ABSTRACT
The question of whether children should be vaccinated against COVID-19 is currently being argued. The risk-benefit analysis of the vaccine in children has been more challenging because of the low prevalence of acute COVID-19 in children and the lack of confidence in the relative effects of the vaccine and the disease. One of the most convincing arguments for vaccinating healthy children is to protect them from long-term consequences. The aim of this study was to assess Jordanian parents’ intention to vaccinate their children. This is an Internet-based cross-sectional survey. The researchers prepared a Google Forms survey and shared the link with a number of Jordanian Facebook generic groups. Data were gathered between September and November 2021. In this study, convenience sampling was used. Knowledge about COVID-19 and preventive practices against COVID-19 were calculated for each participant. A total of 819 participants completed the survey (female = 70.9%). Of these, 274 (30.2%) participants intended to vaccinate their children, whereas the rest were either unsure 176 (21.5%) or intended not to vaccinate their children 396 (48.4%). The variables that increased the odds of answering “No” vs “Yes” to “will you vaccinate your children against COVID-19” included not willing to take the vaccines themselves (OR 3.75; CI, 1.46–9.62) and low protective practice group (OR 1.73;CI, 1.12–2.68). Participants had significant levels of refusal/hesitancy. Several barriers to vaccination were identified; attempts to overcome these should be stepped up.
KEYWORDS: COVID-19, vaccine, children, Jordan, hesitancy
JEL CLASSIFICATION: I10
Introduction
The primary method to restrict the spread of COVID-19 and the risk of additional variations emerging is universal COVID-19 vaccination.1–3 The immunization of large sections of pediatric and adult populations in low/middle-income countries where COVID-19 variants of concern have been discovered is critical to the effectiveness of vaccination campaigns.4,5
Jordan had fully vaccinated 3.67 million persons (36%) against COVID-19 by 22 November 2021.6 Vaccination coverage in Jordan is greater than in low-income nations (on average <2.5%).7 Jordan approved the vaccination of children aged 12 years and older recently (July 2021)8and considering providing the vaccines for children between the ages of 5-11
Parental vaccine hesitancy, defined as parents’ delay in accepting or refusing vaccines for their children despite their availability, may be a significant barrier to immunization.9 However, few studies have investigated parental attitudes for COVID-19 vaccination, and findings have been inconsistent. A survey conducted in the United States (US) and Australia, prior to the first COVID-19 vaccination approvals in December 2020, indicated that 50% of pregnant women were willing to vaccinate their children against COVID-19. Similarly, in lower income countries, such as Brazil, Colombia, and Mexico, over half of expectant women were willing to vaccinate their children.10 Furthermore, a survey conducted in the United Kingdom has reported that about 48% of participants were willing to vaccinate their children against COVID-19.11 In another study conducted in Brazil, only a small percentage of caregivers (2.8%) were hesitant about immunizations.12 Similar results were reported in a survey done in Italy between December 2020 and January 2021, with only a minority of participants (10%) hesitant to vaccinate their children against the COVID-19.13 However, investigations conducted a few months following the establishment of COVID-19 immunization programs indicated that around half of US parents remained hesitant to vaccinate their children against COVID-19.14,15 Importantly, a previous study conducted in Turkey revealed that 56.8% of parents were willing to vaccinate their children with “national” (domestically produced) COVID-19 vaccines. Their acceptance rates were significantly lower when asked about an “International/foreign” vaccine as only 28.9% were willing to vaccinate their children with a foreign vaccine. Most reported reasons for vaccine hesitancy were concerns about vaccine side effects, a lack of knowledge regarding vaccine effectiveness, and a suspicion of vaccines originating from other countries16 Furthermore, in a Saudi Arabian study, 24% of others were reluctant to give their children COVID 19 vaccinations due to concerns about side effects.17 In another study conducted in Saudi Arabia,18 52% were hesitant to vaccinate their children and the need for a reliable source of information about the vaccine was a significant reason behind the hesitancy.18 A lower percentage of hesitancy was reported in a study conducted in Qatar19,23,1as with only 17.9% showed parental vaccine hesitancy, with the main reason cited being “wait and see”, indicating reluctance due to potential vaccine side effects. There is therefore a pressing need to understand attitudes toward current information on vaccine views and COVID-19 vaccine attitudes among parents. The aim of this study was to investigate the prevalence and extent of COVID-19 vaccine hesitancy among parents of children and adolescents living in Jordan.
Materials and methods
Design
This is a web-based cross-sectional study. The study formulated a questionnaire on Google Forms and distributed the link via different Jordanian Facebook generic groups. The study data were collected from September to November 2021. The inclusion criteria included being Jordanian, above the age of 18 and having children who were not yet vaccinated against COVID-19. To ensure that the participants met the inclusion criteria, questions about place of residency and having children who were not yet vaccinated were included in the beginning of the questionnaire (see Figure 1). Those who did not meet the inclusion criteria were automatically directed to submit the form. A prologue that describes the aims of the study and contains an informed consent form were included in the questionnaire. Ethical approval was obtained from Al-Zaytoonah University of Jordan ethical committee. The current study was conducted with accordance to the Declaration of Helsinki ethical principles.
Figure 1.
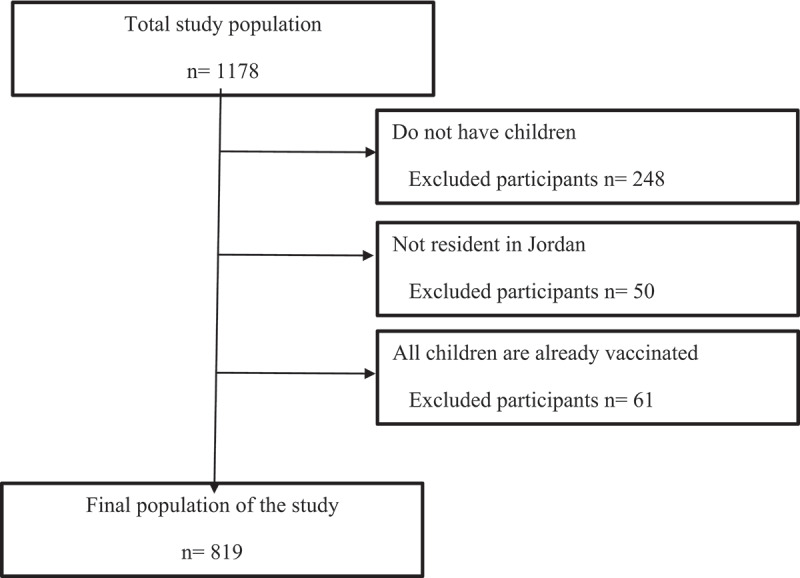
Recruitment flowchart.
Instrument
A questionnaire was constructed after conducting thorough literature review.20,21,22,23 The questionnaire was then presented to an expert committee that confirmed the content validity of the questionnaire. The questionnaire was initially developed in English, the language that was used to conduct the literature review, then translated to Arabic, the most spoken language in Jordan, back-translation was also performed, and the two versions were found to be comparable. A pilot study was conducted to confirm the questionnaire’s face validity, in the pilot study the questionnaire was circulated to 30 participants that who confirmed the clarity of the questions. The data of the pilot study was not included in the final analysis.
The questionnaire included five sections. The first section contains questions related to demographic information, including household monthly income, and the participants were classified into low-middle- and high-income groups based on the average household monthly income as stated by the Jordanian department of statistics24 The second section included questions about the participants’ experiences with COVID-19; if they, their children, or close friend/relative were ever infected with COVID-19, and if the participants were vaccinated or planning to be vaccinated against COVID-19. It also contained questions that evaluated the participants’ perceived seriousness of COVID-19 on them and on their children. The third section evaluated the participants’ knowledge about COVID-19 symptoms, protection methods, mood of transmission and available vaccines. The fourth section evaluated participant’s adherence to protective measure against COVID-19. The fifth section evaluated the participants perception towards COVID-19 vaccines efficacy and safety and their willingness to vaccinate their children. The sixth and final section evaluated the reasons behind vaccine hesitancy/refusal of those who answered ‘no’ or ‘not sure’ regarding intent to be vaccinate their children.
The children of the participants were classified into high-risk and low-risk groups of developing severe illness due to COVID-19. Pre-term children and children who have at least one of the following conditions: asthma, allergies, diabetes, cancer, cardiovascular disease, sickle cell anemia, liver disease and thalassemia, or taking steroids or immunosuppressants medications were included in the high-risk group while the rest were included in the low-risk group.
Knowledge and practice scores were computed for each participant. The knowledge score was calculated based on the participants’ knowledge of COVID-19 symptoms, transmission method and protective measures against the infection as one point was granted for each correct answer, the maximum possible score of 21 (Table A1). Practice score was calculated as the sum of the practice statements for the question ‘What procedures have you done to protect yourself from COVID-19?’ (Table A1), which represent the participants’ adherence to protective measures with answers ranged from “Never” (1 point) to “All the time” (5 points) with a maximum possible score of 25.
The medians for the knowledge and practice scores were calculated and the participants were divided into two groups, the first, group (high-level, group) included participants who got higher than the median scores and the rest were included in the low-level group.
Sampling type and sample size
Convenience sampling was used in this study. The required sample size at 95% significance level and a 5-percentage-point margin of error was 385. To perform a logistic regression that evaluated variables associated with participants intent to vaccinate their children, the rule of Events Per Variable criterion (EPV) ≥1025 was utilized, and as the events of the smallest group in three possible outcomes were 176 (not sure), the number of independent variables that can be included in the model are 17. The model used in the current study included only 15 variables.
Statistical analysis
Categorical variables were presented as frequency and percentages, and continuous variables were presented as means and standard deviations (SD). Cronbach’s alpha was conducted to evaluate the internal consistency of the items used to compute the knowledge and practice scores.
The minimum acceptable Cronbach’s alpha for the practice score was .7, while for the knowledge score it was determined to be above .5 as lower Cronbach’s alphas are expected in binary data.25 The computed Cronbach’s alphas were .83 and .55 for the practice and knowledge scores respectively.
Univariate analysis using Kruskal–Wallis and Chi-square analyses were used to identify variable association with participants intent to vaccinate their children. Variables that yielded p ≤ .20 in the univariable analysis were included in the multinominal logistic regression as independent variables, while participants’ intent to vaccinate their children was the dependent variable.
Results
Overall, 819 participants completed the survey (Table 1). The majority of participants (70.9%) were females, almost half (49.6%) had a child aged between 7 to 12, while 9.9% had a child under the age of one year. Most (85.6%) participants were married, and (7.7%) of the female participants were pregnant. The majority of participants (57%) had both boys and girls. Most participants (75.6%) were nonsmokers. Most of the participants were from Amman (50.4) followed by Zarqa (14.4)
Table 1.
Sample characteristics
| Characteristics | Frequency (%) (n=819) |
|
|---|---|---|
| Participant age | 18-29 | 146 (17.8) |
| 30-39 | 344 (42.0) | |
| 40-49 | 196 (23.9) | |
| 50-59 | 122 (14.9) | |
| 60 or more | 11 (1.3) | |
| Children’s age | Under one year | 81 (9.9) |
| 1–3 year | 274 (33.5) | |
| 4–6 year | 318 (38.8) | |
| 7–12 year | 406 (49.6) | |
| 13–17 year | 259 (31.6) | |
| More than 18 years | 144 (17.6) | |
| Sex | Male | 238 (29.1) |
| Female | 581 (70.9) | |
| Marital status | Single | 118 (14.4) |
| Married | 701 (85.6) | |
| Pregnancy status | Yes | 45 (3.4) |
| Child sex | Boys | 204 (24.9) |
| Girls | 148 (18.1) | |
| Boys and girls | 467 (57.0) | |
| Do you Smoke? | No | 619 (75.6) |
| Ex-smoker | 28 (3.4) | |
| Yes | 172 (21.0) | |
| Educational level | High school or less | 149 (18.2) |
| Diploma | 70 (8.5) | |
| University student | 10 (1.2) | |
| Bachelor | 426 (52.0) | |
| Postgrad | 164 (20.0) | |
| Household average monthly income ($) | Less than 700 | 275 (33.6) |
| 700-1400 | 358 (43.7) | |
| More than 1400 | 186 (22.7) | |
| Are you working/studying in a medical field | Yes | 296 (36.1) |
| No | 523 (63.9) | |
| Residency | North region | 161 (19.7) |
| South region | 66 (6.1) | |
| Zarqa | 118 (14.4) | |
| Middle region | 61 (7.4) | |
| Amman | 413 (50.4) |
$: US dollars.
Bachelor’s degree holders made up 53.5% of the participants, while 1.2% were university students and (43.7%) earned $700-$1400 per month. Lastly, 63.9% did not work or study in a medical field. Participants were classified into high and low adherence to protective practices against COVID-19 and knowledge about COVID-19 and its vaccine, based on the median scores. The median for the practice and knowledge scores were 16 (Quartiles:14–18) and 17 (Quartiles:15–18) respectively. Those who scored above the median were included in the high -level group while the rest were included in the low level group.
In the current sample, only 274 (30.2%) participants intended to vaccinate their children, while the rest were either ‘not sure’ (176; 21.5%) or intended not to vaccinate their children (396; 48.4%). Univariate analysis was conducted using Chi-square and Kruskal Wallis test (Table 2). These indicated that several factors were significantly associated with parents’ intention to vaccinate their children against COVID-19 including: perceived seriousness of COVID-19 on participants’ health (p < .001), children’s sex (p = .05), area of residency (p < .001), household average monthly income (p < .001), working/studying in a medical field (p = .02), knowing someone close infected with COVID-19 (p = .03), if participants’ children had ever had COVID-19 (p = .04), the participant had COVID-19 (p = .05), perceived degree of COVID-19 seriousness for their children (p < .001), perceived degree of COVID-19 vaccine safety and effectiveness on the children (p < .001), opinions about the likelihood that any of their children would be infected during the next 6 months (p < .001), adherence to protective practices against COVID-19 (p < .001) and if the participant was/or planning to be vaccinated against COVID-19 (p < .001).
Table 2.
Intention to vaccinate children by different sample characteristics presented as means (SD) or frequencies (percentages)
| A |
|
|
|||
|---|---|---|---|---|---|
| No |
Not Sure |
Yes |
|
|
|
| (N=396,48.4%) | (N=176,21.5%) | (N=247,30.2%) | Chi-square | P-Value | |
| How many children do you have? | 3.558 | 0.74 | |||
| One | 76 (19.2) | 30 (17.0) | 46 (18.6) | ||
| Two | 126 (31.8) | 62 (35.2) | 77 (31.2) | ||
| Three | 78 (19.7) | 42 (23.9) | 50 (20.2) | ||
| Four children or more | 116 (29.3) | 42 (23.9) | 74 (30.0) | ||
| Children age | |||||
| Less than one year | 40 (10.1) | 16 (9.1) | 25 (10.1) | 0.161 | 0.923 |
| 1–3 years | 133 (33.6) | 60 (34.1) | 81 (32.8) | 0.084 | 0.959 |
| 4–6 years | 160 (40.4) | 67 (38.1) | 91 (36.8) | 0.867 | 0.648 |
| 7–12 years | 204 (51.5) | 84 (47.7) | 118 (47.8) | 1.157 | 0.561 |
| 13–17 years | 125 (31.6) | 55 (31.3) | 79 (32.0) | 0.027 | 0.987 |
| 18 years or more | 59 (14.9) | 33 (18.8) | 52 (21.1) | 4.186 | 0.123 |
| Participant age | 4.743 | 0.78 | |||
| 18-29 | 74 (18.7) | 34 (19.3) | 38 (15.4) | ||
| 30-39 | 168 (42.4) | 69 (39.2) | 107 (43.3) | ||
| 40-49 | 95 (24.0) | 45 (25.6) | 56 (22.7) | ||
| 50-59 | 56 (14.1) | 25 (14.2) | 41 (16.6) | ||
| 60 or more | 3 (.8) | 3 (1.7) | 5 (2.0) | ||
| Children’s sex | 9.59 | 0.05 | |||
| Girls | 64 (16.2) | 43 (24.4) | 41 (16.6) | ||
| Boys | 111 (28.0) | 33 (18.8) | 60 (24.3) | ||
| Both (Girls and boys) | 221 (55.8) | 100 (56.8) | 146 (59.1) | ||
| Marital status | 2.986 | 0.23 | |||
| Other | 49 (12.4) | 31 (17.6) | 38 (15.4) | ||
| Married | 347 (87.6) | 145 (82.4) | 209 (84.6) | ||
| Residence | 22.384 | <.001 | |||
| North region | 94 (23.7) | 28 (15.9) | 39 (15.8) | ||
| South region | 19 (4.8) | 22 (12.5) | 25 (10.1) | ||
| Zarqa | 56 (14.1) | 32 (18.2) | 30 (12.1) | ||
| Middle region | 26 (6.6) | 12 (6.8) | 23 (9.3) | ||
| Amman | 201 (50.8) | 82 (46.6) | 130 (52.6) | ||
| Sex | 0.289 | 0.87 | |||
| Female | 283 (71.5) | 122 (69.3) | 176 (71.3) | ||
| Male | 113 (28.5) | 54 (30.7) | 71 (28.7) | ||
| Smoking | 0.895 | 0.93 | |||
| No | 300 (75.8) | 132 (75.0) | 187 (75.7) | ||
| Ex-smoker | 12 (3.0) | 8 (4.5) | 8 (3.2) | ||
| Yes | 84 (21.2) | 36 (20.5) | 52 (21.1) | ||
| Education level | 6.593 | 0.58 | |||
| High school or less | 66 (16.7) | 37 (21.0) | 46 (18.6) | ||
| University student | 5 (1.3) | 2 (1.1) | 3 (1.2) | ||
| Diploma | 42 (10.6) | 10 (5.7) | 18 (7.3) | ||
| Bachelor’s degree | 210 (53.0) | 90 (51.1) | 126 (51.0) | ||
| Postgrad | 73 (18.4) | 37 (21.0) | 54 (21.9) | ||
| Household average monthly income | 21.045 | <.001 | |||
| Less than $700 | 159 (40.2) | 51 (29.0) | 65 (26.3) | ||
| $700-$1400 | 169 (42.7) | 79 (44.9) | 110 (44.5) | ||
| More than $1400 | 68 (17.2) | 46 (26.1) | 72 (29.1) | ||
| Are you working/studying in a medical field? | 8.184 | 0.02 | |||
| Yes | 128 (32.3) | 61 (34.7) | 107 (43.3) | ||
| No | 268 (67.7) | 115 (65.3) | 140 (56.7) | ||
| Do you have a Chronic disease? | 40 (10.1) | 22 (12.5) | 39 (15.8) | 4.559 | 0.10 |
| Yes | |||||
| No | 356 (89.9) | 154 (87.5) | 208 (84.2) | ||
| Do you know somebody close to you that was infected with COVID-19? | 11.008 | 0.03 | |||
| No | 164 (41.4) | 77 (43.8) | 99 (40.1) | ||
| Not sure | 44 (11.1) | 21 (11.9) | 12 (4.9) | ||
| Yes | 188 (47.5) | 12 (44.3) | 136 (55.1) | ||
| Has any of your children ever been infected with COVID-19? | 10.114 | 0.04 | |||
| No | 268 (67.8) | 117 (66.5) | 141 (57.6) | ||
| Not sure | 36 (9.1) | 24 (13.6) | 32 (13.1) | ||
| Yes | 91 (23.0) | 32 (19.9) | 72 (29.4) | ||
| Have you ever been infected with COVID-19? | 9.483 | 0.05 | |||
| No | 208 (52.5) | 99 (56.3) | 134 (54.3) | ||
| Not sure | 45 (11.4) | 25 (14.2) | 16 (6.5) | ||
| Yes | 143 (36.1) | 52 (29.5) | 97 (39.3) | ||
| In your opinion, what is the likelihood that your children will be infected with COVID-19 during the next 6 months? | 22.80 | <.001 | |||
| I do not think that my child will be infected | 129 (32.6) | 45 (25.6) | 77 (31.2) | ||
| I think that my child will be infected and his symptoms will be mild | 190 (48.0) | 101 (57.4) | 141 (57.1) | ||
| I don’t now | 59 (14.9) | 22 (12.5) | 11 (4.5) | ||
| I think that my child will be infected and his symptoms will be severe | 18 (4.5) | 8 (4.5) | 18 (7.3) | ||
| Child risk toward COVID-19 | 64 (16.2) | 21 (11.9) | 30 (12.1) | 2.859 | 0.24 |
| high risk | |||||
| Low risk | 332 (83.8) | 155 (88.1) | 217 (87.9) | ||
| Knowledge level | 1.01 | 0.60 | |||
| Low | 273 (68.9) | 120 (98.2) | 161 (65.2) | ||
| High | 123 (31.1) | 56 (31.8) | 86 (34.8) | ||
| Practice level | 13.127 | <.001 | |||
| Low | 252 (63.6) | 107 (60.8) | 122 (49.4) | ||
| High | 144 (36.4) | 69 (39.2) | 125 (50.6) | ||
|
Have you taken or planning to take COVID-19 vaccine? yes |
331 (83.6) | 158 (89.8) | 240 (97.2) | 28.814 | <.001 |
| No | 65 (16.4) | 18 (10.2) | 7 (2.8) | ||
| continuous variable for vaccine intention | No (N = 396,48.4%) Median (25–75) |
Not Sure (N = 176,21.5%) Median (25–75) |
Yes (N = 247,30.2%) Median (25–75) |
P-Value | |
| How Dangerous COVID-19 in your health? | 2.92 (±1.25) | 3.31 (±1.1) | 3.43 (±1.13) | ||
| <.001 | |||||
| In your opinion, how dangerous is COVID-19 on your children? | 2.85 (±1.43) | 3.01(±1.03) | 3.39 (±1.22) | <.001 | |
| How effective is the use of COVID-19 vaccine for your children ? | 2.11 (±1.08) | 3.00 (±1.03) | 3.47 (±1.06) | <.001 | |
| How safe is the use of COVID-19 vaccine for your children ? | 1.69 (±.99) | 2.63 (±.93) | 3.36 (±1.08) | <.001 | |
Multinomial regression was applied to evaluate the factors associated with responding “Not Sure” or “No” regarding the intent to be vaccinated. As the results indicate (Table 3), the perceived safety of COVID-19 vaccine on children decreased the odds of responding ‘No’ or ‘Not sure’ vs. ‘Yes’ (OR .28; CI .21–.36) and (OR .52; CI .40–.67) respectively. The perceived effectiveness of the COVID-19 vaccine for children reduced the odds of responding ‘No’ vs ‘Yes’ (OR .76; CI .58–.99). The participants who reported having a chronic disease were significantly less likely to answer ‘No’ vs ‘Yes’ when compared with participants who do not have a chronic disease (OR .43; CL .23–.81).
Table 3.
Multivariate predictors of responding “not sure” or “no” regarding intent to vaccinate your children
| Characteristics | Intent to vaccinate No vs. Yes OR (95%CI) |
Intent to vaccinate Not sure vs. Yes OR (95%CI) |
|---|---|---|
| Estimate seriousness of COVID-19 on child | 0.89 (.71–1.11) | 0.72 (.58–.90)** |
| Estimate Seriousness of COVID-19 on participants | 1.11 (.87–1.41) | 1.32 (1.04–1.69)* |
| How effective is the use of COVID-19 vaccine for your children ? | 0.76 (.58–.99)* | 1.10 (.84–1.44) |
| In your opinion, How safe is the use of COVID-19 vaccine for your children ? | 0.28 (.21–.36)** | 0.52 (.40–.67)** |
|
Residence North region |
1.26 (.70–2.29) | 0.96 (.51–1.83) |
| South region | 0.44 (.19–1.00)* | 1.39 (.67–2.92) |
| Zarqa | 0.90 (.47–1.73) | 1.74 (.91–3.31) |
| Middle region | 0.7 (.31–1.57) | 0.91 (.40–2.08) |
| Amman | Reference | |
|
Household average monthly income Less than $700 |
1.06 (.58–1.93) | 0.84 (.46–1.55) |
| $700-$1400 | 1.13(.66–1.93) | 0.98 (.58–1.66) |
| More than $1400 | Reference | |
|
Are you working/studying in a medical field? YES |
1.03 (.65–1.63) | 0.75 (.47–1.21) |
| NO | Reference | |
|
Do you have a Chronic disease? YES |
0.43 (.23–.81)** | 0.67 (.36–1.27) |
| NO | Reference | |
|
Do you know somebody close to you that was infected with COVID-19? YES |
0.58 (.31–1.07) | 0.65 (.35–1.21) |
| MAYBE | 3.05 (1.03–8.98)* | 2.12 (.73–6.21) |
| NO | Reference | |
|
Have you ever been infected with COVID-19? YES |
1.53 (.83–2.82) | 1.15 (.61–2.17) |
| MAYBE | 1.09 (.40–2.94) | 1.76 (.66–4.70) |
| NO | Reference | |
|
Has any of your children ever been infected with COVID-19? YES |
0.79 (.44–1.41) | 0.78 (.43–1.43) |
| MAYBE | 0.32 (.14–.69)** | 0.53 (.24–1.14) |
| NO | Reference | |
| In your opinion, what is the likelihood that your children will be infected with COVID-19 during the next 6 months? | ||
| I think that my child will be infected and his symptoms will be severe | 0.52 (.57–3.86) | 1.33 (.47–3.75) |
| I don’t know | 2.72 (1.10–6.71)* | 4.09 (1.63–10.24)** |
| I think that my child will be infected and his symptoms will be mild | 1.03 (.63–1.66) | 1.39 (.84–2.28) |
| I do not think that my child will be infected | Reference | |
|
Practice level Low |
1.73 (1.12–2.68)** | 1.53 (.99–2.38) |
| High | Reference | |
|
Have you taken or planning to take COVID-19 vaccine? NO |
3.75 (1.46–9.62)** | 2.78 (1.04–7.42)* |
| YES | Reference | |
|
Children sex Girl |
1.45 (.81–2.61) | 1.75 (.99–3.09) |
| Boys | 1.13 (.66–1.90) | 0.67 (.38–1.19) |
| Both (boys and girls) | Reference |
* Significant at the level of less than .05, ** Significant at the level of less than .01.
Participants who answered ‘maybe’ to the question ‘Do you know somebody close to you that was infected with COVID-19?’ where more likely to answer ‘No’ vs ‘Yes’ (OR 3.05; CI,1.03–8.98) when compared with those reported that they do not know someone close to them that was infected with COVID-19. Participants who answered “maybe” to “Has any of your children ever been infected with COVID-19?” compared to those answered no were significantly less like to refuse to vaccinate their children (OR .32, CI, .14–.69). Participants who were classified into the low practice group were more likely to answer ‘No’ vs ‘Yes’ (OR 1.73; CI, 1.12–2.68). Those who did take and not planning to receive the vaccine against COVID-19 were significantly more likely to answer ‘No’ or ‘Not sure’ vs ‘Yes’ (OR 3.75; CI, 1.46–9.62) and (OR 2.78; CI, 1.04–7.42) respectively.
Table 4 shows the reported reasons for vaccination hesitancy/refusal. The most frequently mentioned causes for participants’ responses regarding their hesitancy to vaccinate their children were: ‘The vaccine will be new, I don’t want to be the first to get the vaccine’ (95%), followed by ‘I don’t want a vaccine I know nothing about; I’ll make my decision if/when one becomes available’ (88.5%), and the least mentioned cause was ‘Vaccine causes autism’ (15.2%).
Table 4.
Reasons participants provided for responding “No” or “Not sure” regarding intent to be vaccinated
| Reasons | Total N (%) |
|---|---|
| Concern about the vaccine | |
| The vaccine will be new, I won’t be the first to get the vaccine | 544 (95.0) |
| Vaccine cause autism | 87 (15.2) |
| I don’t think that I can afford the vaccine | 113 (19.7) |
| Vaccination may cause infected disease | 363 (63.5) |
| Need additional information | |
| I don’t want the vaccine I know nothing about. I’ll make my decision if/when on become available | 506 (88.5) |
| Attitudes | |
| I don’t feel I’m at risk | 259 (45.3) |
| I am scared to put forge in object on my body | 496 (86.7) |
| Lack of trust | |
| If the government recommended it use I will not take it | 350 (61.2) |
| There is no way I trust big pharmaceutical company | 310 (54.2) |
| I believe that this virus was developed by the governments and I won’t take any vaccine | 278 (48.6) |
Discussion
The main objective of the present research was to investigate the prevalence of COVID-19 vaccine hesitancy among parents of children and adolescents in the Jordanian population. Another key task was to identify significant predictors associated with COVID-19 vaccine indecision. The questionnaire covered a range of issues related to COVID-19 including knowledge, attitudes and practices toward COVID-19 and its vaccines.
Worrying findings were reported in the present study as only 30.2% of participants were willing to vaccinate their children—significantly lower than acceptance rates reported in several countries around the world including the US,14 UK,11 Brazil12and Italy13and in the region including Saudi Arabia,17,18 Turkey16and Qatar.26
Univariate analysis was utilized to categorize participants based on the parents’ intention/willingness to vaccinate their children against COVID-19. This revealed that perceived seriousness of COVID-19, geographic area of residency in Jordan, average monthly income, the perceived degree of COVID-19 seriousness on children, perceived degree of COVID-19 vaccine safety and effectiveness on children, personal opinions about the likelihood that children would be infected by COVID-19, adherence level to protective measures against COVID-19 and if the participants have been/are planning to be vaccinated against COVID-19 were strong predictors associated with the tendency to vaccinate their children.
To a lesser extent, children’s gender, working/studying in a medical field, knowing someone close who was infected with COVID-19, any of the participant’s children ever having COVID-19, and the participant having had COVID-19 influenced participants’ hesitancy to vaccinate their children against COVID-19.
These findings were concordant to some extent with the literature. Many studies revealed that seriousness of COVID-19 is associated with the beliefs about COVID-19 vaccination.27,28 Geography was also a strong predictor of vaccine hesitancy. A recent report by the U.S. Office of Assistant Secretary for Planning and Evaluation (ASPE) revealed that although hesitancy toward COVID-19 vaccination has dropped significantly in early 2021, different geographic areas in the USA illustrated different rates of hesitancy.29 This is similar to the results of the present study as parental vaccination intention was associated with residency area as indicated in the univariable and multivariable analysis. The difference found in paternal vaccination acceptance between the capital Amman and southern governates may be associated with income and education levels, as according to the statistics department of Jordan the income and education levels in southern governates are significantly less than the capital Amman (the reference group) and one of the lowest in the kingdom in general.23 This can be also confirmed by the results of the univariable analysis that indicated that the monthly income is a strong predictor of hesitancy toward COVID-19 vaccination. Previous studies have reported the association between education/income levels and parental vaccine acceptance30,31
A further crucial determinant of vaccine acceptance is beliefs about the safety and efficacy of COVID-19 as they are newly developed vaccines. Several studies conducted in the region reported concerns about vaccine safety as a major reason for hesitancy16–18,26 A recent study reported that Americans were also unwilling to receive the vaccine as they had concerns about safety and efficacy.32 Working in the medical field was expected to improve acceptance of vaccination. Research conducted in Thailand found that most physicians were willing to take COVID-19 vaccine, yet a significant proportion were hesitant to vaccinate their family members.33
Our univariate analysis also revealed an interesting finding. Parents with children who they reported have risk factors of high infectious severity of COVID-19 like preterm birth, diabetes, cardiovascular disease, asthma and respiratory conditions did not differ from other parents in terms of their plans regarding their children vaccination. This is a worrying finding as it shows that parents with vulnerable children were unaware of the seriousness of COVID-19 infection for their children.
Multinomial logistic regression was used to identify the factors that might affect parents who expressed low intention to vaccinate their children. Estimated seriousness of COVID-19 on children was a significant predictor of vaccine hesitancy in parents. This was expected as perceived seriousness of COVID-19 can play a crucial role in vaccine acceptance.34 In a Saudi Arabian study, participants felt that routine vaccination was significantly more important to their children’s health when compared with COVID-19 vaccination.18 In the current study, those who suspected that their children may have had COVID-19 were less likely to refuse the vaccine compared to those who reported that their children were not infected with COVID-19. Nevertheless, a study conducted in Qatar indicated that parents of children who had had COVID-19 were more hesitant to vaccinate their children when compared to parents who did not have previously infected children.26 This may be due to the perceived lower severity of symptoms experienced by the children.
Perceived efficacy of COVID-19 vaccine in children reduced the odds ratio in the refusing group. A Saudi Arabian study reported that participants doubted the efficacy of COVID-19 vaccine when compared with routine vaccination.18 A cross-sectional survey conducted in Canada concluded that parental acceptance toward COVID-19 vaccination for children would be improved by public health communication highlighting the safety and necessity of COVID-19 vaccination in children to support a return to normal activities.35 Perceived safety of COVID-19 vaccine in children was also a significant predictor of parental refusal of children’s vaccination and hesitancy both globally36and in the region.16–18,26
Absence of chronic diseases was also a strong predictor of parental children vaccination refusal. A systematic review37 concluded that presence of chronic diseases is associated with willingness to receiving COVID-19 vaccine. Being doubtful of knowing a close person who was infected with COVID-19 was also associated with parental children vaccination refusal and hesitancy. Participants who had low adherence to preventative practices against COVID-19 were less like to state that they would vaccinate their children. Participants who were not vaccinated and were not planning to have the COVID-19 vaccine themselves were significantly more likely to reply ‘No’ or ‘Not sure’ to their intention to vaccinate their children. Similar findings were reported in a Saudi study as vaccinated parents were more willing to vaccinate their children18
The main three reasons for vaccine refusal were the vaccine being a new product, no adequate information about the vaccine available to the public, and the concern of injecting a “mysterious” material into humans’ bodies. Therefore, public education regarding the safety and efficacy of COVID-19 vaccine is urged. Public awareness of COVID-19 vaccine should improve the acceptance and reduce hesitancy regarding vaccination.38 A structured public awareness campaign regarding COVID-19 vaccine addressing issues raised about the vaccine is essential. For example: yes, the vaccine was developed quickly, but it was thoroughly tested for its safety and efficacy. COVID-19 vaccine side effects are temporary and mild.
Taking the vaccine protects us from being sick, and can preserve many people’s lives. Most people with allergic conditions can still take the vaccine without worries of developing allergies against the vaccines. Furthermore, having the vaccine after COVID-19 infection will improve the immune response and further protect against future viral infection. Having the vaccine is not only meant to provide personal protection, it also indirectly delivers protection to other community members by reducing the chance of spreading the COVID-19. Population-wide vaccination will help return us all to a normal “pandemic free” lifestyle. Public awareness should also shed the light on enabling individuals to conduct a personal “risk-benefit assessment” especially for vulnerable individuals. Finally, recent safety reports confirmed the safety and efficacy of the vaccine in pregnant and breastfeeding females39
Strengths and limitations
This study evaluated participants’ knowledge about COVID-19 and its available vaccines, their protective practices against COVID-19 and the intent to vaccinate their children. The data of the present study was collected form most Jordanian governates to ensure a broad national coverage. As this is a self-administered questionnaire, the results may be subjected to selection and recall biases, for instance, 70% of the participants were mothers. Nevertheless, the large sample size included in the present study could limit the bias effect, moreover, in Jordan, and the Middle East generally, mothers are typically more concerned with and in charge of children’s affairs. Furthermore, previous studies have shown that web-based studies are a cost-effective method that can produce a representative sample, provide a safe environment for the respondents to answer questions honestly and accurately and eliminate interviewer bia40, 41As mentioned previously the main objective of the present research was to investigate the prevalence of COVID-19 vaccine hesitancy among parents of children and adolescents. Therefore, although some of participants had offspring above the age of 18, the vast majority of them had children aged under 18 (other siblings) and only 21 participants solely had offspring above the age of 18. Nevertheless, the data of the 21 participants were retained in the analysis because in conservative communities, like Jordan, parents have a substantial influence on their children’s decisions, even if their children are older than 18 and into their early 20s.
Conclusion
We found high parental hesitancy toward vaccine acceptance. These results illustrate the necessity to increase the awareness among the general population about childhood COVID-19 vaccination, in particular the relative risks and rewards.
Supplementary Material
Appendix A.
Table A1.
Knowledge toward COVID-19 and its vaccines
| Variable | Frequency (%) |
|---|---|
| Knowledge determinants | |
| What are the symptoms of COVID19? | |
| Fever† | 1116 (97.6) |
| Chills† | 802 (70.1) |
| Diarrhea† | 815 (71.2) |
| Cough† | 1033 (90.3) |
| Otitis media‡ | 234 (20.5) |
| Loss of smell and taste senses† | 1107 (96.8) |
| No symptoms† | 1017 (88.9) |
| How COVID19 can be transmitted? | |
| Drinking unclean water‡ | 153 (13.4) |
| Eating unclean food‡ | 217 (19.0) |
| Inhalation of respiratory droplets of infected person† | 1135 (99.2) |
| Eating or touching wild animals‡ | 255 (22.3) |
| What procedures do you think may prevent COVID-19 infection? | |
| Wearing face masks† | 1078 (94.2) |
| Washing hands with regular soap† | 1075 (94.0) |
| Using detergents† | 1084 (94.8) |
| Social distancing† | 1116 (97.6) |
| Avoid touching face/mouth/nose/eyes† | 1091 (95.4) |
| Avoid eating meat‡ | 143 (12.5) |
| Consume herbs‡ | 594 (52.2) |
| Believe that there is a cure for COVID19‡ | 22 (1.9) |
| Identified all the possible side effects of the vaccine included in the options correctly | 176(21.5%) |
| Vaccine is given intramuscularly | 621(75.8) |
| Attitudes and Practices | |
| What procedures have you taken to protect yourself from COVID19? | |
| Wearing face masks* | 1101 (96.2) |
| Washing hands with regular soap* | 1091 (95.4) |
| Using detergents* | 1070 (93.5) |
| Social distancing* | 1035 (90.5) |
| Avoid touching face/mouth/nose/eyes* | 936 (81.8) |
†Correct information,‡ Incorrect information, *Scientifically proven protective measure against COVID19.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2044257
References
- 1.Han B, Song Y, Li C, Yang W, Ma Q, Jiang Z, Li M, Lian X, Jiao W, Wang L, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: a double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(12):1645–10. doi: 10.1016/S1473-3099(21)00319-4/ATTACHMENT/3DD10DC6-047E-4C90-B8A1-A17D0B4163C6/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamidani S, Rostad CA, Anderson EJ.. COVID-19 vaccine development: A pediatric perspective. Curr Opin Pediatr. 2021;33(1):144–51. doi: 10.1097/MOP.0000000000000978. [DOI] [PubMed] [Google Scholar]
- 3.Hussein T, Hammad MH, Fung PL, Al-Kloub M, Odeh I, Zaidan MA, Wraith D. COVID-19 pandemic development in Jordan—short-term and long-term forecasting. Vaccines. 2021;9(7):728. doi: 10.3390/vaccines9070728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faria NR, Mellan TA, Whittaker C, Claro IM, Candido DD, Mishra S, Crispim MA, Sales FC, Hawryluk I, McCrone JT, et al. Genomics and epidemiology of a novel SARS-CoV-2 lineage in Manaus, Brazil. medRxiv Prepr Serv Heal Sci. doi: 10.1101/2021.02.26.21252554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay, S, San EJ, Msomi N, et al. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. 2021;592(7854):438–43. doi: 10.1038/s41586-021-03402-9. [DOI] [PubMed] [Google Scholar]
- 6.Covidvax.Live - Jordan. Accessed 2022 January 3. https://covidvax.live/location/jor
- 7.Mathieu E, Ritchie H, Ortiz-Ospina E, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Beltekian D, Roser M, et al. Coronavirus Pandemic (COVID-19). Our World Data. 2020;5(7):947–53. doi: 10.1038/S41562-021-01122-8. [DOI] [Google Scholar]
- 8.Freij M Jordan to vaccinate children aged 12 years and older against COVID-19 | Reuters. Reuters. https://www.reuters.com/world/middle-east/jordan-vaccinate-children-aged-12-years-older-against-covid-19-2021-07-24/. Published 2021. Accessed January 3, 2022.
- 9.Whelan SO, Moriarty F, Lawlor L, Gorman KM, Beamish J. Vaccine hesitancy and reported non-vaccination in an Irish pediatric outpatient population. Eur J Pediatr. 2021;180(9):2839–47. doi: 10.1007/S00431-021-04039-6. [DOI] [PubMed] [Google Scholar]
- 10.Skjefte M, Ngirbabul M, Akeju O, Escudero D, Hernandez-Diaz S, Wyszynski DF, Wu JW. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 2021;36(2):197–211. doi: 10.1007/S10654-021-00728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020;38(49):7789–98. doi: 10.1016/J.VACCINE.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani GP. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines. 2021;9(10):1115. doi: 10.3390/VACCINES9101115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montalti M, Rallo F, Guaraldi F, Bartoli L, Po G, Stillo M, Perrone P, Squillace L, Dallolio L, Pandolfi P, et al. Would parents get their children vaccinated against SARS-CoV-2? rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines. 2021;9(4):366. doi: 10.3390/VACCINES9040366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teasdale CA, Borrell LN, Kimball S, Rinke ML, Rane M, Fleary SA, Nash D. Plans to vaccinate children for coronavirus disease 2019: a survey of United States parents. J Pediatr. 2021;237:292–97. doi: 10.1016/J.JPEDS.2021.07.021/ATTACHMENT/B26E35D7-16B2-427A-98E1-83C3F4F8C450/MMC2.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szilagyi PG, Shah MD, Delgado JR, Thomas K, Vizueta N, Cui Y, Vangala S, Shetgiri R, Kapteyn A. Parents’ intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics. 2021;148(4). doi: 10.1542/PEDS.2021-052335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021. Published online 2021;40(4):E134–E136. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]
- 17.Aldakhil H, Albedah N, Alturaiki N, Alajlan R, Abusalih H. Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J Infect Public Health. 2021;14(10):1497–504. doi: 10.1016/J.JIPH.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Temsah MH, Alhuzaimi AN, Aljamaan F, Bahkali F, Al-Eyadhy A, Alrabiaah A, Alhboob A, Bashiri FA, Alshaer A, Temsah O, et al. Parental attitudes and hesitancy about COVID-19 vs. routine childhood vaccinations: a national survey. Front Public Heal. 2021;9:1513. doi: 10.3389/FPUBH.2021.752323/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Musa S, Dergaa I, Abdulmalik MA, Ammar A, Chamari K, Saad HB. Bnt162b2 COVID-19 vaccine hesitancy among parents of 4023 young adolescents (12–15 years) in Qatar. Vaccines. 2021;9(9):981. doi: 10.3390/VACCINES9090981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Qerem WA, and Jarab AS. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Heal. 2021;9: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Qerem W, Jarab AS, Qarqaz R, Hayek MA. Attitudes of a sample of Jordanian young adults toward different available COVID-19 vaccines. Vacunas. doi: 10.1016/J.VACUN.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu Y, Xu D, Luo L, Ma F, Wang P, Li H, Li Q, Wei L, Diao J, Liu Y, et al. A cross-sectional survey on COVID-19 vaccine hesitancy among parents from Shandong vs. Zhejiang. Front Public Heal. 2021;9:1722. doi: 10.3389/FPUBH.2021.779720/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alfieri NL, Kusma JD, Heard-Garris N, Davis MM, Golbeck E, Barrera L, Macy ML. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. 2021;21(1):1–9. doi: 10.1186/S12889-021-11725-5/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Jordanian Department of statistics. 2018 Year Book.
- 25.Peduzzi P, Concato J, Feinstein AR, and Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48(12):1503–1510. doi: 10.1016/0895-4356(95)00048-8. [DOI] [PubMed] [Google Scholar]
- 26.Cortina JM. What is coefficient alpha? an examination of theory and applications. J Appl Psychol. 1993;78(1):98–104. doi: 10.1037/0021-9010.78.1.98. [DOI] [Google Scholar]
- 27.Du M, Tao L, Liu J. The association between risk perception and COVID-19 vaccine hesitancy for children among reproductive women in China: an online survey. Front Med. 2021;8:1494. doi: 10.3389/FMED.2021.741298/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen H, Li X, Gao J, Liu X, Mao Y, Wang R, Zheng P, Xiao Q, Jia Y, Fu H, et al. Health belief model perspective on the control of COVID-19 vaccine hesitancy and the promotion of vaccination in China: web-based cross-sectional study. J Med Internet Res. 2021;23(9):e29329. doi: 10.2196/29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beleche T, Ruhter J, Kolbe A, Marus J, Bush L, Sommers B. 2021 ISSUE BRIEF 1 ISSUE BRIEF COVID-19 vaccine hesitancy: demographic factors, geographic patterns, and changes over time key points. Published online. 2021. ; doi: 10.1016/j.vaccine.2015.09.035. [DOI] [Google Scholar]
- 30.Petrie JR, Chaturvedi N, Ford I, Brouwer MC, Greenlaw N, Tillin T, Hramiak I, Hughes AD, Jenkins AJ, Klein BE, et al. Cardiovascular and metabolic effects of metformin in patients with type 1 diabetes (REMOVAL): a double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017;5(8):597–609. doi: 10.1016/S2213-8587(17)30194-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bono SA, Siau CS, Chen WS, Low WY, Faria de Moura Villela E, Pengpid S, Hasan MT, Sessou P, Ditekemena JD, Amodan BO, et al. Adults’ acceptance of COVID-19 vaccine for children in selected lower- and middle-income countries. Vaccines. 2021;10(1):11. doi: 10.3390/VACCINES10010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kricorian K, Civen R, Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother. 2021; 1–8. Published online 2021. doi: 10.1080/21645515.2021.1950504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sirikalyanpaiboon M, Ousirimaneechai K, Phannajit J, Pitisuttithum P, Jantarabenjakul W, Chaiteerakij R, Paitoonpong L. COVID-19 vaccine acceptance, hesitancy, and determinants among physicians in a university-based teaching hospital in Thailand. BMC Infect Dis. 2021;21(1):1–12. doi: 10.1186/S12879-021-06863-5/FIGURES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karlsson LC, Soveri A, Lewandowsky S, Karlsson L, Karlsson H, Nolvi S, Karukivi M, Lindfelt M, Antfolk J. Fearing the disease or the vaccine: the case of COVID-19. Pers Individ Dif. 2021;172:110590. doi: 10.1016/J.PAID.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Humble RM, Sell H, Dubé E, MacDonald NE, Robinson J, Driedger SM, Sadarangani M, Meyer SB, Wilson S, Benzies KM, et al. Canadian parents’ perceptions of COVID-19 vaccination and intention to vaccinate their children: results from a cross-sectional national survey. Vaccine. 2021;39(52):7669–76. doi: 10.1016/J.VACCINE.2021.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hudson A, Montelpare WJ. Predictors of vaccine hesitancy: implications for COVID-19 public health messaging. Int J Environ Res Public Health. 2021;18(15):8054. doi: 10.3390/IJERPH18158054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “vaccination refusal could prolong the war of this pandemic” – a systematic review. Risk Manag Healthc Policy. 2021;14:2609–23. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elgendy MO, Abdelrahim MEA. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J Med Virol. 2021;93(12):6535–43. doi: 10.1002/JMV.27199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.COVID-19 Vaccine Hesitancy: 12 Things You Need to Know | Johns Hopkins Medicine.
- 40.Fenner Y, Garland SM, Moore EE, Jayasinghe Y, Fletcher A, Tabrizi SN, Gunasekaran B, Wark JD. Web-Based recruiting for health research using a social networking site: an exploratory study. J Med Internet Res. 2012;14(1):e20. doi: 10.2196/jmir.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cantrell MA, Lupinacci P. Methodological issues in online data collection. J Adv Nurs. 2007;60(5):544–49. doi: 10.1111/j.1365-2648.2007.04448.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


