy technique, dose plan, chemotherapy and surgery information, definition of severe RIL and data collection time, and severe RIL rate. The quality of these final selected studies was evaluated using the Newcastle-Ottawa Quality Assessment Form for Cohort Studies (NOS) [25]. In addition, we extracted the risk factors for potentially developing severe RIL in EC patients from the studies that used multivariate analysis as the calculating method. Furthermore, we extracted the data of absolute lymphocyte count (ALC) from studies which recorded them before and after the start of radiotherapy. The review process, data extraction, and quality assessment were performed by two independent investigators. Disagreements were further discussed and resolved by three reviewers.
2.4. Statistical Analyses
The R 4.0.5 software (http://www.R-project.org (accessed on 4 May 2022); ‘meta’ package) was used for meta-analyses. For the pCR rate, the pooled odds ratio (OR) and 95% CI were calculated. For survival outcomes, the pooled HR and 95% CI were calculated. The pooled analyses were performed through the generic inverse variance method by using the “metagen” function. Only studies with OR or HR calculated between two specified groups (a severe RIL group and a comparably non-severe RIL group) could be included in the meta-analysis. Otherwise, we only listed results as a part of the systematic review. For the studies including duplicate cohorts, the most recent, largest, or best-quality studies were selected for our meta-analysis. The meta-analysis was conducted only if there were equal or over three individual results from multivariate analysis. The statistical heterogeneity was evaluated by the I2 test. The random effect model was used in our meta-analysis since random- and fixed-effects models present similar results when heterogeneity is low [26]. If high heterogeneity occurred, a sensitivity analysis was performed to explore the potential source of heterogeneity by using the “metainf” function. The publication bias was assessed through Egger’s test by using the “metabias” function. Forest plots were used to visually display the results of individual studies and the synthetic results of the current meta-analysis. The curve plots representing the ALC tendency of EC patients who received CRT were plotted by using the “ggplot2” package. A two-sided p value of less than 0.05 was considered statistically significant.
3. Results
3.1. Results of the Review Process
As shown in Figure 1, there were 291 records identified after searching the databases. Among them, we removed 44 duplicated studies, and a further 209 studies by judging the titles and abstracts. The selected 38 studies were further assessed, and we excluded 4 studies with no RIL information, 3 studies which were not about EC, 1 study with participants who had not received radiotherapy, 1 study with duplicate data, and 12 studies with no information on outcome data. Finally, we included 17 retrospective studies [15,16,17,18,19,20,21,22,23,27,28,29,30,31,32,33,34] in our systematic review. The quality assessment results are listed in Table S1. Relatively high quality was identified for all studies. There were 10 studies [15,16,17,18,19,20,21,22,23,34] which calculated the OR or HR on outcomes of EC patients between severe RIL and non-severe RIL groups, of which 3 studies [18,20,21] had the potential to have partial duplicate EC patients in their cohorts; therefore, we included the largest cohort [20] among them in our meta-analysis and kept the other 2 studies [18,21] in our systematic review.
As shown in Table 1, 17 studies were finally included in our systematic review, of which 8 studies [15,16,17,19,20,22,23,34] were included in the meta-analysis and 9 studies [18,21,27,28,29,30,31,32,33] were only included in the systematic review. The studies were published between the years 2017 and 2021. Most studies were from the United States (n = 7) and Eastern Asia (n = 9). The United States had more esophageal adenocarcinoma (EAC) and lower EC, while Eastern Asia had more esophageal squamous cell carcinoma (ESCC) and upper/middle EC. The majority of studies had concurrent chemotherapy with radiotherapy dose around 50.4 Gy and 1.8–2 Gy per fraction. Most studies collected the lowest ALC during the CRT and defined the Criteria for Adverse Events (CTCAE) grade 4 lymphopenia as the severe RIL.
Table 1.
The characteristics of each included study.
| First Author/Year | Ref. | Region | No. Patients/Stage | Age (Years) | Histology | Tumor Location | Median Follow-Up (Months) | RT Technique | Dose (Gy) | Chemotherapy | Surgery Rate after CRT | Definition of Severe RIL/Data Collection Time a | Severe RIL Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| For meta-analysis | |||||||||||||
| Xu H/2021 | [16] | China | 436/I-IVA | Median (range) = 59 (27–74) | ESCC | Upper/Middle (86.7%), Lower (13.3%) | 21.7 | IMRT (73.6%), 3D-CRT (26.4%) | Median (range) = 60 (40–70), with 25–30 fractions. | Concurrent weekly chemotherapy, with 54.8% cisplatin + taxane, 17.2% cisplatin + 5-FU, 28% other | 0% | G4/During RT | 23.6% |
| Liu M/2021 | [15] | China | 99/II-IVA | Median (range) = 67 (43–83) | ESCC | Upper/Middle (75%), Lower (25%) | 24.7 | IMRT (100%) | Median (range) = 55.75 (46–66), with 1.8–2.2 per fraction | Concurrent chemoradiotherapy (59%), sequential chemoradiotherapy (9%); the others were RT alone | 0% | <300/Within 2 months after RT started | NA |
| Wang X/2020 | [17] | China | 189/I-IVA | Median (range) = 67 (44–92) | ESCC | Upper/Middle (76.2%), Lower (23.8%) | 46 | IMRT (65.1%), 3D-CRT (34.9%) | 50–68 | Concurrent chemotherapy receiving platinum and 5-FU doublet chemotherapy (16.9%), followed by combination of platinum and taxane (12.7%) | 0% | <380/During RT | 58.2% |
| Zhou X/2019 | [22] | China | 286/II-IVA | Median (range) = 67 (47–84) | ESCC | Upper/Middle (88.1%), Lower (11.9%) | NA | IMRT (76.6%), Proton (23.4%) | Median = 50.4, with 1.8 per fraction | Concurrent cisplatin + docetaxel (72.4%) or S-1 (27.6%) | NA | G4/During RT | 31.0% |
| Zhang E/2019 | [23] | United States | 189/ I-III | Median (range) = 65 (35–84) | EAC (78%), other (22%) | Upper/Middle (15%), Lower (85%) | 27.6 | NA | Median (range) = 50.4 (41.4–70.2) | Concurrent carboplatin/paclitaxel (55%) or 5-FU (40%)-based regimens | 68% | G4/During RT | 45.0% |
| Li Q/2019 | [19] | China | 220/II-III | Median (range) = 56 (42–73) | ESCC | Upper/Middle (77.3%), Lower (22.7%) | 24.8 | IMRT (33.2%), 3D-CRT (66.8%) | Median (range) =40 (40–50.4), with 20–25 fractions | Concurrent cisplatin + vinorelbine (57.3%), cisplatin + taxane (29.5%), or cisplatin + 5-FU (13.2%) | 100% | G4/During RT | 21.8% |
| Deng W/2019 | [20] | United States | 755/I-III | Median (IQR) = 64 (57–71) | ESCC (17.6%), EAC (81.8%), other (0.5%) |
Upper/Middle (14.8%), Lower (85.2%) | 65.5 | IMRT (67.7%), Proton (32.3%) | Median (range) = 50.4 (41.4–66.0) | Concurrent weekly taxane, 5-FU, or platinum-based compound | 49.9% | G4/During RT | 38.9% |
| Fang P/2018 | [34] | United States | 313/I-IVA | Mean (SD) = 59.3 (10.8) | ESCC (5%), EAC (95%) | Upper/Middle (2.3%), Lower (97.7%) | NA | IMRT (67%), Proton (33%) | Mean (SD) = 50 (1.9) | Concurrent taxane + 5-FU (43.1%), platinum + 5-FU (38.7%), platinum + taxane (10.9%), or other regimens (7.4%) | 100% | <350/During RT | 56.0% |
| Only for systematic review | |||||||||||||
| Wang Q/2021 | [28] | China | 476/I-IV | Median (range) = 63 (37–85) | ESCC | Upper/Middle (84.2%), Lower (15.8%) | Total 60 months | IMRT (65.8%), 3D-CRT (34.2%) | 50–60, with 25–33 fractions | Concurrent vs. Non-concurrent = 12.2% vs. 87.8%, Paclitaxel vs. 5-FU = 58% vs. 42% | NA | <800/During RT | 54.2% |
| Nishida M/2021 | [29] | Japan | 298 | NA | EC | NA | NA | NA | NA | CRT | NA | G3-4/During RT | NA |
| Kroese T/2021 | [31] | Netherlands | 219/I-IV | NA | EC | Upper/Middle (30.6%), Lower (69.4%) | 26.7 | IMRT | 41.4 or 50.4, with 1.8 per fraction | Concurrent chemotherapy for all, CROSS regime | 100% | G4/During RT | 16.0% |
| Cai S/2021 | [30] | China | 146/I-IVA | Median (range) = 71 (50–91) | ESCC (95.2%), EAC and others (4.8%) | Upper/Middle (83.6%), Distal (16.4%) | 17.9 | IMRT | 45–50.4 for neoadjuvant CRT and 60–64 for definitive RT, with 1.8–2 per fraction | 15.1% received neoadjuvant chemotherapy, 45.2% received consolidation chemotherapy; Carboplatin and paclitaxel were most used | 21.90% | G4/During RT and 1 week after RT | 24.7% |
| Xu C/2020 | [18] | United States | 488/I-IV | Median (range) = 61 (20–84) | ESCC (9.8%), EAC (90.2%); | Upper/Middle (7%), Lower (93%) | 29.6 | IMRT | 45–50.4 | Concurrent chemotherapy for all | 55.9% | G4/During RT | 50.0% |
| So T/2020 | [32] | Hong Kong | 92/II-IVA | <65 year (45.7%), ≥65 (54.3%) | ESCC | NA | 16.9 | IMRT (43.5%), 3D-CRT (56.5%) | 41.4, with 23 fractions | Concurrent weekly carboplatin, with area under the curve = 2 and paclitaxel = 50 mg/m2 | 100% | G3-4/During RT and after 2 months after completion of RT | NA |
| Sherry A/2019 | [33] | United States | 93/II-III | Median (IQR) = 64 (55–72) | ESCC (17%), EAC (82%) | Upper/Middle (12%), Lower (88%) | 19.2 | IMRT (35%), 3D-CRT (65%) | 50.4 (IQR, 50–50.4), with 28 fractions (IQR, 25–28) | Concurrent platinum + taxane (78%), platinum + 5-FU (14%), other (7%) | 71% | NA/During RT | NA |
| Routman D/2017 | [27] | United States | 176/NA | NA | EC | NA | 39.6 | NA | NA | NA | NA | G4/During RT and before surgery | 46.0% |
| Davuluri R/2017 | [21] | United States | 504/I-III | Median (SD) = 62.5 (11.2) | ESCC (15%), EAC (85%) | Upper/Middle (11%), Lower (89%) | 32.1 | IMRT (63%), Proton (37%) | 50.4 for all | Concurrent taxane + 5-FU (49%), platinum + taxane (13%), platinum + 5-FU (31%), other (7%) | 46% | G4/During RT | 27.0% |
Abbreviations: NA—not available; IQR—interquartile range; SD—standard deviation; ESCC—esophageal squamous cell carcinoma; EC—esophageal carcinoma; EAC—esophageal adenocarcinoma; IMRT—Intensity-Modulated Radiation Therapy; 3D-CRT—three-dimensional conformal radiation therapy; CRT—chemoradiation therapy; 5-FU—5-fluorouracil; CROSS—chemoradiotherapy for esophageal cancer followed by surgery study; RIL—radiation-induced lymphopenia; RT—radiotherapy. a G3/4—grade 3/4 lymphopenia according to the standardized Common Terminology Criteria for Adverse Events (CTCAE). The unit used for the definition of RIL is cells/μL.
3.2. The Association between RIL and pCR of EC Patients
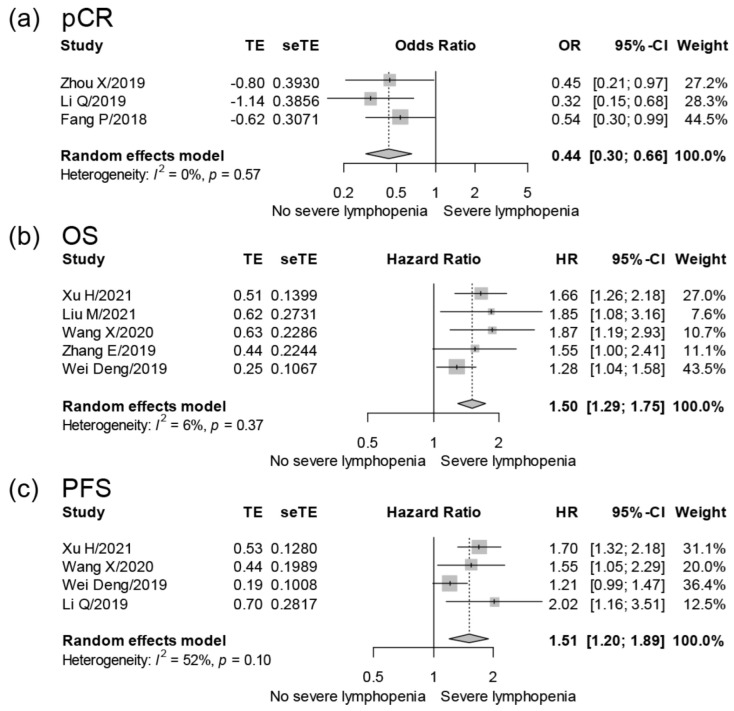
Four studies [19,22,33,34] reported the association between RIL and pCR of EC patients. Zhou X et al. [22] found that the pCR rate of grade 4 RIL vs. grade 0–3 RIL was 11.2% vs. 26.4% in EC patients, whilst Li Q et al. [19] observed that the pCR rate of grade 4 RIL vs. grade 0–3 RIL was 22.9% vs. 48.8% in EC patients. Our meta-analysis included three studies [19,22,34] and showed that the pCR rate was significantly lower in EC patients with severe RIL (OR = 0.44, 95% CI = 0.30–0.66, I2 = 0%; 3 studies with 819 samples; Table 2 and Figure 2).
Table 2.
The meta-analyses of associations between RIL and the outcomes of EC patients.
| Group | Number of Studies | Sample Size | Pooled OR or HR (95% CI) | I2 (%) | Egger’s p Value |
|---|---|---|---|---|---|
| pCR | 3 | 819 | 0.44 (0.30–0.66) a | 0 | 0.4391 |
| OS | 5 | 1668 | 1.50 (1.29–1.75) b | 6 | 0.1053 |
| PFS | 4 | 1660 | 1.51 (1.20–1.89) b | 52 | 0.2824 |
Abbreviations: pCR—pathologic complete response; OS—overall survival; PFS—progression-free survival; OR—odds, ratio; CI—confidence interval; HR—hazard ratio. a OR (95% CI); b HR (95% CI).
Figure 2.
Forest plots depicting meta-analyses for the association between severe RIL and the outcomes of EC patients; meta-analyses for the correlation of severe RIL and pCR (a), OS (b), and PFS (c) of EC patients. The big diamond at the bottom of the plot symbolizes the pooled OR or HR of all studies. The diamond’s width corresponds to 95% CI. For these included multivariate analyses, Zhou X et al. included variables of lymphopenia, tumor length, and baseline ALC. Li Q et al. included variables of lymphopenia, pretreatment platelets, chemotherapy, and interval to surgery in the meta-analysis of pCR, and included age, sex, primary tumor length, clinical stage, chemotherapy, interval to surgery, and pCR status in the meta-analysis of PFS. Fang P et al. included variables of lymphopenia, age, current smoker, clinical stage, histology, differentiation, tumor length and location, radiotherapy dose and modality, induction chemotherapy, and chemotherapy regimen. Xu H et al. included variables of lymphopenia, sex, tumor location and length, induction chemotherapy, clinical stage, radiotherapy modality, and baseline albumin and hemoglobin. Liu M et al. included variables of lymphopenia; age; sex; ECOG score; tumor location; clinical stage; chemotherapy; prescribed radiotherapy dose; pretreatment NLR; mean TVB dose; TVB V5, V10, and V20; and EDIC. Wang X et al. included variables of lymphopenia, age, sex, smoking, drinking, tumor length and location, clinical stage, treatments (concurrent chemotherapy and chemotherapy regimen), radiotherapy technology and dose, and baseline ALC. Zhang E et al. included variables of lymphopenia, clinical stage, and surgery. Deng W et al. included variables of lymphopenia, baseline ALC, sex, age, ECOG score, tumor length and location, histology, differentiation, clinical stage, and treatments (induction and concurrent chemotherapy and surgery).
In addition, Sherry A et al. reported that time-varying ALC was associated with the achievement of pCR (OR = 3.26, p = 0.0180) [33].
3.3. The Association between RIL and Survival Outcomes of EC Patients
Twelve studies [15,16,17,18,20,21,23,28,29,30,31,32] reported the association between RIL and the OS of EC patients. Our meta-analysis included five studies [15,16,17,20,23] and showed that severe RIL affected the OS of EC patients (HR = 1.50, 95% CI = 1.29–1.75, I2 = 6%; 5 studies with 1668 samples; Table 2 and Figure 2). Davuluri R et al. [21] (HR = 1.35, 95% CI = 1.02–1.78) and Xu C et al. [18] (HR = 1.284, 95% CI = 1.002–1.645) also observed that severe RIL affected the OS of EC patients. Nishida M et al. observed that grade 3–4 RIL after CRT was associated with worse OS of EC patients [29]. Cai S et al. showed that the OS significantly decreased in EC patients with grade 4 RIL (p < 0.001) [30]. Wang Q et al. found that for EC patients, the median OS of the lower ALC group (<0.8 × 109/L) vs. higher ALC group (≥0.8 × 109/L) was 35.5 vs. 49.8 months (p = 0.001) after propensity score matching [28]. Kroese T et al. observed that the median OS in EC patients with or without grade 4 RIL was 12.7 months and 42.5 months, respectively (p = 0.045) [31]. So T et al. showed that a higher lymphocyte nadir indicated lower risk for OS of EC patients (HR = 0.75 per 108 cells/L, p = 0.003) by multivariable Cox regression model [32].
Six studies [16,17,19,20,21,30] reported the association between RIL and the PFS of EC patients. Our meta-analysis included four studies [17,19,20,35] and found that severe RIL affected the PFS of EC patients (HR = 1.51, 95% CI = 1.29–1.89, I2 = 52%; 4 studies with 1660 samples; Table 2 and Figure 2). In addition, Davuluri R et al. also observed that severe RIL affected the PFS of EC patients (HR = 1.58, 95% CI = 1.19–1.21) [21]. Cai S et al. found that the PFS of patients with grade 4 RIL was inferior to that of those with grade 0–3 RIL (3-year PFS: 20.7% vs. 45.4%, p = 0.048) [30].
Three studies [20,21,27] reported the association between RIL and the DMFS of EC patients. Deng W et al. [20] (HR = 1.27, 95% CI = 1.03–1.50) and Davuluri R et al. [21] (HR = 1.60, 95% CI = 1.13–2.27) observed that severe RIL affected the DMFS of EC patients. Routman D et al. [27] identified that, as a continuous variable, a higher lymphocyte nadir was significantly related to a decreased incidence of distant recurrence in EC patients (HR = 0.836, p = 0.0209) by multivariate analysis.
Three studies [20,21,27] reported the association between RIL and the LRFS of EC patients. Wang X et al. [17] (HR = 1.60, 95% CI = 1.17–2.17) and Deng W et al. [20] (HR = 1.23, 95% CI = 1.00–1.50) found that severe RIL was associated with inferior LRFS of EC patients, while Davuluri R et al. observed there was no association between RIL and the LRFS of EC patients (HR = 2.3, 95% CI = 0.80–1.90) [21].
In addition, Deng W et al. [20] (HR = 1.39, 95% CI = 1.10–1.76) and Davuluri R et al. [21] (HR = 1.60, 95% CI = 1.17–2.17) observed that severe RIL was associated with worse DSS of EC patients.
3.4. The Heterogeneity and Bias
There was relatively high heterogeneity among our meta-analyses in the association between RIL and the PFS of EC patients (I2 = 52%, Table 2). A sensitivity analysis was then performed, and we found that one study that might have caused heterogeneity [20]. With heterogeneity removed, the updated pooled meta-analysis still showed that severe RIL had a significant impact on EC patients’ PFS (HR = 1.70, 95% CI = 1.40–2.06, I2 = 0%; 3 studies with 905 samples; Figure S1).
The Egger’s test revealed no significant publication bias in our meta-analyses on the correlation of RIL and outcomes of EC patients (p > 0.05, Table 2).
3.5. Summary of Factors Associated with Severe RIL
Table 3 summarizes numerous dosimetric indicators and other risk factors linked to the development of RIL in each study based on multivariate analysis. Among dosimetric factors, larger PTV (four studies [16,17,22,32]), higher mean body dose (two studies [21,34]), higher effective dose to the immune cells (EDIC) (two studies [15,32]), and higher heart V10 (two studies [16,17]) were strong predictors of severe RIL. Higher total radiation dose [19], higher mean thoracic vertebrae dose [15], larger thoracic vertebrae V20 [15], larger body V10 [23], larger aorta V5 [23], larger heart V15 [23], larger T-spine V5 [23], and larger lung V10 [16] were also mentioned as being associated with developing severe RIL. In addition to dosimetric factors, other clinical factors associated with severe RIL were lower baseline ALC [16,17,32], greater tumor length [19,22] or higher clinical stage [17,34], distal EC [19,22], CRT [15] or chemotherapy type [21], older age [22], nonsmoking history [34], and lower ECOG performance status [16].
Table 3.
Risk factors for developing severe RIL in EC patients, as determined via multivariate analysis.
| First Author/Year | Ref. | Dosimetric Factors ab | Others a | Non-Significant Factors b |
|---|---|---|---|---|
| Xu H/2021 | [16] | Larger PTV, higher heart V10, higher lung V10 | Lower baseline ALC, lower ECOG performance status | Sex, smoking history, alcohol history, tumor location (upper vs. middle/distal), clinical N stage (N0–1 vs. N2–3), lung V5, lung V20, MLD, MHD, VB V10, mean VB dose |
| Liu M/2021 | [15] | Higher EDIC, higher mean dose, higher V20 of TVB | Chemotherapy regimen (CRT vs. RT alone) | V5 and V10 of TVB, RT dose (<60 vs. ≥60 Gy) |
| Wang X/2020 | [17] | Larger PTV, higher heart V10 | Higher clinical stage, lower baseline ALC | Tumor length, lung V5, lung V10, lung V20, lung V30, lung V40, lung mean dose, heart V5, heart V30, heart V40, heart mean dose |
| So T/2020 | [32] | Larger PTV, higher EDIC | Lower baseline ALC | The number of courses of chemotherapy (5 courses vs. fewer than 5 courses) |
| Zhou X/2019 | [22] | Larger PTV | Distal EC, tumor length > 5 cm, older age | MLD |
| Zhang E/2019 | [23] | Heart V15 > 73%, TVB V5 > 72%, body V10 > 18%, aorta V5 > 93% | Lower baseline TLC | Total lung V5 > 50%, spleen V20 > 45% |
| Li Q/2019 | [19] | Higher radiation dose (>40 Gy) | Distal EC, tumor length > 5 cm | Age, alcohol history, dose per fraction > 2.0 Gy, IMRT vs. 3D-CRT, clinical TNM stage (II vs. III), pretreatment ALC (<1.8 vs. ≥1.8 × 109/L) |
| Fang P/2018 | [34] | Higher mean body dose | Higher clinical stage, no smoking at diagnosis | Age, tumor histology, tumor differentiation, tumor location, tumor size, RT modality, induction chemotherapy or chemotherapy type between the groups |
| Davuluri R/2017 | [21] | Higher mean body dose | Concurrent Taxane/5-FU vs. platinum/5-FU | Age, comorbidities, tumor characteristics (location, length, stage, histology, differentiation), surgery, RT modality, induction chemotherapy |
Abbreviations: PTV—planning target volume; TVB—thoracic vertebrae; ECOG—Eastern Cooperative Oncology Group; CRT—chemoradiation therapy; RT—radiotherapy; ALC—absolute lymphocyte count; TLC—total lymphocyte count; Distal EC—distal esophageal cancer; 5-FU—5-fluorouracil; IMRT—intensity-modulated radiation therapy; 3D-CRT—three-dimensional conformal radiation therapy; MLD—mean lung dose; MHD—mean heart dose; VB—vertebral body. a Factors with 2 or more significant results are in bold; b Vx—percentage of the total lung, heart, or VB volume receiving more than x Gy.
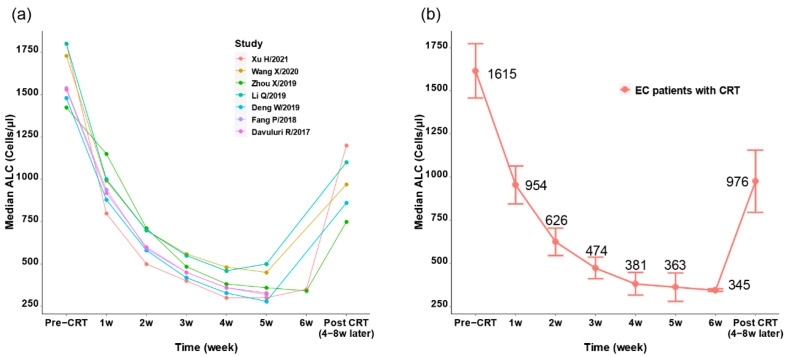
3.6. The Influence of CRT on ALC
As shown in Table S2, nine studies [16,17,19,20,21,22,29,30,34] reported both the pretreatment ALC and the ALC nadir in EC patients who had CRT. The range of pretreatment ALC was 1400–1800 cells/μL, while the range of ALC nadir during or after CRT was 280–460 cells/μL, and the drop rate of ALC ranged from 73.99% to 83.33%. Five studies [16,17,19,20,22] reported the ALC after 4–8 weeks of the CRT completion, and the recovery of ALC ranged from 715 to 1200 cells/μL.
As shown in Figure 3a,b, seven studies recorded the weekly ALC from the initiation of radiotherapy [16,17,19,20,21,22,34]. All studies showed a significant drop of ALC at the first two weeks (ranging from 50.18% to 72.22%, Figure 3a), and the lowest ALC was identified during 4–6 weeks (Figure 3a and Table S2). The pooled analysis showed that the mean median ALC dropped from 1615 cells/μL to 345 cells/μL at the 6th week (drop rate = 78.6%), and recovered to 976 cells/μL after 4–8 weeks from CRT completion.
Figure 3.
The tendency of ALC in EC patients who received CRT. (a) Serial median ALC in EC patients who received CRT from various studies. (b) Merged mean ALC in EC patients who received CRT; the circle represents the mean median ALC of studies and the error bars represent the standard deviation.
4. Discussion
The current systematic review included 17 studies and used meta-analysis to show that the RIL of EC patients was associated with lower pCR rate and worse OS and PFS. We also evaluated a series of factors that might be associated with the incidence of RIL and summarized the ALC tendency of EC patients who received radiotherapy. Compared with the previous meta-analysis [13], which only included three cohorts and found a trend toward statistical significance that RIL was associated with inferior OS of EC patients, our systematic review was much more comprehensive, improving and expanding their findings.
Recently, immunotherapy has emerged as a standard treatment for many cancers, including EC [36,37]. Several immune checkpoint inhibitors that block the connection between PD-1 and PD-L1 are now being utilized to treat EC, such as nivolumab and pembrolizumab [38]. It should be emphasized that combining radiotherapy with immunotherapy is believed to be a promising strategy for improving therapeutic efficacy in a synergistic way [36]. Previous research has demonstrated that radiotherapy can boost tumor antigen presentation [39] as well as checkpoint inhibitor-induced antitumor immune responses in EC patients [40], which might improve the immunotherapy efficacy. However, radiotherapy also causes lymphopenia, which is associated with the reduction of the immune effector lymphocytes, poor response to immunotherapy, and worse prognosis [41]. Hence, it is crucial to lower the RIL rate and maintain an intact adaptive immune system during radiotherapy. Our study found that RIL was associated with worse outcomes of EC patients, which might be associated with reduced anti-cancer immune response and increased risk of infection [42]. Yin T et al. found that RIL was associated with the efficacy of immunotherapy. They found that radiotherapy increased the occurrence of lymphopenia (OR = 0.502, p = 0.035), and the overall response rate of EC patients without RIL was 29.4% while that of patients with RIL was 23.1%. EC patients receiving immunotherapy < 33.5 days (optimal cut-off value by ROC curves) after radiotherapy showed a poorer PFS compared to those ≥ 33.5 days (median PFS: 4.1 vs. 7.3 months, p = 0.008). Plenty of clinical trials of radiotherapy combined with immunotherapy for EC are now ongoing [5]. Our systematic review summarized the detailed ALC tendency among EC patients, which might provide helpful information for future clinical trials on the association between radiotherapy and immunotherapy in EC.
A series of clinical factors were associated with the incidence of RIL in EC. For the dosimetric parameters, the PTV volume, mean body dose, and heart V10 were mostly mentioned to be associated with RIL. The degree of RIL has been considered to depend on the dose/volume of blood flow as well as organs rich in lymphatics and lymphocytes in the radiation field [12]. The concept of EDIC was first introduced by Jin et al. at the 2017 ASTRO annual meeting, who considered the immune system as an organ at risk (OAR) and intended to examine the effects of radiotherapy dose on the immune system and the outcomes of lung cancer [43]. Studies observed that higher EDIC was associated with lower ALC and survival outcomes of small-cell lung cancer [44] and non-small-cell lung cancer [45,46]. Similar EDIC models were applied to EC, as it is also within the thoracic cavity. Liu M et al. found that an EDIC higher than 7.11 Gy predicted a lower ALC and lower OS in EC [15]. Xu C et al. showed that EDIC maintained a risk factor for severe RIL, after controlling for other risk factors such as age, ECOG, and PTV. Furthermore, a higher EDIC was linked to poorer OS, PFS, and DMFS [18]. So T et al. observed that EDIC had a significantly negative correlation with ALC nadir, and that a higher EDIC predicted worse OS (<2 Gy, >2 and <4 Gy, and ≥4 Gy groups) [32]. In these studies, various formulae were designed to estimate EDIC based on the doses to the lung, heart, and liver (which are the organs with the largest pool of circulating or resident immune cells) and the remaining body [15,18,44,46]. However, there might be more organs to account for, such as the spleen. A study showed that higher splenic dose increases the risk of lymphopenia in a series of upper abdominal cancers, including EC [47,48]. Saito et al. showed that when the mean splenic dose increased by 1 Gy, the predicted ALC decreased by 2.9% in EC patients [49]. Our systematic review also showed that a higher dose to the thoracic vertebrae or aorta was associated with the incidence of RIL in EC. Further improvements to the EDIC model of EC with more specified organs are required. EDIC should be introduced in the design of the radiotherapy plan for EC, which might be an important countermeasure to lower the incidence of RIL and improve the prognosis of EC patients.
In addition to dosimetric factors, there were also other factors associated with severe RIL, such as lower baseline ALC, greater tumor length, higher clinical stage, distal EC, CRT, chemotherapy regime, older age, no smoking at diagnosis, and lower ECOG performance status. Greater tumor length and higher clinical stage were associated with larger irradiated area. Distal esophageal location spans across the heart and close to the spleen, the dose of which might have a higher rate of causing RIL. Consistently, our systematic review showed that the rate of grade 4 RIL was higher in the studies [18,20,21,23,34] with majority lower EC (38.9–50.0%) than those [16,19,22,30] with majority upper/middle EC (21.8–31%) (Table 1). The histology of EC differs greatly between the United States and Eastern Asia (Table 1); the United States had more EAC whilst Eastern Asia had more ESCC [50]. Our results show that there is a much higher rate of grade 4 RIL in the United States than in Eastern Asia (Table 1). However, this might be a result of the location difference rather than a histology difference, as the radiotherapy plan does not differ much between ESCC and EAC. The radiotherapy technique might also influence the RIL rate. Lin et al. conducted a randomized phase IIB trial and showed that the rates of grade 4 RIL were 52% and 27% in locally advanced EC patients under IMRT and PBT, respectively [51]. They found that PBT resulted in considerably reduced doses to total lung indicators (V5, 41.4% vs. 19.7%; V20, 13.6% vs. 8.4%; mean lung dose, 8.4 vs. 4.8 Gy; all p < 0.001) and also mean doses to the liver (12.1 vs. 2.4 Gy; p < 0.001) and heart (19.8 vs. 11.3 Gy; p < 0.001) [51], which might greatly lower the EDIC. Davuluri R et al. also found that the incidence of grade 4 RIL is significantly reduced in EC patients treated with proton beam therapy (PBT) when compared to intensity-modulated radiation therapy (IMRT) (15.5% vs. 33.1%, p < 0.001) [21].
There are some limitations in our systematic review. First, since the included studies were all retrospectively designed, there were many potential confounders in linking RIL and clinical outcomes in the included studies. For example, larger PTV, longer tumor length, or GEJ location were more associated with RIL. However, they might also be associated with more advanced disease, which also has worse outcomes. Despite using the multivariate results in the meta-analysis, future data from prognostic and randomized designed studies are required. Second, the details of radiotherapy conduction were often missing, such as the fields and organs at risk. Third, there was heterogeneity in the definition of severe RIL. The method of pooling data from studies with different definitions of severe RIL was from a previous study on the association between RIL and the prognosis of lung cancer [52]. However, there was relatively low heterogeneity in our meta-analysis of the OS (I2 = 6%) and PFS after sensitivity analysis (I2 = 0%). Fourth, our included studies showed the association between RIL and the outcomes of EC patients; however, whether the RIL could influence the benefits of immunotherapy was not studied among these cohorts. Moreover, the rate of RIL in our included studies was mostly recorded during radiotherapy; whether the lymphopenia could recover after treatment and whether prolonged treatment-related lymphopenia could impact the benefits of immunotherapy was meaningful, as much of the data on the use of immunotherapy for locally advanced EC is in the adjuvant setting, such as in the Checkmate 577 trial or the ongoing SKYSCRAPER 07 trial. Although we found that the mean median ALC recovered to 976 cells/μL after 4–8 weeks from CRT completion, it was still much lower than the initial ALC, which was 1615 cells/μL.
5. Conclusions
Our systematic review showed that severe RIL might be associated with a lower pCR rate, worse OS, and worse PFS of EC patients. The ALC nadir was observed during 4–6 weeks after the start of CRT, with a significant recovery during 4–8 weeks after CRT completion. The dosimetric factors associated with severe RIL included larger PTV, higher mean body dose, higher EDIC, and higher heart V10. An improved EDIC model is required to quantify the dose to lymphocytes with more accuracy, and EDIC should be introduced in the design of radiotherapy plans in EC. Minimizing the dosimetric factors, especially among patients with lower baseline ALC, greater tumor length, higher clinical stage, and distal EC, might potentially lower the rate of severe RIL and improve the outcomes of EC.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/cancers14123024/s1. Data S1: Population, intervention, control, outcome, and study design (PICOS) items and searching strategy in PubMed, Embase, and Cochrane Library of the current study. Table S1: NOS scale for cohort studies. Table S2: Median ALC tendency for EC patients who received CRT. Figure S1: Forest plots of sensitivity analysis for meta-analysis on the association between severe RIL and the PFS of EC patients; sensitivity analysis for meta-analysis of the severe RIL and PFS of EC patients. For each line at the body of the plot, the HR and 95% CI correspond to the new pooled results after omitting a single study. The large diamond at the bottom of the plot represents the pooled HR of all studies. The width of the diamond represents 95% CI.
Author Contributions
Review process and assessment of the study quality, D.D. and Q.T.; extracting the data, D.D. and Q.T.; figures, G.Y. and Y.S.; writing the manuscript, D.D. and Q.T.; study design, H.J. and Q.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was supported by the National Natural Science Foundation of China (No. 82073332).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Ajani J.A., D’Amico T.A., Bentrem D.J., Chao J., Corvera C., Das P., Denlinger C.S., Enzinger P.C., Fanta P., Farjah F., et al. Esophageal and Esophagogastric Junction Cancers, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2019;17:855–883. doi: 10.6004/jnccn.2019.0033. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer statistics, 2022. CA Cancer J. Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 4.Deng W., Lin S.H. Advances in radiotherapy for esophageal cancer. Ann. Transl. Med. 2018;6:79. doi: 10.21037/atm.2017.11.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang X., Wang P., Zhao Z., Mao Q., Yu J., Li M. A review of radiation-induced lymphopenia in patients with esophageal cancer: An immunological perspective for radiotherapy. Ther. Adv. Med. Oncol. 2020;12:1758835920926822. doi: 10.1177/1758835920926822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yovino S., Kleinberg L., Grossman S.A., Narayanan M., Ford E. The etiology of treatment-related lymphopenia in patients with malignant gliomas: Modeling radiation dose to circulating lymphocytes explains clinical observations and suggests methods of modifying the impact of radiation on immune cells. Cancer Investig. 2013;31:140–144. doi: 10.3109/07357907.2012.762780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Domouchtsidou A., Barsegian V., Mueller S.P., Best J., Ertle J., Bedreli S., Horn P.A., Bockisch A., Lindemann M. Impaired lymphocyte function in patients with hepatic malignancies after selective internal radiotherapy. Cancer Immunol. Immunother. 2018;67:843–853. doi: 10.1007/s00262-018-2141-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campian J.L., Ye X., Brock M., Grossman S.A. Treatment-related lymphopenia in patients with stage III non-small-cell lung cancer. Cancer Investig. 2013;31:183–188. doi: 10.3109/07357907.2013.767342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Meir H., Nout R.A., Welters M.J., Loof N.M., de Kam M.L., van Ham J.J., Samuels S., Kenter G.G., Cohen A.F., Melief C.J., et al. Impact of (chemo)radiotherapy on immune cell composition and function in cervical cancer patients. Oncoimmunology. 2017;6:e1267095. doi: 10.1080/2162402X.2016.1267095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santin A.D., Hermonat P.L., Ravaggi A., Bellone S., Roman J., Pecorelli S., Cannon M., Parham G.P. Effects of concurrent cisplatinum administration during radiotherapy vs. radiotherapy alone on the immune function of patients with cancer of the uterine cervix. Int. J. Radiat. Oncol. Biol. Phys. 2000;48:997–1006. doi: 10.1016/S0360-3016(00)00769-0. [DOI] [PubMed] [Google Scholar]
- 11.Terrones-Campos C., Ledergerber B., Vogelius I.R., Helleberg M., Specht L., Lundgren J. Hematological toxicity in patients with solid malignant tumors treated with radiation—Temporal analysis, dose response and impact on survival. Radiother. Oncol. 2021;158:175–183. doi: 10.1016/j.radonc.2021.02.029. [DOI] [PubMed] [Google Scholar]
- 12.Venkatesulu B.P., Mallick S., Lin S.H., Krishnan S. A systematic review of the influence of radiation-induced lymphopenia on survival outcomes in solid tumors. Crit. Rev. Oncol. Hematol. 2018;123:42–51. doi: 10.1016/j.critrevonc.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Damen P.J.J., Kroese T.E., van Hillegersberg R., Schuit E., Peters M., Verhoeff J.J.C., Lin S.H., van Rossum P.S.N. The Influence of Severe Radiation-Induced Lymphopenia on Overall Survival in Solid Tumors: A Systematic Review and Meta-Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2021;111:936–948. doi: 10.1016/j.ijrobp.2021.07.1695. [DOI] [PubMed] [Google Scholar]
- 14.Dai D., Tian Q., Shui Y., Li J., Wei Q. The impact of radiation induced lymphopenia in the prognosis of head and neck cancer: A systematic review and meta-analysis. Radiother. Oncol. 2022;168:28–36. doi: 10.1016/j.radonc.2022.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Liu M., Li X., Cheng H., Wang Y., Tian Y. The Impact of Lymphopenia and Dosimetric Parameters on Overall Survival of Esophageal Cancer Patients Treated with Definitive Radiotherapy. Cancer Manag. Res. 2021;13:2917–2924. doi: 10.2147/CMAR.S297010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu H., Lin M., Hu Y., Zhang L., Li Q., Zhu J., Wang S., Xi M. Lymphopenia during Definitive Chemoradiotherapy in Esophageal Squamous Cell Carcinoma: Association with Dosimetric Parameters and Patient Outcomes. Oncologist. 2021;26:e425–e434. doi: 10.1002/onco.13533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang X., Zhao Z., Wang P., Geng X., Zhu L., Li M. Low Lymphocyte Count Is Associated with Radiotherapy Parameters and Affects the Outcomes of Esophageal Squamous Cell Carcinoma Patients. Front. Oncol. 2020;10:997. doi: 10.3389/fonc.2020.00997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu C., Jin J.Y., Zhang M., Liu A., Wang J., Mohan R., Kong F.S., Lin S.H. The impact of the effective dose to immune cells on lymphopenia and survival of esophageal cancer after chemoradiotherapy. Radiother. Oncol. 2020;146:180–186. doi: 10.1016/j.radonc.2020.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Q., Zhou S., Liu S., Liu S., Yang H., Zhao L., Liu M., Hu Y., Xi M. Treatment-Related Lymphopenia Predicts Pathologic Complete Response and Recurrence in Esophageal Squamous Cell Carcinoma Undergoing Neoadjuvant Chemoradiotherapy. Ann. Surg. Oncol. 2019;26:2882–2889. doi: 10.1245/s10434-019-07334-7. [DOI] [PubMed] [Google Scholar]
- 20.Deng W., Xu C., Liu A., van Rossum P.S.N., Deng W., Liao Z., Koong A.C., Mohan R., Lin S.H. The relationship of lymphocyte recovery and prognosis of esophageal cancer patients with severe radiation-induced lymphopenia after chemoradiation therapy. Radiother. Oncol. 2019;133:9–15. doi: 10.1016/j.radonc.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Davuluri R., Jiang W., Fang P., Xu C., Komaki R., Gomez D.R., Welsh J., Cox J.D., Crane C.H., Hsu C.C., et al. Lymphocyte Nadir and Esophageal Cancer Survival Outcomes After Chemoradiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017;99:128–135. doi: 10.1016/j.ijrobp.2017.05.037. [DOI] [PubMed] [Google Scholar]
- 22.Zhou X.L., Zhu W.G., Zhu Z.J., Wang W.W., Deng X., Tao W.J., Ji F.Z., Tong Y.S. Lymphopenia in Esophageal Squamous Cell Carcinoma: Relationship to Malnutrition, Various Disease Parameters, and Response to Concurrent Chemoradiotherapy. Oncologist. 2019;24:e677–e686. doi: 10.1634/theoncologist.2018-0723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang E., Deng M., Egleston B., Wong J.K., Su S., Denlinger C., Meyer J.E. Dose to Heart, Spine, Aorta, and Body Predict for Severe Lymphopenia and Poor Survival in Patients Undergoing Chemoradiation for Esophageal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2019;105:E206–E207. doi: 10.1016/j.ijrobp.2019.06.2041. [DOI] [Google Scholar]
- 24.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wells G.A., O’Connell B.S.D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [(accessed on 4 May 2022)]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 26.Jackson D., White I.R., Riley R.D. Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat. Med. 2012;31:3805–3820. doi: 10.1002/sim.5453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Routman D., Lester S., Arnett A., Harmsen S., Wittich M.N., Martenson J., Haddock M., Hallemeier C., Merrell K. Lymphocyte count nadir and disease recurrence for patients undergoing trimodality therapy for esophageal cancer. J. Radiat. Oncol. 2018;7:112–138. doi: 10.1007/s13566-018-0348-5. [DOI] [Google Scholar]
- 28.Wang Q., Qiu Q., Zhang Z., Zhang J., Yang G., Liu C., Li B. Bone marrow dosimetric analysis of lymphopenia in patients with esophageal squamous cell carcinoma treated with chemoradiotherapy. Cancer Med. 2021;10:5847–5858. doi: 10.1002/cam4.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nishida M., Sato S., Higashizono K., Taki Y., Nagai E., Wataanbe M., Ohata K., Kanemoto H., Oba N. Total lymphocytes count (TLC) predicts the overall survival after chemoradiotherapy in esophageal carcinoma patients. Dis. Esophagus. 2021;34:5. doi: 10.1093/dote/doab052.100. [DOI] [Google Scholar]
- 30.Cai S., Fan Y., Guo Q., Sun Y., Zhao P., Tian Y., Fan Q. Impact of Radiation Dose to Circulating Immune Cells on Tumor Control and Survival in Esophageal Cancer. Cancer Biother. Radiopharm. 2021. Online ahead of print . [DOI] [PubMed]
- 31.Kroese T.E., Jairam J., Ruurda J.P., Lin S.H., Mohan R., Mook S., Haitjema S., Hoefer I., Haj Mohammad N., Peters M., et al. Severe lymphopenia acquired during chemoradiotherapy for esophageal cancer: Incidence and external validation of a prediction model. Radiother. Oncol. 2021;163:192–198. doi: 10.1016/j.radonc.2021.08.009. [DOI] [PubMed] [Google Scholar]
- 32.So T.H., Chan S.K., Chan W.L., Choi H., Chiang C.L., Lee V., Lam T.C., Wong I., Law S., Kwong D., et al. Lymphopenia and Radiation Dose to Circulating Lymphocytes with Neoadjuvant Chemoradiation in Esophageal Squamous Cell Carcinoma. Adv. Radiat. Oncol. 2020;5:880–888. doi: 10.1016/j.adro.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sherry A.D., Newman N.B., Anderson J.L., Osmundson E.C. Systemic inflammatory dynamics during chemoradiotherapy predict response, relapse, metastasis, and survival in esophageal carcinoma. J. Surg. Oncol. 2019;121:303–312. doi: 10.1002/jso.25793. [DOI] [PubMed] [Google Scholar]
- 34.Fang P., Jiang W., Davuluri R., Xu C., Krishnan S., Mohan R., Koong A.C., Hsu C.C., Lin S.H. High lymphocyte count during neoadjuvant chemoradiotherapy is associated with improved pathologic complete response in esophageal cancer. Radiother. Oncol. 2018;128:584–590. doi: 10.1016/j.radonc.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 35.Douglas P.S., O’Toole M.L., Hiller W.D., Hackney K., Reichek N. Cardiac fatigue after prolonged exercise. Circulation. 1987;76:1206–1213. doi: 10.1161/01.CIR.76.6.1206. [DOI] [PubMed] [Google Scholar]
- 36.Kraehenbuehl L., Weng C.H., Eghbali S., Wolchok J.D., Merghoub T. Enhancing immunotherapy in cancer by targeting emerging immunomodulatory pathways. Nat. Rev. Clin. Oncol. 2022;19:37–50. doi: 10.1038/s41571-021-00552-7. [DOI] [PubMed] [Google Scholar]
- 37.Puhr H.C., Preusser M., Ilhan-Mutlu A. Immunotherapy for Esophageal Cancers: What Is Practice Changing in 2021? Cancers. 2021;13:4632. doi: 10.3390/cancers13184632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teixeira Farinha H., Digklia A., Schizas D., Demartines N., Schafer M., Mantziari S. Immunotherapy for Esophageal Cancer: State-of-the Art in 2021. Cancers. 2022;14:554. doi: 10.3390/cancers14030554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aoto K., Mimura K., Okayama H., Saito M., Chida S., Noda M., Nakajima T., Saito K., Abe N., Ohki S., et al. Immunogenic tumor cell death induced by chemotherapy in patients with breast cancer and esophageal squamous cell carcinoma. Oncol. Rep. 2018;39:151–159. doi: 10.3892/or.2017.6097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly R.J., Zaidi A.H., Smith M.A., Omstead A.N., Kosovec J.E., Matsui D., Martin S.A., DiCarlo C., Werts E.D., Silverman J.F., et al. The Dynamic and Transient Immune Microenvironment in Locally Advanced Esophageal Adenocarcinoma Post Chemoradiation. Ann. Surg. 2018;268:992–999. doi: 10.1097/SLA.0000000000002410. [DOI] [PubMed] [Google Scholar]
- 41.Cho Y., Park S., Byun H.K., Lee C.G., Cho J., Hong M.H., Kim H.R., Cho B.C., Kim S., Park J., et al. Impact of Treatment-Related Lymphopenia on Immunotherapy for Advanced Non-Small Cell Lung Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2019;105:1065–1073. doi: 10.1016/j.ijrobp.2019.08.047. [DOI] [PubMed] [Google Scholar]
- 42.Terrones-Campos C., Ledergerber B., Vogelius I.R., Specht L., Helleberg M., Lundgren J. Lymphocyte Count Kinetics, Factors Associated with the End-of-Radiation-Therapy Lymphocyte Count, and Risk of Infection in Patients with Solid Malignant Tumors Treated with Curative-Intent Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2019;105:812–823. doi: 10.1016/j.ijrobp.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 43.Jin J.Y., Hu C., Xiao Y., Zhang H., Ellsworth S., Schild S.E., Bogart J.A., Dobelbower M.C., Kavadi V.S., Narayan S., et al. Higher radiation dose to immune system is correlated with poorer survival in patients with stage III non-small cell lung cancer: A secondary study of a phase 3 cooperative group trial (NRG Oncology RTOG 0617) Int. J. Radiat. Oncol. Biol. Phys. 2017;99:S151–S152. doi: 10.1016/j.ijrobp.2017.06.351. [DOI] [Google Scholar]
- 44.Yu Y., Fu P., Jin J.Y., Gao S., Wang W., Machtay M., Wang L., Kong F.S., Yu J. Impact of effective dose to immune cells (EDIC) on lymphocyte nadir and survival in limited-stage SCLC. Radiother. Oncol. 2021;162:26–33. doi: 10.1016/j.radonc.2021.06.020. [DOI] [PubMed] [Google Scholar]
- 45.Jin J.Y., Hu C., Xiao Y., Zhang H., Paulus R., Ellsworth S.G., Schild S.E., Bogart J.A., Dobelbower M.C., Kavadi V.S., et al. Higher Radiation Dose to the Immune Cells Correlates with Worse Tumor Control and Overall Survival in Patients with Stage III NSCLC: A Secondary Analysis of RTOG0617. Cancers. 2021;13:6193. doi: 10.3390/cancers13246193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ladbury C.J., Rusthoven C.G., Camidge D.R., Kavanagh B.D., Nath S.K. Impact of Radiation Dose to the Host Immune System on Tumor Control and Survival for Stage III Non-Small Cell Lung Cancer Treated with Definitive Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2019;105:346–355. doi: 10.1016/j.ijrobp.2019.05.064. [DOI] [PubMed] [Google Scholar]
- 47.Alexandru M., Rodica A., Dragos-Eugen G., Mihai-Teodor G. Assessing the Spleen as an Organ at Risk in Radiation Therapy and Its Relationship with Radiation-Induced Lymphopenia: A Retrospective Study and Literature Review. Adv. Radiat. Oncol. 2021;6:100761. doi: 10.1016/j.adro.2021.100761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yalamanchali A., Zhang H., Huang K.C., Mohan R., Lin S.H., Zhu C., Grossman S.A., Jin J.Y., Ellsworth S.G. Patient-Specific Lymphocyte Loss Kinetics as Biomarker of Spleen Dose in Patients Undergoing Radiation Therapy for Upper Abdominal Malignancies. Adv. Radiat. Oncol. 2021;6:100545. doi: 10.1016/j.adro.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saito T., Toya R., Yoshida N., Shono T., Matsuyama T., Ninomura S., Watakabe T., Sasaki Y., Baba H., Oya N. Spleen Dose-Volume Parameters as a Predictor of Treatment-related Lymphopenia During Definitive Chemoradiotherapy for Esophageal Cancer. In Vivo. 2018;32:1519–1525. doi: 10.21873/invivo.11409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang J., Liu X., Cao S., Dong X., Rao S., Cai K. Understanding Esophageal Cancer: The Challenges and Opportunities for the Next Decade. Front. Oncol. 2020;10:1727. doi: 10.3389/fonc.2020.01727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lin S.H., Hobbs B.P., Verma V., Tidwell R.S., Smith G.L., Lei X., Corsini E.M., Mok I., Wei X., Yao L., et al. Randomized Phase IIB Trial of Proton Beam Therapy Versus Intensity-Modulated Radiation Therapy for Locally Advanced Esophageal Cancer. J. Clin. Oncol. 2020;38:1569–1579. doi: 10.1200/JCO.19.02503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Upadhyay R., Venkatesulu B.P., Giridhar P., Kim B.K., Sharma A., Elghazawy H., Dhanireddy B., Elumalai T., Mallick S., Harkenrider M. Risk and impact of radiation related lymphopenia in lung cancer: A systematic review and meta-analysis. Radiother. Oncol. 2021;157:225–233. doi: 10.1016/j.radonc.2021.01.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.