Abstract
The COVID-19 pandemic has disproportionately affected pregnant people by increasing health risks of maternal morbidity and mortality, stillbirth, and preterm birth. Although numerous studies have supported the safety and efficacy of COVID-19 vaccination in pregnancy in preventing or mitigating the risk for these adverse outcomes, many pregnant people remain hesitant. Approximately half of US adults regularly consume news from social media platforms, which are a fertile ground for the spread of vaccine disinformation. The lack of information regarding COVID-19 vaccine safety early in the pandemic fueled vaccine myths targeting the fears of pregnant people about vaccination risks. Saddened by the spike in maternal deaths of unvaccinated individuals during the COVID-19 Delta variant surge in the fall of 2021, we created a social media campaign to promote scientific communication regarding the risks of COVID-19 disease in pregnancy and the benefits of vaccination. We called the campaign “One Vax Two Lives,” which refers to the ability of 1 maternal vaccine to benefit the health and lives of both the pregnant individual and their fetus. We present a blueprint of how we leveraged a large, interdisciplinary student workforce to create a social media campaign and research program studying vaccine hesitancy, which can be replicated by other groups. Community engagement and partnerships with key stakeholders, such as the Washington State Department of Health, were essential for amplifying the campaign and providing our team with feedback on content and approach. We present the analytics of our social media advertisements, web articles, and video content that helped inform the iterative design process of the multimedia content. Moving forward, we are launching collaborative research programs to study vaccine hesitancy and inform the development of new social media content designed for pregnant individuals who are: (1) Spanish-speaking Hispanic/Latina/x, (2) Black or Afro-Latinx, and (3) residents of rural communities in the State of Washington. Data from these mixed methods studies will inform new communication campaigns to reach vaccine-hesitant individuals. Finally, we discuss lessons learned and how the most impactful elements of the campaign can be translated to related areas of maternal public health.
Key words: communication, coronavirus, COVID-19, pregnancy, SARS-CoV-2, social media, vaccine hesitancy
Introduction
Although pregnant people tend to be young and healthy, they are a highly vulnerable group to COVID-19 and experience more severe illness and higher rates of maternal death, preterm birth, and stillbirth.1, 2, 3, 4, 5, 6, 7 Maternal mortality during the COVID-19 Delta variant surge spanning July through October 2021 was particularly significant and starkest in undervaccinated states. In Mississippi, there were 9 COVID-19–associated maternal deaths (25 deaths/1000 SARS-CoV-2 infections; 2.5% maternal mortality rate) and a 4-fold increased rate of stillbirths during the Delta variant surge.5 , 8 None of these deaths occurred in fully vaccinated women, and only 1 person was partially vaccinated. At the University of Alabama, 39 pregnant patients were hospitalized with COVID-19 in just the first 18 days of August 2021 (Delta surge); 11 of these required intensive care.9 Sadly, these hospitalizations and maternal deaths came approximately 3 months after all pregnant individuals in the United States became eligible for COVID-19 vaccination, as tiered access to COVID-19 vaccination was lifted for all adults on April 20, 2021. Many states,10, 11, 12, 13 including Mississippi,14 had prioritized pregnant people as a vulnerable group to COVID-19 and offered earlier access to vaccination for several months before April of 2021. However, by the start of the Delta variant surge in July of 2021, only 21.8% of pregnant individuals in the United States were estimated to have been vaccinated with ≥1 COVID-19 vaccines.15
Several factors were identified as contributing to the low and lagging COVID-19 vaccination rates in US pregnant people. Exclusion of pregnant individuals from COVID-19 vaccine trials led to an early perception that COVID-19 vaccines were not safe in pregnancy.16 Public health messaging to pregnant people regarding COVID-19 vaccination was at times confusing and insufficient.16 Furthermore, social media became a pernicious vehicle for spreading misinformation about COVID-19 vaccination in pregnancy, which was fueled by the lack of early information on vaccine safety.17 , 18 For example, a frequently cited pseudoscientific narrative linked a genetic sequence in the placenta with the SARS-CoV-2 viral genome and suggested that COVID-19 vaccination might induce infertility.17 This was rejected by the scientific community,19 but not before it gained traction on social media and bolstered vaccine hesitancy in pregnant communities. By October of 2021, nearly one-third of 1519 US adults surveyed by the KFF (formerly the Kaiser Family Foundation) reported that they heard that COVID-19 vaccines caused infertility and either believed the myth was true or were uncertain.17 In fact, a systematic review of vaccine uptake in US states identified pregnant and breastfeeding women as one of the most COVID-19 vaccine-hesitant groups.20
Saddened and galvanized by the surge in deaths of unvaccinated pregnant women during the SARS-CoV-2 Delta variant wave,8 we created a diverse, interdisciplinary team at the University of Washington to link our synergistic expertise in pregnancy infections, vaccination, health communication, and social media and digital communication. Our first objective was to promote scientifically accurate and evidence-based information about COVID-19 vaccination in pregnancy and while breastfeeding through a social media campaign to combat mis- and disinformation. We called our campaign “One Vax Two Lives” to indicate that a vaccine received in pregnancy can benefit both the pregnant individual and their fetus. By the summer of 2021 and into early 2022, there was substantial and accumulating scientific evidence supporting the safety of COVID-19 vaccination in pregnancy.15 , 21, 22, 23, 24 These studies and others provided the scientific basis for our communication campaign that we piloted in the State of Washington using multiple social media platforms, including Facebook, Instagram, Twitter, and TikTok.
We present our results and lessons learned throughout our social media campaign to provide a template for other groups or organizations to promote health and scientific communication. Ideally, we would have begun by doing market research on our audience, their trusted messengers for health information, vaccine misinformation narratives, and how they receive their health news. Instead, our approach was driven by the urgency of the COVID-19 pandemic and the need to rapidly inform pregnant people on the risks of becoming infected and the benefits of the COVID-19 vaccine. We initially relied on our expertise with obstetrical populations to design social media test advertisements and revised our approach iteratively on the basis of analytics obtained from user interactions with our content. Our results and insights may be valuable for other public health communication campaigns to motivate social and behavioral change in pregnant people.
Vaccine decision-making and hesitancy
Vaccine hesitancy is defined by the World Health Organization as “the reluctance or refusal to vaccinate despite the availability of vaccines.”25 Social media has provided vaccine-hesitant individuals and groups with fertile ground for antivaccination messages, which make up a large proportion of all vaccine content on social media.17 , 26, 27, 28, 29 The content on social media platforms is typically not moderated, which can allow dangerous and frightening myths to perpetuate and spread virally. For example, in early 2021, a vaccine myth spread virally on social media platforms that being near a vaccinated person could cause fertility issues or disruption to menstrual cycles.30 This claim was not true but targeted the fears of young and pregnant individuals. Because pregnant and lactating individuals had not been included in early vaccine trials,31 there was a scientific “data void” regarding the impact of COVID-19 vaccination on reproductive health that allowed antivaccine myths and disinformation to spread virally.31 , 32
Despite more than 1 year of readily available public health information about COVID-19 vaccination and scientific studies supporting safety in pregnancy, a high percentage of women remain uncertain about false vaccine narratives regarding COVID-19 vaccination in pregnancy. A nationally representative survey of 615 women (aged 18–49 years) conducted in May of 2022 in English and Spanish revealed that 7 in 10 women who are pregnant or planning to become pregnant either believe or are unsure about at least 1 of 3 false statements about pregnancy and the COVID-19 vaccines.33 Even among groups expressing high levels of vaccine confidence regarding the safety for adults (Democrats and vaccinated adults), less than half expressed that they are “very confident” that the vaccine is safe in pregnancy. Overcoming vaccine hesitancy in pregnant patients remains a formidable public health challenge.
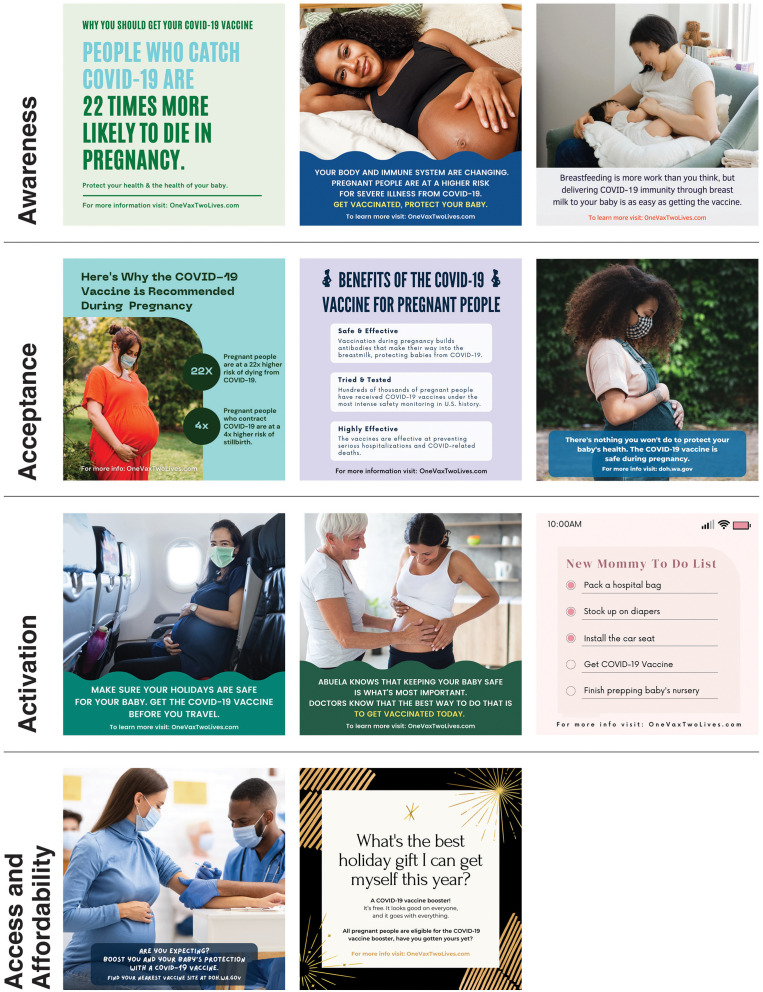
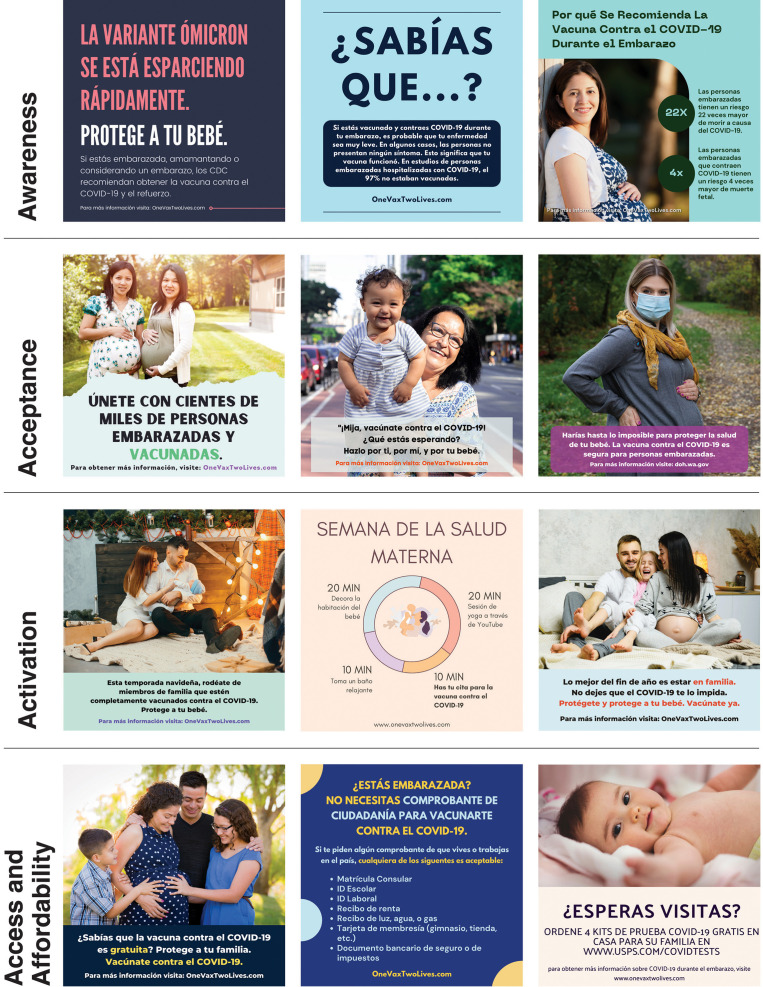
Many models have been proposed to describe the dimensions of vaccine uptake, including a Strategic Advisory Group of Experts working group (3C model),34 a 4C model (extended 3C model),35 and a “5-A” model.36 Although these models are nuanced to achieve slightly different objectives, we addressed the 5-A model tenets of vaccine uptake—access, affordability, awareness, acceptance, and activation—using social media. The One Vax Two Lives campaign targeted these dimensions of vaccine uptake with emphasis on: (1) “awareness” of the risks of COVID-19 in pregnancy, (2) vaccine “acceptance” by providing scientifically accurate information and dispelling misinformation, and (3) “activation” by using social media to remind and encourage the user to receive vaccination (Figures 1 and 2 ). The tenets of “access” and “affordability” were highlighted in test advertisements to inform users that COVID-19 vaccination appointments did not require proof of citizenship or employment and were free regardless of insurance status (Figure 2).
Figure 1.
Social media advertisement posts in English in categories of vaccine acceptance
On the left, categories of vaccine acceptance are shown with examples in the same row of social media advertisements (English) in each category.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Figure 2.
Social media advertisement posts in Spanish in categories of vaccine acceptance
On the left, categories of vaccine acceptance are shown with examples in the same row of social media advertisements (Spanish) in each category.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Of the 5-A model tenets, vaccine acceptance typically poses the greatest challenge because it often requires overcoming multiple barriers. In 2015, a systematic review of vaccine hesitancy studies in pregnancy was performed to evaluate barriers to vaccination.37 The review included studies on vaccine uptake of the seasonal influenza and TDaP (tetanus, diphtheria, and pertussis) vaccines. The study highlighted the primary barriers to vaccination in pregnancy as being concerns related to vaccine safety, a belief that the vaccine was unnecessary or ineffective, lack of a recommendation from a healthcare worker, low vaccine literacy, poor access, concerns of cost, and receipt of conflicting advice. On the basis of these data indicating that vaccine hesitancy in pregnancy is complex, we decided to use the One Vax Two Lives campaign to push users to our website containing an extensive list of frequently asked questions (FAQs) with up-to-date, scientific information on the benefits and risks of COVID-19 vaccination in pregnancy. Here, we also provided direct links and citations to the scientific articles supporting the statements so that users could review our sources.
Whether social media can be used to influence vaccine acceptance is unclear and difficult to prove38 , 39; in contrast, mis- and disinformation can spread virally on social media and promote vaccine hesitancy. There is some evidence that geographic regions in the United States with greater exposure to misinformation related to the human papillomavirus vaccine corresponded to areas with lower vaccine coverage; these data suggest that negative social media content may influence vaccine acceptance.40 It remains unknown whether efforts to dispel vaccine myths with social media campaigns (such as One Vax Two Lives) focused on promoting positive messaging with medically and scientifically accurate information might be sufficient to increase vaccination rates in pregnant women.
Our approach
The One Vax Two Lives team
Distilling COVID-19 vaccine information into short stories and messages to educate, dispel vaccine myths, and motivate behavioral change required the skills of a large team with diverse expertise in obstetrics, infectious diseases and vaccines, public health, multimedia journalism, social media, community engagement, video production, and storytelling. In the absence of grant funding at the campaign onset, we relied on charitable donations to fund a student workforce spanning the Department of Communication and the Schools of Medicine and Public Health at the University of Washington. Oversight by senior faculty with expertise in journalism, vaccine misinformation, and obstetrical infectious disease helped guide the team, but project management was assigned to the students early in the campaign. The campaign was student-led by the University of Washington master students in Communication Leadership, many of whom were specializing in digital creative strategy and/or social media, and medical students with clinical interests in reproductive infectious diseases and public health. Over time, the team grew to include University of Washington master students in Epidemiology and Community-Oriented Public Health. Because we primarily leveraged a student workforce, the campaign was highly cost-effective. From the beginning, the team included bilingual, bicultural Hispanic Latinas who adapted and translated content for pregnant Spanish-speaking people. For the students’ benefit, the project provided real-word practical applications of their learning and opportunities to complete practicum, capstone, and thesis projects for their respective degree programs. Any successes of the program were a product of the entire team’s collective efforts (Videos 1 and 2).
Strategy
In developing public health communication, we consider market research as an ideal early step to learn about how the target audience uses social media and the types of content that they respond to (Box 1 ). However, given the surge in maternal mortality owing to COVID-19, we decided not to perform research in the early campaign and instead used analytics from test campaigns to obtain information on best-performing content and social media platforms with the greatest reach. In the absence of market research, we created multimedia content based on our own experiences with obstetrical populations and common vaccine myths. Content aimed at our target audience was distributed through our known networks including the Facebook groups: Physician Moms Group COVID-19 Subgroup, the OBGYN Physician Moms Group, and the Infectious Disease Society for Obstetrics and Gynecology group. Many of these physicians proceeded to share our content on their personal or office practice social media channels and downloaded the brochure. Within 6 weeks, our social media advertisements were also being distributed to influencers who agreed to partner with us and had tens of thousands of followers interested in pregnancy topics. Finally, we participated in and led webinars on COVID-19 vaccination in pregnancy where we described how to access our content.
Box 1. Approach to a public health communication campaign.
|
|
|
|
|
|
|
|
|
|
| We present 10 steps to creating and launching a public health communication campaign to change social behavior. Because of the urgency of the COVID-19 pandemic, we did not conduct market research before launching our One Vax Two Lives campaign. We are now incorporating research programs studying vaccine hesitancy into new campaign launches targeting specific undervaccined pregnant populations. |
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Content generation
Website
Our primary response was to create a single hub where providers, pregnant people, and their loved ones could learn more about the risks of COVID-19 and the benefits of vaccination in pregnancy.41 One Vax Two Lives multimedia communications were designed using lay language so that they could be accessible and understandable to people from all backgrounds. We created a user-friendly website that houses several resources for the public. The landing page provides an extensive list of FAQs with the most up-to-date evidence-based answers in plain language (Table 1 ) and links to cited scientific articles. Most of the FAQs discuss vaccine safety and risks of COVID-19 disease in pregnancy. As the campaign progressed, we continued to update the page to provide information on boosters, new SARS-CoV-2 variants, and additional myths that surfaced on social media.
Table 1.
Frequently asked questions answered on the homepage of the One Vax Two Lives website
| Categories | Frequently asked questions |
|---|---|
| Vaccine safety and risks |
|
| Risks of COVID-19 disease while pregnant |
|
| Vaccine recommend-ations |
|
| How do vaccines work |
|
| Variants, boosters, and previous COVID-19 disease |
|
| Menstrual periods, fertility |
|
mRNA, messenger RNA.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Language accessibility was critical to reach vaccine-hesitant populations. We enlisted the support of volunteers and received grants to translate the website into the most spoken languages in the State of Washington. Bilingual and bicultural Hispanic Latinas have been active team members since the campaign inception and led the translation of materials into Spanish on a weekly basis. To enhance the accessibility of our campaign, we continue to build the non-English content in other languages on our website. Currently, our FAQ page is translated in Spanish, simplified Chinese, Vietnamese, Tagalog, Somali, Russian, Ukrainian, and Bulgarian. Disseminating this material to non–English-speaking populations requires the partnership of the community, public health partners, and medical providers. Evaluating the reach of our non-English content and creating social media content in languages other than Spanish remains an intentional goal for our team.
Web articles
In response to new developments in the pandemic and trending questions on social media, medical students on our team wrote short web-based articles with titles designed to attract attention and entice users to read further (Table 2 ). The articles were intended to be brief and to distill complex research regarding COVID-19 into content that was accessible for individuals with varied scientific literacy. They addressed many of the popular, false claims circulating on social media, and gave evidence-based counterarguments in a longer format than was possible in our social media advertisements. We avoided polarizing article titles that might dissuade vaccine-hesitant individuals from reading the content and maintained a positive and encouraging tone throughout our pieces. Instead, we titled articles in such a manner that it was unclear if the content supported pro- or antivaccine arguments to help draw in vaccine-hesitant individuals. For example, our first article was titled: “Ten things you should know about the COVID-19 vaccine in pregnancy.” The goal of this approach was to attract social media users with various viewpoints to learn more and direct users to the One Vax Two Lives website. These articles enabled social media users to be exposed to short answers to trending questions without filtering through an extensive list of FAQs.
Table 2.
Titles and content of One Vax Two Lives web articles
| Article title | Content summary |
|---|---|
| 10 things you should know about COVID-19 vaccination in pregnancy |
|
| What is the omicron BA.2 variant and how does it affect my pregnancy? |
|
| 5 things to know about the COVID-19 vaccine and your menstrual cycle |
|
| 5 things to know about the COVID-19 vaccine, women and men’s fertility, and sexual functioning |
|
| 5 things to know about the omicron variant and pregnancy |
|
| 5 things to know about the COVID-19 vaccine and breastfeeding |
|
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Social media advertisements and videos
Running a sponsored advertisement campaign on Facebook and Instagram can be impactful because these platforms can support targeted outreach to specific audience groups. Our team created >40 social media advertisements to test messages and images designed to promote awareness of COVID-19 disease risks in pregnancy and vaccine acceptance (Figures 1 and 2). We brainstormed ideas for content on an ongoing basis, which were transformed into advertisements by the University of Washington Communication Leadership graduate students. During weekly team meetings, social media advertisements were reviewed and selected by the leadership team before posting. Digital creative ads were based on 4 different message types: (1) informational, (2) protection of family, (3) social proof, and (4) seasonal themes. Informational advertisements included text and video messages providing current facts about COVID-19 disease risks and benefits of vaccination in pregnancy, which supported disease and vaccine awareness. Protecting one’s family was a consistent theme that resonated strongly with our audience. Social proof messages included advertisements highlighting the hundreds of thousands of pregnant people who had already been vaccinated safely. Seasonal themes included messages encouraging vaccination in a short time frame before holiday travel or gatherings. We also used social media to dispel vaccine myths, but this approach requires caution because it can have the unintended consequence of amplifying false information. We made a concerted effort to avoid amplification of disinformation, and instead designed our social media messaging to target several common arguments against vaccination and categories of disinformation (Box 2 ).42
Box 2. One Vax Two Lives response to address vaccine myths: “One Vax Two Lives Tactics and Strategies for Addressing and Dispelling Vaccine Myths”.
|
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Video messages are a powerful tool for engaging social media users and influencing young-adult sentiments.43 The social media platform TikTok has been one of the fastest growing social media channels because of its engaging use of short, catchy videos. Globally, COVID-19–related videos on TikTok have been watched approximately 93.1 billion times.44 Instagram has adopted a similar short-video format called “Reels.” To utilize these platforms, we created video posts featuring “trusted messengers” in the healthcare space by interviewing obstetrician-gynecologists, nurses, medical students, vaccine experts, and individuals, many of whom were multilingual, on the topics of COVID-19 disease risk in pregnancy, vaccine safety, and dispelling common myths. We tried to maintain a 30-to-45-second length of edited video interviews, which could be adapted to Facebook and Instagram Reels. Later in the campaign, a graduate student in Communication with TikTok experience began to develop our TikTok channel by modeling content after trending themes and hashtags.
Our most successful messages included advertisements containing information about the COVID-19 Delta and Omicron variants, video messages of doctors debunking COVID-19 vaccination myths, and advertisements linking to our web articles. For example, an advertisement in Spanish with facts about the Omicron variant received 680 link clicks, 20 comments, 84 reactions, was shared 94 times, and had a cost-per-click (CPC) of 11 cents. A University of Washington branded video showing an obstetrician-gynecologist sharing critical information on COVID-19 vaccinations and pregnancy received 368 link clicks, 49 comments, 53 post reactions, was shared 5 times, and had a CPC of 21 cents. These were significant when compared with the campaign average of 212 link clicks, 14 comments, 32 reactions, 13 shares, and a CPC of 39 cents.
Distribution and results
Social media advertisement campaign
To act quickly in the wake of the COVID-19 Delta variant surge in maternal mortality, we launched our social media advertisement campaign without any previous market research on the types of advertisements that might perform best with pregnant individuals. We based our initial approach on past communications campaigns promoting masking and vaccines to the public and our own experiences with pregnant individuals. On a weekly basis, we used Facebook and Instagram analytics to assess advertisement performance and audience feedback and engagement to make iterative changes to our content and campaign goals. We primarily used the Facebook and Instagram platforms to target English and Spanish-speaking pregnant individuals on the basis of location, demographics, interests, and behaviors. The audience segments targeted by our campaign included English and Spanish-speaking individuals with an interest in maternity clothing, pregnancy, infants, childcare, and/or baby showers. Using these audience groups, we ran several advertisement campaigns on Facebook with phase objectives focused on “learning,” “expansion,” and “redirection to the website.”
In the learning phase, we focused on identifying the most effective platform for Spanish-speaking pregnant individuals, a population with low vaccine uptake in the State of Washington. We evaluated metrics associated with user engagement with our posts and “cost per engagement” as a performance metric. We ran the same advertisement set to Spanish-speaking individuals in our target audience on Facebook and Instagram in a 2-week period. The advertisement set on Facebook garnered a higher number of “impressions,” which is the number of times that content was seen by users through a combination of our sponsored advertisements and organic shares by users. We focused our remaining sponsored advertisement campaigns on Facebook to reach Spanish-speaking pregnant individuals.
In the expansion phase, we focused efforts on building brand awareness to increase the size of the One Vax Two Lives audience on Facebook in the State of Washington. This campaign had 6 advertisements that reached 135,037 people with 198,470 impressions; individuals performed 8688 actions on the posts at a cost of $6.79 per 1000 people reached. Although we were able to reach many people interested in pregnancy-related topics, the engagement with our content and outbound clicks to the One Vax Two Lives website remained low. The increase in reach did not result in a corresponding increase in visits to our website.
In the past, our communication team used reach and post engagement (likes, shares, and comments) to measure impact of masking and COVID-19 vaccination campaigns. However, for pregnant people, a “like” or “share” may not be the best metric to reflect a change in behavior (ie, vaccine uptake). Instead, we chose to focus the next phase of the campaign on increasing the number of outbound link clicks to the One Vax Two Lives website, in the hope that engaging with the latest research demonstrating vaccine safety in a trusted, accessible format would help inform vaccination decisions.
In the “redirecting to the website” phase, we created 2 different advertisement campaigns with the objective of sending users to the One Vax Two Lives website. We used a Facebook algorithm to show our advertisements to people who were most likely to click on an outbound link. Between the 2 campaigns, we ran 19 advertisements in English and Spanish. To attract vaccine-hesitant pregnant individuals to click on our advertisements, we also created advertisements pointing to our web articles and wrote attention-grabbing headlines. The first campaign received 1257 link clicks at a cost of 76 cents per link click. This campaign reached 66,241 people and was viewed by 123,872 people. The second campaign received 1,913 link clicks at a CPC of 39 cents and reached 74,803 people with 171,672 impressions. For context, the average CPC for these types of Facebook advertisements nationally in early 2022 was 94.8 cents.45 Nearly 90% of users clicking links identified as “women.” Website traffic data during this time indicated that our strategy was successful, with 63% originating from Facebook and Instagram. During this phase, approximately 1400 website visitors spent an average of 2 minutes and 53 seconds on the website landing page containing answers to FAQs on COVID-19 vaccines. By comparison, the average time on a webpage across various industry websites is 52 seconds.46 Although the calculations behind these metrics are complex and fallible, this direct comparison of CPC and time on page for the One Vax Two Lives content against industry averages demonstrates a comparatively deep engagement with the informational content provided.
Our One Vax Two Lives campaign was run entirely on charitable donations for the first 5 months of the campaign until we procured pilot grant funding to study vaccine hesitancy. Therefore, our Facebook advertisement campaigns were only run in the State of Washington. Expansion of our campaign to other US states using existing social media advertisements is highly cost-effective because the advertisements are already generated and can simply be targeted regionally to Facebook users with interests in maternity clothing, baby showers, and childcare. The Supplemental Table contains estimated costs for campaign expansion in all US states.
Communication toolkit and brochures
Our public health partners began to request access to our content to share on their platforms. To facilitate distribution of our best-performing social media advertisements, video messages, and web-based articles, we created a free, downloadable communication toolkit on our website for use by anyone, including public health partners, physicians, and social media influencers. We also included downloadable brochures in several languages in this toolkit so that partners could provide content for their offline audiences. The hope was that widely distributing this content could provide a broad and rapid response to vaccine myths circulating on social media, and direct our priority audiences to our multilanguage information sources via a recommendation from a trusted community source.
Building community through partnerships
Engagement with public health institutions, community, and national partners was critical to informing the development of the campaign. It was through these relationships that we learned of the hurdles that providers were facing in discussing COVID-19 vaccination with their pregnant patients. These relationships were also essential for distributing the campaign materials through the communication toolkit, and elevating the public credibility of the campaign to broader audiences. Early stakeholders included the Washington State Department of Health (DOH), Washington State Hospital Association, Public Health – Seattle & King County, Washington State Obstetrical Association, Washington State Perinatal Collaborative, the National Black Leadership Commission on Health, and clinical partners, such as the University of Washington Department of Obstetrics and Gynecology and community health centers throughout Washington. In addition, the Washington State DOH provided extensive reviews and edits of our content. As part of our community engagement efforts, we participated in and organized webinars to present our campaign findings and approach to public health messaging.
Current and future directions: researching vaccine hesitancy in pregnancy
Our data on vaccination rates, number of doses, pregnancy status, English language proficiency, racial and ethnic identity, and socioeconomic status are incomplete, which hampers our knowledge of vaccine-hesitant populations. We are now launching several mixed methods studies of vaccine hesitancy in different populations, which will provide feedback for further social media content creation targeted specifically to undervaccinated populations. National data on vaccinated pregnant individuals come from various databases, such as the Vaccine Safety Datalink (VSD) project and v-safe.47 , 48 These databases have important limitations based on their respective reporting structures and on the communities represented. The VSD data are limited to individuals vaccinated within 8 urban health centers and do not report individuals who are not fully vaccinated. Vaccination data provided by participants in the v-safe registry was voluntary, and individuals without access to a smartphone or who decline to provide data are not included. Furthermore, vaccination data on pregnant individuals are not readily available on a county level. States also vary by how race and ethnicity are reported in conjunction with vaccination data.
Racial and ethnic disparities in COVID-19 outcomes and vaccination have been reported in numerous marginalized groups in the United States and globally.49, 50, 51, 52, 53 These disparities reflect social injustice, structural racism, and many forms of inequality. Vaccine hesitancy or acceptance are shaped by social, political, racial or ethnic, and cultural experiences and values. The forces that drive vaccine acceptance and hesitancy are also rooted in past historic and current injustices that marginalized communities have faced.54 , 55 It is vital that vaccine-related health communication originates from “trusted messengers” and addresses population-specific vaccine concerns in a culturally relevant manner to engage in social behavior decisions. Addressing vaccine concerns differently within diverse communities is critical for raising vaccination rates.
Taking this sociopolitical context into account, our research approach aims to develop equitable and bidirectional relationships with community partners, generate resources that address community needs and concerns, and produce initiatives that cultivate trust and confidence in COVID-19 vaccines.56 We are currently launching several research programs to understand the roots of vaccine hesitancy in pregnant people, which will further inform our social media campaign. We will begin by collaborating with community partners to learn from several undervaccinated pregnant populations in the United States, including individuals living in rural areas of the State of Washington and Black, Afro-Latinx, and Spanish-speaking Hispanic/Latina/x populations. Through semistructured interviews, we will ask participants about their attitudes toward vaccination, where they obtain news, COVID-19 vaccine misinformation narratives, and who they consider to be trusted messengers of health information. We will also ask participants for their reaction to digital content to obtain feedback on our social media campaign strategy and how content should be tailored for each population. We have elected to conduct direct interviews instead of focus groups because of the concern that individual members might unintentionally spread vaccine myths and disinformation to other focus group members. Community partners will be an essential resource in drafting the interview guides for direct interviews because they can offer feedback on the appropriateness of the questions and identify assets and trusted leaders who can help disseminate newly developed resources and information. On the basis of these data, we will generate survey tools to collect data from a larger population to validate our preliminary findings and inform new social media campaigns.
Conclusions
Scientifically informed, culturally relevant, and accessible public health communication is critical to educate and engage the public throughout situations requiring an emergency response, such as the current COVID-19 pandemic. Throughout this campaign, we have learned from pregnant individuals about their concerns regarding vaccination against COVID-19 in pregnancy and the ways in which tailored scientific communication can address these concerns, build trust, and help to inform decisions. It was through our bidirectional engagement with public health partners, obstetrical providers, and the public that we were able to develop engaging social media content to share with pregnant individuals and their families. The campaign is highly cost-effective and scalable (Supplemental Table), but to date has only been run in the State of Washington. In the next phase of the campaign, we will be expanding the reach of One Vax Two Lives into vaccine-hesitant pregnant populations. This work will provide a foundation for learning about a community’s unique vaccine concerns and build a responsive social media campaign. We hope that the lessons learned from this campaign might be useful for other groups in launching future vaccine and public health campaigns directed toward improving the health of pregnant people.
Acknowledgments
One Vax Two Lives would not have been possible without philanthropic donors, who funded the first 5 months of the campaign. We thank Marcie Stone, MLIS, for her excellent ideas. We are grateful to the University of Washington (UW) Population Health Initiative, Washington State DOH, Restart Partners, and Mednax for their pilot funding, which continues to propel our work. We are also thankful for the support of the UW Department of Obstetrics and Gynecology and specifically Barbara Goff, MD (Chair), Estrella Weaver, MBA (Vice-Chair, Finance and Administration), and Nicole Wothe, BA, for their support and administrative assistance. No donors or funders had any role in the One Vax Two Lives campaign, manuscript preparation, or decision to publish.
We thank Jevin West, PhD, and the UW Center for an Informed Public for their continued and unwavering support of One Vax Two Lives. The UW Communication Leadership Master’s Program provided the creative strategy and student workforce that propelled the campaign. We are also grateful to Shelby Wilson, PhD, RD for her leadership of master’s students in the UW Communication Leadership spring practicum course who are developing direct interview guides for our research programs on vaccine hesitancy among pregnant people residing in rural areas and Black pregnant people.
We are very appreciative of the team of individuals at the Washington State Department of Health that took an early interest in our campaign, read and edited our content, amplified our messages, and supported the work. We thank Gauri Gupta, MScPH (COVID-19 Health Educator), Danielle Koenig (Health Promotion Supervisor and immunization education expert), and Bat-Sheva Stein, DNP, MSN, RN (Public Health Nurse Consultant).
Obstetrical and public health leaders in the State of Washington amplified our campaign and continue to support the work. We thank Rita Hsu, MD (Physician Chair of the Washington State Perinatal Collaborative), Mary Kay Ausenhus, MSN, WHNP, CPHQ (Director of Safety and Quality for the Washington State Hospital Association), and Katherine Eastwood, MD (President of the Washington State Obstetrical Association).
We thank the National Black Leadership Commission on Health for their excellent partnership and look forward to the next phase of work to collaboratively study vaccine hesitancy in Black pregnant individuals. We are grateful to Evelyn Botwe, MPH (Director of Programs), Melissa Baker (Chief Operating Officer), Bibi Natosha, and Judy Fordjuoh, MPH for their enthusiasm and investment in promoting COVID-19 vaccination.
We are also grateful to Rita Hsu, MD, Linsey Monaghan, MD, Steve Erickson, MD, Carly Ingalls, MD, and Sharilyn Emhoff, RN, BSN who are champions for our research programs to study COVID-19 vaccine hesitancy in rural and Spanish-speaking Latina/x Hispanic communities in the State of Washington.
Finally, we recognize the differences between sex and gender, noting that the term “women” is not inclusive for biologically-born female individuals who identify as nonbinary or transgender. Therefore, we use the terms pregnant women, pregnant individuals, and pregnant people interchangeably throughout the manuscript to be inclusive of this spectrum.
Footnotes
L.M. and E.D. contributed equally to this work.
The authors report no conflict of interest.
The One Vax Two Lives campaign was supported by individual charitable donations and funds from the University of Washington Population Health Initiative, Washington State Department of Health, Restart Partners, and Mednax. None of the funders had a role in the design of the campaign, writing of the report, decision to submit the article for publication, or in the study design of our planned research programs on vaccine hesitancy.
Supplementary Data
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Supplemental Table.
Cost to scale up the One Vax Two Lives campaign to all US states and territories
| US state or territory | Annual birthsa | Pregnant people on social mediab | Expected outbound clicksc | Total Facebook and Instagram ad costsd |
|---|---|---|---|---|
| Alabama | 57,647 | 46,118 | 1176 | $7608.71 |
| Alaska | 9469 | 7575 | 193 | $1249.79 |
| Arizona | 76,947 | 61,558 | 1570 | $10,156.08 |
| Arkansas | 35,251 | 28,201 | 719 | $ 4652.71 |
| California | 420,259 | 336,207 | 8573 | $55,469.14 |
| Colorado | 61,494 | 49,195 | 1254 | $8116.47 |
| Connecticut | 33,460 | 26,768 | 683 | $4416.32 |
| Delaware | 10,392 | 8314 | 212 | $1371.62 |
| District of Columbia | 8874 | 7099 | 181 | $1171.26 |
| Florida | 209,671 | 167,737 | 4277 | $27,674.06 |
| Georgia | 122,473 | 97,978 | 2498 | $16,164.97 |
| Hawaii | 15,785 | 12,628 | 322 | $2083.43 |
| Idaho | 21,533 | 17,226 | 439 | $2842.10 |
| Illinois | 133,298 | 106,638 | 2719 | $17,593.74 |
| Indiana | 78,616 | 62,893 | 1604 | $10,376.37 |
| Iowa | 36,114 | 28,891 | 737 | $4766.61 |
| Kansas | 34,376 | 27,501 | 701 | $4537.22 |
| Kentucky | 51,668 | 41,334 | 1054 | $6819.56 |
| Louisiana | 57,328 | 45,862 | 1169 | $7566.61 |
| Maine | 11,539 | 9231 | 235 | $1523.01 |
| Maryland | 68,554 | 54,843 | 1399 | $9048.31 |
| Massachusetts | 66,428 | 53,142 | 1355 | $8767.70 |
| Michigan | 104,074 | 83,259 | 2123 | $13,736.52 |
| Minnesota | 63,443 | 50,754 | 1294 | $8373.71 |
| Mississippi | 35,473 | 28,378 | 724 | $4682.01 |
| Missouri | 69,285 | 55,428 | 1413 | $9144.79 |
| Montana | 10,791 | 8633 | 220 | $1424.28 |
| Nebraska | 24,291 | 19,433 | 496 | $3206.12 |
| Nevada | 33,653 | 26,922 | 687 | $4441.79 |
| New Hampshire | 11,791 | 9433 | 241 | $1556.27 |
| New Jersey | 97,954 | 78,363 | 1998 | $12,928.75 |
| New Mexico | 21,903 | 17,522 | 447 | $2890.93 |
| New York | 209,338 | 167,470 | 4270 | $27,630.10 |
| North Carolina | 116,730 | 93,384 | 2381 | $15,406.96 |
| North Dakota | 10,059 | 8047 | 205 | $1327.67 |
| Ohio | 129,191 | 103,353 | 2635 | $17,051.66 |
| Oklahoma | 47,623 | 38,098 | 972 | $6285.66 |
| Oregon | 39,820 | 31,856 | 812 | $5255.76 |
| Pennsylvania | 130,693 | 104,554 | 2666 | $17,249.91 |
| Rhode Island | 10,101 | 8081 | 206 | $1333.21 |
| South Carolina | 55,704 | 44,563 | 1136 | $7352.26 |
| South Dakota | 10,960 | 8768 | 224 | $1446.59 |
| Tennessee | 78,689 | 62,951 | 1605 | $10,386.00 |
| Texas | 368,190 | 294,552 | 7511 | $48,596.66 |
| Utah | 45,702 | 36,562 | 932 | $6032.12 |
| Vermont | 5133 | 4106 | 105 | $677.49 |
| Virginia | 94,749 | 75,799 | 1933 | $12,505.73 |
| Washington | 83,086 | 66,469 | 1695 | $10,966.35 |
| West Virginia | 17,323 | 13,858 | 353 | $2286.43 |
| Wisconsin | 60,594 | 48,475 | 1236 | $7997.68 |
| Wyoming | 6128 | 4902 | 125 | $808.82 |
| Puerto Rico | 18,933 | 15,146 | 386 | $2498.93 |
| Virgin Islands | 876 | 701 | 18 | $115.62 |
| Guam | 2935 | 2348 | 60 | $387.38 |
| Northern Mariana Islands | 628 | 502 | 13 | $82.89 |
| Total | $518,307 |
This table shows our estimates for running a 4-week Facebook and Instagram advertisement campaign for each US state or territory based on data obtained from test advertisements run by One Vax Two Lives.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Annual births. The annual births in each state were taken from the US Centers for Disease Control and Prevention data published in the National Center for Health Statistics, accessed on April 22, 2022. There were no data on births in American Samoa, thus this US territory was not included in the estimates
The Pew Research Center estimates that 80% of 18- to 29-year-old adults are on social media. We applied this estimate to the number of annual births in each state to arrive at an estimate of the number of pregnant people on social media in each state
To determine the number of expected outbound clicks, we applied certain assumptions. First, we multiplied the pregnant people on social media by an “inflation factor” (1.5) to account for the additional individuals who would need to be targeted on social media to reach pregnant people in each region because our method for reaching pregnant people was not precise (eg, users targeted with interest in maternity clothes). Secondly, we multiplied this number by an average outbound click-through rate of 1.7%, which was associated with our best-performing advertisements tested in the campaign (pregnant people on social media×1.5×0.017=number of expected outbound clicks)
Total Facebook and Instagram advertisement costs of the campaign for each US state or territory, which does not account for the cost of the student workforce. This estimate assumes a $6.47 average cost per outbound click (number of expected outbound clicks×$6.47=total Facebook and Instagram advertisement costs). This estimated average outbound cost-per-click accounts for only the advertisement costs on Facebook and Instagram and not the cost of the student workforce of the project. Extending the campaign to other social media platforms (ie, TikTok) or Google display advertisements would generate additional costs.
References
- 1.Lokken E.M., Huebner E.M., Taylor G.G., et al. Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. 2021;225:77.e1–77.e14. doi: 10.1016/j.ajog.2020.12.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lokken E.M., Walker C.L., Delaney S., et al. Clinical characteristics of 46 pregnant women with a severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. 2020;223:911.e1–911.e14. doi: 10.1016/j.ajog.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metz T.D., Clifton R.G., Hughes B.L., et al. Association of SARS-CoV-2 infection With serious maternal morbidity and mortality from obstetric complications. JAMA. 2022;327:748–759. doi: 10.1001/jama.2022.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villar J., Ariff S., Gunier R.B., et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study. JAMA Pediatr. 2021;175:817–826. doi: 10.1001/jamapediatrics.2021.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeSisto C.L., Wallace B., Simeone R.M., et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization – United States, March 2020–September 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1640–1645. doi: 10.15585/mmwr.mm7047e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delahoy M.J., Whitaker M., O'Halloran A., et al. Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19 – COVID-NET, 13 states, March 1–August 22, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1347–1354. doi: 10.15585/mmwr.mm6938e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panagiotakopoulos L., Myers T.R., Gee J., et al. SARS-CoV-2 infection among hospitalized pregnant women: reasons for admission and pregnancy characteristics – eight U.S. Health care centers, March 1–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1355–1359. doi: 10.15585/mmwr.mm6938e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kasehagen L., Byers P., Taylor K., et al. COVID-19-Associated deaths after SARS-CoV-2 infection during pregnancy – Mississippi, March 1, 2020-October 6, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1646–1648. doi: 10.15585/mmwr.mm7047e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seasely A.R., Blanchard C.T., Arora N., et al. Maternal and perinatal outcomes associated with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Delta (B.1.617.2) variant. Obstet Gynecol. 2021;138:842–844. doi: 10.1097/AOG.0000000000004607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Texas Department of State Health Services . 2021. COVID-19 vaccine allocation phase.https://www.dshs.texas.gov/coronavirus/immunize/vaccine/EVAP-Phase1B.pdf Available at: Accessed October 1, 2021. [Google Scholar]
- 11.New Hampshire Bureau of Infectious Disease Control . 2021. NH COVID-19 Vaccination Allocation Guidelines for Phase 1b.https://www.dhhs.nh.gov/dphs/cdcs/covid19/documents/phase-1b-technical-assistance.pdf Available at: Accessed October 1, 2021. [Google Scholar]
- 12.New Mexico Department of Health: State of New Mexico. COVID-19 vaccine allocation plan phases 1A, 1B, 1C, and 2. 2021. https://cv.nmhealth.org/wp-content/uploads/2021/01/2021.1.8-DOH-Phase-Guidance.pdf Available at: Accessed July 11, 2022. [Google Scholar]
- 13.Alaska Department of Health and Social Services . 2020. COVID-19 Vaccine Allocation: Phase 1b.http://dhss.alaska.gov/dph/Epi/id/SiteAssets/Pages/HumanCoV/DHSS_VaccineAllocation_Phase1b.pdf Available at: Accessed July 11, 2022. [Google Scholar]
- 14.Mississippi Department of Education News . 2021. Current qualifications for COVID-19 vaccination in Mississippi.https://msachieves.mdek12.org/current-qualifications-for-covid-19-vaccination-in-mississippi/ Available at: Accessed April 1, 2022. [Google Scholar]
- 15.Lipkind H.S., Vazquez-Benitez G., DeSilva M., et al. Receipt of COVID-19 vaccine during pregnancy and preterm or small-for-gestational-age at birth – eight integrated health care organizations, United States, December 15, 2020–July 22, 2021. MMWR Morb Mortal Wkly Rep. 2022;71:26–30. doi: 10.15585/mmwr.mm7101e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin R. Pregnant people’s paradox-excluded from vaccine trials despite having a higher risk of COVID-19 complications. JAMA. 2021;325:1027–1028. doi: 10.1001/jama.2021.2264. [DOI] [PubMed] [Google Scholar]
- 17.Abbasi J. Widespread misinformation about infertility continues to create COVID-19 vaccine hesitancy. JAMA. 2022;327:1013–1015. doi: 10.1001/jama.2022.2404. [DOI] [PubMed] [Google Scholar]
- 18.Ennab F., Babar M.S., Khan A.R., et al. Implications of social media misinformation on COVID-19 vaccine confidence among pregnant women in Africa. Clin Epidemiol Glob Health. 2022;14 doi: 10.1016/j.cegh.2022.100981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prasad M., Lin J.L., Gu Y., Gupta R., Macary P., Schwarz H. No crossreactivity of anti-SARS-CoV-2 spike protein antibodies with Syncytin-1. Cell Mol Immunol. 2021;18:2566–2568. doi: 10.1038/s41423-021-00773-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yasmin F., Najeeb H., Moeed A., et al. COVID-19 vaccine hesitancy in the United States: a systematic review. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.770985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kharbanda E.O., Haapala J., DeSilva M., et al. Spontaneous abortion following COVID-19 vaccination during pregnancy. JAMA. 2021;326:1629–1631. doi: 10.1001/jama.2021.15494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fell D.B., Dhinsa T., Alton G.D., et al. Association of COVID-19 vaccination in pregnancy with adverse peripartum outcomes. JAMA. 2022;327:1478–1487. doi: 10.1001/jama.2022.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimabukuro T.T., Kim S.Y., Myers T.R., et al. Preliminary findings of mRNA Covid-19 vaccine safety in pregnant persons. N Engl J Med. 2021;384:2273–2282. doi: 10.1056/NEJMoa2104983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stock S.J., Carruthers J., Calvert C., et al. SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland. Nat Med. 2022;28(3):504–512. doi: 10.1038/s41591-021-01666-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 Available at: Accessed October 1, 2021.
- 26.Davies P., Chapman S., Leask J. Antivaccination activists on the World Wide Web. Arch Dis Child. 2002;87:22–25. doi: 10.1136/adc.87.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keelan J., Pavri V., Balakrishnan R., Wilson K. An analysis of the human papilloma virus vaccine debate on MySpace blogs. Vaccine. 2010;28:1535–1540. doi: 10.1016/j.vaccine.2009.11.060. [DOI] [PubMed] [Google Scholar]
- 28.Evrony A., Caplan A. The overlooked dangers of anti-vaccination groups’ social media presence. Hum Vaccin Immunother. 2017;13:1–2. doi: 10.1080/21645515.2017.1283467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith N., Graham T. Mapping the anti-vaccination movement on Facebook. Inf Commun Soc. 2019;22:1310–1327. [Google Scholar]
- 30.Koltai K., Moran R.E., Buckley N., Suresh Kumar D., Klentschy C. 2021. Virality Project. Vaccine “shedding” narratives targeted toward women.https://www.viralityproject.org/rapid-response/vaccine-shedding-narratives-targeted-toward-women Available at: Accessed July 11, 2022. [Google Scholar]
- 31.US Food & Drug Administration . 2018. Pregnant women: scientific and ethical considerations for inclusion in clinical trials guidance for industry.https://www.fda.gov/regulatory-information/search-fda-guidance-documents/pregnant-women-scientific-and-ethical-considerations-inclusion-clinical-trial Available at: Accessed July 11, 2022. [Google Scholar]
- 32.Berry S.D., Johnson K.S., Myles L., et al. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J Am Geriatr Soc. 2021;69:1140–1146. doi: 10.1111/jgs.17136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sparks G., Lopes L., Montero A., Hamel L., Brodie M. 2022. Kettering Family Foundation. KFF COVID-19 vaccine monitor: pregnancy misinformation.https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-pregnancy-misinformation-may-2022/ Available at: Accessed July 11, 2022. [Google Scholar]
- 34.MacDonald N.E., SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 35.Betsch C., Böhm R., Chapman G.B. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. 2015;2:61–73. [Google Scholar]
- 36.Thomson A., Robinson K., Vallée-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34:1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 37.Wilson R.J., Paterson P., Jarrett C., Larson H.J. Understanding factors influencing vaccination acceptance during pregnancy globally: a literature review. Vaccine. 2015;33:6420–6429. doi: 10.1016/j.vaccine.2015.08.046. [DOI] [PubMed] [Google Scholar]
- 38.Giustini D., Ali S.M., Fraser M., Kamel Boulos M.N. Effective uses of social media in public health and medicine: a systematic review of systematic reviews. Online J Public Health Inform. 2018;10:e215. doi: 10.5210/ojphi.v10i2.8270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laranjo L., Arguel A., Neves A.L., et al. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc. 2015;22:243–256. doi: 10.1136/amiajnl-2014-002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dunn A.G., Surian D., Leask J., Dey A., Mandl K.D., Coiera E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine. 2017;35:3033–3040. doi: 10.1016/j.vaccine.2017.04.060. [DOI] [PubMed] [Google Scholar]
- 41.Adams Waldorf K.M., Marcell L.M. University of Washington; Seattle: Washington: 2022. Two Lives OV.https://onevaxtwolives.com Available at: Accessed July 11, 2022. [Google Scholar]
- 42.Dubé È., Ward J.K., Verger P., MacDonald N.E. Vaccine hesitancy, acceptance, and anti-vaccination: trends and future prospects for public health. Annu Rev Public Health. 2021;42:175–191. doi: 10.1146/annurev-publhealth-090419-102240. [DOI] [PubMed] [Google Scholar]
- 43.Jensen U.T., Ayers S., Koskan A.M. Video-based messages to reduce COVID-19 vaccine hesitancy and nudge vaccination intentions. PLoS One. 2022;17 doi: 10.1371/journal.pone.0265736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kong W., Song S., Zhao Y.C., Zhu Q., Sha L. TikTok as a health information source: assessment of the quality of information in diabetes-related videos. J Med Internet Res. 2021;23 doi: 10.2196/30409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dopson E. 2022. Shopify blog. How much do Facebook ads cost in 2022? Here’s what the data says.https://www.shopify.com/blog/facebook-ads-cost Available at: Accessed July 11, 2022. [Google Scholar]
- 46.Arora P. 2022. Klipfolio MetricHQ. Average time on.https://www.klipfolio.com/metrics/marketing/average-time-on-page Available at: Accessed July 11, 2022. [Google Scholar]
- 47.Centers for Disease Control and Prevention Vaccine Safety Datalink. https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/vsd/index.html Available at: Accessed July 11, 2022.
- 48.Centers for Disease Control and Prevention V-safe after vaccination health checker. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/vsafe.html Available at: Accessed July 11, 2022.
- 49.Holtgrave D.R., Barranco M.A., Tesoriero J.M., Blog D.S., Rosenberg E.S. Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9–14. doi: 10.1016/j.annepidem.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hatcher S.M., Agnew-Brune C., Anderson M., et al. COVID-19 among American Indian and Alaska native persons - 23 states, January 31–July 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1166–1169. doi: 10.15585/mmwr.mm6934e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moore J.T., Ricaldi J.N., Rose C.E., et al. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020–22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59:137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lokken E.M., Taylor G.G., Huebner E.M., et al. Higher severe acute respiratory syndrome coronavirus 2 infection rate in pregnant patients. Am J Obstet Gynecol. 2021;225:75.e1–75.e16. doi: 10.1016/j.ajog.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alsan M., Wanamaker M., Hardeman R.R. The Tuskegee Study of Untreated Syphilis: a case study in peripheral trauma with implications for health professionals. J Gen Intern Med. 2020;35:322–325. doi: 10.1007/s11606-019-05309-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dawson M.A., Giger J.N., Powell-Young Y., Brannon C.B. Why African-Americans are hesitant to take the newly proposed COVID-19 vaccines: Tuskegee revisited. J Natl Black Nurses Assoc. 2020;31:vi–viii. [PubMed] [Google Scholar]
- 56.Hildreth J.E.K., Alcendor D.J. Targeting COVID-19 vaccine hesitancy in minority populations in the US: implications for herd immunity. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.
Marcell. One Vax Two Lives. Am J Obstet Gynecol 2022.