Abstract
This study was conducted to determine the efficacy of a customized mandibular advancement device (MAD) in the treatment of obstructive sleep apnea (OSA). Eight patients (M = 3; F = 5; mean age = 56.3 ± 9.4) with a diagnosis of OSA confirmed by polysomnography (PSG) were recruited on the basis of the following inclusion criteria: apnea-hypopnea index (AHI) > 5, age between 18 and 75 years, body mass index (BMI) < 25, and PSG data available at baseline (T0). All were treated with the new NOA® MAD by OrthoApnea (NOA®) for at least 3 months; PSG with NOA in situ was performed after 3 months of treatment (T1). The following parameters were calculated at T0 and T1: AHI, supine AHI, oxygen desaturation index (ODI), percentage of recording time spent with oxygen saturation <90% (SpO2 < 90%), and mean oxygen desaturation (MeanSpO2%). Data were submitted for statistical analysis. The baseline values were AHI = 21.33 ± 14.79, supine AHI = 35.64 ± 12.80, ODI = 17.51 ± 13.5, SpO2 < 90% = 7.82 ± 17.08, and MeanSpO2% = 93.45 ± 1.86. Four patients had mild OSA (5 > AHI < 15), one moderate OSA (15 > AHI < 30), and three severe OSA (AHI > 30). After treatment with NOA®, statistically significant improvements in AHI (8.6 ± 4.21) and supine AHI (11.21 ± 7.26) were recorded. OrthoApnea NOA® could be an effective alternative in the treatment of OSA: the device improved the PSG parameters assessed.
Keywords: obstructive sleep apnea, mandibular advancement devices, polysomnography
1. Introduction
Obstructive sleep apnea (OSA) is a breathing disorder characterized by repeated collapse, total or partial, of the upper airway during sleep [1]. A recent systematic review indicated that OSA may affect nearly 1 billion adults aged 30–69 years, and the number with moderate to severe OSA was estimated to be almost 425 million [1]. However, most cases of OSA remain undiagnosed and untreated [1].
Treatments for OSA include the use of continuous positive airway pressure (CPAP) devices that, by blowing air into the upper airway, reverse the collapse and end the apnea event [2]. Although CPAP remains the gold standard treatment in moderate-to-severe OSA, the use of a mandibular advancement device (MAD) is also considered effective, especially in mild-to-moderate OSA and in cases of low adherence to CPAP therapy [2]. A MAD increases the upper airway space and reduces the risk of obstruction by pulling the jaw and tongue forward. The method has been shown to reduce by 50% the number of PSG-detected apnea-hypopnea events per hour (i.e., the apnea-hypopnea index, AHI) and achieve higher patient compliance compared with CPAP [3].
A MAD can be prefabricated or custom-made. Customized devices are titratable and have been reported to show higher comfort and compliance [3,4,5,6]. They have also been shown to be more effective and stable [3,7,8]. Vanderveken et al., comparing the efficacy of a customized versus a prefabricated device, found greater compliance and effectiveness with the custom-made appliance, while the thermoplastic MAD did not obtain a therapeutic effect due to lack of retention and lower comfort for the patients [4].
In the present study, a new MAD is evaluated. MAD is a custom-made, two-piece device designed using CAD-CAM technology to be smaller and less cumbersome than existing devices. It is designed for the individual patient on the basis of a detailed mandibular kinematic evaluation. It allows titration of the protrusive movement and can be reinforced for patients with bruxism. Since the relationship between the degree of mandibular protrusion and mouth opening influences the efficacy of this treatment, MAD is designed to ensure effective protrusion associated with reduced muscular discomfort.
This study aims to evaluate the effectiveness of new MAD in the treatment of OSA.
The null hypothesis is that the new appliance is not associated with a significant improvement of the selected PSG parameters.
2. Materials and Methods
2.1. Patient Selection
The study was approved by the Unit Internal Review Board (17-1023).
All the patients involved in the study were selected by a dentist with expertise in sleep medicine on the basis of medical, psychological, and dental criteria. Individuals aged between 18 and 75 years with a body mass index (BMI) < 25, an AHI > 5, and a PSG-confirmed diagnosis of mild to severe OSA were eligible; all had previously refused CPAP treatment [9].
All prospective participants underwent a complete history and physical examination. Those with an unsuitable stomatognathic situation (fewer than 8 teeth per arch, temporomandibular disorder, periodontitis), central sleep apnea, or cardiovascular diseases were excluded. Pregnancy (from the third month of pregnancy to three months after delivery) was a further exclusion criterion.
In order to evaluate patient satisfaction, each step of the protocol was followed by the administration of a detailed questionnaire collecting information about symptoms, perception of treatment efficacy, side effects (rated in terms of frequency and severity), and adherence to the treatment. The questionnaire also included the Epworth Sleepiness Scale and the Berlin Questionnaire to assess snoring, daytime sleepiness, fatigue, hypertension, and BMI.
Baseline PSG (T0) was compared with PSG after 3 months with the appliance in situ (T1), focusing on the following PSG respiratory parameters: AHI (mean number of apnea and hypopnea events per hour of sleep), supine AHI (mean number of apnea and hypopnea events per hour of sleep in the supine position), oxygen desaturation index (ODI), mean oxygen saturation (MeanSpO2), and hypoxemia index, i.e., the percentage of recording time spent with oxygen saturation <90% (SpO2 < 90%).
Patients read and signed an informed consent document prior to being enrolled in this study.
Sample: Eight patients with symptomatic OSA met the study criteria and were enrolled. They were prevalently females (5 females, 3 males) and generally middle aged (mean age: 56.25 ± 9.75 years). OSA was mild (5 ≥ AHI < 15), moderate (15 ≥ AHI < 30), and severe (AHI ≥ 30) in 4, 1, and 3 patients, respectively. At T0, the patients’ mean respiratory variables were AHI: 21.33 ± 14.79, Supine AHI: 35.64 ± 12.80, ODI: 17.51 ± 13.5, SpO2 < 90%: 7.82 ± 17.08, MeanSpO2: 93.45 ± 1.86.
2.2. Device
The oral appliance chosen for this study was NOA® by OrthoApnea, a new titratable, custom-made, two-piece MAD with interconnected vertical extensions. The appliance comprises a maxillary bite and several mandibular bites that allow for sequential degrees of protrusion. The device is made of polyamide-12 through 3D printing with CAD-CAM technology, which allows reducing its size. NOA® allows the patient a wide range of jaw movements (Figure 1).
Figure 1.
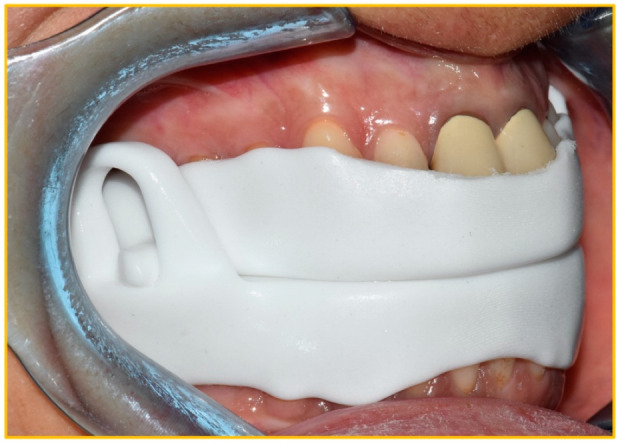
The device worn by the patient.
2.3. Study Design
The first step of the protocol consisted of all the preliminary medical, dental, and neurological analyses, including evaluation of baseline PSG data and administration of questionnaires. TMJ clinical examination according to DC/TMD Axis I was performed [10]. Disease severity was defined by the AHI.
In the second step, eligible patients were treated with NOA® to test their tolerance of the device and, therefore, their likely response to this MAD therapy.
An initial habituation period was envisaged during which the patient kept the device in their mouth for short periods of time while awake. Thereafter, the device was put in at bedtime and worn throughout the night. Advancement (titration protocol) was progressively activated by the dentist until clinical resolution of subjective symptoms [11].
A follow-up PSG with NOA® in situ was performed after 3 months of treatment [12,13].
Statistical analysis: Descriptive statistics (mean, standard deviation, median, minimum and maximum values) were calculated. The normality of the data was calculated using the Kolmogorov-Smirnov test. Subsequently, to analyze the results obtained with the NOA®, paired Student t-tests were performed to compare AHI, supine AHI, ODI, SpO2 < 90%, and MeanSpO2% between T0 and T1. For all tests, the level of significance was set at p < 0.05.
3. Results
Efficacy of the OrthoApnea NOA® Device
Eight patients (3 males, 5 females; mean age: 56.25 ± 9.75 years) consented to use the device. Their respiratory index values at T0 were AHI: 21.33 ± 14.79, supine AHI: 35.64 ± 12.80, ODI: 17.51 ± 13.5, SpO2 < 90%: 7.82 ± 17.08 and MeanSpO2: 93.45 ± 1.86. Four had mild (5 ≥ AHI < 15), one moderate (15 ≥ AHI < 30), and three severe (AHI ≥ 30) OSA (Table 1).
Table 1.
Characteristics of the whole population at baseline (T0).
| Number of patients | 8 |
| Males | 3 |
| Females | 5 |
| Age, mean ± SD | 56.25 ± 9.75 |
| OSAS severity, number of patients | |
| Mild (5 ≥ AHI < 15) | 4 |
| oderate (15 ≥ AHI < 30) | 1 |
| Severe (AHI ≥ 30) | 3 |
| AHI | 21.33 ± 14.79 |
| Supine AHI | 35.64 ± 12.80 |
| ODI | 17.51 ± 13.5 |
| SpO2 < 90% | 7.82 ± 17.08 |
| MeanSpO2% | 93.45 ± 1.86 |
Two patients considered the device uncomfortable and decided not to continue with the therapy.
The remaining six patients were analyzed both at T0, before the treatment started, and after a minimum 3-month treatment with the device (T1) (Table 2).
Table 2.
Short-term effects of the appliance on respiratory variables in the six patients who continued with the therapy.
| T0 | T1 | p | |
|---|---|---|---|
| AHI | 21.33 ± 9.75 | 8.6 ± 4.21 | 0.008 |
| Supine AHI | 35.64 ± 12.80 | 11.21 ± 7.26 | 0.002 |
| ODI | 17.51 ± 13.5 | 8.81 ± 4.59 | 0.07 |
| SpO2 < 90% | 7.82 ± 17.08 | 0.66 ± 1.43 | 0.17 |
| MeanSpO2 | 93.45 ± 1.86 | 93.66 ± 1.03 | 0.82 |
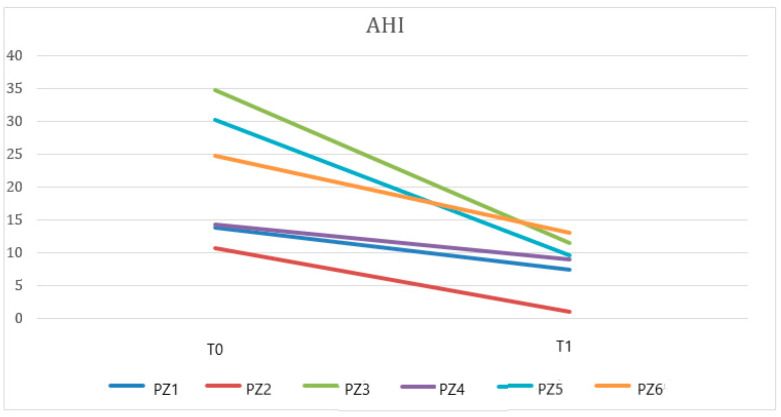
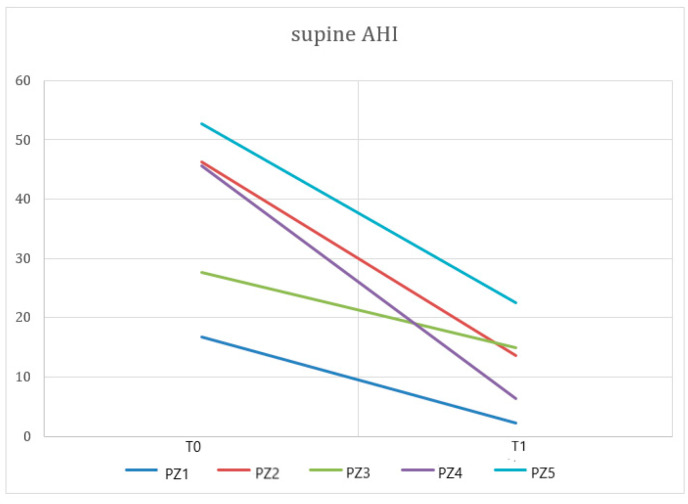
Paired t-tests showed statistically significant differences in AHI at T0 vs. T1 (Figure 2) or in supine AHI at T0 vs. T1 (p < 0.05) (Figure 3). No statistically significant differences were found in ODI, SpO2, and SpO2 < 90%. Table 2 details the short-term effects of treatment with NOA® on the PSG respiratory parameters analyzed.
Figure 2.
A paired data t-test showed a significant difference between AHI at T0 and T1 (p < 0.05) when evaluating data from patients (PZ) treated with the OrthoApnea NOA® device.
Figure 3.
A paired data t-test showed a significant difference between supine AHI recorded at T0 and T1 (p < 0.05) in patients (PZ) using the OrthoApnea NOA® device.
Regardless of the severity of their OSA, all six patients met the AHI and supine AHI criteria defining treatment success. In supine AHI, they showed reductions ranging from −17% to −86% and in AHI from −37% to −91% (Table 3).
Table 3.
Short-term effects of the appliance: changes in AHI and supine AHI.
| Patients | Changes in AHI T0–T1 | Changes in Supine AHI T0–T1 |
|---|---|---|
| 1 | −46% | −75% |
| 2 | −91% | −86% |
| 3 | −67% | −17% |
| 4 | −37% | −46% |
| 5 | −68% | −86% |
| 6 | −47% | −57% |
One patient was reported to have AHI and supine AHI values < 5, which were considered non-pathological.
4. Discussion
Recent years have seen a growing interest in OSA in different fields of medicine due to its considerable prevalence [14] and its important role as a risk factor for cardiovascular and metabolic disorders [15].
Although CPAP remains the gold standard treatment for OSA [16,17], MAD treatment has emerged as an increasingly valuable alternative on account of its higher compliance and remarkable effectiveness in mild-to-moderate cases. MAD treatment is widely reported to reduce the severity of several OSA parameters in the long term, such as the AHI, ODI, and minimum oxygen saturation [18,19,20]. Improvements in daytime sleepiness and subjective perception of snoring were reported in several studies [8,21,22,23,24,25]. Although CPAP therapy was found to be more effective in reducing daytime sleepiness in the long term [24], MAD treatment achieved better therapeutic compliance [26,27,28]; instead, the two methods proved comparable in terms of improved quality of life, cognitive performance, and physical function, also in the long term.
For these reasons, further research into MAD treatment appears warranted.
The wide variability in the response to treatment needs a strict control in each phase of the therapy [29,30,31]. The literature proposes different methods to distinguish responders and not responders, among which DISE-SAM protocol [32] and trial MAD [13]. Adequate follow-up [20,33,34] is essential for evaluating the efficacy of the therapy as well as for monitoring side effects related to long-term MAD use. The present study aims to test a definitive MAD that introduces the concept of maximum customization. NOA®, by OrthoApnea, is a two-piece, custom-made device designed using CAD-CAM technology. The appliance offers the possibility to titrate the protrusive movement, which is crucial for maximizing the therapeutic effect; furthermore, NOA® is designed for the individual patient on the basis of a detailed mandibular kinematic evaluation in order to achieve maximum comfort and compliance.
The results of our study showed statistically significant changes in AHI and supine AHI values at T1 compared with T0 (p < 0.05). Conversely, no statistically significant changes were found in ODI scores (p > 0.05), SpO2 < 90%, or MeanSpO2% (p > 0.05) (Table 2).
According to the literature, a MAD can be considered effective if it leads to an at least 50% reduction in the AHI [21,35]. The NOA® by OrthoApnea met this criterion, leading to statistically significant improvements (reductions) of around 59% in both AHI and supine AHI. A review by Marklund et al. [21] found that MAD treatment reduced AHI values by at least 50%: the treatment was deemed successful (success being defined as an AHI < 5) in 17–75% of patients, while AHI values < 10 were reported in 30–94% of the patients in all the studies considered. De Britto Texeira and colleagues [36] reported that thanks to the use of a suitably modified twin block device, 47% of their OSA sample obtained a 50% reduction in AHI, while in 26%, the parameter returned to normal values. In a study conducted by Duràn-Cantolla [24], 47% of the sample obtained a significant reduction in AHI. Overall, the patients in this study quickly adapted to the NOA®; in one case, treatment adherence was undermined by discomfort associated with the device, while a further patient used the device incorrectly and therefore failed to follow the therapeutic protocol. These findings underline the importance of considering the influence of patient-dependent variables, above all compliance, which is decisive in achieving therapeutic success.
The literature agrees that the side effects initially associated with MAD use are mostly transient and can be resolved simply by modifying certain features of the device. In several studies, the side effects associated with the initial phase of MAD therapy did not lead to discontinuation of the treatment by the patient. In the sample examined by Milano and colleagues [25], for example, some patients experienced side effects in the first month of treatment, such as temporomandibular joint discomfort, difficulty chewing in the morning, and dental tenderness; however, none of these problems precluded continued use of the device.
The literature shows that personalized devices, such as NOA® by OrthoApnea, are associated with greater patient-perceived comfort and better therapeutic outcomes than prefabricated devices, these better outcomes being a result of greater adherence to the treatment. According to an AADMS (American Academy of Dental Sleep Medicine) report, systematic reviews have shown that personalized devices compare better to prefabricated non-customizable ones. Partly because they provide more significant and better retention, they are able to keep the jaw in a more stable position; consequently, they are more effective and comfortable [37]. Guidelines on the clinical management of OSAS with oral devices, published by the AADMS [3], recommend the prescription of a personalized and titratable MAD rather than the prefabricated, non-titratable type. The literature evidence shows that the former type is more effective than the latter in improving AHI and other cardiorespiratory parameters. The 2014 TOMADO crossover study [5] compared the efficacy of three different types of monoblock MAD in a sample of 90 patients. Although the three types gave positive and comparable results, the non-personalized thermoplastic device was the least comfortable due to poorer retention; this led to lower therapeutic adherence compared with the semi-personalized and personalized devices.
In our study, 75% of the sample treated with NOA® accepted the device and followed the treatment protocol without experiencing the problems commonly related to the use of MADs. This could be due to the refined, customized design of this device outlined above. However, to confirm this scientifically, it would be necessary to compare NOA® with other custom-made MADs and enlist a larger sample of patients.
Mandibular advancement devices are capable of improving health and quality of life, including social life [6,26], and thanks to their therapeutic efficacy in treating severe OSAS, MAD therapy is suitable for all patients refusing CPAP. A meta-analysis conducted by Schwartz [26] in 2018 showed a difference in treatment compliance between the two therapies: with CPAP, it was 1.1 h per night lower than with MAD (p = 0.004). This explains why CPAP does not show significant quality-of-life improvements compared with MAD therapy, specifically significantly improved cognitive and functional results. This is despite CPAP being more effective in improving cardiorespiratory parameters.
The present study does not have enough data to obtain statistically significant results regarding the follow-up of the patients beyond the 3-month (T1) assessments. However, numerous studies in the literature attest to the effectiveness of personalized MADs in improving OSAS symptoms over time [18,19,21,31]. The most significant studies in this regard include one conducted by Uniken Venema and colleagues in 2020 [20]. These authors set out to compare the long-term effectiveness of CPAP and MAD in patients with OSAS through evaluation of the effects of treatments over ten years. Polysomnography results showed a favorable outcome of both therapies at ten years: the mean AHI in the MAD group was 9.9 ± 10.3 events/h, versus 3.4 ± 5.4 events/h in the CPAP group. Both therapies led to a substantial improvement in self-reported neurobehavioral outcomes at ten years of follow-up. Attali and colleagues [19] also showed that MADs can effectively treat OSAS in the long term, maintaining good compliance and patient satisfaction. Their study, conducted in a sample of 279 patients with an average age of 58 years and followed up for at least 1000 days, showed that 63% of the sample (at 2.5 years) continued treatment with MAD with adequate efficacy, tolerability, and compliance over time; only in some patients was a recurrence of side effects observed, probably due to the natural course of the disease or to wear and tear of the MAD associated with a loss of therapeutic efficacy.
Limitations and Future Perspectives
Our study was limited mainly by the short follow-up time, the small sample size and the lack of a control group (no treatment/other MAD). These limitations might be overcome by recruiting a larger sample and extending the therapeutic monitoring time, controlling for a series of time-dependent variables. Since OSAS is a chronic disease that can worsen over time, it is important to maintain a constant improvement as the treatment progresses; OSAS is also a risk factor for a series of systemic diseases, meaning that patients’ general health also needs to be monitored. In some cases, clinicians may consider reinforcement of behavioral therapy and sleep hygiene measures in order to address negative habits.
In addition, since there is no standardized titration protocol, it would be appropriate in future research to evaluate whether the level of mandibular advancement determined by the MAD corresponds to the individual therapeutic window. Dieltjens et al. [30] conducted an exhaustive review of the titration techniques in use, especially the “trial and error” method that is currently the most popular. This method involves selecting a particular mandibular protrusion setting and evaluating its side effects and associated benefits, thereafter reaching the individual therapeutic window by process of trial and error. With the OrthoApnea NOA® system, too, the patient is required to follow a protrusive sequence established in advance, in this case, on the basis of individual variables. The device includes a series of lower splints that reproduce the established protrusive line, allowing the patient gradually to reach his/her own most effective level of mandibular advancement. To motivate the patient and enhance the therapeutic alliance, and therefore allow the therapeutic window to be reached, the personalized titration protocol should be carefully explained to the patient.
Finally, the device requires some maintenance since it can deteriorate over time, leading to a reduction in retention, comfort, and therapeutic efficacy. Again, to maintain patient compliance and the effectiveness of the treatment, periodic re-evaluation of the device is recommended so that any necessary modifications or replacements can be made.
5. Conclusions
Treatment with NOA® could be an effective alternative in the treatment of OSAS, having been found to significantly improve some PSG respiratory parameters, specifically AHI and supine AHI, even in cases of severe OSAS (AHI > 15). The other parameters investigated (ODI, SpO2 < 90%, and MeanSpO2) also improved, albeit not significantly. In conclusion, although the statistical data are promising, to establish the potential of the device, further studies are needed.
Author Contributions
Conceptualization, M.S.; methodology, M.S.; software, M.P.; validation, M.S.; formal analysis, G.C.; investigation, G.C.; resources, A.S.; data curation, M.P.; writing—original draft preparation, G.C.; writing—review and editing, A.S.; visualization, M.D.B.; supervision, L.L.; project administration, M.S.; funding acquisition, M.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by the Unit Internal Review Board (17-1023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data are available upon request to the corresponding author.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benjafield A.V., Ayas N.T., Eastwood P.R., Heinzer R., Ip M.S.M., Morrell M.J., Nunez C.M., Patel S.R., Penzel T., Pépin J.L., et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019;7:687–698. doi: 10.1016/S2213-2600(19)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry R.B., Budhiraja R., Gottlieb D.J., Gozal D., Iber C., Kapur V.K., Marcus C.L., Mehra R., Parthasarathy S., Quan S.F., et al. American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2012;8:597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramar K., Dort L.C., Katz S.G., Lettieri C.J., Harrod C.G., Thomas S.M., Chervin R.D. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J. Dent. Sleep Med. 2015;11:773–827. doi: 10.15331/jdsm.4868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vanderveken O.M., Devolder A., Marklund M., Boudewyns A.N., Braem M., Okkerse W., Verbraecken J.A., Franklin K., De Backer W.A., Van de Heyning P. Comparison of a Custom-made and a Thermoplastic Oral Appliance for the Treatment of Mild Sleep Apnea. Am. J. Respir. Crit. Care Med. 2008;178:197–202. doi: 10.1164/rccm.200701-114OC. [DOI] [PubMed] [Google Scholar]
- 5.Sharples L., Glover M., Clutterbuck-James A., Bennett M., Jordan J., Chadwick R., Pittman M., East C., Cameron M., Davies M., et al. Clinical effectiveness and cost-effectiveness results from the randomised controlled Trial of Oral Mandibular Advancement Devices for Obstructive sleep apnoea-hypopnoea (TOMADO) and long-term economic analysis of oral devices and continuous positive airway pressure. Health Technol. Assess. 2014;18:1–296. doi: 10.3310/hta18670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pépin J.L., Raymond N., Lacaze O., Aisenberg N., Forcioli J., Bonte E., Bourdin A., Launois S., Tamisier R., Molinari N. Heat-moulded versus custom-made mandibular advancement devices for obstructive sleep apnoea: A randomised non-inferiority trial. Thorax. 2019;74:667–674. doi: 10.1136/thoraxjnl-2018-212726. [DOI] [PubMed] [Google Scholar]
- 7.Randerath W.J., Verbraecken J., Andreas S., Bettega G., Boudewyns A., Hamans E., Jalbert F., Paoli J.R., Sanner B., Smith I., et al. European Respiratory Society task force on non-CPAP therapies in sleep apnoea. Non-CPAP therapies in obstructive sleep apnoea. Eur. Respir. J. 2011;37:1000–1028. doi: 10.1183/09031936.00099710. [DOI] [PubMed] [Google Scholar]
- 8.Ahrens A., McGrath C., Hägg U. Subjective efficacy of oral appliance design features in the management of obstructive sleep apnea: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2010;138:559–576. doi: 10.1016/j.ajodo.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 9.Levrini L., Sacchi F., Milano F., Polimeni A., Cozza P., Bernkopf E., Segù M. Italian recommendations on dental support in the treatment of adult obstructive sleep apnea syndrome (OSAS) Ann. di Stomatol. 2015;6:81–86. doi: 10.11138/ads/2015.6.3.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skeie M.S., Frid P., Mustafa M., Aßmus J., Rosén A. DC/TMD Examiner Protocol: Longitudinal Evaluation on Interexaminer Reliability. Pain Res. Manag. 2018;2018:7474608. doi: 10.1155/2018/7474608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazemeini E., de Beeck S.O., Vroegop A., Van Loo D., Willemen M., Verbraecken J., Braem M.J., Vanderveken O.M., Dieltjens M. A pilot study on comparison of subjective titration versus remotely controlled mandibular positioning during polysomnography and drug-induced sleep endoscopy, to determine the effective protrusive position for mandibular advancement device therapy. Sleep Breath. 2022:1–9. doi: 10.1007/s11325-022-02569-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaiswal M., Srivastava G.N., Pratap C.B., Sharma V.K., Chaturvedi T. Effect of Oral Appliance for Snoring and Obstructive Sleep Apnea. Int. J. Orthod. (Milwaukee Wis.) 2015;26:67–71. [PubMed] [Google Scholar]
- 13.Segù M., Cosi A., Santagostini A., Scribante A. Efficacy of a Trial Oral Appliance in OSAS Management: A New Protocol to Recognize Responder/Nonresponder Patients. Int. J. Dent. 2021;2021:8811700. doi: 10.1155/2021/8811700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Punjabi N.M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008;5:136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Young T., Palta M., Dempsey J., Skatrud J., Weber S., Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 16.Hoekema A., Stegenga B., Wijkstra P.J., van der Hoeven J.H., Meinesz A.F., de Bont L.G. Obstructive sleep apnea therapy. J. Dent. Res. 2008;87:882–887. doi: 10.1177/154405910808700917. [DOI] [PubMed] [Google Scholar]
- 17.Zhu Y., Long H., Jian F., Lin J., Zhu J., Gao M., Lai W. The effectiveness of oral appliances for obstructive sleep apnea syndrome: A meta-analysis. J. Dent. 2015;43:1394–1402. doi: 10.1016/j.jdent.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Iftikhar I.H., Bittencourt L., Youngstedt S.D., Ayas N., Cistulli P., Schwab R., Durkin M.W., Magalang U.J. Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: A network meta-analysis. Sleep Med. 2017;30:7–14. doi: 10.1016/j.sleep.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 19.Attali V., Chaumereuil C., Arnulf I., Golmard J.-L., Tordjman F., Morin L., Goudot P., Similowski T., Collet J.-M. Predictors of long-term effectiveness to mandibular repositioning device treatment in obstructive sleep apnea patients after 1000 days. Sleep Med. 2016;27–28:107–114. doi: 10.1016/j.sleep.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Uniken Venema J.A.M., Doff M.H.J., Joffe-Sokolova D., Wijkstra P.J., van der Hoeven J.H., Stegenga B., Hoekema A. Long-term obstructive sleep apnea therapy: A 10-year follow-up of mandibular advancement device and continuous positive airway pressure. J. Clin. Sleep Med. 2020;16:353–359. doi: 10.5664/jcsm.8204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marklund M., Verbraecken J., Randerath W. Non-CPAP therapies in obstructive sleep apnoea: Mandibular advancement device therapy. Eur. Respir. J. 2011;39:1241–1247. doi: 10.1183/09031936.00144711. [DOI] [PubMed] [Google Scholar]
- 22.Silva Gomes Ribeiro C.V., Ribeiro-Sobrinho D., Muñoz Lora V.R.M., Morais Dornelas Bezerra L., Del Bel Cury A.A. Association between mandibular advancement device therapy and reduction of excessive daytime sleepiness due to obstructive sleep apnoea. J. Oral Rehabil. 2019;46:1031–1035. doi: 10.1111/joor.12898. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson K.A., Ono T., Lowe A.A., Keenan S.P., Fleetham J.A. A randomized crossover study of an oral appliance vs nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest. 1996;109:1269–1275. doi: 10.1378/chest.109.5.1269. [DOI] [PubMed] [Google Scholar]
- 24.Durán-Cantolla J., Alkhraisat M., Martínez-Null C., Aguirre J.J., Guinea E.R., Anitua E. Frequency of Obstructive Sleep Apnea Syndrome in Dental Patients with Tooth Wear. J. Clin. Sleep Med. 2015;11:445–450. doi: 10.5664/jcsm.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Milano F., Mondini S., Billi M., Gobbi R., Gracco A., Sorrenti G. The impact of a multidisciplinary approach on response rate of mandibular advancing device therapy in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol. Ital. 2013;33:337–342. [PMC free article] [PubMed] [Google Scholar]
- 26.Schwartz M., Acosta L., Hung Y.-L., Padilla M., Enciso R. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: A systematic review and meta-analysis. Sleep Breath. 2017;22:555–568. doi: 10.1007/s11325-017-1590-6. [DOI] [PubMed] [Google Scholar]
- 27.Rotty M.-C., Suehs C.M., Mallet J.-P., Martinez C., Borel J.-C., Rabec C., Bertelli F., Bourdin A., Molinari N., Jaffuel D. Mask side-effects in long-term CPAP-patients impact adherence and sleepiness: The InterfaceVent real-life study. Respir. Res. 2021;22:17. doi: 10.1186/s12931-021-01618-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baratta F., Pastori D., Bucci T., Fabiani M., Fabiani V., Brunori M., Loffredo L., Lillo R., Pannitteri G., Angelico F., et al. Long-term prediction of adherence to continuous positive air pressure therapy for the treatment of moderate/severe obstructive sleep apnea syndrome. Sleep Med. 2017;43:66–70. doi: 10.1016/j.sleep.2017.09.032. [DOI] [PubMed] [Google Scholar]
- 29.García-Campos E., Labra A., Galicia-Polo L., Sánchez-Narváez F., Haro R., Jiménez U., Poblano A. Decrease of respiratory events in patients with obstructive sleep apnea-hypopnea syndrome using a mandibular advancement device assessed with split night polysomnography. Sleep Sci. 2016;9:221–224. doi: 10.1016/j.slsci.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dieltjens M., Vanderveken O.M., Van de Heyning P.H., Braem M.J. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med. Rev. 2012;16:177–185. doi: 10.1016/j.smrv.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Sharples L.D., Clutterbuck-James A.L., Glover M.J., Bennett M.S., Chadwick R., Pittman M.A., Quinnell T.G. Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med. Rev. 2016;27:108–124. doi: 10.1016/j.smrv.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernández-Sanjuán P., Arrieta J.J., Sanabria J., Alcaraz M., Bosco G., Pérez-Martín N., Pérez A., Carrasco-Llatas M., Moreno-Hay I., Ríos-Lago M., et al. Optimizing Mandibular Advancement Maneuvers during Sleep Endoscopy with a Titratable Positioner: DISE-SAM Protocol. J. Clin. Med. 2022;11:658. doi: 10.3390/jcm11030658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sato K., Nakajima T. Review of systematic reviews on mandibular advancement oral appliance for obstructive sleep apnea: The importance of long-term follow-up. Jpn. Dent. Sci. Rev. 2019;56:32–37. doi: 10.1016/j.jdsr.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Almeida F.R., Lowe A.A., Otsuka R., Fastlicht S., Farbood M., Tsuiki S. Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: Part 2. Study-model analysis. Am. J. Orthod. Dentofac. Orthop. 2006;129:205–213. doi: 10.1016/j.ajodo.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 35.Ferguson K.A., Cartwright R., Rogers R., Schmidt-Nowara W. Oral Appliances for Snoring and Obstructive Sleep Apnea: A Review. Sleep. 2006;29:244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 36.De Britto Teixeira A.O., Abi-Ramia L.B., de Oliveira Almeida M.A. Treatment of obstructive sleep apnea with oral appliances. Prog. Orthod. 2013;14:10. doi: 10.1186/2196-1042-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scherr S.C., Almeida F.R., Bennett K.M., Dort L.C., Essick G.K., Katz S.G., McLornan P.M., Phillips K.S., Rogers R.R., Sheats R.D., et al. Definition of an effective oral appliance for the treatment of obstructive sleep apnea and snoring: A report of the American Academy of Dental Sleep Medicine. J. Dent. Sleep Med. 2014;1:39–50. doi: 10.15331/jdsm.3738. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available upon request to the corresponding author.