Abstract
Lockdown resulting from the pandemic led to a change in the health habits of the computer workers community. Sedentary work, together with less active lifestyles, aggravated by the COVID-19 pandemic leads to impacts on physical activity (PA) and can contribute to the development of musculoskeletal symptoms (MSS). Aim(s): Understand the effects of lockdown on the perception of physical activity levels and on the perception of frequency of musculoskeletal symptoms, over periods of 12 months and 7 days, in computer workers. Methods: Longitudinal comparative study between 2019 (M1) and 2021 (M2), over 18 months, in 40 volunteer participants. The inclusion criteria were full-time workers aged between 18 and 65 and the exclusion criteria included diagnosis of non-work-related medical conditions. In addition to a socio-demographic questionnaire, the Nordic musculoskeletal questionnaire (NMQ) was used to evaluate the MSS and the International Physical Activity Questionnaire (IPAQ), was used to analyse the perception of the level of PA. These questionnaires were used in two assessment stages (M1 and M2). McNemar test and Wilcoxon paired test were used to evaluate the effect of lockdown on the perception of PA, and on the perception of frequency of musculoskeletal symptoms. Results: The MSS prevalence in the previous 12 months increased significantly in the neck (M1: 45.0%, M2: 62.5%, p = 0.046), in the shoulders (M1: 37.5%, M2: 55.0%, p = 0.033), and in the hands/wrists (M1: 25.0%, M2: 45.0%, p = 0.019). The mean pain score increased in the shoulders (1.43 ± 2.24, 2.35 ± 2.55, p = 0.003) and in the elbows (0.18 ± 0.59, 0.60 ± 1.34, p = 0.015). No differences were found in the PA between M1 and M2, but the weekly mean sitting time increased from 4.75 ± 2.26 to 6.26 ± 2.65 (p < 0.001). Conclusion: After 18 months it became clear that MSS perception increased mainly in the neck, shoulders and hands/wrists with a significant increase in pain intensity in the shoulder and elbow regions. The weekly sitting time increased significantly. Further studies are needed in order to determine the impact of teleworking in a pandemic context. But multifactor behind these results should be taken into account by health institutions and those responsible for the Prevention of Occupational Risks in Computer Workers in order to adopt educational strategies for the promotion of Physical activity (PA), in these workers.
Keywords: occupational health, musculoskeletal symptoms, physical activity level, homeworking, computer workers
1. Introduction
New technologies contributed not only to an improvement in working conditions, but also to the development of occupational and health problems. In this sense, the number of workers using computers for most of their working hours continues to grow at an ever-increasing rate [1] and results of various studies pointed out the presence of specific health symptoms associated with the use of computers [2,3].
The World Health Organization has characterized work-related illnesses as multifactorial, including physical, organisational, psychosocial, individual and sociocultural factors. Work-related musculoskeletal disorders have grown substantially in recent decades and are the most important causes of absence and disability at work [4,5,6].
Office workers, or computer workers (CWs), are considered to be those who work for approximately two-thirds of their working hours on primary tasks that generally involve the use of computers and a sitting position [7,8,9]. These workers are therefore at increased risk of a number of chronic diseases due to their sedentary behaviour [10,11].
Several risk factors may be associated with the development of musculoskeletal symptoms (MSS). The ones reported in the literature are repetitive activities, maintained postures, long working hours, inadequate furniture and lack of conditions to perform the work. Repetition of movements, maintained positioning and lack of pauses are common in computer workers [4,5]. This sedentary work leads to poor postures, flexion postures adopted during long periods of work, associated with repetition of tasks, causing greater tension in muscle and ligament structure, thus increasing the prevalence of work-related musculoskeletal injuries [5,8,10,12,13,14,15,16]. According to several studies, the cervical and lumbar regions are the most affected, followed by disorders in at least one region of the upper limbs [2,3,8,17,18,19,20,21,22].
Remaining in the sitting posture, associated with the lack of postural variability, generates several changes in the musculoskeletal structures: it increases the internal pressure in the nucleus of the intervertebral disc, stretches all the structures of the spine, reduces the return circulation of the lower limbs and promotes the development of inflammatory processes in bone and muscle structures with associated painful symptoms [23,24,25]. Other studies concluded that long working hours with little or no interruption are risk factors for triggering pain in the cervical region, shoulders and other segments of the spine [4,26].
Some studies identified the great impact of work-related MSSs in economic terms (loss of productivity and higher social expenditure). In Germany for example, musculoskeletal and connective tissue disorders accounted for EUR 17.2 billion of production loss in 2016 [27].
Among the therapeutic approaches to decrease MSS, several authors recommend the regular practice of Physical Activity (PA), which is defined by the WHO as any body movement produced by the muscles that requires energy expenditure. It is observed that a large part of the population that has MSS does not perform PA regularly, with the justification of lack of time, work overload and lack of motivation, among others [4,6,28].
December 2019 saw the appearance of COVID-19, a communicable disease caused by infection of SARS-CoV-2 coronavirus [29]. This health condition spread, affecting several countries, leading the WHO to declare a pandemic that continues today. As such, mandatory teleworking was ordered to prevent transmission. The COVID-19 pandemic has shaken the structures of contemporary society and required a reorganisation of companies and societies in general. Teleworking, home office, was already a practice in some companies and, with the new coronavirus, it became mandatory for all [30].
The need for a lockdown led to a fundamental change in the lifestyles of the entire population. Although this strategy proved to be effective in combating the pandemic, the quarantine had significant effects on other relevant aspects of the health of the population that was subject to this lockdown [31,32]. Restrictions on movement and the ban on carrying out activities in outdoor spaces inevitably disrupted everybody’s routines, increasing the likelihood of individuals experiencing reduced levels of physical activity, an increase in immobility, anxiety and depression, which significantly affects health and increases several health risk factors [33].
This meant that workers’ homes had to become a place of work, education and leisure. Teleworking has some benefits, such as a better family-work balance, reduced fatigue and increased productivity [34]. However, factors such as a lack of clear definition of physical and organisational boundaries between work and home, extended working hours and limited support from organisations can negatively impact the physical and mental health of workers [34], leading to a decrease in health-related quality of life [35,36]. Against this background, recent reviews investigating the effects of physical exercise on the health of office workers [22,37,38] reported significant and protective effects of physical exercise on musculoskeletal pain symptoms (i.e., neck pain and low back pain) [22,38,39]. Recent studies carried out during the pandemic also suggested that regular physical activity can be an accessible auxiliary tool for the immune system against possible COVID-19 infection [40].
Improving PA to reduce MSS is therefore a challenge for occupational health, because the work context is crucial for the development and creation of health promotion actions within the scope of work activity [38,41,42]. In this context, it is extremely important to investigate the perception of PA and perception of MSS that computer workers have and how to change attitudes in order to introduce successful programmes to promote health-oriented physical activity in a variety of social groups [42,43,44].
The aim of this study was to compare (i) the frequency of musculoskeletal symptoms and (ii) the perception of physical activity in computer workers at an automotive sector company in northern Portugal, between the pre-pandemic and pandemic periods. In addition, specific objectives were defined to verify the difference in the frequency of symptoms at the two evaluation moments; to compare the most affected anatomical regions between the two periods; to investigate the difference in the pain score in those anatomic regions in the pre-pandemic and pandemic periods related to the weekly sitting time in both moments. As such, the study hypothesis was that lockdown led to an increase in the perception of musculoskeletal symptoms and the perception of physical activity in computer workers.
2. Materials and Methods
2.1. Study Design
A comparative longitudinal study was performed with two data collection moments, the first one from 5th to 12th of June 2019, and the second between 10th of December 2020 and 29th of January 2021. In addition, our study can be considered single blind, since the data were processed by an independent observer, after self-completion online, and analysed by a different group of observers.
2.2. Ethical Procedures
Data were collected from adult CWs. Ethical approval for this study was obtained from the Ethics Committee at the Abel Salazar Institute of Biomedical Sciences CHUP/ICBAS (963). All the participants were informed about the study aims and procedures and they provided written consent for their participation. The participants could refuse to participate in the study at any point under Law 67/98 of 26 October 1998 (Law on the Protection of Personal Data (transposing into the Portuguese legal system Directive 95/46/EC of the European Parliament and of the Council of 24 October 1995 on the protection of individuals with regard to the processing of personal data and on the free movement of such data) and the World Medical Association Declaration of Helsinki Ethical Principles for Medical Research.
2.3. Sample Recruitment and Elegibility Criteria
The target population of this study consisted of 424 adult CWs at an automotive sector company in northern Portugal.
Defined inclusion criteria were: full-time employees aged between 18 and 65 who had signed the informed consent. The exclusion criteria included diagnosis of non-work-related medical conditions, such as: ankylosing spondylitis, chronic joint diseases, neurological diseases, relevant (osteoarticular) surgeries, significant artificial joint replacement, articulation, multiple sclerosis, myotonic dystrophy or neurodegenerative diseases and congenital malformations of the musculoskeletal system [20,45].
Before the study questionnaire was applied, a visit to the company was made in order to establish initial contact with the possible participants and their work environment.
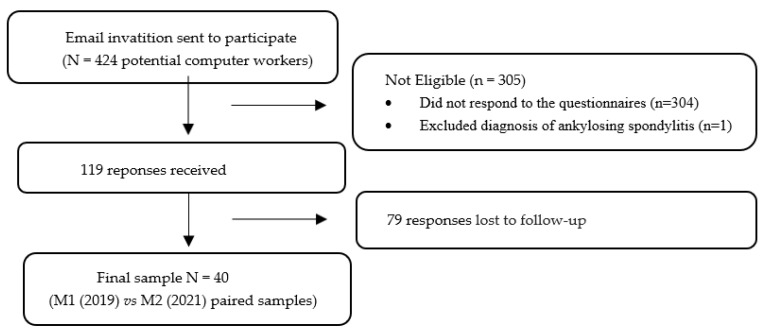
The study questionnaires were entered into the Google Forms platform to make them faster and more accessible for the 424 computer workers to complete. The questionnaire link was provided to the potential participants via email by the company’s human resources management to safeguard the confidentiality of the participants’ personal emails. Previously, all the computer workers were informed by the company’s human resources department about the objectives of the study and, after that, the questionnaires were presented. Subsequently, time was allotted to clarify any doubts and questions that remained. The forms were filled out in two stages. At a first moment (M1) the questionnaire was sent in June of 2019 to the company’s 424 workers. The second moment (M2) was between December 2020 and January 2021. A total of 119 responses were obtained, 304 individuals refused to participate and 1 participant was excluded for having a diagnosis of Ankylosing Spondylitis, thus forming a final non-probabilistic sample of 40 computer workers (Figure 1).
Figure 1.
Flow diagram of the recruitment process.
2.4. Questionnaire for Collecting Data
The final questionnaire consisted of three parts. One with sociodemographic questions, a second with the Nordic Musculoskeletal Questionnaire (NMQ-vPt) [46] and a third with the International Physical Activity Questionnaire—short version [47]. A pilot study was carried out to test the procedures. The survey was designed to take no longer than 15 min to complete and it was a self-administered questionnaire.
2.5. Instruments
2.5.1. Sociodemographic Questionnaire
This questionnaire was designed by the main researcher to characterise the sample and collect sociodemographic data [44]. General information such as sex, birth date, relationship status and education, anthropometric variables, such as weight and height, were self-reported, followed by questions about participants’ medical history and lifestyle and, lastly, work-related questions. The Cronbach’s Alpha of the sociodemographic questionnaire was 0.72—it was calculated through the “optimal scaling” procedure implemented in SPSS. To capture additional contextual information, the number of hours per week in domestic and leisure activities and sitting time working were included.
2.5.2. Nordic Musculoskeletal Questionnaire (NMQ-vPt)
The NMQ is validated for the Portuguese population and facilitates the evaluation of musculoskeletal symptoms [46]. It consists of questions related to nine anatomical regions (neck, shoulders, elbows, wrist, thoracic region, lumbar region, hips, knees, ankles and feet). The individual is asked if he/she had any symptoms in the last 12 months and in the last 7 days in one or more regions and if in the last year he/she has had to avoid his/her normal day to day activities due to symptoms. The anatomical regions are highlighted on a body chart so that there is no doubt about the area they are referring to [48]. The questionnaire also presents a numerical pain scale (NPS) that allows the study participant to classify their pain in the “last 7 days” according to the indicated regions.
This questionnaire has moderate criterion validity and good reliability and is validated for the Portuguese population [46]. The questionnaire presents psychometric values for reliability; test-retest using the Kappa correlation coefficient ranged between 0.677 and 1. The internal validity of the questionnaire was verified by the Kuder-Richarson correlation coefficient, which was good (0.855) [46].
2.5.3. International Physical Activity Questionnaire (IPAQ)–Short Version
The short version IPAQ makes it possible to evaluate the perception of PA level and sedentary behaviour. It is part of an international effort to find an instrument that may be used worldwide in order to determine the level of physical activity of several populations. This instrument has been validated for several countries simultaneously. The validity and reliability of questionnaire published by Craig et al. (2003) has the main objective of developing a self-reported measure of physical activity suitable for assessing population levels of physical activity across countries including for the Portuguese population [47,49]. It consists of 9 questions and provides information on sedentary activity time, vigorous and moderate PA and walking time. Any PA that the participants perform, either at work or on household chores and during their free time, can be included [50].
For the IPAQ data analysis, the Guidelines for data and processing of international physical activity questionnaire were used [51]. These guidelines provide reference metabolic equivalent values (MET). Walking corresponds to 3.3 METs, moderate PA to 4.0 METs and vigorous PA to 8.0 METs. They also have formulas to quantify the total PA per minute/week. The final score (MET minute/week) is the sum of the scores of each PA level:
Walking METs = 3.3 × minutes’ walk × number of days walking
Moderate METs = 4.0 × minutes of moderate activity × number of days doing moderate activity
Vigorous METs = 8.0 × minutes of vigorous activity × number of days doing vigorous activity
Total METs = METs walking
METs of moderate activity + METs of vigorous activity.
Each participant is classified into 1 of 3 categories according to the final score; low, moderate and high level of PA. If the participant does not meet the conditions to enter the other categories, he/she is classified as low PA.
To fall within the moderate PA level category, a participant must meet one of the following criteria: having 3 or more days of vigorous activity for at least 20 min a day or 5 days or more of moderate activity and/or walking for at least 30 min a day, or 5 or more days of any combination of walking, moderate or vigorous intensity activities that reach a minimum of at least 600 MET-minutes/week.
Finally, to qualify for a high level of PA the individual needs to meet one of the following criteria: have vigorous intensity activity on at least 3 days reaching a minimum of 1500 MET-minute/week of total PA; or 7 days of any combination of walking, moderate intensity or vigorous intensity activities achieving a minimum PA of 3000 MET-minute/week.
Issues related to sedentary behaviour are not included in the calculation of minute/week MET, as these were developed as separate indicators [51].
This questionnaire, according to [50] has a criterion validity of r = 0.30 and a reliability of r = 0.76 (95% CI 0.73–0.77). To calculate the score, an open access Excel document developed by Dr Hoi Lun Cheng [52] was used. No cases were excluded during the processing of IPAQ data, following the IPAQ guidelines [51].
2.6. Statistics
Mean and standard deviation were used for describing the continuous variables, and absolute and relative frequencies were used for categorical variables.
For the comparison between M1 and M2 (paired samples), the McNemar test and the paired Wilcoxon test were used for binary variables and for continuous variables, respectively. The effect size of the differences of continuous variables was evaluated with Cohen’s d [53] (d = 0.20 small effect, d = 0.50 medium effect, d = 0.80 large effect). A significance level of 5% was considered for the inferential tests.
Data analysis was performed with IBM SPSS Statistics®, version 27.0 (Statistical Package for the Social Sciences ®, IBM Corp Armonk, NY, USA) [54].
3. Results
3.1. Sample Profile
Table 1 shows the sample characteristics in M1. Sample included 40 computer workers aged from 25 to 50 (M = 35.75, SD = 7.32), mostly men (65.0%), married/cohabitation (55.0%), and with secondary education (35.0%) or a Bachelor′s degree (45.0%). Half of the sample was overweight: 30.0% were pre-obese and 20.0% were obese.
Table 1.
Sample characteristics in M1 (n = 40).
| n | % | |
|---|---|---|
| Gender | ||
| Female | 14 | 35.0 |
| Male | 26 | 65.0 |
| Marital Status | ||
| Single | 15 | 37.5 |
| Married/Cohabitation | 22 | 55.0 |
| Separated/Divorced | 3 | 7.5 |
| Educational Attainment | ||
| Middle school | 1 | 2.5 |
| Secondary school | 14 | 35.0 |
| Bachelor’s degree | 18 | 45.0 |
| Master’s degree | 7 | 17.5 |
| BMI Category | ||
| Low weight | 1 | 2.5 |
| Normal weight | 19 | 47.5 |
| Pre-obesity | 12 | 30.0 |
| Obesity | 8 | 20.0 |
| Mean | Standard Deviation | |
| Age (years) | 35.75 | 7.32 |
| Height (m) | 1.72 | 0.10 |
| Body mass (kg) | 76.58 | 16.86 |
| BMI (kg/m2) | 25.72 | 4.97 |
BMI—body mass index.
3.2. Musculoskeletal Symptomatology
Table 2 shows the results of musculoskeletal symptomatology in M1 and in M2.
Table 2.
Musculoskeletal symptomatology, limitation in daily activities and pain intensity in M1 and M2 (n = 40).
| Musculoskeletal Symptoms | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anatomical Regions |
Symptomatology Last 12 Months |
ADL Limitation Last 12 Months |
Symptomatology Last 7 Days |
Pain Intensity | |||||||||
| M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | ||||||
| n (%) | n (%) | p (1) | n (%) | n (%) | p (1) | n (%) | n (%) | p (1) | M(SD) | M(SD) | p (2) | d | |
| Neck | 18 (45.0) | 25 (62.5) | 0.046 | 7 (17.5) | 6 (15.0) | 0.500 | 9 (22.5) | 15 (37.5) | 0.073 | 1.83 (2.26) | 2.23 (2.42) | 0.156 | 0.17 |
| Shoulders | 15 (37.5) | 22 (55.0) | 0.033 | 2 (5.0) | 6 (15.0) | 0.109 | 4 (10.0) | 10 (25.0) | 0.055 | 1.43 (2.24) | 2.35 (2.55) | 0.003 | 0.38 |
| Elbows | 3 (7.5) | 8 (20.0) | 0.063 | 0 (0.0) | 1 (2.5) | 0.500 | 0 (0.0) | 3 (7.5) | 0.125 | 0.18 (0.59) | 0.60 (1.34) | 0.015 | 0.41 |
| Wrists and hands | 10 (25.0) | 18 (45.0) | 0.019 | 1 (2.5) | 5 (12.5) | 0.063 | 2 (5.0) | 2 (5.0) | 0.750 | 0.65 (1.19) | 0.93 (1.56) | 0.183 | 0.20 |
| Thoracic | 5 (12.5) | 4 (10.0) | 0.500 | 1 (2.5) | 3 (7.5) | 0.250 | 1 (2.5) | 0 (0.0) | 0.500 | 0.38 (1.21) | 0.20 (0.56) | 0.273 | 0.19 |
| Low back | 22 (55.0) | 24 (60.0) | 0.395 | 6 (15.0) | 7 (17.5) | 0.500 | 10 (25.0) | 13 (32.5) | 0.291 | 2.10 (2.72) | 2.38 (2.48) | 0.330 | 0.11 |
| Hips and thighs | 11 (27.5) | 8 (20.0) | 0.291 | 1 (2.5) | 1 (2.5) | 0.750 | 2 (5.0) | 2 (5.0) | 0.750 | 0.68 (1.49) | 0.48 (1.04) | 0.363 | 0.16 |
| Knees | 14 (35.0) | 16 (40.0) | 0.387 | 3 (7.5) | 2 (5.0) | 0.500 | 5 (12.5) | 5 (12.5) | 0.656 | 1.13 (2.03) | 1.00 (1.52) | 0.367 | 0.07 |
| Ankles and feet | 12 (30.0) | 9 (22.5) | 0.304 | 1 (2.5) | 2 (5.0) | 0.500 | 2 (5.0) | 4 (10.0) | 0.313 | 0.70 (1.56) | 0.50 (1.40) | 0.280 | 0.13 |
n—absolute frequency; %—relative frequency; M—mean; SD—standard deviation; ADL—activities of daily life; d—Cohen´s d; (1) significant value of McNemar test; (2) significant value of paired Student’s t-test.
Results comparing M1 and M2 showed that the percentage of computer workers with symptoms in the past 12 months increased in the neck (45.0% in M1, 62.5% in M2, p = 0.046), shoulders (37.5% in M1, 55.0% in M2, p = 0.033), elbows (7.5% in M1, 20.0% in M2, p = 0.063), and wrists and hands (25.0% in M1, 45.0% in M2, p = 0.019).
Regarding the activities of daily life limitations in the past 12 months, the only increase found was in the wrists and hands (2.5% in M1, 12.5% in M2, p = 0.063), with significant differences at a 10% level.
As for the symptoms in the past 7 days, the percentages increased in the neck (22.5% in M1, 37.5% in M2, p = 0.073) and in the shoulders (10.0% in M1, 25.0% in M2, p = 0.055), with significant differences at a 10% level.
The mean pain intensity increased significantly in two regions: the shoulders (M1: M = 1.43, SD = 2.24; M2: M = 2.35, SD = 2.55; p = 0.003; d = 0.38) and the elbows (M1: M = 0.18, SD = 0.59; M2: M = 0.60, SD = 1.34; p = 0.015; d = 0.015).
3.3. Physical Activity and Sitting Time
Regarding physical activity and sitting time, Table 3 shows that there were no differences in the physical activity indicators (METs, physical activity level, meeting the WHO recommendations) between M1 and M2.
Table 3.
Physical activity and sitting time in M1 and M2 (n = 40).
| M1 | M2 | p | d | |
|---|---|---|---|---|
| Physical Activity (METs) | M (SD) | M (SD) | ||
| Vigorous (minutes/week) | 791.00 (1252.18) | 1044.00 (1739.67) | 0.291 (1) | 0.17 |
| Moderate (minutes/week) | 340.00 (576.30) | 279.50 (519.69) | 0.241 (1) | 0.11 |
| Walking (minutes/week) | 526.76 (594.86) | 727.24 (925.81) | 0.281 (1) | 0.26 |
| Total (minutes/week) | 1657.80 (1825.07) | 2050.78 (2675.69) | 0.475 (1) | 0.17 |
| Physical Activity Level | n (%) | n (%) | ||
| Low | 16 (40.0%) | 16 (40.0%) | 0.372 (1) | |
| Medium | 15 (37.5%) | 13 (32.5%) | ||
| High | 9 (22.5%) | 11 (27.5%) | ||
| Meets WHO recommendations | n (%) | n (%) | ||
| No | 21 (52.5%) | 22 (55.0%) | 0.500 (2) | |
| Yes | 19 (47.5%) | 18 (45.0%) | ||
| Sitting time | M (SD) | M (SD) | ||
| Weekday (hours/day) | 4.85 (3.05) | 6.75 (3.41) | < 0.001 (1) | 0.59 |
| Weekend day (hours/day) | 4.48 (2.59) | 5.03 (2.61) | 0.064 (1) | 0.21 |
n—absolute frequency; %—relative frequency; M—mean; SD—standard deviation; ADL—activities of daily life; d—Cohen’s d; (1) significant value of paired Wilcoxon test; (2) significant value of McNemar test.
The mean sitting time on weekdays increased significantly from 4.85 (SD = 3.05) in M1 to 6.75 (SD = 3.41) in M2 (p < 0.001, d = 0.59). There was also an increase in the mean sitting time on weekend days (M1: M = 4.48, SD = 2.59; M2: M = 5.03, SD = 2.61), however, the differences were not significant (p = 0.064), and the effect size of the differences was small (d = 0.21).
4. Discussion
This study evaluated the effects of lockdown on the perception of physical activity, sitting time levels and perception of frequency of musculoskeletal symptoms over periods of 12 months and 7 days in CWs.
Comparing the pre-pandemic and pandemic results regarding the practice of PA, it was found that there was a decrease in the percentage of workers classified as having a medium category of PA and an increase in the percentage of workers classified as having a vigorous category. However, this change was not enough to meet the PA standards recommended by the WHO [6]. These changes in PA levels may be explained by the isolation measures imposed by the pandemic, as people could only leave the house to perform PA, with a number of individuals opting for activities with higher metabolic expenditure (such as running).
A growing number of studies from the COVID-19 period reported that the limitations imposed by the pandemic lockdown are associated with significant negative changes in physical activity habits [55,56]. Also, eating behaviours and lifestyle were affected by the lockdown, with increased consumption of unhealthy food, which may have a possible negative influence on immune response [31]. Negative psychological outcomes like increasing levels of depression, anxiety and stress were also observed during lockdown [57]. Understanding the possible association between these factors and decreasing physical activity habits will be important for the development of further interventions.
According to the literature, CWs are prone to MSS in various body regions [58,59,60,61,62,63] and regular PA practice has been shown to be a beneficial strategy to reduce the onset of MSS and lead to a reduction in pain intensity [64,65,66,67,68,69]. In previous works by our group, we also found that MSS were less frequent in CWs who followed PA recommendations [69] and we also observed a large effect of PA in the reduction of pain in CWs [68]. Additionally, PA practice can result in lower BMI, body fat percentage and blood pressure, as well as better job performance [64]. The increased systemic circulation and vasodilator capability caused by PA [10,28,58,65,70] could be one explanation for the reduction in MSS rates in this group. It is also important to remember that PA should include activities for all body parts to prevent worker’s MSS [69].
The average sitting time on weekdays increased significantly in the pandemic period. Teleworking has been associated with more time spent in sedentary activities [71,72]. In this sense our findings agree with recent studies in which the need to work from home has been shown to lead to more hours spent sitting, in online meetings and working [72,73]. The sudden change to having to work from home caused a decrease in ergonomics and relative comfort in the workspace. As in other studies, our analysis suggests that this fact may be associated with an increase in MSS during the period of lockdown [66].
The bodily discomforts generated by work can affect any individual who follows a work pattern where activities and tasks are poorly performed, due to the poor adaptation of the environment and the work routine to the individual capabilities and characteristics of each worker. Several studies indicate that the presence of symptoms in different body regions is due to the flexion postures adopted during long periods of work, associated with the repetition of the task, causing greater tension in the muscular and ligament structures [40,41,42]. Inadequate postural habits, such as those imposed by the sitting position and the repetitiveness of certain movements, such as CW’s, act on the human organism as an overload and are capable of leading its various defence mechanisms to compensatory actions [74]. In the sitting position, the weight of the body exerts significant pressure on the vertebral column, causing the water contained in the gelatinous substance of the nucleus to exit through the orifices of the vertebral plateau towards the centre of the vertebral bodies. Maintaining this type of posture for a long time makes the core less hydrated and thick at the end of the day. During the night, with rest, the pressure exerted on the disc decreases considerably, due to the body being relaxed. At this moment, the opposite occurs, that is, the core attracts water, returning to its initial thickness at the end of the night. However, for the disc to return to its normal thickness, a significant period of rest is necessary [74].
However, the form of work is not necessarily the only determinant of the causality of these symptoms, it is necessary to take into account other multifactor, including physical and psychological factors present inside and outside the work environment [75,76].
Regarding the most affected anatomical regions, in both moments of analysis, the regions that reported increased symptoms in the last 12 months were neck, shoulders, elbows, wrists and hands; these findings were also reported in previous studies [65]. As previously mentioned, staying in the sitting position for long periods is a risk factor for the increase of this symptomatology [65].
We also found that those who had symptoms in the last 7 days in the aforementioned regions (as well as in the other variables of the Nordic questionnaire) had a higher average number of sitting hours per week in relation to individuals who did not report the presence of these symptoms. Another factor that may have led to the worsening of symptoms and that was not taken into account in this study are the ergonomic issues of the work environment at home, because, although the technical gesture has not changed, the organisation of the work space at home is different and can be less adaptable to the needs of workers compared to the conditions offered at this company [71].
Study Limitations
One of the limitations has to do with the low number of participants in the study meaning that the sample is not representative of the population and therefore has no external validity. Also, the fact that the gender was mostly male, which led to heterogeneity between the groups. Furthermore, it was not possible to verify whether the workers answered the questionnaire themselves as it was answered online. As such, many personal variables, including physiological, behavioural and psychological factors, may influence motivation to join physical activity programmes.
As such, to make physical activity part of the daily life of CWs, it will be important to understand common barriers to physical activity and to create strategies to overcome them. Regarding the applied assessment, both biases are dual issues, taking into account that the questions referred to the past. As for the population under study, it belongs to a specific population of a company that has adopted strategies intended to promote the health of its workers by applying various health promotion actions.
In future works it will be important to follow up these workers in order to analyse whether the new physical habits resulting from lockdown and teleworking are maintained. We also suggest the analysis of variables such as sleep and the ergonomics of the workspace that were not taken into account in this study and are referred to as risk factors for MSS symptoms. In addition, more objective PA assessment measures (such as a pedometer) could be introduced to obtain more reliable data from the practice of PA.
Considering the well-established link between physical activity and health, it is likely that persistent or increased physical inactivity has medium or long-term implications for people’s physical and mental health, as well as for the quality of life of each individual. More occupational health efforts should be made to boost the level of physical activity in the workplace, in particular for groups at higher risk of inactivity or reduced physical activity, such as computer workers. Physically active people are more content and more alert [31]. There is evidence in the literature that exercise is beneficial for mental health; it reduces depression, negative moods and anxiety, and improves self-esteem and cognitive functioning [77].
Our study contributes to increasing the knowledge of this important topic, giving support for occupational risk prevention of MSSs. In line with the results obtained in this study, we recommend the introduction of active health education strategies to train workers who are involved in jobs with repetitive tasks, to increase PA levels, and greater efforts to prepare the home environment as a more comfortable and ergonomic workplace for CWs. These factors can play an important role in a healthier transition to working from home.
5. Conclusions
The main strength of this study was evaluating the impact of lockdown on the perception of physical activity, sitting time levels and the perception of frequency of musculoskeletal symptoms over periods of 12 months and 7 days in computer workers.
We conclude that MSS perception increased mainly in the neck, shoulders and hands/wrists with a significant increase in pain intensity in the shoulder and elbow regions. It was clear that weekly sitting time increased significantly. Multifactor behind these results must be taken into account by health institutions and those responsible for the Prevention of Occupational Risks in Computer Workers. These findings are also important as they can be useful to adopt educational strategies for the promotion of Physical activity in the workplace, reflecting a positive perception of health in these workers.
More studies are needed to understand the effects of the lockdown on CWs, but it seems clear that there is a need to introduce exercise programmes to promote physical activity, as this is a health promoting element for the prevention of MSS in computer workers. In this context, further analysis is needed to confirm the observed results, but there seems to be a clear need to direct efforts and resources towards improving computer workers’ PA by boosting CWs’ motivation to join exercise programmes in the workplace and introducing suitable exercise programmes and policies, with the consequent social, economic and environmental impacts on physically active, healthy populations.
Acknowledgments
The authors thank all the computer workers from the company for the support given to the study, Abel Salazar Institute for Biomedical Sciences for hosting the study.
Author Contributions
Conceptualisation, S.M., P.C.S., M.S.F. and J.M.; methodology, S.M., P.C.S., M.S.F., J.M., C.G., C.M. and S.L.; software, S.M., C.G., P.C.S., M.S.F. and J.M.; validation, S.M., P.C.S., M.S.F., J.M., C.M. and S.L.; formal analysis, S.M., C.G., M.B.C., P.C.S., M.S.F. and J.M.; investigation, S.M., P.C.S., M.S.F., J.M., C.M. and S.L.; resources, S.M., M.B.C., P.C.S., M.S.F., J.M., C.M. and S.L.; data curation, S.M., M.B.C., P.C.S., C.G., M.S.F. and J.M.; writing—original draft preparation, S.M., P.C.S., M.S.F. and J.M.; writing—review and editing, S.M., M.B.C., P.C.S., M.S.F. and J.M.; visualization, S.M., M.B.C., P.C.S., M.S.F. and J.M.; supervision, M.B.C., P.C.S., C.G., M.S.F., J.M. and C.M.; project administration, S.M., M.B.C., P.C.S., M.S.F., J.M., C.M. and S.L. All the authors have contributed substantially to the work reported. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the ICBAS (CHUP/ICBAS-963).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available as the confidentiality agreement reached with the company does not allow public disclosure of the data available.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eurostat E.C. Health and Safety at Work in Europe (1999–2007) Publications Office of the European Union; Luxembourg: 2010. A Statistical Portrait. [Google Scholar]
- 2.Akodu A., Akinfeleye A. Work-related musculoskeletal disorders of the upper extremity with reference to working posture of secretaries. S. Afr. J. Occup. Ther. 2015;45:16–22. doi: 10.17159/2310-3833/2015/v45n3/a4. [DOI] [Google Scholar]
- 3.Eijckelhof B.H., Bruno Garza J.L., Huysmans M.A., Blatter B.M., Johnson P.W., van Dieen J.H., van der Beek A.J., Dennerlein J.T. The effect of overcommitment and reward on muscle activity, posture, and forces in the arm-wrist-hand region—A field study among computer workers. Scand. J. Work Environ. Health. 2013;39:379–389. doi: 10.5271/sjweh.3346. [DOI] [PubMed] [Google Scholar]
- 4.Hugue T.D., Júnior A.A.P. Prevalência de dor Osteomuscular Entre os Funcionários Administrativos da UNIFEBE. Revista da UNIFEBE 2011. [(accessed on 19 July 2019)]. Available online: https://periodicos.unifebe.edu.br/index.php/RevistaUnifebe/article/view/54.
- 5.Waongenngarm P., van der Beek A.J., Akkarakittichoke N., Janwantanakul P. Perceived musculoskeletal discomfort and its association with postural shifts during 4-h prolonged sitting in office workers. Appl. Ergon. 2020;89:103225. doi: 10.1016/j.apergo.2020.103225. [DOI] [PubMed] [Google Scholar]
- 6.Bull F.C., Al-Ansari S.S., Biddle S., Borodulin K., Buman M.P., Cardon G., Carty C., Chaput J.P., Chastin S., Chou R., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ijmker S., Blatter B.M., van der Beek A.J., van Mechelen W., Bongers P.M. Prospective research on musculoskeletal disorders in office workers (PROMO): Study protocol. BMC Musculoskelet. Disord. 2006;7:55. doi: 10.1186/1471-2474-7-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker R., Coenen P., Howie E., Williamson A., Straker L. The Short Term Musculoskeletal and Cognitive Effects of Prolonged Sitting During Office Computer Work. Int. J. Environ. Res. Public Health. 2018;15:1678. doi: 10.3390/ijerph15081678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chambers A.J., Robertson M.M., Baker N.A. The effect of sit-stand desks on office worker behavioral and health outcomes: A scoping review. Appl. Ergon. 2019;78:37–53. doi: 10.1016/j.apergo.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 10.Arslan S.S., Alemdaroğlu İ., Karaduman A.A., Yilmaz Ö.T. The effects of physical activity on sleep quality, job satisfaction, and quality of life in office workers. Work. 2019;63:3–7. doi: 10.3233/WOR-192902. [DOI] [PubMed] [Google Scholar]
- 11.Hu F.B., Li T.Y., Colditz G.A., Willett W.C., Manson J.E. Television Watching and Other Sedentary Behaviors in Relation to Risk of Obesity and Type 2 Diabetes Mellitus in Women. JAMA. 2003;289:1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 12.Juul-Kristensen B., Søgaard K., Støyer J., Jensen C. Computer users’ risk factors for developing shoulder, elbow and back symptoms. Scand. J. Work. Environ. Health. 2004;30:390–398. doi: 10.5271/sjweh.827. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez L.R., Lucca S.R., Kitamura S., Oliveira J.I., Lido A.V., Manzano L.F., Soares A.L. Contribuições para a investigação de lesões por esforços repetitivos—Distúrbios ósteomusculares relacionados com o trabalho em membros superiores. Rev. Soc. Bras. Clín. Méd. 2008;6:72–78. [Google Scholar]
- 14.Paksaichol A., Janwantanakul P., Purepong N., Pensri P., van der Beek A.J. Office workers’ risk factors for the development of non-specific neck pain: A systematic review of prospective cohort studies. Occup. Environ. Med. 2012;69:610–618. doi: 10.1136/oemed-2011-100459. [DOI] [PubMed] [Google Scholar]
- 15.Smith M.D., Kwan C.S.J., Zhang S., Wheeler J., Sewell T., Johnston V. The Influence of Using a Footstool during a Prolonged Standing Task on Low Back Pain in Office Workers. Int. J. Environ. Res. Public Health. 2019;16:1405. doi: 10.3390/ijerph16081405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ye S., Jing Q., Wei C., Lu J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: A cross-sectional study. BMJ Open. 2017;7:e014914. doi: 10.1136/bmjopen-2016-014914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eltayeb S., Staal J.B., Kennes J., Lamberts P.H., de Bie R.A. Prevalence of complaints of arm, neck and shoulder among computer office workers and psychometric evaluation of a risk factor questionnaire. BMC Musculoskelet. Disord. 2007;8:68. doi: 10.1186/1471-2474-8-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaliniene G., Ustinaviciene R., Skemiene L., Januskevicius V. Associations between neck musculoskeletal complaints and work related factors among public service computer workers in Kaunas. Int. J. Occup. Med. Environ. Health. 2013;26:670–681. doi: 10.2478/s13382-013-0141-z. [DOI] [PubMed] [Google Scholar]
- 19.Valipour Noroozi M., Hajibabaei M., Saki A., Memari Z. Prevalence of Musculoskeletal Disorders Among Office Workers. Jundishapur J. Health Sci. 2015;7:e27157. doi: 10.5812/jjhs.27157. [DOI] [Google Scholar]
- 20.Holzgreve F., Maltry L., Lampe J., Schmidt H., Bader A., Rey J., Groneberg D.A., van Mark A., Ohlendorf D. The office work and stretch training (OST) study: An individualized and standardized approach for reducing musculoskeletal disorders in office workers. J. Occup. Med. Toxicol. 2018;13:37. doi: 10.1186/s12995-018-0220-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerr F., Marcus M., Ensor C., Kleinbaum D., Cohen S., Edwards A., Gentry E., Ortiz D.J., Monteilh C. A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Am. J. Ind. Med. 2002;41:221–235. doi: 10.1002/ajim.10066. [DOI] [PubMed] [Google Scholar]
- 22.Gobbo S., Bullo V., Bergamo M., Duregon F., Vendramin B., Battista F., Roma E., Bocalini D.S., Rica R.L., Alberton C.L., et al. Physical Exercise Is Confirmed to Reduce Low Back Pain Symptoms in Office Workers: A Systematic Review of the Evidence to Improve Best Practices in the Workplace. J. Funct. Morphol. Kinesiol. 2019;4:43. doi: 10.3390/jfmk4030043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shariat A., Alizadeh R., Moradi V., Afsharnia E., Hakakzadeh A., Ansari N.N., Ingle L., Shaw B.S., Shaw I. The impact of modified exercise and relaxation therapy on chronic lower back pain in office workers: A randomized clinical trial. J. Exerc. Rehabil. 2019;15:703–708. doi: 10.12965/jer.1938490.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soares C.O., Pereira B.F., Pereira Gomes M.V., Marcondes L.P., de Campos Gomes F., de Melo-Neto J.S. Preventive factors against work-related musculoskeletal disorders: Narrative review. Rev. Bras. Med. Trab. 2019;17:415–430. doi: 10.5327/Z1679443520190360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vitta A., Canonici A., de Conti M.H.S., Simeão S.F.D.A.P. Prevalência e fatores associados à dor musculoesquelética em profissionais de atividades sedentárias. Fisioter. Em Mov. 2012;25:273–280. doi: 10.1590/S0103-51502012000200004. [DOI] [Google Scholar]
- 26.Lipscomb J.A., Trinkoff A.M., Geiger-Brown J., Brady B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand. J. Work. Environ. Health. 2002;28:394–401. doi: 10.5271/sjweh.691. [DOI] [PubMed] [Google Scholar]
- 27.European Agency for Safety & Health at Work. Kok J., Vroonhof P., Snijders J., Roullis G., Clarke M., Peereboom K., Dorst P., Isusi I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics. EU. Publications Office; Luxembourg, Luxembourg: 2020. [Google Scholar]
- 28.Rodriguez-Nogueira O., Leiros-Rodriguez R., Benitez-Andrades J.A., Alvarez-Alvarez M.J., Marques-Sanchez P., Pinto-Carral A. Musculoskeletal Pain and Teleworking in Times of the COVID-19: Analysis of the Impact on the Workers at Two Spanish Universities. Int. J. Environ. Res. Public Health. 2020;18:31. doi: 10.3390/ijerph18010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Direção-Geral da Saúde, COVID-19. [(accessed on 9 March 2021)];2021 Available online: https://www.sns24.gov.pt/tema/doencas-infecciosas/covid-19/#sec-0.
- 30.Raquel Gonçalves Caldeira Brant L., Helena Cardoso M. DESAFIOS DO TELETRABALHO NA PANDEMIA COVID-19: QUANDO O HOME VIRA OFFICE. Cad. De Adm. 2020;28:71–75. doi: 10.4025/cadadm.v28i0.53637. [DOI] [Google Scholar]
- 31.Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lesser I.A., Nienhuis C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health. 2020;17:3899. doi: 10.3390/ijerph17113899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shariat A., Ghannadi S., Anastasio A.T., Rostad M., Cleland J.A. Novel stretching and strength-building exercise recommendations for computer-based workers during the COVID-19 quarantine. Work. 2020;66:739–749. doi: 10.3233/WOR-203220. [DOI] [PubMed] [Google Scholar]
- 34.Figueiredo E., Ribeiro C., Pereira P., Passos C. Teletrabalho: Contributos e desafios para as organizações. Rev. Psicol. Organ. E Trab. 2021;2:1427–1438. doi: 10.5935/rpot/2021.2.21642. [DOI] [Google Scholar]
- 35.Oakman J., Kinsman N., Stuckey R., Graham M., Weale V. A rapid review of mental and physical health effects of working at home: How do we optimise health? BMC Public Health. 2020;20:1825. doi: 10.1186/s12889-020-09875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Venegas Tresierra C.E., Leyva Pozo A.C. La fatiga y la carga mental en los teletrabajadores: A propósito del distanciamiento social. Rev. Esp. De Salud Publica. 2020;94:126. [PMC free article] [PubMed] [Google Scholar]
- 37.Abdin S., Welch R.K., Byron-Daniel J., Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health. 2018;160:70–76. doi: 10.1016/j.puhe.2018.03.029. [DOI] [PubMed] [Google Scholar]
- 38.Louw S., Makwela S., Manas L., Meyer L., Terblanche D., Brink Y. Effectiveness of exercise in office workers with neck pain: A systematic review and meta-analysis. S. Afr. J. Physiother. 2017;73:392. doi: 10.4102/sajp.v73i1.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suni J.H., Rinne M., Tokola K., Mänttäri A., Vasankari T. Effectiveness of a standardised exercise programme for recurrent neck and low back pain: A multicentre, randomised, two-arm, parallel group trial across 34 fitness clubs in Finland. BMJ Open Sport Exerc. Med. 2017;3:e000233. doi: 10.1136/bmjsem-2017-000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roviello V., Gilhen-Baker M., Vicidomini C., Roviello G.N. Forest-bathing and physical activity as weapons against COVID-19: A review. Environ. Chem. Lett. 2021;20:131–140. doi: 10.1007/s10311-021-01321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization . Global Recommendations on Physical Activity for Health. World Health Organization; Geneva, Switzerland: 2010. [PubMed] [Google Scholar]
- 42.Nguyen T.M., Nguyen V.H., Kim J.H. Physical Exercise and Health-Related Quality of Life in Office Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2021;18:3791. doi: 10.3390/ijerph18073791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Debska M., Polechonski J., Mynarski A., Polechonski P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health. 2019;16:3673. doi: 10.3390/ijerph16193673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ryde G.C., Atkinson P., Stead M., Gorely T., Evans J.M. Physical activity in paid work time for deskbased employees: A qualitative study of employers’ and employees’ perspectives. BMC Public Health. 2020;20:460. doi: 10.1186/s12889-020-08580-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arruda Z.M.T.D. Atuação do Fisioterapeuta na Saúde e Qualidade de Vida de Trabalhadores Utilizadores de Terminais de Computador. Faculdade de Medicina da Universidade de Coimbra; Coimbra, Portugal: 2019. [Google Scholar]
- 46.Mesquita C.C., Ribeiro J.C., Moreira P. Portuguese version of the standardized Nordic musculoskeletal questionnaire: Cross cultural and reliability. J. Public Health. 2010;18:461–466. doi: 10.1007/s10389-010-0331-0. [DOI] [Google Scholar]
- 47.Mota J., Sardinha L. Livro de Resumos do 8° Congresso de Educação Física e Ciências do Desporto dos Países de Língua Portuguesa. Desporto, Educação e Saúde. 8° Congresso de Educação Física e Ciências do Desporto dos Países de Língua Portuguesa; Faculdade de Motricidade Humana—Universidade Técnica de Lisboa; Lisboa, Portugal: 2000. Questionário Internacional de Actividade Física. Estudo piloto da garantia e validade numa população portuguesa; p. 323. [Google Scholar]
- 48.Kuorinka I., Jonsson B., Kilbom A., Vinterberg H., Biering-Sorensen F., Andersson G., Jorgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 49.Campaniço H. Validade Simultânea do Questionário Internacional de Actividade. Física Através da Medição Objectiva da Actividade Física por Actigrafia Proporcional. Master’s Thesis. Universidade de Lisboa (Portugal), ProQuest Dissertations Publishing; Lisboa, Portugal: 2016. [Google Scholar]
- 50.Craig C.L., Marshall A.L., Sjostrom M., Bauman A.E., Booth M.L., Ainsworth B.E., Pratt M., Ekelund U., Yngve A., Sallis J.F., et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 51.IPAQ . Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire. IPAQ; Tokyo, Japan: 2005. [(accessed on 23 September 2021)]. Available online: https://sites.google.com/site/theipaq/ [Google Scholar]
- 52.Cheng H. A Simple, Easy-to-Use Spreadsheet for Automatic Scoring of the Three Factor Eating Questionnaire (TFEQ)—Note to Users. 2016. [(accessed on 23 September 2021)]. Available online: https://www.researchgate.net/profile/Hoi_Lun_helen_Cheng/publication/311067926_A_simple_easy-to-use_spreadsheet_for_automatic_scoring_of_the_Three_Factor_Eating_Questionnaire_TFEQ/data/583d10e608ae1ff459833d94/TFEQ-Scoring.xlsx.
- 53.Cohen J. A power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 54.IBM Corp . IBM SPSS Statistics for Windows. IBM Corp; Armonk, NY, USA: 2020. [(accessed on 23 March 2022)]. Version 27.0. Available online: https://www.ibm.com/support/pages/how-cite-ibm-spss-statistics-or-earlier-versions-spss. [Google Scholar]
- 55.Bu F., Bone J.K., Mitchell J.J., Steptoe A., Fancourt D. Longitudinal changes in physical activity during and after the first national lockdown due to the COVID-19 pandemic in England. Sci. Rep. 2021;11:17723. doi: 10.1038/s41598-021-97065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roggio F., Trovato B., Ravalli S., Di Rosa M., Maugeri G., Bianco A., Palma A., Musumeci G. One Year of COVID-19 Pandemic in Italy: Effect of Sedentary Behavior on Physical Activity Levels and Musculoskeletal Pain among University Students. Int. J. Environ. Res. Public Health. 2021;18:8680. doi: 10.3390/ijerph18168680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhoyroo R., Chivers P., Millar L., Bulsara C., Piggott B., Lambert M., Codde J. Life in a time of COVID: A mixed method study of the changes in lifestyle, mental and psychosocial health during and after lockdown in Western Australians. BMC Public Health. 2021;21:1947. doi: 10.1186/s12889-021-11971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jain R., Meena M.L., Rana K.B. Risk factors of musculoskeletal symptoms among mobile device users during work from home. Int. J. Occup. Saf. Ergon. 2021:1–7. doi: 10.1080/10803548.2021.1979318. [DOI] [PubMed] [Google Scholar]
- 59.Woo E.H.C., White P., Lai C.W.K. Musculoskeletal impact of the use of various types of electronic devices on university students in Hong Kong: An evaluation by means of self-reported questionnaire. Man. Ther. 2016;26:47–53. doi: 10.1016/j.math.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 60.Intolo P., Shalokhon B., Wongwech G., Wisiasut P., Nanthavanij S., Baxter D.G. Analysis of neck and shoulder postures, and muscle activities relative to perceived pain during laptop computer use at a low-height table, sofa and bed. Work. 2019;63:361–367. doi: 10.3233/WOR-192942. [DOI] [PubMed] [Google Scholar]
- 61.Berolo S., Wells R.P., Amick B.C. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: A preliminary study in a Canadian university population. Appl. Ergon. 2011;42:371–378. doi: 10.1016/j.apergo.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 62.Legan M., Zupan K. Prevalence of mobile device-related musculoskeletal pain among working university students: A cross-sectional study. Int. J. Occup. Saf. Ergon. 2022;28:734–742. doi: 10.1080/10803548.2020.1827561. [DOI] [PubMed] [Google Scholar]
- 63.Scarabottolo C.C., Pinto R.Z., Oliveira C.B., Zanuto E.F., Cardoso J.R., Christofaro D.G.D. Back and neck pain prevalence and their association with physical inactivity domains in adolescents. Eur. Spine J. 2017;26:2274–2280. doi: 10.1007/s00586-017-5144-1. [DOI] [PubMed] [Google Scholar]
- 64.Madeleine P., Vangsgaard S., Hviid Andersen J., Ge H.Y., Arendt-Nielsen L. Computer work and self-reported variables on anthropometrics, computer usage, work ability, productivity, pain, and physical activity. BMC Musculoskelet. Disord. 2013;14:226. doi: 10.1186/1471-2474-14-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jain R., Verma V., Rana K.B., Meena M.L. Effect of physical activity intervention on the musculoskeletal health of university student computer users during homestay. Int. J. Occup. Saf. Ergon. 2021:1–6. doi: 10.1080/10803548.2021.1979318. [DOI] [PubMed] [Google Scholar]
- 66.Argus M., Pääsuke M. Effects of the COVID-19 lockdown on musculoskeletal pain, physical activity, and work environment in Estonian office workers transitioning to working from home. Work. 2021;69:741–749. doi: 10.3233/WOR-210033. [DOI] [PubMed] [Google Scholar]
- 67.Moreira-Silva I., Teixeira P.M., Santos R., Abreu S., Moreira C., Mota J. The Effects of Workplace Physical Activity Programs on Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Workplace Health Saf. 2016;64:210–222. doi: 10.1177/2165079916629688. [DOI] [PubMed] [Google Scholar]
- 68.Moreira S., Criado M.B., Ferreira M.S., Machado J., Gonçalves C., Clemente F.M., Mesquita C., Lopes S., Santos P.C. Positive Effects of an Online Workplace Exercise Intervention during the COVID-19 Pandemic on Quality of Life Perception in Computer Workers: A Quasi-Experimental Study Design. Int. J. Environ. Res. Public Health. 2022;19:3142. doi: 10.3390/ijerph19053142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moreira S., Ferreira M.S., Criado M.B., Machado J., Mesquita C., Lopes S., Santos P.C. Occupational Health: Does Compliance with Physical Activity Recommendations Have a Preventive Effect on Musculoskeletal Symptoms in Computer Workers? A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:7604. doi: 10.3390/ijerph18147604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Serra M., Camargo P.R., Zaia J.E., Tonello M.G.M., Quemelo P.R.V. Effects of physical exercise on musculoskeletal disorders, stress and quality of life in workers. Int. J. Occup. Saf. Ergon. 2018;24:62–67. doi: 10.1080/10803548.2016.1234132. [DOI] [PubMed] [Google Scholar]
- 71.Seghetto A., Piccoli J.C.J. Nível de atividade física, prevalência de desconforto e dor muscular e capacidade de trabalho: Uma avaliação no setor de call center de um banco do Rio Grande do Sul, Brasil. Rev. Bras. De Ciência E Mov. 2012;20:105–117. [Google Scholar]
- 72.Stamatakis E., Gale J., Bauman A., Ekelund U., Hamer M., Ding D. Sitting Time, Physical Activity, and Risk of Mortality in Adults. J. Am. Coll. Cardiol. 2019;73:2062–2072. doi: 10.1016/j.jacc.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 73.McDowell C.P., Herring M.P., Lansing J., Brower C., Meyer J.D. Working From Home and Job Loss Due to the COVID-19 Pandemic Are Associated With Greater Time in Sedentary Behaviors. Frontiers in Public Health. 2020;8:750. doi: 10.3389/fpubh.2020.597619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Braccialli L.M.P., Vilarta R. Aspectos a serem considerados na elaboração de programas de prevenção e orientação de problemas posturais. Rev. Paul. Educ. Fís. 2000;14:159–171. [Google Scholar]
- 75.Buckle P.W., Jason Devereux J. The nature of work-related neck and upper limb musculoskeletal disorders. Appl. Ergon. 2002;33:207–217. doi: 10.1016/S0003-6870(02)00014-5. [DOI] [PubMed] [Google Scholar]
- 76.Augusto V.G., Sampaio R.F., Tirado M.G.A., Mancini M.C., Parreira V.F. A look into Repetitive Strain Injury/Work-Related Musculoskeletal Disorders within physical therapists’ clinical context. Braz. J. Phys. Ther. 2008;12:49–56. [Google Scholar]
- 77.Callaghan P. Exercise: A neglected intervention in mental health care? J. Psychiatr. Ment. Health Nurs. 2004;11:476–483. doi: 10.1111/j.1365-2850.2004.00751.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available as the confidentiality agreement reached with the company does not allow public disclosure of the data available.