Abstract
The c-fos gene was first described as a proto-oncogene responsible for the induction of bone tumors. A few decades ago, activation of the protein product c-fos was reported in the brain after seizures and other noxious stimuli. Since then, multiple studies have used c-fos as a brain activity marker. Although it has been attributed to neurons, growing evidence demonstrates that c-fos expression in the brain may also include glial cells. In this review, we collect data showing that glial cells also express this proto-oncogene. We present evidence demonstrating that at least astrocytes, oligodendrocytes, and microglia express this immediate early gene (IEG). Unlike neurons, whose expression changes used to be associated with depolarization, glial cells seem to express the c-fos proto-oncogene under the influence of proliferation, differentiation, growth, inflammation, repair, damage, plasticity, and other conditions. The collected evidence provides a complementary view of c-fos as an activity marker and urges the introduction of the glial cell perspective into brain activity studies. This glial cell view may provide additional information related to the brain microenvironment that is difficult to obtain from the isolated neuron paradigm. Thus, it is highly recommended that detection techniques are improved in order to better differentiate the phenotypes expressing c-fos in the brain and to elucidate the specific roles of c-fos expression in glial cells.
Keywords: c-fos, glial cell, astrocytes, microglia, oligodendrocytes, neurons
1. Introduction
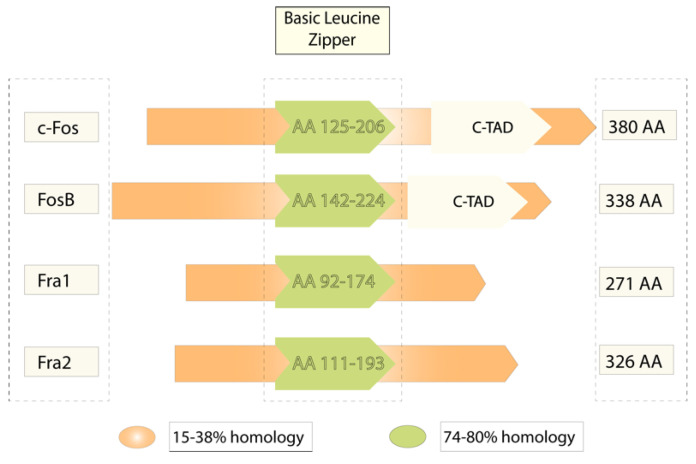
The c-fos proto-oncogene was first described as the gene responsible for the induction of bone tumors by the Finkel–Biskis–Jinkins murine sarcoma virus [1]. It was observed in many species including humans, rats, mice, and chickens [2,3,4,5]. Its length was stated as around 4 kb organized in four exons that encode a unique mRNA and translate into a 55 kDa protein [6]. According to the GenBank of the National Center for Biotechnology Information (NCBI), the FOS family includes the members Fos, Fos-B, Fra1 (FOSL1), and Fra2 (FOSL2), which encode for proteins that contain a leucine zipper and can dimerize with the JUN family. Dimerization forms the activator protein 1 (AP1) complex, which works as a transcription factor (NCBI, 2020; Gene ID: 2353) (Figure 1).
Figure 1.
The Fos gene family members. The picture shows a comparative structure of the products of the fos gene, all of which contain a basic leucine zipper domain, but only c-fos and FosB have a c-terminal transactivator domain (c-TAD). It also indicates the high homology level in the basic leucine zipper domain, which is more variable in other regions.
The product of the c-fos gene is a protein named Fos that may act as a transactivator or transrepressor factor. For instance, dimerization with Jun exerts positive modulation, while binding with the activation transcription factor (ATF) leads to negative control. This activation versatility lies in their relative affinity for binding to various interacting complexes [7,8]. Cell-transforming properties of the fos gene are related to a c-terminus transactivator domain (c-TAD), which is present in Fos and FosB [9]. Since c-fos is not derived from the cell cycle progression and is quickly induced by extracellular stimuli [10,11], it has been identified as an immediate expression gene (IEG) [12].
Fos and c-fos genes have been associated with proliferation, differentiation, transformation, and cellular death [13,14,15,16]. Rapid and transiently, c-fos can be expressed by almost every cell as an important piece in cell signal transduction derived from growth, maturation, factor release, or physic stress (wounds, heat, etc.). It can be induced by many stimuli, including the protein kinase C (PKC), intracellular calcium release, steroid hormones, and neurotransmitters [6,17,18,19,20]. Since its expression is transitory in synchronized cells, it can be difficult to observe in non-synchronized cells [16]. Thus, c-fos is a transcription factor whose expression is quickly and synchronically induced; many studies have promoted its use as a marker of stimuli-induced changes in brain activity. Expression changes have mostly been attributed to neurons; however, as glial cells are the main regulators of growth, regeneration, and inflammation in the brain, it is highly expected that some of the c-fos-expressing cells correspond to glial phenotypes. Next, we will explore the main data linking c-fos to the brain, and then, we will focus on evidence specifically linking this marker to the glial phenotypes.
2. c-fos in the Brain
At the end of the past century, some IEGs were associated with stimuli–transcription activity in the brain. The most commonly used reporter for this phenomenon was the c-fos gene, whose expression in neurons was described to be transient [21]. As a marker of cellular activity, c-fos was subsequently used to identify brain regions implicated in stimuli processing [22,23] or relationships between two or more brain areas [4]. Similar to electrophysiology, it was used to measure neuronal activity but also provided information about morphology and cell type both in vivo [24,25,26,27] and in vitro [28,29]. The most commonly used methods to reveal c-fos changes became immunohistochemistry and Western blotting (in situ hybridization). In addition, c-fos expression was also employed in transgenic models (i.e., fos-LacZ) to inactivate some genes in a quantitative manner [10,30,31,32]. More recently, optogenetic models used c-fos to mark and manipulate specific brain nuclei [33].
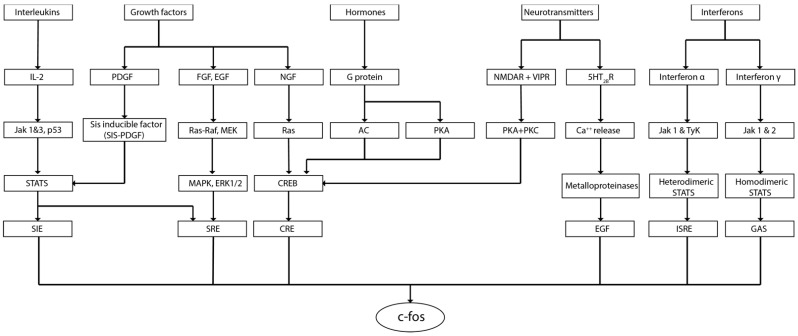
Former studies investigating the expression of c-fos in neuroblastic cells supported the use of this marker to evidence changes in brain activity. Neuroblastic cultures demonstrated that nerve growth factor (NGF) [10], phosphatidic acid [34], epidermal growth factor (EGF), fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), insulin, and potassium chloride (KCl) could induce the expression of c-fos in these cells [35]. Following experiments characterized the main cell pathways able to activate c-fos in neural cells [10,34,35]. It was demonstrated that growth factors, interferons, interleukins, calcium release, and G-protein ligands could initiate phosphorylation cascades, affecting c-fos expression. The phosphorylation proteins Jak 1-2, tyrosine kinase 2 (Tyk2), calmodulin kinases (CaMks), and protein kinase A (PKA) were described as key components of these pathways. The second messengers cAMP, GTP, and Ca2+ were evidenced as main mediators. Signaling complexes such as ras-raf, MEK-MAPK, or cAMP Response Element-Binding proteins (CREB) were also recognized in the c-fos signaling map. The list of transcription regulators affecting c-fos expression included the serum response element (SRE), cAMP response element (CRE), SIF-inducible element (SIE), interferon stimulation response element (ISRE), and IFN-γ-activated site (GAS) [6,11,36,37]. Pathways affecting c-fos expression are summarized in Figure 2.
Figure 2.
Cell signaling pathways that might induce c-fos expression.
To our knowledge, c-fos was initially used in brain research to measure the neural activity after seizures. In this area, it allowed researchers, for example, to map the neuronal pathways involved in different models/intensities of the seizure [38,39,40]; to estimate the effect of antiepileptic drugs [41]; or to analyze new-born cells and asymmetries after seizures [42,43]. c-fos has also been consolidated as a reliable marker for cell activation derived from learning [14] and memory [44,45]. The use of c-fos expression permitted researchers to predict cognitive worsening in Alzheimer’s disease and other conditions [46,47]. The relevance of sleep for memory acquisition and synaptic plasticity was also investigated by measuring c-fos during REM sleep [48]. Furthermore, c-fos was crucial to elucidating the role of the amygdala, thalamus, and hypothalamus in conditioned fear processing [49] and the epigenetic regulation of neuroplasticity [50], and cognition [51].
Studies of psychiatric disorders and their therapeutics also benefited from the use of c-fos. Fos, Fos-B, Jun, and Egr1 were reported to be upregulated in patients suffering from schizophrenia [52]. The antidepressant effect of optogenetic stimulation in the medial prefrontal cortex (mPFC) was assessed by mapping c-fos expression [53], and some antipsychotic drug effects in the brain were located through fos expression [54,55]. Stress studies, on the other hand, demonstrated activity changes in the frontal cortex and many limbic structures [56,57,58] that may predict susceptibility [59] or resilience to stress [60]. Moreover, it has been suggested that c-fos/Fos-B could be reliable markers for investigating the adaptive capabilities of the brain under stress conditions [61,62]. In addition, the study of endocrine responses demonstrated that suckling can modify the c-fos expression in the cerebral cortex [63], and that metabolic dysfunction produced by diabetes activates c-fos in the bed nucleus of stria terminalis (BNST) [64]. Research on circadian cycles and their alterations also evidenced c-fos changes in the suprachiasmatic nuclei (SCN), the main pacemaker in mammals [65,66]. Hypothalamic changes in c-fos levels may be used to measure altered circadian rhythmicity [67], intraspecific alternative chronotypes [68], or differences between diurnal and nocturnal animals [69,70].
Models inducing brain injury evidenced that c-fos increases 3 h after damage but also 3 days later. Thus, c-fos can accompany the immediate neuroprotective effects after brain edema, but also the delayed apoptosis in later stages of the lesion [71]. On the other hand, models inducing pain in the brain confirmed c-fos’s ability to map the brain areas involved in nociception [72,73], and allowed researchers to elucidate the role of periaqueductal gray and adenylate-cyclase-activating polypeptide-38 (PACAP-38) [74] in nociception [75]. In addition, fos immunoreactivity permitted researchers to describe a non-canonical auditory nociceptive system evidencing that cochlear nuclei could be active in deaf mice exposed to noxious levels of noise (120 dB) [76]. Thus, it is clear that c-fos has a crucial role in signal transduction across the brain, but studies have prioritized neuronal cells. As mentioned before, c-fos could potentially be expressed in every cell type, and that could include the non-neuronal residents of the brain, the glial cells.
3. Glial Cells
Although glial cells have been acknowledged for their supportive role in maintaining neurons and brain homeostasis for years, a number of studies have shown that these non-neuronal cells are active regulators for the majority of the brain functions. For instance, glial cells regulate immune and stress responses [77,78], formation, development, and pruning of synapses [79], neurotransmitter uptake [80], blood–brain barrier formation [81], axonal guidance [82], and myelinization [83]. Glial cells have been typically grouped into two great groups: macroglia and microglia, which in turn subdivide again to describe more specific cell phenotypes.
Macroglia include astrocytes, oligodendrocytes, NG2 cells (oligodendroglial precursor cells), and ependymal cells [78]. Macroglia possess many physiological roles, ranging from neural progenitors (i.e., neurogenesis, astrogenesis, oligodendrogenesis) to structural pieces of the brain (the classic supportive role of glia) [84].
Astrocytes are perhaps the most versatile cells in the brain. They are one of the integral components of the synapse (tripartite synapse) [85,86], play a major role in the uptake and metabolism of neurotransmitters [80,87], modulate the energetical metabolism [88,89], promote and support neuronal migration [90,91], maintain the ionic balance in the synaptic and extrasynaptic space [92,93], take part in the blood–brain barrier [81,94], and represent the main source of neurogenesis and gliogenesis [82,95,96]. Astrocytes can be classified as fibrous, protoplasmic, and radial astrocytes, mainly attending to their morphology and localization. Figure 3 illustrates this.
Figure 3.
Illustration of the main astrocyte subtypes.
Oligodendrocytes are mainly known for their role as myelinating cells. They are responsible for the optimal conduction of neuronal impulses and are able to influence and modify electrical activity [83,97,98]; in addition, oligodendrocytes supply iron to the brain, provide growth factors, and offer metabolic support [99,100,101,102]. Brain myelinating cells can be classified as interfascicular, perivascular, or perineuronal [101,103].
NG2 cells are also known as oligodendrocyte precursor cells (OPCs). They are multipotent glial cells that can carry out morphological and proliferative changes in response to several stimuli, such as demyelination and injury [104,105]. OPCs can also induce proinflammatory responses through cytokine release [106] or through regulation of microglial transition into states of activation [107]. These cells can differentiate into other glial cell types [108] or even neuronal phenotypes [109,110].
Ependymocytes are the cells lining the ventricular walls and the ones that produce the cerebrospinal fluid [111]; they can also help and guide neuronal migration through cerebrospinal currents [112]. Ependymal cells are derived from radial glia, and even though their proliferative properties remain controversial, evidence suggests they have no proliferative role in the mature brain [113].
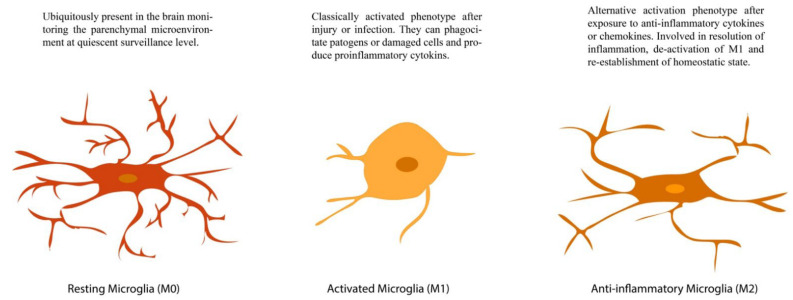
Microglia, on the other hand, were first described as the innate immune cell of the brain [114]. Beyond immune function, microglia also influence the pruning of dendrite processes, regulate the physiochemical microenvironment, influence the production and release of growth and survival factors, and promote apoptosis and cleaning of cell detritus [115,116,117]. Many of these roles depend on their activation state, which, according to morphological changes, can be classified as M0 (resting), M1 (pro-inflammatory, classical, or macrophage activation), and M2 (anti-inflammatory or alternative activation) [114,118]. Figure 4 illustrates this.
Figure 4.
Activation states in microglial cells. Schematic representation of an M0 (left), M1 (center), and M2 (right) microglia.
Hence, glial cells exert crucial roles for the correct functioning of the brain, ranging from proliferation to communication, both under physiological circumstances and pathological conditions. c-fos has been shown to be crucially involved in most of these conditions; so, it is not illogical to think that this IEG may be specifically involved in glial cell activity and signaling. On the contrary, as c-fos a rapidly activated gene in stimulated cells, it may also provide information on the glial activation patterns. Thus, in the next section, we will summarize the findings supporting this idea.
4. c-fos and Glial Cells: Evidence and Perspectives
As mentioned before, glial cells are the most abundant and versatile cells in the brain; they interact with neurons, blood vessels, and other glial cells to regulate the many functions of the brain. We stated that they act in coordination and interact with each other to maintain homeostasis and shape the distinctive actions of the CNS. We also summarized the current knowledge of c-fos dynamics and highlighted the crucial role of this family of genes in promoting and maintaining the homeostasis of the CNS microenvironment. Now, we propose that glial cells are sensitive to the actions of the IEG c-fos.
To our knowledge, the first set of studies exploring in vivo expression of c-fos in glial cells was published at the end of the 1980s, when researchers investigated the nature of proliferative cells in the surroundings of a damaged area. These studies suggested that some of the cells expressing c-fos near the injured area corresponded to a glial phenotype. Since the proliferation of neurons was not expected, initial observations assumed that c-fos-positive new-born cells were glial cells. Complementary experiments allowed researchers to demonstrate that at least some of the c-fos-expressing cells could be GFAP-positive (astrocytes) [119,120]. Since then, astrocytes have been the most investigated cell type regarding c-fos expression.
4.1. c-fos in Astrocytes
Initial studies investigating c-fos in this population explored implications in proliferation/maturation. Former in vitro experiments evaluated whether the mitogenic agents EGF, FGF, tetradecanoyl phorbol acetate (TPA), dbcAMP, or forskolin were able to induce c-fos in astrocytes. They found that these agents strongly induce c-fos and that major expression rates should be expected from 20 to 45 min after treatment [121]. In vitro stimulation of neurotransmitter systems also induced c-fos in astrocytes. Carbachol (cholinergic agonist), norepinephrine (NE), isoproterenol (ISO; β-adrenergic agonist), and phenylephrine (PHE; α-adrenergic agonist) were used to demonstrate that stimulation of c-fos through cholinergic or adrenergic pathways can modulate secondary genes or induce phenotypic changes [122]. The role of c-fos in astrocyte proliferation and differentiation was also explored by using mitogens (EGF, bFGF, db-cAMP, TPA) or depolarizing conditions (elevations in Ca2+ uptake or high concentrations of K+). Results showing that mitogens but not depolarization enhanced the expression indicate that c-fos could be specifically involved in astrocyte proliferation/differentiation [123]. Additionally, serotonin induces c-fos in astrocytes through its receptor 5HT2BR, which in turn enhances calcium release, metalloproteinases, and EGF release [20]. The use of endothelins to stimulate astrocytes corroborated that c-fos might be implicated in NGF expression during brain development [124]. Later in the 1990s, it was evidenced that the calcitonin-gene-related peptide (CGRP), a molecule produced by damage, was able to induce dose–response expression of c-fos in astrocytes. Since forskolin (an adenylate cyclase activator) reduced its effect, it was supposed cAMP had a role in the induction of c-fos associated with transformation and reparation of the injured brain [125].
Immune system mediators are also implicated in the glial expression of IEGs. c-fos and c-jun have been reported to be increased in astrocytes exposed to IFN-γ in a dose–response manner [11]. The IFN-γ-induced expression of c-fos in astrocytes regulates the complement factor H, whose abnormal levels instead induce neuronal loss in pathologies such as Alzheimer’s disease [126]. Other cytokines (TNF-α, IL-1β, and IFN-γ) and lipopolysaccharides (LPS) involved in inflammation modulate the expression of c-fos in astrocytes. LPS, LPS+ IL-1β, and IFN-γ induce c-fos in these cells. TNF-α, on the other hand, may enhance the LPS-induced increases in c-fos [127]. LPS induction of c-fos involves the p38 MAPK pathway, which activates Elk1, CREB/ATF-1, and later the SRE or CRE promoter [128]. Astrocytes infected with the adenovirus Ad.βGal expressed both c-fos and the apoptotic marker caspase-3, suggesting that c-fos can also indicate apoptosis [129]. Moreover, experimental autoimmune encephalitis allowed researchers to characterize a subpopulation of c-fos-expressing astrocytes named ieastrocytes. In this experimental model, the reporter system TetTag/green fluorescent protein was used to reveal the historical activity of c-fos in astrocytes. Promising results suggest astrocyte c-fos activity is a biomarker for autoimmune encephalitis [3].
Experimental models of damage also evidenced the activity of c-fos in astrocytes. In vitro models of heat shock and scratch wound showed not only that astrocytes express c-fos, but also that quercetin can inhibit the hypertrophy induced by scratches. That suggests that reactive astrogliosis could be associated with c-fos expression [130]. Experimental ocular hypertension models also demonstrated c-fos expression in astroglia. Monkeys with experimental glaucoma and astrocyte cultures of human glaucomatous optic nervous were found to overexpress c-fos [32]. Ischemia was also reported to induce quick and transient expression of the c-fos gene in cultured astrocytes. Those experiments exhibited that astrocytes rapidly increase the expression of c-fos after 30 min, reach a maximal expression level after 60 min, and diminish their expression levels after 2 h [131]. Chemical hypoxia, in turn, reverted the enhancing effect of ATP on the expression of c-fos [132]. Mimicking excitotoxicity, it was found that glutamate stimulation of astrocytes can rapidly increase the expression of c-fos since peak levels were reached 1 h after exposure [133]. Glutamate enhancements of c-fos could be mediated by mGluR5 and calcium dynamics since the addition of BAPTA (a calcium chelator) inhibits this enhancement [134].
Other conditions have been demonstrated to induce c-fos in astrocytes. Angiotensin II (AngII), for instance, can differentially regulate IEGs with lower increases in c-jun in contrast to c-fos. For some researchers, AngII dysregulation could lead to pathological responses through modulation of astrocytic c-fos expression [135]. The antidepressant fluoxetine was also evidenced to show a dual response varying with the effect of the dose; higher doses (5, 10 μM) enhance c-fos expression through ERK1/2, while lower doses (0.5, 1 μM) inhibit astrocyte expression of c-fos by the Akt pathway [136]. Conditions such as stress exposure or cognitive assessments have also evidenced c-fos induction in this population. It has been reported, for example, that learning activates c-fos in hippocampal astrocytes [137] and that restraint stress increases GFAP/c-fos+ in exposed subjects [138]. Table 1 summarizes these works.
Table 1.
Papers evidencing c-fos expression in astrocytes. Arrows indicate ↑ increased expression or ↓ diminished expression under different stimulation models.
| Paper | Effect | Model | Approach | Methodology | Studied Area | Species |
|---|---|---|---|---|---|---|
| [119] | ↑ After 1 h | Heat shock insult | In vivo | Immunohistochemical | Thalamus, hippocampus, corpus callosum, internal capsule, and fornix/fimbria | Rat |
| [121] | ↑ After 30 min | Mitogens and growth factor exposure | In vitro | Northern blot | Primary cultures of cortical astrocytes (In secondary cultures) |
Rat |
| [122] | ↑ After 30–60 min | Muscarinic and adrenergic agonist exposure | In vitro | Northern blot | Primary cultures of cortical astrocytes (In secondary cultures) |
Rat |
| [123] | -↑ After 30 min mRNA and 2 h protein -No change |
-Mitogen exposure -Depolarizing conditions |
In vitro | Northern blot and immunohistochemical | Primary cultures of neocortical astrocytes | Rat |
| [125] | ↑After 30 min | Damage-associated molecular pattern (DAMPs) | In vitro | Northern blot | Primary cultures of cortical astrocytes | Rat |
| [124] | ↑After 30 min | Endothelin exposure | In vitro | Northern blot | Rat astrocytoma C6 cells (C6-S and C6-V subclones) and primary cultures of cortical and striatal astrocytes | Rat/Mouse |
| [139] | ↑After 30–60 min | Scratch wound of culture astrocytes | In vitro | Quantitative reverse transcriptase polymerase chain reaction (RT-PCR | Primary cultures of cortical astrocytes | Rat |
| [131] | ↑0.5–2 h, peak at 1 h | Ischemic model (mineral oil) | In vitro | RT-PCR | Primary cultures of cortical astrocytes | Rat |
| [11] | ↑After 30 min | Proinflammatory factor exposure | In vitro | Northern blot and flow cytometry | Primary cultures of cortical astrocytes | Mouse |
| [132] | ↑After 15–60 min | Chemical hypoxia (0.5 mM cyanide for 1 h) | In vitro | Northern blot | RBA-2 type 2 astrocytes cell line | Rat |
| [130] | ↑ NA | Heat shock insult | In vitro | Western blot | Primary cultures of astrocytes | Mouse |
| [140] | ↑1 h, peak at 2 h | LPS administration | In vivo | Immunohistochemical | Hypothalamic supraoptic nucleus, posterior and anterior pituitary | Rat |
| [129] | ↑0.5–1 h, peak at 30 min | Adenovirus (Ad.βGal) exposure | In vitro | Northern blot | Primary cultures of cortical astrocytes | Mouse |
| [127] | ↑1 h | Proinflammatory factor exposure | In vitro | Northern blot | Primary cultures of astrocytes | Rat |
| [134] | ↑After 15–30 min, peak at 30 min | Glutamate stimulation in excitotoxic levels | In vitro | Northern blot and immunohistochemical | Primary cortical glial cell cultures | Rat |
| [141] | ↑After 1 h | Bradykinin exposure | In vitro | Western blot and RT-PCR | RBA-1 cell line | Rat |
| [126] | c-fos binding to mCFH promoter | NA | In vitro | Electrophoretic mobility shift assay (EMSA) and supershift assay | Astrocyte 2.1 (Ast 2.1) cell line and primary astrocytes, microglia and oligodendrocytes cultures |
Mouse |
| [142] | Nuclear translocation | Amitriptyline exposure | In vitro | Western blot and real-time PCR | Primary cultures of astrocytes | Rat |
| [143] | ↑After 1 h | Forskolin and IL-1 exposure | In vitro/ in vivo | Western blot and qPCR | Human cortical astrocytes/KO mouse | Human/ Mouse |
| [136] | ↓ After 1 h at low doses (0.5–1 μM) ↑After 1 h at high doses (5–10 μM) |
Fluoxetine exposure | In vitro | Western blot and RT-PCR | Primary cultures of astrocytes | Mouse |
| [137] | ↑ After 90 min | Viral vector injection and CNO administration | In vivo | Immunohistochemical | Hippocampus | Mouse |
| [3] | ↑ NA | Experimental autoimmune encephalomyelitis (EAE) | In vivo | Immunolabeling-enabled three-dimensional imaging of solvent-cleared organs (iDISCO) and flow cytometry | TetTag-cFos reporter mice | Mouse |
4.2. c-fos in Oligodendrocytes
Although astrocytes represent the vast majority of experiments investigating c-fos in glial cells, oligodendrocytes have also been the target of some experiments. Like astrocytes, growth factors (bFGF, EGF, PDGF, and IGF-1) were reported to stimulate proliferation or maturation in OPCs, also known as NG2-glia. It was then reported that PKC and c-fos were required for this effect since blocking with H-7 (a PKC inactivator) resulted in inhibited proliferation [144,145]. The idea of c-fos as a promoter of proliferation/maturation of oligodendroglia became strengthened when experiments demonstrated that maturation of NG2 cells was preceded by c-fos expression [146]. Moreover, reports showed that c-fos-expressing oligodendrocytes exhibited a dose-dependent decrease in proliferation [147]. Oligodendrocyte proliferation can also be induced by carbachol, a cholinergic analogous that acts as a growth factor and also activates PKC and c-fos [148]. Norepinephrine, on the other hand, was also proved to exert a c-fos proliferative effect on oligodendrocytes. Calcium dependence of this process was suggested since sensitive G proteins, inositol phosphate 3 kinase (IP3K), and PKC were also activated [149].
Some pathologic conditions also affect the expression of c-fos in oligodendroglia. It was demonstrated that oligodendrocytes can express c-fos under glutamate stimulation too. Maximal expression levels were reported 60 min after exposure, and returns to basal levels were observed 6 h later. Glutamate experiments demonstrated that c-fos induction is mediated by AMPA-R and KA-R but not NMDA-R since specific antagonist CNQX and DNQX inhibited the effect, but MK-801 (NMDA-specific antagonist) failed to inhibit c-fos expression. Hypoxic conditions are also able to induce c-fos in oligodendrocytes. Hypoxia models demonstrated that oligodendrocytes express c-fos as an event preceding myelin loss, axonal damage, and apoptotic death [150]. There is also evidence that c-fos expression is stimulated by the hallucinogen d-LSD in vivo, an action possibly linked to the modulation of neuronal impulses or growth factor production [151]. Finally, it was reported that c-fos expression diminished with maturation in oligodendrocytes, but ethanol consumption retarded this decrease as well as the myelin basic protein (MBP) production [152]. These works are summarized in Table 2.
Table 2.
Papers evidencing c-fos expression in oligodendrocytes.
| Paper | Effect | Model | Approach | Methodology | Studied Area | Species |
|---|---|---|---|---|---|---|
| [144] | ↑After 30 min | Mitogenic and growth factors exposure | In vitro | Northern blot and immunohistochemical | OPCs isolated from mixed glial cell cultures | Rat |
| [145] | ↑After 0.25–8 h, peak at 1 h | Basic fibroblast growth factor (bFGF) exposure | In vitro | Northern blot and immunohistochemical | OPCs isolated from mixed glial cell cultures | Rat |
| [147] | ↑After 0.25–6 h, peak at 1 h | Glutamate exposure | In vitro | Northern blot | OPCs isolated from mixed glial cell cultures | Rat |
| [148] | ↑After 30–60 min | Carbachol exposure | In vitro | Northern blot and immunohistochemical | OPCs isolated from mixed glial cell cultures | Rat |
| [149] | ↑After 30–60 min | NE exposure | In vitro | Western and Northern blot | OPCs isolated from mixed glial cell cultures | Rat |
| [150] | ↑ 1, 6, and 9 days after induction with progressive increases | Experimental anterior optic nerve ischemia | In vivo | Quantitative real-time PCR (qRT-PCR) and immunohistochemical | Optic nerve | Mouse |
| [151] | ↑After 90 min | d-LSD exposure | In vivo | Immunohistochemical | Prefrontal cortex | Rat |
| [152] | Delayed downregulation of c-fos levels during differentiation |
Ethanol administration | In vitro | Western blot | CG-4 glial cell line | Rat |
| [146] | ↑After 2 hours/day of SMF stimulation (0.3 T) for a period of 14 days | Static magnetic field (SMF) stimulation | In vitro | qRT-PCR | Human OPCs derived from induced pluripotent stem cells | Human |
4.3. c-fos in Microglia
Given the mesodermal immune origin of microglia, it is highly expected that c-fos modulates some actions in this lineage. Even so, less research has explored this, with some pieces of evidence indicating that c-fos can be expressed by the immune residents of the brain. For instance, there are experiments showing that excitotoxic glutamate stimulation, through any of its ionotropic receptors or group I of metabotropic receptors, is able to induce c-fos expression and microglial activation [153]. In addition, it was reported that stimulation with kainic acid (KA) increases the expression of MHCII and class II transactivator (CIITA) in microglia, but coincidently, both are inhibited by pretreatment with triptolide, which actually decreases the phosphorylation of c-fos and c-jun and the consequent formation of AP1 [154].
Proinflammatory effects have been proposed for the expression of c-fos in microglia. It is known that microglial NOD-like receptor 3 (NLRP3) is associated with neuroinflammation and is also a therapeutic target in Alzheimer’s disease. Thus, the anti-inflammatory effects of dexmedetomidine inhibit NLRP3-derived inflammasome, modulating the c-fos upregulated expression [155]. As in other glial types, there is also evidence showing that LPS can induce the expression of c-fos in microglia and the consequent inflammation in the brain [156]. Additionally, studies of paraquat, an herbicide that is associated with a higher incidence of Parkinson’s disease, have evidenced that this substance can induce c-fos expression, as well as HSP60 and TLR4, which then increases the proinflammatory cytokine production and accelerates inflammatory responses [157]. We recapitulate these studies in Table 3.
Table 3.
Papers evidencing c-fos expression in microglia.
| Paper | Effect | Model | Approach | Methodology | Studied Area | Species |
|---|---|---|---|---|---|---|
| [153] | ↑After 30 min (mRNA) ↑After 2 h postexposure (protein) |
10-50-fold higher doses of glutamate than physiological exposure | In vitro | RT-PCR, Western blot, and immunohistochemical | Primary cortical microglial cells | Rat |
| [154] | ↑p-c-fos after 2 h (KA) | Kainic acid (KA) exposure | In vitro | Western blot | BV-2 microglia cell line | Mouse |
| [155] | ↓ Dose-dependent (Dex) | LPS/ATP and Dexmedetomi-dine (Dex) treatment | In vitro | PCR, Western blot, and immunohistochemical | Human microglia clone 3 cell line (HMC3) |
Human |
| [156] | ↑2 h after treatment (BV-2 cells) ↑2–6 h after treatment (hypothalamus) |
LPS treatment | In vivo/in vitro | PCR, Western blot, and immunohistochemical | BV-2 microglia cell line/hippocampus and hypothalamus | Mouse/rat |
| [157] | ↑6, 12, and 24 h of treatment | Paraquat and LPS exposure | In vitro | qRT-PCR | BV-2 microglia cell line | Mouse |
5. Conclusions and Perspectives
Here, we compiled evidence supporting the relevance of c-fos for brain functions. Beyond neurons whose implications have been well-documented, we showed that glial cells represent an unexplored but very attractive target for c-fos investigation. Beyond depolarization, whose actions have been well-documented in neurons, the available evidence supports that c-fos expression may also accompany proliferation, maturation, repair, and damage in the brain. All of these functions are intensely linked to glial functions.
As stated above, astrocytes have been by far the most attended cells regarding c-fos expression in glial cells. It seems that proliferation/reparation are the phenomena most strongly linked to c-fos expression in this glial type. Thus, identification of c-fos changes in this phenotype could be useful to rapid and reliably predict physiological or pathological responses to specific stimuli. Reactive gliosis, scar formation, and other astrocyte actions involving proliferation/transformation could be predicted by measuring c-fos dynamics.
Oligodendrocyte research permitted researchers to posit that this activity marker may also be involved in differentiation, maturation, and obviously myelin formation. In this case, c-fos expression could be helpful in gaining knowledge on how the brain responds to stimuli affecting axonal conductivity. It is worth mentioning the relevance of the NG2 cells not only as oligodendrocyte precursors but also as specialized/differentiated cells able to support and contribute to the good functioning of the brain. Thus, exploration of c-fos changes in this subpopulation is now mandatory.
Microglia, on the other hand, evidenced that c-fos may be a powerful tool with which the immune/inflammatory responses conducted in the brain can be elucidated. Given that many cytokine genes are regulated cooperatively by a transcription factor complex that includes AP-1, c-fos could be an accurate sensor of inflammation in the brain and a reliable marker for the progression of some inflammatory diseases.
As studies investigating the link between c-fos and glial cells are still scarce, and many questions remain unanswered, we can now suggest the need for an effort to increase the specificity to evaluate neuronal and non-neuronal activity through c-fos.
First, we would like to conclude by affirming that the evidence presented here allows researchers to maintain that studies evaluating brain activity through c-fos must consider the possibility that some of the activated cells could be glial cells. Second, we would like to invite the scientific community to attend the question of the role of c-fos in glial cells. Answers on how, where, or when specific cells express c-fos will strongly contribute to the understanding of the brain function. We would also like to urge the community to determine and use adequate approaches to accurately define phenotypes involved in the cellular response to a myriad of physiological and/or pathological stimuli commonly assessed by c-fos expression. By doing this, we can make sure that brain activity changes correspond to different cell phenotypes and gain knowledge on how glial cells participate in the many functions of the brain.
Acknowledgments
We thank the Neuroscience Department of the University of Guadalajara for the space and human resources donated to the accomplishment of this review.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by APPAC-CUCS-2022 and Programa de fortalecimiento a Institutos, Centros y Laboratorios de Investigación CGIPV 2022.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Curran T., Peters G., Van Beveren C., Teich N.M., Verma I.M. FBJ murine osteosarcoma virus: Identification and molecular cloning of biologically active proviral DNA. J. Virol. 1982;44:674–682. doi: 10.1128/jvi.44.2.674-682.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larsen H.M., Hansen S.K., Mikkelsen J.D., Hyttel P., Stummann T.C. Alpha7 nicotinic acetylcholine receptors and neural network synaptic transmission in human induced pluripotent stem cell-derived neurons. Stem Cell Res. 2019;41:101642. doi: 10.1016/j.scr.2019.101642. [DOI] [PubMed] [Google Scholar]
- 3.Groves A., Kihara Y., Jonnalagadda D., Rivera R., Kennedy G., Mayford M., Chun J. A Functionally Defined In Vivo Astrocyte Population Identified by c-Fos Activation in a Mouse Model of Multiple Sclerosis Modulated by S1P Signaling: Immediate-Early Astrocytes (ieAstrocytes) eNeuro. 2018;5 doi: 10.1523/ENEURO.0239-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Ortega E., Canadas F., Carvajal F., Cardona D. In vivo stimulation of locus coeruleus: Effects on amygdala subnuclei. Acta Neurobiol. Exp. 2017;77:261–268. doi: 10.21307/ane-2017-060. [DOI] [PubMed] [Google Scholar]
- 5.Bussolino D.F., de Arriba Zerpa G.A., Grabois V.R., Conde C.B., Guido M.E., Caputto B.L. Light affects c-fos expression and phospholipid synthesis in both retinal ganglion cells and photoreceptor cells in an opposite way for each cell type. Brain Res. Mol. Brain Res. 1998;58:10–15. doi: 10.1016/S0169-328X(98)00065-5. [DOI] [PubMed] [Google Scholar]
- 6.Piechaczyk M., Blanchard J.M. C-fos proto-oncogene regulation and function. Crit. Rev. Oncol. Hematol. 1994;17:93–131. doi: 10.1016/1040-8428(94)90021-3. [DOI] [PubMed] [Google Scholar]
- 7.Distel R.J., Spiegelman B.M. Protooncogene c-fos as a transcription factor. Adv. Cancer Res. 1990;55:37–55. doi: 10.1016/s0065-230x(08)60467-4. [DOI] [PubMed] [Google Scholar]
- 8.Wilson T., Treisman R. Fos C-terminal mutations block down-regulation of c-fos transcription following serum stimulation. EMBO J. 1988;7:4193–4202. doi: 10.1002/j.1460-2075.1988.tb03316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wisdon R., Verma I.M. Transformation by Fos proteins requires a C-terminal transactivation domain. Mol. Cell. Biol. 1993;13:7429–7438. doi: 10.1128/mcb.13.12.7429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curran T., Morgan J.I. Fos: An immediate-early transcription factor in neurons. J. Neurobiol. 1995;26:403–412. doi: 10.1002/neu.480260312. [DOI] [PubMed] [Google Scholar]
- 11.Rubio N. Interferon-gamma induces the expression of immediate early genes c-fos and c-jun in astrocytes. Immunology. 1997;91:560–564. doi: 10.1046/j.1365-2567.1997.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cochran B.H., Reffel A.C., Stiles C.D. Molecular cloning of gene sequences regulated by platelet-derived growth factor. Cell. 1983;33:939–947. doi: 10.1016/0092-8674(83)90037-5. [DOI] [PubMed] [Google Scholar]
- 13.Miao G.G., Curran T. Cell transformation by c-fos requires an extended period of expression and is independent of the cell cycle. Mol. Cell. Biol. 1994;14:4295–4310. doi: 10.1128/mcb.14.6.4295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goelet P., Castellucci V.F., Schacher S., Kandel E.R. The long and the short of long-term memory—A molecular framework. Nature. 1986;322:419–422. doi: 10.1038/322419a0. [DOI] [PubMed] [Google Scholar]
- 15.Gonda T.J., Metcalf D. Expression of myb, myc and fos proto-oncogenes during the differentiation of a murine myeloid leukaemia. Nature. 1984;310:249–251. doi: 10.1038/310249a0. [DOI] [PubMed] [Google Scholar]
- 16.Greenberg M.E., Ziff E.B. Stimulation of 3T3 cells induces transcription of the c-fos proto-oncogene. Nature. 1984;311:433–438. doi: 10.1038/311433a0. [DOI] [PubMed] [Google Scholar]
- 17.Morgan J.I., Curran T. Stimulus-transcription coupling in the nervous system: Involvement of the inducible proto-oncogenes fos and jun. Annu. Rev. Neurosci. 1991;14:421–451. doi: 10.1146/annurev.ne.14.030191.002225. [DOI] [PubMed] [Google Scholar]
- 18.Kanda N., Watanabe S. 17Beta-estradiol enhances the production of nerve growth factor in THP-1-derived macrophages or peripheral blood monocyte-derived macrophages. J. Investig. Dermatol. 2003;121:771–780. doi: 10.1046/j.1523-1747.2003.12487.x. [DOI] [PubMed] [Google Scholar]
- 19.Magistretti P.J., Cardinaux J.R., Martin J.L. VIP and PACAP in the CNS: Regulators of glial energy metabolism and modulators of glutamatergic signaling. Ann. N. Y. Acad. Sci. 1998;865:213–225. doi: 10.1111/j.1749-6632.1998.tb11181.x. [DOI] [PubMed] [Google Scholar]
- 20.Peng L., Li B., Du T., Kong E.K., Hu X., Zhang S., Shan X., Zhang M. Astrocytic transactivation by alpha2A-adrenergic and 5-HT2B serotonergic signaling. Neurochem. Int. 2010;57:421–431. doi: 10.1016/j.neuint.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 21.Hudson A.E. Genetic Reporters of Neuronal Activity: C-Fos and G-CaMP6. Methods Enzymol. 2018;603:197–220. doi: 10.1016/bs.mie.2018.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campeau S., Akil H., Watson S.J. Lesions of the medial geniculate nuclei specifically block corticosterone release and induction of c-fos mRNA in the forebrain associated with audiogenic stress in rats. J. Neurosci. 1997;17:5979–5992. doi: 10.1523/JNEUROSCI.17-15-05979.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campeau S., Dolan D., Akil H., Watson S.J. C-fos mRNA induction in acute and chronic audiogenic stress: Possible role of the orbitofrontal cortex in habituation. Stress. 2002;5:121–130. doi: 10.1080/10253890290027895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Umezu T., Shibata Y. Brain regions and monoaminergic neurotransmitters that are involved in mouse ambulatory activity promoted by bupropion. Toxicol. Rep. 2016;3:552–562. doi: 10.1016/j.toxrep.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fetterly T.L., Basu A., Nabit B.P., Awad E., Williford K.M., Centanni S.W., Matthews R.T., Silberman Y., Winder D.G. Alpha2A-Adrenergic Receptor Activation Decreases Parabrachial Nucleus Excitatory Drive onto BNST CRF Neurons and Reduces Their Activity In Vivo. J. Neurosci. 2019;39:472–484. doi: 10.1523/JNEUROSCI.1035-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mak S.O.K., Zhang L., Chow B.K.C. In vivo actions of SCTR/AT1aR heteromer in controlling Vp expression and release via cFos/cAMP/CREB pathway in magnocellular neurons of PVN. FASEB J. 2019;33:5389–5398. doi: 10.1096/fj.201801732RR. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt K.T., Makhijani V.H., Boyt K.M., Cogan E.S., Pati D., Pina M.M., Bravo I.M., Locke J.L., Jones S.R., Besheer J., et al. Stress-Induced Alterations of Norepinephrine Release in the Bed Nucleus of the Stria Terminalis of Mice. ACS Chem. Neurosci. 2019;10:1908–1914. doi: 10.1021/acschemneuro.8b00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hashimoto K., Parker A., Malone P., Gabelt B.T., Rasmussen C., Kaufman P.S., Hernandez M.R. Long-term activation of c-Fos and c-Jun in optic nerve head astrocytes in experimental ocular hypertension in monkeys and after exposure to elevated pressure in vitro. Brain Res. 2005;1054:103–115. doi: 10.1016/j.brainres.2005.06.050. [DOI] [PubMed] [Google Scholar]
- 29.Prosser R.A., Macdonald E.S., Heller H.C. C-fos mRNA in the suprachiasmatic nuclei in vitro shows a circadian rhythm and responds to a serotonergic agonist. Brain Res. Mol. Brain Res. 1994;25:151–156. doi: 10.1016/0169-328X(94)90292-5. [DOI] [PubMed] [Google Scholar]
- 30.Koya E., Margetts-Smith G., Hope B.T. Daun02 Inactivation of Behaviorally Activated Fos-Expressing Neuronal Ensembles. Curr. Protoc. Neurosci. 2016;76:8–36. doi: 10.1002/cpns.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warren B.L., Mendoza M.P., Cruz F.C., Leao R.M., Caprioli D., Rubio F.J., Whitaker L.R., McPherson K.B., Bossert J.M., Shaham Y., et al. Distinct Fos-Expressing Neuronal Ensembles in the Ventromedial Prefrontal Cortex Mediate Food Reward and Extinction Memories. J. Neurosci. 2016;36:6691–6703. doi: 10.1523/JNEUROSCI.0140-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitaker L.R., Warren B.L., Venniro M., Harte T.C., McPherson K.B., Beidel J., Bossert J.M., Shaham Y., Bonci A., Hope B.T. Bidirectional Modulation of Intrinsic Excitability in Rat Prelimbic Cortex Neuronal Ensembles and Non-Ensembles after Operant Learning. J. Neurosci. 2017;37:8845–8856. doi: 10.1523/JNEUROSCI.3761-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richter F., Bauer A., Perl S., Schulz A., Richter A. Optogenetic augmentation of the hypercholinergic endophenotype in DYT1 knock-in mice induced erratic hyperactive movements but not dystonia. EBioMedicine. 2019;41:649–658. doi: 10.1016/j.ebiom.2019.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moolenaar W.H., Kruijer W., Tilly B.C., Verlaan I., Bierman A.J., de Laat S.W. Growth factor-like action of phosphatidic acid. Nature. 1986;323:171–173. doi: 10.1038/323171a0. [DOI] [PubMed] [Google Scholar]
- 35.Greenberg M.E., Greene L.A., Ziff E.B. Nerve growth factor and epidermal growth factor induce rapid transient changes in proto-oncogene transcription in PC12 cells. J. Biol. Chem. 1985;260:14101–14110. doi: 10.1016/S0021-9258(17)38689-1. [DOI] [PubMed] [Google Scholar]
- 36.Gauthier-Rouviere C., Fernandez A., Lamb N.J. Ras-induced c-fos expression and proliferation in living rat fibroblasts involves C-kinase activation and the serum response element pathway. EMBO J. 1990;9:171–180. doi: 10.1002/j.1460-2075.1990.tb08093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Janknecht R., Cahill M.A., Nordheim A. Signal integration at the c-fos promoter. Carcinogenesis. 1995;16:443–450. doi: 10.1093/carcin/16.3.443. [DOI] [PubMed] [Google Scholar]
- 38.Andre V., Pineau N., Motte J.E., Marescaux C., Nehlig A. Mapping of neuronal networks underlying generalized seizures induced by increasing doses of pentylenetetrazol in the immature and adult rat: A c-Fos immunohistochemical study. Eur. J. Neurosci. 1998;10:2094–2106. doi: 10.1046/j.1460-9568.1998.00223.x. [DOI] [PubMed] [Google Scholar]
- 39.Yang H., Shan W., Zhu F., Yu T., Fan J., Guo A., Li F., Yang X., Wang Q. C-Fos mapping and EEG characteristics of multiple mice brain regions in pentylenetetrazol-induced seizure mice model. Neurol. Res. 2019;41:749–761. doi: 10.1080/01616412.2019.1610839. [DOI] [PubMed] [Google Scholar]
- 40.Krisztin-Peva B., Mihaly A., Toth Z. Differential expression of the c-fos protein and synaptophysin in zebrin II positive and zebrin II negative cerebellar cortical areas in 4-aminopyridine seizures. Acta Neurobiol. Exp. 2019;79:238–250. doi: 10.21307/ane-2019-022. [DOI] [PubMed] [Google Scholar]
- 41.Wallengren C., Li S., Morris M.J., Jupp B., O’Brien T.J. Aggravation of absence seizures by carbamazepine in a genetic rat model does not induce neuronal c-Fos activation. Clin. Neuropharmacol. 2005;28:60–65. doi: 10.1097/01.wnf.0000159955.87511.bc. [DOI] [PubMed] [Google Scholar]
- 42.Kalinina A., Maletta T., Carr J., Lehmann H., Fournier N.M. Spatial exploration induced expression of immediate early genes Fos and Zif268 in adult-born neurons Is reduced after pentylenetetrazole kindling. Brain Res. Bull. 2019;152:74–84. doi: 10.1016/j.brainresbull.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 43.Burnsed J., Skwarzynska D., Wagley P.K., Isbell L., Kapur J. Neuronal Circuit Activity during Neonatal Hypoxic-Ischemic Seizures in Mice. Ann. Neurol. 2019;86:927–938. doi: 10.1002/ana.25601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hall J., Thomas K.L., Everitt B.J. Fear memory retrieval induces CREB phosphorylation and Fos expression within the amygdala. Eur. J. Neurosci. 2001;13:1453–1458. doi: 10.1046/j.0953-816x.2001.01531.x. [DOI] [PubMed] [Google Scholar]
- 45.Vann S.D., Brown M.W., Erichsen J.T., Aggleton J.P. Fos imaging reveals differential patterns of hippocampal and parahippocampal subfield activation in rats in response to different spatial memory tests. J. Neurosci. 2000;20:2711–2718. doi: 10.1523/JNEUROSCI.20-07-02711.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Corbett B.F., You J.C., Zhang X., Pyfer M.S., Tosi U., Iascone D.M., Petrof I., Hazra A., Fu C.H., Stephens G.S., et al. DeltaFosB Regulates Gene Expression and Cognitive Dysfunction in a Mouse Model of Alzheimer’s Disease. Cell Rep. 2017;20:344–355. doi: 10.1016/j.celrep.2017.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Calais J.B., Valvassori S.S., Resende W.R., Feier G., Athie M.C., Ribeiro S., Gattaz W.F., Quevedo J., Ojopi E.B. Long-term decrease in immediate early gene expression after electroconvulsive seizures. J. Neural Transm. 2013;120:259–266. doi: 10.1007/s00702-012-0861-4. [DOI] [PubMed] [Google Scholar]
- 48.Calais J.B., Ojopi E.B., Morya E., Sameshima K., Ribeiro S. Experience-dependent upregulation of multiple plasticity factors in the hippocampus during early REM sleep. Neurobiol. Learn. Mem. 2015;122:19–27. doi: 10.1016/j.nlm.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 49.Nikolaev E., Kaczmarek L., Zhu S.W., Winblad B., Mohammed A.H. Environmental manipulation differentially alters c-Fos expression in amygdaloid nuclei following aversive conditioning. Brain Res. 2002;957:91–98. doi: 10.1016/S0006-8993(02)03606-5. [DOI] [PubMed] [Google Scholar]
- 50.Su Y., Shin J., Zhong C., Wang S., Roychowdhury P., Lim J., Kim D., Ming G.L., Song H. Neuronal activity modifies the chromatin accessibility landscape in the adult brain. Nat. Neurosci. 2017;20:476–483. doi: 10.1038/nn.4494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.West A.E., Greenberg M.E. Neuronal activity-regulated gene transcription in synapse development and cognitive function. Cold Spring Harb. Perspect. Biol. 2011;3:a005744. doi: 10.1101/cshperspect.a005744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cattane N., Minelli A., Milanesi E., Maj C., Bignotti S., Bortolomasi M., Chiavetto L.B., Gennarelli M. Altered gene expression in schizophrenia: Findings from transcriptional signatures in fibroblasts and blood. PLoS ONE. 2015;10:e0116686. doi: 10.1371/journal.pone.0116686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Covington H.E., 3rd, Lobo M.K., Maze I., Vialou V., Hyman J.M., Zaman S., LaPlant Q., Mouzon E., Ghose S., Tamminga C.A., et al. Antidepressant effect of optogenetic stimulation of the medial prefrontal cortex. J. Neurosci. 2010;30:16082–16090. doi: 10.1523/JNEUROSCI.1731-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.MacGibbon G.A., Lawlor P.A., Bravo R., Dragunow M. Clozapine and haloperidol produce a differential pattern of immediate early gene expression in rat caudate-putamen, nucleus accumbens, lateral septum and islands of Calleja. Brain Res. Mol. Brain Res. 1994;23:21–32. doi: 10.1016/0169-328X(94)90207-0. [DOI] [PubMed] [Google Scholar]
- 55.Verma V., Rasmussen K., Dawe G.S. Effects of short-term and chronic olanzapine treatment on immediate early gene protein and tyrosine hydroxylase immunoreactivity in the rat locus coeruleus and medial prefrontal cortex. Neuroscience. 2006;143:573–585. doi: 10.1016/j.neuroscience.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 56.Quezada D.F. Cambios Cognitivos, Expresión de C-Fos y Arborización Dendrítica Después de la Exposición a Ruido Ambiental Crónico en Ratas Macho Adultas. Universidad de Guadalajara; Guadalajara, México: 2020. [Google Scholar]
- 57.Fernández-Quezada D., Luquín S., Ruvalcaba-Delgadillo Y., García-Estrada J., Jauregui-Huerta F. Sex Differences in the Expression of c-fos in a Rat Brain after Exposure to Environmental Noise. Sustainability. 2022;14:2798. doi: 10.3390/su14052798. [DOI] [Google Scholar]
- 58.Ons S., Rotllant D., Marin-Blasco I.J., Armario A. Immediate-early gene response to repeated immobilization: Fos protein and arc mRNA levels appear to be less sensitive than c-fos mRNA to adaptation. Eur. J. Neurosci. 2010;31:2043–2052. doi: 10.1111/j.1460-9568.2010.07242.x. [DOI] [PubMed] [Google Scholar]
- 59.Vialou V., Robison A.J., Laplant Q.C., Covington H.E., 3rd, Dietz D.M., Ohnishi Y.N., Mouzon E., Rush A.J., 3rd, Watts E.L., Wallace D.L., et al. DeltaFosB in brain reward circuits mediates resilience to stress and antidepressant responses. Nat. Neurosci. 2010;13:745–752. doi: 10.1038/nn.2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vialou V., Bagot R.C., Cahill M.E., Ferguson D., Robison A.J., Dietz D.M., Fallon B., Mazei-Robison M., Ku S.M., Harrigan E., et al. Prefrontal cortical circuit for depression- and anxiety-related behaviors mediated by cholecystokinin: Role of DeltaFosB. J. Neurosci. 2014;34:3878–3887. doi: 10.1523/JNEUROSCI.1787-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perrotti L.I., Hadeishi Y., Ulery P.G., Barrot M., Monteggia L., Duman R.S., Nestler E.J. Induction of deltaFosB in reward-related brain structures after chronic stress. J. Neurosci. 2004;24:10594–10602. doi: 10.1523/JNEUROSCI.2542-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Machida M., Lonart G., Sanford L.D. Effects of stressor controllability on transcriptional levels of c-fos, Arc, and brain-derived neurotrophic factor in mouse amygdala and medial prefrontal cortex. Neuroreport. 2018;29:112–117. doi: 10.1097/WNR.0000000000000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abbud R., Lee W.S., Hoffman G., Smith M.S. Lactation inhibits hippocampal and cortical activation of cFos expression by nivida but not kainate receptor agonists. Mol. Cell. Neurosci. 1992;3:244–250. doi: 10.1016/1044-7431(92)90044-3. [DOI] [PubMed] [Google Scholar]
- 64.Wosiski-Kuhn M., Bota M., Snider C.A., Wilson S.P., Venkataraju K.U., Osten P., Stranahan A.M. Hippocampal brain-derived neurotrophic factor determines recruitment of anatomically connected networks after stress in diabetic mice. Hippocampus. 2018;28:900–912. doi: 10.1002/hipo.23018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Houben T., Coomans C.P., Meijer J.H. Regulation of circadian and acute activity levels by the murine suprachiasmatic nuclei. PLoS ONE. 2014;9:e110172. doi: 10.1371/journal.pone.0110172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Caldelas I., Poirel V.J., Sicard B., Pevet P., Challet E. Circadian profile and photic regulation of clock genes in the suprachiasmatic nucleus of a diurnal mammal Arvicanthis ansorgei. Neuroscience. 2003;116:583–591. doi: 10.1016/S0306-4522(02)00654-1. [DOI] [PubMed] [Google Scholar]
- 67.Schwartz M.D., Nunez A.A., Smale L. Rhythmic cFos expression in the ventral subparaventricular zone influences general activity rhythms in the Nile grass rat, Arvicanthis niloticus. Chronobiol. Int. 2009;26:1290–1306. doi: 10.3109/07420520903415742. [DOI] [PubMed] [Google Scholar]
- 68.Langel J., Yan L., Nunez A.A., Smale L. Behavioral Masking and cFos Responses to Light in Day- and Night-Active Grass Rats. J. Biol. Rhythm. 2014;29:192–202. doi: 10.1177/0748730414533289. [DOI] [PubMed] [Google Scholar]
- 69.Shuboni-Mulligan D.D., Cavanaugh B.L., Tonson A., Shapiro E.M., Gall A.J. Functional and anatomical variations in retinorecipient brain areas in Arvicanthis niloticus and Rattus norvegicus: Implications for the circadian and masking systems. Chronobiol. Int. 2019;36:1464–1481. doi: 10.1080/07420528.2019.1651325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schottner K., Vuillez P., Challet E., Pevet P., Weinert D. Light-induced c-Fos expression in the SCN and behavioural phase shifts of Djungarian hamsters with a delayed activity onset. Chronobiol. Int. 2015;32:596–607. doi: 10.3109/07420528.2015.1018422. [DOI] [PubMed] [Google Scholar]
- 71.Zheng W., Niu L., Zhang C., Zhu C., Xie F., Cao C., Li G. Brain edema and protein expression of c-Fos and c-Jun in the brain after diffused brain injury. Int. J. Clin. Exp. Pathol. 2014;7:2809–2817. [PMC free article] [PubMed] [Google Scholar]
- 72.Telford S., Wang S., Redgrave P. Analysis of nociceptive neurones in the rat superior colliculus using c-fos immunohistochemistry. J. Comp. Neurol. 1996;375:601–617. doi: 10.1002/(SICI)1096-9861(19961125)375:4<601::AID-CNE4>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 73.Pinto M., Lima D., Tavares I. Correlation of noxious evoked c-fos expression in areas of the somatosensory system during chronic pain: Involvement of spino-medullary and intra-medullary connections. Neurosci. Lett. 2006;409:100–105. doi: 10.1016/j.neulet.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 74.Sandor K., Kormos V., Botz B., Imreh A., Bolcskei K., Gaszner B., Markovics A., Szolcsanyi J., Shintani N., Hashimoto H., et al. Impaired nocifensive behaviours and mechanical hyperalgesia, but enhanced thermal allodynia in pituitary adenylate cyclase-activating polypeptide deficient mice. Neuropeptides. 2010;44:363–371. doi: 10.1016/j.npep.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 75.Araujo P., Coelho C.A., Oliveira M.G., Tufik S., Andersen M.L. Neonatal Sleep Restriction Increases Nociceptive Sensitivity in Adolescent Mice. Pain Physician. 2018;21:E137–E148. [PubMed] [Google Scholar]
- 76.Flores E.N., Duggan A., Madathany T., Hogan A.K., Márquez F.G., Kumar G., Seal R.P., Edwards R.H., Liberman M.C., García-Añoveros J. A Non-Canonical Pathway from Cochlea to Brain Signals Tissue-Damaging Noise. Curr. Biol. 2015;25:606–612. doi: 10.1016/j.cub.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chan A., Hummel V., Weilbach F.X., Kieseier B.C., Gold R. Phagocytosis of apoptotic inflammatory cells downregulates microglial chemoattractive function and migration of encephalitogenic T cells. J. Neurosci. Res. 2006;84:1217–1224. doi: 10.1002/jnr.21029. [DOI] [PubMed] [Google Scholar]
- 78.Jauregui-Huerta F., Ruvalcaba-Delgadillo Y., Gonzalez-Castañeda R., Garcia-Estrada J., Gonzalez-Perez O., Luquin S. Responses of glial cells to stress and glucocorticoids. Curr. Immunol. Rev. 2010;6:195–204. doi: 10.2174/157339510791823790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sominsky L., De Luca S., Spencer S.J. Microglia: Key players in neurodevelopment and neuronal plasticity. Int. J. Biochem. Cell Biol. 2018;94:56–60. doi: 10.1016/j.biocel.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 80.Palmada M., Centelles J.J. Excitatory amino acid neurotransmission. Pathways for metabolism, storage and reuptake of glutamate in brain. Front. Biosci. 1998;3:d701–d718. doi: 10.2741/a314. [DOI] [PubMed] [Google Scholar]
- 81.Daneman R., Prat A. The blood-brain barrier. Cold Spring Harb. Perspect. Biol. 2015;7:a020412. doi: 10.1101/cshperspect.a020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lim D.A., Alvarez-Buylla A. The Adult Ventricular-Subventricular Zone (V-SVZ) and Olfactory Bulb (OB) Neurogenesis. Cold Spring Harb. Perspect. Biol. 2016;8:a018820. doi: 10.1101/cshperspect.a018820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chong S.Y., Rosenberg S.S., Fancy S.P., Zhao C., Shen Y.A., Hahn A.T., McGee A.W., Xu X., Zheng B., Zhang L.I., et al. Neurite outgrowth inhibitor Nogo-A establishes spatial segregation and extent of oligodendrocyte myelination. Proc. Natl. Acad. Sci. USA. 2012;109:1299–1304. doi: 10.1073/pnas.1113540109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jessen K.R. Glial cells. Int. J. Biochem. Cell Biol. 2004;36:1861–1867. doi: 10.1016/j.biocel.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 85.Hassinger T.D., Atkinson P.B., Strecker G.J., Whalen L.R., Dudek F.E., Kossel A.H., Kater S.B. Evidence for glutamate-mediated activation of hippocampal neurons by glial calcium waves. J. Neurobiol. 1995;28:159–170. doi: 10.1002/neu.480280204. [DOI] [PubMed] [Google Scholar]
- 86.Araque A., Parpura V., Sanzgiri R.P., Haydon P.G. Tripartite synapses: Glia, the unacknowledged partner. Trends Neurosci. 1999;22:208–215. doi: 10.1016/S0166-2236(98)01349-6. [DOI] [PubMed] [Google Scholar]
- 87.Cui W., Allen N.D., Skynner M., Gusterson B., Clark A.J. Inducible ablation of astrocytes shows that these cells are required for neuronal survival in the adult brain. Glia. 2001;34:272–282. doi: 10.1002/glia.1061. [DOI] [PubMed] [Google Scholar]
- 88.McAllister M.S., Krizanac-Bengez L., Macchia F., Naftalin R.J., Pedley K.C., Mayberg M.R., Marroni M., Leaman S., Stanness K.A., Janigro D. Mechanisms of glucose transport at the blood-brain barrier: An in vitro study. Brain Res. 2001;904:20–30. doi: 10.1016/S0006-8993(01)02418-0. [DOI] [PubMed] [Google Scholar]
- 89.Gourine A.V., Kasparov S. Astrocytes as brain interoceptors. Exp. Physiol. 2011;96:411–416. doi: 10.1113/expphysiol.2010.053165. [DOI] [PubMed] [Google Scholar]
- 90.Lois C., Garcia-Verdugo J.M., Alvarez-Buylla A. Chain migration of neuronal precursors. Science. 1996;271:978–981. doi: 10.1126/science.271.5251.978. [DOI] [PubMed] [Google Scholar]
- 91.Kaneko N., Sawada M., Sawamoto K. Mechanisms of neuronal migration in the adult brain. J. Neurochem. 2017;141:835–847. doi: 10.1111/jnc.14002. [DOI] [PubMed] [Google Scholar]
- 92.Walz W. Role of astrocytes in the clearance of excess extracellular potassium. Neurochem. Int. 2000;36:291–300. doi: 10.1016/S0197-0186(99)00137-0. [DOI] [PubMed] [Google Scholar]
- 93.Wilson C.S., Mongin A.A. The signaling role for chloride in the bidirectional communication between neurons and astrocytes. Neurosci. Lett. 2019;689:33–44. doi: 10.1016/j.neulet.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dehouck M.P., Meresse S., Delorme P., Fruchart J.C., Cecchelli R. An easier, reproducible, and mass-production method to study the blood-brain barrier in vitro. J. Neurochem. 1990;54:1798–1801. doi: 10.1111/j.1471-4159.1990.tb01236.x. [DOI] [PubMed] [Google Scholar]
- 95.Doetsch F., Caille I., Lim D.A., Garcia-Verdugo J.M., Alvarez-Buylla A. Subventricular zone astrocytes are neural stem cells in the adult mammalian brain. Cell. 1999;97:703–716. doi: 10.1016/S0092-8674(00)80783-7. [DOI] [PubMed] [Google Scholar]
- 96.Falk S., Götz M. Glial control of neurogenesis. Curr. Opin. Neurobiol. 2017;47:188–195. doi: 10.1016/j.conb.2017.10.025. [DOI] [PubMed] [Google Scholar]
- 97.Czopka T., Ffrench-Constant C., Lyons D.A. Individual oligodendrocytes have only a few hours in which to generate new myelin sheaths in vivo. Dev. Cell. 2013;25:599–609. doi: 10.1016/j.devcel.2013.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Larson V.A., Mironova Y., Vanderpool K.G., Waisman A., Rash J.E., Agarwal A., Bergles D.E. Oligodendrocytes control potassium accumulation in white matter and seizure susceptibility. eLife. 2018;7:e34829. doi: 10.7554/eLife.34829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bloch B., Popovici T., Levin M.J., Tuil D., Kahn A. Transferrin gene expression visualized in oligodendrocytes of the rat brain by using in situ hybridization and immunohistochemistry. Proc. Natl. Acad. Sci. USA. 1985;82:6706–6710. doi: 10.1073/pnas.82.19.6706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.De los Monteros A.E., Peña L.A., de Vellis J. Does transferrin have a special role in the nervous system? J. Neurosci. Res. 1989;24:125–136. doi: 10.1002/jnr.490240202. [DOI] [PubMed] [Google Scholar]
- 101.Baumann N., Pham-Dinh D. Biology of oligodendrocyte and myelin in the mammalian central nervous system. Physiol. Rev. 2001;81:871–927. doi: 10.1152/physrev.2001.81.2.871. [DOI] [PubMed] [Google Scholar]
- 102.Philips T., Rothstein J.D. Oligodendroglia: Metabolic supporters of neurons. J. Clin. Investig. 2017;127:3271–3280. doi: 10.1172/JCI90610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Simons M., Nave K.A. Oligodendrocytes: Myelination and Axonal Support. Cold Spring Harb. Perspect. Biol. 2015;8:a020479. doi: 10.1101/cshperspect.a020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Boda E., Di Maria S., Rosa P., Taylor V., Abbracchio M.P., Buffo A. Early phenotypic asymmetry of sister oligodendrocyte progenitor cells after mitosis and its modulation by aging and extrinsic factors. Glia. 2015;63:271–286. doi: 10.1002/glia.22750. [DOI] [PubMed] [Google Scholar]
- 105.Hesp Z.C., Yoseph R.Y., Suzuki R., Jukkola P., Wilson C., Nishiyama A., McTigue D.M. Proliferating NG2-Cell-Dependent Angiogenesis and Scar Formation Alter Axon Growth and Functional Recovery after Spinal Cord Injury in Mice. J. Neurosci. 2018;38:1366–1382. doi: 10.1523/JNEUROSCI.3953-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhu L., Su Q., Jie X., Liu A., Wang H., He B., Jiang H. NG2 expression in microglial cells affects the expression of neurotrophic and proinflammatory factors by regulating FAK phosphorylation. Sci. Rep. 2016;6:27983. doi: 10.1038/srep27983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liu Y., Aguzzi A. NG2 glia are required for maintaining microglia homeostatic state. Glia. 2020;68:345–355. doi: 10.1002/glia.23721. [DOI] [PubMed] [Google Scholar]
- 108.Raff M.C., Miller R.H., Noble M. A glial progenitor cell that develops in vitro into an astrocyte or an oligodendrocyte depending on culture medium. Nature. 1983;303:390–396. doi: 10.1038/303390a0. [DOI] [PubMed] [Google Scholar]
- 109.Robins S.C., Trudel E., Rotondi O., Liu X., Djogo T., Kryzskaya D., Bourque C.W., Kokoeva M.V. Evidence for NG2-glia derived, adult-born functional neurons in the hypothalamus. PLoS ONE. 2013;8:e78236. doi: 10.1371/journal.pone.0078236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Du X., Zhang Z., Zhou H., Zhou J. Differential Modulators of NG2-Glia Differentiation into Neurons and Glia and Their Crosstalk. Cell. Mol. Neurobiol. 2020;41:1–15. doi: 10.1007/s10571-020-00843-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Morest D.K., Silver J. Precursors of neurons, neuroglia, and ependymal cells in the CNS: What are they? Where are they from? How do they get where they are going? Glia. 2003;43:6–18. doi: 10.1002/glia.10238. [DOI] [PubMed] [Google Scholar]
- 112.Sawamoto K., Wichterle H., Gonzalez-Perez O., Cholfin J.A., Yamada M., Spassky N., Murcia N.S., Garcia-Verdugo J.M., Marin O., Rubenstein J.L., et al. New neurons follow the flow of cerebrospinal fluid in the adult brain. Science. 2006;311:629–632. doi: 10.1126/science.1119133. [DOI] [PubMed] [Google Scholar]
- 113.Spassky N., Merkle F.T., Flames N., Tramontin A.D., Garcia-Verdugo J.M., Alvarez-Buylla A. Adult ependymal cells are postmitotic and are derived from radial glial cells during embryogenesis. J. Neurosci. 2005;25:10–18. doi: 10.1523/JNEUROSCI.1108-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Saijo K., Glass C.K. Microglial cell origin and phenotypes in health and disease. Nat. Rev. Immunol. 2011;11:775–787. doi: 10.1038/nri3086. [DOI] [PubMed] [Google Scholar]
- 115.Cho K., Choi G.E. Microglia: Physiological Functions Revealed through Morphological Profiles. Folia Biol. 2017;63:85–90. doi: 10.14712/fb2017063030085. [DOI] [PubMed] [Google Scholar]
- 116.Zhang L., Zhang J., You Z. Switching of the Microglial Activation Phenotype is a Possible Treatment for Depression Disorder. Front. Cell. Neurosci. 2018;12:306. doi: 10.3389/fncel.2018.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pósfai B., Cserép C., Orsolits B., Dénes Á. New Insights into Microglia-Neuron Interactions: A Neuron’s Perspective. Neuroscience. 2019;405:103–117. doi: 10.1016/j.neuroscience.2018.04.046. [DOI] [PubMed] [Google Scholar]
- 118.Karperien A., Ahammer H., Jelinek H.F. Quantitating the subtleties of microglial morphology with fractal analysis. Front. Cell. Neurosci. 2013;7:3. doi: 10.3389/fncel.2013.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dragunow M., Currie R.W., Robertson H.A., Faull R.L. Heat shock induces c-fos protein-like immunoreactivity in glial cells in adult rat brain. Exp. Neurol. 1989;106:105–109. doi: 10.1016/0014-4886(89)90152-0. [DOI] [PubMed] [Google Scholar]
- 120.Dragunow M., Robertson H.A. Brain injury induces c-fos protein(s) in nerve and glial-like cells in adult mammalian brain. Brain Res. 1988;455:295–299. doi: 10.1016/0006-8993(88)90088-1. [DOI] [PubMed] [Google Scholar]
- 121.Arenander A.T., Lim R.W., Varnum B.C., Cole R., de Vellis J., Herschman H.R. TIS gene expression in cultured rat astrocytes: Multiple pathways of induction by mitogens. J. Neurosci. Res. 1989;23:257–265. doi: 10.1002/jnr.490230303. [DOI] [PubMed] [Google Scholar]
- 122.Arenander A.T., de Vellis J., Herschman H.R. Induction of c-fos and TIS genes in cultured rat astrocytes by neurotransmitters. J. Neurosci. Res. 1989;24:107–114. doi: 10.1002/jnr.490240115. [DOI] [PubMed] [Google Scholar]
- 123.Hisanaga K., Sagar S.M., Hicks K.J., Swanson R.A., Sharp F.R. c-fos proto-oncogene expression in astrocytes associated with differentiation or proliferation but not depolarization. Brain Res. Mol. Brain Res. 1990;8:69–75. doi: 10.1016/0169-328X(90)90011-2. [DOI] [PubMed] [Google Scholar]
- 124.Ladenheim R.G., Lacroix I., Foignant-Chaverot N., Strosberg A.D., Couraud P.O. Endothelins stimulate c-fos and nerve growth factor expression in astrocytes and astrocytoma. J. Neurochem. 1993;60:260–266. doi: 10.1111/j.1471-4159.1993.tb05846.x. [DOI] [PubMed] [Google Scholar]
- 125.Haas C.A., Reddington M., Kreutzberg G.W. Calcitonin Gene-related Peptide Stimulates the Induction of c-fos Gene Expression in Rat Astrocyte Cultures. Eur. J. Neurosci. 1991;3:708–712. doi: 10.1111/j.1460-9568.1991.tb00856.x. [DOI] [PubMed] [Google Scholar]
- 126.Fraczek L.A., Martin C.B., Martin B.K. C-Jun and c-Fos regulate the complement factor H promoter in murine astrocytes. Mol. Immunol. 2011;49:201–210. doi: 10.1016/j.molimm.2011.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Suh H.W., Choi S.S., Lee J.K., Lee H.K., Han E.J., Lee J. Regulation of c-fos and c-jun gene expression by lipopolysaccharide and cytokines in primary cultured astrocytes: Effect of PKA and PKC pathways. Arch. Pharm. Res. 2004;27:396–401. doi: 10.1007/BF02980080. [DOI] [PubMed] [Google Scholar]
- 128.Simi A., Edling Y., Ingelman-Sundberg M., Tindberg N. Activation of c-fos by lipopolysaccharide in glial cells via p38 mitogen-activated protein kinase-dependent activation of serum or cyclic AMP/calcium response element. J. Neurochem. 2005;92:915–924. doi: 10.1111/j.1471-4159.2004.02938.x. [DOI] [PubMed] [Google Scholar]
- 129.Rubio N., Martin-Clemente B. Binding of adenovirus to its receptors in mouse astrocytes induces c-fos proto-oncogene and apoptosis. Virology. 2002;297:211–219. doi: 10.1006/viro.2002.1426. [DOI] [PubMed] [Google Scholar]
- 130.Wu B.Y., Yu A.C. Quercetin inhibits c-fos, heat shock protein, and glial fibrillary acidic protein expression in injured astrocytes. J. Neurosci. Res. 2000;62:730–736. doi: 10.1002/1097-4547(20001201)62:5<730::AID-JNR13>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 131.Yu A.C., Lee Y.L., Fu W.Y., Eng L.F. Gene expression in astrocytes during and after ischemia. Prog. Brain Res. 1995;105:245–253. doi: 10.1016/s0079-6123(08)63301-4. [DOI] [PubMed] [Google Scholar]
- 132.Hung A.C., Huang H.M., Tsay H.J., Lin T.N., Kuo J.S., Sun S.H. ATP-stimulated c-fos and zif268 mRNA expression is inhibited by chemical hypoxia in a rat brain-derived type 2 astrocyte cell line, RBA-2. J. Cell. Biochem. 2000;77:323–332. doi: 10.1002/(SICI)1097-4644(20000501)77:2<323::AID-JCB14>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 133.Pechan P.A., Chowdhury K., Gerdes W., Seifert W. Glutamate induces the growth factors NGF, bFGF, the receptor FGF-R1 and c-fos mRNA expression in rat astrocyte culture. Neurosci. Lett. 1993;153:111–114. doi: 10.1016/0304-3940(93)90089-4. [DOI] [PubMed] [Google Scholar]
- 134.Edling Y., Ingelman-Sundberg M., Simi A. Glutamate activates c-fos in glial cells via a novel mechanism involving the glutamate receptor subtype mGlu5 and the transcriptional repressor DREAM. Glia. 2007;55:328–340. doi: 10.1002/glia.20464. [DOI] [PubMed] [Google Scholar]
- 135.Delaney J., Chiarello R., Villar D., Kandalam U., Castejon A.M., Clark M.A. Regulation of c-fos, c-jun and c-myc gene expression by angiotensin II in primary cultured rat astrocytes: Role of ERK1/2 MAP kinases. Neurochem. Res. 2008;33:545–550. doi: 10.1007/s11064-007-9474-y. [DOI] [PubMed] [Google Scholar]
- 136.Li B., Jia S., Yue T., Yang L., Huang C., Verkhratsky A., Peng L. Biphasic Regulation of Caveolin-1 Gene Expression by Fluoxetine in Astrocytes: Opposite Effects of PI3K/AKT and MAPK/ERK Signaling Pathways on c-fos. Front. Cell. Neurosci. 2017;11:335. doi: 10.3389/fncel.2017.00335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Adamsky A., Kol A., Kreisel T., Doron A., Ozeri-Engelhard N., Melcer T., Refaeli R., Horn H., Regev L., Groysman M., et al. Astrocytic Activation Generates De Novo Neuronal Potentiation and Memory Enhancement. Cell. 2018;174:59–71.e14. doi: 10.1016/j.cell.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 138.Fan F., Li L., Liu W., Yang M., Ma X., Sun H. Astrocytes and neurons in locus coeruleus mediate restraint water immersion stress-induced gastric mucosal damage through the ERK1/2 signaling pathway. Neurosci. Lett. 2018;675:95–102. doi: 10.1016/j.neulet.2018.03.054. [DOI] [PubMed] [Google Scholar]
- 139.Eng L.F., Lee Y.L., Murphy G.M., Yu A.C. A RT-PCR study of gene expression in a mechanical injury model. Prog. Brain Res. 1995;105:219–229. doi: 10.1016/s0079-6123(08)63298-7. [DOI] [PubMed] [Google Scholar]
- 140.Matsunaga W., Osawa S., Miyata S., Kiyohara T. Astrocytic Fos expression in the rat posterior pituitary following LPS administration. Brain Res. 2001;898:215–223. doi: 10.1016/S0006-8993(01)02185-0. [DOI] [PubMed] [Google Scholar]
- 141.Hsieh H.L., Wang H.H., Wu C.Y., Yang C.M. Reactive Oxygen Species-Dependent c-Fos/Activator Protein 1 Induction Upregulates Heme Oxygenase-1 Expression by Bradykinin in Brain Astrocytes. Antioxid. Redox Signal. 2010;13:1829–1844. doi: 10.1089/ars.2009.2957. [DOI] [PubMed] [Google Scholar]
- 142.Morioka N., Suekama K., Zhang F.F., Kajitani N., Hisaoka-Nakashima K., Takebayashi M., Nakata Y. Amitriptyline up-regulates connexin43-gap junction in rat cultured cortical astrocytes via activation of the p38 and c-Fos/AP-1 signalling pathway. Br. J. Pharmacol. 2014;171:2854–2867. doi: 10.1111/bph.12614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yester J.W., Bryan L., Waters M.R., Mierzenski B., Biswas D.D., Gupta A.S., Bhardwaj R., Surace M.J., Eltit J.M., Milstien S., et al. Sphingosine-1-phosphate inhibits IL-1-induced expression of C-C motif ligand 5 via c-Fos-dependent suppression of IFN-beta amplification loop. FASEB J. 2015;29:4853–4865. doi: 10.1096/fj.15-275180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Bhat N.R., Hauser K.F., Kindy M.S. Cell proliferation and protooncogene induction in oligodendroglial progenitors. J. Neurosci. Res. 1992;32:340–349. doi: 10.1002/jnr.490320306. [DOI] [PubMed] [Google Scholar]
- 145.Radhakrishna M., Almazan G. Protein kinases mediate basic fibroblast growth factor’s stimulation of proliferation and c-fos induction in oligodendrocyte progenitors. Brain Res. Mol. Brain Res. 1994;24:118–128. doi: 10.1016/0169-328X(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 146.Prasad A., Teh D.B.L., Blasiak A., Chai C., Wu Y., Gharibani P.M., Yang I.H., Phan T.T., Lim K.L., Yang H., et al. Static Magnetic Field Stimulation Enhances Oligodendrocyte Differentiation and Secretion of Neurotrophic Factors. Sci. Rep. 2017;7:6743. doi: 10.1038/s41598-017-06331-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liu H.N., Almazan G. Glutamate induces c-fos proto-oncogene expression and inhibits proliferation in oligodendrocyte progenitors: Receptor characterization. Eur. J. Neurosci. 1995;7:2355–2363. doi: 10.1111/j.1460-9568.1995.tb01032.x. [DOI] [PubMed] [Google Scholar]
- 148.Cohen R.I., Molina-Holgado E., Almazan G. Carbachol stimulates c-fos expression and proliferation in oligodendrocyte progenitors. Brain Res. Mol. Brain Res. 1996;43:193–201. doi: 10.1016/S0169-328X(96)00176-3. [DOI] [PubMed] [Google Scholar]
- 149.Khorchid A., Larocca J.N., Almazan G. Characterization of the signal transduction pathways mediating noradrenaline-stimulated MAPK activation and c-fos expression in oligodendrocyte progenitors. J. Neurosci. Res. 1999;58:765–778. doi: 10.1002/(SICI)1097-4547(19991215)58:6<765::AID-JNR4>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 150.Goldenberg-Cohen N., Guo Y., Margolis F., Cohen Y., Miller N.R., Bernstein S.L. Oligodendrocyte dysfunction after induction of experimental anterior optic nerve ischemia. Investig. Ophthalmol. Vis. Sci. 2005;46:2716–2725. doi: 10.1167/iovs.04-0547. [DOI] [PubMed] [Google Scholar]
- 151.Reissig C.J., Rabin R.A., Winter J.C., Dlugos C.A. D-LSD-induced c-Fos expression occurs in a population of oligodendrocytes in rat prefrontal cortex. Eur. J. Pharmacol. 2008;583:40–47. doi: 10.1016/j.ejphar.2007.12.031. [DOI] [PubMed] [Google Scholar]
- 152.Bichenkov E., Ellingson J.S. Ethanol alters the expressions of c-Fos and myelin basic protein in differentiating oligodendrocytes. Alcohol. 2009;43:627–634. doi: 10.1016/j.alcohol.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 153.Eun S.Y., Hong Y.H., Kim E.H., Jeon H., Suh Y.H., Lee J.E., Jo C., Jo S.A., Kim J. Glutamate receptor-mediated regulation of c-fos expression in cultured microglia. Biochem. Biophys. Res. Commun. 2004;325:320–327. doi: 10.1016/j.bbrc.2004.10.035. [DOI] [PubMed] [Google Scholar]
- 154.Sun Z., Du M., Lu Y., Zeng C.Q. Effects of triptolide on the expression of MHC II in microglia in kainic acidinduced epilepsy. Mol. Med. Rep. 2018;17:8357–8362. doi: 10.3892/mmr.2018.8891. [DOI] [PubMed] [Google Scholar]
- 155.Li H., Zhang X., Chen M., Chen J., Gao T., Yao S. Dexmedetomidine inhibits inflammation in microglia cells under stimulation of LPS and ATP by c-Fos/NLRP3/caspase-1 cascades. EXCLI J. 2018;17:302–311. doi: 10.17179/excli2017-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rigillo G., Vilella A., Benatti C., Schaeffer L., Brunello N., Blom J.M.C., Zoli M., Tascedda F. LPS-induced histone H3 phospho(Ser10)-acetylation(Lys14) regulates neuronal and microglial neuroinflammatory response. Brain Behav. Immun. 2018;74:277–290. doi: 10.1016/j.bbi.2018.09.019. [DOI] [PubMed] [Google Scholar]
- 157.Sun Y., Zheng J., Xu Y., Zhang X. Paraquat-induced inflammatory response of microglia through HSP60/TLR4 signaling. Hum. Exp. Toxicol. 2018;37:1161–1168. doi: 10.1177/0960327118758152. [DOI] [PubMed] [Google Scholar]