Abstract
Severe mental illness could be defined through its diagnosis, disability, and duration, and one of their main characteristics is the high prevalence of some clinical conditions such as obesity and metabolic syndrome. Although the promotion of a healthier lifestyle has been demonstrated as an effective strategy to reduce both body mass index and abdominal circumference in this population, there is a lack of studies focusing on digital intervention in this population. The aim of this systematic review was to evaluate the efficacy of studies that used digital technologies to reduce weight, body mass index (BMI) and abdominal circumference in individuals with severe mental illness. This current review also compared remote and hybrid interventions, the effects of those interventions in metabolic biomarkers as well as in the development of a healthier lifestyle. The main findings included the following: (a) the use of digital devices or strategies might be feasible and useful to reduce sedentary behavior among individuals with severe mental illnesses, 2) most interventions used digital pedometers and mobile phone communication (either text messages or phone calls) as main strategies, 3) all remote interventions and six of nine hybrid interventions found significant outcomes in favor of their interventions. In conclusion, even with a limited number of studies promoting healthier lifestyle through digital interventions among individuals with severe mental illnesses, evidence from studies included in this review showed that they might be useful to improve a healthier lifestyle and increase the frequency of physical activity behavior.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11126-022-09994-3.
Keywords: Severe mental illness, Psychosocial intervention, Digital intervention, e-health, Weight loss, Sedentary behavior, Systematic review
Introduction
Severe mental illness could be defined through its diagnosis, disability, and duration, and includes schizophrenia spectrum disorders, schizoaffective disorders, bipolar disorders as well as other psychotic disorders. One of the main characteristics of those disorders is the high prevalence of clinical conditions such as obesity and metabolic syndrome as comorbidity, which increases the likelihood of cardiovascular morbidity [1, 2]. Moreover, the risk for premature death is higher in this group, shortening life expectancy by up to 30 years [3], particularly due to cardiovascular diseases. Moreover, individuals with severe mental illness are two to three times more likely to die from cardiovascular diseases when compared with general population [4, 5], and the risk of death is also higher to die from related diseases such as diabetes, acute myocardial infarction, and obesity [6, 7].
The development of metabolic syndrome and its negative consequences affect the quality of life of individuals with severe mental illness, which are associated with modified risk factors such as smoking, dietary habits, sedentary lifestyle, and obesity. Second-generation antipsychotic treatment, common among those individuals, also contributes to the development of metabolic syndrome [8, 9]. The promotion of a healthier lifestyle, through an increase in physical activity and the adoption of balanced and healthy dietary habits, has been demonstrated as an effective strategy to reduce both body mass index (BMI) and abdominal circumference in this population [10–13].
Some studies have demonstrated that either individual or group in face-to-face interventions focused on healthy lifestyles presented positive outcomes regarding weight loss and improvement of metabolic parameters among obese individuals with severe mental illnesses [14–18]. To diversify interventions and increase adherence to healthier lifestyles, digital technologies have been arising as a way to promote wider and more qualified access to mental healthcare services to individuals with severe mental health diseases [19, 20]. Some of the targets of those interventions include the increase of the frequency of physical activity and bodyweight reduction [21, 22].
Given the high prevalence of cardiovascular diseases and their effects on individuals with severe mental health diseases, and the rapid emerging of digital technologies, the current systematic review aims to evaluate the efficacy of studies that used digital technologies to reduce weight, body mass index (BMI) and abdominal circumference in individuals with severe mental illness. As secondary targets we also compared totally remote and hybrid interventions, their effects on metabolic biomarkers as well as on the development of a healthier lifestyle.
Method
A review was performed to investigate the efficacy of studies that used digital technologies to reduce weight, body mass index (BMI), metabolic parameters, and abdominal circumference in individuals with severe mental illnesses. All studies including either digital interventions, through mobile phone applications, pedometers or regular email, text message, or phone calls contact (named in this current review as remote interventions) and digital interventions associated with face-to-face strategies (named in this current article as hybrid interventions). Studies targeting lifestyle, behavioral, educational, or digital interventions to increase both weight loss and health behavior frequency were included. This review has been conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement guidelines [23], and was registered in PROSPERO database (registration number CRD42020191980 https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=191980).
Search Strategy
We systematically searched four electronic databases: PuBMed/ Medline, PsycINFO, EMBASE, and Web of Science. We performed the first search in March 2021, concluding the extraction in April 2021. Additional search and extraction were performed in May 2021. The search combined the following keywords and MeSH terms, adapted to the different databases cited: Schizophrenia OR Schizoaffective disorder OR Bipolar Disorder OR Serious Mental Illness OR Psychosis AND Psychoeducational Intervention (related search terms: Internet-based intervention, Intervention, Apps, Mobile application, Psychiatric Rehabilitation, Psychotherapy, Psychotherapy, Group, Cognitive Behavioral Therapy, Patient Education as Topic, Psychoeducation) AND Health Promotion (related search term: Obesity, Metabolic Syndrome, Inflammation). The excerpt of the search term is in the supplementary material (Supplementary Material 1).
Eligibility and Exclusion Criteria
The present review considered eligible articles those study of psychosocial interventions either remote or hybrid conducted among patients with serious mental illnesses, which reported outcomes related to obesity, metabolism, metabolic syndrome, and inflammation. The studies included were published until March 2021 and written in all languages. Additionally, a broad eligibility criterion was used to capture all potential studies, based on the PICO model described as follow: (a) population: severe mental disorder (e.g., bipolar disorder; schizophrenia; schizoaffective disorder; psychotic disorder); (b) intervention: all psychoeducational interventions using digital technologies; (c) control: there were no specific inclusion or exclusion criteria for a comparison group in the selected studies; (d) outcomes: related to obesity, metabolic syndrome, weight loss, and/ or health promotion. We included original full papers satisfying the following criteria: a) studies were included independent of size, publication date, and language, b) outpatients have to have criteria diagnosis for serious mental disorder; c) men and women aged between 18 and 65 years, d) psychosocial interventions defined as approaches included to modify behavior through psychoeducation intervention or digital technologies; e) aiming to decreased anthropometric measures (i.e., weight, BMI, waist or abdominal circumference), and f) improve health behavior, such as reduce sedentary behavior and improve physical activity. The exclusion criteria for participants in the studies included diagnoses of severe mental disorders due to medical diseases, medication/substances, brain injury, as well being in the acute phase of the disease.
Study Selection, Data Extraction and Analysis
All articles were imported into Mendeley (version 1.19.8), where they were screened independently by the first and second authors. During this first screening process, both researchers assessed all articles based on the titles and abstracts. Then, during the second screening process, both researchers independently read abstracts and full-texts and, if the latter were not available online, corresponding authors were contacted. Inconsistencies were resolved in consensus and checked with the third author. Finally, unclear articles and disagreements among researchers were discussed with supervisors.
We developed a form based on the objectives of the current review to extract the most relevant data. The extraction form contained the following information: article code, title, authors, DOI number, primary aim, country of data collection, sample size, the average age of participants (or any related information), study design, instruments/tools administered throughout the study, outcomes, limitations/ strengths, and conclusions. Following data extraction, qualitative analysis was also performed, to organize and summarize the evidence found.
Results
General Findings
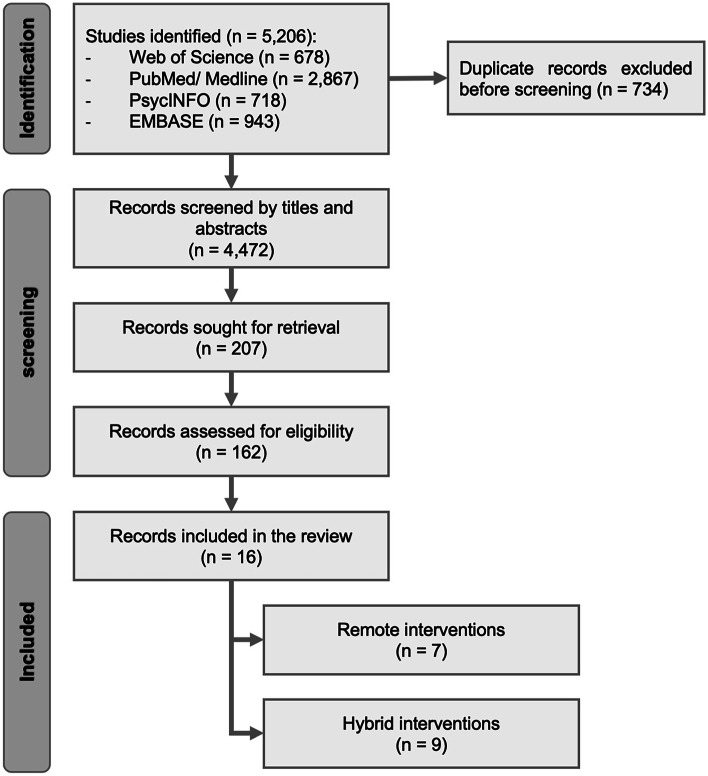
The initial research identified 5,206 articles. After the screening of titles and abstracts, 207 articles were obtained. In the end, after reading articles in full, sixteen studies were included in this current review, of which seven were digital interventions, through mobile phone applications, pedometers or regular email, text message, or phone calls contact, and nine were hybrid interventions, associating digital interventions with face-to-face strategies (see PRISMA Flowchart Diagram in Fig. 1).
Fig. 1.
PRISMA flow diagram
Remote Interventions
From the studies identified as a hybrid intervention, four of them were conducted in the United States, and one of each of the following countries: Sweden, Taiwan, and South Africa. Studies were published between 2013 and 2018, particularly in 2016 and 2017, when four of remote studies included in this review were published. Regarding research design, two studies were identified as randomized studies [24, 25], two as exploratory studies [26, 27], one as RCT [28], one as open-label study [29], and one as a pilot single-blinded [30].
The total number of participants in remote intervention studies was 739, an average of 105.6 participants per study. Sample sizes ranged from 15 [30] to 333 [29]. Regarding gender, there were more men than women in the total number of participants (respectively 55% and 45%), and four of seven studies reported more men than women in their sample.
None of the studies described the duration criteria adopted for intervention, which ranged from 8 weeks [28] to 48 weeks [29], while the most frequent intervention period was 24 weeks, reported by three studies [25–27]. Only Lee et al. [28] conducted a follow-up evaluation after one month of the end of the intervention.
Age means ranged from 37 [24] to 55.5 years of age [25]. However, age was not described homogeneously across studies. While some studies described the average age mean for the whole sample, others described the same information by study groups. One study did not report age means, but instead did by age groups [29]. In this study, most of the participants were from 20 to 49 years old (for each study see Table 1).
Table 1.
Characteristics of the remote intervention studies among severe mental disorders
| N | Article | Country | Sample (n)* | Diagnosis (n) |
Age (years) X̄ ± SD (min–max) |
Study design | Duration (weeks) | Follow-up (months) | Study outcomes |
|---|---|---|---|---|---|---|---|---|---|
| 01 | Chen et al. [30] | Taiwan |
15 A: 8 ** B: 7 |
- Schizophrenia (11) - Affective disorders (4) |
37.3 ± 10.8 A: 40.9 ± 9.9 B: 33.9 ± 11.4 |
Pilot single blinded | 12 | None |
- Daily steps using pedometer - Six-Minute Walk Test (6-MWT) - Short Form Health Survey 36 (SF-36) - Weight - BMI - Self-developed survey to measure the feasibility and usage frequency |
| 02 | Lee et al. [28] | United States |
22 Int: 12 Con: 10 |
- Schizophrenia spectrum - Bipolar disorder - Major depressive disorder*** |
44.1 ± 7.6 | RCT | 8 | 1 |
- Short-Form International Physical Activity Questionnaire (IPAQ) - Physical activity using pedometer - Abdominal circumference - BMI - Weight - Blood pressure - Laboratorial biomarkers (e.g., total cholesterol, low-density lipoprotein, high-density lipoprotein, and triglycerides, glucose, lipid profile) |
| 03 | Temmingh et al. [29] | South Africa | 333 |
- Bipolar disorder (259) - Schizophrenia spectrum disorders (102) - Unipolar mood disorder (84) - Other (33) |
- 18–29 (135) - 30–39 (229) - 40–49 (224) - More than 50 (173)**** |
Open-label study | 48 | None |
- Abdominal circumference - BMI - Weight - Blood pressure - Metabolic syndrome assessment - General health assessment (specific questionnaire) |
| 04 | Gyllensten and Forsberg [24] | Sweden |
73 Int: 43 Con: 30 |
- Schizophrenia (14) - Neuropsychiatric disorder (14) - Psychosis other (4) - Bipolar disorders (4) - Other diagnosis (9) - Non specified (28) |
Int: 38 Con: 37 |
Randomized study | 40 | None |
- Six-Minute Walk Test (6-MWT) - Abdominal circumference - BMI - Weight - Blood pressure - Short Form Health Survey 36 (SF-36) - Global assessment of Functioning (GAF) - Social interaction |
| 05 | Naslund et al. [27] | United States |
25 Int: 19& Con: 6 |
- Major depressive disorder (11) - Bipolar disorder (9) - Schizophrenia spectrum disorders (5) |
49.2 ± 11.8 Int: 50.5 ± 11.7 Con: 45.2 ± 12.1 |
Exploratory study | 24 | None |
- Facebook interactions - Six-Minute Walk Test (6-MWT) - Group attendance - Weight loss |
| 06 | Naslund et al. [26] | United States | 34 |
- Major depressive disorder (17) - Bipolar disorder (9) - Schizophrenia spectrum disorders (8) |
49.2 ± 11.8 | Exploratory study without control group | 24 | None |
- Daily steps using pedometer - Six-Minute Walk Test (6-MWT) - Weight |
| 07 | Young et al. [25] | United States |
237**** WebMOVE: 71 In person: 78 Con: 88 |
- Schizophrenia - Schizoaffective disorder - Bipolar Disorder - Major depressive disorder with psychosis - PTSD*** |
WebMOVE: 55.5 ± 9.2 MOVE SMI: 53.8 ± 10.1 Con: 54.2 ± 9.9 |
Randomized study with mixed methods | 24 | None |
- Weight - BMI - Brief qualitative interview |
Con Control/ usual care, Int Intervention, RCT Randomized control trial, SD Standard deviation, PTSD Post-traumatic stress disorder
* The whole sample size, as well as the number of participants allocated to each group, either intervention or control
** There were two different intervention groups, one-way and two-way messages, named respectively as A and B
*** Lee et al. [28] and Young et al. [25] did not report the exact number of participants according to psychiatric diagnosis
**** Young et al. [25] reported the number of participants for each age group instead of average age and SD. There were three different groups: one received face-to-face intervention (MOVE SMI), one received digital intervention (WebMOVE) and a third one usual care, identified as Con
The diagnostic profile of participants was also heterogeneous across studies. When studies were taken together, the most frequent diagnostic criteria was bipolar disorder with 281 participants, followed by schizophrenia (all subgroups), with 140 participants, and major depressive disorder and unipolar mood disorder, with 84 participants. The following diagnosis were also included in the studies: psychosis, PTSD, and schizoaffective disorders. One study did not specify the exact number of participants of each diagnoses [25], while 70 participants were described as other/ non-specified diagnosis.
Regarding study outcomes, most of the studies evaluated physical activity and metabolic measurements, as well as the overall quality of the intervention. Physical activity was measured by five studies, of which four of them used the Six-Minute Walk Test (6-MWT) [24, 26, 27, 30], three evaluated the frequency of physical activity through a pedometer [27, 28, 30], one used the Short-Form International Physical Activity Questionnaire (IPAQ) [28], and one used the Physical Activity Readiness Questionnaire (PAR-Q) [25]. Regarding metabolic parameters, six studies measured weight, five assessed BMI, three measured the abdominal circumference, three measured blood pressure, and one conducted a metabolic syndrome assessment. Metabolic biomarkers such as total cholesterol, low-density lipoprotein, high-density lipoprotein, and triglycerides, glucose, and lipid profile were assessed only by Lee et al. [28].
Interventions were also evaluated through self-developed questionnaires and brief interviews. Naslund et al. [27] measured Facebook’s interaction while Gyllensten and Forsberg [24] measured social interaction as an indicator of the success of the intervention. Quality of life and functionality was also assessed through Short Form Health Survey 36 (SF-36) by Chen et al. [30] and Gyllensten and Forsberg [24], and Global assessment of Functioning (GAF) by Gyllensten and Forsberg [24].
The frequency of physical exercise was the primary outcome in three studies [24, 28, 30], while BMI and weight was in one study each [25, 29]. The association between parameters of physical exercises, weight, and cardiovascular risk other parameters throughout the intervention was the primary outcome in two interventions [26, 27]. All studies identified better outcomes among intervention groups in comparison with control groups (or equivalents). However, there were only a few secondary outcomes with significant differences in both groups (see Table 2).
Table 2.
Summary of primary outcomes and secondary outcomes reported by remote intervention studies
| N | Article | Primary Outcome* | Secondary outcomes* |
|---|---|---|---|
| 01 | Chen et al. [30] |
↑ Physical activity (N = 15, p = 0.15, r = 0.39) |
= weight = BMI = quality of life = feasibility and usage frequency |
| 02 | Lee et al. [28] |
↑ Physical activity (N = 16, p = 0.11, r = 0.40) |
= Abdominal circumference = BMI = Weight = Blood pressure = Laboratorial biomarkers (e.g., total cholesterol, low-density lipoprotein, high-density lipoprotein, and triglycerides, glucose, lipid profile) |
| 03 | Temmingh et al. [29] |
↓ Weight (N = 467, logscale β = -0.0004705, p < 0.001) |
↓ BMI ↓ Abdominal circumference ↑ General health |
| 04 | Gyllensten and Forsberg [24] |
= Physical activity (N = 44, non-significant between and within groups)** |
= Blood pressure = Weight = BMI = Abdominal circumference = Quality of life = Social interaction = Functionality |
| 05 | Naslund et al. [27] | Association between cardiovascular risk reduction and weight loss and number of interactions in the Facebook group (respectively (N = 18, t = 2.12, p = 0.06, and N = 19, t = -2.26, p = 0.06) | No significant association between improved fitness and number of interactions in the Facebook group |
| 06 | Naslund et al. [26] | Higher daily step count was significantly associated with greater weight loss (N = 34, F = 5.07, df = 1.32, p = 0.0314) | Daily step count was significantly associated with fitness change (N = 34, F = 1.92, df = 1.31, p = 0.176) |
| 07 | Young et al. [25] | ↓ BMI in WebMOVE (t = 3.3, p = 0.001) compared with either in-person (t = 0.10, p = 0.92) or usual care (t = − 0.25, p = 0.80) | Feasibility and acceptability of the intervention was well received |
N number of participants who completed intervention in each study, r calculation of effect size, r, by dividing the z value by the square root of N (the number of total observations or sample)
*Comparison between intervention group (or equivalent) and control group after the end of intervention (or follow-up assessment)
** p-values were not reported in the study
Due to the heterogeneity of primary and secondary outcomes, as well as statistical analyses performed, direct comparisons between studies were not possible. Studies with small sample sizes, such as Chen et al. [30], Lee et al. [28], Gyllensten and Forsberg [24], and Naslund et al. [27] did not find significant differences between intervention groups and control groups (or equivalents) and withing groups. Chen et al. [30] and Lee et al. [28] only reported statistical significance outcomes between groups only for primary outcomes and withing groups for secondary outcomes. Comparisons between groups for primary outcomes at the end of both interventions were not significant (respectively p = 0.15 and p = 0.11), but medium effect sizes were noted at the end of both interventions (respectively r = 0.39 and r = 0.40). Studies conducted by Gyllensten and Forsberg [24], Naslund et al. [26], and Naslund et al. [27] also preseted a small sample size (respectively 44, 34, and 25). The first one did not find significant differences between groups or within groups, and also did not reported p-values. The latter two studies found significant associations between daily steps and weight loss (F = 5.07, df = 1.32, p = 0.0314) and number of interactions in the intervention and both weight loss and cardiovascular risk reduction (respectively t = -2.26, p = 0.06 and t = 2.12, p = 0.06). Finally, studies with a larger sample size found significant outcomes for weight reduction, BMI, and general health. In the study conducted by Temmingh et al. [29], 467 participants conclude the intervention, and mixed regression models over time demonstrated a significant reduction in weight (logscale β = -0.000471, p < 0.001), BMI (logscale β = 0.000460, p < 0.001) and improved general health (logscale β = 0.00674, p < 0.001). Young et al. [25] conducted their study with 237 participants and found substantial change in BMI among participants who received the digital intervention (t = 3.3, p = 0.001), in comparison with either in person intervention (t = 0.10, p = 0.92) or usual care (t = − 0.25, p = 0.80; see Table 2).
Hybrid Interventions
From the studies identified as a hybrid intervention, six of them were conducted in the United States, two in England, and one in the Netherlands, and were published from 2010 and 2019. Most of studies included in this review were published from 2016 onwards, showing an increase in the number of studies published over the years. Regarding research design, five studies could be identified as randomized control trials, of which one was described by authors as a pilot randomized control trial study [31] and one as a cluster randomized control trial study [32]. Three studies were described as pilot trials [33–35], and one study as a randomized pre- and pots-test study [11].
The total number of participants in all hybrid studies included in this current review was 1,145, an average of 127 participants. However, sample sizes ranged from 13 to 412 across studies. Regarding gender, there were more women than men in the total number of participants (respectively 55.19% and 44.81%), but the latter group was more predominately in four of nine studies.
Like remote studies, none of the hybrid interventions described the duration criteria adopted for intervention, which ranged from 10 weeks [35] to 52 weeks [36, 37]. As identified among remote intervention studies, the most frequent intervention period for hybrid interventions was 24 weeks, reported by three studies [33–35]. There were also interventions lasted 17 weeks [31] and 48 weeks [32, 38]. From the nine studies, one of them conducted a follow-up evaluation after one month [35], and two studies conducted the follow-up after six months of the end of the study [11, 31], and two studies conducted two follow-up evaluations, after 6 and 12 months of the end of the intervention [11, 32].
Information regarding age was described heterogeneously across studies. Some studies described the average age and its standard deviation in the whole sample while the other described both information in each group. One study reported only the average age, as well as minimum and maximum age of participants, making it impossible to compare this piece of information among studies (for each study see Table 3).
Table 3.
Characteristics of the hybrid intervention studies among severe mental disorders
| N | Article | Country | Sample (n)* | Diagnosis (n) |
Age (years) X̄ ± SD |
Study design | Duration (weeks) | Follow-up (months) | Study outcomes |
|---|---|---|---|---|---|---|---|---|---|
| 01 | McKibbin et al. [11] | United States |
52** Int: 26 Con: 26 |
- Schizophrenia (42) - Schizoaffective disorder (10) |
Int: 52.4 ± 8.6 Con: 55.6 ± 8.7 |
Randomized pre-test, post-test control group | 24 | 6 and 12 |
- Positive and Negative Syndrome Scale (PANSS) - Hamilton Depression Rating Scale (HAM-D) - Mattis' Dementia Rating Scale (DRS) - Energy expenditure - Diabetes knowledge - BMI - Abdominal circumference - Glycated hemoglobin |
| 02 | Brown et al. [36] | United States |
136 Int: 70 Con: 66 |
- Serious mental disorder (136) |
Int: 44.4 ± 11.7 Con: 44.9 ± 10.1 |
RCT | 52 | None |
- 24 item Brief Psychiatric Rating Scale - Physical activity measured by accelerometer - Weight |
| 03 | Green et al. [37] | United States |
200 Int: 104 Con: 96 |
- Schizophrenia and spectrum (58) - Bipolar or affective disorder with psychosis (138) - PSTD (4) |
47.2 ± 10.6 Int: 46.2 ± 11.4 Con: 48.3 ± 9.7 |
RCT | 52 | None |
- Modified Colorado Symptom Index (CSI) - Behavior and Symptom Identification Scale 24 (BASIS-24) - Short Form Health Survey 36 (SF-36v2) - Weight - BMI - Metabolic syndrome - Laboratorial parameters (e.g., lipidic profile, glycated hemoglobin, serum glucose) |
| 04 | Browne et al. [35] | United States | 16 |
- Schizophrenia (5) - Schizoaffective disorder (10) - Psychotic syndrome without specification (1) |
43.3 ± 7.8 | Pilot study | 10 | 1 |
- Positive and Negative Syndrome Scale (PANSS) - Multidimensional Scale of Perceived Social Support (MSPSS) - The World Health Organization Quality of Life Scale (WHOQoL-bref) - Physical Activity Readiness Questionnaire (PAR-Q) - Short Form International Physical Activity Questionnaire (IPAQ) - Six-Minute Walk Test (6-MWT) - Short Form Health Survey 36 (SF-36) - Client Satisfaction Questionnaire (CSQ-8) - Weight - BMI - Blood pressure |
| 05 | Aschbrenner et al. [33] | United States | 13 |
- Schizophrenia (3) - Major depressive disorder (7) - Bipolar disorder (3) |
48.8 ± 10.6 | Pilot trial | 24 | 6 |
- Six-Minute Walk Test (6-MWT) - Adapted participant attendance and satisfaction questionnaire - Weight |
| 06 | Aschbrenner et al. [34] | United States | 32 |
- Schizophrenia spectrum(7) - Major depressive disorder (14) - Bipolar disorder (11) |
48.8 ± 11.9 | Intervention Pilot study | 24 | none |
- Six-Minute Walk Test (6-MWT) - 10-item Social Provisions Scale - Weight - BMI |
| 07 | Holt et al. [38] | England |
412 Int: 208 Con: 206 |
- Schizophrenia (283) - Schizoaffective disorder (66) - First psychotic episode (63) |
Int: 40.0 ± 11.3 Con: 40.1 ± 11.5 |
RCT | 48 | 12 |
- Adapted Dietary Instrumentfor Nutrition Education questionnaire - Short Form Health Survey 36 (SF-36) - EuroQol- 5 Dimension (EQ-5D-5L) - Brief Psychiatric Rating Scale - 9-item Patient Health Questionnaire - Weight - Medical history - Abdominal circumference - Blood pressure - Physical activity measured by accelerometer - Laboratorial parameters (e.g., lipidic profile, glycated hemoglobin, serum glucose) |
| 08 | Looijmans et al. [32] | Netherlands |
244 Int: 140 Con: 104 |
Psychotic syndrome (140) - Mood disorder (68) - Personality disorder (64) - Anxious disorder (33) - Psychiatric comorbidities (75) |
46.1 ± 10.8 Int: 44.3 ± 10.9 Con: 48.6 ± 10.2 |
Cluster RCT | 48 | 6 and 12 |
- Waist circumference - BMI - Metabolic syndrome parameters - Blood pressure - Laboratorial biomarkers (e.g., lipidic profile, glycated hemoglobin) |
| 09 | Williams et al. [31] | England |
40 Int: 20 Con: 20 |
- Schizophrenia (22) - Bipolar disorder (5) - Psychotic disorder (3) - Other (10) |
43 (20–56 anos) | Pilot RCT | 17 | 6 |
- Acceptability, feasibility and recruitment rates - Physical activity measured by accelerometer - Laboratory biomarkers (total cholesterol, high density lipoprotein, low density lipoprotein and triglycerides, high sensitivity C reactive protein, insulin levels and blood glucose levels) - Blood pressure - Weight - Waist circumference - Metabolic Syndrome parameters |
Con Control/ usual care, Int Intervention, RCT Randomized control trial, SD Standard deviation, PTSD Post-traumatic stress disorder
* The whole sample size, as well as the number of participants allocated to each group, either intervention or control
** 52 participants completed the follow-up evaluation and were included in the study. The original sample size was 64 participants
As identified across remote interventions, the diagnostic profile of participants was also heterogeneous across studies. Each study has different inclusion and exclusion criteria such as current medication and a large range of diagnostic criteria according to DSM. When studies were taken together, the most frequent diagnoses was schizophrenia with 420 participants, followed by bipolar and mood disorders with 225 participants. There were also 144 participants with psychotic disorders, 86 participants with schizoaffective disorder, 63 participants identified with first-episode psychosis, 63 participants diagnosed with major depressive disorder, and 21 with other psychiatric disorders (e.g., personality disorders, anxiety disorders, post-traumatic stress disorder, and other psychiatric comorbidities). It is important to highlight that some studies included schizoaffective disorders as part of the schizophrenia spectrum while others included it as a separated category. One study did not specify each diagnostic, identifying all sample as generically as individuals with severe mental disorder [36].
Regarding study outcomes, the following studies measured symptoms severity, throughout different measurements, such as Positive and Negative Syndrome Scale (PANSS) [11, 35], Hamilton Depression Rating Scale (HAM-D) [11], 9-item Patient Health Questionnaire [38], 24 item Brief Psychiatric Rating Scale [36, 38], Modified Colorado Symptom Index (CSI) [37], and Behavior and Symptom Identification Scale 24 (BASIS-2) [37]. Cognitive symptoms were measured by McKibbin et al. [11] through Mattis' Dementia Rating Scale (DRS), whereas functionality was also measured through BASIS-24 [37]. Well-being and functionality were measured by Browne et al. [35], Green et al. [37], and Holt et al. [38] through Short Form Health Survey 36 (SF-36). Browne et al. [35] measured quality of life through the abbreviated version of the World Health Organization quality of life Scale (WHOQoL-bref), while Holt et al. [38] measured quality of life using the EuroQol- 5 Dimension (EQ-5D-5L).
Social support was evaluated in two interventions, using the following measurements: 10-item Social Provisions Scale in the study conducted by Aschbrenner et al. [34] and Multidimensional Scale of Perceived Social Support (MSPSS) in the study conducted by Browne et al. [35]. Brief Illness Perception Questionnaire was assessed only by Holt et al. [38]. Satisfaction with the intervention was assessed by Browne et al. [35] and Aschbrenner et al. [33], respectively using the Client Satisfaction Questionnaire (CSQ-8) and an adapted participant satisfaction questionnaire (See Table 3).
Among hybrid interventions, weight was the primary outcome in five hybrid intervention studies, BMI and physical activity in two studies each, and acceptability, feasibility, and recruitment rates, and waist circumference in one study each. Browne et al. [35] also included as primary outcome social support, activity level, and mental health parameters. Physical activity, weight, blood pressure, lifestyle behaviors, and laboratory parameters were also investigated as secondary outcomes (Table 3).
Similarly to remote interventions, there were a large heterogeneity among hybrid interventions, regarding primary and secondary outcomes, as well as statistical analyses. Due to this, direct comparisons between studies were not possible. Regarding main outcomes, Browne et al. [35] did not perform inferential statistical analysis and only reported effects sizes of both primary and secondary outcomes. They small and medium effect sizes for physical activity, social and mental health domains either at the end of the intervention or follow-up assessments. Only one of the domains accessed for activity levels presented also presented large effect sizes. In the study conducted by Aschbrenner et al. [34], 25 participants concluded the intervention and weight reduction was significative at the end of the intervention (t = 3.13, df = 24, p = 0.005). The association between weight and peer group support was also significative (r(24) = 0.59, p = 0.002). Williams et al. [31], even with a small sample size (N = 21), also found significative change in sedentary behavior in their study (p = 0.018).
Studies with a larger sample size found significant outcomes for their primary and secondary outcomes. In McKibbin et al. study, 52 participants were assessed at the end of the intervention, and mixed model analysis showed changes in BMI (F(1,50) = 10.40, p < 0.01), waist circumference (F(1,50) = 6.6, p < 0.05), and diabetes knowlegde (F(1,50) = 10.86, p < 0.01) at the end of the intervention [11]. Brown et al. [36] also conducted mixed model analysis and found interaction effects with differences for intervention and control groups at the end of the intervention period (F = 6.936, p = 0.01), but not at the end of 12-months follow-up (F = 0.522, p = 0.47). Green et al. [37] found time by group effect for weight at 6-months (F = 11.9, df = 1,171, p = 0.001) and 12-months (F = 4.9, df = β = 1,161, p = 0.03). Looijmans et al. [32] did not found differences for waist circumference (N = 238, 2.26, p = 0.45), BMI (N = 240, β = 1.47, p = 0.08), and metabolic syndrome (N = 115, β = -0.10, p = 0.63). Holt et al. [38] conducted their study with 340 participants and also did not found significant outcomes for weight change (p = 0.963; Table 4).
Table 4.
Summary of primary and second outcomes reported by hybrid intervention studies
| N | Article | Primary Outcome* | Secondary outcomes* |
|---|---|---|---|
| 01 | McKibbin et al. [11] |
↓ BMI (N = 52, F(1,50) = 10.40, p < 0.01) ↓ Abdominal circumference (N = 52, F(1,50) = 6.60, p < 0.05) |
↓ Diabetes knowledge = Glycated hemoglobin = Energy expendidure |
| 02 | Brown et al. [36] | ↓ Weight between groups at the end of intervention period (N = 92, F = 6.936, p = 0.01), but not at 6 (F = 1.527, p = 0.22) or 12 months (F = 0.522, p = 0.47) | ↓ Weight between settings |
| 03 | Green et al. [37] |
↓ Weight Baseline to 6-months (N = 178, F = 11.9, df = 1,171, p = 0.001) Baseline to 6-months (N = 168, F = 4.9, df = 1,161, p = 0.03) |
↓ Glucose = Insulin = Blood pressure = Triglycerides = LDL = HDL |
| 04 | Browne et al. [35]** |
↑ Physical health (N = 16, Posttest: d = 0.39; follow-up: d = 0.30)**** ↑ Activity level (N = 16, Posttest: d = from 0.33 to 3.19; follow-up: d = from 0.02 to 1.36) ↑ Social support (N = 16, Posttest: d = 0.11; follow-up: d = 0.25) ↑ Mental health (N = 16, Posttest: d = from -0.06 to 0.72; follow-up: d = from 0.00 to 0.41) |
= BMI = Weight = Systolic blood pressure = Diastolic blood pressure = Resting heart rate ↑ pedometer adherence among intervention group Moderate to high levels of acceptability High levels of satisfaction with reporting daily steps |
| 05 | Aschbrenner et al. [33] | = Weight and Physical activity (N = 13) |
↑ Attendance ↑ Satisfaction ↓ Cardiovascular risk |
| 06 | Aschbrenner et al. [34] | ↓ Weight (N = 25, t = 3.13, df = 24, p = 0.005) |
= cardiovascular risk ↑ Participants’ perceptions of peer group support and ↓ weight |
| 07 | Holt et al. [38] | = Weight (N = 340, p = 0.963) |
= Dietary habits = Smoking habits = Quality of life = Obesity perception = Psychiatric symptoms = Abdominal circumference ↑ Physical activity |
| 08 | Looijmans et al. [32] | = Waist circumference (N = 238, β = 2.26, p = 0.45) |
= Metabolic syndrome = BMI |
| 01 | Williams et al. [31] | ↑ acceptability, feasibility, and recruitment rates |
= Sedentary behavior = Blood pressure ↓ Metabolic syndrome |
*Comparison between intervention group (or equivalent) and control group after the end of intervention (or follow-up assessment)
** Given the small sample size and nature of the pilot study, formal inferential statistics are not appropriate, within-group effect sizes for continuous outcome variables were computed to evaluate the magnitude of pre-post and follow-up
**** Effect sizes were calculated by dividing the mean difference (baseline to posttest and baseline to follow-up) by the baseline standard deviation, and evaluated as ranges small (d = 0.20), medium (d = 0.50), and large (d = 0.80)
Discussion
This current review shows that the use of digital devices and strategies, such as pedometers, phone calls, and social media might be feasible, valid, and useful to reduce sedentary behavior and increase the frequency of physical activity. They also might be useful and valid to improve general health parameters, such as weight, BMI, abdominal circumference, as well as cardiovascular conditioning. The positive correlation trend between psychosocial intervention strategies and clinical outcomes was described by Speyer et al. [39] in a recent meta-analysis evaluating the effect of face-to-face interventions focused on lifestyle among individuals with severe mental illnesses. In general, psychosocial interventions have several limitations related to both low adherence and high drop-out rates, and loss to follow-up, which sometimes are not well described in the literature [40]. Even with those limitations, face-to-face interventions are useful to improve changes in lifestyle among this population, impacting a longer life expectancy.
Moreover, it is important to point out how intervention studies have been evolving over the years, particularly in the last decade. As described earlier, most of studies included in this review were published from 2016 onwards, showing the increasing number of interventions utilizing digital technologies. We believe that the number of published studies will rapidly increase in coming years, particularly due to the conditions imposed by COVID-19 pandemic [41, 42].
All remote as well as hybrid intervention studies included in this current review are considered as inclusion criteria schizophrenia spectrum disorders, bipolar disorder, neuropsychiatric disorders, as well as psychotic disorder, usually identified by authors as severe mental disorders. However, those studies also included diagnostic profiles beyond those identified as severe mental illnesses, due to the fact that their intervention were conducted in mental health center, where a broad range of mental disorder patients receive mental health support, such as war veterans diagnosed with post-traumatic stress disorder, or individuals with depressive disorders [43], making difficult either to split different groups or separate them different groups to include in the study.
Regarding intervention strategies, most studies among remote interventions used digital pedometers, as well as mobile phone communication (either text messages or phone calls) as main strategies to conduct their intervention. Similarly, pedometers [11, 31] and mobile phone communication [11, 31, 34, 36–38] were also frequent among hybrid interventions, showing the importance of those strategies in psychosocial interventions focusing on lifestyle interventions. Additionally, one study developed a smartphone application aiming to motivate and monitor participants [34] while a second one evaluated a private Facebook group [33]. According to the authors, high levels of satisfaction and acceptability among participants were found, hypothesizing that the first strategy provided real feedback to both participants and researchers regarding physical exercises progress, while the second motivate them to keep the routine proposed in the intervention groups.
Regarding outcomes related to the main outcomes of this review, among remote studies, all studies found significative outcomes in favor of their intervention, specifically when primary outcome is considered. Similarly, among hybrid studies, six of them showed positive outcomes in favor of their interventions [11, 34–38]. Regarding BMI, from six hybrid interventions investigating this variable, five of them reported significant outcomes [26, 32, 33, 35, 37, 38]. One of the remote intervention studies investigated BMI as secondary outcome, also showing a significative reduction [29]. Only one hybrid intervention found an increase in BMI among participants included in the Diabetes Awareness and Rehabilitation Training (DART) [11]. Those outcomes demonstrate that either remote or hybrid shows the advantage of hybrid interventions to improve quality of life and healthier lifestyle as well as to lose weight.
When comparisons were made between hybrid and remote intervention, it is possible to hypothesize that remote interventions displayed better outcomes in comparison with totally hybrid interventions. However, remote interventions presented larger sample sizes and more robust statistical analysis when compared with hybrid interventions, as described in “Results” section. Moreover, when we compare our outcomes with those reported by Speyer et al. [39] in their meta-analysis, it is possible to conclude that usual face-to-face interventions presented limited clinical relevance with unconclusive outcomes, regarding diet and exercises interventions. One possible explanation would be related to patients’ characteristics. Usually, patients who receive digital interventions might presented better socioeconomic conditions, educational level, and ability to interact and complete tasks using electronic devices, such as smartphones or personal computer, when compared with those who are likely to looking for in-person support.
Strengths and Limitations of the Study
Some strengths of this current review need to be taken into account. The first one is the fact that it was conceived, developed, and concluded during the COVID-19 pandemic, in which physical social distancing was imposed as a way to stop or minimize the spread of the virus. In this context, digital technologies have popularly emerged as an alternative to keep providing healthcare services. Although mHealth studies have been conducted over the last years, it was during pandemic that it became popular, and several professionals adopted as main strategy to keep healthcare services. Telehealth medicine needed to quickly meet the demands of patients in quarantine and proved an effective way to implement mental health services in people with severe mental illnesses [41, 42]. A recent rapid meta-review investigating how digital interventions mitigated negative impacts of the COVID-19 pandemic on mental health identified good evidence on the usability, safety, acceptance, and effectiveness of those sort of interventions to treat and prevent mental health disorders [44]. However, ever with quick development, particularly during COVID-19 outbreak, there are a lot of patients who did not have access to either internet connections or mHealth technologies, including developed countries, such as the United States [45]. As demonstrated in this current review, digital technologies have been proved as important adjunctive strategies to improve the overall quality of life and minimize the impact of metabolic and cardiovascular comorbidities among patients with severe mental illnesses. In this way, it is important to develop a larger number of digital technologies to offer more mHealth services [30].
A second important strength of this study was the full following of PRISMA guidelines statement, proposed to improve the transparency and the merit of a reported review. Additionally, it is important to highlight that the whole data extraction and selection throughout the was conducted paired by blinded reviewers, and disagreements were discussed by a third author [23]. It was also discussed with supervisors, as reported in the metho section. Thirdly, this current review provides a detailed description of the method used in the interventions which used digital technologies in individuals with severe mental illness, providing a clear overview of each intervention, as well main outcomes. Finally, all studies included in this review were published from 2010 onwards, particularly in the last five years, showing that this is an updated field of study.
However, several limitations were identified, such as the heterogeneity among methods and strategies used for each intervention study, such as the duration of the intervention, strategies, and measurements, which were described in the results section. This fact restrains a more complete comparison between studies, as well as the conduction of a meta-analysis. Secondly, to our knowledge, there is no published remote or hybrid intervention published in Brazil, the country of this research group, and from all studies included in the review, there is only one published in a non-developed country [29]. This fact does not enable the generalization of the outcomes found in those studies to different populations and cultures, particularly in those without access to an internet connection, technological devices, as well as continuous healthcare services. In general, there is a lack of resources in low- and middle-income countries, particularly related to access to public healthcare and social services, making telepsychiatry services an interesting alternative to provide mental health services to the general population [46]. In this way, we suggest further studies investigating the impact and feasibility of telepsychiatry services in those contexts. Finally, an important limitation is related to the studies included in the review. In general, most of the studies had a limited sample size, did not have a control group, or were only described as a pilot study, which does not enable accurate predictions or assumptions, reduces the statistical power of the intervention, and increases the margin of error.
Conclusion
To our knowledge, this is the first review study investigating either remote or hybrid psychosocial interventions (either exclusively remote or hybrid), reporting an analytical description of the most recent evidence of this kind of intervention as an adjunctive treatment for individuals with severe mental illnesses. In general, those patients have a 10 to 20 years shorter life expectancy in comparison with the general population [47], particularly due to cardiovascular diseases, metabolic syndrome, and type 2 diabetes [48]. A recent global meta-analysis showed that individuals with severe mental illnesses are less likely to follow recommendations related to health, lifestyle, and physical activity in comparison with individuals without mental illnesses diagnoses, particularly more vigorous activities [49]. Although there are several studies describing the benefices of lifestyle interventions for obesity and overweight among individuals with severe mental illnesses, most of them focused exclusively on face-to-face interventions [50, 51], showing the need of a larger number of studies focusing on digital interventions for this population.
Supplementary Information
Below is the link to the electronic supplementary material.
Robson Zazula
is an Assistant Professor in Medical School of Federal University of Latin American Integration (UNILA) in Foz do Iguacu, Parana, Brazil. He received a Bachelor of Psychology in 2008, master’s degree in Behavior Analysis in 2011 and PhD in Health Sciences in 2019 from State University of Londrina. Between 2016 and 2017 he completed graduate studies in Health Professions Education at FAIMER-Brazil (Foundation for Advancement of International Medical Education and Research) in association with Federal University of Ceara, Fortaleza, Brazil. From 2016 to 2019 he was a doctoral student from Health Science Graduate Program at the same university, undertaking a research project titled “The assessment of cognitive dysfunction in unipolar and bipolar patients” under the supervision of Dr. Sandra Odebrecht Vargas Nunes. He worked with bipolar and depressed patients in other fields as well as smoking cessation groups and interventions. He was also a visiting researcher at IMPACT SRC, Deakin University from August 2018 to July 2019. Between 2008 and 2012 he works as a Clinical Psychologist in different settings. There, he gained valuable experience in mental and behavioral interventions as well as Behavior Analytic principles in the assessment and treatment of mental patients. During this period, he concluded his master’s degree in Behavior Analysis and started to work as a lecturer in a private psychology school. Between 2012 and 2014 he worked as an Educational Psychologist in a Federal School with teenagers. Since 2014 he has worked at UNILA as a lecturer of Medical Psychology and Communication for first term students At the School of Medicine as well as a lecturer and a supervisor for Mental Health in medical internship. Since 2020 he has been researching the association between epigenetics, human development and early adverse experiences, as well as investigating digital technologies and digital psychosocial interventions for individuals with severe mental illnesses. He has experience as a researcher in psychological and behavioral assessment, medical and health psychology and counseling. Education: PhD. (Health Sciences), State University of Londrina, Londrina, Parana, Brazil, 2016–2019. Graduate Study, Foundation for Advancement of International Medical Education and Research, Fortaleza, Brazil, 2017. MSc. (Behavior Analysis), State University of Londrina, Londrina, Parana, Brazil, 2011. B.S. (Psychology), State University of Londrina, Londrina, Parana, Brazil, 2008. Research Interests and Projects: Mood disorders and Mental Health, Smoking cessation, Behavioral and Psychological Assessment, Medical and Health Psychology, Epigenetics, Behavioral interventions.
Declarations
Informed Consent
Not applicable.
Research Involving Human Participants and/or Animals
Not applicable.
Disclosure of Potential Conflicts of Interest
On behalf of all authors, I certify that we have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Daumit GL, Dalcin AT, Dickerson FB, Miller ER, Evins AE, Cather C, et al. Effect of a comprehensive cardiovascular risk reduction intervention in persons with serious mental illness: a randomized clinical trial. JAMA Netw Open. 2020;3:e207247–e207247. doi: 10.1001/JAMANETWORKOPEN.2020.7247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen DAN, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52–77. doi: 10.1002/J.2051-5545.2011.TB00014.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295–301. doi: 10.1016/S2215-0366(17)30078-0. [DOI] [PubMed] [Google Scholar]
- 4.Das-Munshi J, Chang CK, Dutta R, Morgan C, Nazroo J, Stewart R, et al. Ethnicity and excess mortality in severe mental illness: a cohort study. Lancet Psychiatry. 2017;4:389–399. doi: 10.1016/S2215-0366(17)30097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu NH, Daumit GL, Dua T, Aquila R, Charlson F, Cuijpers P, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16:30–40. doi: 10.1002/WPS.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Penninx BWJH, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neurosci. 2018;20:63–73. 10.31887/DCNS.2018.20.1/BPENNINX. [DOI] [PMC free article] [PubMed]
- 7.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72:334–341. doi: 10.1001/JAMAPSYCHIATRY.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartels SJ, Aschbrenner KA, Pratt SI, Naslund JA, Scherer EA, Zubkoff L, et al. Implementation of a lifestyle intervention for people with serious mental illness in state-funded mental health centers. Psychiatr Serv. 2018;69:664–670. doi: 10.1176/APPI.PS.201700368/ASSET/IMAGES/LARGE/APPI.PS.201700368F1.JPEG. [DOI] [PubMed] [Google Scholar]
- 9.Fernández Guijarro S, Pomarol-Clotet E, Rubio Muñoz MC, Miguel García C, Egea López E, Fernández Guijarro R, et al. Effectiveness of a community-based nurse-led lifestyle-modification intervention for people with serious mental illness and metabolic syndrome. Int J Ment Health Nurs. 2019;28:1328–1337. doi: 10.1111/INM.12644. [DOI] [PubMed] [Google Scholar]
- 10.Blomqvist M, Ivarsson A, Carlsson IM, Sandgren A, Jormfeldt H. Health effects of an individualized lifestyle intervention for people with psychotic disorders in psychiatric outpatient services: a two year follow-up. Issues Ment Health Nurs. 2019;40:839–850. doi: 10.1080/01612840.2019.1642425. [DOI] [PubMed] [Google Scholar]
- 11.McKibbin CL, Golshan S, Griver K, Kitchen K, Wykes TL. A healthy lifestyle intervention for middle-aged and older schizophrenia patients with diabetes mellitus: a 6-month follow-up analysis. Schizophr Res. 2010;121:203–206. doi: 10.1016/J.SCHRES.2009.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muralidharan A, Karel MJ. Interest group session - mental health practice and aging: holistic recovery from mental illness for older veterans. Innov Aging. 2018;2:594–594. doi: 10.1093/GERONI/IGY023.2205. [DOI] [Google Scholar]
- 13.Williams J, Stubbs B, Gaughran F, Craig T. “Walk This Way” - a pilot of a health coaching intervention to reduce sedentary behaviour and increase low intensity exercise in people with serious mental illness: Study protocol for a randomised controlled trial. Trials. 2016 doi: 10.1186/s13063-016-1660-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Attux C, Martini LC, Elkis H, Tamai S, Freirias A, Camargo MDGM, et al. A 6-month randomized controlled trial to test the efficacy of a lifestyle intervention for weight gain management in schizophrenia. BMC Psychiatry. 2013;13:1–9. doi: 10.1186/1471-244X-13-60/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown C, Read H, Stanton M, Zeeb M, Jonikas JA, Cook JA. A pilot study of the Nutrition and Exercise for Wellness and Recovery (NEW-R): A weight loss program for individuals with serious mental illnesses. Psychiatr Rehabil J. 2015;38:371–373. doi: 10.1037/PRJ0000115. [DOI] [PubMed] [Google Scholar]
- 16.Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CAM, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368:1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magni LR, Ferrari C, Rossi G, Staffieri E, Uberti A, Lamonaca D, et al. Superwellness Program: a cognitive-behavioral therapy-based group intervention to reduce weight gain in patients treated with antipsychotic drugs. Rev Bras Psiquiatr. 2017;39:244–251. doi: 10.1590/1516-4446-2016-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pendlebury J, Haddad P, Dursun S. Evaluation of a behavioural weight management programme for patients with severe mental illness: 3 year results. Hum Psychopharmacol Clin Exp. 2005;20:447–448. doi: 10.1002/HUP.707. [DOI] [PubMed] [Google Scholar]
- 19.Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unützer J, Patel V, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry. 2017;4:486–500. doi: 10.1016/S2215-0366(17)30096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fortuna KL, Naslund JA, LaCroix JM, Bianco CL, Brooks JM, Zisman-Ilani Y, et al. Digital peer support mental health interventions for people with a lived experience of a serious mental illness: systematic review. JMIR Ment Heal. 2020 doi: 10.2196/16460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kozak AT, Buscemi J, Hawkins MAW, Wang ML, Breland JY, Ross KM, et al. Technology-based interventions for weight management: current randomized controlled trial evidence and future directions. J Behav Med. 2017;40:99–111. doi: 10.1007/S10865-016-9805-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28:320–329. doi: 10.1097/JCN.0B013E318250A3E7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed) 2021;74:790–799. doi: 10.1016/J.REC.2021.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Gyllensten AL, Forsberg KA. Computerized physical activity training for persons with severe mental illness - experiences from a communal supported housing project. Disabil Rehabil Assist Technol. 2017;12:780–788. doi: 10.1080/17483107.2016.1263881. [DOI] [PubMed] [Google Scholar]
- 25.Young AS, Cohen AN, Goldberg R, Hellemann G, Kreyenbuhl J, Niv N, et al. Improving weight in people with serious mental illness: the effectiveness of computerized services with peer coaches. J Gen Intern Med. 2017;32:48–55. doi: 10.1007/S11606-016-3963-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naslund JA, Aschbrenner KA, Scherer EA, McHugo GJ, Marsch LA, Bartels SJ. Wearable devices and mobile technologies for supporting behavioral weight loss among people with serious mental illness. Psychiatry Res. 2016;244:139–144. doi: 10.1016/j.psychres.2016.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naslund JA, Aschbrenner KA, Marsch LA, McHugo GJ, Bartels SJ. Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: an exploratory study. Psychiatr Q. 2018;89:81–94. doi: 10.1007/s11126-017-9512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H, Kane I, Brar J, Sereika S. Telephone-delivered physical activity intervention for individuals with serious mental illness: a feasibility study. J Am Psychiatr Nurses Assoc. 2014;20:389–397. doi: 10.1177/1078390314561497. [DOI] [PubMed] [Google Scholar]
- 29.Temmingh H, Claassen A, Van Zyl S, Carrara H, Dayakalashe NM, Myer L, et al. The evaluation of a telephonic wellness coaching intervention for weight reduction and wellness improvement in a community-based cohort of persons with serious mental illness. J Nerv Ment Dis. 2013;201:977–986. doi: 10.1097/NMD.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 30.De CM, Chang JJ, Kuo CC, Yu JW, Huang MF, Marks B, et al. A pilot comparative study of one-way versus two-way text message program to promote physical activity among people with severe mental illness. Ment Health Phys Act. 2017;13:143–151. doi: 10.1016/J.MHPA.2017.09.010. [DOI] [Google Scholar]
- 31.Williams J, Stubbs B, Richardson S, Flower C, Barr-Hamilton L, Grey B, et al. “Walk this way”: results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry. 2019 doi: 10.1186/S12888-019-2274-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Looijmans A, Jörg F, Bruggeman R, Schoevers RA, Corpeleijn E. Multimodal lifestyle intervention using a web-based tool to improve cardiometabolic health in patients with serious mental illness: results of a cluster randomized controlled trial (LION) BMC Psychiatry. 2019 doi: 10.1186/S12888-019-2310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aschbrenner KA, Naslund JA, Shevenell M, Kinney E, Bartels SJ. A pilot study of a peer-group lifestyle intervention enhanced with mhealth technology and social media for adults with serious mental illness. J Nerv Ment Dis. 2016;204:483–486. doi: 10.1097/NMD.0000000000000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, Bartels SJ. Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatr Q. 2016;87:401–415. doi: 10.1007/S11126-015-9395-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Browne J, Penn DL, Battaglini CL, Ludwig K. Work out by walking: a pilot exercise program for individuals with schizophrenia spectrum disorders. J Nerv Ment Dis. 2016;204:651–657. doi: 10.1097/NMD.0000000000000556. [DOI] [PubMed] [Google Scholar]
- 36.Brown C, Goetz J, Hamera E, Gajewski B. Treatment response to the RENEW weight loss intervention in schizophrenia: Impact of intervention setting. Schizophr Res. 2014;159:421. doi: 10.1016/J.SCHRES.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Green CA, Yarborough BJH, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. Am J Psychiatry. 2015;172:71–81. doi: 10.1176/APPI.AJP.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holt RIG, Gossage-Worrall R, Hind D, Bradburn MJ, McCrone P, Morris T, et al. Structured lifestyle education for people with schizophrenia, schizoaffective disorder and first-episode psychosis (STEPWISE): randomised controlled trial. Br J Psychiatry. 2019;214:63–73. doi: 10.1192/BJP.2018.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Speyer H, Jakobsen AS, Westergaard C, Nørgaard HCB, Pisinger C, Krogh J, et al. Lifestyle interventions for weight management in people with serious mental illness: a systematic review with meta-analysis, trial sequential analysis, and meta-regression analysis exploring the mediators and moderators of treatment effects. Psychother Psychosom. 2019;88:350–362. doi: 10.1159/000502293. [DOI] [PubMed] [Google Scholar]
- 40.Vera-Garcia E, Mayoral-Cleries F, Vancampfort D, Stubbs B, Cuesta-Vargas AI. A systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with schizophrenia: An update. Psychiatry Res. 2015;229:828–839. doi: 10.1016/J.PSYCHRES.2015.07.083. [DOI] [PubMed] [Google Scholar]
- 41.Haque SN. Telehealth beyond COVID-19. Psychiatr Serv. 2021;72:100–103. doi: 10.1176/APPI.PS.202000368. [DOI] [PubMed] [Google Scholar]
- 42.Torous J, Keshavan M. COVID-19, mobile health and serious mental illness. Schizophr Res. 2020;218:36. doi: 10.1016/J.SCHRES.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Korman N, Armour M, Chapman J, Rosenbaum S, Kisely S, Suetani S, et al. High Intensity Interval training (HIIT) for people with severe mental illness: A systematic review & meta-analysis of intervention studies– considering diverse approaches for mental and physical recovery. Psychiatry Res. 2020;284:112601. doi: 10.1016/J.PSYCHRES.2019.112601. [DOI] [PubMed] [Google Scholar]
- 44.Rauschenberg C, Schick A, Hirjak D, Seidler A, Paetzold I, Apfelbacher C, et al. Evidence synthesis of digital interventions to mitigate the negative impact of the COVID-19 pandemic on public mental health: rapid meta-review. J Med Internet Res. 2021;23(3):e23365. doi: 10.2196/23365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cantor JH, McBain RK, Kofner A, Stein BD, Yu H. Availability of outpatient telemental health services in the United States at the outset of the COVID-19 pandemic. Med Care. 2021;59:319–323. doi: 10.1097/MLR.0000000000001512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carter H, Araya R, Anjur K, Deng D, Naslund JA. The emergence of digital mental health in low-income and middle-income countries: A review of recent advances and implications for the treatment and prevention of mental disorders. J Psychiatr Res. 2021;133:223–246. doi: 10.1016/J.JPSYCHIRES.2020.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ashdown-Franks G, Williams J, Vancampfort D, Firth J, Schuch F, Hubbard K, et al. Is it possible for people with severe mental illness to sit less and move more? A systematic review of interventions to increase physical activity or reduce sedentary behaviour. Schizophr Res. 2018;202:3–16. doi: 10.1016/J.SCHRES.2018.06.058. [DOI] [PubMed] [Google Scholar]
- 48.Vancampfort D, Probst M, Basangwa D, De Hert M, Myin-Germeys I, van Winkel R, et al. Adherence to physical activity recommendations and physical and mental health risk in people with severe mental illness in Uganda. Psychiatry Res. 2018;260:236–240. doi: 10.1016/j.psychres.2017.11.067. [DOI] [PubMed] [Google Scholar]
- 49.Vancampfort D, Firth J, Schuch FB, Rosenbaum S, Mugisha J, Hallgren M, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16:308–315. doi: 10.1002/wps.20458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Singh VK, Karmani S, Malo PK, Virupaksha HG, Muralidhar D, Venkatasubramanian G, et al. Impact of lifestyle modification on some components of metabolic syndrome in persons with severe mental disorders: A meta-analysis. Schizophr Res. 2018;202:17–25. doi: 10.1016/J.SCHRES.2018.06.066. [DOI] [PubMed] [Google Scholar]
- 51.Brown KL, LaRose JG, Mezuk B. The relationship between body mass index, binge eating disorder and suicidality. BMC Psychiatry. 2018;18:1–9. doi: 10.1186/S12888-018-1766-Z/FIGURES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.