Abstract
Purpose
This report presents the first known use of a rigid endoscope with augmented reality technology for the removal of an odontogenic cyst that penetrated the maxillary sinus and illustrates its practical use in a patient.
Materials and Methods
In the preoperative period, cone-beam computed tomography was performed in a specially designed marker holder frame, and the contours of the cyst and the nearest anatomical formations were segmented in the 3D Slicer program. During the operation, a marker was installed on the patient’s head, as well as on the tip of the endoscope, which made it possible to visualize the mass and the movement of the endoscope. The surgical intervention was performed with the support of augmented reality in HoloLens glasses (Microsoft Corporation, Redmond, WA, USA).
Results
The use of this technology improved the accuracy of surgical manipulations, reduced operational risks, and shortened the time of surgery and the rehabilitation period.
Conclusion
With the help of modern technologies, a navigation system was created that helped to track the position of the endoscope in mixed reality in real time, as well as to fully visualize anatomical formations.
Keywords: Endoscopes, Augmented Reality, Cysts, Tooth, Jaw
Introduction
The maxillary sinus is closely located to the roots of the teeth; for this reason, jaw cysts can increase in size and protrude into its lower wall. The success of an operation is often associated with the surgeon’s spatial thinking and experience, while poor visualization increases the risks of complications in the form of bleeding, perforation of other anatomical structures, and only partial removal of the cyst.1 Therefore, the development of new methods remains relevant.
Augmented reality (AR) technology is now commonly encountered. It is used in orthognathic and plastic surgery, and the first experiences of using AR when performing operations in maxillofacial surgery have been described.2,3,4,5 For example, in 2017, an AR system was developed to display bundles of alveolar nerves in maxillofacial surgery. The overall accuracy reached 1 mm.6 AR has also found applications in dentistry, both in educational and clinical practice.7,8
AR technology would help to carry out primary planning with the help of computed tomography (CT) and in the patient’s oral cavity in real time during the treatment of odontogenic cysts. This effect can be achieved by directly superimposing medical images on anatomical formations through AR. Intraoperative visualization of images obtained on the basis of preoperative CT data, supplemented by the location of the tracked tool tip, can be beneficial in improving the methods of surgical treatment of volumetric formations of the jaws with the help of developed programs and markers.9,10
The purpose of the present report was to describe the clinical picture and study the possibility of using AR technology as a navigation system during a surgical intervention targeting the maxillary sinus.
Materials and Methods
This study was approved by the Ethical Commission of First Pavlov State Medical University of the Ministry of Health of the Russian Federation. A 38-year-old male patient presented to the dental clinic of the Central Research Institute of Dentistry and Maxillofacial Surgery with complaints of discomfort in the area of the upper left second and third molars.
About 10 years previously, an operation was performed for a volumetric cyst of the upper jaw, with the volume of cystectomy encompassing the area from the left upper second incisor to the left upper second premolar and resection of the tops of the roots of the teeth protruding into the cyst. No anomalies were recorded in the postoperative period.
About a month ago, the patient noticed discomfort in the area in the area of the upper left second and third molars. He presented to the clinic of maxillofacial surgery of the First Pavlov State Medical University of the Ministry of Health of the Russian Federation.
Upon examination, it was revealed that the patient’s face was symmetrical. The skin of the face had a physiological color, without pathological elements of a rash. The patient could open his mouth completely and painlessly. Swallowing was also painless. The left upper first incisor and left upper third molar were the supporting teeth for a bridge-shaped metal-ceramic prosthesis. Palpation of the upper arch of the vestibule on the right and left was painless, as was palpation in the area of the canine fossa on the right and left. The regional lymph nodes were not palpated. In the oral cavity, the mucous membrane was pale pink and moderately moist. At the time of examination, nasal breathing was not intermittent, and there was no discharge from the nasal passages.
Cone-beam computed tomography (CBCT) of the upper jaw was performed. There was a defect of the alveolar process, and in some places, a violation of the integrity of the vestibular and palatine cortical plates. In the area of the upper left second and third molars after endodontic treatment, the focus of bone tissue destruction was determined to be the area of the tips of the roots, with fairly clear, relatively smooth contours, an irregular oval shape, and extension into the lumen of the left maxillary sinus. The buccal cortical plate was thinned and pushed outward, and in some places, its integrity was violated.
The patient was diagnosed with a cyst of the upper jaw in the area from the left upper second incisor to the left upper second premolar (a condition after complex treatment in 2010). There was also a cyst in the upper jaw from the left upper second molar.
To obtain a 3-dimensional (3D) view of the formations and their relationship with surrounding structures, the X-ray examination file in Digital Imaging and Communications in Medicine (DICOM) format was uploaded to the open-source 3D Slicer medical image segmentation program. Segmentation of the contours of the cyst that was removed earlier and the cyst from the left upper second molar, as well as the nearest anatomical structures, was performed.
The bone boundaries of both cysts were found to be in close proximity to each other. The cyst that was removed earlier had been partially replaced by fibrous tissue. The medial buccal root of the left upper second molar protruded into one-third of the cavity of the newly formed cyst.
Considering the large size of the formation, its location, and the condition of the teeth, it was decided to perform cystectomy and resection of the medial buccal root of the left upper second molar. Computer planning of the operational access zone was performed, taking into account the close location of both cysts and root tips. The optimal entry point for endoscopes with viewing angles of 0°, 30°, and 75° was planned.
In accordance with the developed technology for using AR during surgical operations,9 the following activities were carried out. A specially designed frame holder for an AR marker was used,10 which was fixed on the patient’s head while a CBCT examination was performed. During the examination, the marker holder was fixed on the patient’s head (Fig. 1).
Fig. 1. Cone-beam computed tomography with radiopaque markers.
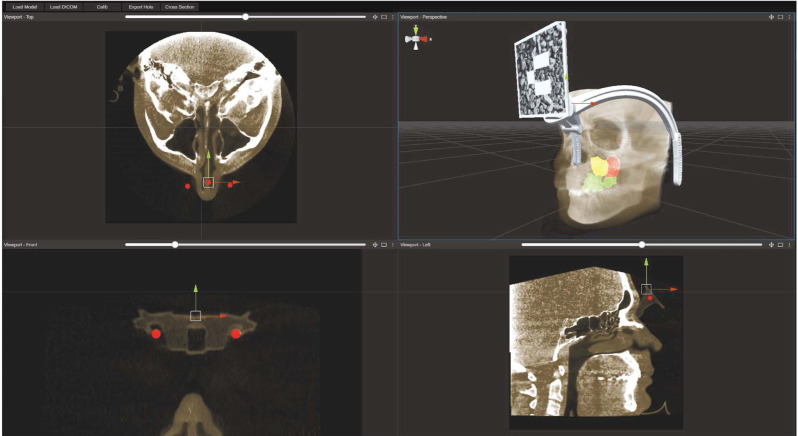
The CBCT examination data (DICOM file) was loaded into an open-source computer program for segmentation of medical images. Manual segmentation of the formations of interest was performed, and planning of operative access for the endoscope was carried out to identify the approach where the zone of its visualization would be optimal (Fig. 2). Radiopaque markers embedded in the holder were used to calibrate and link the patient’s radiological data to the position of the holder and the marker fixed in it.
Fig. 2. Segmented image of an odontogenic cyst.
Target registration error (TRE) for the frame was evaluated using a head phantom that was 3D-printed from the patient’s CBCT. A number of predefined points in different places were marked on the skull of the head phantom. Using mixed reality glasses with a loaded model of the phantom’s skull, the possible displacement of each point was measured with a ruler. The median TRE was between 1 and 3 mm, depending on how accurately the frame was placed.
The received data were loaded into AR glasses. It was decided to perform the operation under endoscopic control in order to reduce the traumatic nature of the operation and to improve the visualization of the boundaries of formations. For this purpose, a rigid endoscope (Karl Storz, Stuttgart, Germany) with viewing angles of 0°, 30°, and 75° was used.
To visualize the tip of the endoscope in mixed reality glasses, an endoscope and a removable tube were accurately measured. Based on these measurements, a marker holder was designed and printed on a 3D printer, after which it was installed on a surgical instrument. Finally, during the procedure, the software on the mixed reality glasses tracked the position of the attached marker and visualized the tip with the necessary offset based on the endoscope and marker holder dimensions.
To maximize the accuracy of the surgical intervention, a system for tracking the tip of the endoscope in mixed reality in real time was created. The overall hologram positioning accuracy with this method depended on 1) marker-based 3D visual localization11 (the translation error from a 1-m distance varies between 2 and 5 mm); 2) the manufacturing accuracy of the fabricated marker holder (for FDM technology, this is about 0.2 mm); 3) CT slice thickness (in this case, all datasets had 1-mm thickness); and 4) head frame positioning.
Results
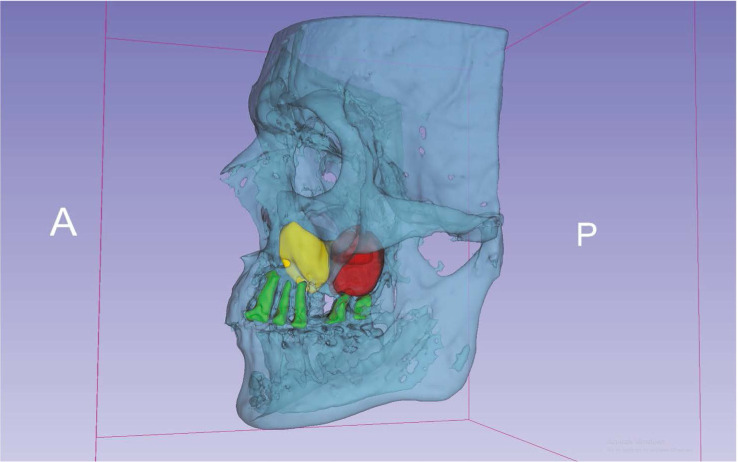
During the surgical intervention, the AR marker was again fixed on the patient’s head in its original position (Fig. 3). An image of the segmented formations of the upper jaw was attached to marker 1. A marker with a QR code was also attached to the handle of the endoscope. The projection of the endoscope tip was attached to marker 2 (Fig. 4).
Fig. 3. An augmented reality marker fixed on the head.

Fig. 4. A hologram of the segmented formations.

The surgical intervention was performed with AR support in HoloLens glasses (Microsoft Corporation, Redmond, WA, USA). During the formation of the operative access, the surgeon was guided by the projection of anatomical structures and the recommended, pre-planned access for the endoscope. With the help of an AR navigation system, the surgeon saw the position of the endoscope tip when it was unavailable for review. This made it possible to remove the cyst from the area of the left upper second molar without damaging the walls of the previously operated cyst and the walls of the maxillary sinus (Fig. 5). Resection of the apex of the medial buccal root of the left upper second molar was performed.
Fig. 5. Visualization of the cyst envelope during surgery.

No abnormalities were recorded during the postoperative period. In an examination on the third day after the operation, no pronounced inflammatory reaction of the surrounding tissues was detected. The stitches were removed on the 12th day. CBCT was performed 6 months after the operation. This scan was compared with preoperative planning using preoperative CBCT, and the quantitative accuracy was estimated using the root mean square (RMS) value of landmarks (Fig. 6).
Fig. 6. Visualization of a cyst before surgery (upper), visualization of a bone defect after surgery (bottom).
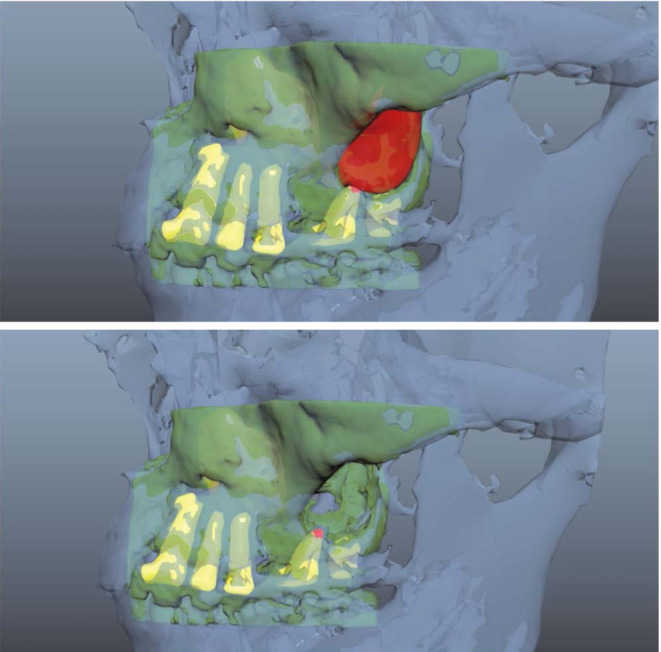
Guidelines were needed to assess 1) the level of resection of the left upper second molar; 2) the bone defect visualized before surgery (the entrance location corresponded to the planned one); and 3) the absence of defects in the bone walls of the previously operated cyst. Based on these aspects, the total RMS error was between 3 and 6 mm depending on the viewing angle and how the marker was recognized/tracked.
Discussion
AR in medicine demonstrates how healthcare can change in the 21st century with the help of digital medicine. In previous studies, AR has been used as a method of visualizing anatomical structures that cannot normally be seen during operations. An example is furnished by the use of an AR system to display the lower alveolar nerve bundles during facial bone contouring surgery.6 In another case, this system was also used for oral surgery. A 3D virtual image of bone structures was projected into the patient’s body. Surgical procedures, including drilling holes and fixing with screws, were performed under the control of AR.7 However, no study has yet focused on the use of AR navigation technology in combination with endoscopic surgery.
The use of this technology will provide an individualized approach to the diagnosis and treatment of patients with odontogenic cysts, which will significantly improve the quality of treatment. The use of a navigation system based on mixed reality technology for endovideo-associated interventions in the maxillofacial region improves the accuracy of surgical manipulations, reduces operational risks, and shortens the operation time and the recovery period.
Dynamic navigation in mixed reality makes it possible to adjust the direction of the endoscope in real time during surgery based on virtual preoperative planning. Such a navigation system demonstrates the accuracy and safety sufficient for everyday clinical practice. However, further research on this topic is necessary to maximize accuracy, evaluate efficiency, and assess cost-effectiveness.
In the demonstrated clinical case, according to the results of segmentation of CT data with subsequent 3D modeling, topographic features of the upper jaw formations were revealed, which made it possible to determine the optimal treatment strategy. Cystectomy and resection of the root tip of the causal tooth were performed based on the anatomical and topographic location, shape, and volume of the cyst. The volume and topography of the formations and adjacent anatomical structures fully corresponded to the data obtained during virtual planning.
Footnotes
The study was funded by a group of authors.
Conflicts of Interest: None
References
- 1.Siwach P, Joy T, Gaikwad S, Meshram V. Postoperative maxillary cyst. Indian J Dent Res. 2020;31:157–159. doi: 10.4103/ijdr.IJDR_259_18. [DOI] [PubMed] [Google Scholar]
- 2.Lysenko A, Razumova A, Yaremenko A, Mirzakhmedov R, Zubareva A, Chibisova M. The first clinical use of augmented reality to treat salivary stones. Case Rep Dent. 2020;2020:5960421. doi: 10.1155/2020/5960421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Waard O, Baan F, Verhamme L, Breuning H, Kuijpers-Jagtman AM, Maal T. A novel method for fusion of intra-oral scans and cone-beam computed tomography scans for orthognathic surgery planning. J Craniomaxillofac Surg. 2016;44:160–166. doi: 10.1016/j.jcms.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Ivanov VM, Krivtsov AM, Strelkov SV, Kalakutskiy NV, Yaremenko AI, Petropavlovskaya MY, et al. Intraoperative use of mixed reality technology in median neck and branchial cyst excision. Future Internet. 2021;13:214 [Google Scholar]
- 5.Ayoub A, Pulijala Y. The application of virtual reality and augmented reality in Oral & Maxillofacial Surgery. BMC Oral Health. 2019;19:238. doi: 10.1186/s12903-019-0937-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu M, Liu F, Chai G, Pan JJ, Jiang T, Lin L, et al. A novel augmented reality system for displaying alveolar nerve bundles in maxillofacial surgery. Sci Rep. 2017;7:42365. doi: 10.1038/srep42365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang TK, Yang CH, Hsieh YH, Wang JC, Hung CC. Augmented reality (AR) and virtual reality (VR) applied in dentistry. Kaohsiung J Med Sci. 2018;34:243–248. doi: 10.1016/j.kjms.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Joda T, Gallucci GO, Wismeijer D, Zitzmann NU. Augmented and virtual reality in dental medicine: a systematic review. Comput Biol Med. 2019;108:93–100. doi: 10.1016/j.compbiomed.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Ivanov VM, Klygach AS, Strelkov SV, inventors. A method of preparing and performing a surgical operation on the head using mixed reality. 2754288/2020132952. Russian Federation patent. 2021 Aug 31;
- 10.Ivanov VM, Klygach AS, Strelkov SV, inventors. A marker holder used for mixed reality head surgery. 202367/2020132951. Russian Federation patent. 2020 Jun 10;
- 11.Pentenrieder K, Meier P, Klinker G. Analysis of tracking accuracy for single camera square-marker-based tracking; Proc. Dritter Workshop Virtuelle und Erweiterte Realittder GIFachgruppe VR/AR; Koblenz, Germany. 2006. [Google Scholar]