Abstract
The Russia-Ukraine crisis has been at the center of international talks since early 2022. This conflict, bursting after the sanitary crisis of the covid 19 pandemic, creates an atmosphere of uncertainty and instability, which negatively impacts many aspects, including mental health. Young Ukrainians have been suffering from socio-political instability for decades, and the current war, together with the Covid 19 pandemic, shatters hopes of brighter days. This commentary covers the challenges facing the younger generation in Ukraine and the impact of this situation on their mental health.
Keywords: Mental health, Ukraine-Russia, COVID-19, Conflict, Russia-Ukraine
1. Introduction
The Russian-Ukrainian conflict started in February 2014 following the Ukrainian Revolution of Dignity which focused on Crimea and parts of the Donbas. The Russians have succeeded in annexing Crimea, but the fight in Donbas is still ongoing. By the end of 2021, thousands of Russian personnel and military equipment started massing on Russia–Ukraine border. The conflict escalated when the Russian president decided to start a large-scale invasion of Ukraine on February 24, 2022. Throughout history, Armed conflicts have had catastrophic impacts on the well-being of nations [25]. Among these effects are long-term physical and psychological harm to children and adults. There are a lot of studies of the general population that show an increase in mental problems' incidence and prevalence due to wars. Women and children are the most vulnerable groups [1]. Research s also shown that such tough experiences could lead to severe consequences, including PTSD, depression and anxiety [2]. The Russian-Ukrainian crisis seems to play a magnifying effect with the pandemic on the health of Ukrainians, especially mental [25]. Knowing that the health care system in Ukraine was substantial but somehow fragile. And in the middle of the ongoing COVID-19 pandemic, which has already put health systems and health care workers under enormous pressure, such attacks have the potential to be even more catastrophic for Ukraine. An estimated 157 attacks on health care facilities were recorded by SURVEILLANCE SYSTEM FOR ATTACKS ON HEALTH CARE (SSA) by the end of April 2022. According to the world health organization (WHO), the attacks on vital health infrastructure prevent many from having access to health services despite the urgent needs. As of now, over 5 million Ukrainians have fled their homes, cities, and jobs for safety in Poland and other European countries. Pictures show Ukrainian young huddled together on benches, fear in their eyes and a billion thoughts in their heads, looking at their parent's faces who are constantly wishing the next missile doesn't hit their child. The effect of this trauma is not limited to people who experienced it, but also it can be transferred from parents to their future children via subtle but heritable shifts to the genome [3]. The aim of this commentary is to highlight the harsh impacts of the Russian-Ukrainian conflict on the young population of Ukraine and urge mental health advocates to take serious and immediate actions to buffer these effects (see Fig. 1, Fig. 2).
Fig. 1.
Ukraine – Russia Crisis and its impacts on the mental health of Ukrainian young people during the COVID-19 Pandemic [11,12,16,17].
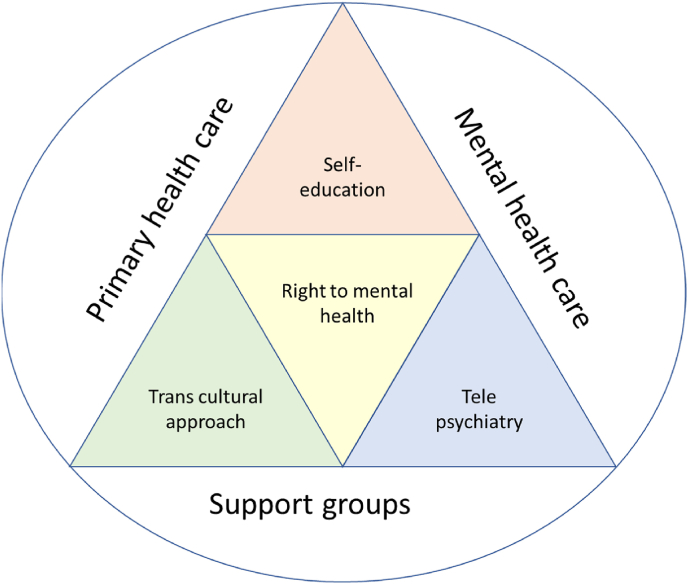
Fig. 2.
Model representing strategies to improve mental health during the Ukraine-Russia crisis [[14], [15], [16], [17]].
2. Challenges facing young people in Ukraine – Russia crisis during COVID-19
The Russian invasion had drastic negative effects on the Ukrainian health system. The health care system of Ukraine is functioning at a reduced capacity [4]. On the one hand, the continuous attacks of Russian forces on Ukrainian hospitals and other health facilities increased the prevalence of diseases [4]. On the other hand, the reduced supply of food and water threatens the vital infrastructure. Moreover, more than 4 million people had to flee Ukraine as of today, including health professionals [5], these people were left in need of shelter to escape the vicious attacks. Therefore, they were forced to live in overcrowded areas which lack hygiene and health measurements. This eventually usher to strike in COVID-19 cases, to mean that those situations cause an increase in the number of COVID-19 cases. Also, the country's concern shifted to the war leading to shortage in health products. This adds to the critality of Ukraine's health system. Many believe that the impacts of Covid-19 were felt more deeply in resource-limited countries that suffer from less established health-care systems [6,[18], [19], [20], [21], [22], [23], [24]]. This is becoming the case in Ukraine.
Nowadays, the prevention of Covid-19 relies on social distancing, hygiene, isolation and quarantine, and the fact that none of these measures can be achieved because of the ongoing war, the rate of people at higher risk for serious complications of Covid-19 is increasing dramatically leading to high rates of illness and death cases. The current vaccination rate in Ukraine is less than 40% [7]. This means that the rest 60% of the population, are susceptible to developing serious complications if infected. Therefore, Ukraine is struggling with the covid pandemic more than ever. Moreover, in Ukraine a polio outbreak started in October 2021 due to the low immunization rates among the population [8]. A catch-up immunization campaign was started on February 1, 2022. However, it was cut short because of the invasion that started shortly after on the 24th of February. Hence, the campaign could not reach its target. Shortly before the beginning of the invasion on Feb 10th, Ukraine reported their highest daily corona cases, where it reached 37,000 cases. More than a million cases out of the 5 million cases were reported in 2022 alone. Thus, the war started simultaneously as COVID cases were striking an all-time high. Nowadays, it's not clear how many COVID cases and deaths are there in Ukraine since they were forced to slowly cut collecting data until it stopped completely. This further illustrates the condemning situation over there, COVID cases are ignored, causing more death and health issues [9].
Considering the situation, the challenges facing young people in Ukraine during the Ukraine-Russia crisis are increasing because of the current Covid-19 pandemic. Armament of young men puts them in riskier and unhealthy areas. Even if their immune systems are strong, their collective action poses them a threat. Young women are living in overcrowded shelters. Young people are more vulnerable when fleeing because of the disruption of protective social networks and the loss of access to healthcare [10]. Due to reduced access to health services and supplies, reduced immunization and testing rates threaten public health for infectious disease and non-communicable diseases.
3. Impacts of Ukraine – Russia crisis on mental health of Ukrainian young people
Ukraine has been in a war with Russia since 2014, and this continued conflict has led to a variant mental health crisis among Ukrainian young people. Although the Ukraine-Russia crisis has received enormous attention from all over the world, the resulting mental health crisis among young Ukrainian people wasn't given special consideration. Several studies have shown an increased level of psychological problems, such as Post-traumatic stress disorders (PTSD), depression and anxiety disorders. During the war, Ukrainian young people have suffered from exposure to abuse and violence and the loss of their closest friends and family members. This results in severe amounts of psychological trauma [11,12].
The World health organization (WHO) mental health surveys stated that the recovery from Post-traumatic stress disorder (PTSD) during the war is slow, meaning that the mental health problems among Ukrainian youth could last for a long time, and it needs time and effort to be solved. Although, the recent Ukraine-Russia crisis represents a very severe escalation in fighting. The cumulative impact of war on mental health and displacement will predispose Ukrainian young people to more significant mental health outcomes [13].
The United Nations Children's Fund (UNICEF), together with the Ministry of Education and Science of Ukraine, the Ukrainian Institute of Cognitive Behavioral Therapy and the ALL-Ukrainian Public Center have launched a project called (PROUCH) which is mental health support group targeting the negatively impacted youth & parents by the war in Ukraine. The project offers free physical and online zoom sessions under the supervision of professional psychologists and specialists about how to deal with psychological challenges during wars and national conflicts. Participants have the opportunity to share their fears, anxious thoughts and worries about war, and they also learn how to heal themselves, their family and friends. Therefore, they learn how to adapt to living in war situations and how to plan their lives accordingly [13].
4. Recommendations
-
1)
Educate about self-recognition of symptoms of mental health disorders and overcome the social and linguistic barriers to access mental health services. This can be done through various approaches, including-evidence-based virtual self-help interventions involving coping techniques like cognitive-behavioural therapy [14,27]; and enhancing awareness through person-centered and community-driven strategies tailored to the pandemic and war-related concerns.
-
2)
Ensure provision of services for the wellbeing and augment safe, socially acceptable basic services to protect the dignity of people with the help of local support groups, non-governmental agencies, international coordination, and collaborative mechanisms 15. Priority should be given to providing quality and continuity of care to the populations with pre-existing mental health conditions, chronic diseases, financially unstable groups, and those with limited access to health care.
-
3)
Strengthen the capacity to ensure screening for mental health diseases at emergency care visits and primary care health facilities [26,27]– Expand the diversification and training of the mental health workforce across sectors and utilize transcultural approaches to enhance the assessment and provide high-quality health care to the refugees and immigrant populations [16]. Focus on providing psychological first aid and personalized care to vulnerable populations and increasing the workforce to prevent major complications and suicidal tendencies.
-
4)
Enhance the capacity to provide specialized services by mental health professionals beyond the scope of support groups and primary care providers in an appropriate, accurate timely manner. Rising levels of stress and emotional trauma overwhelm and create an enormous burden on mental health professionals and would need strong support from colleagues from other parts of the world to treat and rehabilitate war victims.
-
5)
Nonetheless, utilize the growing telepsychiatry to fill the voids created in the health care by the pandemic and war. Remote services play a crucial role in crisis triage and alleviate the pressure on overburdened health systems in war conflicts [17].
Considering all, the Right to mental health should not be neglected at any cost and it should become an utmost priority as not only the acute psychological trauma is a threat amidst the war and pandemic but can also have long term consequences on the overall health of people. Psychosocial services and support should be expanded and improved as mental health problems affect at an individual level and lead to drastic negative impacts on the younger generations.
5. Conclusion
The cumulative effect of the Covid 19 pandemic and the Russian invasion of Ukraine resulted in a surge of mental health disorders – including anxiety, PTSD, depression, reduction in mental healthcare-seeking behavior, substance use disorders, and disruptive behavioral and impulse disorders. Often, mental health is overlooked in Ukraine due to the social stigma and taboos, yet more during the state of war and pandemics.
This highlights the need to ramp up vital assistance to proactive and preventive care for the new mental health needs and interventions to improve access to care for existing and rising mental health conditions.
Please state any sources of funding for your research
None.
Ethical approval
Not Applicable.
Funding
We have not received any financial support for this manuscript.
Author contribution
Olivier Uwishema: Conceptualization, Project administration, Writing-review, and Designing. Manuscript writing: All authors. Olivier Uwishema: Reviewed and edited the first draft. Collection and assembly of data: All authors. Olivier Uwishema: Reviewed and edited the second draft. Helen Onyeaka, PhD: Reviewed and edited the final draft. Figure 1. was drawn and analyzed by authors Olivier Uwishema1,7,8* and Vimala Devi Thambi1,3. Figure 2. was drawn and analyzed by authors Olivier Uwishema1,7,8* and Vimala Devi Thambi [1,3]
Please state any conflicts of interest
No conflicts of interest declared.
Consent
Not Applicable.
Registration of research studies
-
1.
Name of the registry: Not Applicable
-
2.
Unique Identifying number or registration ID: Not Applicable
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Not Applicable
Guarantor
Not Applicable.
Not Applicable.
Financial support
None.
Data availability statement
Not Applicable.
Acknowledgement
None.
Contributor Information
Celine Chaaya, Email: celine.chaya@hotmail.com.
Vimala Devi Thambi, Email: vimala.vims123@gmail.com.
Özge Sabuncu, Email: ozgesabuncuuu@gmail.com.
Reem Abedi, Email: reemabedi@live.com.
Awab Osman Ahmed Osman, Email: awabosman55@gmail.com.
Olivier Uwishema, Email: uwolivier1@ktu.edu.tr.
Helen Onyeaka, Email: h.onyeaka@bham.ac.uk.
References
- 1.Abu Suhaiban H., Grasser L.R., Javanbakht A. Mental health of refugees and torture survivors: a critical review of prevalence, predictors, and integrated care. Int. J. Environ. Res. Publ. Health. 2019;16(13) doi: 10.3390/ijerph16132309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hynes H. On the battlefield of women's bodies: an overview of the harm of war to women. Womens Studies Int. Forum - Women stud int forum. 2004;27:431–445. doi: 10.1016/j.wsif.2004.09.001. [DOI] [Google Scholar]
- 3.Yehuda R., Lehrner A. Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World Psychiatr. 2018;17(3):243–257. doi: 10.1002/wps.20568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mossialos E., Zaliska O., Oleshchuk O., Forman R. Health impacts of the Russian invasion in Ukraine: need for global health action. Lancet. 2022;399(10334):3. doi: 10.1016/S0140-6736(22)00615-8. [DOI] [PubMed] [Google Scholar]
- 5.Situation Ukraine Refugee Situation. (n.d.). UNHCR data portal. Retrieved April 17, 2022, from https://data2.unhcr.org/en/situations/ukraine.
- 6.Uwishema O., Taylor C., Lawal L., Hamiidah N., Robert I., Nasir A., Chalhoub E., Sun J., Akin B.T., Adanur I., Mwazighe R.M., Onyeaka H. The syndemic burden of HIV/AIDS in Africa amidst the COVID‐19 pandemic. Immun. Inflamm. Dis. 2021;10(1):26–32. doi: 10.1002/iid3.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ukraine: the latest coronavirus counts, charts and maps. (n.d.). Reuters Graphics. Retrieved April 17, 2022, from https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/ukraine/.
- 8.McKee M., Murphy A. Russia invades Ukraine again: how can the health community respond? Br. Med. J. 2022;376(8329):2. doi: 10.1136/bmj.o548. https://www.bmj.com/content/376/bmj.o548.full [DOI] [PubMed] [Google Scholar]
- 9.Head M. Ukraine: disease control is a casualty of war – so a surge in COVID cases is likely. The Conversation. 2022, March 18 https://theconversation.com/amp/ukraine-disease-control-is-a-casualty-of-war-so-a-surge-in-covid-cases-is-likely-179218 Retrieved April 17, 2022, from. [Google Scholar]
- 10.Lee, A. (n.d.). Ukraine: war has an impact on people's health beyond bullets and bombs. The Conversation. Retrieved April 17, 2022, from https://theconversation.com/ukraine-war-has-an-impact-on-peoples-health-beyond-bullets-and-bombs-178062.
- 11.Cai H., Bai W., Zheng Y., Zhang L., Cheung T., Su Z., Jackson T., Xiang Y.T. International collaboration for addressing the mental health crisis among child and adolescent refugees during the Russia-Ukraine war. Asian J. Psychiatr. 2022 Apr 8;72 doi: 10.1016/j.ajp.2022.103109. Epub ahead of print. PMID: 35427933. [DOI] [PubMed] [Google Scholar]
- 12.Bryant R.A., Schnurr P.P., Pedlar D. 5-Eyes Mental Health Research and Innovation Collaboration in military and veteran mental health. Addressing the mental health needs of civilian combatants in Ukraine. Lancet Psychiatr. 2022 May;9(5):346–347. doi: 10.1016/S2215-0366(22)00097-9. https://reliefweb.int/report/ukraine/mental-health-lifeline-launches-families-ukraine-enuk Epub 2022 Mar 16. PMID: 35305300. [DOI] [PubMed] [Google Scholar]
- 13.Heckendorf H., Lehr D., Boß L. Effectiveness of an internet-based self-help intervention versus public mental health advice to reduce worry during the COVID-19 pandemic: a Pragmatic, parallel-group, randomized controlled trial. Psychother. Psychosom. 2022, January 20 doi: 10.1159/000521302. https://www.karger.com/Article/Abstract/521302 Retrieved April 29, 2022, from. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . 1970, January 1. Ukraine Crisis. Public Health Situation Analysis: Refugee-Hosting Countries.https://apps.who.int/iris/handle/10665/352494 17 March 2022. World Health Organization. Retrieved. from. [Google Scholar]
- 15.Wylie L., Van Meyel R., Harder H., Sukhera J., Luc C., Ganjavi H., Elfakhani M., Wardrop N. Assessing trauma in a transcultural context: challenges in mental health care with immigrants and refugees. Publ. Health Rev. 2018;39(1) doi: 10.1186/s40985-018-0102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gordon D. Amid Russian invasion, new initiative launches free telemedicine for Ukrainians under siege. Forbes. 2022, March 21 https://www.forbes.com/sites/debgordon/2022/03/21/amid-russian-invasion-new-initiative-launches-free-telemedicine-for-ukrainians-under-siege/?sh=2bb5e8304470 Retrieved April 29, 2022, from. [Google Scholar]
- 17.Ingabire C.M., Richters A. Suicidal ideation and behavior among Congolese refugees in Rwanda: contributing factors, consequences, and support mechanisms in the context of culture. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uwishema O., Onyeaka H., Alshareif B.A.A., Omer M.E.A., Sablay A.L.R., Tariq R., et al. Current context of pneumonia amidst the COVID-19 pandemic in Africa. J. Contemp. Stud. Epidemiol. Public Health. 2021;2(2) doi: 10.30935/jconseph/11281. [DOI] [Google Scholar]
- 19.Uwishema O., Nnagha E.M., Chalhoub E., Nchasi G., Mwazighe R.M., Akin B.T., Adanur I., Onyeaka H. Dengue fever outbreak in Cook Island: a rising concern, efforts, challenges, and future recommendations. J. Med. Virol. 2021;93(11):6073–6076. doi: 10.1002/jmv.27223. [DOI] [PubMed] [Google Scholar]
- 20.Sun J., Uwishema O., Kassem H., Abbass M., Uweis L., Rai A., El Saleh R., Adanur I., Onyeaka H. Ebola virus outbreak returns to the Democratic Republic of Congo: an urgent rising concern. Ann. Med. Surg. 2022 doi: 10.1016/j.amsu.2022.103958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uwishema O., Okereke M., Onyeaka H., Hasan M.M., Donatus D., Martin Z., Oluwatomisin L.A., Mhanna M., Olumide A.O., Sun J., Adanur I. Threats and outbreaks of cholera in Africa amidst COVID-19 pandemic: a double burden on Africa's health systems. Trop. Med. Health. 2021;49(1):93. doi: 10.1186/s41182-021-00376-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uwishema O., Chalhoub E., Torbati T., David S.C., Khoury C., Ribeiro L., Nasrallah Y., Bekele B.K., Onyeaka H. Rift Valley fever during the COVID-19 pandemic in Africa: a double burden for Africa's healthcare system. Health Sci. Rep. 2022;5(1):e468. doi: 10.1002/hsr2.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uwishema O., Badri R., Onyeaka H., Okereke M., Akhtar S., Mhanna M., Zafar B., Zahabioun A., Said K.A., Tovani-Palone M.R. 1–12. Advance online publication; 2022. (Fighting Tuberculosis in Africa: the Current Situation amidst the COVID-19 Pandemic. Disaster Medicine and Public Health Preparedness). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uwishema O., Chalhoub E., Zahabioun A., David S.C., Khoury C., Al-Saraireh T.H., Bekele B.K., Mwazighe R.M., Onyeaka H. The rising incidence of African swine fever during the COVID-19 pandemic in Africa: efforts, challenges and recommendations. Int. J. Health Plann. Manag. 2022;37(1):561–567. doi: 10.1002/hpm.3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uwishema O., Sujanamulk B., Abbass M., Fawaz R., Javed A., Aboudib K., Mahmoud A., Oluyemisi A., Onyeaka H. Russia-Ukraine conflict and COVID-19: a double burden for Ukraine's healthcare system and a concern for global citizens. Postgrad. Med. 2022 doi: 10.1136/postgradmedj-2022-141895. postgradmedj-2022-141895. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uwishema, O., Ayoub, G., Badri, R., Onyeaka, H., Berjaoui, C., Karabulut, E., Anis, H., Sammour, C., Mohammed Yagoub, F., & Chalhoub, E. (2022). Neurological disorders in HIV: Hope despite challenges. Immun. Inflamm. Dis., 10(3), e591. 10.1002/iid3.591. [DOI] [PMC free article] [PubMed]
- 27.Uwishema O., Onyeaka H., Badri R., Yücel A.N., Korkusuz A.K., Ajagbe A.O., Abuleil A., Chaaya C., Alhendawi B., Chalhoub E. The understanding of Parkinson's disease through genetics and new therapies. Brain Behavior. 2022;12(5) doi: 10.1002/brb3.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not Applicable.