INTRODUCTION
Systemic lupus erythematosus (SLE) is a connective tissue disorder characterized by the production of autoantibodies that can affect multiple organs in the body.1 Cardiac involvement is one of the most affected organs in the SLE.2 It can affect any part of the heart, including the pericardium, myocardium, heart valves, cardiac conduction system, and coronary arteries, leading to significant cardiac morbidity and mortality. Elderly patients are more likely to have cardiac involvement.3
Only a few cases of cardiac involvement as the initial manifestation of SLE have been reported in the literature. Pericardial effusion and cardiac tamponade are the rare initial manifestations of the SLE.4 Complete pericardial drainage by pericardiocentesis along with steroids and anti-inflammatory drug treatment is the mainstay of therapy in lupus-induced pericardial effusions.5 Refractory cases also may need surgery.
In this case report, a young female was described who presented to the hospital with non-specific symptoms, found to have pericardial effusion, and diagnosed with SLE.
CASE REPORT
A 23-year-old patient with no significant past medical history came in for generalized malaise, nausea, vomiting, and diarrhea. She started feeling unwell two months prior when she took over-the-counter medications for symptom relief, but they did not help. She went to a local hospital, had a chest x-ray, and was told that it looked normal. She was recommended to continue symptomatic treatment for a possible viral upper respiratory infection. Over the next three weeks, she experienced body aches, decreased appetite, intermittent nausea, and vomiting. She was sent back to the hospital where a chest x-ray showed a left-sided pleural effusion, confirmed on the chest CT scan. She had a thoracentesis with a total of 650 mL fluid removed.
She was diagnosed with an uncomplicated parapneumonic effusion, given empiric antibiotics, and was discharged home to complete her course of antibiotics orally. After two weeks, she was seen by her primary care physician and given a short five-day course of prednisone without much improvement. Her symptoms worsened over the next two weeks, and she was seen in the emergency room. Her symptoms this time included fever, chills, fatigue, malaise, dyspnea on exertion, non-productive cough, nausea, vomiting, and diarrhea.
The physical examination showed an arterial blood pressure of 119/77 mmHg, a respiratory rate of 32/min, a pulse rate of 134, and a body temperature of 101.2°F with distant cardiac sounds and left-sided decreased breath sounds. An electrocardiogram showed sinus tachycardia. Chest x-ray showed cardiomegaly without pulmonary edema and left pleural effusion with basilar airspace opacity. She was diagnosed with sepsis from left lower lobe pneumonia; cultures were taken, intravenous fluids were given, and empiric antibiotics were started.
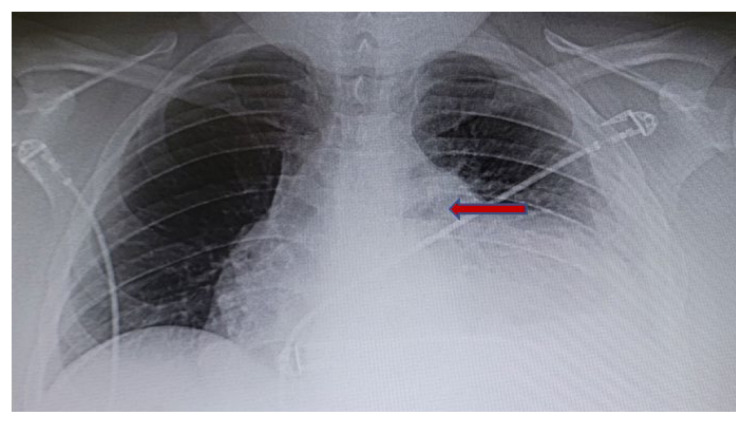
Over the next two days, the patient made minimal improvement clinically. A repeat chest x-ray showed a moderate left-sided pleural effusion and cardiomegaly (Figure 1). Thoracentesis was ordered, but ultrasound showed there was not enough pleural fluid to be drained. There was a concern for immunodeficiency with repeated infections and pneumonia. Blood and sputum cultures were negative.
Figure 1.
Chest x-ray showed cardiomegaly due to pericardial effusion.
Laboratory tests, including troponins, were within the normal range, except for moderate anemia with hemoglobin of 10.6 g/dl. A 2-D transthoracic echocardiogram showed a moderate to large pericardial effusion (Figure 2). The echocardiogram did not show any findings of cardiac tamponade, such as respiratory mitral/tricuspid inflow variation, or right atrial or ventricular diastolic collapse.
Figure 2.
2-D transthoracic echocardiogram showed pericardial effusion (arrows).
The cardiology service was consulted, and the patient underwent pericardiocentesis. Analysis of fluid revealed a white blood cell count of 314/mm3 (neutrophils 24%, lymphocytes 19%, monocytes 57%), total protein 4.2 g/dl, albumin of 1.7 g/dl (serum Alb 2.5), glucose of 46 (serum glucose 78). Further questioning revealed that she had pain in her metacarpophalangeal and interphalangeal joints. Blood analysis for the autoimmune panel was positive for anti-dsDNA antibodies (Table 1).
Table 1.
Pertinent serum autoimmune panel.
| Smith IgG Ab | > 8 U/ml |
| dsDNA Ab | > 300 IU/ml |
| Chromatin Ab | > 8 U/ml |
| Anti U1-RNP Ab | > 8 U/ml |
| RF | < 1 IU/ml |
Abbreviations: Smith IgG Ab = Anti-Smith antibodies, dsDNA Ab = Anti deoxyribonucleic acid antibodies, Chromatin Ab = Anti chromatin antibodies, U1-RNP Ab = Anti ribonucleoprotein antibodies, RF = Rheumatoid factor.
The patient had a pericardial drain placed after pericardiocentesis, which was removed the next day. She met the criteria for SLE and lupus-induced pericardial effusion. She was discharged and referred to a rheumatology clinic, where she was started on immunosuppressive therapy.
DISCUSSION
SLE can cause many cardiac manifestations, such as myocarditis, pericarditis, endocarditis, and cardiac conduction system abnormalities.6 The acute or chronic inflammatory changes of SLE can involve pericardium causing granular deposition of immunoglobin and c3 immune complexes detected by direct immunofluorescence. The detection of these immune complexes ropes the mechanism of pericardial involvement in SLE, especially in pericarditis. Echo cardiac studies have reported the prevalence of pericardial abnormalities among SLE patients ranging from 10 – 55%. Pericarditis is considered the most common symptomatic clinical manifestation of SLE and is estimated to occur in 25% of cases at some point in the disease course. Pericardial effusions are more common to occur in SLE patients. More than 40% of SLE cases can have asymptomatic pericardial effusion detected by echocardiography during the disease course.5,6
When present, pericardial effusions in SLE are usually small and do not cause severe hemodynamic complications.7 Signs and symptoms of pericardial effusions more likely can be pericardial pain and active lupus symptoms elsewhere in the body. Echocardiography is the standard method to detect small pericardial effusions in SLE patients. SLE-related pericardial effusion differential diagnosis includes viral, bacterial, tuberculosis, post-myocardial infarction, traumatic, uremic, neoplastic, and idiopathic.7,8
Cardiac manifestations usually occur in the later stage of the disease course in older patients.1,8 Pericardial effusion in this young patient as an initial manifestation was another striking finding. Topaloglu et al.9 reported a case of cardiac tamponade due to large pericardial effusion in a young male patient leading to the surgical treatment. Weich et al.10 described large pericardial effusions diagnosed by echocardiography in a case series of eight patients, but none of them had pericardial effusions as the presenting manifestation of SLE.
CONCLUSIONS
In essence, this case report highlighted pericardial effusion as an unusual initial manifestation of SLE even in the absence of typical symptoms. It should be part of differential diagnosis, especially in young patients presenting with non-specific repeated infections. Undetected pericardial effusion can lead to the pericardial tamponade, thus increasing significant mortality risk.
REFERENCES
- 1.Baker SB, Rovira JR, Campion EW, Mills JA. Late onset systemic lupus erythematosus. Am J Med. 1979;66(5):727–732. doi: 10.1016/0002-9343(79)91109-4. [DOI] [PubMed] [Google Scholar]
- 2.Moder KG, Miller TD, Tazelaar HD. Cardiac involvement in systemic lupus erythematosus. Mayo Clin Proc. 1999;74(3):275–284. doi: 10.4065/74.3.275. [DOI] [PubMed] [Google Scholar]
- 3.Gulati S, Kumar L. Cardiac tamponade as an initial manifestation of systemic lupus erythematosus in early childhood. Ann Rheum Dis. 1992;51(2):279–280. doi: 10.1136/ard.51.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hejtmancik MR, Wright JC, Quint R, Jennings FL. The cardiovascular manifestations of systemic lupus erythematosus. Am Heart J. 1964;68:119–130. doi: 10.1016/0002-8703(64)90248-0. [DOI] [PubMed] [Google Scholar]
- 5.Kao AH, Manzi S. How to manage patients with cardiopulmonary disease? Best Pract Res Clin Rheumatol. 2002;16(2):211–227. doi: 10.1053/berh.2001.0222. [DOI] [PubMed] [Google Scholar]
- 6.Doria A, Petri M, Doria A, Pauletto P. Cardiac involvement in systemic lupus erythematosus. In: Atzeni F, Dorea A, Nurmohamed M, Pauletto P, editors. The Heart in Systemic Autoimmune Disease. First Edition. Amsterdam: Elsevier; 2004. pp. 146–162. [Google Scholar]
- 7.Leung WH, Wong KL, Lau CP, Wong CK, Cheng CH. Cardiac abnormalities in systemic lupus erythematosus: A prospective M-mode, cross-sectional and Doppler echocardiographic study. Int J Cardiol. 1990;27(3):367–375. doi: 10.1016/0167-5273(90)90294-f. [DOI] [PubMed] [Google Scholar]
- 8.Tincani A, Rebaioli CB, Taglietti M, Shoenfeld Y. Heart involvement in systemic lupus erythematosus, anti-phospholipid syndrome and neonatal lupus. Rheumatology (Oxford) 2006;45(Suppl 4):iv8–13. doi: 10.1093/rheumatology/kel308. [DOI] [PubMed] [Google Scholar]
- 9.Topaloglu S, Aras D, Ergun K, Altay H, Alyan O, Akgul A. Systemic lupus erythematosus: An unusual cause of cardiac tamponade in a young man. Eur J Echocardiog. 2006;7(6):460–462. doi: 10.1016/j.euje.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Weich HS, Burgess LJ, Reuter H, Brice EA, Doubell AF. Large pericardial effusions due to systemic lupus erythematosus: A report of eight cases. Lupus. 2005;14(6):450–457. doi: 10.1191/0961203305lu2131oa. [DOI] [PubMed] [Google Scholar]