Abstract
Objectives. To test whether the prevalence of reported psychological distress increased among working-age adults in the United States between 1999 and 2018.
Methods. I examined psychological distress in the past 30 days using the Kessler-6 Distress Scale, completed by 403 223 participants aged 25 to 64 years across 20 annual waves of the National Health Interview Study conducted from 1999 to 2018. I examined overall and demographic-specific trends.
Results. The prevalence of psychological distress in the past 30 days increased from 16.1% in 1999–2000 to 22.6% in 2017–2018, an increase of 6.5 percentage points (95% confidence interval [CI] = 5.6, 7.3) or 40% from 1999–2000 levels. Statistically significant increases in the prevalence of distress were observed across all age, gender, race/ethnicity, and educational attainment subgroups examined. Rates of serious psychological distress increased from 2.7% in 1999–2000 to 4% in 2017–2018, an increase of 1.3 percentage points (95% CI = 0.9, 1.6).
Conclusions. Since 1999, there has been an upward trend in reported psychological distress among working-aged adults in the United States. (Am J Public Health. 2022;112(7):1045–1049. https://doi.org/10.2105/AJPH.2022.306828)
Following a century of progress, life expectancy in the United States plateaued in 2010 and declined from 2015 to 2017.1 This concerning trend has been attributed to an increase in mortality among working-age adults (aged 25–64 years) driven largely by a rise in suicide and drug and alcohol-related causes, which have been collectively labeled “deaths of despair.”2 In the United States, the suicide rate increased by 35% between 1999 and 2018.3 An increase in feelings of distress over this period may provide at least a partial explanation for high and rising mortality rates in the United States.2–4 However, it is unclear whether the recent reversal in life expectancy gains was precipitated by an increase in psychological distress among working-age adults.
A nationally representative study of US adults found that the prevalence of serious psychological distress increased from 3.9% to 4.8% among non-Hispanic Whites aged 45 to 54 years between 1997–1999 and 2011–2013.5 Increases in depressive symptoms and suicidal ideation have been identified across racial/ethnic groups in a US cohort of young adults reaching midlife.6 Finally, a recent study showed that the percentage of US citizens reporting “not good” mental health every day in the past 30 days increased from 3.6% in 1993 to 6.4% in 2019.7
Although these studies suggest a potential increase in distress in recent decades, estimates of national trends in psychological distress across the entire working-age population using well-validated multi-item measures are needed. To address this gap, this study drew on a national sample of working-age adults to test whether the prevalence of psychological distress, measured using the Kessler-6 Distress Scale,8 has changed over 2 decades, from 1999 to 2018.
METHODS
Participants were adults aged 25 to 64 years from 20 waves of the National Health Interview Survey (NHIS), collected from 1999 to 2018. The NHIS is an annual nationally representative probability-based survey of the noninstitutionalized US population with a high household response rate (64%–88%).9
Psychological Distress
I examined psychological distress using the valid and reliable Kessler-6 Distress Scale (K6).8 Participants indicated how frequently they experienced 6 symptoms of psychological distress in the past 30 days:
-
1.
nervous,
-
2.
hopeless,
-
3.
restless or fidgety,
-
4.
so depressed that nothing could cheer you up,
-
5.
that everything was an effort, and
-
6.
worthless.
Responses were provided on a 5-point scale (coded 0 = none of the time, 1 = a little of the time, 2 = some of the time, 3 = most of the time, and 4 = all of the time). K6 scores ranged from 0 to 24 (Cronbach’s α = 0.87). Those scoring 5 or higher were coded as experiencing psychological distress.10 This cutpoint has been identified as optimal in identifying those experiencing at least moderate distress.
I conducted supplementary analyses using a more stringent cutoff of 13 or greater on the K6 scale, typically termed “serious psychological distress.”8 I also examined changes in each individual distress symptom over the study period. Responses were coded as 0 (none of the time) and 1 (a little of the time, some of the time, most of the time, all of the time), indicating the absence or presence of each symptom in the past 30 days.
Statistical Analysis
I used logistic regression analysis followed by the Stata version 17 margins postestimation command (StataCorp LP, College Station, TX) to estimate percentage-point differences in the prevalence of psychological distress and serious psychological distress grouped in 2-year blocks from 1999–2000 to 2017–2018. I conducted additional analyses with survey year treated as a continuous variable. I also conducted sensitivity analyses to test whether adjusting for differences in demographic characteristics between study waves affected the study results and whether changes in distress from 1999–2000 to 2017–2018 differed across demographic groups or distress symptoms. I applied sampling weights to adjust for differential selection into the sample, household nonresponse, and potential bias due to undercoverage, and to provide a poststratification adjustment based on population age, gender, and race/ethnicity levels. All analyses also adjusted for the impact of the sample design stratification and clustering on standard errors. Instructions on how to access the data and code supporting the study are available via the Open Science Framework (https://osf.io/xc7zy).
RESULTS
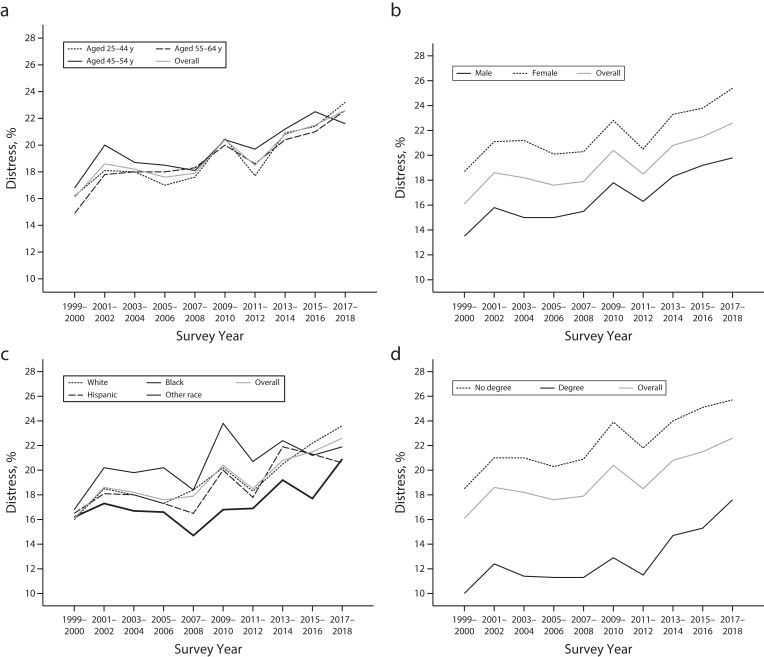
In total, 403 223 participants provided survey responses in the NHIS from 1999 to 2018. In the NHIS, the prevalence of psychological distress increased from 16.1% in 1999–2000 to 22.6% in 2017–2018, an overall increase of 6.5 percentage points (95% confidence interval [CI] = 5.6, 7.3) or 40% (Figure 1; Table A, available as a supplement to the online version of this article at http://www.ajph.org). Analysis of the time trend in distress showed that distress increased by 0.29% (95% CI = 0.26, 0.33) per year on average (Table B, available as a supplement to the online version of this article at http://www.ajph.org). Overall increases in distress between 1999–2000 and 2017–2018 were similar in magnitude for males (6.3%; 95% CI = 5.3, 7.3) and females (6.7%; 95% CI = 5.6, 7.8) and were observed across all demographic groups (Figure 1, Table A). Sensitivity analyses showed that adjusting for differences in demographic characteristics between survey waves increased estimates of change in distress by 22% to 28% (Table B).
FIGURE 1—
Prevalence of Psychological Distress Among Working-Aged Adults as a Function of Participant (a) Age, (b) Gender, (c) Race/Ethnicity, and (d) Educational Attainment: United States, National Health Interview Survey (NHIS), 1999–2000 to 2017–2018
Note. Graphs are based on an analysis of 403 223 NHIS participants. Distress is defined as scoring 5 or higher on the Kessler-6 Distress Scale.8,10
The magnitude of increases in distress did not differ as a function of participants’ gender or education level. However, non-Hispanic White participants experienced a significantly larger increase in distress than Hispanic participants (3.5% difference; 95% CI = 1.5, 5.5) and non-Hispanic Black participants (2.5% difference; 95% CI = 0.3, 4.8; Table C, available as a supplement to the online version of this article at http://www.ajph.org). An analysis of the time trend in distress showed that non-Hispanic White participants experienced a 0.33% (95% CI = 0.29, 0.38) increase on average each year (Table D, available as a supplement to the online version of this article at http://www.ajph.org), which was significantly larger than the 0.22% (95% CI = 0.17, 0.27) increase per year experienced by other participants. Those aged 45 to 54 years experienced a less pronounced increase in distress levels than those aged 25 to 44 years (Tables C and D).
Serious distress levels increased significantly, from 2.7% (95% CI = 2.5, 2.9) in 1999–2000 to 4.0% (95% CI = 3.7, 4.2) in 2017–2018, an increase of 1.3 percentage points (95% CI = 0.9, 1.6; Table E, available as a supplement to the online version of this article at http://www.ajph.org) or 48%. Significant increases in serious distress were observed for all demographic groups examined except for Hispanic and “other race/ethnicity” participants (Table E).
Statistically significant increases were observed for each K6 distress symptom between 1999–2000 and 2017–2018 (Table F, available as a supplement to the online version of this article at http://www.ajph.org). Feeling “that everything was an effort” increased from 20.5% to 30.9%, an increase of 10.4 percentage points (95% CI = 9.3, 11.4) or 50.7%. Feelings of hopelessness increased from 10.2% to 14.3%, an increase of 4.1 percentage points (95% CI = 3.5, 4.8) or 40.2%. Feelings of nervousness, restlessness, and worthlessness also increased substantially (Table F).
DISCUSSION
Rising feelings of distress have been proposed as an explanation for the increases in premature death that have contributed to the recent reversal of life expectancy improvements in the United States.2,3 This study of over 400 000 adults used 2 decades of nationally representative data to show that distress increased by 6.5 percentage points, from 16.1% in 1999–2000 to 22.6% in 2017–2018, an increase of 40%. Significant increases in distress were observed across demographic groups and were found when changes in serious distress were examined.
The population-level rise in psychological distress identified in this study occurred over the same period during which deaths due to mortality from suicides, drug poisonings, and alcoholic liver disease increased among working-age adults in the United States.1,3 The current findings provide support for a premise of studies examining “deaths of despair”: that feelings of distress have increased among working-age adults in the 21st century. Additional empirical evidence is now needed to understand how changes in psychological distress may link to premature mortality from suicide and drug- and alcohol-related causes and their precursors, such as suicidal ideation and dangerous levels of opioid and alcohol usage.4 Further, it will be important to pinpoint the social and economic changes that triggered the recent rise in distress, which may include stagnant wage growth, labor force disengagement, and increased social isolation.11,12
The current study is limited by its reliance on a self-reported measure of general distress that does not provide a clinical diagnosis of specific psychiatric disorders. However, it is the pervasive symptoms of distress (e.g., hopelessness, worthlessness) captured by this measure that have been proposed to link economic stagnation to premature death.11 Finally, because this study relied on reported feelings, it remains possible that the increase in distress observed could be partly attributed to an increased likelihood of reporting distress over the study period (e.g., through greater awareness of mental health issues).
In conclusion, this study drew on repeated assessments of psychological distress from probability-based samples with high response rates collected over 2 decades to show a pronounced upward trend in reported psychological distress among working-aged adults from 1999–2000 to 2017–2018. Understanding the role that this rise in distress has played in connecting changing societal and economic conditions to premature death and reduced life expectancy will now be crucial.
ACKNOWLEDGMENTS
I am grateful to the Centers for Disease Control and Prevention’s National Center for Health Statistics for making available data from the National Health Interview Survey, 1999–2018.
Note. These organizations bear no responsibility for the analysis or interpretation of the data. This research was unfunded.
CONFLICTS OF INTEREST
The author has no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study involved secondary analysis of the National Health Interview Survey anonymized microdata files, which did not require institutional approval from the Maynooth University Social Research Ethics Sub-Committee.
REFERENCES
- 1.Harris KM, Woolf SH, Gaskin DJ. High and rising working-age mortality in the US: a report from the National Academies of Sciences, Engineering, and Medicine. JAMA. 2021;325(20):2045–2046. doi: 10.1001/jama.2021.4073. [DOI] [PubMed] [Google Scholar]
- 2.Case A, Deaton A. Deaths of Despair and the Future of Capitalism. Princeton, NJ: Princeton University Press; 2020. [Google Scholar]
- 3.Hedegaard H, Curtin SC, Warner M. Increase in suicide mortality in the United States, 1999–2018. NCHS Data Brief. 2020;(362):1–8. [PubMed] [Google Scholar]
- 4.Copeland WE, Gaydosh L, Hill SN, et al. Associations of despair with suicidality and substance misuse among young adults. JAMA Netw Open. 2020;3(6):e208627. doi: 10.1001/jamanetworkopen.2020.8627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaydosh L, Hummer RA, Hargrove TW, et al. The depths of despair among US adults entering midlife. Am J Public Health. 2019;109(5):774–780. doi: 10.2105/AJPH.2019.305002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanchflower DG, Oswald AJ. Trends in extreme distress in the United States, 1993–2019. Am J Public Health. 2020;110(10):1538–1544. doi: 10.2105/AJPH.2020.305811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. 2018. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2018/srvydesc.pdf
- 10.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21(2):88–97. doi: 10.1002/mpr.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanahan L, Hill SN, Gaydosh LM, et al. Does despair really kill? A roadmap for an evidence-based answer. Am J Public Health. 2019;109(6):854–858. doi: 10.2105/AJPH.2019.305016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scutchfield FD, Keck CW. Deaths of despair: why? What to do? Am J Public Health. 2017;107(10):1564–1565. doi: 10.2105/AJPH.2017.303992. [DOI] [PMC free article] [PubMed] [Google Scholar]