Abstract
Background: Since the beginning of the COVID-19 pandemic, empiric antibiotics (ATBs) have been prescribed on a large scale in both in- and outpatients. We aimed to assess the impact of antibiotic treatment on the outcomes of hospitalised patients with moderate and severe coronavirus disease 2019 (COVID-19). Methods: We conducted a prospective multicentre cohort study in six clinical hospitals, between January 2021 and May 2021. Results: We included 553 hospitalised COVID-19 patients, of whom 58% (311/553) were prescribed antibiotics, while bacteriological tests were performed in 57% (178/311) of them. Death was the outcome in 48 patients—39 from the ATBs group and 9 from the non-ATBs group. The patients who received antibiotics during hospitalisation had a higher mortality (RR = 3.37, CI 95%: 1.7–6.8), and this association was stronger in the subgroup of patients without reasons for antimicrobial treatment (RR = 6.1, CI 95%: 1.9–19.1), while in the subgroup with reasons for antimicrobial therapy the association was not statistically significant (OR = 2.33, CI 95%: 0.76–7.17). After adjusting for the confounders, receiving antibiotics remained associated with a higher mortality only in the subgroup of patients without criteria for antibiotic prescription (OR = 10.3, CI 95%: 2–52). Conclusions: In our study, antibiotic treatment did not decrease the risk of death in the patients with mild and severe COVID-19, but was associated with a higher risk of death in the subgroup of patients without reasons for it.
Keywords: antibiotics, antibacterial agents, COVID-19, SARS-CoV-2, mortality, hospital mortality, cohort studies, prospective studies
1. Introduction
Since the beginning of the COVID-19 pandemic, empiric antibiotics (ATBs) have been prescribed on a large scale in both hospitalised patients and outpatients. In its early stages, almost three-quarters of coronavirus disease 2019 (COVID-19) patients received ATBs despite the low rates of confirmed bacterial infections—especially regarding pulmonary involvement [1,2]. Some guidelines reserved the use of antibiotics for strong clinical suspicion of bacterial infection [3]; others advocated for empiric administration in severe COVID-19 patients while assessing for de-escalation or reconsidering the indication daily [4,5].
However, since treatments used for COVID-19 can alter the classical inflammation markers, detecting a bacterial infection in the earlier phase of the pandemic was more difficult [6]. In addition, COVID-19 itself increases C-reactive protein (CRP) and procalcitonin values—markers for bacterial infection, whose values are associated with disease severity [7].
Moreover, colonisation is frequently confused with infection, and the isolation of a bacterium may automatically lead to antibiotic prescription in patients with severe disease [8].
Considering the increased risk of death in COVID-19 patients with bacterial infections, as well as the consequences of inappropriate antibiotic prescription, physicians faced the risk of overprescription.
The aim of our study was to assess the impact of antibiotic treatment on the outcomes of hospitalised patients with COVID-19, as well as document the types of bacteria isolated and antibiotics prescribed.
2. Materials and Methods
2.1. Study Design and Population
This was a prospective multicentre cohort study, conducted in 6 clinical hospitals in Romania. We included adult patients with confirmed COVID-19 admitted to the hospital between January 2021 and May 2021. Study participants were enrolled from departments of infectious diseases, internal medicine, and pneumology.
The inclusion criteria for the study were (a) patients 18 years of age or older, and (b) confirmed COVID-19 diagnosed by a positive real-time polymerase chain reaction (RT-PCR) test or SARS-CoV-2 rapid antigen test.
The exclusion criteria were (a) patients initially admitted to the ICU, (b) end-stage kidney disease undergoing haemodialysis or peritoneal dialysis, and (c) lympho- and myeloproliferative disorders.
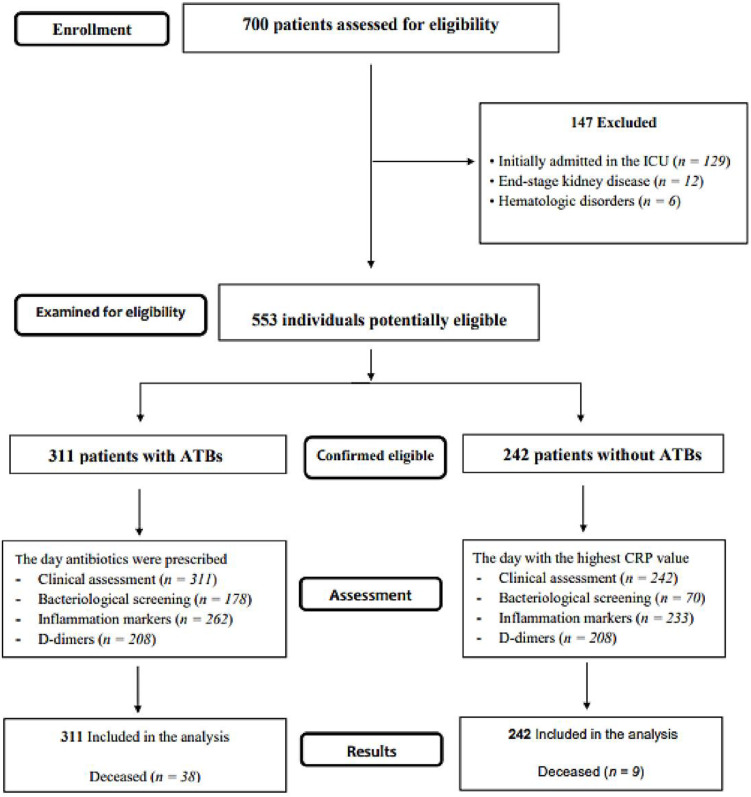
The treatment decision remained at the discretion of the attending physician. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines [9]. The flow diagram of the study is presented in Figure 1.
Figure 1.
The flow diagram of the study describing the methods: participants’ recruitment, inclusion, exclusion, and outcomes.
2.2. Ethical Consideration
This study was conducted in accordance with the principles of the Declaration of Helsinki, and accepted by the ethics committee of the medical centres involved (32/8 December 2020). Patients signed written informed consent during hospital admission and, due to biosecurity reasons, the consent was also collected verbally and registered in the medical chart by the treating physician.
2.3. Variables and Data Measurement
The uniformity of the cohort was ensured using the following criteria for classifying the form of the disease and the degree of lung involvement.
Disease severity was defined as mild (normal O2 saturation and normal chest X-ray), medium (radiological evidence of COVID-19 pneumonia), or severe, based on at least one of the following criteria: peripheral oxygen saturation (SpO2) ≤ 93% in ambient air, respiratory rate (RR) > 30/minute, arterial oxygenation partial pressure to fractional inspired oxygen ratio (PaO2/FiO2 ratio) < 300, or lung infiltrates > 50% of lung parenchyma).
Evidence for pulmonary bacterial infection was suggestive symptoms (e.g., fever, productive cough) or alveolar consolidation on chest CT, with or without positive microbiology. Given the fact that corticosteroids cause false leucocytosis with neutrophilia, and that COVID-19 induces a systemic inflammatory response, we considered that these biological markers had a lower contribution when assessing for bacterial infection. Isolated fever, in the absence of other clinical symptoms, with a procalcitonin value within normal range, was not considered sufficient reason to initiate antibiotic treatment.
Confirmed bacterial respiratory infection was diagnosed based on positive cultures of respiratory pathogens isolated from good-quality sputum (>25 polymorphonuclear leukocytes and <10 epithelial cells). Urinary tract infections (UTIs) were diagnosed based on symptoms and a positive urine culture (≥103 UFC/mL). Bloodstream-invasive infections were defined as the growth of non-skin flora commensal on one or more blood cultures. For skin colonisers, we considered at least two positive blood cultures from different sets as microbiologically significant, unless the patient had high clinical suspicion and a predisposing condition (e.g., central venous catheter).
During their stay in the hospital, complete blood counts, inflammation markers, and d-dimer values were documented daily. We used the admission values, those prior to antibiotic administration (for patients who received antibiotics), and from the day with the highest CRP value (for patients who did not receive antibiotics).
The antimicrobial therapy was considered as appropriate for those who had reasons for pulmonary, urinary, or bloodstream infection, as previously described. Patients who received oral vancomycin for Clostridioides difficile colitis were included in the non-antibiotic group, even though they received empiric antibiotics before admission.
2.4. Sample Size
From the previous COVID-19 wave, in our hospital we had found a mortality of 10%, and a rate of antibiotic prescription of about 50%. For an alpha-error of 5%, a power of 80%, and an estimated 50% reduction in mortality in the antimicrobial therapy group, we calculated a sample size of 870 patients [10].
2.5. Data Analysis
Demographic, clinical, laboratory, biological, and imaging data of the enrolled patients were descriptively analysed. Continuous and categorical variables were presented as medians (min, max) and absolute numbers (percentage), respectively. A p-value of <0.05 was considered statistically significant. In the multivariable model, we introduced the variables associated with death with a p-value ≤ 0.10, and the regression was ruled stepwise forward because we had a relatively small number of patients who suffered that outcome. We analysed the collected data using the Statistical Package for Social Sciences (SPSS version 20, IBM Corp., Armonk, NY, USA) and Microsoft Excel 2018 (Microsoft Corporation, Redmond, WA, USA). The relative risk was calculated with EBM calculator (https://ebm-tools.knowledgetranslation.net/calculator, accessed on 3 March 2022) [11].
3. Results
A total of 700 patients was admitted into the six centres during the study period (January–May 2021). After eligibility assessment, 553 hospitalised COVID-19 patients were included in the study (Figure 1). The cohort had a median age of 67 (18–94) years, and 51% (283/553) of the enrolled patients were males. In terms of severity, 8% (44/553) of the patients had mild, 54% (297/553) moderate, and 38% (212/553) severe COVID-19. Three percent (14/553) of the patients were diagnosed with pulmonary thromboembolism (PE).
Treatment for COVID-19 included corticotherapy in 78% (431/553), anti-IL-6 tocilizumab in 6% (34/553), anti-IL-1-anakinra in 16% (89/553), and antivirals, including remdesivir in 22.4% (124/553), favipiravir in 15.6% (86/553) and umifenovir in 0.5% (3/553).
3.1. Bacteriological Results
Bacteriological tests requested by the attending physicians were performed in 57% (178/311) of the patients prior to ATB administration. After the microbiological screening, a total of 95 patients was diagnosed with bacterial infections. Positive results with clinical significance consisted of sputum examination (38 positive), urine cultures (31 positive), and blood cultures (39 positive). Based on the clinical and laboratory features, the organisms isolated were considered true infections, as opposed to colonisations. Ten percent (17/178) of them also had a fungal infection. Seven percent (12/178) of the screened patients had more than one positive bacteriological sample: sputum and urine culture (6/12), sputum and blood culture (2/12), urine and blood culture (3/12), or all three samples positive (1/12). In addition, 14 sputum and 2 urine cultures identified co-infections.
The detailed epidemiology of microbiological documented associated infections is presented in Table 1.
Table 1.
Epidemiology of microbiological documented associated infections.
| Aetiological Agents | Microbiological Sample * | Cases **, N | ||
|---|---|---|---|---|
| Sputum | Urine | Blood | ||
| Gram-positive bacteria | 33 | |||
| S. aureus | 11 | |||
| Coagulase-negative staphylococci | 8 | |||
| Streptococcus spp. | 5 | |||
| Streptococcus pneumoniae | 5 | |||
| Enterococcus spp. | 4 | |||
| Fungi | 17 | |||
| Candida spp. | 16 | |||
| Aspergillus spp. | 1 | |||
| Gram-negative bacteria | 75 | |||
| K. pneumoniae | 26 | |||
| E. coli | 25 | |||
| P. aeruginosa | 4 | |||
| H. influenzae | 4 | |||
| A. baumannii | 3 | |||
| S. maltophilia | 3 | |||
| Serratia spp. | 2 | |||
| Hafnia paralvei | 2 | |||
| Sphingomonas paucimobilis | 2 | |||
| K. oxytoca | 1 | |||
| Enterobacter cloacae | 1 | |||
| P. fluorescens | 1 | |||
| Proteus mirabilis | 1 | |||
* The microbiological samples are marked by colour (blue for positive sputum samples, green for positive urine samples and red for positive blood samples), ** Multiple positive samples were identified per patient, and multiple pathological agents were identified per sample.
3.2. Antibiotic Prescription
A total of 58% (311/553) of the patients received antibiotic treatment during hospitalisation.
The patients who received ATBs were older, had a higher Charlson comorbidity index, and had more severe COVID-19. The median time for antibiotics prescription was 7 (min 0, max 78) days from symptom onset and 0 (min 0, max 24) days from admission. In total, 62% (193/311) of the patients received just one antibiotic during hospitalisation. The median number of antibiotics administered per patient was one (min 1, max 7). The most common classes of antibiotics prescribed were β-lactams, followed by fluoroquinolones and oxazolidinone (linezolid). When used in combination, carbapenems and oxazolidinone (linezolid) or vancomycin was the preferred regimen.
Antibiotics were administered according to antibiogram in 25% (77/311) of the patients. Empiric and antibiogram-guided antibiotic classes prescribed during hospitalisation are presented in Table 2.
Table 2.
Antibiotic prescription.
| Antibiotic Classes | Patients *, N |
|---|---|
| B-lactam drugs | |
| Penicillins +/− BLI | 85 |
| Cephalosporins +/− BLI | 163 |
| Carbapenems | 79 |
| Fluoroquinolones | |
| Ciprofloxacin | 14 |
| Levofloxacin | 26 |
| Moxifloxacin | 11 |
| Oxazolidinones (linezolid) | 27 |
| Cyclines | |
| Doxycycline | 13 |
| Tigecycline | 10 |
| Glycopeptides | |
| Vancomycin | 17 |
| Teicoplanin | 2 |
| Aminoglycosides | |
| Gentamicin | 4 |
| Amikacin | 6 |
| Macrolides (clarithromycin) | 3 |
| Others | |
| TMP/SMX | 23 |
| Polymyxin E (colistin) | 11 |
| Metronidazole | 11 |
| Fosfomycin | 4 |
| Clindamycin | 2 |
| Chloramphenicol | 1 |
| Nitrofurantoin | 1 |
* More than one antibiotic was administered in 38% of the patients.
Death was the outcome in 48 patients—39 from the ATBs group and 9 from the non-ATBs group. No difference was observed between the two groups in terms of median length of hospitalisation—13 days (min, max: 2–50) in the patients who survived vs. 12 days (min, max: 3–48) in the patients who died (p = 0.8).
3.3. Factors Associated with Patients’ Outcomes
The distribution of the variables in the deceased and surviving patients is presented in Table 3, as well as in the Supplementary Materials (Table S1).
Table 3.
The distribution of the variables in the survivors vs. non-survivors groups.
| Variable | Survivors, N = 505 |
Non-Survivors, N = 48 |
AUROC (CI 95%) * or RR (CI 95%) ** |
p-Value | Missing |
|---|---|---|---|---|---|
| Antibiotics during hospitalisation, N (%) | 272 (53.9) | 39 (81.2) | 3.37 (1.7–6.8) | <0.001 | |
| Prescription reason: yes, N (%) | 223 (82) | 30 (77) | 2 (0.8–4.9) | 0.124 | |
| Prescription reason: no, N (%) | 49 (18) | 9 (23) | 6.1 (1.9–19.1) | 0.001 | |
| Gender, female, N (%) | 250 (49.5) | 20 (41.7) | 1.3 (0.8–2.3) | 0.375 | |
| Age, median (min, max) | 67 (18–94) | 74 (50–91) | 0.642 (0.567–0.716) | 0.001 | |
| Charlson comorbidity index, median (min, max) |
4 (0–12) | 4.5 (1–11) | 0.645 (0.567–0.724) | 0.001 | |
| COVID-19 severity (ordinal variable) | <0.001 | ||||
| Mild | 41 (8.1) | 3 (6.2) | |||
| Moderate | 290 (57.4) | 7 (14.6) | |||
| Severe | 174 (34.5) | 38 (79.2) | |||
| Pulmonary involvement $, % (min, max) |
40 (0–95) | 70 (0–95) | 0.662 (0.526–0.797) | 0.007 | |
| Pulmonary embolism, N (%) | 13 (2.6) | 1 (2.1) | 0.8 (0.1–5.5) | 1 | |
| SpO2_admission, median (min, max) |
93 (60–99) | 89.5 (58–99) | 0.610 (0.518–0.701) | 0.012 | 4 |
| SpO2_at ATB prescription, median (min, max) | 93 (53, 99) | 86.5 (56, 99) | 0.660 (0.555–0.764) | 0.001 | 66 |
| Positive microbiology, N (%) | 81 (29.8) | 14 (35.9) | 0.460 | ||
| Appropriate ATB, N (%) | 74 (27.2) | 3 (7.7) | 0.23 (0.08–0.7) | 0.009 | |
| Corticotherapy, N (%) | 395 (78.2) | 36 (75) | 0.85 (0.46–1.6) | 0.588 | |
| Tocilizumab, N (%) | 28 (5.5) | 6 (12.5) | 2.2 (0.99–4.76) | 0.105 | |
| Anakinra, N (%) | 73 (14.5) | 16 (33.3) | 2.6 (1.5–4.5) | 0.001 | |
| Antiviral | 11 (22.9) | 179 (35.4) | 0.111 | ||
| CRP at admission, median (min, max) |
55.7 (0.2–397.6) | 80.2 (1.95–390.6) | 0.583 (0.492–0.673) | 0.060 | 9 |
| CRP at ATB prescription, median (min, max) | 60.4 (0.2–385.3) | 86.5 (7.7–390.6) | 0.616 (0.536–0.697) | 0.011 | 58 |
| IL-6 at admission, median (min, max) |
30.2 (1–1406) | 58.2 (7–656) | 0.640 (0.536–0.743) | 0.016 | 242 |
| Leukocytes at admission, median (min, max) | 7200 (1060–40,930) | 8265 (2570–23,510) | 0.591 (0.502–0.681) | 0.037 | 9 |
| Leukocytes at ATB prescription, median (min, max) | 7670 (1060–29,760) | 10180 (2570–28,570) | 0.618 (0.527–0.710) | 0.009 | 62 |
| Neutrophils at admission, median (min, max) | 5440 (650–36,790) | 7135 (1120–20,410) | 0.624 (0.539–0.709) | 0.005 | 10 |
| Neutrophils at ATB prescription, median (min, max) | 6000 (650–24,690) | 7810 (1800–26,400) | 0.652 (0.567–0.738) | 0.001 | 62 |
| Lymphocytes at admission, median (min, max) | 1000 (160–6470) | 880 (150–5930) | 0.606 (0.523–0.690) | 0.015 | 10 |
| Lymphocytes at ATB prescription, median (min, max) | 1050 (160–4100) | 850 (150–5930) | 0.629 (0.541–0.717) | 0.005 | 63 |
| NLR at admission, median (min, max) | 5.26 (0.29–60.8) | 8.66 (0.69–84) | 0.678 (0.604–0.753) | <0.001 | 11 |
| NLR at ATB prescription, median (min, max) | 5.42 (0.45–56) | 9.13 (1.18–86.33) | 0.698 (0.620–0.776) | <0.001 | 63 |
| D-dimers at admission, median (min, max) | 0.8 (0.1–15.4) | 1.15 (0.1–7.2) | 0.574 (0.481–0.667) | 0.109 | 78 |
| D-dimers highest value, median (min, max) | 1.1 (0.1–20) | 4.4 (0.5–20) | 0.813 (0.744–0.882) | <0.001 | 74 |
| D-dimers at ATB prescription, median (min, max) | 0.7 (0.1–20) | 1.9 (0.2–20) | 0.677 (0.580–0.774) | <0.001 | 137 |
| Urea at admission, median (min, max) | 41 (11–189) | 60.3 (7–129) | 0.669 (0.591–0.748) | <0.001 | 17 |
AUROC—area under the receiver operating characteristic curve, CI—confidence interval, RR—relative risk, ATB—antibiotic, SpO2—oxygen saturation levels, CRP—C-reactive protein, IL-6—interleukin-6, NLR—neutrophil-to-lymphocyte ratio. $ Assessed in only one centre. Statistically significant values are marked in bold. We calculated * AUROC for quantitative variables and ** RR for qualitative dichotomous variables.
In our study, the variables associated with death were older age, higher Charlson comorbidity index, COVID-19 severity, lower O2 saturation, higher inflammation markers (e.g., CRP, ferritin), and leucocyte and NLR values, as well as lower lymphocyte count.
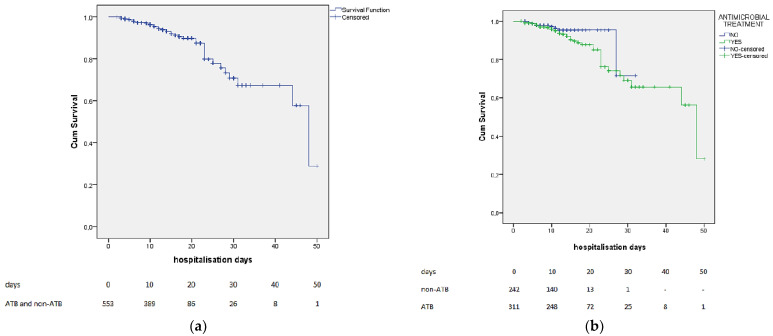
The Kaplan–Meier curves for the whole group and subgroups (ATB and non-ATB) are presented in Figure 2.
Figure 2.
The Kaplan–Meier curves for the whole group (a) and subgroups (ATB and non-ATB) (b).
Overall, the patients who received antibiotics during hospitalisation had a threefold higher mortality rate (12.5% vs. 3.7%, RR = 3.37, p < 0.001). In a subgroup analysis, among the patients without reasons for prescription, those who received antibiotics had a sixfold greater risk of death, while among those with reasons, there was no difference regarding the outcome—both in bivariate analysis (Table 3 and Table S1), and after adjusting for the other prognostic variables (Table 4).
Table 4.
The association of antibiotic treatments with death after adjustment for the prognostic factors (logistic regression).
| Variable | Coefficient | p -Value | Odds Ratio (95% CI) |
| Age (years) | 0.044 | 0.049 | 1.05 (1.0–1.09) |
| Form of disease * | 0.034 | ||
| Moderate COVID-19 | −0.864 | 0.482 | 0.4 (0.08–2.1) |
| Severe COVID-19 | 0.663 | 0.585 | 1.9 (0.18–20.9) |
| D-dimers (highest value) | 0.250 | <0.001 | 1.3 (1.15–1.43) |
| Antibiotics (yes/no) | 0.846 | 0.140 | 2.33 (0.76–7.17) |
CI—confidence interval. Statistically significant values are marked in bold. * Compared with mild COVID-19.
In the subgroup of patients with reasons for antibiotic prescription, only D-dimers (highest value) and SpO2 at admission were independent predictors of death (Table 5), while antibacterial therapy remained statistically associated with death even after adjustment among the patients without reasons for antibiotic treatment (Table 6).
Table 5.
The association of antibiotic treatment with death in the patients with reasons for prescription, after the adjustment for the prognostic factors (logistic regression).
| Variable | Coefficient | p | Odds Ratio (95% CI) |
|---|---|---|---|
| D-dimers (highest value) | 0.340 | <0.001 | 1.41 (1.21–1.63) |
| SpO2 (admission) | −0.086 | 0.014 | 0.92 (0.86–0.98) |
| Antibiotics (yes/no) | 0.112 | 0.145 | 3.04 (0.68–13.55) |
SpO2—oxygen saturation levels, CI—confidence interval. Statistically significant values are marked in bold.
Table 6.
The association of antibiotic treatment with death in the patients without reasons for prescription, after the adjustment for the prognostic factors (logistic regression).
| Variable | Coefficient | p | Odds Ratio (95% CI) |
|---|---|---|---|
| Form of disease * | 0.038 | ||
| Moderate COVID-19 | −0.583 | 0.728 | 0.56 (0.02–14.9) |
| Severe COVID-19 | 1.586 | 0.326 | 4.9 (0.2–115.3) |
| D-dimers (highest value) | 0.211 | 0.009 | 1.2 (1.05–1.44) |
| NLR (admission) | 0.140 | 0.017 | 1.15 (1.02–1.3) |
| Antibiotics (yes/no) | 2.33 | 0.005 | 10.3 (2.0–52) |
CI—confidence interval, NLR—neutrophil-to-lymphocyte ratio. * Compared with mild COVID-19. Statistically significant values are marked in bold.
The patients who died had a higher median duration from onset of COVID-19 symptoms to administration of antibiotics (11 vs. 8, p = 0.023), and received a median of two antibiotics during hospitalisation (min, max: 1–5).
With an AUROC value of 0.813 (0.744, 0.882), the highest D-dimer values documented during hospitalisation represented the best predictors of death. Moreover, the median value for D-dimers in the deceased group was four times higher compared with the patients who survived. Since there were no significant differences concerning the other laboratory variables between the values at admission and those during hospitalisation, the values at admission could be used.
A total of 48/91 tests for C. difficile came back positive; most of them were related to antibiotic prescription either during hospitalisation (39/48) or prior to admission (3/48).
4. Discussion
In our study, antibiotic administration did not decrease the mortality rate of patients with moderate and severe COVID-19, but it was associated with higher mortality in the subgroup of patients without documented bacterial infection. Previous studies have described the rates of antibiotic administration during the first and subsequent waves and the appropriateness of their prescription [12], but only a few of them assessed their impact on a hard outcome (death). As expected, in our study, the patients who died were older, had more comorbidities, and had more severe forms of COVID-19.
During the first waves of the pandemic, there was a high rate of antibiotic prescription—almost 70–80% of the hospitalised patients received antibiotics [13,14]. Azithromycin, ceftriaxone, and broad-spectrum antibiotics used to treat community-acquired pneumonia were the most commonly prescribed antibiotic regimens during the pandemic, probably due to the concern of bacterial co-infection [15,16]. Initially, azithromycin was also prescribed due to its supposed immunomodulatory and antiviral action, but later studies have shown no additional effect on survival or clinical outcomes compared to the standard of care [17,18,19]. In addition, regarding its antimicrobial effects, in Romania, as rates of macrolide resistance of S. pneumoniae are high, azithromycin is of little value in treating potential community bacterial co- or superinfections. During the pandemic, it was believed that prescribing antibiotics at large scale—especially in moderate and severe COVID-19 patients—might in fact have diminished the rate of bacterial infections [20], and probably helped save thousands of lives [21].
However, no more than 14.3% of hospitalised COVID-19 patients had a bacterial infection [22,23]. Seven percent (38/553) of our patients had an identified respiratory pathogen by positive sputum culture. As shown in previous studies, the rate of non-respiratory bacterial infections was even lower—only 0.8% of the patients had venous-catheter-related bacteraemia or urinary tract infections, and even fewer had intra-abdominal (0.3%) or skin and soft tissue (0.1%) infections [12]. In our study, the rate of non-respiratory bacterial infections was 11% (61/553), but since the patients enrolled had a relatively long stay in the hospital, some of these were hospital-acquired. In order to prevent overprescription, Giannella et al. proposed a predictive model using leucocytes, procalcitonin, and the Charlson index to quantify the risk of bacterial co-infection in hospitalised COVID-19 patients [24].
As expected, in our study, the patients who received antibiotics were those with more severe COVID-19; therefore, there was a selection bias that could have obscured any potential benefits of antibiotic therapy. Although we measured and adjusted for the variables proven until now to be correlated with death [25,26], it is possible that other unassessed variables might have been involved [27]. A severe evolution of the viral infection, unrelated to the bacterial superinfection, could also explain these results.
Pre-COVID-19 research showed that even when prescribed appropriately, antibiotics could not reverse the risk of death in the presence of other patient-related factors such as older age, neoplastic disease, non-ambulatory state, orientation disturbance, hypoalbuminaemia, tachycardia, tachypnoea, and hypoxemia—factors also frequently encountered in severe and moderate COVID-19 disease [28].
Due to the extensive bacterial screening, we consider the involvement of coexisting unidentified infectious agents or bacterial resistance less probable, and this was one of the reasons that we did not include patients previously admitted to the ICU. As expected, studies have shown that when adding hospitals to the community-acquired infections, the bacteraemia rate rises to 3.2–5.6% [29,30].
The main limitation of this study is its observational design. We adjusted for the factors known to be related to survival in order to address this issue.
When this project started, it was the first multicentre prospective study that aimed to evaluate the impact of antibiotic prescription on a hard outcome (death/survival). To date, three studies with a similar aim have been published, but two of them were retrospective and monocentric [31,32], and the third, although it had a large sample size, took into account only gender, age, and comorbidities as confounders [33]. However, their results are consistent with ours.
Overall, we showed that antibiotics, when prescribed in the absence of clear reasons suggestive of bacterial infection, were associated with higher mortality among patients with mild and severe COVID-19. In addition, our results could apply in the post-COVID-19 era as well, to patients with viral infections and/or immunosuppressive treatment, in whom unnecessary antibiotics might not positively influence the outcome.
Acknowledgments
We value the important contributions of Iustina Ostafie, Alexandra-Diana Diaconu, Giorgiana Voloc, Georgeta Daniela Ionescu, Maria-Ilinca Iosub, and Ruxandra Ilina, who contributed to patients’ inclusion and data gathering.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm12060877/s1, Table S1: The distribution of the variables in the survivors vs. non-survivors groups.
Author Contributions
Conceptualisation, L.P. and C.B. (Cristian Baicus); Data Curation, L.P., A.C., C.-M.N., L.E.S., R.A.I., R.C.C., N.V., C.B. (Camelia Badea), and L.S.; Formal Analysis, L.P., A.H. and C.B. (Cristian Baicus); Investigation, L.P., A.C., C.-M.N., L.E.S., R.A.I., R.C.C., N.V., V.P., A.P., C.B. (Camelia Badea), A.H. and L.S.; Methodology, L.P. and C.B. (Cristian Baicus); Project Administration, L.P. and C.B. (Cristian Baicus); Resources, L.P., A.C., C.-M.N., L.E.S., R.A.I., M.I.B., N.V., V.P., A.P., C.B. (Camelia Badea), A.H. and L.S.; Software, L.P.; Supervision, M.I.B. and C.B. (Cristian Baicus); Visualisation, L.P.; Writing—Original Draft L.P. and C.-M.N.; Writing—Review and Editing, A.C., L.E.S., R.C.C., V.P., A.P., A.H. and C.B. (Cristian Baicus). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics committee of Colentina Clinical Hospital (32/8 December 2020) and the involved medical centres.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Patients signed written informed consent during hospital admission and, due to biosecurity reasons, the consent was also collected verbally and registered in the medical chart by the treating physician.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Karami Z., Knoop B.T., Dofferhoff A.S.M., Blaauw M.J.T., Janssen N.A., van Apeldoorn M., Kerckhoffs A.P.M., van de Maat J.S., Hoogerwerf J.J., Oever J.T. Few bacterial co-infections but frequent empiric antibiotic use in the early phase of hospitalized patients with COVID-19: Results from a multicentre retrospective cohort study in The Netherlands. Infect. Dis. 2021;53:102–110. doi: 10.1080/23744235.2020.1839672. [DOI] [PubMed] [Google Scholar]
- 2.Langford B.J., So M., Raybardhan S., Leung V., Soucy J.-P.R., Westwood D., Daneman N., MacFadden D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19 Rapid Guideline: Antibiotics for Pneumonia in Adults in Hospital|Guidance|NICE. [(accessed on 1 June 2021)]. Available online: https://www.nice.org.uk/guidance/ng173.
- 4.Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E., Oczkowski S., Levy M.M., Derde L., Dzierba A., et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19) Crit. Care Med. 2020;48:e440–e469. doi: 10.1097/CCM.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization COVID-19 Clinical Management: Living Guidance. [(accessed on 1 June 2021)]. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2.
- 6.Rouzé A., Labreuche J., Nseir S. Reply to Kasugai et al.: The Mystery of Futility of Appropriate Antibiotics for Coinfection in COVID-19. Am. J. Respir. Crit. Care Med. 2021;204:1489–1491. doi: 10.1164/rccm.202108-1846LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tong-Minh K., van der Does Y., Engelen S., de Jong E., Ramakers C., Gommers D., van Gorp E., Endeman H. High procalcitonin levels associated with increased intensive care unit admission and mortality in patients with a COVID-19 infection in the emergency department. BMC Infect. Dis. 2022;22:165. doi: 10.1186/s12879-022-07144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Laethem J., Wuyts S.C.M., Pierreux J., Seyler L., Verschelden G., Depondt T., Meuwissen A., Lacor P., Piérard D., Allard S.D. Presumed Urinary Tract Infection in Patients Admitted with COVID-19: Are We Treating Too Much? Antibiotics. 2021;10:1493. doi: 10.3390/antibiotics10121493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katz M.H. Multivariable Analysis. Cambridge University Press (CUP); Cambridge, UK: 2011. Outcome variables in multivariable analysis; pp. 25–73. [Google Scholar]
- 11.Evidence-Based Medicine Toolbox|EBM Calculators. [(accessed on 3 March 2022)]. Available online: https://ebm-tools.knowledgetranslation.net/calculator.
- 12.Calderón-Parra J., Muiño-Miguez A., Bendala-Estrada A.D., Ramos-Martínez A., Muñez-Rubio E., Carracedo E.F., Montes J.T., Rubio-Rivas M., Arnalich-Fernandez F., Pérez J.L.B., et al. Inappropriate antibiotic use in the COVID-19 era: Factors associated with inappropriate prescribing and secondary complications. Analysis of the registry SEMI-COVID. PLoS ONE. 2021;16:e0251340. doi: 10.1371/journal.pone.0251340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giacomelli A., Ridolfo A.L., Milazzo L., Oreni L., Bernacchia D., Siano M., Bonazzetti C., Covizzi A., Schiuma M., Passerini M., et al. 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: A prospective cohort study. Pharmacol. Res. 2020;158:104931. doi: 10.1016/j.phrs.2020.104931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia-Vidal C., Sanjuan G., Moreno-García E., Puerta-Alcalde P., Garcia-Pouton N., Chumbita M., Fernandez-Pittol M., Pitart C., Inciarte A., Bodro M., et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: A retrospective cohort study. Clin. Microbiol. Infect. 2021;27:83–88. doi: 10.1016/j.cmi.2020.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giacomelli A., Ridolfo A.L., Oreni L., Vimercati S., Albrecht M., Cattaneo D., Rimoldi S.G., Rizzardini G., Galli M., Antinori S. Consumption of antibiotics at an Italian university hospital during the early months of the COVID-19 pandemic: Were all antibiotic prescriptions appropriate? Pharmacol. Res. 2021;164:105403. doi: 10.1016/j.phrs.2020.105403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nestler M.J., Godbout E., Lee K., Kim J., Noda A.J., Taylor P., Pryor R., Markley J.D., Doll M., Bearman G., et al. Impact of COVID-19 on pneumonia-focused antibiotic use at an academic medical center. Infect. Control Hosp. Epidemiol. 2020;42:915–916. doi: 10.1017/ice.2020.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verdejo C., Vergara-Merino L., Meza N., Pérez-Bracchiglione J., Carvajal-Juliá N., Madrid E., Rada G., Reyes M.X.R. Macrolides for the treatment of COVID-19: A living, systematic review. Medwave. 2020;20:e8073. doi: 10.5867/medwave.2020.11.8073. [DOI] [PubMed] [Google Scholar]
- 18.Abaleke E., Abbas M., Abbasi S., Abbott A., Abdelaziz A., Abdelbadiee S., Abdelfattah M., Abdul B., Rasheed A.A., Abdul-Kadir R., et al. Azithromycin in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet. 2021;397:605–612. doi: 10.1016/S0140-6736(21)00149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Furtado R.H.M., Berwanger O., Fonseca H.A., Corrêa T.D., Ferraz L.R., Lapa M.G., Zampieri F.G., Veiga V.C., Azevedo L.C.P., Rosa R.G., et al. Azithromycin in addition to standard of care versus standard of care alone in the treatment of patients admitted to the hospital with severe COVID-19 in Brazil (COALITION II): A randomised clinical trial. Lancet. 2020;396:959–967. doi: 10.1016/S0140-6736(20)31862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang C.-Y., Chan K.G. Underestimation of co-infections in COVID-19 due to non-discriminatory use of antibiotics. J. Infect. 2020;81:e29–e30. doi: 10.1016/j.jinf.2020.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ginsburg A.S., Klugman K.P. COVID-19 pneumonia and the appropriate use of antibiotics. Lancet Glob. Health. 2020;8:e1453–e1454. doi: 10.1016/S2214-109X(20)30444-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lansbury L., Lim B., Baskaran V., Lim W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020;81:266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., Soucy J.-P.R., Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giannella M., Rinaldi M., Tesini G., Gallo M., Cipriani V., Vatamanu O., Campoli C., Toschi A., Ferraro G., Horna C.S., et al. Predictive model for bacterial co-infection in patients hospitalized for COVID-19: A multicenter observational cohort study. Infection. 2022:1–11. doi: 10.1007/s15010-022-01801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knight S.R., Ho A., Pius R., Buchan I., Carson G., Drake T.M., Dunning J., Fairfield C.J., Gamble C., Green C.A., et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: Development and validation of the 4C Mortality Score. BMJ. 2020;370:m3339. doi: 10.1136/bmj.m3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lombardi Y., Azoyan L., Szychowiak P., Bellamine A., Lemaitre G., Bernaux M., Daniel C., Leblanc J., Riller Q., Steichen O., et al. External validation of prognostic scores for COVID-19: A multicenter cohort study of patients hospitalized in Greater Paris University Hospitals. Intensiv. Care Med. 2021;47:1426–1439. doi: 10.1007/s00134-021-06524-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta R.K., Marks M., Samuels T.H.A., Luintel A., Rampling T., Chowdhury H., Quartagno M., Nair A., Lipman M., Abubakar I., et al. Systematic evaluation and external validation of 22 prognostic models among hospitalised adults with COVID-19: An observational cohort study. Eur. Respir. J. 2020;56:2003498. doi: 10.1183/13993003.03498-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shindo Y., Ito R., Kobayashi D., Ando M., Ichikawa M., Goto Y., Fukui Y., Iwaki M., Okumura J., Yamaguchi I., et al. Risk factors for 30-day mortality in patients with pneumonia who receive appropriate initial antibiotics: An observational cohort study. Lancet Infect. Dis. 2015;15:1055–1065. doi: 10.1016/S1473-3099(15)00151-6. [DOI] [PubMed] [Google Scholar]
- 29.Hughes S., Troise O., Donaldson H., Mughal N., Moore L.S.P. Bacterial and fungal coinfection among hospitalized patients with COVID-19: A retrospective cohort study in a UK secondary-care setting. Clin. Microbiol. Infect. 2020;26:1395–1399. doi: 10.1016/j.cmi.2020.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goyal P., Choi J.J., Pinheiro L.C., Schenck E.J., Chen R., Jabri A., Satlin M.J., Campion T.R., Jr., Nahid M., Ringel J.B., et al. Clinical Characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moretto F., Sixt T., Devilliers H., Abdallahoui M., Eberl I., Rogier T., Buisson M., Chavanet P., Duong M., Esteve C., et al. Is there a need to widely prescribe antibiotics in patients hospitalized with COVID-19? Int. J. Infect. Dis. 2021;105:256–260. doi: 10.1016/j.ijid.2021.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosca A., Balcaen T., Lanoix J.-P., Michaud A., Moyet J., Marcq I., Schmit J.-L., Bloch F., Deschasse G. Mortality risk and antibiotic use for COVID-19 in hospitalized patients over 80. Biomed. Pharmacother. 2022;146:112481. doi: 10.1016/j.biopha.2021.112481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schons M.J., Caliebe A., Spinner C.D., Classen A.Y., Pilgram L., Ruethrich M.M., Rupp J., de Miranda S.N., Römmele C., Vehreschild J., et al. All-cause mortality and disease progression in SARS-CoV-2-infected patients with or without antibiotic therapy: An analysis of the LEOSS cohort. Infection. 2022;50:423–436. doi: 10.1007/s15010-021-01699-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.