ABSTRACT
Background
This study was conducted to characterize the long-term effect of mobile-based education on Chinese female freshmen and disclose the possible predictors of their willingness to get vaccinated based on the information-motivation-behavioral skills (IMB) model.
Methods
We randomly assigned 509 participants to a 7-day mobile-based educational intervention or control group and collected information about general information, health, and sexual behavior, HPV vaccination intention and action, HPV-related knowledge, cognition, and behavioral skill by an online self-administrated questionnaire at baseline, post-intervention, and at the 1-month and 3-month follow-ups.
Results
The intervention arm showed an improvement in IMB scores after education. Despite the persistent improvement in knowledge, the improvement in their motivation and behavioral skills decreased at the 1-month and 3-month follow-ups. Participants’ vaccination willingness was elevated after the baseline survey in both the intervention and control groups, while the overall appointment/vaccination rate was only 3.73% 3 months later. The intention to get vaccinated was associated with knowing HPV (adjusted OR: 2.37, 95% CI: 1.44 – 3.89), perceiving more barriers (adjusted OR: 2.16, 95% CI: 1.44 – 3.25), higher subjective norms (adjusted OR: 2.05, 95% CI: 1.26 – 3.32), and having more behavioral skills (adjusted OR: 2.95, 95% CI: 1.79 – 4.87).
Conclusion
Seven-day mobile-based education was effective to increase IMB model scores among female freshmen. However, the improvement in motivation and behavioral skills was not persistent. Information, perceived barriers, subjective norms, and behavioral skills were discovered to be influencing factors of vaccination intention. Future research with longer, more convenient, and more tailored education to the main influencing factors is warranted.
KEYWORDS: HPV vaccine, IMB, mobile-based education, long-term effect, vaccination willingness, Chinese female freshmen
Introduction
As the fourth most common cancer and the fourth leading cause of cancer death in women,1 cervical cancer is a major worldwide health problem. The estimated new cases and deaths of cervical cancer worldwide increased from 528,000 and 266,000 in 2012 to 604,000 and 342,000 in 2020, respectively.1–4 Meanwhile, the number of cervical cancer cases in China was the highest in the world (106,000),2 and the age-standardized rates of cancer incidence (ASIR) of cervical cancer in China increased from 5.86/100,000 in 1998 to 7.28/100,000 in 2012.5 Fortunately, cervical cancer is preventable, as almost all cervical cancers are caused by carcinogenic human papillomavirus (HPV) infection.6 Thus, the prophylactic HPV vaccine effectively prevents HPV infection and reduces the mortality of cervical cancer.6
The HPV vaccine has been introduced to more than 111 member states of the World Health Organization (WHO), and 106 countries have included HPV vaccines in their national immunization programs (as of 12 February 2020).7–9 Although the safety and efficacy of the HPV vaccine have been widely proven worldwide,6,10–13 vaccination coverage has remained low among the ideal target population since its approval in mainland China in 2016.14–17
Previous studies have found several reasons for such a low vaccination rate and willingness, including concerns about the safety, efficacy, and side effects of HPV vaccines, conservative sexual attitudes and no sexual activity, a lack of knowledge, low perceived susceptibility, and the unaffordable cost of the vaccine.8,17–19 Female college students are one of the sexually active and HPV susceptible groups, and thus one of the main target population of HPV vaccination in China. Besides, studies found that HPV vaccination was cost-effective until the age of 24–26.20 Hence, it is important to improve female college students’ vaccination willingness and rate through a comprehensive analysis of the determinants of vaccination willingness and appropriate intervention.
Nowadays, numerous studies applied the information-motivation-behavioral skills (IMB) model to promote health behaviors like diabetes self-management,21–23 HIV prevention,24,25 and HPV uptake.26 The IMB model emphasizes that information is not the only thing that individuals need to be equipped with to adopt a health behavior. Well-informed individuals require adequate motivation and appropriate behavioral skills to overcome all kinds of difficulties and persist in health habits.26,27 Therefore, our study aims to detect the long-term impact of mobile phone-based education on Chinese female freshmen and analyze the predictors of willingness based on IMB model.
Methods
Study design and population
This was a randomized control trial conducted at Shanxi University of Finance and Economics in China, which involved a 7-day mobile phone-based educational intervention with the 1-month and 3-month follow-ups. Female college students from either literature or science majors were recruited in April 2020 using convenience sampling. Female freshmen over 18 years old who had not been vaccinated against HPV with no contraindications to vaccination were invited to participate in the study. Students who met the inclusion criteria were stratified according to majors and then randomly assigned to the intervention group or control group in a 1:1 ratio. Thus, we balanced intervention and control groups on the baseline characteristics. The random sequence was generated by SAS V.12. (SAS Institute) software. This study was approved by the Institutional Review Board of the Chinese Center for Disease Control and Prevention. All subjects were informed of the purposes, expected risks, and benefits and signed the informed consent before the study implementation.
Data collection and outcome measurement
An online anonymous self-administered baseline questionnaire was designed to collect data, including general information, health and sexual behavior, HPV vaccination intention, HPV-related knowledge, cognition involving perceived severity, perceived susceptibility, perceived benefits, and perceived obstacles, social norms, and behavioral skills involving self-decision making, self-efficacy, and objective skills. The post-education questionnaire was the same as the baseline questionnaire except for socio-demographic characteristics and health-related perceptions and experiences.
Primary outcomes were the IMB model scores. True answers of HPV-related knowledge received a “+1” point, while false or don’t know answers received a “0” points. Motivation and behavioral skills scores were assessed by a 5-point Likert scale (“−2” points for strongly disagree, “−1” point for disagree, “0” point for not sure, “+1” point for agree, and “+2” points for strongly agree). The higher scores indicated better knowledge, motivation, and behavioral skills, except for the perceived barriers item. Secondary outcomes were the rate of HPV vaccination willingness, recommend vaccination willingness, and reservation/vaccination action (“Yes” or “No”).
Baseline survey and intervention
Before the intervention, all participants were required to complete the baseline questionnaire. Then, the intervention group received mobile phone-based education over 10 minutes every day for 7 days, which included the following topics: (1) information on the prevention of infectious diseases, vaccination and sexual health, (2) information on HPV infection, cervix, and cervical cancer among Chinese women, (3) information on the preventive measure for cervical cancer: HPV vaccine, (4) case study of the prognosis of Chinese women with advanced cervical cancer, (5) a story of a college girl’s experience from being unaware of HPV to deciding to get the HPV vaccine, (6) information on how to improve self-efficacy and self-determination to adopt a healthy behavior, and (7) information on the availability, cost and other behavioral techniques of the HPV vaccine. When the intervention finished, participants were asked to fill out the post-education questionnaire. As for control group, we offered them health information on COVID-19 and collected questionnaires at the same time as the intervention group.
Follow-Up
At 1 and 3 months after the intervention, participants in both intervention and control groups were asked to finish the post-education questionnaire again to assess the sustainability of the intervention effects. A flow diagram of the study is shown in Figure 1.
Figure 1.
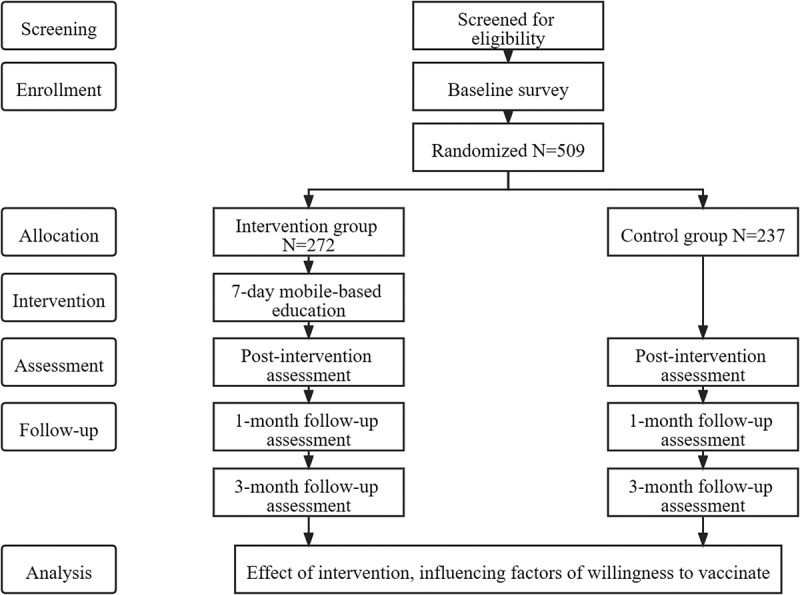
Study flowchart.
Statistical analysis
SPSS 20.0 software (IBM Corp, Armonk, New York) was used to conduct statistical analysis for this study. Categorical variables such as socio-demographic characteristics used the chi-square test, while continuous variables such as the score of perceived susceptibility used Student’s t test or one-way ANOVA to identify the difference between intervention and control groups. Significant parameters found by univariate analysis (P < .10) were incorporated and examined using multivariate analysis. Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were calculated and reported based on Wald chi-square statistics.
Results
Participants’ characteristics
Among 509 respondents who had finished the baseline questionnaire, 272 were allocated to the intervention group, and 237 were allocated to the control group. As shown in Table 1, 52.7% majored in science, and virtually all of them (97.6%) were Han Chinese. A total of 68.8% had lived in urban areas for more than 1 year, 65.2% had monthly living expenses ranging from 1000 to 2000 Chinese Yuan (CNY), and 77.4% had no relatives or friends with cancer. There was 68.8% of the participants’ parents had lived in urban areas for more than one year, 83.1% were married, and 26.1% had a college degree or higher.
Table 1.
Socio-demographics and health-related characteristics of study participants at baseline (N = 509)
| Variables |
Total, n (%) |
Control group, n (%) |
Intervention group, n (%) |
P |
| Socio-demographic | ||||
| Major in school | ||||
| Literature | 241 (47.3) | 103 (43.5) | 138 (50.7) | .101 |
| Science | 268 (52.7) | 134 (56.5) | 134 (49.3) | |
| Ethnicity | ||||
| Han Chinese | 497 (97.6) | 229 (96.6) | 268 (98.5) | .158 |
| Other | 12 (2.4) | 8 (3.4) | 4 (1.5) | |
| Permanent residence (for more than one year) | ||||
| Urban | 350 (68.8) | 164 (69.2) | 186 (68.4) | .843 |
| Rural | 159 (31.2) | 73 (30.8) | 86 (31.6) | |
| Parental residence (for more than one year) | ||||
| Urban | 350 (68.8) | 162 (68.4) | 188 (69.1) | .853 |
| Rural | 159 (31.2) | 75 (31.6) | 84 (30.9) | |
| Marital status of parents | ||||
| Married | 423 (83.1) | 191 (80.6) | 232 (85.3) | .158 |
| Divorce/Separation/Cohabit/Widowed | 86 (16.9) | 46 (19.4) | 40 (14.7) | |
| Education level of parents | ||||
| ≤ 9 years | 222 (43.6) | 98 (41.4) | 124 (45.6) | .624 |
| 10 - 12 years | 154 (30.3) | 74 (31.2) | 80 (29.4) | |
| ≥ 13 years | 133 (26.1) | 65 (27.4) | 68 (25.0) | |
| Living expenses (CNY/month) | ||||
| < 1000 | 148 (29.1) | 66 (27.8) | 82 (30.1) | .619a |
| 1000 - 2000 | 332 (65.2) | 155 (65.4) | 177 (65.1) | |
| > 2000 | 29 (5.7) | 16 (6.8) | 13 (4.8) | |
| Family/friends with any cancer | ||||
| Yes | 115 (22.6) | 51 (21.5) | 64 (23.5) | .588 |
| No | 394 (77.4) | 186 (78.5) | 208 (76.5) | |
| Health-related variables | ||||
| Believe vaccination is effective in preventing disease | ||||
| Yes | 485 (95.3) | 222 (93.7) | 263 (96.7) | .109 |
| No | 24 (4.7) | 15 (6.3) | 9 (3.3) | |
| Received self-paid vaccines | ||||
| Yes | 316 (62.1) | 145 (61.2) | 171 (62.9) | .696 |
| No | 193 (37.9) | 92 (38.8) | 101 (37.1) | |
| Received sexual education | ||||
| Yes | 366 (71.9) | 165 (69.6) | 201 (73.9) | .284 |
| No | 143 (28.1) | 72 (30.4) | 71 (26.1) | |
| Actively searched for or consulted on HPV vaccine | ||||
| Yes | 151 (29.7) | 78 (32.9) | 73 (26.8) | .135 |
| No | 358 (70.3) | 159 (67.1) | 199 (73.2) | |
| Previous sexual experience | ||||
| Yes | 9 (1.8) | 6 (2.5) | 3 (1.1) | .315a |
| No | 500 (98.2) | 231 (97.5) | 269 (98.9) | |
| Currently relationship | ||||
| Yes | 433 (85.1) | 193 (81.4) | 240 (88.2) | .032 |
| No | 76 (14.9) | 44 (18.6) | 32 (11.8) | |
| Attitude toward premarital sex | ||||
| Yes | 147 (28.9) | 71 (30.0) | 76 (27.9) | .617 |
| No | 362 (71.1) | 166 (70.0) | 196 (72.1) | |
aFisher’s exact test. CNY, Chinese Yuan; 6.92 CNY = 1 USD; HPV, human papillomavirus.
For health-related variables, most of participants (95.3%) believed vaccination helps to prevent disease. Yet, only 62.1% had ever received self-paid vaccines, and even fewer participants (29.7%) had ever searched for the HPV vaccine. Among the participants, the majority (71.9%) had ever received sexual education, they (98.2%) scarcely had prior sexual experience, and most of them (71.1%) held negative attitudes toward premarital sex. The bulk of participants (85.1%) were in a relationship. However, there were marginally more participants in a relationship in intervention group than in control group (P = .032).
Intervention effects on IMB
Information
At baseline, approximately half of the participants in both intervention and control groups had ever heard of HPV, HPV-related disease, and the HPV vaccine (Table S1). After the intervention, more than 90% of participants in intervention group knew the three issues listed above (96.1%, 91.2%, and 93.1% for HPV, HPV-related disease, and HPV vaccine, respectively) and the awareness rates sustained at a high level over time (P < .001). Although control group received no formal education, we discovered that the awareness of the three items increased over time, with over 80% of them knowing HPV (89.3%), HPV-related disease (84.4%), and the HPV vaccine (87.8%) after 3 months (P < .001). In terms of total knowledge scores, we identified a significant improvement in intervention arm after education (P < .001), while we detected no similar changes in control arm (P = .161, Figure 2). In addition, the level of knowledge was higher in intervention arm (6.98 ± 1.55) compared to control arm (4.75 ± 2.41) after 7-day mobile-based education (P < .001). During the 3-month follow-up period, the knowledge score of intervention group sustained at a high level (P < .001). Although it was not statistically significant, we observed a slightly improvement of knowledge score in control group (P = .188).
Figure 2.
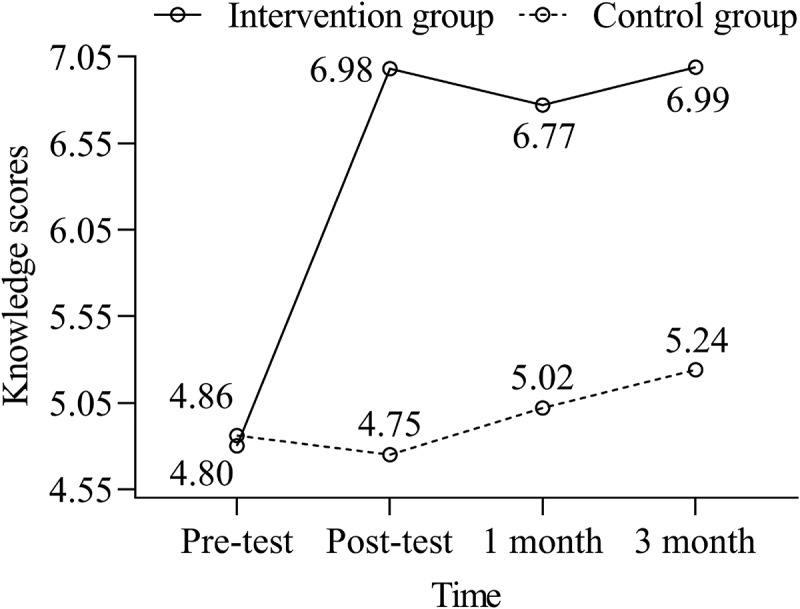
Mean value of intervention and control groups for total knowledge scores for condition across time.
Motivation
Before the intervention, there were no differences in motivation between the two groups, except that control group scored higher on subjective norms than intervention group (3.21 ± 0.61 vs. 3.10 ± 0.57, P = .043). The intervention group had a statistically significant increase in perceived susceptibility (2.49 ± 0.85 vs. 2.90 ± 0.88, P < .001), perceived benefit (3.86 ± 0.59 vs. 4.02 ± 0.49, P = .001), and perceived barrier (2.76 ± 0.59 vs. 2.87 ± 0.60, P = .045) from baseline to post-intervention and significantly scored higher than control group in these three aspects after education (P < .010). However, the differences between intervention and control groups in perceived severity and subjective norms scores were not statistically significant after education (P > .05). One month later, only an increase in perceived susceptibility in intervention group was statistically significant (1-month follow-up: 2.76 ± 0.92, P = .002). Nevertheless, compared to the baseline level, we detected significant changes in perceived severity (3.56 ± 0.76 vs. 3.38 ± 0.79, P = .014), perceived susceptibility (2.49 ± 0.85 vs. 2.72 ± 0.96, P = .008), and subjective norms (3.10 ± 0.57 vs. 3.22 ± 0.65, P = .042) in intervention group at the 3-month follow-up. The perceived susceptibility score was higher after 3 months than at baseline in control group (2.65 ± 0.93 vs. 2.45 ± 0.88, P = .022). Figure 3 depicts the changes in motivation over time in intervention and control groups.
Figure 3.
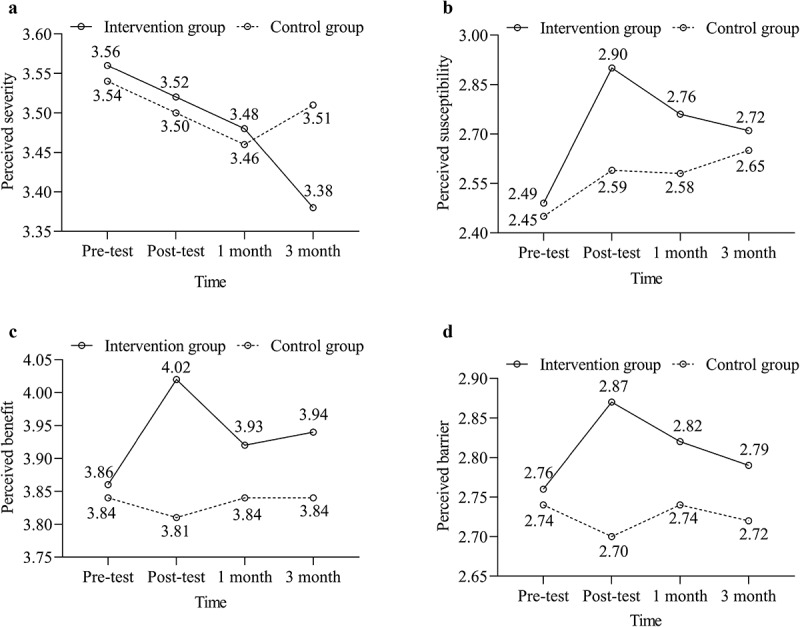
Mean values of intervention and control groups for (A) perceived severity, (B) perceived susceptibility, (C) perceived benefit, and (D) perceived barrier for condition across time.
Behavioral skills
At baseline, the mean scores of behavioral skills of intervention and control groups were 3.31 ± 0.58 and 3.35 ± 0.63, respectively (P = .520, Table S1). After 7-day mobile-based education, there was an improvement of behavioral skills in intervention group (P = .001), and the mean score of behavioral skills was lower in control group (3.34 ± 0.65) than in intervention group (3.48 ± 0.57, P = .018). During the follow-up period, we only detected an increase in intervention group from baseline to the 3-month follow-up (P = .033), while there was no statistically significant change from baseline to the 1-month follow-up in intervention group (P > .05).
Vaccination willingness and action
As shown in Table 2, the vaccination and recommended vaccination willingness were 28.2% and 62.1% in intervention group at baseline. In control group, the vaccination willingness and recommended vaccination willingness at baseline were 25.7% and 57.8%, respectively. In addition, vaccination and recommended vaccination intentions increased over time regardless of group allocation (P < .001). It is worth noting that the vaccination and recommended vaccination willingness in both groups increased evidently 3 months later (see Table 2). Furthermore, despite the persistent increasing of vaccination intention in both intervention and control group, the cumulative appointment/vaccination rate of intervention group was 2.94% 3 months later, which was similar to that of control group (4.64%).
Table 2.
Changes of HPV vaccination willingness and behavior in the intervention and control group before intervention, after intervention, 1-month and 3-month after intervention
| Vaccination willingness |
Recommend vaccination willingness |
Booked an appointment / got vaccinated |
||||
| |
Yes |
No |
Yes |
No |
Yes |
No |
| Intervention group | ||||||
| Pre-intervention, n (%) | 77 (28.3) | 195 (71.7) | 169 (62.1) | 103 (37.9) | 0 (0.0) | 272 (100.0) |
| Post-intervention, n (%) | 62 (30.5) | 141 (69.5) | 161 (78.9) | 43 (21.1) | 1 (0.5) | 203 (99.5) |
| One-month, n (%) | 61 (28.4) | 154 (71.6) | 162 (74.7) | 55 (25.3) | 2 (0.5) | 215 (99.5) |
| Three-month, n (%) | 109 (62.6) | 65 (37.4) | 166 (92.7) | 13 (7.3) | 5 (2.8) | 174 (97.2) |
| P | <.001 | <.001 | .015a | |||
| Control group | ||||||
| Pre-intervention, n (%) | 61 (25.7) | 176 (74.3) | 137 (57.8) | 100 (42.2) | 0 (0.0) | 237 (100.0) |
| Post-intervention, n (%) | 51 (24.9) | 154 (75.1) | 128 (62.1) | 78 (37.9) | 1 (0.5%) | 205 (99.5) |
| One-month, n (%) | 59 (30.1) | 137 (69.9) | 132 (66.0) | 68 (34.0) | 4 (2.0) | 196 (98.0) |
| Three-month, n (%) | 121 (60.8) | 78 (39.2) | 172 (83.9) | 33 (16.1) | 6 (2.9) | 199 (97.1) |
| P | <.001 | <.001 | .013a | |||
aFisher’s exact test. The numbers of participants at post-intervention, 1 month later, and 3 months later were not equal to the pre-intervention participants’ number in both groups due to loss of follow-up.
Influencing factors of HPV vaccination willingness
We divided the participants into two groups that were willing or unwilling to get vaccinated according to their intention at baseline to explore the differences between the two groups. The variables with a statistically significant difference (P < .10) between the two groups were having heard of HPV, HPV-related disease, HPV vaccine, knowledge of HPV and HPV vaccine, perceived susceptibility, perceived benefit, perceived barrier, subjective norms, and behavioral skills (Table S2).
As shown in Table 3, four variables were found to be associated with HPV vaccination willingness by multivariable logistic regression analysis. Participants who had ever heard of HPV were more willing to receive the HPV vaccine than those who had not heard of HPV (adjusted OR: 2.37, 95% CI: 1.44 – 3.89). Participants who perceived more barriers were more inclined to take HPV vaccine uptake (adjusted OR: 2.16, 95% CI: 1.44 – 3.25). In addition, participants who had higher subjective norms tended to get vaccinated (adjusted OR: 2.05, 95% CI: 1.26 – 3.32). Besides, participants equipped with more behavioral skills were more likely to get vaccinated (adjusted OR: 2.95, 95% CI: 1.79 – 4.87).
Table 3.
Factors associated with HPV vaccination willingness among female freshmen before intervention
| Variables |
OR (95% CI) |
P |
| Information | ||
| Ever heard of HPV | ||
| No | 1.00 | |
| Yes | 2.37 (1.44 - 3.89) | .001 |
| Motivation | ||
| Perceived barrier | 2.16 (1.44 - 3.25) | <.001 |
| Subjective norms | 2.05 (1.26 - 3.32) | .004 |
| Behavioral skills | 2.95 (1.79 - 4.87) | <.001 |
Discussion
Enhancing HPV vaccination coverage is of great importance for preventing cervical cancer, which necessitates raising public awareness.28 We had previously reported that a mobile phone-based educational intervention could improve vaccine knowledge among female college students,8 and more excitingly, we found that this improvement was persistent. Similar impacts were found in other educational interventions.29–32 However, as a health education that is not constrained by time and space, mobile phone-based education intervention conforms to the habits of college students and appears to be as effective as traditional education intervention.33 Meanwhile, it would be easier to promote this educational intervention because of the widespread use of mobile technology.34 Although lower than intervention group, we found that the awareness and knowledge level also increased in control group during the 1 month and 3-month follow-ups, which was consistent with a study by Perez et al.26 The reasons for this improvement are worth exploring. First, filling in the questionnaire may help to popularize the conception of the HPV vaccine and induce participants to learn more about the HPV vaccine.35 Second, the COVID-19 pandemic arouses public interest in vaccines, and countless resources are available to college students on the internet and at universities.26,36 So, participants in control group may learn pertinent information by these means to improve themselves.
Consistent with our hypothesis, the motivation to get vaccinated was promoted in intervention group after 7-day education, mainly reflected in the following aspects: perceived susceptibility, perceived benefit, and perceived barrier. The motivation of intervention group was higher compared with control group, indicating that mobile phone-based education can draw female college students’ attention to related issues. Nevertheless, this improvement faded to some extent during follow-up, which was consistent with other studies.26,30 The same change was found when we tested the effects of education on behavioral skills. Significant improvement of behavioral skills was made immediately after the intervention, but this kind of improvement gradually decreasing over time. Thus, to promote and maintain female college students’ motivation and behavioral skills to get vaccinated, we recommend an intermittent long-term education rather than a single 7-day educational intervention.26,33
In spite of tremendous improvement in knowledge level about HPV-related issues in intervention group, we did not detect significant increase in their vaccination willingness until 3 months after 7-day education, which was inconsistent with other studies involved educational intervention.29,30,37 An explanation may be our restriction of vaccination willingness in the next 6 months38 while our study time happened to be carried out during the COVID-19 pandemic, which may also contribute to lower vaccination willingness at baseline in our study compared to prior studies taking college students as their study participants.38–41 The 3-month follow-up was conducted from June to July 2020, when most cities in mainland China had recovered from the COVID-19 pandemic. Furthermore, we found similar variation tendency of vaccination willingness after intervention and during the 3-month follow-up in intervention and control group. One possible attribution for this is that control group acquired knowledge through questionnaires in the study,35 which aroused their intention to seek further information and get vaccination. In accordance with Liu’s study,38 we found recommend vaccination willingness was higher than vaccination willingness in both groups, and the reasons need further study.
As a harmful but ameliorable global public health issue, the WHO proposed “90-70-90” targets to be achieved by 2030 to effectively lower the incidence and mortality of cervical cancer worldwide and increase the rate of early diagnosis and treatment.42 Specifically, the goal for HPV vaccination is for 90% of girls aged 15 to be fully vaccinated.42 However, there is still a long way to go to achieve this goal in China. Despite the improvement in IMB scores, the cumulative HPV vaccine appointment/vaccination rate in our study was only 3.73% three months after the intervention, which was similar to other studies.14,15,17,26 The following factors may contribute to the low reservation/vaccination rate. First, the study was conducted in the period of the COVID-19 pandemic, which increased the subjective and objective barriers to vaccination.43–46 During the COVID-19 pandemic, some regions were forbidden from distributing the HPV vaccine, and experts recommended that the HPV vaccine and the COVID-19 vaccine not be administered concurrently.47 Second, the HPV vaccine is not covered by the national expanded program on immunization (EPI) in China, resulting in a considerable financial burden for college students and their families.17,18,38,40 Third, the demand for the HPV vaccine, especially the nine-valent HPV vaccine, has outpaced the supply in mainland China, making appointments challenging to come by.48,49 On the other hand, the 3-month follow-up period may not be long enough to detect changes in vaccine uptake.50 Fourth, subjects might not have sufficient motivation and behavioral skills to make an appointment or obtain the HPV vaccine, according to our findings.
In the current study, factors associated with the intention of HPV vaccination were information about whether one had ever heard of HPV, perceived barriers, subjective norms, and behavioral skills. Knowledge gaps concerning HPV have been widely reported,17,51–54 highlighting the significance of an education intervention for the vaccine’s target population. In contrast to earlier findings,55–58 participants who perceived more barriers would be more inclined to get vaccinated in our findings. Nonetheless, the association between perceived barriers and vaccination intention was cross-sectional. Hence, one probable explanation was that those who desired to get vaccinated knew more thoroughly about the HPV vaccine and understood the practical barriers that they might come across in mainland China to getting vaccinated, such as getting a reservation, completing multiple shots, and paying for vaccination. Consistent with prior studies,19,55,59–61 we found that subjective norms play a crucial part in people’s decision-making processes. Thus, a vaccine-friendly environment should be prioritized, and peer-led educational intervention would be more beneficial.55 We discovered that people with poor behavioral skills would have difficulty getting vaccinated, which could partially explain the low reservation/vaccination rate in our study. To enhance behavioral skills, we should focus on the role of the college youngster in the decision-making process because some female college students were unwilling to get vaccinated due to a lack of self-determination.19 Furthermore, previous studies have highlighted the importance of self-efficacy in getting vaccinated.62–64 Hence, future education should place a greater emphasis on boosting self-efficacy.
Compared with previous studies, our study has some strengths. First, our mobile-based education was more convenient and seemed equally valid compared to traditional education. Thus, the prospect for the mobile-based educational intervention looks bright. Second, we explored the effects of education not only immediately after the intervention but also the long-term impact on information, motivation, and behavioral skills after 1- and 3-month intervals. Third, to assure study quality, the components in the IMB model were derived from high-quality research. Forth, we adopted the IMB model to investigate the predictors of HPV vaccination willingness and underline another strategy to improve the vaccination intention and action of the target population, namely, to promote personal and social motivation as well as behavioral skills.
However, the limitations of this study should be noted. This was a single-center study with limited representativeness and sample size, so we should be cautious about promoting the conclusion. In addition, the coincidence of the COVID-19 pandemic and follow-up may affect vaccine booking and vaccination. Therefore, we may underestimate the influence of our 7-day mobile phone-based educational intervention on improving the intention to get vaccinated. Besides, we could not compare the advantages and disadvantages of the current intervention with other educational interventions since we designed a blank control. Furthermore, missing data due to the loss of follow-up can lead to bias to some extent. Fifthly, we found an increase in awareness and vaccination willingness in control group, which may be caused by some confounders we had not considered in study design. Lastly, although the questionnaire used in this study was compiled by literature review and expert discussion, and had been widely used in preview studies. The questionnaire has not been validated among Chinese female college students.
Conclusion
This IMB model-based study set out to evaluate the long-term effect of a 7-day mobile-based educational intervention on female college youngsters’ intention to receive the HPV vaccination and determine the potential predictors of vaccination intention. The results revealed that our intervention was effective in persistently improving college young people’s knowledge. However, after the 7-day intervention, continued education was required to maintain the improvement in motivation and behavioral skills. Besides, information, perceived barriers, subjective norms, and behavioral skills emerged as influential factors of HPV vaccination intention. In summary, these results suggest that we should prolong the intervention period and tailor education to the main influential factors.
Supplementary Material
Funding Statement
This work was supported by the The National Nature Science Foundation of Zhejiang #1 under Grant number LQ18H040001, LY20H040011; Medical Scientific Projects from Health Department of Zhejiang Province #2 under Grant number 2017KY101.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2051990.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F.. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–9. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Arbyn M, Weiderpass E, Bruni L, de Sanjose S, Saraiya M, Ferlay J, Bray F. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organizational WH . Cervical cancer. 2021.
- 4.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 5.Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond). 2021;41(10):1037–48. doi: 10.1002/cac2.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herzog TJ. New approaches for the management of cervical cancer. Gynecol Oncol. 2003;90(3):S22–7. doi: 10.1016/S0090-8258(03)00466-9. [DOI] [PubMed] [Google Scholar]
- 7.Organization WH . Immunization coverage. 2021.
- 8.Xi Z, Shiyu Y, Liying S, Xiangxian F, Mingyu S, Xiaoyou S, Xiaoyu F.. The utility of mobile phone-based intervention in promoting awareness and willingness to uptake human papillomavirus vaccine among female college students. Mod Preventive Med. 2021;48:888–92+934. [Google Scholar]
- 9.Organization WH . Existence of national HPV vaccination programme. 2021.
- 10.Zhu FC, Hu SY, Hong Y, Hu YM, Zhang X, Zhang YJ, Pan Q-J, Zhang W-H, Zhao F-H, Zhang C-F, et al. Efficacy, immunogenicity and safety of the AS04-HPV-16/18 vaccine in Chinese women aged 18-25 years: end-of-study results from a phase II/III, randomised, controlled trial. Cancer Med. 2019;8(14):6195–211. doi: 10.1002/cam4.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arbyn M, Xu L. Efficacy and safety of prophylactic HPV vaccines. a Cochrane review of randomized trials. Expert Rev Vaccines. 2018;17(12):1085–91. doi: 10.1080/14760584.2018.1548282. [DOI] [PubMed] [Google Scholar]
- 12.Huh WK, Joura EA, Giuliano AR, Iversen OE, de Andrade RP, Ault KA, Bartholomew D, Cestero RM, Fedrizzi EN, Hirschberg AL, et al. Final efficacy, immunogenicity, and safety analyses of a nine-valent human papillomavirus vaccine in women aged 16–26 years: a randomised, double-blind trial. Lancet. 2017;390(10108):2143–59. doi: 10.1016/S0140-6736(17)31821-4. [DOI] [PubMed] [Google Scholar]
- 13.Garland SM, Cheung TH, McNeill S, Petersen LK, Romaguera J, Vazquez-Narvaez J, Bautista O, Shields C, Vuocolo S, Luxembourg A, et al. Safety and immunogenicity of a 9-valent HPV vaccine in females 12–26 years of age who previously received the quadrivalent HPV vaccine. Vaccine. 2015;33(48):6855–64. doi: 10.1016/j.vaccine.2015.08.059. [DOI] [PubMed] [Google Scholar]
- 14.Ma Y, Wang C, Liu F, Lian G, Li S, He Q, Li T. Human papillomavirus vaccination coverage and knowledge, perceptions and influencing factors among university students in Guangzhou, China. Hum Vaccin Immunother. 2021;17(10):3603–12. doi: 10.1080/21645515.2021.1927411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiaoxiao Z, Jinjing S, Xuan Z, Yanyang Z, Wenzhou Y. Awareness and coverage of human papilomavirus vaccine among female university students in 2019. Chin J Vaccines Immunization. 2021;27:458–61+67. [Google Scholar]
- 16.Jiechen L, Linlin W, Qingrui B, Jia R, Huiyong S, Zhuoying H. Surveillance for coverage of human papillomavirus (HPV) vaccine and adverse events following immunization with HPV vaccine in Shanghai, 2017-2019. Chin J Vaccines Immunization. 2020;26:322–5+48. [Google Scholar]
- 17.Hu S, Xu X, Zhang Y, Liu Y, Yang C, Wang Y, Wang Y, Yu Y, Hong Y, Zhang X, et al. A nationwide post-marketing survey of knowledge, attitude and practice toward human papillomavirus vaccine in general population: implications for vaccine roll-out in mainland China. Vaccine. 2021;39(1):35–44. doi: 10.1016/j.vaccine.2020.11.029. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Wang Y, Liu L, Fan Y, Liu Z, Wang Y, Nie S. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16(1):216. doi: 10.1186/s12889-016-2873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jongen VW, van der Loeff MFS, Boyd A, Petrignani M, Prins M, van der Wal M, Nielen A, de Melker H, Paulussen TGWM, Alberts CJ, et al. Human papillomavirus vaccination uptake: a longitudinal study showing ethnic differences in the influence of the intention-to-vaccinate among parent-daughter dyads. Hum Vaccin Immunother. 2021;17(4):990–99. doi: 10.1080/21645515.2020.1808411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng SS, Hutubessy R, Chaiyakunapruk N. Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-valent vaccine, gender-neutral and multiple age cohort vaccination. Vaccine. 2018;36(19):2529–44. doi: 10.1016/j.vaccine.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y, Lee H, Seo JM. Integrated diabetes self-management program using smartphone application: a randomized controlled trial. West J Nurs Res. 2021;44(4):193945921994912. doi: 10.1177/0193945921994912. [DOI] [PubMed] [Google Scholar]
- 22.Motahari-Tabari NS, Nasiri-Amiri F, Faramarzi M, Shirvani MA, Bakhtiari A, Omidvar S. The effectiveness of information-motivation-behavioral skills model on self-care practices in early pregnancy to prevent gestational diabetes mellitus in Iranian overweight and obese women: a randomized controlled trial. Int Q Community Health Educ. 2021:272684x211020300. doi: 10.1177/0272684X211020300. [DOI] [PubMed] [Google Scholar]
- 23.Bakır E, Çavuşoğlu H, Mengen E. Effects of the information-motivation-behavioral skills model on metabolic control of adolescents with Type 1 diabetes in Turkey: randomized controlled study. J Pediatr Nurs. 2021;58:e19–e27. doi: 10.1016/j.pedn.2020.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Liang X, Yang J, Abdullah AS, He Z, Yang L. The evaluation of the effect of ICT in HIV prevention in the general population in China based on an information-motivation-behavioral skill model. Biomed Res Int. 2020;2020:8786467. doi: 10.1155/2020/8786467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114–23. doi: 10.1037/0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- 26.Perez GK, Cruess DG, Strauss NM. A brief information-motivation-behavioral skills intervention to promote human papillomavirus vaccination among college-aged women. Psychol Res Behav Manag. 2016;9:285–96. doi: 10.2147/PRBM.S112504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fisher WA. Understanding human papillomavirus vaccine uptake. Vaccine. 2012;30(Suppl 5):F149–56. doi: 10.1016/j.vaccine.2012.04.107. [DOI] [PubMed] [Google Scholar]
- 28.Zhang X, Wang Z, Ren Z, Li Z, Ma W, Gao X, Zhang R, Qiao Y, Li J. HPV vaccine acceptability and willingness-related factors among Chinese adolescents: a nation-wide study. Hum Vaccin Immunother. 2021;17(4):1025–32. doi: 10.1080/21645515.2020.1812314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Liu CR, Wang ZZ, Ren ZF, Feng XX, Ma W, Gao X-H, Zhang R, Brown MD, Qiao Y-L, et al. Effect of a school-based educational intervention on HPV and HPV vaccine knowledge and willingness to be vaccinated among Chinese adolescents : a multi-center intervention follow-up study. Vaccine. 2020;38(20):3665–70. doi: 10.1016/j.vaccine.2020.03.032. [DOI] [PubMed] [Google Scholar]
- 30.Liu CR, Liang H, Zhang X, Pu C, Li Q, Li QL, Ren F-Y, Li J. Effect of an educational intervention on HPV knowledge and attitudes towards HPV and its vaccines among junior middle school students in Chengdu, China. BMC Public Health. 2019;19(1):488. doi: 10.1186/s12889-019-6823-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kester LM, Shedd-Steele RB, Dotson-Roberts CA, Smith J, Zimet GD. The effects of a brief educational intervention on human papillomavirus knowledge and intention to initiate HPV vaccination in 18-26 year old young adults. Gynecol Oncol. 2014;132(Suppl 1):S9–12. doi: 10.1016/j.ygyno.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 32.Molokwu J, Dwivedi A, Mallawaarachchi I, Hernandez A, Shokar N. Tiempo de Vacunarte (time to get vaccinated): outcomes of an intervention to improve HPV vaccination rates in a predominantly Hispanic community. Prev Med. 2019;121:115–20. doi: 10.1016/j.ypmed.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 33.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901–20. doi: 10.1016/j.vaccine.2014.01.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karanth SS, Lairson DR, Savas LS, Vernon SW, Fernandez ME. The cost of developing a computerized tailored interactive multimedia intervention vs. a print based Photonovella intervention for HPV vaccine education. Eval Program Plann. 2017;63:1–6. doi: 10.1016/j.evalprogplan.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 35.Gottvall M, Tydén T, Höglund AT, Larsson M. Knowledge of human papillomavirus among high school students can be increased by an educational intervention. Int J STD AIDS. 2010;21(8):558–62. doi: 10.1258/ijsa.2010.010063. [DOI] [PubMed] [Google Scholar]
- 36.Pitts MK, Dyson SJ, Rosenthal DA, Garland SM. Knowledge and awareness of human papillomavirus (HPV): attitudes towards HPV vaccination among a representative sample of women in Victoria, Australia. Sex Health. 2007;4(3):177–80. doi: 10.1071/SH07023. [DOI] [PubMed] [Google Scholar]
- 37.Thanasas I, Lavranos G, Gkogkou P, Paraskevis D. The effect of health education on adolescents’ awareness of HPV infections and attitudes towards HPV vaccination in Greece. Int J Environ Res Public Health. 2022;19(1):503. doi: 10.3390/ijerph19010503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu Y, Di N, Tao X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum Vaccin Immunother. 2020;16(1):116–23. doi: 10.1080/21645515.2019.1638727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deng C, Chen X, Liu Y. Human papillomavirus vaccination: coverage rate, knowledge, acceptance, and associated factors in college students in mainland China. Hum Vaccin Immunother. 2021;17:828–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.You D, Han L, Li L, Hu J, Zimet GD, Alias H, Danaee M, Cai L, Zeng F, Wong LP, et al. Human Papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in China: a multicenter study. Vaccines (Basel). 2020;8(1). doi: 10.3390/vaccines8010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mascaro V, Pileggi C, Currà A, Bianco A, Pavia M. HPV vaccination coverage and willingness to be vaccinated among 18–30 year-old students in Italy. Vaccine. 2019;37(25):3310–16. doi: 10.1016/j.vaccine.2019.04.081. [DOI] [PubMed] [Google Scholar]
- 42.Organization WH . Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2021.
- 43.Ogundele OA, Omotoso AA, Fagbemi AT. COVID-19 outbreak: a potential threat to routine vaccination programme activities in Nigeria. Hum Vaccin Immunother. 2021;17(3):661–63. doi: 10.1080/21645515.2020.1815490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ota MOC, Badur S, Romano-Mazzotti L, Friedland LR. Impact of COVID-19 pandemic on routine immunization. Ann Med. 2021;53(1):2286–97. doi: 10.1080/07853890.2021.2009128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aizawa Y, Katsuta T, Sakiyama H, Tanaka-Taya K, Moriuchi H, Saitoh A. Changes in childhood vaccination during the coronavirus disease 2019 pandemic in Japan. Vaccine. 2021;39(29):4006–12. doi: 10.1016/j.vaccine.2021.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, Burey S, Feldman M, Morris SK. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario, Canada. Vaccine. 2021;39(31):4373–82. doi: 10.1016/j.vaccine.2021.05.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fei C, Jun L, Yuli L. Chinese expert consensus on comprehensive management in the three-level prevention and control of cervical cancer in prevention and control of COVID-19 pandemi. Chin J Pract Gynecol Obstetrics. 2021;37:185–88. [Google Scholar]
- 48.Wong LP, Han L, Li H, Zhao J, Zhao Q, Zimet GD. Current issues facing the introduction of human papillomavirus vaccine in China and future prospects. Hum Vaccin Immunother. 2019;15(7–8):1533–40. doi: 10.1080/21645515.2019.1611157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhao F, Qiao Y. Cervical cancer prevention in China: a key to cancer control. Lancet. 2019;393(10175):969–70. doi: 10.1016/S0140-6736(18)32849-6. [DOI] [PubMed] [Google Scholar]
- 50.Patel DA, Zochowski M, Peterman S, Dempsey AF, Ernst S, Dalton VK. Human papillomavirus vaccine intent and uptake among female college students. J Am Coll Health. 2012;60(2):151–61. doi: 10.1080/07448481.2011.580028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lenehan JG, Leonard KC, Nandra S, Isaacs CR, Mathew A, Fisher WA. Women’s knowledge, attitudes, and intentions concerning Human Papillomavirus vaccination: findings of a waiting room survey of obstetrics-gynaecology outpatients. J Obstet Gynaecol Can. 2008;30(6):489–99. doi: 10.1016/S1701-2163(16)32864-X. [DOI] [PubMed] [Google Scholar]
- 52.Giede C, McFadden LL, Komonoski P, Agrawal A, Stauffer A, Pierson R. The acceptability of HPV vaccination among women attending the University of Saskatchewan Student Health Services. J Obstet Gynaecol Can. 2010;32(7):679–86. doi: 10.1016/S1701-2163(16)34572-8. [DOI] [PubMed] [Google Scholar]
- 53.Zimet GD, Weiss TW, Rosenthal SL, Good MB, Vichnin MD. Reasons for non-vaccination against HPV and future vaccination intentions among 19-26 year-old women. BMC Womens Health. 2010;10(1):27. doi: 10.1186/1472-6874-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brabin L, Roberts SA, Stretch R, Baxter D, Chambers G, Kitchener H, McCann R. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. Bmj. 2008;336(7652):1056–58. doi: 10.1136/bmj.39541.534109.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Allen JD, Mohllajee AP, Shelton RC, Othus MK, Fontenot HB, Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Prev Med. 2009;48(5):420–25. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 56.Reiter PL, Brewer NT, Gottlieb SL, McRee AL, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–80. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 57.Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith JS. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstet Gynecol. 2008;111(5):1103–10. doi: 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- 59.DiClemente RJ, Murray CC, Graham T, Still J. Overcoming barriers to HPV vaccination: a randomized clinical trial of a culturally-tailored, media intervention among African American girls. Hum Vaccin Immunother. 2015;11(12):2883–94. doi: 10.1080/21645515.2015.1070996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Krawczyk AL, Perez S, Lau E, Holcroft CA, Amsel R, Knauper B, Rosberger Z. Human papillomavirus vaccination intentions and uptake in college women. Health Psychol. 2012;31(5):685–93. doi: 10.1037/a0027012. [DOI] [PubMed] [Google Scholar]
- 61.Allen JD, Othus MK, Shelton RC, Li Y, Norman N, Tom L, Del Carmen MG. Parental decision making about the HPV vaccine. Cancer Epidemiol Biomarkers Prev. 2010;19(9):2187–98. doi: 10.1158/1055-9965.EPI-10-0217. [DOI] [PubMed] [Google Scholar]
- 62.Rhodes SD, Diclemente RJ. Psychosocial predictors of hepatitis B vaccination among young African-American gay men in the deep south. Sex Transm Dis. 2003;30(5):449–54. doi: 10.1097/00007435-200305000-00013. [DOI] [PubMed] [Google Scholar]
- 63.Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, Ryan M, Fuemmeler BF, Carlyle KE. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–42. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44(2):171–80. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


