Abstract
Medical nutrition therapy may have a key role in the COVID-19 pandemic. Given the spread of misinformation, the present review organizes and summarizes nutrition recommendations regarding COVID-19, serving as a reference guide for health professionals. Nineteen official recommendations were included of international, US, Asian, European, Canadian, and Australian origin on (i) lactation, (ii) nutrition during quarantine, (iii) nutrition in high-risk groups, (iv) nutrition for recovery at home, and (v) nutrition in hospital. Breastfeeding is encouraged, and the role of hydration and the adoption of a healthy diet during quarantine are emphasized. Older people and/or people with comorbidities should be checked for malnutrition and follow a healthy diet. For patients recovering at home, hydration, protein, and energy intake should be ensured. For hospitalized patients, early feeding with a priority on enteral route is recommended.
Keywords: coronavirus, COVID-19, hospital, lactation, nutrition, quarantine, recommendations
THE ROLE of nutrition is critical in health and development.1 The relationship between diet and disease is evident in several ways: malnutrition affects the immune system and thus increases susceptibility to disease; vitamin deficiencies or suboptimal intake can worsen or have a causal role in disease; and an unhealthy diet is a predisposing factor for chronic diseases such as cardiovascular disease and cancer.1 Moreover, nutrition seems to be implicated in viral infections.1
Taking the role of nutrition in disease prevention and therapy as a starting point, several considerations can be made on its potential role in the COVID-19 pandemic. Older individuals and/or those with comorbidities, such as diabetes, obesity, cardiovascular disease, lung problems, and kidney and liver diseases, and with special nutrition needs seem to be more vulnerable to the pandemic.2 In parallel, quarantine, which has been applied in most countries as a measure to reduce the transmission of COVID-19, may affect dietary habits, with a trend toward more “comfort” energy- or carbohydrate-dense foods (stress-eating)3 and increase body weight.4 The prolonged duration of such behaviors, if combined with reduction in physical activity, may negatively influence health status.1 Moreover, a special reference should be made to breastfeeding mothers with COVID-195 and nutritional approaches for hospitalized COVID-19 patients6–9 or those recovering at home.10
Despite the increasing scientific evidence regarding the COVID-19 pandemic, concerns have been raised about the high level of misinformation and pseudoscience.11,12 Health professionals (including dietitians and general practitioners) act as key players in the delivery of evidence-based information. In addition, official information regarding nutrition and COVID-19 has been launched from international and national bodies, such as the World Health Organization (WHO),13 the European Society of Clinical Nutrition and Metabolism (ESPEN),6 the American Society for Parenteral and Enteral Nutrition (ASPEN),10 and the European Food Information Council (EUFIC).14
The aim of the present review was to classify/organize nutrition recommendations and summarize key messages from official sources so as to serve as a reference guide for both health professionals and public.
METHODS
Two independent researchers searched PubMed, LitCOVID, and the Web by inserting the search terms “COVID OR coronavirus AND nutrition,” “coronavirus AND nutrition,” “COVID OR coronavirus AND recommendations AND diet.” Moreover, several repositories on COVID and nutrition were searched, that is, European Federation of the Associations of Dietitians (EFAD),15 the Global Resource for Nutrition Practice,16 the Global Nutrition Cluster,17 and the ASPEN Web site.18 Only sources in the English language were considered. After retrieving the selected documents, duplicates were excluded. Articles and reports were screened to identify data that met the eligibility criteria. An effort was made to include recommendations from different geographic areas. However, contributions of smaller regional bodies are not separately referenced because of the immensity and overlapping of information. Recommendations on food safety issues and hand hygiene were not included, since the focus of the present work was on nutrition.
RESULTS
Our results were categorized into 5 sections: (i) lactation, (ii) nutrition during quarantine, (iii) nutrition for disease prevention in high-risk groups, (iv) nutrition for recovery at home, and (v) nutrition in hospital (Table 1).
Table 1. Nutritional Recommendations of International and National Bodies Regarding COVID-19.
| International | United States | Asia | Europea | Australia | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WHO | UNICEF | WFP | ILCA | FAO | CDC | ASN | ASPEN | Academy Nutrition/Dietetics | USDA | Turkish Dietetic Association | Indian Dietetic Association | China National Health Commission | ESPEN | EUFIC | BDA | Canada Dietitians of Canada | Dietitians Association of Australia | Australian Government Department of Health | |
| Lactation/young children | X | X | X | X | ...b | ...c | |||||||||||||
| Healthy nutrition during quarantine | X | Χ | X | X | X | X | X | X | X | X | Χ | X | X | ||||||
| Nutrition for disease prevention in high-risk groups | X | X | |||||||||||||||||
| Nutrition for COVID patients recovering at home | X | X | X | X | X | ||||||||||||||
| Nutrition for hospitalized patients | X | X | X | X | X | X | |||||||||||||
Abbreviations: ASN, American Society for Nutrition; ASPEN, American Society of Parenteral and Enteral Nutrition; BDA, British Dietetic Association; CDC, Centers for Disease Control and Prevention; ESPEN, European Society of Clinical Nutrition and Metabolism; EUFIC, European Food Information Council; FAO, Food and Agriculture Organization; ILCA, International Lactation Consultant Association; USDA, United States Department of Agriculture; WFP, World Food Programme; WHO, World Health Organization.
aIt is noted that further information on dietary issues has been provided by other countries (such as Spain, Germany, Greece, etc), but they were not included since it was not in the English language.
bBDA redirects to the guidelines provided by the Royal College of Pediatrics and Child Health and the Royal College of Obstetricians and Gynaecologists, which are similar to other recommendations presented.
cDietitians of Canada refer to the guidelines of the Society of Obstetricians and Gynecologists of Canada (SOGC) regarding lactation, which are similar to other recommendations presented.
Lactation
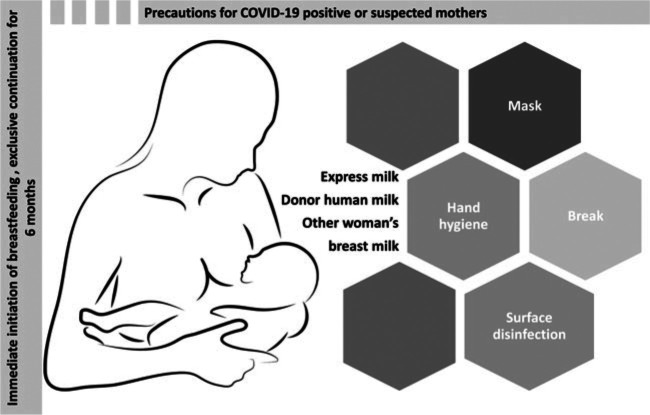
Several organizations provide advice on lactation in the COVID-19 pandemic, such as the WHO, United Nations Children's Fund (UNICEF), Centers for Disease Control and Prevention (CDC), and International Lactation Consultant Association (ILCA). The WHO recommends the immediate initiation (within the first hour) of breastfeeding, its exclusive continuation for 6 months, the introduction of complementary feeding at no earlier than 6 months, and the prolongation of breastfeeding for 2 years or more.5 In COVID-19–positive or suspected positive mothers, all the aforementioned official organizations encourage breastfeeding (after taking appropriate precautions, such as hand hygiene, mask during feeding, and surface disinfection), since it is the best diet for infants.5,19–21 In case of severe malaise, it is suggested that mothers can express milk, use donor human milk, consider having a break, and then restart breastfeeding or consider letting another woman breastfeed their child (Figure 1).5 UNICEF on top of other recommendations underlines that COVID-19 provides an opportunity to replace formula milk and manufactured food with freshly homemade food.20
Figure 1.
Recommendations for lactation. Image from www.pixabay.com
Nutrition during quarantine
The recommendations regarding healthy eating during quarantine (governmental order “stay at home” or medically determined mandate due to possible exposure) are summarized in Table 2. Almost all official sources emphasize the role of hydration and the adoption of a healthy diet with fruits, vegetables, whole grains, and healthy sources of fat.13,14,22–30 Several tips are given on the limitation of salt (such as avoidance of canned meat, heavily processed foods, high-sodium condiments), sugar (such as sweetened beverages, sweet snacks),13,22,23,29 and alcohol,23,27–29 while other aspects of diet are also highlighted, such as variety,14,22,23 “fun in the kitchen,”23 and balanced and “mindful eating.”14 Dietitians Australia provides shopping ideas so that food sufficiency is ensured along with minimal market visits during the quarantine.26 ESPEN also underlines that regular physical activity should be continued during quarantine while taking precautions.6
Table 2. Specific Recommendations of International and National Bodies on Healthy Nutrition During Quarantinea.
| WHO | WFP | ASN | FAO | Academy Nutrition and Dietetics | Turkish Dietetic Association | China National Health Commission | EUFIC | Dietitians of Canada | Dietitians Association of Australia | Australian Government Department of Health | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hydration | Water (8-10 cups) | Hydrate | Water (6-8 cups) | Hydrate | Adequate water | Drink boiled water or tea | 1.6-2 L | Hydrate | Plenty of water | ||
| Fruits | 2 cups (4 serv) | Build a colorful plate | Plenty | Plenty | Fresh fruits, frozen of precooked Higher consumption of citrus fruits (rich in vitamin C) |
Fresh fruits, rather than juice | Plenty | Plenty | Choose fresh that last longer | Plenty | |
| Vegetables | 2.5 cups (5 serv) | Build a colorful plate | Plenty | Plenty | Fresh vegetables, frozen, or precooked | Fresh vegetables, deep color, mushroom, agaric, and kelp | Plenty | Plenty | Choose fresh vegetables that last longer | Plenty including different types and color | |
| Grains | 180 g | Whole grain bread and mixed-grain rice | Whole grains | Whole grains | Whole grains | Whole grains, mixed beans, and potatoes are preferable | Whole grains | Whole grains | Rice, pasta, quinoa | Mostly whole grain and/or high cereal fiber varieties | |
| Protein foods (meat/beans/fish) | 160 g Red meat 1-2 times/wk, poultry 2-3 times/wk |
Limit the consumption of canned meat | Small meat portions to limit saturated fat | Consume high-protein foods, fish twice a week, legumes may be consumed daily, probiotics | Avoid fatty or smoked meats, and say no to meat of wild animals; dairy products, especially yogurt | Legumes, eggs, fish, meat | Canned fish, legumes (canned or dried) | Lean meats, poultry, fish, eggs, tofu, nuts, seeds, legumes or beans | |||
| Fats/oils | Moderate amount of fat and oil (unsaturated) | Nuts, olive/sesame oil | Olive oil daily | Avoid fried foods | Healthy fats | Nuts and seeds | Nuts and seeds (including nut butters) | Limit foods containing saturated fat | |||
| Salt | <5 g/d | Limit | Avoid salty foods | Limit | Limit foods containing added salt | ||||||
| Sugar | Less sugar | Limit, avoid sweetened beverages | Less sugar | Limit sugar and sugar-containing foods and beverages | Limit | Limit foods containing added sugars | |||||
| Other | Avoid eating out | Variety | Limit commercially prepared frozen dinners Prefer packed foods that will stay fresh for longer |
Variety Limit alcohol |
Healthful choices, “fun in the kitchen” | Avoid alcohol; vitamin and mineral supplements as an alternative for a short period of time | Balance, balanced diet including grains, fruits, vegetables, meat, and eggs Avoid alcohol and soft drinks |
Balance, Variety Limit alcohol Smaller portions Tips on mindful eating |
No single food is authorized to fight COVID-19 | Shopping tips | Limit alcohol intake |
Abbreviations: BDA, British Dietetic Association; EUFIC, European Food Information Council; FAO, Food and Agriculture Organization; WFP, World Food Programme; WHO, World Health Organization.
aThe United States Department of Agriculture (USDA) recommends a mix of self-stable, frozen, and fresh foods and provides links to more specific dietary guidance (www.choosemyplate.gov).
Nutrition for disease prevention in high-risk groups
Groups at high risk for severe illness from COVID-19 are the elderly (aged >65 years), those who live in nursing homes, and those with comorbidities (chronic lung disease or asthma, heart problems, immunosuppression, obesity, diabetes, and kidney and liver diseases).2 Moreover, people with disabilities, those who are homeless, and pregnant women need extra precautions.2
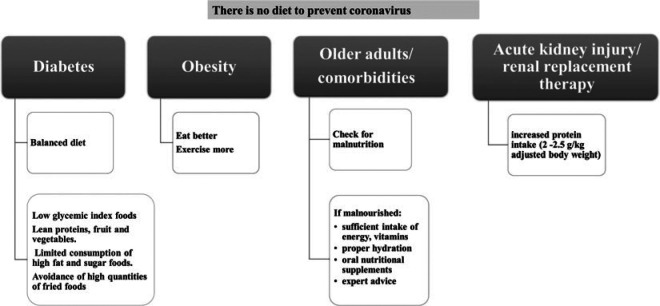
The British Dietetic Association (BDA) emphasizes that “there is no diet to prevent coronavirus”11 and that there is no food or food component with an authorized claim by the European Food Safety Authority (EFSA) to protect against infection.11 With respect to obesity, the Department of Health and Social Care in the United Kingdom launched a campaign to help people lose weight, exercise more, and eat better.31 Other measures have been taken to tackle obesity and “protect” the British against COVID-19, such as menu labeling, ban on TV advertisements, and ban on certain supermarket deals regarding foods high in salt, sugar, and fat.31
The International Diabetes Federation underlines that in the era of COVID-19, individuals with diabetes should eat a balanced diet so as to have normal blood glucose levels and an enhanced immune system.32 More specifically, it recommends the consumption of low glycemic index foods (eg, vegetables, whole wheat pasta), lean proteins, fruits and vegetables, the limited consumption of high fat and sugar foods, and the avoidance of high quantities of fried foods.32
According to the ESPEN Expert Statement on COVID-19, older people and/or people with comorbidities should be screened for malnutrition with the use of validated tools (ie, MUST, NRS-2002, etc).6 In the case of malnutrition, sufficient intake of energy, vitamins (such as vitamins A, C, D, E, B complex), omega-3 fatty acids, and minerals (such as zinc, selenium, and iron) should be ensured and expert advice should be taken in order to optimize nutritional intake.6
The role of proper hydration is also critical in the management of malnourished patients.11 Moreover, oral nutritional supplements (ONSs) should be ingested, if necessary, in order to cover nutritional needs.6
For critically ill patients with acute kidney injury undergoing renal replacement therapy, increased protein intake is recommended (2-2.5 g/kg adjusted body weight [ABW] per day).7
The aforementioned recommendations are summarized in Figure 2.
Figure 2.
Recommendations for high-risk groups.
Nutrition for recovery at home
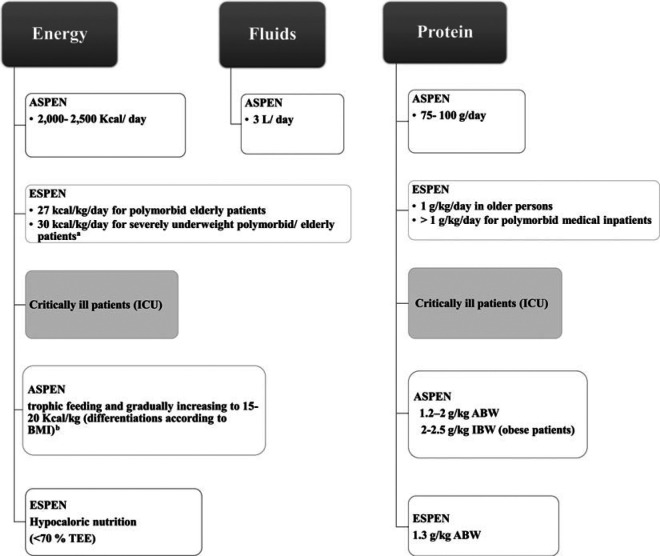
The nutritional status of each infected patient should be evaluated before the administration of general treatments.6 Patients with COVID-19 recovering at home should ensure that they are eating and drinking regularly to maintain good nutrition status.33 Older people and/or people with comorbidities and COVID-19 should be checked for malnutrition and treated accordingly, as underlined by ESPEN.6 ASPEN also highlights the importance of addressing malnutrition, emphasizing the role of hydration and energy and protein intake, and providing practical ideas for the general public (ie, rehydration recipes and ideas for protein-rich foods).10 This step is of particular importance since malnutrition may delay recovery and increase frailty. More particularly, the recommendations for energy, protein, and fluids are shown in Figure 3.6,10 If nutritional needs are not met after dietary counseling and food fortification, ONSs should be used.6,10 A supplement providing at least 400 kcal/d and 30 g or more of protein per day should be started for at least 1 month and then rerevaluated.6
Figure 3.
Nutrition recommendations for patients with COVID-19 for energy, fluids, and protein. Data from references Barazzoni,6 Martindale,7 and ASPEN.10 aIt is noted that recommendations should be individualized and that risk of refeeding syndrome is high in this group. Consultation by nutritional experts is recommended.6 bEnergy recommendations are 11 to 14 kcal/kg ABW per day in patients with BMI from 30 to 50 and 22 to 25 kcal/kg ideal body weight per day in patients with BMI more than 50. ASPEN indicates American Society for Parenteral and Enteral Nutrition; ESPEN, European Society of Clinical Nutrition and Metabolism; ICU, intensive care unit; TEE, total energy expenditure; BMI, body mass index; ABW, adjusted body weight; IBW, ideal body weight; kcal, kilocalories; L, liters.
Nutrition in hospital
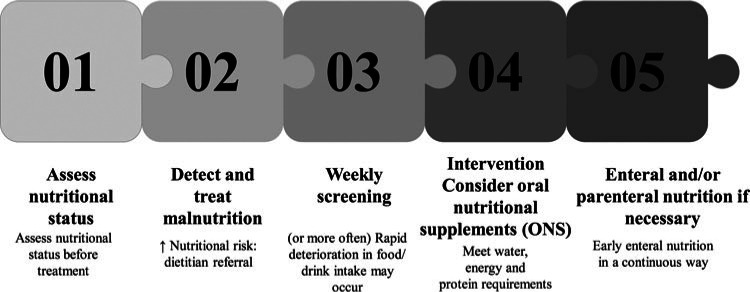
It is suggested that nutritional status should be assessed before treatment initiation.7,34 Malnutrition should be detected and adequately treated.6 Indeed, patients with COVID-19 with high nutritional risk scores had worse outcomes and higher mortality rates.33 As stressed by recent guidelines, patients with high nutritional risk scores should be referred to a dietitian for evaluation and individualized nutrition therapy.35,36 Patients should be routinely screened at least weekly (for non-ICU [intensive care unit] patients) or more regularly.35 It is noted that rapid deterioration in food/drink intake may occur in COVID-19 patients.35
Fever and respiratory distress may increase energy needs of patients with COVID-19, while isolation and bed rest gradually lead to reductions in muscle tissue.37 The lack of visitors in hospitals may reduce access to snacks.35 Moreover, shortness of breath, dry mouth, as well as loss of smell and taste may render oral intake difficult.35 Medications such as chloroquine may cause gastrointestinal (GI) distress, which, in turn, may influence food intake.38
Nutrition recommendations are differentiated along with severity of disease and ventilation initiation, as presented later, but they follow the basic principles of hospital nutrition. For malnourished patients, gradual increases in food/energy intake should be considered to avoid refeeding syndrome.6,7,35 ASPEN raises a concern for early enteral nutrition (EN) in the subset of patients with COVID-19 presenting with GI symptoms (such as diarrhea, nausea, and vomiting).7
Nonventilated patients
A basic nutritional goal for hospitalized patients is the prevention and treatment of malnutrition (Figure 4). For this purpose, high-energy, high-protein meals, snacks, and drinks should be considered and consistency of food should be modified if required.35 Soft/moist foods may be better tolerated in patients with shortness of breath and/or dry mouth, while foods with a strong taste may be useful for patients with loss of smell and taste.35 Personalized meals may be of added value, as shown from clinical practice.37 Feeding assistance should also be offered if needed.35
Figure 4.
Steps to prevent malnutrition in nonventilated hospitalized patients. ONS indicates oral nutritional supplements.
According to Australian recommendations, energy needs are about 25 kilocalories per kilogram per day (kcal/kg/d) (up to 30 kcal/kg/d in cases of malnutrition) after the first 5 days in the ICU.36 The protein goal should be at least 1.2 g/kg/d.36 ONSs should be considered in nonventilated patients.6 More specifically, 2 oral supplements per day should be administered to patients consuming less than 50% of their usual intake.8 An energy-dense formula providing 1.25 to 1.5 kcal/mL is recommended.37 The next step is EN if nutritional needs cannot be met by the oral route.6 Early EN (within 24-48 hours of admission) via continuous infusion rather than bolus is recommended.6,7,9 Continuous EN may reduce the exposure of the health care providers to the virus and may possibly reduce the risk of diarrhea.7 Specific recommendations on nasogastric feeding and minimizing its associated risks in patients requiring noninvasive ventilation or continuous positive airways pressure have been launched by a collaboration of British Scientific Societies.39 Parenteral nutrition (PN) can also be considered as a second-choice option if contraindications for EN are present or if the nutritional goals are not reached.6,7,9
Ventilated patients
Early EN is preferred over PN, if possible,6,7,9 as stated earlier. Australian recommendations suggest commencing EN support within 24 hours of ICU admission in low-risk patients with mechanical ventilation, while for high-risk patients, nutrition consultation should initially take place.36
For several patients with COVID-19 and acute respiratory distress syndrome, prone position may be indicated to reduce the risk of pulmonary complications,40 but this position is compatible with enteral feeding.6,7,9 It is noted that the Critical Care Specialist Group of BDA has launched detailed recommendations for feeding in the prone position regarding the tube position, feed delivery, choice of feed, monitoring of feed tolerance, and managing potential food intolerance.8 If EN is not possible, PN can be provided.6,7,9 Energy and protein requirements for ICU patients are shown in Figure 3.
Rehabilitation after extubation
Patients who gradually recover and are extubated may experience dysphagia and difficulties in swallowing,6 and referral to a speech and language therapist should be considered.35 In this case, food with adapted texture can be considered as a first option.6 If not tolerated, EN can be initiated or resumed.6 It is noted that Australian guidelines recommend keeping enteral tubes in place after extubation since patients' recovery may be prolonged.36 In case that EN is contraindicated because of high aspiration risk, temporary PN can be administered.6 At the stage of rehabilitation, active mobilization should also be encouraged to preserve muscle mass.6,9
DISCUSSION
The scientific community has promptly responded to the emerging needs of nutritional recommendations in the COVID-19 pandemic in an effort to limit its consequences. Although there is a striking dearth of evidence concerning applied clinical nutrition protocols for patients with COVID-19,37,41,42 there is a consensus of international bodies regarding the nutritional management of healthy adults and children in quarantine,13,14,22–26 as well as hospitalized patients in different stages of severity.6,7,9
Breastfeeding is recommended for COVID-19–positive or suspected positive mothers (after taking appropriate precautions), since it is the best diet for infants.5,19–21 It is noted that the virus seems not to be detectable in breast milk,43 although certain case reports have shown the opposite.44–46 In addition, breast milk provides antibodies and generally protects against infectious diseases47 along with vaccines, which produce antibodies transferred to the baby.48 It is noted that COVID-19 vaccination in pregnant and breastfeeding women is safe and effective.48 In this context, there is no contradiction for breastfeeding. Moreover, breast milk may help against malnutrition in children, which increases in the era of COVID-19.49
“There is no diet to prevent coronavirus.”11,25 However, since the host metabolic status influences the course of the disease, a healthy balanced diet should be followed.50 Indeed, a healthy diet as promoted by international bodies13,14,22–26 ensures the provision of vitamins and minerals, such as vitamins A, C, D, E, and B complex, selenium, iron, zinc, copper, and omega-3 fatty acids, which play a role in the immune system often acting synergistically.34,51 Traditional foods, such as kelp, are also recommended to achieve a better nutritional status in China,29 possibly because they include angiotensin-converting enzyme inhibitory peptides, fibers, omega-3 fatty acids, and other antioxidant and anti-inflammatory components.52 The antioxidant and antithrombotic effects of Mediterranean diet as a whole and its several individual components may act as a “weapon” against the cytokine storm of the disease53 and the activation of newly defined key molecules of COVID-19 pathogenesis, such as platelet activating factor (PAF).54,55 Indeed, micronutrients, non-nutrients, and Mediterranean diet have been proposed to exert a potential protective role against COVID-19 through modulation of PAF actions and metabolism.56
To optimize vitamin D, a few minutes of sunlight exposure should be considered along with vitamin D–rich and -enriched foods.11 Although several lines of evidence indicate a role of vitamin D supplementation in acute respiratory tract infection,57 and ongoing studies with COVID-19 patients have included vitamin D as an adjunct therapeutic line in their protocol,41 the supplementation with vitamin D is not officially recommended for COVID-19 prevention and/or treatment. A National Institute for Health and Care Excellence (NICE) rapid guideline on COVID-19 and vitamin D concluded that “there is no evidence to support taking vitamin D supplements to specifically prevent or treat COVID-19.”58 BDA and NICE guidelines, however, state that if people are unable to go outside, a daily supplement containing 10 μg (400 IU) should be considered.11,58 Recently, a cross-sectional European study reported an inverse association between mean levels of vitamin D and the number of COVID-19 cases per million.59 Moreover, low levels of vitamin D have been measured in hospitalized patients with COVID-19 (76% of patients).60 Therapeutic doses of vitamin C (24 g/d intravenously for 7 days) were also tested in critically ill patients with COVID-19.61 The study found no differences in mortality, nor duration of mechanical ventilation, but reported improvements in oxygenation (ratio of arterial partial pressure of oxygen to fraction of inspired oxygen [Pao2/Fio2]).61 Official sources have alerted that there is no evidence at this time point to support intravenous high-dose vitamin C in the management of COVID-19.62
Dietary changes during quarantine have been documented in most studies, but they were not all in line with guidelines. More particularly, an increased intake of fruits and vegetables was observed in China63 and an increase in Mediterranean diet adherence was observed in young Italian subjects64 and Spanish people of all ages.65 In contrast, a deterioration in food quality was observed during quarantine, possibly due to mood changes and health concerns in France,66 Italy (increase of comfort foods),67 Australia,68 United Arab Emirates,69 China (youth subjects),70 and in an international study including subjects from Europe, North Africa, Western Asia, and the United States,71 In adolescents from Spain, Italy, Brazil, Colombia, and Chile, a “mixed effect” of quarantine was observed, with increases in intake of legumes, vegetables, fruits, sweets, and fried foods and decreases in intake of fast foods.72 For the interpretation of the available data, other behaviors should be also recorded such as increased screen time, which is connected to the consumption of refined foods during the COVID-19 pandemic.69,73 Physical activity status, although strongly recommended, was not achieved in all studies, with some showing increases in physical activity64,65 and others showing decreases.40,68,71,74
Water intake is emphasized by the vast majority of international bodies, ranging from 6 to 10 glasses per day,13,23 with a parallel limit in alcohol.23,27–29 Indeed, proper hydration status is necessary for the function of all organs and temperature control, which becomes critical in case of fever and disease.75 Suboptimal hydration has additionally been hypothesized to increase mortality in patients with COVID-19.76 During the COVID-19 lockdown, both decreases (binge or normal drinking patterns)65,71 and increases in alcohol consumption have been observed.77,78 An interesting case of methanol poisoning was documented in Iran, where hundreds of people died believing that drinking alcohol could cure and/or prevent the disease, which once more underlines the importance of scientific guidance during the pandemic.79
As far as nutrition for high-risk groups is concerned, proper dietary habits and the prevention of malnutrition are highlighted.6,10 In patients with type 1 diabetes, worsening of glucose control was observed during quarantine, which was mainly due to the limited availability of glucose/insulin strips in this period, while diet incompliance was also documented.80 Overweight and obese subjects tended to increase snacking and gained weight, while underweight subjects tended to lose weight, indicating possible malnutrition.77 However, it should be stressed that rapid weight loss for obese/overweight patients is contraindicated since muscle loss may have an adverse effect on recovery.35
Malnutrition is common in free-living and hospitalized older adults.81 In addition, GI symptoms may accompany COVID-19,82 worsening dietary intake; thus, malnutrition is definitely an issue to be addressed. Moreover, malnutrition is connected with complications and worsened prognosis in hospitalized patients83 and has been found to be a predictor of mortality in influenza infections.84 In patients with COVID-19, a high nutrition risk was related to worsened outcomes, higher mortality, higher procalcitonin values, and inflammatory markers.33 In this context, hospital menu changes,85 ONSs and early EN may prove beneficial.6,7 Early EN is generally associated with improved mortality and lower infection rates.86 In all cases, individualization in the estimation of energy and protein requirements, as well as the route and way of nutrition delivery procedures, should take place.6,7,10 However, in clinical practice, patient weight and/or indirect calorimetry measurements may not be performed in order to minimize interaction with infected patients,87 which may render nutrition assessment and nutrition care difficult. Indeed, patients' actual energy needs may differ from those estimated by equations due to hypermetabolism.88 Moreover, patients tend to have nasogastric tubes for a longer time, rather than endoscopic gastrostomy placement, in order to minimize procedures in patients with COVID-19.87
Specific dietetic advice by dietitians is useful, and telehealth can be used in order to assess and monitor patients remotely.35 Moreover, the available data suggest that dietitians in the hospital setting may be discouraged from entering rooms of COVID-19 patients87 but can contribute their knowledge through electronic health records.87
It is noted that only a few high-quality review articles regarding official nutrition recommendations have been published.89,90 One focused on nutrition during quarantine but has not included clinically relevant information for hospitalized or seriously diseases patients.89 Moreover, in the aforementioned review, recommendations from Australia, Brazil, Canada, Italy, Spain, and the United States were included while Asian countries were not referenced.89 Other articles focused only on critically ill patients in general90,91 or with a special focus on cachexia.92 The present work is of scientific interest to both public health professionals and health professionals working with hospitalized patients, and it includes a large spectrum of recommendations from scientific bodies (Europe, Canada, Australia, Asia, and international).
Several issues have not been addressed by international recommendations, such as diet-drug interactions, if clinically relevant. This subject may be of increasing importance to people under medical treatment who stay at home and do not have close medical monitoring.
In summary, there is a consensus regarding breastfeeding5,19–21 and healthy nutrition during quarantine.13,14,22–26 The risk of malnutrition should be assessed in high-risk groups and hospitalized patients.6,7,9 Early feeding should be provided with a priority on EN and/or ONSs covering energy and protein needs as well as recommended allowances of vitamins and minerals.6,7,9 Parenteral feeding should be provided if enteral feeding is contraindicated or if the caloric and/or protein goals are not achieved through the enteral route.
CONCLUSION
The present review presents the national and international official dietary recommendations during the COVID-19 pandemic. Although there is no diet to prevent coronavirus, the aim is to follow a healthy diet in order to boost the immune system. Health and nutrition professionals can make tailored nutrition plans taking into account nutritional risk and underlying diseases and in this way may reduce the deleterious effects of the COVID-19 pandemic. The present work can help and/or “guide” nutrition and health care professionals since it is a consolidated reference for practicing clinicians and other health professionals.
Footnotes
The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Paraskevi Detopoulou, Email: viviandeto@gmail.com.
Christina Tsouma, Email: ctsouma@gmail.com.
Vassilios Papamikos, Email: vpapamikos@gmail.com.
REFERENCES
- 1.Shils MD. Modern Nutrition in Health and Disease. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 2.Centers for Disease Control and Prevention. People who need to take extra precautions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. Published 2020. Accessed January 20, 2022.
- 3.Muscogiuri G, Barrea L, Savastano S, Colao A. Nutritional recommendations for COVID-19 quarantine. Eur J Clin Nutr. 2020;74(6):850–851. doi:10.1038/s41430-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mediouni M, Madiouni R, Kaczor-Urbanowicz KE. COVID-19: how the quarantine could lead to the depreobesity. Obes Med. 2020;19:100255. doi:10.1016/j.obmed.2020.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Breastfeeding advice during the COVID-19 outbreak. http://www.emro.who.int/nutrition/nutrition-infocus/breastfeeding-advice-during-covid-19-outbreak.html. Published 2020. Accessed January 20, 2022.
- 6.Barazzoni R, Bischoff SC, Breda J, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39(6):1631–1638. doi:10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martindale R, Patel JJ, Taylor B, Arabi YM, Warren M, McClave SA. Nutrition therapy in critically ill patients with coronavirus disease 2019. JPEN J Parenter Enteral Nutr. 2020;44(7):1174–1184. doi:10.1002/jpen.1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.British Dietetic Association. BDA Critical Care Specialist Group COVID-19 best practice guidance: enteral feeding in prone position. https://www.bda.uk.com/resource/best-practice-guidance-enteral-feeding-in-prone-position.html. Published 2020. Accessed January 20, 2022.
- 9.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. https://apps.who.int/iris/handle/10665/331446. Published 2020. Accessed January 20, 2022.
- 10.American Society for Parenteral and Enteral Nutrition (ASPEN). Nutrition and hydration: key weapons in the fight against COVID-19 (for patients recovering at home). https://www.nutritioncare.org/uploadedFiles/Documents/Guidelines_and_Clinical_Resources/COVID19/COVID19%20Patient%20Nutrition%20Paper.pdf. Published 2020. Accessed January 20, 2022.
- 11.British Dietetic Association. COVID-19/coronavirus—advice for the general public. https://www.bda.uk.com/resource/covid-19-corona-virus-advice-for-the-general-public.html. Published April 17, 2020. Accessed January 20, 2022.
- 12.Correia MITD. Nutrition in times of COVID-19, how to trust the deluge of scientific information. Curr Opin Clin Nutr Metab Care. 2020;23(4):288–293. doi:10.1097/MCO.0000000000000666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Nutrition advice for adults during the COVID-19 outbreak. http://www.emro.who.int/nutrition/nutrition-infocus/nutrition-advice-for-adults-during-the-covid-19-outbreak.html. Published 2020. Accessed January 20, 2022.
- 14.EUFIC. How to keep healthy while in isolation or quarantine (COVID-19). https://www.eufic.org/en/healthy-living/article/7-tips-to-keep-healthy-while-in-isolation-or-quarantine-covid-19. Published 2020. Accessed January 20, 2022.
- 15.EFAD. COVID-19 resources, research and information. Web page. http://www.efad.org/en-us/covid-19-resources-research-and-information. Accessed June 30, 2021.
- 16.PEN Global Resource for Nutrition Practice. COVID-19. Web page. https://www.pennutrition.com/covid19. Accessed June 30, 2021.
- 17.Global Nutrition Cluster. Web page. https://www.nutritioncluster.net. Accessed June 30, 2021.
- 18.ASPEN. Resources for clinicians caring for patients with coronavirus. Web page. https://www.nutritioncare.org/COVID19/#Education. Accessed June 30, 2021.
- 19.Centers for Disease Control and Prevention. Coronavirus disease (COVID-19) and breastfeeding. https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/covid-19-and-breastfeeding.html. Published 2020. Accessed January 20, 2022.
- 20.UNICEF. Feeding young children during the COVID-19 pandemic. https://www.unicef.org/eap/feeding-young-children-during-covid-19-pandemic. Published 2020. Accessed January 20, 2022.
- 21.International Lactation Consultant Association. ILCA statement on breastfeeding and lactation support during the covid-19 pandemic. https://lactationmatters.org/2020/03/18/ilca-statement-on-breastfeeding-and-lactation-support-during-the-covid-19-pandemic. Published 2020. Accessed January 20, 2022.
- 22.World Food Programme Insight. Food for thought: 7 tips on keeping a healthy diet in the face of coronavirus. https://insight.wfp.org/food-for-thought-7-tips-on-keeping-a-healthy-diet-in-the-face-of-coronavirus-7fab7f06177. Published 2020. Accessed January 20, 2022.
- 23.Food and Agriculture Organization of the United Nations. Maintaining a healthy diet during the COVID-19 pandemic. http://www.fao.org/3/ca8380en/CA8380EN.pdf. Published March 27, 2020. Accessed January 20, 2022.
- 24.Academy of Nutrition and Dietetics. Coronavirus (COVID-19). https://www.eatright.org/coronavirus. Published 2020. Accessed January 20, 2022.
- 25.Dietitians of Canada. Advice for the general public about COVID-19. https://www.dietitians.ca/News/2020/Advice-for-the-general-public-about-COVID-19. Published 2020. Accessed January 20, 2022.
- 26.Dietitians Association of Australia. COVID-19 tips and resources. https://daa.asn.au/smart-eating-for-you/planning-your-pantry-during-the-covid-19-pandemic. Published 2020. Accessed January 20, 2022.
- 27.Turkish Dietetic Association. Turkish Dietetic Association's recommendations on nutrition and COVID-19. http://www.efad.org/media/1956/turkish-dietetic-association-nutrition-recommendations-about-coronavirus-covid-19.pdf. Published 2020. Accessed January 20, 2022.
- 28.Australian Government, Department of Health. Healthy eating during coronavirus (COVID-19) restrictions. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/ongoing-support-during-coronavirus-covid-19/healthy-eating-during-coronavirus-covid-19-restrictions. Published 2020. Accessed January 20, 2022.
- 29.National Health Commission of the People's Republic of China. What makes for a healthy diet during an outbreak? http://govt.chinadaily.com.cn/s/202003/26/WS5e7c1dc6498ea01b9aea1e61/what-makes-for-a-healthy-diet-during-an-outbreak.html. Published 2020. Accessed January 20, 2022.
- 30.Byrd-Bredbenner C, Eck K, Abbot JM. Making health and nutrition a priority during the coronavirus (COVID-19) pandemic. https://nutrition.org/making-health-and-nutrition-a-priority-during-the-coronavirus-covid-19-pandemic. Published March 18, 2020. Accessed January 20, 2022.
- 31.Department of Health and Social Care. New obesity strategy unveiled as country urged to lose weight to beat coronavirus (COVID-19) and protect the NHS. https://www.gov.uk/government/news/new-obesity-strategy-unveiled-as-country-urged-to-lose-weight-to-beat-coronavirus-covid-19-and-protect-the-nhs. Published 2020. Accessed January 20, 2022.
- 32.International Diabetes Federation. Healthy nutrition and home-based exercise. https://www.idf.org/aboutdiabetes/what-is-diabetes/covid-19-and-diabetes/1-covid-19-and-diabetes.html. Published 2020. Accessed January 20, 2022.
- 33.Zhao X, Li Y, Ge Y, et al. Evaluation of nutrition risk and its association with mortality risk in severely and critically ill COVID-19 patients. JPEN J Parenter Enteral Nutr. 2021;45(1):32–42. doi:10.1002/jpen.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang L, Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92(5):479–490. doi:10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.British Dietetic Association. Practical considerations for nutritional management of non-ICU COVID-19 patients in hospital. https://www.bda.uk.com/uploads/assets/5422cf91-4cd2-4aac-9bc20c2a643f09cd/200512-Practical-considerations-for-nutritional-management-of-non-ICU-COVID-19-patients-in-hospital-v1.pdf. Published 2020. Accessed January 20, 2022.
- 36.Chapple LAS, Fetterplace K, Asrani V, et al. Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID-19) in Australia and New Zealand. Nutr Diet. 2020;77(4):426–436. doi:10.1111/1747-0080.12636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cintoni M, Rinninella E, Annetta MG, Mele MC. Nutritional management in hospital setting during SARS-CoV-2 pandemic: a real-life experience. Eur J Clin Nutr. 2020;74(5):846–847. doi:10.1038/s41430-020-0625-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Srinivasa A, Tosounidou S, Gordon C. Increased incidence of gastrointestinal side effects in patients taking hydroxychloroquine: a brand-related issue? J Rheumatol. 2017;44(3):398. doi:10.3899/jrheum.161063. [DOI] [PubMed] [Google Scholar]
- 39.Turner P, Terblanche E, Cronin R, et al. Route of Nutrition Support in Patients Requiring NIV & CPAP During the COVID-19 Response (BAPEN, BDA, NNNG, British Thoracic Society/Endorsed by the Intensive Care Society). Redditch, England: BAPEN; 2020. [Google Scholar]
- 40.Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020;48(6):e440–e469. doi:10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caccialanza R, Laviano A, Lobascio F, et al. Early nutritional supplementation in non-critically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): rationale and feasibility of a shared pragmatic protocol. Nutrition. 2020;74:110835. doi:10.1016/j.nut.2020.110835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Formisano E, Di Maio P, Ivaldi C, et al. Nutritional therapy for patients with coronavirus disease 2019 (COVID-19): practical protocol from a single center highly affected by an outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Nutrition. 2021;82:111048. doi:10.1016/j.nut.2020.111048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet North Am Ed. 2020;395(10226):809–815. doi:10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Groß R, Conzelmann C, Müller JA, et al. Detection of SARS-CoV-2 in human breast milk. Lancet North Am Ed. 2020;395(10239):1757–1758. doi:10.1016/S0140-6736(20)31181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buonsenso D, Costa S, Sanguinetti M, et al. Neonatal late onset infection with severe acute respiratory syndrome coronavirus 2. Am J Perinatol. 2020;37(8):869–872. doi:10.1055/s-0040-1710541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu Y, Liu C, Dong L, et al. Coronavirus disease 2019 among pregnant Chinese women: case series data on the safety of vaginal birth and breastfeeding. BJOG. 2020;127(9):1109–1115. doi:10.1111/1471-0528.16276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van de Perre P. Transfer of antibody via mother's milk. Vaccine. 2003;21(24):3374–3376. doi:10.1016/s0264-410x(03)00336-0. [DOI] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. COVID-19 vaccines while pregnant or breastfeeding. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html?s_cid=10484:can%20nursing%20mothers%20get%20the%20covid%20vaccine:sem.ga:p:RG:GM:gen:PTN:FY21. Published 2021. Accessed January 27, 2022.
- 49.Headey D, Heidkamp R, Osendarp S, et al. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. Lancet. 2020;396(10250):519–521. doi:10.1016/S0140-6736(20)31647-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gasmi A, Noor S, Tippairote T, Dadar M, Menzel A, Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin Immunol. 2020;215:108409. doi:10.1016/j.clim.2020.108409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system—working in harmony to reduce the risk of infection. Nutrients. 2020;12(1):236. doi:10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tamama K. Potential benefits of dietary seaweeds as protection against COVID-19. Nutr Rev. 2021;79(7):814–823. doi:10.1093/nutrit/nuaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tsoupras A, Lordan R, Zabetakis I. Thrombosis and COVID-19: the potential role of nutrition. Front Nutr. 2020;7:583080. doi:10.3389/fnut.2020.583080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Demopoulos C, Antonopoulou S, Theocharides T. COVID-19, microthromboses, inflammation and platelet activating factor (PAF). Biofactors. 2020;46(6):927–933. [DOI] [PubMed] [Google Scholar]
- 55.Detopoulou P, Fragopoulou E, Nomikos T, et al. The relation of diet with PAF and its metabolic enzymes in healthy volunteers. Eur J Nutr. 2015;54(1):25–34. doi:10.1007/s00394-014-0682-3. [DOI] [PubMed] [Google Scholar]
- 56.Detopoulou P, Demopoulos C, Antonopoulou S. Micronutrients, non-nutrients and Mediterranean diet: a potential protective role against COVID-19 through modulation of PAF actions and metabolism. Nutrients. 2020;13(2):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grant WB, Lahore H, McDonnell SL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988. doi:10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.NICE. COVID-19 rapid guideline: vitamin D. www.nice.org.uk/guidance/ng187. Published December 17, 2020. Accessed January 20, 2022.
- 59.Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020;32(7):1195–1198. doi:10.1007/s40520-020-01570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS. Nutritional status of patients with coronavirus disease 2019 (COVID-19). Int J Infect Dis. 2020;100:390–393. doi:10.1016/j.ijid.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang J, Rao X, Li Y, et al. Pilot trial of high-dose vitamin C in critically ill COVID-19 patients. Ann Intensive Care. 2021;11(1):5. doi:10.1186/s13613-020-00792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Australian Government, Department of Health. No evidence to support intravenous high-dose vitamin C in the management of COVID-19. https://www.tga.gov.au/node/904121. Published 2020. Accessed May 20, 2022.
- 63.Wang X, Lei SM, Le S, et al. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among Chinese adults. Int J Environ Res Public Health. 2020;17(15):5575. doi:10.3390/ijerph17155575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. doi:10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodríguez-Pérez C, Molina-Montes E, Verardo V, et al. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. 2020;12(6):1730. doi:10.3390/nu12061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marty L, de Lauzon-Guillain B, Labesse M, Nicklaus S. Food choice motives and the nutritional quality of diet during the COVID-19 lockdown in France. Appetite. 2020;157:105005. doi:10.1016/j.appet.2020.105005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Scarmozzino F, Visioli F. COVID-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5):675. doi:10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gallo LA, Gallo TF, Young SL, Moritz KM, Akison LK. The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. Nutrients. 2020;12(6):1865. doi:10.3390/nu12061865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheikh Ismail L, Osaili TM, Mohamad MN, et al. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study. Nutrients. 2020;12(11):3314. doi:10.3390/nu12113314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jia P, Liu L, Xie X, et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 impact on lifestyle change survey (COINLICS). Appetite. 2020;158:105015. doi:10.1016/j.appet.2020.105015. [DOI] [PubMed] [Google Scholar]
- 71.Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. doi:10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, et al. COVID-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12(6):1807. doi:10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Werneck AO, Silva DR, Malta DC, et al. Associations of sedentary behaviours and incidence of unhealthy diet during the COVID-19 quarantine in Brazil. Public Health Nutr. 2020;24(3):422–426. doi:10.1017/S1368980020004188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during COVID-19 pandemic: an observational study. Nutrients. 2020;12(8):2289. doi:10.3390/nu12082289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Popkin BM, D'Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. 2010;68(8):439–458. doi:10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stookey JD, Allu PKR, Chabas D, Pearce D, Lang F. Hypotheses about sub-optimal hydration in the weeks before coronavirus disease (COVID-19) as a risk factor for dying from COVID-19. Med Hypotheses. 2020;144:110237. doi:10.1016/j.mehy.2020.110237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12(6):1657. doi:10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chodkiewicz J, Talarowska M, Miniszewska J, Nawrocka N, Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health. 2020;17(13):4677. doi:10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aghababaeian H, Hamdanieh L, Ostadtaghizadeh A. Alcohol intake in an attempt to fight COVID-19: a medical myth in Iran. Alcohol. 2020;88:29–32. doi:10.1016/j.alcohol.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Verma A, Rajput R, Verma S, Balania VKB, Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 diabetes mellitus. Diabetes Metab Syndr. 2020;14(5):1213–1216. doi:10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dent E, Hoogendijk EO, Visvanathan R, Wright ORL. Malnutrition screening and assessment in hospitalised older people: a review. J Nutr Health Aging. 2019;23(5):431–441. doi:10.1007/s12603-019-1176-z. [DOI] [PubMed] [Google Scholar]
- 82.Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51(9):843–851. doi:10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review [formula: see text]. JPEN J Parenter Enteral Nutr. 2017;41(5):744–758. doi:10.1177/0148607115625638. [DOI] [PubMed] [Google Scholar]
- 84.Reyes L, Arvelo W, Estevez A, et al. Population-based surveillance for 2009 pandemic influenza A (H1N1) virus in Guatemala, 2009. Influenza Other Respir Viruses. 2010;4(3):129–140. doi:10.1111/j.1750-2659.2010.00138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Detopoulou P, Al-Khelefawi ZH, Kalonarchi G, Papamikos V. Formulation of the menu of a general hospital after its conversion to a “COVID Hospital”: a nutrient analysis of 28-day menus. Front Nutr. 2022;9:833628. doi: 10.3389/fnut.2022.833628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Taylor BE, McClave SA, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016;44(2):390–438. doi:10.1097/CCM.0000000000001525. [DOI] [PubMed] [Google Scholar]
- 87.Wells Mulherin D, Walker R, Holcombe B, Guenter P. ASPEN report on nutrition support practice processes with COVID-19: the first response. Nutr Clin Pract. 2020;35(5):783–791. doi:10.1002/ncp.10553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yu P, Cassiere H, DeRosa S, Bocchieri K, Yar S, Hartman A. Hypermetabolism and coronavirus disease 2019. JPEN J Parenter Enteral Nutr. 2020;44(7):1234–1236. doi:10.1002/jpen.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.de Faria Coelho-Ravagnani C, Corgosinho FC, Sanches FLFZ, Prado CMM, Laviano A, Mota JF. Dietary recommendations during the COVID-19 pandemic. Nutr Rev. 2021;79(4):382–393. doi:10.1093/nutrit/nuaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chapple LAS, Tatucu-Babet OA, Lambell KJ, Fetterplace K, Ridley EJ. Nutrition guidelines for critically ill adults admitted with COVID-19: is there consensus? Clin Nutr ESPEN. 2021;44:69–77. doi:10.1016/j.clnesp.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Martínez Rodríguez J, Roca Fontbona M. Comparison of expert recommendations on clinical nutrition for hospitalized patients with COVID-19. Nutr Hosp. 2020;37(5):984–998. doi:10.20960/nh.03194. [DOI] [PubMed] [Google Scholar]
- 92.Virgens IPA, Santana NM, Lima SCVC, Fayh APT. Can COVID-19 be a risk for cachexia for patients during intensive care? Narrative review and nutritional recommendations. Br J Nutr. 2021;126(4):552–560. doi:10.1017/S0007114520004420. [DOI] [PMC free article] [PubMed] [Google Scholar]