Abstract
The purpose of this study is to update the available literature with information on the current use of robotic assisted surgery (RAS) in the Department of Defense (DoD) compared to the civilian world, and how the coronavirus disease 2019 (COVID-19) pandemic impacted RAS in the DoD. A total of 9,979 RAS cases between 01st October 2017 and 31st December 2020 were reviewed from every DoD Military Treatment Facility (MTF) that meets our inclusion criteria and employs various models of da Vinci robotic surgical systems (Intuitive Surgical). Specialty, number, and facility were recorded for each case. These data were then compared to previously known trends about RAS use in the DoD as well as with civilian trends. Before COVID-19, the use of RAS had increased over time, but not at the same rate as in the civilian sector. General surgery cases constituted most RAS cases in both the DoD and the civilian sector. The arrival of COVID-19 in the United States significantly decreased the use of RAS in the DoD as well as in the civilian sector in all surgical specialties because it led to postponement or cancellation of many non-emergent surgical procedures. In conclusion, the use of RAS has continued to increase, and general surgery cases continue to constitute most of these cases. However, since the COVID-19 pandemic began, there was a significant decline in both DoD and civilian RAS cases, with a more pronounced decline in the DoD.
Keywords: da Vinci, Robotic assisted surgery, Coronavirus, Department of Defense
Introduction
The use of robotics in surgery started as an idea back in 1967 [1]. This idea became a reality 30 years later with the help of the Department of Defense (DoD) and the Defense Advanced Research Projects Agency (DARPA) [1]. Robotic assisted surgery (RAS) was originally intended for trauma surgery in the battlefield, and DARPA was able to conduct high-risk research and development for this purpose [1]. RAS has now become a standard in many hospitals in the United States for non-trauma-related surgery, with increasing volumes of cases performed annually [1]. One investigation concluded that increased visualization, dexterity, range-of-motion, and surgeon comfort in the minimally invasive surgical context is the reason for this increase in usage [2]. Although overall conclusions about the benefits of RAS and its advantages over unassisted laparoscopy are still unclear, papers have reported improved outcomes including decreased hospital length of stay, decreased wound complications, decreased post-operative pain, and a decreased time away from work when compared to conventional open approaches [3, 4]. The most commonly used RAS platform in the DoD and civilian surgical realms is the da Vinci robotic surgical system (Intuitive Surgical, Sunnyvale, California) [2]. A recent iteration of this system, the da Vinci Xi, released in 2014, improved robotic architecture, as it included a simplified docking procedure facilitated by laser targeting and improved cannula mounts, rotating boom-mounted arms, enhanced endoscopic visualization, greater range of motion, and longer instrument shafts. These improvements have made the da Vinci Xi popular amongst many surgical specialties. [2, 5]
The most recent update for the da Vinci robotic surgical system is the SP or single port system released in 2018. However, this SP device is currently approved only for urological procedures, radical tonsillectomy procedures, and tongue base resections, making its use limited in many surgical fields [6]. Recent preclinical studies looking at transanal total mesorectal excisions (taTME) with the da Vinci SP have shown promising results, demonstrating that more surgical procedures will likely be approved for use with a single-port RAS [6]. In the past 3 years, the number of civilian hospitals that are operating five or more da Vinci systems at a single campus has grown by more than 400% [7]. Intuitive Surgical has also branched out to countries outside of the United States, and these foreign countries have increased their overall annual da Vinci case volume over time similar to their American counterparts. [7]
The DoD military treatment facilities (MTFs), and its surgeons have continued to increase their use of RAS to provide the best, most up-to-date surgical care for their patients [2]. As surgeons become more comfortable and efficient with increasing case volumes, high-volume RAS demonstrates lower hospital length-of-stay and lower conversion rates, without an increase in total cost, complications, or readmissions [8]. With the improvement of surgeon comfort and skill with RAS, most MTFs now have at least one da Vinci model, while many have two or even three.
The surgical field has changed significantly since the arrival of the COVID-19 pandemic in the United States beginning in early 2020, as lockdowns were put in place and operating rooms were reserved only for emergent surgeries. Among various complications associated with COVID-19, multiple gastrointestinal (GI) complications have been reported [9]. In a single-center study, 184 patients with COVID-related acute respiratory distress syndrome (ARDS) were found to have higher rates of ileus (48 versus 22%), bowel ischemia (4 versus 0%), and elevated aminotransferase levels (55 versus 27%) compared to non-COVID-19-related ARDS patients, respectively. [9] It has also been found that there are high rates of post-operative pulmonary complications and mortality in surgical patients with COVID-19 [10]. An international study of 1,128 patients with COVID-19 undergoing a variety of surgical procedures demonstrated pulmonary complications in 51% of patients, and 30-day mortality was 38% [10]. Due to the increased risk in morbidity and mortality in COVID-19 patients, the rationing of surgical resources and personnel to assist with the pandemic, and the increased risk of exposure, elective surgical procedures, were halted across the United States during the COVID-19 pandemic [11]. Many of these elective surgical procedures were RAS.
It has been estimated that 28,404,603 operations were either canceled or postponed during 12 weeks of disruption due to COVID‐19, or 2,367,050 operations per week globally [11]. Even though most operations postponed would be for benign disease, many urgent surgeries such as operations for malignancy have also been postponed. In North America, is it estimated that 4,518,619 elective surgical procedures have been canceled secondary to COVID-19, including 4,156,253 operations for benign disease, 336,510 operations for malignancies, and 25,855 obstetric operations [11]. The decision to cancel elective surgeries has had a large impact on patients and healthcare systems worldwide [11]. Delaying elective operations caused a delay in patient care, leading to more difficult procedures with increased morbidity [11]. This impact has also been seen in the DoD, demonstrated by the decline in elective procedures, including RAS.
The primary endpoints of this review will include the evolution of RAS in the DoD since 01st October 2017, the prevalence in the DoD based on number of da Vinci consoles at a given facility, and the usage among practicing surgeons in each surgical specialty. Secondary outcomes will include a continued comparison with growth rate in the civilian sector, as well as the effect of coronavirus disease 2019 (COVID-19) on the use of RAS in the DoD.
Materials and methods
This study was reviewed and deemed exempt by our local Institutional Review Board (IRB). RAS data from the DoD data was obtained from “The Department of Defense Robotic Surgery Dashboard.” This database of information is managed by Ft. Detrick, MD, and it is published quarter-annually to DoD surgeons who are involved with RAS [2]. It includes information about RAS being performed at DoD institutions to include case volume for surgeon, specialty, and location. This information was used to address our primary endpoints as listed above. Inclusion criteria were any MTF performing RAS whose data was reported without interruption in the aforementioned dashboard. 10,759 RAS cases between 01 October 2017 and 31 December 2020 were examined, met criteria, and used for this study. Cases from all surgical specialties performing RAS were included. Comparable data about civilian RAS prevalence and trends were evaluated as secondary outcomes. A review of Quarter 1 (Q1, between 01 January 2020 and 31 March 2020), and Quarter 2 (Q2, between 01st April 2020 and 30th June 2020) was performed to determine COVID-19 impact on RAS use in the DoD. A review of Quarter 3 (Q3, between 01st July 2020 and 30th September 2020), and Quarter 4 (Q4, between 01st October 2020 and 31st December 2020) was performed to analyze the increase in RAS cases in the DoD as elective cases were gradually resumed.
Results
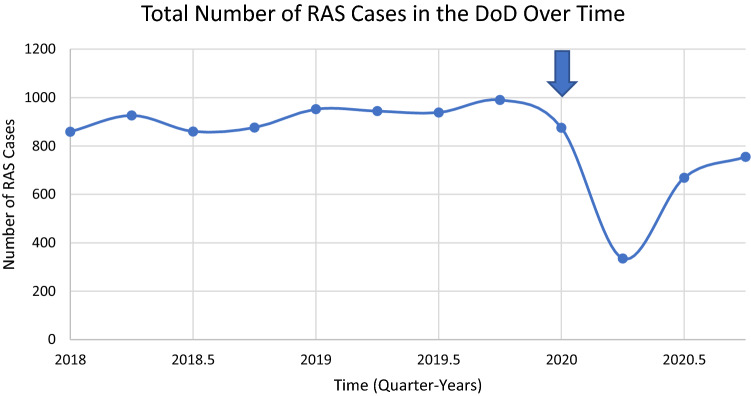
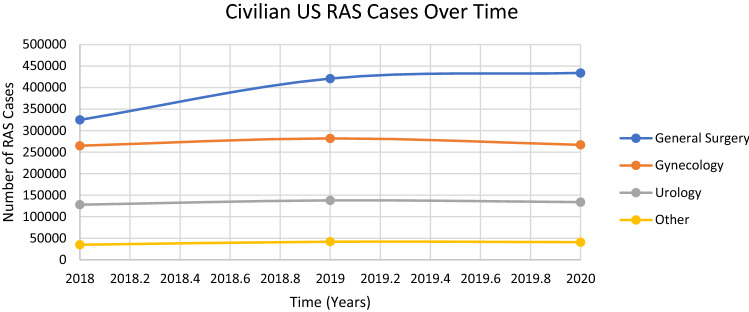
The number of RAS cases in the DoD continued to rise within the timeline examined in this study. There were 3712 cases performed in 2018, and 4117 cases performed in 2019, demonstrating a 10.91% increase in RAS use in the DoD. However, the COVID-19 pandemic led to most elective surgeries being postponed starting Q2 of 2020. As seen in Fig. 1, the number of RAS cases decreased from 875 to 335 cases. This decrease in an upward trend of RAS cases is also present in the civilian sector. Figure 2 demonstrates the slowing of RAS cases in the civilian sector once COVID-19 emerged, with some specialties seeing a decreasing trend in RAS cases secondary to COVID-19. Since the reopening of elective surgical procedures, the DoD has since seen an increase in RAS cases starting at Q3 2020. The number of cases increased from 335 during Q2 to 669 during Q3, and again to 755 during Q4. However, the total number of RAS cases in the DoD in 2020 was 2,634 cases, a decrease of 36.02% from 2019.
Fig. 1.
Number of RAS cases performed in the DoD, recorded quarter-annually. Arrow indicates start of COVID-19 pandemic
Fig. 2.
Number of civilian RAS cases performed annually in America by specialty
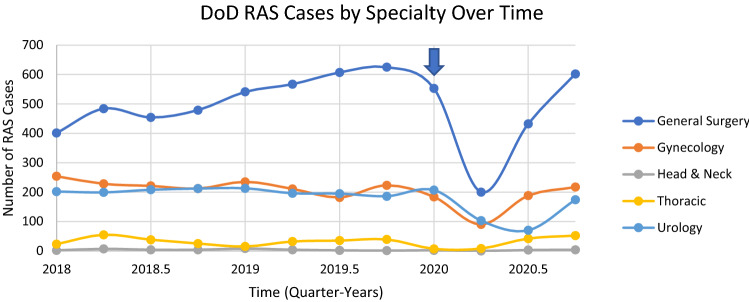
Data from DoD RAS cases by specialty can be seen in Fig. 3. General surgery continues to be the specialty that performs the most RAS in the DoD since Q4 2015. RAS use in DoD general surgery had an increase in use from 2018 to 2019 by 28.71%. Gynecology and urology show a similar trend and similar number of cases quarterly, as well as a drop in cases during the start of COVID-19. Thoracic and head and neck surgery show similar trends as well in relation to each other.
Fig. 3.
Number of RAS cases by specialty performed in the DoD, recorded quarter-annually. Arrow indicates start of COVID-19 pandemic
Since the introduction of RAS in MTFs, there were no additional MTFs or surgical specialties added to these data. These data have been extrapolated from the same MTFs and specialties since 2017. There are, on average, between three and four surgical specialties performing RAS at each MTF.
Civilian RAS use was retrieved from estimated annual case volumes reported by Intuitive Surgical. The total number of RAS cases in 2018 were 753,000, and 883,000 in 2019, demonstrating a 17.26% increase. The number of RAS cases in 2020 were 876,000, demonstrating a 0.79% decrease from 2019 amidst COVID-19.
Discussion
The use of RAS has continued to increase since the introduction of RAS in the DOD [2]. From 2015–2017, DoD surgeons saw an average 9.27% growth every quarter-year in the number of RAS cases [2]. From 2018-Q1 2020, DoD surgeons saw an average growth of 10.91% every quarter-year until the emergence of COVID-19. This increase in RAS included overall volume in the DoD and number of cases by specialty, addressing the primary and secondary endpoints of this paper. Of note, there were no new military treatment facilities (MTFs), or specialties added during those years.
The primary endpoint of this paper, the overall RAS volume increase in the DoD, can be attributed to many factors, including an increased number of available RAS devices in each MTF, increased surgeon confidence, and increasing patient interest in RAS. The 16 MTFs with RAS reviewed in this paper have at least one da Vinci device, six MTFs have two da Vinci devices, and one MTF has three da Vinci devices. These numbers do not include the External Resource Sharing Agreements (ERSAs) in which many DoD surgeons are involved with outside civilian hospitals [2]. ERSAs allow DoD healthcare personnel to provide medical services to soldiers and TRICARE (i.e., military health insurance) beneficiaries at outside hospitals in a network facility. This availability of RAS devices has allowed surgeons to perform more RAS than previous years, contributing to an increase in overall volume and surgeon confidence in performing RAS. Compared to the civilian sector, the use of RAS in the DoD increases at a slower rate, likely secondary to the number of civilian facilities that have access to RAS compared to the DoD MTFs. In the United States, 753,000 robotic procedures were performed in 2018, 883,000 in 2019, and 876,000 in 2020 [12]. When comparing these numbers to the yearly RAS cases in the DoD, the smaller population of surgeons in the DoD cannot produce the same number of cases as the civilian sector. The secondary endpoint of this paper, overall increase based on specialty, demonstrates that general surgery robotic procedures continue to represent the majority of DoD RAS. The increase in general surgery case percentages ranged from 17 to 45% from 2018 to 2019. The average percent change in the United States for general surgery procedures was 30% in 2019.
COVID-19 severely impacted the overall use and use amongst all specialties of RAS within the DoD and the civilian sector. Within the DoD, there was only a 2% increase in general surgery RAS during Q1 2020, and Q2 2020 saw a 65% decrease secondary to COVID-19. Gynecologic procedures saw a 22% decrease in RAS during Q1 2020 and a 57% decrease in RAS during Q2 2020. Urologic procedures similarly saw a decline in RAS in the DoD with a 3% decrease in RAS during Q1 2020 and a 47% decrease during Q2 2020. In the United States, general surgery saw a 30% increase in robotic procedures in 2019, and 6% decrease in 2020 [13]. Gynecologic procedures saw a 6% increase in robotic procedures in 2019, and no increase in 2020 [13]. Urologic procedures saw an 8% increase in robotic procedures in 2019, and a 3% decrease in 2020 [13]. In the DoD, the number of RAS cases increased from 335 during Q2 2020 to 669 cases during Q3 2020 and 755 during Q4 2020, demonstrating a 99.70% and 12.85% increase, respectively. With the emergency authorization of multiple COVID-19 vaccines, elective and RAS cases are expected to further increase.
A limitation in this study is that there is no data on non-military facility robotic procedure uses amongst DoD surgeons. This likely underestimates the number of cases performed by DoD surgeons in every specialty. DoD surgeons do not report their procedures outside of MTFs to the DoD, making it difficult to acquire these numbers. Another limitation of this study is that there is no separate civilian robotic usage data alone. The data included is the overall RAS usage in the United States, encompassing the DoD usage as well. This makes it difficult to analyze the trends between the two populations.
In conclusion, the use of RAS has continued to increase within the DoD through 2019, with general surgery cases constituting the majority of these cases [2]. During the initial beginning of the COVID-19 pandemic, there was a more significant decline in RAS cases in the DoD compared to the civilian sector. With the release of COVID-19 vaccines and improved COVID-19 testing, there has been an increase in RAS within the DoD and civilian sector. As seen in Fig. 1, the number of RAS cases in the DOD have increased in Q2 of 2020, with promise to continue this upward trend.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kayla Rizzo, DO. The first draft of the manuscript was written by Kayla Rizzo, DO and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors. This is an observational study. The William Beaumont Army Medical Center Research Ethics Committee has confirmed that no ethical approval is required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.George EI, Brand TC, LaPorta A, Marescaux J, Satava RM. Origins of robotic surgery: from skepticism to standard of care. J Soc Laparoendoscopic Surg. 2018 doi: 10.4293/JSLS.2018.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grasso S, Dilday J, Yoon B, Walker A, Ahnfeldt E. Status of Robotic-Assisted Surgery (RAS) in the Department of Defense (DoD) Military Med. 2019 doi: 10.1093/milmed/usz145. [DOI] [PubMed] [Google Scholar]
- 3.Arita NA, Nguyen MT, Nguyen DH, et al. Laparoscopic repair reduces incidence of surgical site infections for all ventral hernias. Surg Endosc. 2015 doi: 10.1007/s00464-014-3859-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsuda S, Oleynikov D, Gould J, et al. SAGES TAVAC safety and effectiveness analysis: da Vinci® Surgical System (Intuitive Surgical, Sunnyvale, CA) Surg Endosc. 2015 doi: 10.1007/s00464-015-4428-y. [DOI] [PubMed] [Google Scholar]
- 5.Ngu J, Tsang C, Koh D. The da Vinci Xi: a review of its capabilities, versatility, and potential role in robotic colorectal surgery. Robotic Surg Res Rev. 2017 doi: 10.2147/RSRR.S119317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kneist W, Stein H, Rheinwald M. Da Vinci Single-Port robot-assisted transanal mesorectal excision: a promising preclinical experience. Surg Endosc. 2020 doi: 10.1007/s00464-020-07444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Intuitive Surgical. Intuitive Surgical Annual Report 2019 (2019). Accessed 2 May 2021. https://isrg.gcs-web.com/static-files/31b5c428-1d95-4c01-9c85-a7293bac5e05
- 8.Rashidi L, Neighorn C, Bastawrous A. Outcome comparisons between high-volume robotic and laparoscopic surgeons in a large healthcare system. Am J Surg. 2017 doi: 10.1016/j.amjsurg.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 9.el Moheb M, Naar L, Christensen MA, et al. Gastrointestinal complications in critically ill patients with and without COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.19400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. The Lancet. 2020;396(10243):27–30. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Intuitive Surgical. Investor Overview.; 2021. Accessed 2 May 2021. http://investor.intuitivesurgical.com/?c=122359&p=irol-IRHome
- 13.Intuitive Surgical. Unaudited Preliminary Quarterly and Annual Revenue Data and Metrics.; 2020. Accessed 2 May 2021. https://isrg.intuitive.com/static-files/7b0470fb-cfd2-456a-b6eb-24af76d68f6d