Abstract
Healthcare workers (HCWs) have suffered physical and psychological threats since the beginning of the coronavirus disease 2019 (COVID-19) pandemic. Mind-body modalities (MBMs) can reduce the long-term adverse health effects associated with COVID-specific chronic stress. This systematic review aims to investigate the role of MBMs in managing the mental health of HCWs during the COVID-19 pandemic. A comprehensive search was conducted using 6 electronic databases, resulting in 18 clinical studies from 2019 to September 2021. Meta-analysis showed that MBMs significantly improved the perceived stress of HCWs (standardized mean difference, −0.37; 95% confidence intervals, −0.53 to −0.21). In addition, some MBMs had significant positive effects on psychological trauma, burnout, insomnia, anxiety, depression, self-compassion, mindfulness, quality of life, resilience, and well-being, but not psychological trauma and self-efficacy of HCWs. This review provides data supporting the potential of some MBMs to improve the mental health of HCWs during COVID-19. However, owing to poor methodological quality and heterogeneity of interventions and outcomes of the included studies, further high-quality clinical trials are needed on this topic in the future.
Keywords: healthcare personnel, mental health, mind-body therapies, COVID-19, pandemics
1. Introduction
Globally, the coronavirus disease 2019 (COVID-19) pandemic has been a threat to mental and physical health of humanity [1]. Since the start of this pandemic, healthcare workers (HCWs) have suffered the physical and psychological threat of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [2,3]. In this context, the prevalence of anxiety, depression, and stress among HCWs in the COVID-19 pandemic was reported to be as high as 67.55%, 55.89%, and 62.99%, respectively [3]. Moreover, women, younger nurses, frontline HCWs, and workers in areas with higher infection rates are more likely to be severely affected by mental health effects in HCW during the pandemic [3]. Mental health difficulties of HCWs can lead to burnout, worsening attitudes toward patient safety, and hindering the efficient and safe use of medical resources when they are important [4]. As a result, several countries are implementing initiatives to improve health and well-being in HCW in the context of the COVID-19 pandemic, the most common of which are mental health initiatives [5].
Mind–body modality (MBM) can be defined as “a health practice that combines mental focus, controlled breathing, and body movements to help relax the body and mind [6]”. MBMs, including meditation, yoga, and mindfulness training, have been considered helpful in stress-related diseases by fostering resilience through self-care [7,8]. Researchers have also found that MBMs are effective in a variety of physical and psychological conditions, including chronic pain, anxiety, depression, cancer-related fatigue, tobacco addiction, inflammatory bowel disease, and cardiovascular disease [7]. MBMs are popular not only in patients with diagnosed diseases, but also in the general population. According to a survey in 2017, the use of yoga and meditation among American adults reached 14.3% and 14.2%, respectively [9]. Currently, MBMs are receiving attention as strategies to reduce the long-term adverse health effects associated with COVID-specific chronic stress and are being evaluated as specific, practical, affordable, and viable strategies to help manage chronic stress [10].
Maintaining the integrity of HCW’s mental health has emerged as an important topic in the COVID-19 pandemic [5], and the use of MBMs to manage and improve it and prevent progression to mental disorders has received attention [11]. In the context of the COVID-19 pandemic, some hospitals have introduced MBMs, including meditation and yoga, to protect the mental health of frontline HCWs [12,13]. Additionally, although contact-to-contact visits to psychiatric clinics have declined due to concerns about SARS-CoV-2 infection [14,15], MBMs are becoming more popular in combination with information and communications technology (ICT) [16].
As such, MBMs are likely to be a promising component of strategies for improving the mental health of HCW during the COVID-19 pandemic. However, how MBMs benefit the mental health aspects of HCWs in the context of COVID-19 has not yet been comprehensively reviewed. Therefore, this systematic review explores the roles of mind-body modalities in managing the mental health of HCWs during the COVID-19.
2. Materials and Methods
The protocol of this systematic review was published as a paper [17] and registered in the Open Science Framework registry (https://osf.io/tudbw, accessed on 13 August 2021). This systematic review complies with Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 statement (Supplementary Material File S1) [18].
2.1. Data Sources and Search Strategy
The following 6 electronic databases were searched for studies published from December 2019 (when the first case of COVID-19 was identified [19]) to September 2021: Medline (via PubMed), EMBASE (via Elsevier), Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature (via EBSCO), Allied and Complementary Medicine Database (via EBSCO), and PsycARTICLES (via ProQuest). In addition, we searched the reference lists of relevant articles and conducted a manual search on Google Scholar to include all of the relevant articles. We included both the literature published in peer-reviewed journals and gray literature, such as dissertations. We designed search strategies for all databases based on the advice of experts in the systematic review (Supplementary Material File S2).
2.2. Eligibility Criteria
2.2.1. Types of Study Design
Given the urgency of COVID-19, we included all types of original prospective quantitative intervention studies, including randomized controlled trials (RCTs), non-randomized controlled clinical trials (CCTs), and before-after studies. Retrospective and qualitative studies were excluded. There were no restrictions on publication language or publication status.
2.2.2. Types of Participants
We included studies on all types of HCWs, such as physicians, nurses, hospital staff, and health managers, without restrictions on the sex, age, and ethnicity of the participants. However, we excluded studies that did not describe whether participants were directly or indirectly affected by COVID-19.
2.2.3. Types of Interventions
As treatment interventions, MBMs, including meditation, mindfulness-based intervention, autogenic training, yoga, tai chi, qigong, breathing exercises, music therapy, guided imagery, biofeedback, prayer, and faith-based techniques were allowed. As control interventions, no treatment, waitlist, sham control, attention control, or active comparators were allowed.
2.2.4. Types of Outcome Measures
The primary outcome was the level of perceived stress, assessed using validated tools, including the Perceived Stress Scale [20]. Secondary outcomes included mental health-related outcomes, such as depression, anxiety, burnout, and safety data of the intervention.
2.3. Study Selection
A study selection was conducted through a three-step screening process based on the eligibility criteria. First, titles and/or abstracts of the searched studies were screened to identify potentially eligible articles. Second, potentially eligible reports were sought for retrieval. Third, the full text of the retrieved reports was reviewed. Two researchers (C.-Y.K. and B.L.) independently conducted the study selection process, and disagreements between the researchers were resolved through discussion.
2.4. Data Extraction
Two researchers (C.-Y.K. and B.L.) independently extracted the following information using a predefined, pilot-tested excel form: the first author’s name, year of publication, country, study design, sample size, details of participants, treatment and control interventions, a treatment period of intervention, outcome measures, results, and safety data. Any discrepancies between the researchers were resolved through discussion. When the data were insufficient or ambiguous, the corresponding authors of the original studies were contacted via e-mail.
2.5. Methodological Quality and Risk of Bias Assessment
The methodological quality of the included studies was assessed using the corresponding critical appraisal skills program tools, depending on the study type [21]. For RCTs, the Cochrane Collaboration risk of bias tool was used to assess the related risk of bias [22]. For CCTs and before-after studies, the Quality Assessment of Controlled Intervention Studies and the Quality Assessment Tool for Before-After (Pre-Post) studies with no control group by the National Heart, Lung, and Blood Institute were used to assess methodological quality [23]. Two researchers (C.-Y.K. and B.L.) independently assessed the methodological quality and risk of bias of the included studies and any disagreements between the researchers were resolved through discussion.
2.6. Data Analysis and Synthesis
Descriptive analyses of the participants, interventions, controls, and outcomes of all of the studies were performed. If there were 2 or more RCTs or CCTs with the same outcome measures, a meta-analysis was performed using RevMan 5.4 (the Cochrane Collaboration, London, UK). In the meta-analysis, dichotomous and continuous data were presented as risk ratios (RR) and standardized mean differences (SMD) with 95% confidence intervals (CIs). The I2 values of ≥50% and ≥75% were considered substantial and statistically heterogeneous, respectively. In the meta-analysis, a random-effects model was used if the included studies had significant heterogeneity (I2 value ≥ 50%), whereas the fixed-effect model was used when the heterogeneity was insignificant or the number of studies included in the meta-analysis was less than five [24]. If sufficient data were available, subgroup analyses were planned according to the (a) type of HCWs and (b) type of mind-body modality. In addition, sensitivity analyses were conducted to identify the robustness of the results by excluding (a) studies with a high risk of bias and (b) data outliers. Evidence of publication bias was assessed using funnel plots if at least ten RCTs were included in each meta-analysis. The results of the included before-and-after studies were only described without quantitative synthesis.
3. Results
3.1. Study Search
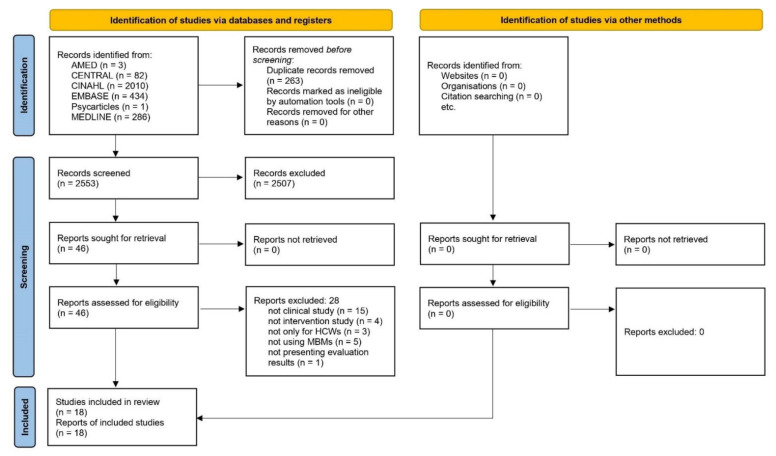
In the initial search, 2816 documents were found, and 263 duplications were removed. Among the 2553 documents, 46 potentially relevant articles were selected after title and abstract screening. On the full-text screening, fifteen non-clinical studies [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], four non-intervention studies [40,41,42,43], three generic studies [44,45,46], five studies not using MBMs [47,48,49,50,51], and one not presenting evaluation results [52] were excluded. Ultimately, this review included 18 studies [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70] (Figure 1).
Figure 1.
PRISMA flow chart of this review.
3.2. Characteristics of Included Studies
Among the included studies, 16 [53,54,56,57,58,59,60,61,62,63,64,65,66,68,69,70] were published articles and 2 [55,67] were conference abstracts. Researchers from nine countries conducted these studies, and the study conducted in the United States was the most common, with six studies [54,55,59,60,63,68], followed by India with three studies [56,57,69]. Among the included studies, five were RCTs [58,65,66,68,69], four were CCTs [57,59,62,70], and the remaining ten were before-after studies [53,54,55,56,60,61,63,64,67]. Except for one study [69], the types of HCWs in the included subjects were all described. Among them, 14 [53,54,56,57,58,59,60,61,63,64,65,66,68,70] included nurses (14/17, 82.35%), 9 [53,54,55,56,58,62,63,67,68] included clinicians (9/17, 52.94%), and 6 [54,56,58,60,63,68] included non-clinical workers (6/17, 35.29%). The sample sizes of the included studies ranged from 3 to 482, with a mean of 102.44. Although the MBMs used in the included studies were heterogeneous, their components could be classified into nine types: music, mindfulness, wellness/welfare/well-being, yoga, meditation, empathy/self-compassion, breathing exercise, relaxation, and guided imagery. The interventions included an average of 1.61 mind-body modality components, with mindfulness being the most common component (6/18, 33.33%), followed by breathing exercises (5/18, 27.78%), yoga (4/18, 22.22%), wellness/welfare/well-being, meditation, and relaxation (3/18, 16.67%), music and empathy/self-compassion (2/18, 11.11%, respectively), and guided imagery (1/18, 5.56%). Except for 2 studies that did not describe the duration of intervention [55,57], the duration varied from 1 to 150 days, with a mean of 36.75 days (Table 1).
Table 1.
Characteristics of included studies.
| Author (Country) | Population | Sample Size (Included→Analyzed) | Intervention (Delivery) | Treatment Period | Outcomes |
|---|---|---|---|---|---|
| RCTs (n = 5) | |||||
| Fiol-DeRoque 2021 [58] (Spain) | HCWs (including physicians, nurses, and others) | EG: 248→248 CG: 234→234 (ITT analysis) |
Self-managed psychoeducational intervention, based on CBT and mindfulness vs. Control app (Mobile phone-based intervention) |
14 days | 1. DASS-21; 2. DTS; 3. MBI–HSS; 4. ISI; 5. General Self-Efficacy Scale |
| Nourian 2021 [65] (Iran) | Nurses working in COVID-19 care wards | 44→41 * | MBSR vs. waitlist (WhatsApp group, otherwise unclear) |
7 weeks | 1. PSQI |
| Sanadgol 2021 [66] (Iran) | ICU nurses | EG: 25→25 CG: 25→25 |
Guided imagery training vs. no intervention (1. 90 min of the group training session (two sessions); 2. at least three sessions a week at home) |
1 month | 1. 15-item DAS |
| Thimmapuram 2021 [68] (US) | Physicians and advance practice providers (including physicians, nurse, and other hospital staff) | EG: 77→41 + CG: 78→58 + |
Heartfulness meditation vs. usual clinical care (Home practice: daily 6 min of heartfulness meditation via audio file) |
4 weeks | 1. UCLA Loneliness Scale Version 3; 2. PSQI |
| Vajpeyee 2021 [69] (India) | HCWs (the types of HCWs were not described) | 240→209 (EG: 116, CG: 93) + | Yoga and music intervention vs. no intervention (1. Daily 30 min of yoga and music by WhatsApp video; 2. Help of social workers to motivate the participants by personal visits or telephonic communication) |
30 days | 1. DASS-42 |
| CCTs (n = 4) | |||||
| Emmanuel 2021 [57] (India) | ICU nurses | EG: 30→30 CG: 30→30 |
Welfare program including stress management and breathing exercise vs. NR (30 min for breathing exercise, otherwise unclear) |
NR | 1. ENSS |
| Franco 2021 [59] (US) | Pediatric nurses | 53→48 (EG: 22, CG: 26) + | Self-compassion training program vs. no intervention (One day training program, 6 h) |
1 day | 2 weeks post-intervention 1. SCS; 2. CAMS; 3. Compassion Scale; 4. ProQOL; 5. DASS; 6. Resiliency activation and decompression and job engagement |
| Luton 2021 [62] (UK) | Surgical trainees in a single UK statutory education body | EG: 24→14 + CG: 14→14 |
Enhanced stress-resilience training course (mindfulness-based exercises) vs. no intervention (1. Weekly 75 min online tutorials (15 min of debrief, and 60 min of training course); 2. Daily up to 20 min of mindfulness exercises following guided media) |
5 weeks | 1. MBI; 2. PSS; 3. PHQ-2; 4. CAMS–R; 5. STAI |
| Ibrahim 2022 [70] (Indonesia) | Nurses who worked in COVID-19 patient services of health care facilities | EG: 25→25 CG: 25→25 |
Mindfulness breathing meditation vs. waitlist (Twice a week, 15 min (video practice) per session in WhatsApp group) |
4 weeks | 1. WEMWBS Indonesian version |
| Before-after study (n = 9) | |||||
| Giordano 2020 [53] (Italy) | Clinical staff in COVID-19 unit (including physicians and nurses) | 34→29 + | Tailored music therapy (15–20 min, mobile phones, otherwise unclear) |
4 weeks | Before listening to music, and within one hour after the end of listening 1. MusicTeamCare-Q1 End of the study 2. MusicTeamCare-Q2 |
| Klatt 2020 [54] (US) | HCWs (including physicians, nurses, other clinical staff, and non-clinical healthcare staff) | 465→267 + | Mindfulness-based intervention (Mindfulness in Motion) (1. 12 min, weekly group meeting; 2. Individual practice by using audio or video practice (via smartphone or computer)) |
8 weeks | 1. MBI; 2. PSS; 3. CDRS; 4. UWES |
| Coffey 2021 [55] (US) | Geriatric medicine fellows | 3 | Wellness program (Wellness, Empathy, and Philanthropy) (Incorporate the wellness program to curriculum) |
NR | 1. Abbreviated MBI; 2. Brief Resilience Scale |
| Divya 2021 [56] (India) | HCWs (including physicians, nurses, other clinical staff, and non-clinical healthcare staff) | 100→92 + | Yogic breathing technique (1. 4-day online breath and meditation workshop (video conference); 2. 35 min home practice) |
40 days | 1. DASS-21; 2. PSQI; 3. CDRS; 4. SWLS |
| Heeter 2021 [60] (US) | Hospice HCWs (including nurses, other clinical staff, and non-clinical healthcare staff) | 151→76 + | Yoga-based meditation (1. Half-hour online introduction to the program; 2. Weekly meditation session at each team’s monthly all-staff meeting (12 min, accessible via the program website)) |
6 weeks | 1. Brief PFI; 2. MAIA |
| Liu 2021 [61] (China) | Clinical first-line nurses in COVID-19 designated hospitals | 151→140 + | Diaphragmatic breathing relaxation training (Daily, 30 min at 8 PM via MP3 audio and demonstration video) |
4 weeks | 1. PSQI; 2. SAS; 3. SDS |
| Narayanan 2021 [63] (US) | HCWs (including physicians, nurses, other clinical staff, and non-clinical healthcare staff) | 100→88 + | Breathing practice and meditation (Simha kriya) (5 min, one to two times daily, Video with instruction) |
4 weeks | 1. Meditation perception questionnaire |
| Nijland 2021 [64] (Netherlands) | ICU nurses in an academic hospital | 86 | VR relaxation (high-quality immersive 360-degree videos of calming natural environments) (10 min during their shift, otherwise unclear) |
1 session | 1. PSS; 2. CDRS |
| So 2021 [67] (UK) | Junior doctors working at a single UK cancer center | 10 | Well-being program including breathing and relaxation exercise, clinical debriefing, reflective practice, and mindfulness strategies (Weekly 30 min well-being sessions throughout their oncology placement) |
4–6 months | 1. WEMWBS |
Abbreviations. CAMS–R, Cognitive and Affective Mindfulness Scale–Revised; CBT, cognitive-behavioral therapy; CCT, non-randomized controlled clinical trial; CDRS, Connor–Davidson Resilience Scale; CG, control group; COVID–19, Coronavirus Disease 2019; DAS, Templer Death Anxiety Scale; DASS, Depression, Anxiety and Stress Scale; DTS, Davidson Trauma Scale; EG, experimental group; ENSS, Expanded Nursing Stress Scale; HCW, healthcare worker; ICU, intensive care unit; ISI, Insomnia Severity Index; ITT, intent–to–treat; MAIA, Multidimensional Assessment of Interoceptive Awareness; MBI–HSS, Maslach Burnout Inventory–Human Services Survey; MBI, Maslach Burnout Inventory; MBSR, mindfulness-based stress reduction; NR, not reported; PFI, Stanford Professional Fulfillment Index; PHQ, Patient Health Questionnaire; PP, per-protocol; ProQOL, Professional Quality of Life; PSQI, Pittsburgh sleep quality index; PSS, Perceived Stress Scale; RCT, randomized controlled clinical trial; SAS, Self–rating Anxiety Scale; SCS, Self-Compassion Scale; SDS, Self–rating Depression Scale; STAI, State–Trait Anxiety Inventory; SWLS, Satisfaction With Life Scale; UWES, Utrecht Work Engagement Scale; VR, virtual reality; WEMWBS, Warwick–Edinburgh Mental Well-being Scale. Note. *, The numbers of participants of EG and CG were unclear; +, The reason for the dropout is not stated.
3.3. Methodological Qualities of Included Studies
3.3.1. RCTs
Three RCTs [58,65,68] described appropriate random sequence generation methods such as computerized randomization; conversely, the other two studies [66,69] did not describe this method. No study has described the method of allocation concealment. Fiol-DeRoque et al. [58] conducted a study using a mobile application and reported that double-blind was implemented. The remaining four RCTs [65,66,68,69] did not report the implementation of blinding but were evaluated as high due to the nature of the intervention. Only one study [58] reported that blinding of the outcome assessment was not performed; in the remaining studies [65,66,68,69], blinding of the outcome assessor was not described. For incomplete outcome data, one study [58] performed an intention-to-treat analysis, and another study [66] with no dropouts was rated low in this domain. In the remaining three studies [65,68,69], dropouts existed, but the cause was not described, and a per-protocol (PP) analysis was performed; therefore, this domain was rated highly. With regard to selective reporting, the protocol was confirmed in only one study [58], and the pre-planned outcome was confirmed to be reported and evaluated as low. Other studies [65,66,68,69] evaluated selective reporting as unclear. Three studies [65,66,68], in which clinical and demographic homogeneity between the two groups was confirmed at baseline, were evaluated as low in other sources of bias, and the remaining studies were evaluated as unclear (Supplementary Material File S3).
3.3.2. CCTs
As the included CCTs were not RCTs, they were evaluated as “no” in Q1 and “not applicable (NA)” in Q2. Allocation concealment and blinding procedures were not reported in any of the studies. Therefore, Q3 and Q5 were evaluated as not reported (NR), and Q4 was evaluated as “no,” considering that double-blinding was impossible due to the nature of the intervention. In a study [59], statistical heterogeneity of baseline characteristics was reported, and it was evaluated as “no” in Q6; the heterogeneity was not described in the remaining studies [57,62,70]. In another study [62], the overall dropout rate from the study at the endpoint was more than 20% of the number allocated to treatment, and the differential dropout rate at the endpoint was more than 15 percent. Therefore, Q7 and Q8 of this study [62] were evaluated as “no.” As treatment adherence was not reported in all of the studies, Q9 was evaluated as NR. As only one study [57] recommended avoidance of other interventions in the groups, it was evaluated as “yes” in Q10. As validated outcomes were used in all of the studies, they were evaluated as “yes” in Q11. The sample size was calculated in only one study [70] and was evaluated as “yes” in Q12. The pre-registered protocol was confirmed in only one study [62], its Q13 was evaluated as “yes,” and the remaining studies [57,59,70] were evaluated as cannot be determined. Two studies [57,70] with no dropouts were evaluated as NA in Q14, whereas the other two studies [59,62] with PP analysis were evaluated as “no” (Supplementary Material File S3).
3.3.3. Before-after Studies
The purpose of the studies was clearly described; therefore, it was evaluated as “yes” in Q1. As the selection criteria for the study population were not clearly described in the four studies [54,55,56,60], Q2 and CD were not evaluated in Q4. Except for one study [61] that included only geriatric fellows as participants, other studies [53,54,55,56,60,63,64,67] included two or more occupations, so their Q3 were evaluated as “yes.” In only one study [61], the sample size was calculated and evaluated as “yes” in Q5. Because the intervention was insufficiently described in two studies [55,67], it was evaluated as “no” in their Q6. Two studies [53,63] that did not use a validated outcome were rated as “no” in their Q7. Only one study [64] reported that the outcome assessor was blinded. As not described in other studies [53,54,55,56,60,61,63,67], all were assessed as CD in their Q8. In two studies [54,60], loss to follow-up after baseline was >20%; therefore, it was evaluated as “no” in their Q9. One study [63] without a statistical test for pre-to post-changes, was rated as “no” in Q10. In only one study [56], the outcome assessment was performed three times, and it was evaluated as “yes” in Q11. In other studies [53,54,55,60,61,63,64,67], it was evaluated as “no” in Q11 because it was only evaluated twice: before and after. There was no intervention at the group level; therefore, all were evaluated as NA in Q12 (Supplementary Material File S3).
3.4. Main Results
The outcomes used among the included studies varied, but they can be classified into 12 categories: perceived stress (the primary outcome), psychological trauma, burnout, insomnia, self-efficacy, anxiety, depression, self-compassion, mindfulness, and quality of life (QOL), resilience, and well-being. Among these, meta-analyses of stress, depression, and anxiety are possible.
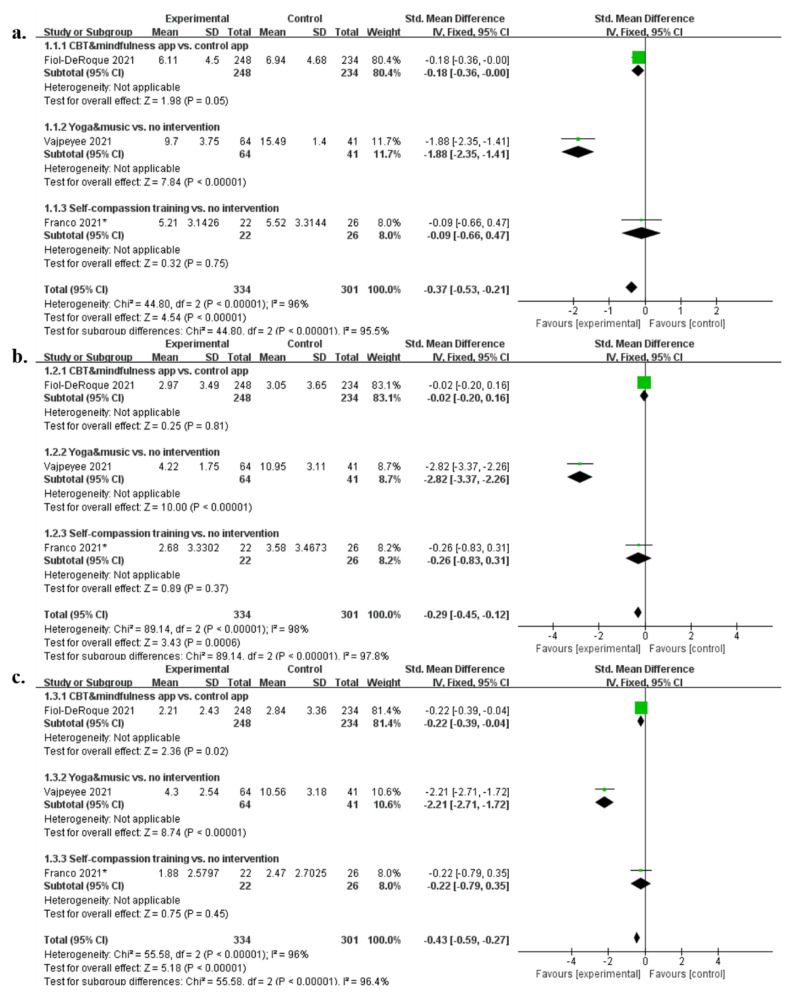
In terms of perceived stress, a meta-analysis of Depression, Anxiety and Stress Scale (DASS), including two RCTs and one CCT, was possible. Consequently, MBMs showed a significantly greater effect on improving perceived stress compared to the control interventions (SMD, −0.37; 95% CI, −0.53 to −0.21; I2 = 96%). However, in the individual analysis, compared to no intervention, yoga and music-based intervention had a significant effect on perceived stress improvement (SMD, −1.88; 95% CI, −2.35 to −1.41), whereas self-compassion-based intervention had no significant effect (SMD, −0.09; 95% CI, −0.66 to 0.47). Otherwise, cognitive-behavioral therapy (CBT) and mindfulness-based intervention showed borderline significance compared to the psychoeducational intervention (SMD, −0.18; 95% CI, −0.36 to −0.00) (Figure 2a). Regarding depression, a meta-analysis of DASS, including two RCTs and one CCT, was possible. Consequently, MBMs showed a significantly greater effect on improving depression than the control interventions (SMD, −0.29; 95% CI, −0.45 to −0.12; I2 = 98%). However, in the case of individual analysis, only yoga- and music-based intervention had a significant effect on depression improvement compared to no intervention (SMD, −2.82; 95% CI, −3.37 to −2.26). Self-compassion-based intervention and CBT and mindfulness-based intervention, on the other hand, did not show significant effect compared to control interventions (SMD, −0.26; 95% CI, −0.83 to 0.31; SMD, −0.02; 95% CI, −0.20 to 0.16) (Figure 2b). Regarding anxiety, a meta-analysis of DASS, including two RCTs and one CCT, was possible. Consequently, MBMs showed a significantly greater effect on improving anxiety compared to the control interventions (SMD, −0.43; 95% CI, −0.59 to −0.27; I2 = 96%). However, in the case of individual analysis, compared to no intervention, yoga and music-based intervention had a significant effect on anxiety improvement (SMD, −2.21%; CI, −2.71 to −1.72), whereas self-compassion-based intervention had no significant effect (SMD, −0.22; 95% CI, −0.79 to 0.35). CBT and mindfulness-based intervention also significantly improved anxiety compared to psychoeducational intervention (SMD, −0.22; 95% CI, −0.39 to −0.04) (Figure 2c). MBMs for each outcome showed a significantly positive effect compared to the control group or before treatment as follows (in descending order): self-compassion (2/2, 100%), QOL (2/2, 100%), perceived stress (6/8, 75%), resilience (4/6, 66.67%), burnout (3/5, 60%), insomnia (3/5, 60%), well-being (1/2, 50%), anxiety (3/7, 42.86%), depression (3/8, 37.5%), mindfulness (1/4, 25%), psychological trauma (0/1, 0%), and self-efficacy (0/1, 0%) (Table 2).
Figure 2.
Meta-analysis results of Depression, Anxiety and Stress Scale: (a) stress; (b) depression; and (c) anxiety. Note. *, non-randomized controlled clinical trials.
Table 2.
Main results of included studies.
| Outcomes | Comparison (Treatment Period) | Results | Reference |
|---|---|---|---|
| Outcomes related to perceived stress | |||
| 1. DASS (perceived stress) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| Yoga and music intervention vs. no intervention (30 days) | Participants with baseline abnormality: EG < CG (p = 8.28 × 10−19) Participants without baseline abnormality: No statistical comparison between groups |
Vajpeyee 2021 [69] | |
| Self-compassion training vs. no intervention (1 day) | EG < CG (p < 0.05) | Franco 2021 [59] | |
| Yogic breathing technique (40 days) | NS (p = 0.49) | Divya 2021 [56] | |
| 2. ENSS (nursing stress) | Welfare program including breathing exercise vs. no intervention (NR) | EG: pre < post (p < 0.05) CG: NS (p > 0.05) |
Emmanuel 2021 [57] |
| 3. PSS (perceived stress) | Mindfulness-based stress-resilience training vs. no intervention (5 weeks) | EG < CG (p < 0.01) | Luton 2021 [62] |
| Mindfulness-based movement (8 weeks) | pre > post (p = 0.00001) | Klatt 2020 [54] | |
| VR relaxation (1 session) | pre > post (p < 0.005) | Nijland 2021 [64] | |
| Outcomes related to psychological trauma | |||
| 1. DTS (psychological trauma) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| Outcomes related to burnout | |||
| 1. MBI–HSS (burnout) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | (1) Emotional exhaustion: NS (p > 0.05); (2) Professional accomplishment: NS (p > 0.05) (3) depersonalization: NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| 2. MBI (burnout) | Mindfulness-based stress-resilience training vs. no intervention (5 weeks) | NS (p = 0.630) | Luton 2021 [62] |
| Mindfulness-based movement (8 weeks) | (1) Total: pre > post (p = 0.00001); (2) Emotional exhaustion: pre > post (p = 0.00001); (3) Depersonalization: pre > post (p = 0.0012); (4) Personal accomplishment: pre > post (p = 0.00001) | Klatt 2020 [54] | |
| 3. Brief MBI (burnout) | Wellness program (NR) | Statistical analysis was not performed. | Coffey 2021 [55] |
| 4. Brief PFI (burnout) | Yoga-based meditation (6 weeks) | (1) Professional fulfillment: pre > post (p = 0.008); (2) Work exhaustion: pre > post (p = 0.049); (3) Interpersonal disengagement: NS (p > 0.05); (4) Total: NS (p > 0.05) | Heeter 2021 [60] |
| Outcomes related to insomnia | |||
| 1. ISI (insomnia severity) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| 2. PSQI (sleep quality) | MBSR vs. no intervention (7 weeks) | (1) Global score: NS (p = 0.105); (2) Subjective sleep quality: EG < CG (p = 0.000); (3) Sleep latency: EG < CG (p = 0.020); (4) Sleep duration: NS (p = 0.084); (5) Habitual sleep efficiency: NS (p = 0.148); (6) Sleep disturbances: NS (p = 0.587); (7) Use of sleep medication: NS (p = 0.118); (8) Daytime drowsiness: NS (p = 0.050) | Nourian 2021 [65] |
| Heartfulness meditation vs. usual care (4 weeks) | EG: pre > post (p = 0.001) CG: NS (p = 0.122) |
Thimmapuram 2021 [68] | |
| Yogic breathing technique (40 days) | NS (p = 0.154) | Divya 2021 [56] | |
| Diaphragmatic breathing relaxation training (4 weeks) | (1) Global: pre > post (p < 0.001); (2) Subjective sleep quality: pre > post (p < 0.001); (3) Sleep duration: pre > post (p < 0.001); (4) Sleep latency: pre > post (p < 0.001); (5) Habitual sleep efficiency: pre > post (p = 0.015); (6) Sleep disturbances: pre > post (p < 0.001); (7) Use of sleeping medication: NS (p = 0.134); (8) Daytime dysfunction: pre > post (p = 0.001) | Liu 2021 [61] | |
| Outcomes related to self-efficacy | |||
| 1. General Self-Efficacy Scale (self-efficacy) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| Outcomes related to anxiety | |||
| 1. DASS (anxiety) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| Yoga and music intervention vs. no intervention (30 days) | Participants with baseline abnormality: EG < CG (p = 1.02 × 10−16) Participants without baseline abnormality: No statistical comparison between groups |
Vajpeyee 2021 [69] | |
| Self-compassion training vs. no intervention (1 day) | NS (p = 0.05) | Franco 2021 [59] | |
| Yogic breathing technique (40 days) | NS (p = 0.613) | Divya 2021 [56] | |
| 2. 15-item DAS (death anxiety) | Guided imagery training vs. no intervention (1 month) | EG < CG (p = 0.004) | Sanadgol 2021 [66] |
| 3. STAI (anxiety) | Mindfulness-based stress-resilience training vs. no intervention (5 weeks) | NS (p = 0.450) | Luton 2021 [62] |
| 4. SAS (anxiety) | Diaphragmatic breathing relaxation training (4 weeks) | pre > post (p < 0.001) | Liu 2021 [61] |
| Outcomes related to depression | |||
| 1. DASS (depression) | CBT and mindfulness-based app vs. Psychoeducation app (14 days) | NS (p > 0.05) | Fiol-DeRoque 2021 [58] |
| Yoga and music intervention vs. no intervention (30 days) | Participants with baseline abnormality: EG < CG (p = 2.55 × 10−18) Participants without baseline abnormality: No statistical comparison between groups |
Vajpeyee 2021 [69] | |
| Self-compassion training vs. no intervention (1 day) | NS (p = 0.23) | Franco 2021 [59] | |
| Yogic breathing technique (40 days) | NS (p = 0.563) | Divya 2021 [56] | |
| 2. UCLA Loneliness Scale Version 3 (loneliness) | Heartfulness meditation vs. usual care (4 weeks) | EG: pre > post (p = 0.009) CG: NS (p = 0.254) |
Thimmapuram 2021 [68] |
| 3. PHQ-2 (depression) | Mindfulness-based stress-resilience training vs. no intervention (5 weeks) | NS (p > 0.05) | Luton 2021 [62] |
| 4. MusicTeamCare-Q1 (tiredness, sadness, fear, and worry) | Tailored music therapy (4 weeks) | (1) Breathing playlist: the scores of four symptoms were all significantly decreased (p < 0.05); (2) Energy playlist: the scores of four symptoms were all significantly decreased (p < 0.05); (3) Breathing customized playlist: the scores of sadness, fear, and worry were significantly decreased (p < 0.05); (4) Energy customized playlist: the scores of four symptoms were all significantly decreased (p < 0.05); (5) Serenity customized playlist: the scores of sadness, fear, and worry were significantly decreased (p < 0.05). | Giordano 2020 [53] |
| 5. SDS (depression) | Diaphragmatic breathing relaxation training (4 weeks) | NS (p = 0.359) | Liu 2021 [61] |
| Outcomes related to self-compassion | |||
| 1. SCS (self-compassion) | Self-compassion training vs. no intervention (1 day) | EG > CG (p < 0.001) | Franco 2021 [59] |
| 2. Compassion scale (compassion) | Self-compassion training vs. no intervention (1 day) | EG < CG (p < 0.01) | Franco 2021 [59] |
| Outcomes related to mindfulness | |||
| 1. CAMS (mindfulness) | Self-compassion training vs. no intervention (1 day) | EG > CG (p < 0.001) | Franco 2021 [59] |
| Mindfulness-based stress-resilience training vs. no intervention (5 weeks) | NS (p > 0.05) | Luton 2021 [62] | |
| 2. MAIA (interoceptive awareness) | Yoga-based meditation (6 weeks) | (1) Self-regulation: NS (p > 0.05); (2) Attention regulation: NS (p > 0.05); (3) Emotional awareness: NS (p > 0.05); (4) Body noticing: NS (p > 0.05); (5) Body listening: NS (p > 0.05); (6) Body trusting: NS (p > 0.05); (7) Total: NS (p > 0.05) | Heeter 2021 [60] |
| 3. Meditation Perception Questionnaire (perception about meditation) | Breathing practice and meditation (4 weeks) | Statistical analysis was not performed. | Narayanan 2021 [63] |
| Outcomes related to QOL | |||
| 1. ProQOL (professional QOL) | Self-compassion training vs. no intervention (1 day) | (1) Compassion satisfaction: EG > CG (p = 0.01); (2) Burnout: EG < CG (p < 0.01); (3) Secondary traumatic stress: NS (p = 0.08) | Franco 2021 [59] |
| 2. SWLS (satisfaction with life) | Yogic breathing technique (40 days) | pre < post (p < 0.001) | Divya 2021 [56] |
| Outcomes related to resilience | |||
| 1. Resiliency activation and decompression and job engagement (resilience and job engagement) | Self-compassion training vs. no intervention (1 day) | (1) Resiliency activation: NS (p = 0.55); (2) Resiliency decompression: EG < CG (p < 0.01); (3) Job engagement: NS (p = 0.21) | Franco 2021 [59] |
| 2. CDRS (resilience) | Mindfulness-based movement (8 weeks) | pre < post (p = 0.00001) | Klatt 2020 [54] |
| Yogic breathing technique (40 days) | pre < post (p = 0.015) | Divya 2021 [56] | |
| VR relaxation (1 session) | Statistical analysis was not performed. | Nijland 2021 [64] | |
| 3. UWES (work engagement) | Mindfulness-based movement (8 weeks) | (1) Total: pre < post (p = 0.00001); (2) Vigor: pre < post (p = 0.00001); (3) Absorption: pre < post (p = 0.00001); (4) Dedication: pre < post (p = 0.00001) | Klatt 2020 [54] |
| 4. Brief Resilience Scale (resilience) | Wellness program (NR) | NR | Coffey 2021 [55] |
| Outcomes related to well-being | |||
| 1. WEMWBS (well-being) | Mindfulness breathing meditation vs. no intervention (4 weeks) | EG < CG (p = 0.013) | Ibrahim 2022 [70] |
| Well-being program (4–6 months) | NS (p = 0.34) | So 2021 [67] | |
Abbreviations. CAMS, Cognitive and Affective Mindfulness Scale; CBT, cognitive-behavioral therapy; CCT, non-randomized controlled clinical trial; CDRS, Connor–Davidson Resilience Scale; CG, control group; DAS, Templer Death Anxiety Scale; DASS, Depression, Anxiety and Stress Scale; DTS, Davidson Trauma Scale; EG, experimental group; ENSS, Expanded Nursing Stress Scale; ISI, Insomnia Severity Index; MAIA, Multidimensional Assessment of Interoceptive Awareness; MBI–HSS, Maslach Burnout Inventory–Human Services Survey; MBI, Maslach Burnout Inventory; MBSR, mindfulness-based stress reduction; NR, not reported; PFI, Stanford Professional Fulfillment Index; PHQ, Patient Health Questionnaire; ProQOL, Professional Quality of Life; PSQI, Pittsburgh sleep quality index; PSS, Perceived Stress Scale; RCT, randomized controlled clinical trial; SAS, Self–rating Anxiety Scale; SCS, Self-Compassion Scale; SDS, Self–rating Depression Scale; STAI, State–Trait Anxiety Inventory; SWLS, Satisfaction With Life Scale; UWES, Utrecht Work Engagement Scale; VR, virtual reality; WEMWBS, Warwick–Edinburgh Mental Well-being Scale. Note. If it was associated with a statistically significant benefit compared to the control group, the intervention was highlighted in bold.
3.5. Safety Data
None of the included studies reported adverse events or safety data.
3.6. Publication Bias
As fewer than ten studies were included in the meta-analysis, publication bias through funnel plot generation was not evaluated.
4. Discussion
4.1. Main Findings
This review was performed in order to investigate the benefits of MBMs on the mental health aspects of HCWs in the context of COVID-19. Through a comprehensive literature search, 18 studies [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70] were included. According to the meta-analysis, MBMs had a significantly positive effect on the perceived stress of HCWs, which was the primary outcome of this study. Regarding the types of individual MBMs, the effects of yoga- and music-based interventions appeared to be the most prominent. In a meta-analysis of depression and anxiety, MBMs showed a significantly positive improvement compared to the control group. In this case, yoga- and music-based interventions had the largest effect size. However, the effect of self-compassion-based interventions on stress, depression, and anxiety was not significant. In other words, the effects of MBMs on mental health of HCWs may differ according to individual MBMs. For individual outcomes, some MBMs had significant positive effects on psychological trauma, burnout, insomnia, anxiety, depression, self-compassion, mindfulness, QOL, resilience, and well-being, but not psychological trauma and self-efficacy, compared to controls (in RCTs and CCTs) or baseline (in before-after studies). Although these results provide data that some MBMs may be useful options for mental health management of HCWs in the context of COVID-19, the methodological quality of the included studies was not optimal. In addition, the number of RCTs performed with rigorous design was insufficient, and CCT or before-after studies accounted for more than half of the studies. Therefore, the findings of this study could be greatly influenced by the results of large-scale rigorous clinical studies in the future.
4.2. Clinical Implications
The mental health of HCWs in the context of COVID-19 is a serious threat [3,4], and measures to manage it are urgently needed [5]. At present, to protect the mental health of this population and reduce stress as much as possible, there is an emphasis on establishing tailored, effective stress reduction interventions [71]. To develop effective anti-stress interventions, empirical evidence exists for some MBMs, such as mindfulness-based interventions, diaphragmatic respiration, and acting on self-efficacy [71]. Breath-focused mind-body therapies, as a strategy in precision medicine, have recently been claimed by some researchers to be effective in managing stress and anxiety [72,73]. Therefore, leveraging MBMs to manage the mental health of HCWs in the context of COVID-19 could be a promising strategy [10].
According to the results of the studies included in this review, some MBMs have shown positive effects in improving the mental health aspects of HCWs. When classified as individual outcomes, MBMs showed a relatively high rate of positive effects on self-compassion, QOL, perceived stress, resilience, burnout, insomnia, and well-being in this population. In addition, the individual MBMs used were heterogeneous, and no studies have compared two or more MBMs in this population. Therefore, it was difficult to find the optimal MBMs for mental health and psychological stress management in HCWs during the COVID-19 era. Nevertheless, according to the meta-analysis of the review, yoga- and music-based interventions had a larger effect size on perceived stress (DASS) than CBT and mindfulness-based or self-compassion-based interventions. A recent meta-analysis also found that yoga may help relieve stress in people who live under high stress or negative emotions, including HCWs, and the mechanism may be related to the modulation of sympathetic-vagal balance [74,75]. Moreover, in a systematic review of MBMs for nurses, yoga may be helpful in improving burnout and perceived stress among nurses in hospital setting [76].
Important considerations should be taken into account when introducing interventions for mental health management of HCWs in the context of COVID-19. The reality of a busy clinical setting must be considered. Strategies for managing stress and mental health in this population should be feasible and accessible. In this context, more than half of the included studies [53,54,56,58,60,61,62,63,65,68,69,70] (12/18, 66.67%) provided participants with MBMs combined with ICT, including mobile phone applications, guided audio files, video files, and video conferences. In addition, three studies [55,64,67] integrated MBMs into the work environment of participants, such as the educational curriculum and time for a shift. These results suggest that MBMs may be introduced to reflect the work environment of HCWs in the context of COVID-19.
4.3. Limitations and Suggestions for Further Studies
This systematic review has several limitations. First, the MBMs and outcomes used in the included studies were heterogeneous. Therefore, quantitative synthesis was not possible for most outcomes in this study. However, given that the mental health of HCWs in the context of COVID-19 has important clinical relevance and MBMs are a promising option, future research in this field needs to be further standardized and refined. In particular, a head-to-head trial may be attempted to investigate the most effective MBMs for improving perceived stress among HCWs during the COVID-19 era. Second, the methodological quality of the included studies was suboptimal. These methodological limitations may negatively affect the reliability of this study’s findings. In addition, it was rare among the included studies to be conducted with strict designs, including RCT (5/18, 27.78%). Future research in this field will be able to reflect a research design that reflects the characteristics of MBMs. For example, to investigate the effectiveness and safety of MBMs, n-of-1 trials may be ideal than traditional RCT [77]. Third, this study did not consider the temporal and environmental effects of COVID-19. Given that the impact of COVID-19 on the mental health of HCWs may vary depending on the time, place, and clinical setting, future research in this field will be able to develop customized interventions that take into account the temporal and environmental impacts of COVID-19 on HCWs.
5. Conclusions
This is the most comprehensive review available on the impact of MBMs on the mental health of HCWs during the COVID-19 era. This review provides data supporting the potential of some MBMs to improve the mental health of HCWs during COVID-19. There is evidence that yoga- and music-based interventions are helpful for improvement for perceived stress, the primary outcome. In addition, some MBMs had significant positive effects on psychological trauma, burnout, insomnia, anxiety, depression, self-compassion, mindfulness, QOL, resilience, and well-being, but not psychological trauma and self-efficacy of HCWs. However, owing to poor methodological quality and heterogeneity of interventions and outcomes of the included studies, further high-quality clinical trials are needed on this topic in the future.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10061027/s1, Supplementary Material File S1: PRIMSA 2020 checklist; Supplementary Material File S2. Search strategies used in each database; Supplementary Material File S3. Methodological qualities of included studies.
Author Contributions
Conceptualization, C.-Y.K.; Methodology, C.-Y.K. and B.L.; Writing—original draft, C.-Y.K. and B.L.; Writing—review & editing, C.-Y.K.; Funding, C.-Y.K.; Supervision, C.-Y.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study, as this study is a systematic review of previously published studies.
Informed Consent Statement
Patient consent was waived, as this study is a systematic review of previously published studies.
Data Availability Statement
The data presented in this study are available in the article and Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the MSIT (Ministry of Science and ICT), Korea, under the Grand Information Technology Research Center support program (IITP-2022-2020-0-01791) supervised by the IITP (Institute for Information & communications Technology Planning & Evaluation).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaukat N., Ali D.M., Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020;13:40. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vizheh M., Qorbani M., Arzaghi S.M., Muhidin S., Javanmard Z., Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020;19:1967–1978. doi: 10.1007/s40200-020-00643-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abhiram K., Tan B.Y.Q., Tan M., Tan L., Sia C.-H., Chua Y.X., Lim L.J.H., Suppiah C.M., Sim K., Chan Y.H., et al. The Effect of COVID-19 Endemicity on the Mental Health of Health Workers. J. Am. Med. Dir. Assoc. 2022;23:405–413.e3. doi: 10.1016/j.jamda.2022.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Brien N., Flott K., Bray O., Shaw A., Durkin M. Implementation of initiatives designed to improve healthcare worker health and wellbeing during the COVID-19 pandemic: Comparative case studies from 13 healthcare provider organisations globally. Glob. Health. 2022;18:24. doi: 10.1186/s12992-022-00818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Cancer Institute at the National Instituties of Health Definition of Mind-Body Modality. [(accessed on 28 May 2022)]; Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/mind-body-modality.
- 7.Dossett M.L., Fricchione G.L., Benson H. A New Era for Mind-Body Medicine. N. Engl. J. Med. 2020;382:1390–1391. doi: 10.1056/NEJMp1917461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vitetta L., Anton B., Cortizo F., Sali A. Mind-body medicine: Stress and its impact on overall health and longevity. Ann. N. Y. Acad. Sci. 2005;1057:492–505. doi: 10.1196/annals.1322.038. [DOI] [PubMed] [Google Scholar]
- 9.Clarke T.C., Barnes P.M., Black L.I., Stussman B.J., Nahin R.L. Use of Yoga, Meditation, and Chiropractors among U.S. Adults Aged 18 and Over. National Center for Health Statistics; Hyattsville, MD, USA: 2018. pp. 1–8. NCHS Data Brief, No 325. [PubMed] [Google Scholar]
- 10.Maric V., Mishra J., Ramanathan D.S. Using Mind-Body Medicine to Reduce the Long-Term Health Impacts of COVID-Specific Chronic Stress. Front. Psychiatry. 2021;12:585952. doi: 10.3389/fpsyt.2021.585952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liljestrand R., Martin S. Stress and Resilience among Healthcare Workers during the COVID-19 Pandemic: Consideration of Case Studies. Rehabil. Nurs. 2021;46:300–304. doi: 10.1097/RNJ.0000000000000344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trevino K.M., Raghunathan N., Latte-Naor S., Polubriaginof F.C.G., Jensen C., Atkinson T.M., Emard N., Seluzicki C.M., Ostroff J.S., Mao J.J. Rapid deployment of virtual mind-body interventions during the COVID-19 outbreak: Feasibility, acceptability, and implications for future care. Support. Care Cancer. 2021;29:543–546. doi: 10.1007/s00520-020-05740-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ben-Arye E., Zohar S., Keshet Y., Gressel O., Samuels N., Eden A., Vagedes J., Kassem S. Sensing the lightness: A narrative analysis of an integrative medicine program for healthcare providers in the COVID-19 department. Support. Care Cancer. 2022;30:1419–1426. doi: 10.1007/s00520-021-06546-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pikkel Igal Y., Meretyk I., Darawshe A., Hayek S., Givon L., Levy A., Sipori I., Nuriel Y., Bloch B., Buniak S., et al. Trends in Psychiatric Emergency Department Visits in Northern Israel during the COVID-19 Outbreak. Front. Psychiatry. 2021;12:603318. doi: 10.3389/fpsyt.2021.603318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryu S., Nam H.J., Baek S.H., Jhon M., Kim J.M., Kim S.W. Decline in Hospital Visits by Patients with Schizophrenia Early in the COVID-19 Outbreak in Korea. Clin. Psychopharmacol. Neurosci. 2022;20:185–189. doi: 10.9758/cpn.2022.20.1.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor G., Bylund C.L., Kastrinos A., Alpert J.M., Puig A., Krajewski J.M.T., Sharma B., Fisher C.L. Practicing Mindfulness through mHealth Applications: Emerging Adults’ Health-Enhancing and Inhibiting Experiences. Int. J. Environ. Res. Public Health. 2022;19:2619. doi: 10.3390/ijerph19052619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwon C.Y., Lee B. A Protocol for a Systematic Review and Meta-Analysis of Mind-Body Modalities to Manage the Mental Health of Healthcare Workers during the COVID-19 Era. Healthcare. 2021;9:1320. doi: 10.3390/healthcare9101320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 21.Critical Appraisal Skills Programme CASP (Randomised Controlled Trial) Checklist. [(accessed on 20 April 2022)]. Available online: https://casp-uk.net/casp-tools-checklists/
- 22.Higgins J.P., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Heart, Lung, and Blood Institute . Study Quality Assessment Tools. National Institutes of Health; Bethesda, MD, USA: 2013. [(accessed on 20 April 2022)]. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. [Google Scholar]
- 24.Guyatt G., Rennie D., Meade M.O., Cook D.J. Users’ Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. 3rd ed. McGraw-Hill; New York, NY, USA: 2015. [Google Scholar]
- 25.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gulzar M.M., Ahmad J., Tariq M., Syed A.A. Tackling stress among healthcare workers during the covid-19 pandemic. Ir. Med. J. 2020;113:108. [PubMed] [Google Scholar]
- 27.Horvath J. Mindfulness for dental nurses. Dent. Nurs. 2020;16:488–489. doi: 10.12968/denn.2020.16.10.488. [DOI] [Google Scholar]
- 28.Palmer J. Worker wellness: Stress reduction and mental health. Med. Environ. Update. 2020;30:1–3. [Google Scholar]
- 29.Reyes A.T. A Mindfulness Mobile App for Traumatized COVID-19 Healthcare Workers and Recovered Patients: A Response to “The Use of Digital Applications and COVID-19”. Community Ment. Health J. 2020;56:1204–1205. doi: 10.1007/s10597-020-00690-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robbins K.C. Support for Nurses during the Global COVID-19 Pandemic. Nephrol. Nurs. J. 2020;47:267–271. doi: 10.37526/1526-744X.2020.47.3.271. [DOI] [Google Scholar]
- 31.Vinayak S. Enhancing the Psychological Well-Being of Frontline Essential Service Providers of COVID-19. Ann. Neurosci. 2020;27:89–90. doi: 10.1177/0972753120965082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weingarten K., Galván-Durán A.R., D’Urso S., Garcia D. The Witness to Witness Program: Helping the Helpers in the Context of the COVID-19 Pandemic. Fam. Process. 2020;59:883–897. doi: 10.1111/famp.12580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahc M. Program Helps with Surgical Staff’s Stress and Burnout. Same-Day Surg. 2021;45:1–3. [Google Scholar]
- 34.Baverstock S., Hulatt I. Developing the mindful nurse practitioner. Ment. Health Pract. 2021;24:21–24. doi: 10.7748/mhp.2020.e1406. [DOI] [Google Scholar]
- 35.Bayon A. Wellness spaces for hospital staff at Confluence hospitals. Rev. L’infirmiere. 2021;70:36–37. doi: 10.1016/j.revinf.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 36.Chatmon B.N. Taking care of the caretaker: Navigating compassion fatigue through a pandemic. Aust. J. Adv. Nurs. 2021;38:1–4. doi: 10.37464/2020.383.603. [DOI] [Google Scholar]
- 37.Harwood L., Wilson B., Crandall J., Morano C. Resilience, Mindfulness, and Self-Compassion: Tools for Nephrology Nurses. Nephrol. Nurs. J. 2021;48:241–249. doi: 10.37526/1526-744X.2021.48.3.241. [DOI] [PubMed] [Google Scholar]
- 38.Morrow E., Call M., Ransco M., Hofmann K.M., Locke A. Sustaining Workforce Well-being: A Model for Supporting System Resilience during the COVID-19 Pandemic. Glob. Adv. Health Med. 2021;10 doi: 10.1177/2164956121991816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reidy J., MacDonald M.-C. Use of Palliative Care Music Therapy in a Hospital Setting during COVID-19. J. Palliat. Med. 2021;24:1603–1605. doi: 10.1089/jpm.2020.0739. [DOI] [PubMed] [Google Scholar]
- 40.Liu Y., Luo S.X., Ye J.L., Chen Y.Z., Li J.F., Li Y.X. The use of online MBSR audio in medical staff during the COVID-19 in China. Eur. Rev. Med. Pharmacol. Sci. 2020;24:10874–10878. doi: 10.26355/eurrev_202010_23451. [DOI] [PubMed] [Google Scholar]
- 41.Rodriguez-Vega B., Palao Á., Muñoz-Sanjose A., Torrijos M., Aguirre P., Fernández A., Amador B., Rocamora C., Blanco L., Marti-Esquitino J., et al. Implementation of a Mindfulness-Based Crisis Intervention for Frontline Healthcare Workers during the COVID-19 Outbreak in a Public General Hospital in Madrid, Spain. Front. Psychiatry. 2020;11:562578. doi: 10.3389/fpsyt.2020.562578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park E.R., Sylvia L.G., Streck J.M., Luberto C.M., Stanton A.M., Perez G.K., Baim M., Bliss C.C., Convery M.S., Crute S., et al. Launching a resiliency group program to assist frontline clinicians in meeting the challenges of the COVID-19 pandemic: Results of a hospital-based systems trial. Gen. Hosp. Psychiatry. 2021;68:111–112. doi: 10.1016/j.genhosppsych.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pinho L., Correia T., Sampaio F., Sequeira C., Teixeira L., Lopes M., Fonseca C. The use of mental health promotion strategies by nurses to reduce anxiety, stress, and depression during the COVID-19 outbreak: A prospective cohort study. Environ. Res. 2021;195:110828. doi: 10.1016/j.envres.2021.110828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Farris S.R., Grazzi L., Holley M., Dorsett A., Xing K., Pierce C.R., Estave P., O’Connell N., Wells R.E. Online Mindfulness Improves Emotional Health during COVID-19 for Patients with Migraine, Healthcare Providers, and the General Population. J. Headache Pain. 2021;22:172. doi: 10.1186/s10194-021-01293-9. [DOI] [Google Scholar]
- 45.Grabbe L., Higgins M.K., Baird M., Pfeiffer K.M. Impact of a Resiliency Training to Support the Mental Well-being of Front-line Workers: Brief Report of a Quasi-experimental Study of the Community Resiliency Model. Med. Care. 2021;59:616–621. doi: 10.1097/MLR.0000000000001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klatt M.D., Bawa R., Gabram O., Westrick A., Blake A. The Necessary Thread of Mindfulness Intervention Fidelity Assurance: Enabling an Organizational Strategy to Promote Health Care Professional Well-Being. Glob. Adv. Health Med. 2021;10:1–5. doi: 10.1177/21649561211052902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bazán P.R., de Azevedo Neto R.M., Lacerda S.S., Ribeiro M.W., Balardin J.B., Amaro E., Kozasa E.H. Can news with positive or negative content affect and a relaxation pause improve the emotional state of health care professionals? A randomized online experiment during COVID-19 pandemic. Internet Interv. 2021;26:100441. doi: 10.1016/j.invent.2021.100441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Buch K.A., Daye D., Wood M.J., Alvarez C., Del Carmen M.G., Mehta D.H., Bredella M.A. Wellness Program Implementation in an Academic Radiology Department: Determination of Need, Organizational Buy-in, and Outcomes. J. Am. Coll. Radiol. 2021;18:663–668. doi: 10.1016/j.jacr.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 49.Del Vecchio A., Homme J.L., Moschella P. Results from an innovative, theater-based communication course for emergency medicine residents in the COVID-19 era. Acad. Emerg. Med. 2021;28:S384. doi: 10.1111/acem.14249. [DOI] [Google Scholar]
- 50.Malik M., Peirce J., Wert M.V., Wood C., Burhanullah H., Swartz K. Psychological First Aid Well-Being Support Rounds for Frontline Healthcare Workers during COVID-19. Front. Psychiatry. 2021;12:669009. doi: 10.3389/fpsyt.2021.669009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smoller A.M. Emails provide staff support through COVID-19. J. Psychosoc. Oncol. 2021;39:324–326. doi: 10.1080/07347332.2021.1900485. [DOI] [PubMed] [Google Scholar]
- 52.Cotter P., Jhumat N., Garcha E., Papasileka E., Parker J., Mupfupi I., Currie I. A systemic response to supporting frontline inpatient mental health staff in coping with the COVID-19 outbreak. Ment. Health Rev. J. 2021;26:18–31. doi: 10.1108/MHRJ-05-2020-0026. [DOI] [Google Scholar]
- 53.Giordano F., Scarlata E., Baroni M., Gentile E., Puntillo F., Brienza N., Gesualdo L. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: A preliminary study. Arts Psychother. 2020;70:101688. doi: 10.1016/j.aip.2020.101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Klatt M.D., Bawa R., Gabram O., Blake A., Steinberg B., Westrick A., Holliday S. Embracing Change: A Mindful Medical Center Meets COVID-19. Glob. Adv. Health Med. 2020;9 doi: 10.1177/2164956120975369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coffey C., Hayley D.C. Wellness curriculum in geriatric medicine fellowship. J. Am. Geriatr. Soc. 2021;69:S122. doi: 10.1111/jgs.17115. [DOI] [Google Scholar]
- 56.Divya K., Bharathi S., Somya R., Darshan M.H. Impact of a Yogic Breathing Technique on the Well-Being of Healthcare Professionals during the COVID-19 Pandemic. Glob. Adv. Health Med. 2021;10:1–8. doi: 10.1177/2164956120982956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Emmanuel F.J., Vala Y., Dodia T. Study on effectiveness of staff welfare program regarding occupational stress during covid 19 pandemic among nursing officers. Med.-Leg. Update. 2021;21:263–268. doi: 10.37506/mlu.v21i1.2315. [DOI] [Google Scholar]
- 58.Fiol-DeRoque M.A., Serrano-Ripoll M.J., Jiménez R., Zamanillo-Campos R., Yáñez-Juan A.M., Bennasar-Veny M., Leiva A., Gervilla E., García-Buades M.E., García-Toro M., et al. A Mobile Phone-Based Intervention to Reduce Mental Health Problems in Health Care Workers during the COVID-19 Pandemic (PsyCovidApp): Randomized Controlled Trial. JMIR Mhealth Uhealth. 2021;9:e27039. doi: 10.2196/27039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Franco P.L., Christie L.M. Effectiveness of a one day self-compassion training for pediatric nurses’ resilience. J. Pediatr. Nurs. 2021;61:109–114. doi: 10.1016/j.pedn.2021.03.020. [DOI] [PubMed] [Google Scholar]
- 60.Heeter C., Allbritton M., Lehto R., Miller P., McDaniel P., Paletta M. Feasibility, acceptability, and outcomes of a yoga-based meditation intervention for hospice professionals to combat burnout. Int. J. Environ. Res. Public Health. 2021;18:2515. doi: 10.3390/ijerph18052515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu Y., Jiang T.T., Shi T.Y., Liu Y.N., Liu X.M., Xu G.J., Li F.L., Wang Y.L., Wu X.Y. The effectiveness of diaphragmatic breathing relaxation training for improving sleep quality among nursing staff during the COVID-19 outbreak: A before and after study. Sleep Med. 2021;78:8–14. doi: 10.1016/j.sleep.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Luton O.W., James O.P., Mellor K., Eley C., Hopkins L., Robinson D.B.T., Lebares C.C., Powell A., Lewis W.G., Egan R.J. Enhanced stress-resilience training for surgical trainees. BJS Open. 2021;5:zrab054. doi: 10.1093/bjsopen/zrab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Narayanan S., Tennison J., Cohen L., Urso C., Subramaniam B., Bruera E. Yoga-Based Breathing Techniques for Health Care Workers during COVID-19 Pandemic: Interests, Feasibility, and Acceptance. J. Altern. Complement. Med. 2021;27:706–709. doi: 10.1089/acm.2020.0536. [DOI] [PubMed] [Google Scholar]
- 64.Nijland J., Veling W., Lestestuiver B.P., Van Driel C.M.G. Virtual Reality Relaxation for Reducing Perceived Stress of Intensive Care Nurses during the COVID-19 Pandemic. Front. Psychol. 2021;12:706527. doi: 10.3389/fpsyg.2021.706527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nourian M., Nikfarid L., Khavari A.M., Barati M., Allahgholipour A.R. The Impact of an Online Mindfulness-Based Stress Reduction Program on Sleep Quality of Nurses Working in COVID-19 Care Units: A Clinical Trial. Holist. Nurs. Pract. 2021;35:257–263. doi: 10.1097/HNP.0000000000000466. [DOI] [PubMed] [Google Scholar]
- 66.Sanadgol S., Firouzkouhi M., Badakhsh M., Abdollahimohammad A., Shahraki-Vahed A. Effect of guided imagery training on death anxiety of nurses at COVID-19 intensive care units: A quasi-experimental study. Neuropsychiatr. Neuropsychol. 2021;15:83–88. doi: 10.5114/nan.2020.101290. [DOI] [Google Scholar]
- 67.So A.C.P., Hunter S., Chan K., Rigg A.S., Smith S., Miller R., Thillai K. A pilot study to prevent burnout in junior oncology doctors during the COVID-19 pandemic in a tertiary U.K. center. J. Clin. Oncol. 2021;39:11015. doi: 10.1200/JCO.2021.39.15_suppl.11015. [DOI] [Google Scholar]
- 68.Thimmapuram J., Pargament R., Bell T., Schurk H., Madhusudhan D.K. Heartfulness meditation improves loneliness and sleep in physicians and advance practice providers during COVID-19 pandemic. Hosp. Pract. 2021;49:194–202. doi: 10.1080/21548331.2021.1896858. [DOI] [PubMed] [Google Scholar]
- 69.Vajpeyee M., Tiwari S., Jain K., Modi P., Bhandari P., Monga G., Yadav L.B., Bhardwaj H., Shroti A.K., Singh S., et al. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. Int. J. Soc. Psychiatry. 2021;68 doi: 10.1177/00207640211006742. [DOI] [PubMed] [Google Scholar]
- 70.Ibrahim K., Komariah M., Herliani Y.K. The Effect of Mindfulness Breathing Meditation on Psychological Well-being: A Quasi-Experimental Study among Nurses Working for COVID-19 Patients. Holist. Nurs. Pract. 2022;36:46–51. doi: 10.1097/HNP.0000000000000464. [DOI] [PubMed] [Google Scholar]
- 71.Callus E., Bassola B., Fiolo V., Bertoldo E.G., Pagliuca S., Lusignani M. Stress Reduction Techniques for Health Care Providers Dealing With Severe Coronavirus Infections (SARS, MERS, and COVID-19): A Rapid Review. Front. Psychol. 2020;11:589698. doi: 10.3389/fpsyg.2020.589698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lavretsky H., Feldman Ph D.J. Precision Medicine for Breath-Focused Mind-Body Therapies for Stress and Anxiety: Are We Ready Yet? Glob. Adv. Health Med. 2021;10 doi: 10.1177/2164956120986129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Carlson L.E., Tamagawa R., Stephen J., Doll R., Faris P., Dirkse D., Speca M. Tailoring mind-body therapies to individual needs: Patients’ program preference and psychological traits as moderators of the effects of mindfulness-based cancer recovery and supportive-expressive therapy in distressed breast cancer survivors. J. Natl. Cancer Inst. Monogr. 2014;2014:308–314. doi: 10.1093/jncimonographs/lgu034. [DOI] [PubMed] [Google Scholar]
- 74.Zou L., Sasaki J.E., Wei G.-X., Huang T., Yeung A.S., Neto O.B., Chen K.W., Hui S.S.-C. Effects of Mind–Body Exercises (Tai Chi/Yoga) on Heart Rate Variability Parameters and Perceived Stress: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2018;7:404. doi: 10.3390/jcm7110404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cocchiara R.A., Peruzzo M., Mannocci A., Ottolenghi L., Villari P., Polimeni A., Guerra F., La Torre G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J. Clin. Med. 2019;8:284. doi: 10.3390/jcm8030284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jung S.-E., Ha D.-J., Park J.-H., Lee B., Kim M.-S., Sim K.-L., Choi Y.-H., Kwon C.-Y. The Effectiveness and Safety of Mind-Body Modalities for Mental Health of Nurses in Hospital Setting: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:8855. doi: 10.3390/ijerph18168855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Penrod N.M., Moore J.H. Why mind-body medicine is poised to set a new standard for clinical research. J. Clin. Epidemiol. 2019;116:167–170. doi: 10.1016/j.jclinepi.2019.05.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available in the article and Supplementary Materials.