Abstract
Background
The impact of COVID-19 in families and patients with congenital diaphragmatic hernia (CDH) is unknown, this situation has generated uncertainty not only in family members but also in the optimal outpatient follow-up. Telehealth has become a fundamental tool for the follow-up during the pandemic. The objective of this survey is to evaluated the impact of SARS-CoV-2 in families and patients with CDH and the satisfaction with telematic follow-up.
Methods
Telephone survey of patient's caregivers with CHD, aged 1–16 years, followed in neonatal surgery outpatients, from January 31, 2020 to November 15, 2020. The ethical clearance for this study was taken from the Clinical Research Ethics Committee of our Research Institute vide letter number VHIR/239283/01.01.2021.
Results
81 surveys of 100 patients with active follow-up were carried out. There were no refusals in any contacted parents. There were 30 contacts (37%), 44.8% at school and 27.6% from cohabiting family members. Four infections (4.9%) were diagnosed, half symptomatic. In 40 patients (49.4%) the follow-up was telematic, with a mean score of 3.1 ± 1.3 out of 5. For future controls, 65% prefer presential follow-up, 25% alternate and 10% telematics. 50.6% reported greater anxiety and 34.6% (28/81) extreme measures of isolation, being more accentuated in the group of 3–6 years (p < 0.05).
Conclusion
The impact of COVID19 in patients with CHD is not greater than in the general pediatric population. Although the incorporation of the telehealth was well valued, most of the caregivers prefer the face-to-face outpatient follow-up.
Abbreviations: CDH, congenital diaphragmatic hernia; COVID-19, Coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
Keywords: Telemedicine, Congenital diaphragmatic hernia, SARS-CoV-2, COVID-19, Follow-up
Abstract
Antecedentes
Se desconoce el impacto de la COVID-19 en los familiares y pacientes con hernia diafragmática congénita (HDC). Esta situación ha generado incertidumbre, no solo en los familiares, sino también en el seguimiento óptimo de los pacientes. La telesalud se ha convertido en una herramienta fundamental para el seguimiento durante la pandemia. El objetivo de esta encuesta es evaluar el impacto del SARS-CoV-2 en los familiares y pacientes con HDC, así como la satisfacción con el seguimiento telemático.
Métodos
Encuesta telefónica realizada a los cuidadores de los pacientes con HDC, de edades comprendidas entre 1 y 16 años, a quienes se realizó un seguimiento en la unidad ambulatoria de cirugía neonatal desde el 31 de enero al 15 de noviembre de 2020. La autorización ética para este estudio se obtuvo del Comité de Ética de Investigación Clínica de nuestro Instituto de Investigación, con número de referencia VHIR/239283/01.01.2021.
Resultados
Se llevaron a cabo 81 encuestas de 100 pacientes con seguimiento activo. Ninguno de los padres contactados rechazó el seguimiento. Se produjeron 30 contactos (37%): el 44,8% en la escuela, y el 27,6% a los familiares convivientes. Se diagnosticaron cuatro infecciones (4,9%), la mitad de ellas sintomáticas. En 40 pacientes (49,4%), el seguimiento fue telemático, con una puntuación media de 3,1 ± 1,3 sobre 5. Para los controles futuros, el 65% prefirió el seguimiento presencial, el 25% alternativo, y el 10% telemático. El 50,6% reportó una mayor ansiedad, y el 34,6% (28/81) medidas extremas de aislamiento, siendo más acentuadas en el grupo de 3 a 6 años (p < 0,05).
Conclusión
El impacto de la COVID19 en los pacientes con HDC no es mayor en la población pediátrica general. Aunque la incorporación de la telesalud fue bien valorada, la mayoría de los cuidadores prefieren el seguimiento presencial.
Palabras clave: Telemedicina, Hernia diafragmática congenital, SARS-CoV-2, COVID-19, Seguimiento
Introduction
Coronavirus disease 2019 (COVID-19), caused by a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged from China in December 2019.1, 2 Patients with comorbidities are considered vulnerable to infection and acquiring complications associated with it, to the date there is no data in congenital diaphragmatic hernia (CDH) patients. The lack of knowledge of SARS-CoV-2 affects the pediatric population, especially lung disease patients, more specifically concerning CDH patients and their families. Lately, children with COVID-19 have been reported to be asymptomatic or with mild clinical symptoms compared to adults.3, 4, 5
On the other hand, outpatient follow up has been severely affected by the pandemic. Awareness of the importance of long term multidisciplinary follow-up of CDH survivals has increased with the years. As a result, several follow-up programs were brought to life worldwide6 but none of them included telematic monitoring.
Previously, a temporary and rapid pivotal change to telehealth has been shown to be useful and efficient for delivering healthcare to pediatric patients in disaster situations.7 Which the changes in the lifestyle of our population and medical care due to COVID-19 could be comparable to.
Our aim is to know how SAR-CoV-2 has affected patients with CDH and their caregivers and also to evaluate their satisfaction with the introduction of telematic follow-up during the COVID 19 pandemic.
Material and methods
From 15th November, 2020 to 15th December, 2020 a telephone survey was conducted by the Neonatal Surgery Unit of the Department of Pediatric Surgery, using an institutional patient database. It consists of one hundred consecutive family members of patients with congenital diaphragmatic hernia, aged between 1 and 16 years, who were operated and followed up The ethical clearance for this study was taken from the Clinical Research Ethics Committee of Research Institute vide letter number 239283/01.01.2021.
Excluded patients were those who were either operated in our center but not followed up, who did not answer to repeated telephone calls (or we had no access to their telephone contact number), who were followed up less than 6 months or those who died before the start of this study.
Telephone calls were conducted by independent staff who do not follow up these patients in the outpatient care center. Each interview lasted approximately 10 min. Participants were informed that the survey was related to medical and personal issues and was carried out once verbal consent to proceed was obtained.
Time period for which these surveys were conducted was 31st January 2020, first case of SARS-CoV-2 declared in Spain, till the start of the study on 15th November 2020.
The survey consisted of several sections such as demographics, information about SARS-CoV-2 infection, changes in the lifestyle and anxiety related to having a CDH survival family member during the pandemic. Questions concerning follow-up assessment included evaluation of the telematic follow-up and preferences for future controls. The evaluation of the telematic consultation was done by a scale of 1–5 (1 being “not useful” and 5 “similar to presential”).
Statistical analysis was performed using Stata 13.1 (StataCorp, College Station, TX).
The categorical variables were represented as absolute and relative frequencies (%). The continuous variables were expressed as average and standard deviation. The Chi square or Fisher tests were used to compare categorical variables. The Kolmogorov–Smirnov test was performed to assess the normal distribution of continuous variables. Continuous variables of non normal distribution were compared using Mann–Whitney's U test and those of normal distribution with Student's t test. Multivariate analysis was not necessary for this study. Those differences in which p < 0.05 were considered significant.
Results
Eighty one telephonic surveys were carried out of 100 consecutive patients who were controlled and due an active follow-up during the study period. No refusal to carry out the survey in any patient contacted was registered. In 75.3% the mother was the surveyed caregiver. The mean number of cohabitants in the family house was 4 ± 1 SD. Three patients (3.7%) reported changes in their baseline status, two of them reported improvement (reduction of the number of bronchitis episodes) that they attributed to isolation.
There were 30 contacts with SARS-CoV-2 patients reported (30/81, 37%). In 44.8% the contact occurred in the school, in 27.6% of the cases with cohabiting family members and in 20.7% with non cohabiting family members. There were no differences in the different age groups (<3 years, 3–6 years, 6–12 years and >12 years). Four infection cases were confirmed (4/81, 4.9%), two of them symptomatic (fever, muscular pain and gastrointestinal symptoms). None of the patients required hospital admission.
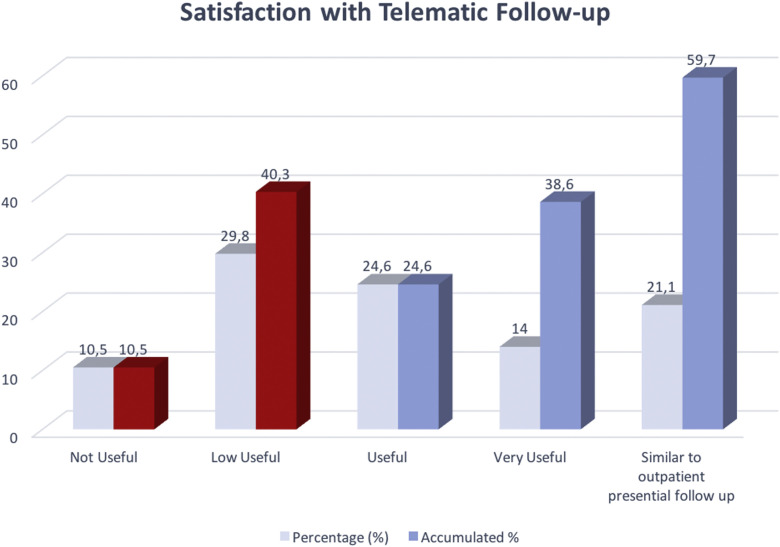
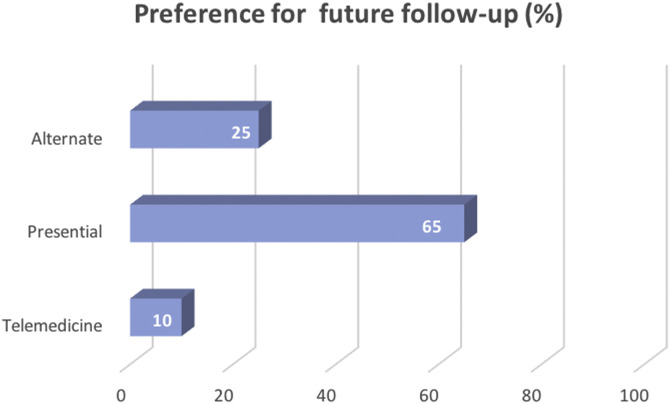
In 32 patients (39.5%) there was a change in the planned follow-up date of the outpatient visit. In 40 patients (49.4%) the outpatient visit was carried out telematically (through telephone call). The mean score for telematic follow up was 3.1 ± 1.3 out of 5. Only 21% of the surveyed evaluated it as similar to face to face [Fig. 1 ]. For future controls 65% of them preferred face-to-face follow up, 25% of them preferred to alternate between in person and telematic and 10% of them preferred exclusively telematics [Fig. 2 ]. There were no significant differences between follow-up preferences and different age groups.
Figure 1.
Satisfaction with the telematic follow-up. The percentage of each answer is represented in light blue. The cumulative percentage of negative assessment (1 and 2) is represented in red. The cumulative percentage of positive assessment (3–5) is represented in dark blue.
Figure 2.
Preference for future follow-up (%).
During this period 50.6% of the surveyed reported greater anxiety. To the question: “Do you think your life has changed differently than it would have changed if your child did not have a congenital diaphragmatic hernia?” 34.6% (28/81) answered yes. The actions most commonly taken were to extreme isolation measures and temporarily prolong it. These changes were significantly higher in the group of patients aged between 3 and 6 years (p < 0.05).
Discussion
This study shows how the pandemic caused by SARS-CoV-2 has affected families and patients with congenital diaphragmatic hernia and their follow-up. It also provides an initial vision of the telematic follow-up of these patients and how we can incorporate it into the current scheme of follow-ups.
Even though SARS-CoV-2 can affect all age groups, children with COVID-19 have been reported to be asymptomatic or with mild clinical symptoms compared to adults.3, 8 Many of these studies refer to the general effects of COVID-19 in the pediatric population but there is no data in regards to different pathological groups like pediatric pneumopathies and especially in congenital diaphragmatic hernia. Goldshtrom et al present a series of seven neonates with congenital malformations, one of them with congenital diaphragmatic hernia, born of mothers affected by COVID-19. Infants SARS-CoV-2-PCR (nasal swab) was negative in all of them, all seven neonates followed a hospital course that appeared comparable to patients with similar diagnoses in the pre-pandemic era.9 There are not scientific literature that explicitly mention Congenital Diaphragmatic Hernia and COVID-19.
Although our survey is not an epidemiological study, only 4 patients (4.9%) were confirmed infection cases (positive SARS-CoV-2-PCR). Those who presented any symptoms were mild and none of them required a hospital admission. Yasuhara et al conducted a systematic review of the clinical characteristics of COVID-19 in children. In that review of 46 case reports and case series with 114 pediatric patients who had a confirmed SARS-CoV-2 infection, they demonstrated that the main clinical features of COVID-19 in children were mild respiratory symptoms including fever, cough, rhinorrhea or no symptoms at all. Dyspnea was more common in infants as compared to the other age groups and gastrointestinal symptoms including diarrhea and vomiting were reported in the older age group.4
Survivors of congenital diaphragmatic hernia have a high incidence of morbidity. Variability in follow-up practices between institutions may affect perception of disability and standardization of follow-up practices is essential.10 Many authors emphasize the importance of multidisciplinary follow-up of these patients. It is well recognized that CDH survivors suffer from morbidities related to their under-lying pathophysiology (pulmonary hypoplasia), but other significant morbidities also result from their neonatal intensive care period. They discuss the clinical strategies to support CDH survivors through the implementation of multidisciplinary follow-up and registries.6, 11, 12 Surgical complications in CDH survivors are common, the high incidence of late surgical morbidity underscores the essential role of the pediatric surgeon in the long-term surveillance and management of these patients.13
With the emergence of Coronavirus Disease 2019 (COVID-19) and its spreading around the world, health-care systems have been seriously affected, impacting not only those affected by SARS-CoV-2, but on a broader scale to all users and workers of these health systems. The standard clinical activity changed drastically being impossible to provide outpatient visits or diagnostic exams except for emergencies. Telemedicine has been encouraged and employed in order to cope with this disruption, email and phone calls with patients and their families emerged as an alternative to follow these patients.14, 15, 16
The use of telemedicine, understood as care of patients and remote monitoring through the use of information technology (cell phones, email, computers or other electronic devices) had already been carried out in pediatric surgery after select surgical procedures in normal conditions. Telephone follow-up offers several advantages such as more efficient use of time and increased accessibility to postoperative care for the family, decreased use of clinic space and resources and potential major cost savings for the institution without sacrificing patient safety.17 In this work a satisfaction survey was performed with families at the time they received their postoperative phone call with 93% reporting being satisfied with the process compared with making a clinic appointment. In our survey this satisfaction rate with the telematic follow-up was 60% (rating of 3 or more out of 5). These differences observed may be due to the fact that the pathology being followed in our case is of higher complexity, the survey was performed during a global pandemic and this change in follow-up from had to be made unexpectedly without any prior information or notification to the patient or their family.
Telemedicine in response to natural disasters in pediatric patients has also been described, Murren-Boezen et al. suggest that telemedicine platforms can deliver efficient health care to children in need of services during the course of extreme weather events and should be considered and incorporated into national disaster preparedness plans as alternatives for patients who may not have access to their medical homes.7 Our study differs from this type of situation because we are not evaluating the need for hospital medical care, but it is similar in the limitations of access to the hospital during the pandemic.
The implementation of telemedicine during the COVID-19 pandemic has been a reality, health systems around the globe have put this way of understanding medicine into practice to provide such needed healthcare that otherwise could not have been possible to offer. In this context, several challenges remain for telemedicine to be used worldwide and be integrated into the public health systems responding to COVID-19 and future outbreaks not only in the context of public health emergencies but also as a strategy and operational plan guiding health care providers to switch to outpatient teleconsultations and increase tele-expertise and remote patient monitoring.14 Multiple specialties like traumatology, neurology and pediatric otolaryngology have put into practice the use of telemedicine for the outpatient follow-up of their patients with the idea of incorporating it into future clinical practice.15, 16, 18 Limited physical exam presents a challenge, however, with adequate information and preparation of the parents and the physicians some of these obstacles can be overcome.15 Our study is the first to assess the implementation of telemedicine in pediatric surgery, more specifically in congenital diaphragmatic hernia as a consequence of the COVID-19 pandemic.
Another of the issues assessed in our study was the anxiety and the perception of risk of the relatives of patients with congenital diaphragmatic hernia, as well as the changes adopted in their lifestyle due to the pandemic. In our case, half of those responding had anxiety to a greater or lesser degree. They adopted more extraordinary measures than they would have if they had not had a family member with CDH. These issues have previously been raised in other pandemics, although their impact is not comparable to the one of COVID-19. Leung et al. documented the psychosocial impact of severe acute respiratory syndrome (SARS) during the peak of the 2003 Hong Kong epidemic and showed that individuals who had a heightened sense of risk perception, as well as moderate anxiety levels, were more likely than others to take personal protective measures against infection.19 The literature on severe acute respiratory syndrome suggests that people may be more likely to comply with health related recommendations if they perceive a high likelihood that they may be affected by the outbreak or they perceive that the illness has severe consequences. Higher levels of anxiety or worry may be associated with an increase in behavioral changes.20, 21
Our study has several limitations, there may be a selection bias given it is a telephone survey, the implementation of telemedicine has been carried out not in a programmed plan but motivated by the pandemic restrictions, the assessment of anxiety and risk perception has not followed reviewed, validated nor standardized scales for this purpose.
Conclusions
In conclusion, the impact of COVID-19 in patients with congenital diaphragmatic hernia has not been greater than in the general pediatric population. Even though it has affected the perception of risk in their family members and produced lifestyle changes, increasing isolation measures given the condition. The incorporation of the telematic follow-up visit was valued good but not comparable to presential, this limitation can be solved by improving telematic visit format and preparing both the family and the medical professionals for its use.
Level of Evidence: V
Ethical clearance
The ethical clearance for this study was taken from the Clinical Research Ethics Committee of the Vall d́Hebron Research Institute vide letter number VHIR/239283/01.01.2021
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Authors declare that there is no conflict of interest involved.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan J.F.W., Yuan S., Kok K.H., To K.K., Chu H., Yang J., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet Lond Engl. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 4.Yasuhara J., Kuno T., Takagi H., Sumitomo N. Clinical characteristics of COVID-19 in children: a systematic review. Pediatr Pulmonol. 2020 doi: 10.1002/ppul.24991. Published online July 29. [DOI] [PubMed] [Google Scholar]
- 5.Liguoro I., Pilotto C., Bonanni M., Ferrari M.E., Pusiol A., Nocerino A., et al. SARS-CoV-2 infection in children and newborns: a systematic review. Eur J Pediatr. 2020;179:1029–1046. doi: 10.1007/s00431-020-03684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morini F., Valfrè L., Bagolan P. Long-term morbidity of congenital diaphragmatic hernia: a plea for standardization. Semin Pediatr Surg. 2017;26:301–310. doi: 10.1053/j.sempedsurg.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Murren-Boezem J., Solo-Josephson P., Zettler-Greeley C.M. A pediatric telemedicine response to a natural disaster. Telemed J E-Health Off J Am Telemed Assoc. 2020;26:720–724. doi: 10.1089/tmj.2019.0100. [DOI] [PubMed] [Google Scholar]
- 8.de Winter J.P., De Luca D., Tingay D.G. COVID-19 surveillance for all newborns at the NICU; conditio sine qua non? Eur J Pediatr. 2020;179:1945–1947. doi: 10.1007/s00431-020-03773-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldshtrom N., Vargas D., Vasquez A., Kim F., Desai K., Turner M.E., et al. Neonates with complex cardiac malformation and congenital diaphragmatic hernia born to SARS-CoV-2 positive women – a single center experience. World J Pediatr Congenit Heart Surg. 2020;11:697–703. doi: 10.1177/2150135120950256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Safavi A., Synnes A.R., O’Brien K., Chiang M., Skarsgard E.D., Chiu P.P. Multi-institutional follow-up of patients with congenital diaphragmatic hernia reveals severe disability and variations in practice. J Pediatr Surg. 2012;47:836–841. doi: 10.1016/j.jpedsurg.2012.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Chiu P.P.L., Ijsselstijn H. Morbidity and long-term follow-up in CDH patients. Eur J Pediatr Surg. 2012;22:384–392. doi: 10.1055/s-0032-1329412. [DOI] [PubMed] [Google Scholar]
- 12.Peetsold M.G., Heij H.A., Kneepkens C.M.F., Nagelkerke A.F., Huisman J., Gemke R.J.B.J. The long-term follow-up of patients with a congenital diaphragmatic hernia: a broad spectrum of morbidity. Pediatr Surg Int. 2009;25:1–17. doi: 10.1007/s00383-008-2257-y. [DOI] [PubMed] [Google Scholar]
- 13.Jancelewicz T., Chiang M., Oliveira C., Chiu P.P. Late surgical outcomes among congenital diaphragmatic hernia (CDH) patients: why long-term follow-up with surgeons is recommended. J Pediatr Surg. 2013;48:935–941. doi: 10.1016/j.jpedsurg.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanham N.S., Bockelman K.J., McCriskin B.J. Telemedicine and orthopaedic surgery: the COVID-19 pandemic and our new normal. JBJS Rev. 2020;8:e2000083. doi: 10.2106/JBJS.RVW.20.00083. [DOI] [PubMed] [Google Scholar]
- 16.Pasca L., Zanaboni M.P., Grumi S., Totaro M., Ballante E., Varesio C., et al. Impact of COVID-19 pandemic in pediatric patients with epilepsy with neuropsychiatric comorbidities: a telemedicine evaluation. Epilepsy Behav. 2020:107519. doi: 10.1016/j.yebeh.2020.107519. Published online November 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fischer K., Hogan V., Jager A., von Allmen D. Efficacy and utility of phone call follow-up after pediatric general surgery versus traditional clinic follow-up. Perm J. 2015;19:11–14. doi: 10.7812/TPP/14-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belcher R.H., Phillips J., Virgin F., Werkhaven J., Whigham A., Wilcox L., et al. Pediatric otolaryngology telehealth in response to COVID-19 pandemic: lessons learned and impact on the future management of pediatric patients. Ann Otol Rhinol Laryngol. 2020 doi: 10.1177/0003489420976163. 3489420976163. Published online November 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung G.M., Lam T.H., Ho L.M., Ho S.Y., Chan B.H., Wong I.O., et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57:857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubin G.J., Amlôt R., Page L., Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339:b2651. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26:136–145. doi: 10.1037/0278-6133.26.2.1. [DOI] [PubMed] [Google Scholar]