Abstract
Introduction
Sclerotomy related retinal breaks (SRRBs) are a risk factor for postoperative retinal detachment (RD). Endolaser posterior to sclerotomy wounds decreased the risk of SRRBs after 20G pars plana vitrectomy (PPV) for macular disease. However, similar data do not exist for 25G and 23G wounds.
Methods
A retrospective cohort study of patients after 23G and 25G PPV for macular pathology was conducted between August 2017 and August 2020. The primary outcome was the postoperative rate of SRRBs or RDs. The secondary outcome was the postoperative rate of pupillary dysfunction and neurotrophic keratopathy. All participants had a minimum postoperative follow-up of one year.
Results
One hundred seventeen patients were included in the study (62 in the laser group and 55 in the control group). Mean age was 65.4 ± 11.3 years (56.4% female and 43.6% male). Most of the laser group underwent 23G PPV (90%) while most of the control group underwent 25G PPV (96%). One patient in the control group developed RD secondary to a SRRB. No SRRBs or RDs developed in the laser group. None of the secondary outcomes developed in either group after one year.
Conclusions
To the best of the authors’ knowledge, this is the first report in the literature on prophylactic laser posterior to small gauge sclerotomies (25G and 23G) during macular surgery. Laser treatment posterior to small gauge sclerotomies (25G and 23G) had a similar incidence of SRRBs as with 20G sclerotomies. Larger prospective studies are needed to further understand the role of laser in lowering SRRB risk.
Keywords: retinal breaks, retinal detachment, ophthalmological surgical procedures, vitrectomy, treatment outcome
INTRODUCTION
Retinal detachment (RD) after pars plana vitrectomy (PPV) for macular surgery is a devastating vision threatening condition. A significant risk factor for RD development after macular surgery is surgical wound related retinal breaks, also known as sclerotomy related retinal breaks (SRRBs).1 SRRBs incidence reach up to 5.1% with 25-gauge (25G) and 7.2% with 20-gauge (20G) macular surgeries. SRRBs have been associated with 22.2% of RDs after idiopathic macular hole surgery and 44.4% of RDs after epiretinal membrane peel.2 A key factor in the development of SRRBs includes vitreous incarceration into the surgical wound, which subsequently contracts and creates SRRBs.3
Wound structure modifications attempt to decrease vitreous incarceration by creating a self-sealing wound (e.g., two step oblique wounds), using smaller surgical instruments (e.g., 25G versus 20G), and utilizing valved pars plana cannulas. Despite these measures, postoperative vitreous incarceration occurs similarly between 23G, 25G, and 27G surgeries.4 There have been other attempts aimed towards supporting the retina at traction sites, including prophylactic scleral buckling, 360-degree cryotherapy, and 360-degree laser. These have been shown to decrease successfully postoperative SRRBs,5–7 but they can cause undesirable side effects (e.g., pupillary dysfunction, refractive error, and ocular inflammation).8,9
Laser posterior to sclerotomy sites in 20G vitrectomy has been shown to decrease postoperative SRRBs and avoids the risks associated with 360-degree endolaser.10 However, the benefits of localized prophylactic laser treatment in smaller 23G and 25G macular surgeries remain unknown. To fill the current gap in knowledge, this study was conducted to identify the effect of localized prophylactic laser treatment in 23G and 25G macular vitrectomies.
METHODS
The authors implemented a retrospective cohort study design. To identify study participants, 23G and 25G macular surgeries performed between August 2017 and August 2020 at the tertiary referral center were reviewed. Screening extended until August 2020 to allow for one year of postoperative follow up. Study population included adults who were compliant with their postoperative care, and excluded patients with proliferative vitreoretinopathy (PVR), proliferative diabetic retinopathy (PDR), open globe injuries, loss of follow up, or were less than 18 years old.
The study had two groups: the control group did not have prophylactic laser performed while the treatment group had prophylactic laser performed posterior to sclerotomy wounds. The primary outcome of the study was to determine the rate of SRRBs and RDs after macular vitrectomy surgery. The secondary outcome was to determine the rate of pupillary dysfunction and neurotrophic keratopathy. The end point of this study’s primary and secondary outcomes was one year after surgery.
All participants’ operative reports included documentation of careful peripheral vitreous shaving and an intraoperative scleral depressed fundus exam to exclude intraoperative SRRBs. Surgeries were performed using the Constellation® vitrectomy system (Alcon, Inc., USA). In the laser group, prophylactic laser treatment consisted of three rows of confluent medium intensity endolaser posterior to the sclerotomy wound, with laser extending for approximately one-half clock hour on either side of each wound (Figure 1).
Figure 1.
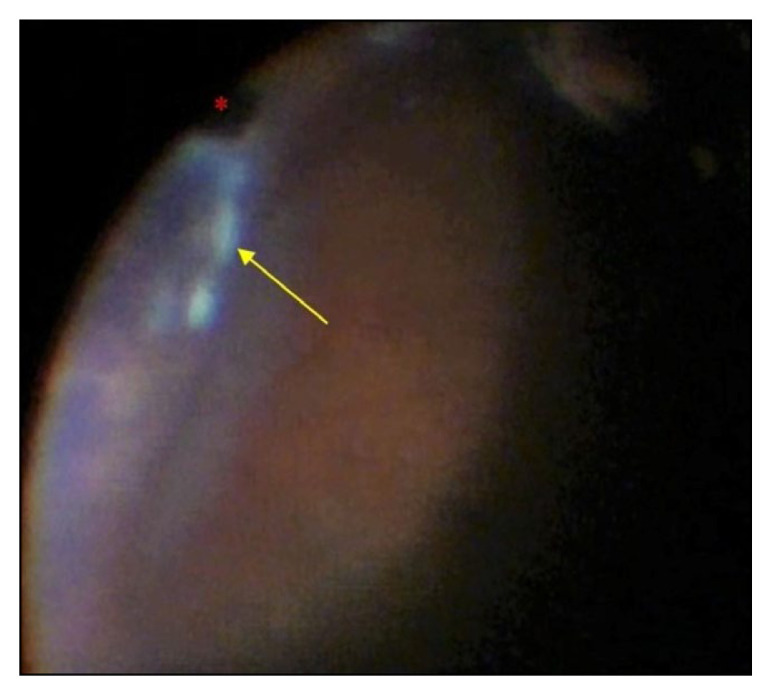
Surgical microscope fundus view during endolaser treatment posterior to sclerotomy wound. White laser marks (yellow arrow) posterior to sclerotomy wound and infusion cannula (red asterisk).
Statistical analysis was performed using RStudio® (version: 1.1.453; Boston, MA). Categorical variables were described using proportions. Continuous variables were described as means ± standard deviations. A series of independent sample t-tests, dependent sample t-tests, and independent sample tests of proportion were conducted. A sub-analysis of outcomes and complications between groups was conducted. A p value of 0.05 was used as the threshold value for statistical significance, and a confidence interval of 95% was chosen. Microsoft Office® Excel® 2020 was used for data collection (e.g., age, gender, vitrectomy gauge, reason for surgery, and postoperative adverse events). The institutional ethics review board (IRB) approved this study.
RESULTS
The study demographics included 117 patients who met the inclusion criteria. Patients’ ages ranged from 23 to 90 years old (mean age of 65.4 ± 11.3 years old). The study cohort was 56.4% female and 43.6% male. Of the 117 patients, 90% of the laser treatment group underwent 23G vitrectomy while 96% of the control group underwent 25G vitrectomy. Study cohort demographics and results are summarized in Table 1.
Table 1.
Cohort demographics and results summary.
| Control Group | Laser Group | p Value | |
|---|---|---|---|
| Sample size | 55 | 62 | 0.58 |
| Age | 66.15 ± 10.66 | 64.69 ± 11.93 | 0.49 |
| Gender | |||
| Females | 27 (49%) | 39 (63%) | 0.19 |
| Males | 28 (51%) | 23 (37%) | 0.19 |
| PPV‡ | |||
| 23G* | 2 (4%) | 56 (90%) | <0.001 |
| 25G** | 53 (96%) | 6 (10%) | <0.001 |
| Primary outcome | 1 (1.8%) | 0 | 0.95 |
| Secondary outcome | 0 | 0 | n/a |
PPV‡: pars plana vitrectomy; 23G*: 23-gauge; 25G**: 25-gauge
The control group had 55 patients with mean age of 66.2 ± 10.7 years old. There were 27 females and 28 males (49% and 51%, respectively). Fifty-three patients had 25G vitrectomy and two patients had 23G vitrectomy (96% and 4%, respectively). Primary outcome analysis of the control group identified one patient with a superior rhegmatogenous RD secondary to a SRRB one month after 25G PPV (1.82%), this was consistent with reported postoperative SRRBs rates in the literature.1 Secondary outcomes analysis had no patients with pupillary dysfunction or neurotrophic keratopathy.
The prophylactic laser group had 62 patients with mean age of 64.7 ± 11.9 years old. There were 39 females and 23 males (63% and 37%, respectively). Fifty-six patients had 23G vitrectomy and six patients had 25G vitrectomy (90% and 10%, respectively). Primary outcome analysis of the laser group identified no patients with postoperative SRRBs or RDs. Secondary outcome analysis had no patients with postoperative pupillary dysfunction or neurotrophic keratopathy.
Statistical analysis detected balanced study groups when comparing sample size (p = 0.58), mean age (p = 0.59), and gender (p = 0.19). There was a statistically significant difference between groups when comparing surgical wound size (p < 0.001) with 96% of the control group having smaller surgical wounds (25G) and 90% of the laser group having larger surgical wounds (23G). This difference places the laser group at a disadvantage because smaller (25G) surgical wounds have a lower chance of SRRBs development compared to larger (23G) wounds.
DISCUSSION
This study compared the effect of prophylactic laser treatment posterior to sclerotomy wounds on SRRB development after 23G and 25G macular vitrectomies. There were no SRRBs, RDs, pupillary dysfunction, or neurotrophic keratopathy in the prophylactic laser group after one year. This is similar to reported data of localized laser treatment posterior to sclerotomy sites in 20G vitrectomy.10 On the other hand, the control group had one patient who developed a superior RD secondary to a SRRB after 25G vitrectomy, which is within the reported incidence rate in the literature. No pupillary dysfunction or neurotrophic keratopathy developed in the control group.
Residual vitreous plays a major role in SRRBs development. Incarcerated vitreous in the surgical wound contracts and pulls on the retina causing postoperative SRRBs.3 In prior literature, attempts to decrease vitreous incarceration by creating smaller self-sealing wounds have decreased the rate of postoperative SRRBs and RDs.4 However, it did not completely prevent vitreous incarceration, which was similar across 23G, 25G, and 27G wounds. In this study, all patients had their surgical wounds evaluated for closure by the end of surgery. If a possible wound leak was present, a 7-0 Vicryl® suture was used to confirm wound closure.
Supporting neurosensory retina adhesion to the underlying retinal pigment epithelium (RPE) is another approach to decrease SRRBs development. This is achieved by creating a tightly adherent retinal scar using laser treatment or cryotherapy. Surgical 360-degree endolaser treatment has been shown to decrease postoperative SRRBs and retinal detachment after macular surgery.6 However, 360-degree endolaser damages short and long posterior ciliary nerves, decreases corneal sensation, and can cause anisocoria and mid-dilated pupils.8,9 Local laser treatment behind sclerotomy sites avoids damaging the horizontal long posterior ciliary nerves. In this study, none of the laser treatment group patients developed pupillary dysfunction. Corneal sensation was not assessed in this retrospective study, but the corneal surface was evaluated as part of the comprehensive clinical exam.
Epiretinal membrane (ERM) formation is a hypothesized side effect after 360-degree endolaser.11 Blood-retina barrier damage and serum leakage into the vitreous cavity may attract RPE migration and ERM formation.12 None of the laser group patients developed ERM within one year after surgery. This finding may be explained by the fact that localized laser treatment around sclerotomy sites causes less extensive retinal damage compared to 360-degree laser or cryotherapy. Another possible explanation is that the peeling of the internal limiting membrane during macular surgery removes the physiological scaffold for recurrent macular ERM formation.
Cryotherapy decreases postoperative SRRBs and RDs by creating a strong retinal scar.7 However, 360-cryotherapy affects a larger surface area and causes more tissue damage compared to laser. This increases the risk of postoperative PVR and membrane formation. In addition, cryotherapy is more painful and can cause severe postoperative eye inflammation. Scleral buckling is another approach to support neurosensory retina attachment that avoids retinal scarring by scleral indentation.5 While scleral buckling supports the retina periphery 360-degree when treating retinal detachments, it is too invasive to perform prophylactically with macular surgery and can cause undesirable side effects (e.g., increased postoperative pain, double vision, refractive error, and anterior segment ischemia). In the presented study, the laser group had zero SRRBs and RDs, like reported results after 20G macular vitrectomy,10 and avoided the negative side effects associated with cryotherapy or scleral buckling.
Surgical experience is an important factor that frequently arises when studying surgical outcomes. The surgeon’s experience has not been shown to affect the rate of intraoperative retinal tears or postoperative RDs.13 Wilkinson et al.14 did not find an increased incidence of RDs after PPV surgeries performed by vitreoretinal fellows when compared to attending surgeons. In the presented study, participating surgeons had five to six years of experience performing retinal surgery. It was hypothesized that the similarity in experience levels between the surgeons minimizes surgeon’s experience bias between the study groups. Furthermore, the rate of SRRBs and RDs in the control group was 1.82%, which was in the lower range of the rates reported after 25G macular surgery. It is essential to highlight that this study focused on macular vitrectomy patients, and the results should not be applied to RD cases. Many of the techniques discussed earlier (e.g., 360-degree endolaser, cryotherapy, and scleral buckling) improve the success rate of RD repair and have an important role in today’s retina procedures.
This study has several strengths. A key strength was the extended postoperative follow-up duration of one year. This duration exceeded the three to six months postoperative duration for SRRBs and RDs reported in prior literature.15 It also surpassed the mean postoperative period for other complications like ERM formation, pupillary dysfunction, or decreased corneal sensation.9 The one-year follow-up also provided input on delayed wound-related outcomes.
Age is another important factor that affects wound healing. When compared to older patients, young patients have greater healing ability and a higher risk for proliferative vitreoretinopathy.16 The age balanced groups were a strength of this study because it reduced the age-related bias in wound healing and vitreous-retinal traction risk.
Another strength in the study was the larger number of 23G surgical wound patients in the laser group. Wound-related complications have been shown to increase with larger wound size (23G) compared to smaller wound size (25G).1,17 Despite the increased wound-related complication risk in the laser group, none of the laser group patients developed postoperative SRRBs or RDs after one year. It was hypothesized that these results were because of the protective effect of localized laser treatment in stabilizing the retina posterior to sclerotomy wounds.
The retrospective nature of the study was one of its limitations. It did not allow for randomization of participants and resulted in an unbalanced distribution of 23G and 25G vitrectomies between groups (p < 0.001). Another study limitation was the difference in the number of phakic and pseudophakic/aphakic patients between groups since phakic patients are at increased risk of developing SRRB. The one patient who developed SRRB in the control group was phakic. However, there was no statistically significant difference in the proportion of phakic patients between the study groups; 27 patients in the control group (49%), and 23 in patients in the laser group (37%; p = 0.26).
The effect of localized laser treatment posterior to 27G sclerotomy wounds remains unknown. Although 27G vitrectomy wounds are made perpendicular to the sclera because of their smaller wound size, the rate of vitreous wound incarceration was found to be similar to larger gauge wounds.4 Reports on postoperative outcomes after 27G vitrectomy have inconsistent results and complications.4,18,19 Our institution rarely performed 27G vitrectomy, but it was hypothesized that the smaller gauge wounds limit the amount of vitreous incarcerated and later contracted. Further studies need to be conducted to understand the effect of localized laser treatment on SRRBs after 27G vitrectomy.
CONCLUSIONS
The present study was designed to determine the effect of prophylactic laser treatment posterior to sclerotomy sites in 23G and 25G macular surgeries. The prophylactic laser treatment group had a superior outcome compared to the control group with no postoperative SRRBs or RDs. However, this difference was minimal and not statistically significant. Larger prospective studies are needed to further an understanding of the role of retina laser treatment posterior to sclerotomy wounds.
REFERENCES
- 1.Tan HS, Mura M, de Smet MD. Iatrogenic retinal breaks in 25-gauge macular surgery. Am J Ophthalmol. 2009;148(3):427–430. doi: 10.1016/j.ajo.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Guillaubey A, Malvitte L, Lafontaine PO, et al. Incidence of retinal detachment after macular surgery: A retrospective study of 634 cases. Br J Ophthalmol. 2007;91(10):1327–1330. doi: 10.1136/bjo.2007.115162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krieger AE. The pars plana incision: Experimental studies, pathologic observations, and clinical experience. Trans Am Ophthalmol Soc. 1991;89:549–621. [PMC free article] [PubMed] [Google Scholar]
- 4.Tosi GM, Malandrini A, Cevenini G, et al. Vitreous incarceration in sclerotomies after valved 23-, 25-, or 27-gauge and nonvalved 23- or 25-gauge macular surgery. Retina. 2017;37(10):1948–1955. doi: 10.1097/IAE.0000000000001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang TS, McGill E, Hay DA, et al. Prophylactic scleral buckle for prevention of retinal detachment following vitrectomy for macular hole. Br J Ophthalmol. 1999;83(8):944–948. doi: 10.1136/bjo.83.8.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iwase T, Jo YJ, Oveson BC. Effect of prophylactic 360° laser treatment for prevention of retinal detachment after phacovitrectomy: (Prophylactic 360° laser treatment for prevention of retinal detachment) BMC Ophthalmol. 2013;13:77. doi: 10.1186/1471-2415-13-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wimpissinger B, Binder S. Entry-site-related retinal detachment after pars plana vitrectomy. Acta Ophthalmol Scand. 2007;85(7):782–785. doi: 10.1111/j.1600-0420.2007.00930.x. [DOI] [PubMed] [Google Scholar]
- 8.Barrada OA, Nabih MH, Khattabm AM, Nosseir AA. 360° laser retinopexy in preventing retinal re-detachment after 23-gauge vitrectomy for primary repair of retinal detachment. Egyptian Retina Journal. 2015;3(1):1–9. [Google Scholar]
- 9.Bouheraoua N, Hrarat L, Parsa CF, et al. Decreased corneal sensation and subbasal nerve density, and thinned corneal epithelium as a result of 360-degree laser retinopexy. Ophthalmology. 2015;122(10):2095–2102. doi: 10.1016/j.ophtha.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Kim CS, Kim KN, Kim WJ, Kim JY. Intraoperative endolaser retinopexy around the sclerotomy site for prevention of retinal detachment after pars plana vitrectomy. Retina. 2011;31(9):1772–1776. doi: 10.1097/IAE.0b013e31820b6129. [DOI] [PubMed] [Google Scholar]
- 11.Chaturvedi V, Basham RP, Rezaei KA. Scleral depressed vitreous shaving, 360 laser, and perfluoropropane (C3 F8) for retinal detachment. Indian J Ophthalmol. 2014;62(7):804–808. doi: 10.4103/0301-4738.138621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaccoma EH, Conway BP, Campochiaro PA. Cryotherapy causes extensive breakdown of the blood-retinal barrier. A comparison with argon laser photocoagulation. Arch Ophthalmol. 1985;103(11):1728–1730. doi: 10.1001/archopht.1985.01050110124039. [DOI] [PubMed] [Google Scholar]
- 13.Covert DJ, Henry CR, Bhatia SK, Croskrey J, Sanchez CR, Han DP. Intraoperative retinal tear formation and postoperative rhegmatogenous retinal detachment in transconjunctival cannulated vitrectomy systems compared with the standard 20-gauge system. Arch Ophthalmol. 2012;130(2):186–189. doi: 10.1001/archopthalmol.2011.1378. [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson JT, Richards AB, Choi D, Robertson JE, Jr, Flaxel CJ. Incidence of retinal detachment after fellow-performed primary pars plana vitrectomy. ISRN Ophthalmol. 2013;2013:353209. doi: 10.1155/2013/353209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Harthi E, Abboud EB, Al-Dhibi H, Dhindsa H. Incidence of sclerotomy-related retinal breaks. Retina. 2005;25(3):281–284. doi: 10.1097/00006982-200504000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hu Y, Tang S. Major challenges in vitreoretinal surgery. Taiwan J Ophthalmol. 2015;5(1):9–14. doi: 10.1016/j.tjo.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim M, Park YS, Lee DH, Koh HJ, Lee SC, Kim SS. Comparison of surgical outcome of 23-gauge and 25-gauge microincision vitrectomy surgery for management of idiopathic epiretinal membrane in pseudophakic eyes. Retina. 2015;35(10):2115–2120. doi: 10.1097/IAE.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 18.Khan MA, Shahlaee A, Toussaint B, et al. Outcomes of 27-gauge microincision vitrectomy surgery for posterior segment disease. Am J Ophthalmol. 2016;161:36–43e1. doi: 10.1016/j.ajo.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 19.Sborgia G, Niro A, Sborgia L, et al. One-year outcomes of 27-gauge versus 25-gauge pars plana vitrectomy for uncomplicated rhegmatogenous retinal detachment repair. Int J Retina Vitreous. 2019;5:13. doi: 10.1186/s40942-019-0164-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


