Abstract
The respiratory epithelium is highly complex, and its composition varies along the conducting airways and alveoli. In addition to their primary function in maintaining the respiratory barrier and lung homeostasis for gas exchange, epithelial cells interact with inhaled pathogens, which can manipulate cell signaling pathways, promoting adhesion to these cells or hosting tissue invasion. Moreover, pathogens (or their products) can induce the secretion of chemokines and cytokines by epithelial cells, and in this way, these host cells communicate with the immune system, modulating host defenses and inflammatory outcomes. This review will focus on the response of respiratory epithelial cells to two human fungal pathogens that cause systemic mycoses: Aspergillus and Paracoccidioides. Some of the host epithelial cell receptors and signaling pathways, in addition to fungal adhesins or other molecules that are responsible for fungal adhesion, invasion, or induction of cytokine secretion will be addressed in this review.
Keywords: epithelial cell, respiratory, lung, airway, Aspergillus, Paracoccidioides, cytokine, adhesion, invasion
1. Introduction
As we breathe, several microorganisms and other stimuli enter our respiratory system and make the primary contact with the epithelium, which acts not only as a physical barrier but also as an important key for the host’s immune defense. The functional differences and the cell complexity of the epithelia can be verified along the upper respiratory tract (nasal cavity, pharynx, and larynx), through the conducting airways (trachea, bronchi, and bronchioles) and to the alveoli [1,2,3]. Through cell–cell communication, including with immune cells, epithelial cells are essential for respiratory system homeostasis. If the regulatory mechanisms are in disequilibrium, a disease state may be triggered in the individual [2].
Histology of the airway epithelium varies according to the region of the respiratory tract. Most of this epithelium is pseudostratified and composed of (i) basal cells, which can renew the epithelium and differentiate into other cell types; (ii) club cells that also have epithelial renewal properties and secrete an important anti-inflammatory protein called uteroglobin; (iii) ciliated cells, which beat their cilia and play an essential role in expelling microorganisms and other foreign particles; (iv) goblet cells, which produce mucus and act with ciliated cells to assist airway clearance; and (v) pulmonary neuroendocrine cells, which are rare cells that secrete neuropeptides, promoting nervous and immune responses (see ref. [2] for review). Tuft cells, pulmonary ionocytes, hillock cells, and microfold cells were also identified in the airways, but the precise functions of these cells in the respiratory system require further study [2]. In contrast, the alveolar epithelium consists mostly of types I and II alveolar epithelial cells (also known as pneumocytes). The type I alveolar epithelial cell is a large and very thin cell, and its primary function is gas exchange. The type II cell has a cuboidal shape and secretory functions, such as surfactant production [3,4].
In addition to forming a physical barrier, lung epithelial cells function as sensors in the respiratory tract, interacting and responding to microorganisms and other particles. Stable lung homeostasis is also maintained by interactions with a sparse and diverse microbiome, but when dysbiosis occurs, lung diseases may develop. Lung microbiome disruption is associated with the progression of chronic obstructive pulmonary disease, cystic fibrosis, and idiopathic pulmonary fibrosis [5,6,7].
Pathogenic bacteria, viruses, or fungi also interact with lung epithelial cells and may exploit host cell receptors, leading to a better cell adhesion (and frequent invasion), establishing an infection in the host. In the context of the host immunological response, epithelial cells present on their surfaces pattern recognition receptors (PRRs) that recognize pathogen-associated molecular patterns (PAMPs) in microorganisms, triggering the release of chemokines and cytokines that modulate the immune response [3]. In fungi, mannans or glucans are examples of PAMPs that are recognized by PRRs such as toll-like receptors (TLRs) and dectins [8].
According to The Global Action For Fungal Infections (GAFFI), 2 million people die of fungal diseases every year [9]. Some of these fungi can cause endemic or opportunistic respiratory mycoses, which can result from the inhalation of fungal spores, reactivation of latent fungi, or hematological dissemination. Endemic fungi are usually found in specific regions of the world, and they are thermally dimorphic, i.e., these fungi exhibit a mycelial form in the environment and a yeast form within the host. While endemic fungi may promote disease in healthy individuals, most opportunistic cases occur in immunocompromised people [10,11].
This review addresses the important responses of epithelial cells to two relevant fungi that cause pulmonary mycoses. The first fungus is the filamentous Aspergillus which the COVID-19 pandemic brought to light once again [12], and the second is Paracoccidioides which causes an endemic mycosis in Latin America and is considered a neglected disease that may lead to severe sequelae of the lungs and other organs [13].
2. Aspergillus
Lung diseases caused by Aspergillus affect more than 10 million people, resulting in approximately 200,000 deaths annually [14]. This fungus causes a complex variety of diseases that have different pathogenic mechanisms and clinical manifestations, and are associated with patients who exhibit distinct immune responses [15]. Latgé and Chamilos [15] described three major groups of aspergillosis syndromes: (i) hypersensitivity-allergy, which includes severe asthma with fungal sensitization and allergic bronchial pulmonary aspergillosis; (ii) structural disease, including aspergilloma, chronic pulmonary aspergillosis, and semi-invasive forms; and (iii) severe immunodeficiency, which contains invasive pulmonary aspergillosis, invasive bronchial aspergillosis, and central nervous system aspergillosis (extrapulmonary).
Recently, the incidence of COVID-19-associated pulmonary aspergillosis in intensive care units was indicated to be approximately 10% to 15% [16]. This coinfection raises concerns about the high mortality among critically ill patients during the COVID-19 pandemic [12]. The problem requires multiple approaches to find a solution, including prevention, diagnosis, and treatment. In addition, new drugs or treatment protocols are necessary to overcome drug resistance in fungi. As an antifungal agent and an immunoadjuvant, all-trans retinoic acid is a promising agent that could be used in combination with classic antifungal drugs, reducing their dose and side effects [17,18].
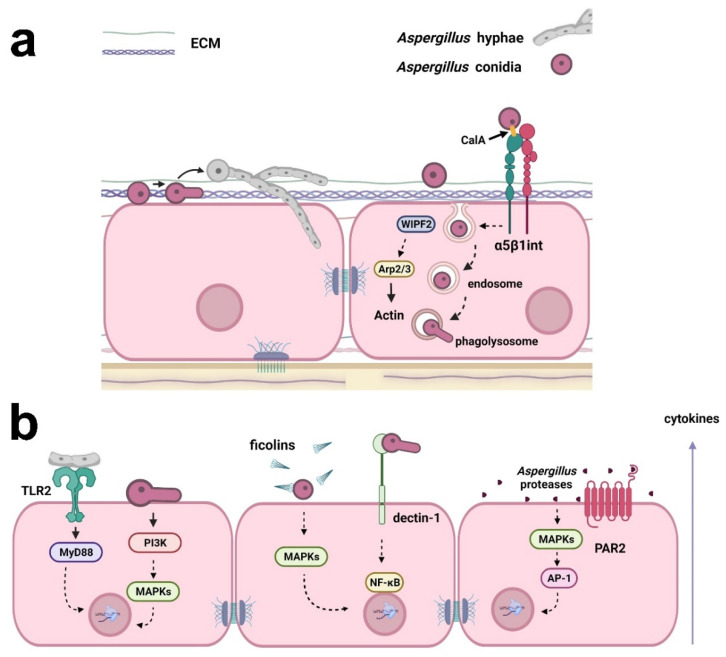
It is essential to understand the signaling processes in host-fungus interactions to pave the way for future clinical improvements, which will benefit the patient. Host-fungus interactions involve a plethora of mechanisms and evoke different explanations for Aspergillus invasion in the lung. This is important because lung epithelial cells respond diversely depending on the kind of insult or stress that is causing the injury [19]. The major view on this aspect indicates that conidia can bind and germinate on the surface of alveolar epithelial cells following active hyphal invasion (Figure 1) [20]. Despite the invasion, the morphology of epithelial cells seems to remain unaltered. Whether invasion requires the impairment of cell integrity is still a matter of debate, although there is sufficient evidence suggesting that epithelial invasion by hyphae can be achieved through actin remodeling in bronchial epithelial cells without disturbing morphology or epithelial integrity [21]. Thus, questions remain about the mechanisms responsible for this fungal cell invasion.
Figure 1.
Examples of the responses of respiratory epithelial cells to Aspergillus infection. (a) Aspergillus conidia can bind to extracellular matrix (ECM) proteins and epithelial cell surface. Conidia may germinate on the surface of epithelial cells, and the resulting hyphae can actively invade the cells. Conidia internalization may occur through fungal CalA interaction with host α5β1 integrin and WIPF2, Arp2/3, and actin reorganization. Conidia can also be trafficked in the endosomal system and germinate in phagolysosomes, reentering the extracellular space. (b) Cytokine secretion by epithelial cells may be a result of (i) the interaction of Aspergillus hyphae with TLR2, activating MyD88; (ii) the activation of PI3K and MAPKs by germinating conidia; (iii) the opsonization of Aspergillus conidia by ficolins and MAPK activation; (iv) interaction with dectin-1 and the activation of NF-κB; and (v) activation of MAPKs and the transcription factor AP-1 by Aspergillus proteases. Aspergillus proteases can also activate PAR2, inducing cytokine production. Created with Biorender.com.
Several research groups have been working on identifying the molecules involved in several steps of Aspergillus infection. At first, Aspergillus conidia adhere mostly to proteins and/or carbohydrates found in the membrane of epithelial cells or the surrounding host extracellular matrix (ECM) [22]. Kerr et al. [23], for example, have indicated that A. fumigatus conidia and the fungal lectin FleA, which recognizes fucosylated structures, avidly bind to purified lung mucins. Some proteins that participate in epithelial cell–cell adhesion, such as E-cadherin, were also described as molecules that cooperate in the adhesion of A. fumigatus conidia to lung epithelial cells [24]. The polysaccharide galactosaminogalactan, which is found in the hyphal cell wall of Aspergillus, mediates adhesion to epithelial cells and fibronectin [25]. Bouchara et al. [26] described that the binding of laminin and fibrinogen to a possible lectin present in A. fumigatus conidia was dependent on sialic acid residues present in these glycoproteins, and Warwas et al. [27] indicated that sialidase treatment of A. fumigatus spores decreased adherence to fibronectin in coated wells and conidia uptake by lung epithelial A549 cells. Conversely and strangely, the binding of A. fumigatus conidia to those cells increased when treated with sialidase. Thus, further studies are necessary to completely understand the role of different carbohydrates, including sialic acids, in fungal adhesion to ECM components or host cells.
In addition to adhesion, Aspergillus can also invade respiratory epithelial cells. Liu et al. [28] described that the thaumatin-like protein CalA, which is expressed on the surface of A. fumigatus conidia, participates in the mechanism of epithelial cell invasion by interacting with the host receptor α5β1 integrin. When using a CalA mutant, the authors did not observe a reduction of A. fumigatus conidia adhesion to the human alveolar epithelial cell line A549, suggesting that although CalA was expressed on the cell surface of the fungus, it was dispensable for the adhesion step. More importantly, endocytosis of the CalA mutant was reduced by epithelial cells, indicating the role of Aspergillus CalA as a fungal invasin rather than an adhesin [28]. Another mechanism was described by Culibrk et al. [29], who demonstrated a reduction of conidia internalization by the human airway epithelial cell line 1HAEo- after WAS-interacting protein family member 2 (WIPF2) silencing. As WIPF2 is known to mediate the function of actin related protein (Arp) 2/3 complex, which is responsible for actin reorganization, the authors presented the participation of this protein complex in this process [29].
Some studies have indicated that fungal spores can be absorbed by respiratory epithelial cells efficiently and rapidly, which contributes to Aspergillus spores digestion by mature host phagolysosomes [14,30]. Briefly, conidia are internalized and most of them are killed by epithelial cells. The conidia that survive are trafficked by the endosomal system to phagolysosomes, where they germinate and reenter the extracellular space, sustaining infection [22]. NADPH oxidase and reactive oxygen species (ROS) produced by mitochondria are redundant mechanisms by which alveolar macrophages and neutrophils kill fungi [31]. However, human epithelial cells are still neglected in this scenario and few studies have used them as an infection model.
Several studies have assessed the role of immune cells during fungal infection in the respiratory epithelium. For example, it is known that repeated exposure to Aspergillus conidia induces neutrophil transmigration [32] through a probable caspase recruitment domain (CARD) 9 signaling-dependent mechanism [33]. A study by Jepsen et al. [34] demonstrated that fibrinogen C domain-containing protein 1 (FIBCD1) acts as a PRR in epithelial cells, recognizing polysaccharides of the A. fumigatus cell wall, such as chitin, and modulating the TLR-dependent inflammatory response in the host [34].
A classic response against fungal pathogens involves the expression of interleukin (IL)-8, an important chemokine for neutrophil chemotaxis [35,36]. Liu et al. [37] have indicated that the conidia of A. fumigatus can induce IL-8 secretion in a time-dependent manner in A549 epithelial cells. A similar effect was observed when the release of monocyte chemoattractant protein 1 (MCP-1) was analyzed, but not for tumor necrosis factor (TNF)-α [37]. Another study using A549 cells and transcriptome analysis by RNA-seq indicated an increase in IL-6, IL-8, and, in contrast to Liu et al. [37], TNF-ɑ after interaction with A. fumigatus conidia. The mRNA level was confirmed by qRT-PCR [38]. This discrepancy between the findings with respect to TNF-ɑ expression in A549 cells may be explained by using different strains of A. fumigatus and varying experimental protocols. Meanwhile, the production of IL-6 and IL-8 by epithelial cells due to A. fumigatus infection was observed in several studies [39,40,41,42,43,44].
While IL-8 expression by macrophages is a well-known event dependent on TLR activation, the expression of IL-8 by respiratory epithelial cells in response to Aspergillus infection may also occur in a myeloid differentiation primary response (MyD) 88-independent manner as indicated by Balloy et al. [41], who demonstrated that germinating conidia promoted IL-8 secretion by epithelial cells after activation of the phosphatidylinositol 3-kinase (PI3K) and mitogen-activated protein kinase (MAPK) pathways [41]. On the other hand, Oya et al. [39] verified that pretreatment with TLR2 blocking antibodies promoted a reduction of IL-6 and IL-8 secretion levels in BEAS-2B bronchial epithelial cells incubated with A. fumigatus hyphal fragments, suggesting the involvement of this receptor [39]. In addition, there is evidence that A. fumigatus hyphae regulate the expression of IL-1β, IL-1ɑ, and TNF-α by mechanisms that involve the participation of TLR2, but these cytokines are not released by host cells [39]. By using A549 epithelial cells overexpressing FIBCD1, Jepsen et al. [34] verified that this protein suppressed TLR2- and TLR4-dependent IL-8 secretion when cells were infected with the conidia of A. fumigatus [34]. In contrast, the overexpression of FIBCD1 increased IL-8 secretion when it was induced by TLR5 in this model [34].
Another receptor that participates in signal transduction during Aspergillus infection is the C-type lectin receptor dectin-1 [37,44,45]. Liu et al. [37] demonstrated that Aspergillus conidia promoted the secretion of IL-8 and MCP-1 by epithelial cells through dectin-1 and nuclear factor κ-light-chain-enhancer of activated B cells (NFκB) activation [37]. In addition, Sun et al. [40] demonstrated that dectin-1 was regulated by TLR2 and was required for ROS production and TNFα, granulocyte-macrophage colony-stimulating factor (GM-CSF), and IL-8 mRNA expression in human bronchial epithelial cells incubated with Aspergillus [40].
One of the receptor families that participates in the activation of the lectin complement pathway is the soluble secreted PRR ficolin (in humans, there are three types of ficolins: M, H, and L) [46]. Ficolins have been reported to be mediators of the inflammatory response in epithelial cells due to Aspergillus infection by enhancing neutrophil recruitment [47]. H-ficolin, for example, binds to A. fumigatus conidia and, after opsonization, induces an increase in IL-8 secretion by A549 epithelial cells. This process is mediated by p38 MAPK, c-Jun N-terminal kinase (JNK), and mitogen-activated protein kinase (MEK) 1/2 [48].
Proteases from Aspergillus can disrupt epithelial integrity and disturb homeostasis and barrier function, culminating in an inflammatory response and consequently promoting disease in the individual [49,50]. A. fumigatus proteases are also described as a potential source for ECM component degradation [50], and most A. fumigatus allergens exert proteolytic activity. For example, Asp f 5 is a metalloprotease, while Asp f 13 and Asp f 18 are serine proteases [51,52]. Proteases present in fungi have been proven to interfere with epithelial barrier integrity by disrupting tight junctions, acting on occludin, zonula occludens-1 (ZO-1), and claudins, which increases permeability and facilitates antigen access through the epithelium [53].
Regarding the inflammatory response, Kim et al. [49] verified that Aspergillus proteases could increase the expression and secretion levels of IL-1β, IL-6, IL-8, and transforming growth factor (TGF)-β by human primary bronchial epithelial cells. In addition, these authors also demonstrated that proteases from Aspergillus induced mitochondrial ROS, which in turn activated MAPK and activator protein 1 (AP-1), enhancing the inflammatory response in these cells [49]. In a recent study, Rowley et al. [44] demonstrated that inhibitors of serine-, cysteine-, and metalloproteases reduced IL-8 level secretion by the human bronchial epithelial 16HBE14o- cell line in the presence of Aspergillus conidia, suggesting a potential role of those proteases in the inflammatory response induced by the fungus [44]. Moreover, proteases can cleave an extracellular domain of protease-activated receptors (PARs). PAR2, for example, is a target of fungal serine proteases and participates in IL-33 expression when human sinonasal epithelial cells are incubated with A. fumigatus [54].
We know that fungal proteases and extracellular vesicles (EVs) can trigger paracrine signals and prepare the environment for infection while fungal structures are still not in contact with the host tissue. EVs can deliver cargo to tissue, inducing changes in the host and ultimately benefiting the fungus [55,56,57]. On the other hand, although Aspergillus EVs can transport proteins related to redox signaling, cell wall remodeling, and lipid/sugar metabolism, they induce M1 macrophage polarization, leading to phagocytosis and fungal clearance [56,58,59]. Whether Aspergillus EV interactions with host immune cells are beneficial or detrimental to the fungus remains a matter of debate. Moreover, the role of these EVs when they interact with respiratory epithelial cells remains largely unknown and is an opportunity for further investigation.
Considered together, there is consistent evidence that A. fumigatus adheres to the epithelial surface by using a range of receptors and ECM components, activates different receptors, and modulates cell signaling pathways, culminating in inflammatory responses, in addition to affecting epithelial barrier integrity. However, how the initial response in respiratory epithelial cells against A. fumigatus drives the immune adaptive response and long-term epithelial remodeling events is still unclear [50].
3. Paracoccidioides
Paracoccidioidomycosis (PCM) is the most prevalent systemic mycosis in Latin America [60]. It is estimated that 80% of confirmed PCM cases occur in Brazil [61], but until 2020, this mycosis was not considered a mandatory notifiable disease in this country; thus, the true number of individuals affected by PCM is not known. An increase in PCM microepidemics has also been reported in different regions of Brazil. Environmental factors resulting from the opening of new agricultural frontiers through forest clearing may contribute to the current epidemiological situation of this mycosis [62]. Other activities that disturb the soil, such as the construction of highways, as seen in the state of Rio de Janeiro, Brazil [63], can also cause PCM outbreaks. Clusters of this mycosis may also be associated with climate events, such as El Niño, which provide optimal conditions for fungal growth, enhancing human exposure [64]. PCM has a social impact on areas where this disease is endemic because it frequently affects poor rural workers. PCM impacts these individuals by the chronicity of the disease, the long duration of treatment, and sequelae that lead to low quality of life and inability to work [65].
The etiologic agent of PCM is the thermally dimorphic fungus Paracoccidioides, which comprises the species P. lutzii and P. brasiliensis [66,67]. While P. lutzii mostly occurs in the midwestern and northern regions of Brazil and Ecuador, P. brasiliensis is endemic in all Brazilian regions, Argentina, Paraguay, Uruguay, Peru, Colombia, and Venezuela [61,68]. Recently, by analyzing nuclear and mitochondrial genes, Turissini et al. [69] proposed three new species attributed to the cryptic species of P. brasiliensis PS2, PS3, and PS4 as, respectively, P. americana, P. restrepiensis, and P. venezuelensis [69,70,71].
It is accepted that infection by Paracoccidioides occurs after the inhalation of fungal propagules (mycelium), which are usually present in the soil in rural areas. Once in the host lungs, the mycelium differentiates into yeast. Yeasts may remain in a latent state or trigger the disease [60,70]. The development of PCM is dependent on some characteristics of the host, such as sex, age, and immunological competence, in addition to factors related to the fungus, such as virulence and the ability to modulate the host’s immune system [60]. Some of these characteristics may act as a host protection factor, such as the presence of the female hormone 17-β estradiol, which inhibits the synthesis of proteins involved in the morphological transition from mycelium to yeast, a crucial process for the establishment of the infection, which would explain the prevalence of cases in male patients, even if both sexes are exposed to the same risk factors [72,73,74].
In the last three decades, the interaction and responses of epithelial cells to Paracoccidioides infection have been investigated by some groups. One of the first articles that described the interaction of epithelial cells and Paracoccidioides yeasts was published in 1994 by Mendes Giannini’s group. Despite the use of Vero cells (monkey kidney) in this work (i.e., not from the respiratory tract), the authors demonstrated for the first time that Paracoccidioides yeasts could adhere to these epithelial cells [75]. In the same year, Vicentini et al. [76] indicated that Paracoccidioides yeasts were capable of adhering to another epithelial cell (MDCK, canine kidney), and this adhesion was enhanced when laminin was added to the cultures. Interestingly, these authors also observed that laminin increased the number of granulomas when P. brasiliensis yeasts were inoculated in hamster testicles, suggesting that laminin was important for Paracoccidioides pathogenesis [76]. In fact, following these studies, many Paracoccidioides molecules were proven to interact with several ECM proteins. For example, glycoprotein 43, glyceraldehyde-3-phosphate dehydrogenase, and triosephosphate isomerase of Paracoccidioides yeasts have been described as capable of binding to laminin and fibronectin [76,77,78,79,80,81,82,83,84,85], while the 19 and 32 kDa proteins, present on the fungal surface, also interact with laminin, fibronectin, and fibrinogen [86]. The 14-3-3 protein, which is widely present in the cytoplasm and fungal cell wall, can also adhere to laminin [87]. Assays performed with alveolar epithelial cells indicated that during infection with P. brasiliensis (Pb18 isolate), 14-3-3 protein localized predominantly in the cell wall and antibodies anti-14-3-3 reduced P. brasiliensis adhesion, indicating that this protein participates in fungal interaction with host epithelial cells [87].
Studies comparing distinct species of Paracoccidioides indicated that fungal adhesion to ECM proteins or epithelial cells differed. Oliveira et al. [88] demonstrated that while P. brasiliensis (Pb18 isolate) adhered more to fibronectin than P. lutzii (Pb01 isolate), P. lutzii presented higher adhesion rates to laminin and collagen types I and IV [88]. Even though these authors verified that the adhesion of these two species to epithelial cells was similar, Almeida et al. [89] demonstrated that P. lutzii (Pb01 isolate) adhesion rates were seven times higher than those of P. brasiliensis (Pb18 isolate) and P. americana (Pb03 isolate) [88,89]. Such differences might be explained by the distinct methods used among the laboratories to analyze fungal adhesion.
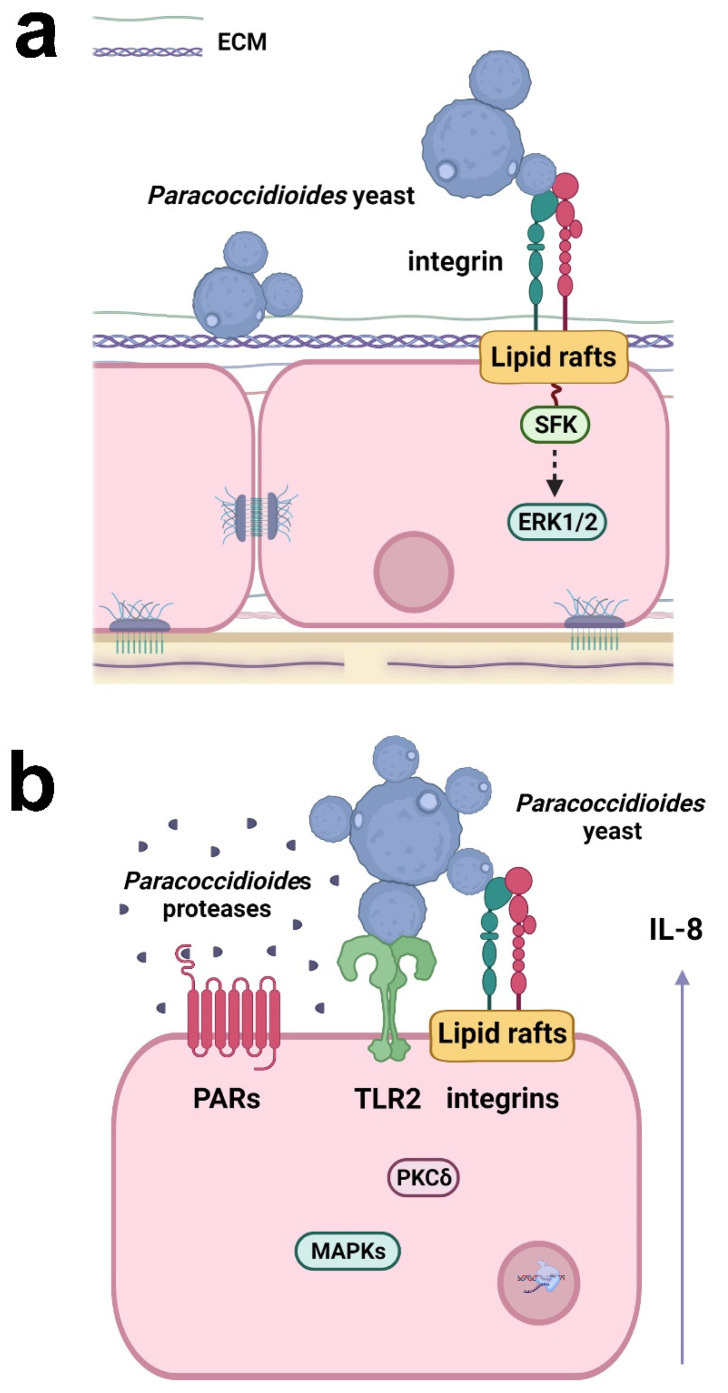
Some studies have demonstrated the ability of P. brasiliensis yeasts to hijack host epithelial cell signaling to establish fungal infection. Maza et al. [90], for example, observed that P. brasiliensis (Pb18 isolate) yeasts promoted clustering of lipid rafts on the surface of alveolar epithelial cells, which is important for fungal adhesion to host cells [90]. Although invasion in epithelial cells is a rare event, Mendes Giannini’s group demonstrated that P. brasiliensis (Pb18 isolate) may also invade Vero cells by inducing cytoskeletal rearrangement in the host cell. The same authors also verified that protein tyrosine kinases (PTKs) are involved in the P. brasiliensis adhesion and invasion of epithelial cells [91]; moreover, this fungus may promote apoptosis in epithelial cells [92].
Recently, Almeida et al. [89] demonstrated that α3 and α5 integrins, which are present on the surface of alveolar epithelial cells, participate in the adhesion of P. lutzii (Pb01 isolate) (Figure 2). In a previous study, the same group verified that the other species of Paracoccidioides, P. brasiliensis (Pb18 isolate), promoted an increase in the levels of these integrins in the alveolar epithelial cell line A549 during the first 5 h of infection, but after 24 h, surprisingly, a decrease of α3 integrin levels was observed, which was dependent on direct contact between fungi and epithelial cells [93], indicating that Paracoccidioides can manipulate host cell receptor levels along with the infection.
Figure 2.
Responses of respiratory epithelial cells to Paracoccidioides infection. (a) Paracoccidioides yeasts can bind to host ECM proteins and α3 and α5 integrins. Fungal adhesion is also dependent on lipid raft clustering, which promotes Src-family kinase (SFK) and ERK1/2 activation. (b) Paracoccidioides induces IL-8 cytokine secretion in epithelial cells by interacting with α3 and α5 integrins and TLR2. Fungal proteases may also activate PAR-1 and PAR-2 in epithelial cells, leading to IL-8 production. The secretion of IL-8 is promoted by Paracoccidioides and is dependent on lipid raft clustering and the activation of MAPK (p38MAPK, ERK1/2) and PKCδ. Created with Biorender.com.
P. brasiliensis (Pb18 isolate) can manipulate epithelial cell signaling pathways to secrete the proinflammatory cytokines IL-6 and IL-8, but not the anti-inflammatory cytokine IL-10 [94,95,96]. The interaction of P. brasiliensis with epithelial cells promotes the activation of protein kinase C (PKC) δ and the MAPKs p38 and extracellular signal-regulated kinase (ERK) 1/2, which are important for the secretion of IL-6 and IL-8 (Figure 2) [94,95]. TLR2, α3 and α5 integrins, and lipid rafts also participate in IL-8 secretion (Figure 2) [93,96]. Moreover, proteases secreted by P. restrepiensis (Pb339 isolate) can also induce cytokine secretion in epithelial cells. Oliveira et al. [97] demonstrated that this fungus secretes serine and cysteine proteases that activate PARs 1 and 2 and then induce IL-6 and IL-8 secretion (Figure 2).
As observed for the adhesion of Paracoccidioides yeasts to alveolar epithelial cells, different species induce distinct cytokine levels in these cells. It was observed that P. brasiliensis (Pb18 isolate) promoted the highest IL-8 level secretion, followed by P. americana (Pb03 isolate) which induced intermediate levels. P. lutzii (Pb01 isolate) promoted the lowest levels of this cytokine. Interestingly, while P. brasiliensis and P. lutzii promoted IL-8 secretion mostly through secreted products, P. americana requires direct contact with the epithelial cell [89], indicating that different species of Paracoccidioides induce distinct responses in these epithelial cells.
4. Conclusions
Respiratory fungal infectious diseases are widespread around the world and contribute to an increase in the mortality rate among human mycoses. In addition, the usual lack of compulsory notification leads to underestimated epidemiological data, affecting the knowledge of the true number of individuals afflicted with respiratory fungal diseases. In this context, studies that aim to understand the mechanisms behind the establishment of respiratory fungal mycoses are indispensable. In the last decades, several research groups have investigated the responses of respiratory epithelial cells to infections by viruses, bacteria, or fungi. These studies have indicated that epithelial cells act not only as a physical barrier but also as sensors of the respiratory environment, cooperating with the modulation of the host immune response. The literature has indicated several mechanisms by which fungi interact with respiratory epithelial cells, e.g., hijacking of host cell signaling pathways, which leads to fungal adhesion, and, depending on the fungal species, an active invasion into these cells. Moreover, during fungal infection, epithelial cells secrete chemokines and cytokines that mediate communication with host immune cells. Despite the recent progress in understanding the cellular mechanisms of this crosstalk between epithelial cells and immune cells, data available in the literature are still scarce and occasionally contradictory. Thus, more studies are necessary to elucidate the signaling pathways that lead to the establishment of infection and inflammatory responses. A promising strategy consists of in vitro cell culture systems (such as air liquid interface, polymer scaffolds, and organoids—see ref. [98] for review) that are more closely related to the in vivo respiratory system, which may help researchers discover new therapeutic approaches for respiratory infectious diseases.
Author Contributions
Writing—original draft preparation, E.S., B.C.S.C.B., B.R.A. and D.T.L.B.; writing—review, E.S. and M.S.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), grant number 2019/26693-9 (E.S.); Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), 170209/2018-0 (B.R.A.); and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), 88887.670584/2022-00 (D.T.L.B.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hewitt R.J., Lloyd C.M. Regulation of immune responses by the airway epithelial cell landscape. Nat. Rev. Immunol. 2021;21:347–362. doi: 10.1038/s41577-020-00477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis J.D., Wypych T.P. Cellular and functional heterogeneity of the airway eithelium. Mucosal Immunol. 2021;14:978–990. doi: 10.1038/s41385-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leiva-Juárez M.M., Kolls J.K., Evans S.E. Lung epithelial cells: Therapeutically inducible effectors of antimicrobial defense. Mucosal Immunol. 2018;11:21–34. doi: 10.1038/mi.2017.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Waal A.M., Hiemstra P.S., Ottenhoff T.H., Joosten S.A., van der Does A.M. Lung epithelial cells interact with immune cells and bacteria to shape the microenvironment in Tuberculosis. Thorax. 2022;77:408–416. doi: 10.1136/thoraxjnl-2021-217997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fromentin M., Ricard J.-D., Roux D. Lung microbiome in critically ill patients. Life. 2021;12:7. doi: 10.3390/life12010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLean A.E.B., Kao S.C., Barnes D.J., Wong K.K.H., Scolyer R.A., Cooper W.A., Kohonen-Corish M.R.J. The emerging role of the lung microbiome and its importance in non-small cell lung cancer diagnosis and treatment. Lung Cancer. 2022;165:124–132. doi: 10.1016/j.lungcan.2022.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Invernizzi R., Lloyd C.M., Molyneaux P.L. Respiratory microbiome and epithelial interactions shape immunity in the lungs. Immunology. 2020;160:171–182. doi: 10.1111/imm.13195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gow N.A.R., Latge J.-P., Munro C.A. The fungal cell wall: Structure, biosynthesis, and function. Microbiol. Spectr. 2017;5:FUNK-0035-2016. doi: 10.1128/microbiolspec.FUNK-0035-2016. [DOI] [PubMed] [Google Scholar]
- 9.Gaffi. [(accessed on 25 March 2022)]. Available online: https://gaffi.org/
- 10.Miller A.S., Wilmott R.W. 31—The pulmonary mycoses. In: Wilmott R.W., Deterding R., Li A., Ratjen F., Sly P., Zar H.J., Bush A., editors. Kendig’s Disorders of the Respiratory Tract in Children. 9th ed. Elsevier; Philadelphia, PA, USA: 2019. pp. 507–527.e3. [Google Scholar]
- 11.Salzer H.J.F., Burchard G., Cornely O.A., Lange C., Rolling T., Schmiedel S., Libman M., Capone D., Le T., Dalcolmo M.P., et al. Diagnosis and management of systemic endemic mycoses causing pulmonary disease. Respiration. 2018;96:283–301. doi: 10.1159/000489501. [DOI] [PubMed] [Google Scholar]
- 12.Koehler P., Bassetti M., Chakrabarti A., Chen S.C.A., Colombo A.L., Hoenigl M., Klimko N., Lass-Flörl C., Oladele R.O., Vinh D.C., et al. Defining and managing COVID-19-associated pulmonary Aspergillosis: The 2020 ECMM/ISHAM Consensus criteria for research and clinical guidance. Lancet Infect. Dis. 2021;21:e149–e162. doi: 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griffiths J., Lopes Colombo A., Denning D.W. The case for Paracoccidioidomycosis to be accepted as a neglected tropical (fungal) disease. PLoS Negl. Trop. Dis. 2019;13:e0007195. doi: 10.1371/journal.pntd.0007195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ben-Ghazzi N., Moreno-Velásquez S., Seidel C., Thomson D., Denning D.W., Read N.D., Bowyer P., Gago S. Characterisation of Aspergillus fumigatus endocytic trafficking within airway epithelial cells using high-resolution automated Quantitative confocal microscopy. J. Fungi. 2021;7:454. doi: 10.3390/jof7060454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latgé J.-P., Chamilos G. Aspergillus fumigatus and Aspergillosis in 2019. Clin. Microbiol. Rev. 2019;33:e00140-18. doi: 10.1128/CMR.00140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janssen N.A.F., Nyga R., Vanderbeke L., Jacobs C., Ergün M., Buil J.B., van Dijk K., Altenburg J., Bouman C.S.C., van der Spoel H.I., et al. Multinational observational cohort study of COVID-19–associated pulmonary Aspergillosis. Emerg. Infect. Dis. 2021;27:2892–2898. doi: 10.3201/eid2711.211174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campione E., Gaziano R., Doldo E., Marino D., Falconi M., Iacovelli F., Tagliaferri D., Pacello L., Bianchi L., Lanna C., et al. Antifungal effect of all-trans retinoic acid against Aspergillus fumigatus in vitro and in a pulmonary Aspergillosis in vivo Model. Antimicrob. Agents Chemother. 2021;65:e01874-20. doi: 10.1128/AAC.01874-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cosio T., Gaziano R., Zuccari G., Costanza G., Grelli S., Di Francesco P., Bianchi L., Campione E. Retinoids in fungal infections: From bench to bedside. Pharmaceuticals. 2021;14:962. doi: 10.3390/ph14100962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ammendolia D.A., Bement W.M., Brumell J.H. Plasma membrane integrity: Implications for health and disease. BMC Biol. 2021;19:71. doi: 10.1186/s12915-021-00972-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeHart D.J., Agwu D.E., Julian N.C., Washburn R.G. Binding and germination of Aspergillus fumigatus conidia on cultured A549 Pneumocytes. J. Infect. Dis. 1997;175:146–150. doi: 10.1093/infdis/175.1.146. [DOI] [PubMed] [Google Scholar]
- 21.Fernandes J., Hamidi F., Leborgne R., Beau R., Castier Y., Mordant P., Boukkerou A., Latgé J.P., Pretolani M. Penetration of the human pulmonary epithelium by Aspergillus fumigatus hyphae. J. Infect. Dis. 2018;218:1306–1313. doi: 10.1093/infdis/jiy298. [DOI] [PubMed] [Google Scholar]
- 22.Croft C.A., Culibrk L., Moore M.M., Tebbutt S.J. Interactions of Aspergillus fumigatus conidia with airway epithelial cells: A critical review. Front. Microbiol. 2016;7:472. doi: 10.3389/fmicb.2016.00472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kerr S.C., Fischer G.J., Sinha M., McCabe O., Palmer J.M., Choera T., Lim F.Y., Wimmerova M., Carrington S.D., Yuan S., et al. FleA Expression in Aspergillus fumigatus is recognized by fucosylated structures on mucins and macrophages to prevent lung infection. PLoS Pathog. 2016;12:e1005555. doi: 10.1371/journal.ppat.1005555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yan T., Han J., Yu X. E-cadherin mediates adhesion of Aspergillus fumigatus to non-small cell lung cancer cells. Tumour Biol. 2016;37:15593–15599. doi: 10.1007/s13277-015-4195-3. [DOI] [PubMed] [Google Scholar]
- 25.Gravelat F.N., Beauvais A., Liu H., Lee M.J., Snarr B.D., Chen D., Xu W., Kravtsov I., Hoareau C.M.Q., Vanier G., et al. Aspergillus galactosaminogalactan mediates adherence to host constituents and conceals hyphal β-glucan from the immune system. PLoS Pathog. 2013;9:e1003575. doi: 10.1371/journal.ppat.1003575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouchara J.P., Sanchez M., Chevailler A., Marot-Leblond A., Lissitzky J.C., Tronchin G., Chabasse D. Sialic acid-dependent recognition of laminin and fibrinogen by Aspergillus fumigatus conidia. Infect. Immun. 1997;65:2717–2724. doi: 10.1128/iai.65.7.2717-2724.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Warwas M.L., Watson J.N., Bennet A.J., Moore M.M. Structure and role of sialic acids on the surface of Aspergillus fumigatus conidiospores. Glycobiology. 2007;17:401–410. doi: 10.1093/glycob/cwl085. [DOI] [PubMed] [Google Scholar]
- 28.Liu H., Lee M.J., Solis N.V., Phan Q.T., Swidergall M., Ralph B., Ibrahim A.S., Sheppard D.C., Filler S.G. Aspergillus fumigatus CalA binds to integrin α5β1 and mediates host cell invasion. Nat. Microbiol. 2016;2:16211. doi: 10.1038/nmicrobiol.2016.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Culibrk L., Croft C.A., Toor A., Yang S.J., Singhera G.K., Dorscheid D.R., Moore M.M., Tebbutt S.J. Phagocytosis of Aspergillus fumigatus by human bronchial epithelial cells is mediated by the Arp2/3 complex and WIPF2. Front. Cell. Infect. Microbiol. 2019;9:16. doi: 10.3389/fcimb.2019.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bertuzzi M., Hayes G., Icheoku U., van Rhijn N., Denning D., Osherov N., Bignell E. Anti-Aspergillus activities of the respiratory epithelium in health and disease. J. Fungi. 2018;4:8. doi: 10.3390/jof4010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shlezinger N., Hohl T.M. Mitochondrial reactive oxygen species enhance alveolar macrophage activity against Aspergillus fumigatus but are dispensable for host protection. mSphere. 2021;6:e0026021. doi: 10.1128/mSphere.00260-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feldman M.B., Dutko R.A., Wood M.A., Ward R.A., Leung H.M., Snow R.F., De La Flor D.J., Yonker L.M., Reedy J.L., Tearney G.J., et al. Aspergillus fumigatus cell wall promotes apical airway epithelial recruitment of human neutrophils. Infect. Immun. 2020;88:e00813-19. doi: 10.1128/IAI.00813-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheng R., Zhong X., Yang Z., Wang X. The role of CARD9 deficiency in neutrophils. Mediat. Inflamm. 2021:6643603. doi: 10.1155/2021/6643603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jepsen C.S., Dubey L.K., Colmorten K.B., Moeller J.B., Hammond M.A., Nielsen O., Schlosser A., Templeton S.P., Sorensen G.L., Holmskov U. FIBCD1 binds Aspergillus fumigatus and regulates lung epithelial response to cell wall components. Front. Immunol. 2018;9:1967. doi: 10.3389/fimmu.2018.01967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schalper K.A., Carleton M., Zhou M., Chen T., Feng Y., Huang S.-P., Walsh A.M., Baxi V., Pandya D., Baradet T., et al. Elevated serum interleukin-8 is associated with enhanced intratumor neutrophils and reduced clinical benefit of immune-checkpoint inhibitors. Nat. Med. 2020;26:688–692. doi: 10.1038/s41591-020-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Z., Lu G., Meng G. Pathogenic fungal infection in the lung. Front. Immunol. 2019;10:1524. doi: 10.3389/fimmu.2019.01524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Y., Li Z., Wang S., Zhang C., Han L., Sun Q., Han X. Aspergillus fumigatus induces the release of IL-8 and MCP-1 by activating nuclear transcription through Dectin-1 and CR3 receptors in alveolar epithelial cells. Curr. Microbiol. 2021;78:3474–3482. doi: 10.1007/s00284-021-02534-5. [DOI] [PubMed] [Google Scholar]
- 38.Chen F., Zhang C., Jia X., Wang S., Wang J., Chen Y., Zhao J., Tian S., Han X., Han L. Transcriptome profiles of human lung epithelial cells A549 interacting with Aspergillus fumigatus by RNA-Seq. PLoS ONE. 2015;10:e0135720. doi: 10.1371/journal.pone.0135720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oya E., Becher R., Ekeren L., Afanou A.K.J., Ovrevik J., Holme J.A. Pro-inflammatory responses in human bronchial epithelial cells induced by spores and hyphal fragments of common damp indoor molds. Int. J. Environ. Res. Public Health. 2019;16:1085. doi: 10.3390/ijerph16061085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun W.-K., Lu X., Li X., Sun Q.-Y., Su X., Song Y., Sun H.-M., Shi Y. Dectin-1 is Inducible and plays a crucial role in Aspergillus-induced innate immune responses in human bronchial epithelial cells. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:2755–2764. doi: 10.1007/s10096-012-1624-8. [DOI] [PubMed] [Google Scholar]
- 41.Balloy V., Sallenave J.-M., Wu Y., Touqui L., Latgé J.-P., Si-Tahar M., Chignard M. Aspergillus fumigatus-induced interleukin-8 synthesis by respiratory epithelial cells is controlled by the phosphatidylinositol 3-kinase, P38 MAPK, and ERK1/2 pathways and not by the toll-like receptor-MyD88 pathway. J. Biol. Chem. 2008;283:30513–30521. doi: 10.1074/jbc.M803149200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oosthuizen J.L., Gomez P., Ruan J., Hackett T.L., Moore M.M., Knight D.A., Tebbutt S.J. Dual organism transcriptomics of airway epithelial cells interacting with conidia of Aspergillus fumigatus. PLoS ONE. 2011;6:e20527. doi: 10.1371/journal.pone.0020527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bellanger A.-P., Millon L., Khoufache K., Rivollet D., Bièche I., Laurendeau I., Vidaud M., Botterel F., Bretagne S. Aspergillus fumigatus germ tube growth and not conidia ingestion induces expression of inflammatory mediator genes in the human lung epithelial cell line A549. J. Med. Microbiol. 2009;58:174–179. doi: 10.1099/jmm.0.005488-0. [DOI] [PubMed] [Google Scholar]
- 44.Rowley J., Namvar S., Gago S., Labram B., Bowyer P., Richardson M.D., Herrick S.E. Differential proinflammatory responses to Aspergillus fumigatus by airway epithelial cells in vitro are protease dependent. J. Fungi. 2021;7:468. doi: 10.3390/jof7060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Espinosa V., Rivera A. First line of defense: Innate cell-mediated control of pulmonary Aspergillosis. Front. Microbiol. 2016;7:272. doi: 10.3389/fmicb.2016.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garth J.M., Steele C. Innate lung defense during invasive Aspergillosis: New mechanisms. J. Innate Immun. 2017;9:271–280. doi: 10.1159/000455125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jensen K., Lund K.P., Christensen K.B., Holm A.T., Dubey L.K., Moeller J.B., Jepsen C.S., Schlosser A., Galgóczy L., Thiel S., et al. M-ficolin is present in Aspergillus fumigatus infected lung and modulates epithelial cell immune responses elicited by fungal cell wall polysaccharides. Virulence. 2017;8:1870–1879. doi: 10.1080/21505594.2016.1278337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bidula S., Sexton D.W., Yates M., Abdolrasouli A., Shah A., Wallis R., Reed A., Armstrong-James D., Schelenz S. H-ficolin binds Aspergillus fumigatus leading to activation of the lectin complement pathway and modulation of lung epithelial immune responses. Immunology. 2015;146:281–291. doi: 10.1111/imm.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim Y.H., Lee S.-H. TGF-β/SMAD4 mediated ucp2 downregulation contributes to Aspergillus protease-induced inflammation in primary bronchial epithelial cells. Redox Biol. 2018;18:104–113. doi: 10.1016/j.redox.2018.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Namvar S., Labram B., Rowley J., Herrick S. Aspergillus fumigatus—Host interactions mediating airway wall remodelling in asthma. J. Fungi. 2022;8:159. doi: 10.3390/jof8020159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Namvar S., Warn P., Farnell E., Bromley M., Fraczek M., Bowyer P., Herrick S. Aspergillus fumigatus proteases, Asp f 5 and Asp f 13, are essential for airway inflammation and remodelling in a murine inhalation model. Clin. Exp. Allergy. 2015;45:982–993. doi: 10.1111/cea.12426. [DOI] [PubMed] [Google Scholar]
- 52.Shen H.D., Lin W.L., Tam M.F., Chou H., Wang C.W., Tsai J.J., Wang S.R., Han S.H. Identification of vacuolar serine proteinase as a major allergen of Aspergillus fumigatus by immunoblotting and N-Terminal amino acid sequence analysis. Clin. Exp. Allergy. 2001;31:295–302. doi: 10.1046/j.1365-2222.2001.01026.x. [DOI] [PubMed] [Google Scholar]
- 53.Deckers J., De Bosscher K., Lambrecht B.N., Hammad H. Interplay between barrier epithelial cells and dendritic cells in allergic sensitization through the lung and the skin. Immunol. Rev. 2017;278:131–144. doi: 10.1111/imr.12542. [DOI] [PubMed] [Google Scholar]
- 54.Dietz C.J., Sun H., Yao W.C., Citardi M.J., Corry D.B., Luong A.U. Aspergillus fumigatus induction of IL-33 expression in chronic rhinosinusitis is PAR2-dependent. Laryngoscope. 2019;129:2230–2235. doi: 10.1002/lary.28000. [DOI] [PubMed] [Google Scholar]
- 55.Liebana-Jordan M., Brotons B., Falcon-Perez J.M., Gonzalez E. Extracellular vesicles in the fungi kingdom. Int. J. Mol. Sci. 2021;22:7221. doi: 10.3390/ijms22137221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rizzo J., Rodrigues M.L., Janbon G. Extracellular vesicles in fungi: Past, present, and future perspectives. Front. Cell. Infect. Microbiol. 2020;10:346. doi: 10.3389/fcimb.2020.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Makarova M., May R.C. Fungal extracellular vesicles in interkingdom communication. Curr. Top. Microbiol. Immunol. 2021;432:81–88. doi: 10.1007/978-3-030-83391-6_8. [DOI] [PubMed] [Google Scholar]
- 58.Brauer V.S., Pessoni A.M., Bitencourt T.A., de Paula R.G., de Oliveira Rocha L., Goldman G.H., Almeida F. Extracellular vesicles from Aspergillus flavus induce M1 polarization in vitro. mSphere. 2020;5:e00190-20. doi: 10.1128/mSphere.00190-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Souza J.A.M., Baltazar L.D.M., Carregal V.M., Gouveia-Eufrasio L., de Oliveira A.G., Dias W.G., Campos Rocha M., Rocha de Miranda K., Malavazi I., Santos D.D.A., et al. Characterization of Aspergillus fumigatus extracellular vesicles and their effects on macrophages and neutrophils functions. Front. Microbiol. 2019;10:2008. doi: 10.3389/fmicb.2019.02008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shikanai-Yasuda M.A., Mendes R.P., Colombo A.L., Queiroz-Telles F.D., Kono A.S.G., Paniago A.M.M., Nathan A., Valle A.C.F.D., Bagagli E., Benard G., et al. Brazilian guidelines for the clinical management of Paracoccidioidomycosis. Rev. Soc. Bras. Med. Trop. 2017;50:715–740. doi: 10.1590/0037-8682-0230-2017. [DOI] [PubMed] [Google Scholar]
- 61.Martinez R. New trends in Paracoccidioidomycosis epidemiology. J. Fungi. 2017;3:1. doi: 10.3390/jof3010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Millington M.A., Nishioka S.D.A., Martins S.T., Dos Santos Z.M.G., de Lima Júnior F.E.F., Alves R.V. Paracoccidioidomycosis: Historical approach and perspectives for implementation of surveillance and control. Epidemiol. Serv. Saude. 2018;27:e0500002. doi: 10.5123/S1679-49742018000500002. [DOI] [PubMed] [Google Scholar]
- 63.do Valle A.C.F., Marques de Macedo P., Almeida-Paes R., Romão A.R., dos Santos Lazéra M., Wanke B. Paracoccidioidomycosis after highway construction, Rio de Janeiro, Brazil. Emerg. Infect. Dis. 2017;23:1917–1919. doi: 10.3201/eid2311.170934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barrozo L.V., Benard G., Silva M.E.S., Bagagli E., Marques S.A., Mendes R.P. First Description of a cluster of acute/subacute Paracoccidioidomycosis cases and its association with a climatic anomaly. PLoS Negl. Trop. Dis. 2010;4:e643. doi: 10.1371/journal.pntd.0000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martinez R. Epidemiology of Paracoccidioidomycosis. Rev. Inst. Med. Trop. Sao Paulo. 2015;57((Suppl. 19)):11–20. doi: 10.1590/S0036-46652015000700004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Teixeira M.D.M., Theodoro R.C., Oliveira F.F.M.D., Machado G.C., Hahn R.C., Bagagli E., San-Blas G., Soares Felipe M.S. Paracoccidioides lutzii Sp. Nov.: Biological and clinical implications. Med. Mycol. 2014;52:19–28. doi: 10.3109/13693786.2013.794311. [DOI] [PubMed] [Google Scholar]
- 67.Bocca A.L., Amaral A.C., Teixeira M.M., Sato P.K., Shikanai-Yasuda M.A., Soares Felipe M.S. Paracoccidioidomycosis: Eco-Epidemiology, taxonomy and clinical and therapeutic issues. Future Microbiol. 2013;8:1177–1191. doi: 10.2217/fmb.13.68. [DOI] [PubMed] [Google Scholar]
- 68.Theodoro R.C., de Melo Teixeira M., Felipe M.S.S., dos Santos Paduan K., Ribolla P.M., San-Blas G., Bagagli E. Genus Paracoccidioides: Species recognition and biogeographic aspects. PLoS ONE. 2012;7:e37694. doi: 10.1371/journal.pone.0037694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Turissini D.A., Gomez O.M., Teixeira M.M., McEwen J.G., Matute D.R. Species boundaries in the human pathogen Paracoccidioides. Fungal Genet. Biol. 2017;106:9–25. doi: 10.1016/j.fgb.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Matute D.R., McEwen J.G., Puccia R., Montes B.A., San-Blas G., Bagagli E., Rauscher J.T., Restrepo A., Morais F., Niño-Vega G., et al. Cryptic speciation and recombination in the fungus Paracoccidioides brasiliensis as revealed by gene genealogies. Mol. Biol. Evol. 2006;23:65–73. doi: 10.1093/molbev/msj008. [DOI] [PubMed] [Google Scholar]
- 71.Mattos K., Cocio T.A., Chaves E.G.A., Borges C.L., Venturini J., de Carvalho L.R., Mendes R.P., Paniago A.M.M., Weber S.S. An Update on the occurrence of Paracoccidioides species in the midwest region, Brazil: Molecular epidemiology, clinical aspects and serological profile of patients from Mato Grosso Do Sul state. PLoS Negl. Trop. Dis. 2021;15:e0009317. doi: 10.1371/journal.pntd.0009317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Salazar M.E., Restrepo A., Stevens D.A. Inhibition by Estrogens of conidium-to-yeast conversion in the fungus Paracoccidioides brasiliensis. Infect. Immun. 1988;56:711–713. doi: 10.1128/iai.56.3.711-713.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Restrepo A., Salazar M.E., Cano L.E., Stover E.P., Feldman D., Stevens D.A. Estrogens inhibit mycelium-to-yeast transformation in the fungus Paracoccidioides brasiliensis: Implications for resistance of females to Paracoccidioidomycosis. Infect. Immun. 1984;46:346–353. doi: 10.1128/iai.46.2.346-353.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aristizábal B.H., Clemons K.V., Cock A.M., Restrepo A., Stevens D.A. Experimental paracoccidioides brasiliensis Infection in mice: Influence of the hormonal status of the host on tissue responses. Med. Mycol. 2002;40:169–178. doi: 10.1080/mmy.40.2.169.178. [DOI] [PubMed] [Google Scholar]
- 75.Mendes-Giannini M.J., Ricci L.C., Uemura M.A., Toscano E., Arns C.W. Infection and apparent invasion of vero cells by Paracoccidioides brasiliensis. J. Med. Vet. Mycol. 1994;32:189–197. doi: 10.1080/02681219480000251. [DOI] [PubMed] [Google Scholar]
- 76.Vicentini A.P., Gesztesi J.L., Franco M.F., de Souza W., de Moraes J.Z., Travassos L.R., Lopes J.D. Binding of Paracoccidioides brasiliensis to laminin through surface glycoprotein gp43 leads to enhancement of fungal pathogenesis. Infect. Immun. 1994;62:1465–1469. doi: 10.1128/iai.62.4.1465-1469.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.da Silva Neto B.R., de Fátima da Silva J., Mendes-Giannini M.J.S., Lenzi H.L., de Almeida Soares C.M., Pereira M. The Malate Synthase of Paracoccidioides brasiliensisis a linked surface protein that behaves as an anchorless adhesin. BMC Microbiol. 2009;9:1–12. doi: 10.1186/1471-2180-9-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Andreotti P.F., Monteiro da Silva J.L., Bailão A.M., de Almeida Soares C.M., Benard G., Soares C.P., Mendes-Giannini M.J.S. Isolation and partial characterization of a 30 KDa adhesin from Paracoccidioides brasiliensis. Microbes Infect. 2005;7:875–881. doi: 10.1016/j.micinf.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 79.Barbosa M.S., Báo S.N., Andreotti P.F., de Faria F.P., Felipe M.S.S., dos Santos Feitosa L., Mendes-Giannini M.J.S., de Almeida Soares C.M. Glyceraldehyde-3-phosphate dehydrogenase of Paracoccidioides brasiliensis is a cell surface protein involved in fungal adhesion to extracellular matrix proteins and interaction with cells. Infect. Immun. 2006;74:382–389. doi: 10.1128/IAI.74.1.382-389.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lopes J.D., Moura-Campos M.C., Vicentini A.P., Gesztesi J.L., de-Souza W., Camargo Z.P. Characterization of glycoprotein Gp43, the major laminin-binding protein of Paracoccidioides brasiliensis. Braz. J. Med. Biol. Res. 1994;27:2309–2313. [PubMed] [Google Scholar]
- 81.Pereira L.A., Báo S.N., Barbosa M.S., da Silva J.L.M., Felipe M.S.S., de Santana J.M., Mendes-Giannini M.J.S., de Almeida Soares C.M. Analysis of the Paracoccidioides brasiliensis triosephosphate isomerase suggests the potential for adhesin function. FEMS Yeast Res. 2007;7:1381–1388. doi: 10.1111/j.1567-1364.2007.00292.x. [DOI] [PubMed] [Google Scholar]
- 82.Mendes-Giannini M.J.S., Andreotti P.F., Vincenzi L.R., da Silva J.L.M., Lenzi H.L., Benard G., Zancopé-Oliveira R., de Matos Guedes H.L., Soares C.P. Binding of extracellular matrix proteins to Paracoccidioides brasiliensis. Microbes Infect. 2006;8:1550–1559. doi: 10.1016/j.micinf.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 83.Gesztesi J.L., Puccia R., Travassos L.R., Vicentini A.P., de Moraes J.Z., Franco M.F., Lopes J.D. Monoclonal antibodies against the 43,000 Da glycoprotein from Paracoccidioides brasiliensis modulate laminin-mediated fungal adhesion to epithelial cells and pathogenesis. Hybridoma. 1996;15:415–422. doi: 10.1089/hyb.1996.15.415. [DOI] [PubMed] [Google Scholar]
- 84.Vicentini A.P., Moraes J.Z., Gesztesi J.L., Franco M.F., de Souza W., Lopes J.D. Laminin-binding epitope on Gp43 from Paracoccidioides brasiliensis is recognized by a monoclonal antibody raised against Staphylococcus aureus laminin receptor. J. Med. Vet. Mycol. 1997;35:37–43. doi: 10.1080/02681219780000851. [DOI] [PubMed] [Google Scholar]
- 85.Ywazaki C.Y., Maza P.K., Suzuki E., Takahashi H.K., Straus A.H. Role of host glycosphingolipids on Paracoccidioides brasiliensis adhesion. Mycopathologia. 2011;171:325–332. doi: 10.1007/s11046-010-9376-4. [DOI] [PubMed] [Google Scholar]
- 86.Gonzalez A., Gomez B.L., Restrepo A., Hamilton A.J., Cano L.E. Recognition of extracellular matrix proteins by Paracoccidioides brasiliensis yeast cells. Med. Mycol. 2005;43:637–645. doi: 10.1080/13693780500064599. [DOI] [PubMed] [Google Scholar]
- 87.da Silva J.D.F., de Oliveira H.C., Marcos C.M., da Silva R.A.M., da Costa T.A., Calich V.L.G., Almeida A.M.F., Mendes-Giannini M.J.S. Paracoccidoides brasiliensis 30 KDa adhesin: Identification as a 14-3-3 protein, cloning and subcellular localization in infection models. PLoS ONE. 2013;8:e62533. doi: 10.1371/journal.pone.0062533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.de Oliveira H.C., da Silva J.D.F., Scorzoni L., Marcos C.M., Rossi S.A., de Paula E Silva A.C.A., Assato P.A., da Silva R.A.M., Fusco-Almeida A.M., Mendes-Giannini M.J.S. Importance of adhesins in virulence of Paracoccidioides spp. Front. Microbiol. 2015;6:303. doi: 10.3389/fmicb.2015.00303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Almeida B.R., Barros B.C.S., Araújo A.C.L., Alcantara C., Suzuki E. Paracoccidioides Species present distinct fungal adherence to epithelial lung cells and promote different IL-8 secretion levels. Med. Microbiol Immunol. 2020;209:59–67. doi: 10.1007/s00430-019-00639-0. [DOI] [PubMed] [Google Scholar]
- 90.Maza P.K., Straus A.H., Toledo M.S., Takahashi H.K., Suzuki E. Interaction of epithelial cell membrane rafts with Paracoccidioides brasiliensis leads to fungal adhesion and Src-family kinase activation. Microbes Infect. 2008;10:540–547. doi: 10.1016/j.micinf.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 91.Monteiro da Silva J.L., Andreotti P.F., Benard G., Soares C.P., Miranda E.T., Mendes-Giannini M.J.S. Epithelial cells treated with genistein inhibit adhesion and endocytosis of Paracoccidioides brasiliensis. Antonie Van Leeuwenhoek. 2007;92:129–135. doi: 10.1007/s10482-006-9129-z. [DOI] [PubMed] [Google Scholar]
- 92.Del Vecchio A., Silva J.D.F.D., Silva J.L.M.D., Andreotti P.F., Soares C.P., Benard G., Giannini M.J.S.M. Induction of apoptosis in A549 pulmonary cells by two Paracoccidioides brasiliensis samples. Mem. Inst. Oswaldo Cruz. 2009;104:749–754. doi: 10.1590/S0074-02762009000500015. [DOI] [PubMed] [Google Scholar]
- 93.de Barros B.C.S.C., Almeida B.R., Suzuki E. Paracoccidioides brasiliensis downmodulates α3 integrin levels in human lung epithelial cells in a TLR2-dependent manner. Sci. Rep. 2020;10:1–9. doi: 10.1038/s41598-020-76557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maza P.K., Oliveira P., Toledo M.S., Paula D.M.B., Takahashi H.K., Straus A.H., Suzuki E. Paracoccidioides brasiliensis induces secretion of IL-6 and IL-8 by lung epithelial cells. modulation of host cytokine levels by fungal proteases. Microbes Infect. 2012;14:1077–1085. doi: 10.1016/j.micinf.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 95.Alcantara C., Maza P.K., Barros B.C.S.C., Suzuki E. Role of protein kinase c in cytokine secretion by lung epithelial cells during infection with Paracoccidioides brasiliensis. Pathog. Dis. 2015;73:ftv045. doi: 10.1093/femspd/ftv045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Barros B.C.S.C., Maza P.K., Alcantara C., Suzuki E. Paracoccidioides brasiliensis Induces recruitment of α3 and α5 integrins into epithelial cell membrane rafts, leading to cytokine secretion. Microbes Infect. 2016;18:68–77. doi: 10.1016/j.micinf.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 97.de Oliveira P., Juliano M.A., Tanaka A.S., Carmona A.K., Dos Santos S.M.B., de Barros B.C.S.C., Maza P.K., Puccia R., Suzuki E. Paracoccidioides brasiliensis induces cytokine secretion in epithelial cells in a protease-activated receptor-dependent (PAR) manner. Med. Microbiol. Immunol. 2017;206:149–156. doi: 10.1007/s00430-016-0490-x. [DOI] [PubMed] [Google Scholar]
- 98.Barron S.L., Saez J., Owens R.M. In vitro models for studying respiratory host-pathogen interactions. Adv. Biol. 2021;5:e2000624. doi: 10.1002/adbi.202000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.