Abstract
Introduction
During the COVID-19 pandemic, emergency nurses have been adversely affected physically, socially, and psychologically by factors such as increased workload, longer working hours, isolation from family, and limited resources. This study aimed to investigate the effect of motivational messages sent to emergency nurses during the COVID-19 pandemic on their job satisfaction, compassion fatigue, and communication skills.
Methods
This was a randomized controlled experimental study. The study was conducted with 60 emergency nurses in 2 training and research hospitals in Istanbul between July 31 and August 31, 2021. The participants were randomly assigned to the intervention and control groups. Participants in the intervention group (n = 30) received daily motivational messages to their mobile phones by short message service for 21 days; those in the control group (n = 30) received no motivational messages. The Job Satisfaction Scale, Compassion Fatigue Scale, and Communication Skills Scale were administered before and after the intervention.
Results
The mean age was 29.8 (SD = 7.5) and 28.7 years (SD = 6.9) in the intervention and control groups, respectively. Before the intervention, there were no significant differences in the groups’ scores for job satisfaction (P = .561), compassion fatigue (P = .687), or communication skills (P = .355). After the intervention, the intervention group had significantly higher scores for job satisfaction (P < .001) and communication skills (P < .001) and significantly lower compassion fatigue scores than the control group (P < .001).
Discussion
Our results suggest that motivational messages sent to emergency nurses during the COVID-19 pandemic increase job satisfaction and improve communication skills while reducing compassion fatigue.
Key words: Emergency, Nursing, Motivation, Job satisfaction, Compassion fatigue, Communication skills
Contribution to Emergency Nursing Practice
-
•
What is already known about this topic? Lack of motivation in emergency nurses can cause a decrease in job satisfaction and compassion fatigue. Low motivation can also negatively affect the communication skills of emergency nurses.
-
•
What does this paper add to the currently published literature? This study showed that motivational messages increase emergency nurses' job satisfaction and improve communication skills while reducing their compassion fatigue.
-
•
What is the most important implication for clinical practice? It is seen that motivational messages have positive effects on job satisfaction, communication skills, and compassion fatigue of emergency nurses.
Introduction
The COVID-19 pandemic has become one of the most important health problems in the world today.1 During the pandemic, there was a marked increase in ED admissions of both walk-in and ambulance-conveyed patients. In many countries, a separate triage system and separate physical areas were established for COVID-19 patients.2 In Turkey, pretriage areas staffed by one of the doctors and nurses on shift were established outside many emergency departments to identify suspected COVID-19 cases. Suspected cases were directed to isolated areas of the emergency department, whereas nonsuspect patients were referred to clean areas based on their severity.3 As a result, emergency teams in these departments provided care for both emergency patients and COVID-19 patients simultaneously. This has led to an increase in the workload of emergency staff, especially nurses.4 In addition to the increased workload, other problems faced by emergency personnel during the pandemic include the management of limited resources, the added difficulty of working in personal protective equipment, fear of COVID-19 transmission, being separated from family, and negative interactions with patients' relatives. These issues have adversely affected nurses physically, and the stress, anxiety, and uncertainty have lowered their motivation levels.5
Improving nurses’ job satisfaction and motivation levels is necessary to increase the effectiveness of nursing services, which are a key component of health services.6 Job satisfaction, which is an emotional response to the appraisal of one’s job and work life, is generally addressed together with the concept of motivation. This is because motivation has the power to influence not only the behaviors and performance of nurses responsible for patient care but also their professional job satisfaction.7 Nurses’ job satisfaction can be enhanced by feelings that they are successful and are well suited to the profession as well as factors such as effective communication and being respected, appreciated, and rewarded.8 For patients to receive appropriate and effective care, nurses must derive satisfaction from the care services they provide and the unit in which they work.9 Emergency nurses in particular experience the negative impact on their emotional well-being and ability to provide compassionate care, resulting in compassion fatigue in some nurses.10
Compassion fatigue was first described by nurse Joinson11 as the emotional effect of indirect trauma while helping people who experience direct traumatic stress. Researchers later described compassion fatigue as a natural consequence of the care relationship between 2 people and defined it as a gradual decrease in compassion toward patients over time.11 Unlike compassion fatigue, burnout is a long-term condition associated with the work environment and can be seen in every profession. Studies have revealed that compassion fatigue is common among workers in intensive care, surgery, and emergency units because these units serve patients experiencing significant emotional pain and physical stress, which can readily lead to physical, emotional, and mental burnout in their caregivers.12, 13, 14 Hegney et al15 determined in their study that emergency nurses had high levels of compassion fatigue, which was associated with anxiety, depression, and shift-based work conditions. Peters16 also reported that nurses were at risk of compassion fatigue. Figley17 reported that compassion fatigue is the cost of nursing care because the basis of compassion fatigue is both the individual needing care and the individual providing care. Job dissatisfaction may increase if measures to counter compassion fatigue are not taken or support is not provided, and the care relationship between nurse and patient may be adversely affected. This can result in poor communication with both colleagues and patients.18 Strategies to prevent compassion fatigue should be developed so that nurses do not lose their selfless approach toward patients, especially in this period of intense physical and mental fatigue during the COVID-19 pandemic. One study indicated that the increased workload owing to the pandemic and the resulting stress, compassion fatigue, and burnout were inversely associated with happiness and perceived organizational justice. Therefore, the authors concluded that interventions to improve employees’ work and social life are urgently needed.19 One such intervention may consist of easy-to-send, inexpensive, effective motivational messages (appreciation, gratitude, etc) to promote well-being. Another possibility is social support-based approaches (colleagues, managers, etc) to strengthen professional interpersonal relationships and enable communication.20
Nursing is a profession based on human relations, and communication is essential in terms of the quality and effectiveness of patient care because nurses use communication techniques when identifying and solving problems, coping with stress, and providing health education. Communication skills help ensure that messages are understood correctly and promote the development of interpersonal relationships. Inadequate and ineffective communication skills are associated with negative patient outcomes and medical errors and also have a negative effect on pandemic management.21 Supporting health care professionals psychologically during the pandemic may help them adapt better to this period. A qualitative study conducted in China by Khoo et al22 revealed that appreciation from colleagues and patients reduced health care professionals’ stress and increased their morale. This was reported to positively affect teamwork and communication with patients. A different study showed that motivation made individuals happy and happiness was directly associated with communication.23 Kandemir et al24 observed that positive informal communication increased happiness in the workplace and positively affected employee motivation.
Emergency nurses have arguably borne the greatest burden during the pandemic, with long working hours and high care loads, and this high level of performance has adversely affected their mental health. Therefore, this study aimed to examine the effect of motivational messages sent to emergency nurses during the COVID-19 pandemic on their levels of job satisfaction, compassion fatigue, and communication skills. We hypothesized that motivational messages would enhance nurses’ job satisfaction, decrease their compassion fatigue, and favorably affect their communication skills.
Methods
Trial Design
This study was a randomized controlled trial. The study protocol was preregistered publicly (NCT05158504) to ClinicalTrials.gov.tr, which is managed by the National Institutes of Health, National Library of Medicine, Office of Management and Budget, and Department of Health and Human Services for the evaluation and approval of research studies at an international level.
Study Sample
The population of the study comprised 89 nurses working in the emergency departments of 2 training and research hospitals (both designated as pandemic hospitals) affiliated with the Ministry of Health in Istanbul, Turkey, between July 31, 2021, and August 31, 2021. Power analysis was performed to determine the necessary sample size using G∗Power version 3.1 (Franz Faul, Universität Kiel, Germany). In a similar study by Shin et al,25 the effect size for compassion fatigue was calculated as 0.617. In the power analysis, we determined that a total of 60 people, 30 in each group, were necessary for a study power greater than 95% at a significance level of 5% and effect size of 0.617 (df = 116, t = 1.658).
Inclusion criteria were working in the emergency department, working only the day shift on weekdays, having a mobile phone, and volunteering to participate in the study. In the hospitals where the study was conducted, nurses follow an alternating monthly work schedule with 1 month of night shift and 1 month of day shift. Exclusion criteria for the study included being on leave for any reason (maternity, annual, medical) during the study dates, not completely filling in the data collection forms, or withdrawing from the study. In addition, during the online one-on-one interview with all participants before the study, the participants were asked about their psychiatric history or psychiatric drug use. Individuals with a psychiatric diagnosis or a history of using psychiatric drugs were excluded from the study.
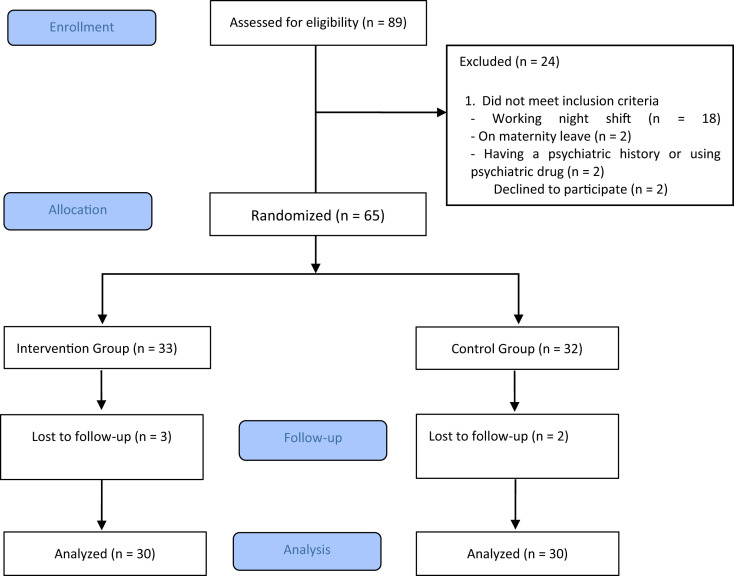
After excluding nurses that did not meet the study selection criteria (n = 24), we decided to include all 65 eligible nurses in the study sample (33 in the intervention group and 32 in the control group) to account for potential losses (73% of the population). As 3 nurses in the intervention group and 2 nurses in the control group did not respond at post-test, the study was completed with a total of 60 nurses, 30 in each group (Figure ).
Figure.
CONSORT flow diagram. CONSORT, Consolidated Standards of Reporting Trials.
Randomization
Randomization was performed using a computer-based random number generator.26 The random allocation sequence and assignment of the participants to the control and intervention groups were performed by the researchers. Participants who agreed to participate in the study were numbered in the order in which they were enrolled and were assigned to the intervention or control group according to the random number sequence on the randomization list. Owing to the study design, blinding was not possible because the participants knew about the intervention.
Outcomes Measures
Data were collected in face-to-face interviews using a personal information form, the Job Satisfaction Scale, Compassion Fatigue Scale, and Communication Skills Scale. Owing to the COVID-19 pandemic, the first interview with the participants was conducted online and the participants were informed about the study. Data were collected using the personal information form before the intervention (day 1 of the study), and the participants completed the Job Satisfaction Scale, Compassion Fatigue Scale, and Communication Skills Scale once before the intervention (pretest) and again after the intervention (post-test). The primary outcomes of the study were changes in the participants’ job satisfaction, compassion fatigue, and communication skills scores after the intervention.
Personal Information Form
Based on the relevant literature, this form contained a total of 8 questions including descriptive characteristics such as the participant’s age, sex, education level, professional experience, time working in current unit, weekly working hours, whether they feel the nursing profession suits them, and whether they intend to continue working.27 , 28
Job Satisfaction Scale
This 5-item scale was adapted by Judge, Locke, Durham, and Kluger in 1998 from a longer measure of job satisfaction developed by Brayfield and Rothe in 1951. The Turkish validity and reliability of the scale were conducted by Keser and Bilir29 in 2019. The items are rated on a 5-point Likert scale from strongly disagree (1) to strongly agree (5), and the average score is obtained. A higher average score indicates greater job satisfaction. The Cronbach alpha value of the scale was previously reported to be 0.85 and was calculated as 0.91 in this study.
Compassion Fatigue Scale
This instrument was developed as a 13-item short form by Adams et al in 2006, and the Turkish validity and reliability study was conducted by Dinç and Ekinci30 in 2019. The scale aims to measure secondary trauma and occupational burnout. Items are rated on a 10-point Likert-type scale from rarely/never (1) to very often (10). The total score that can be obtained ranges from 13 to 130, with higher scores representing a higher level of compassion fatigue. The Cronbach alpha value of the scale was reported as 0.87 in the validity study and was calculated as 0.96 in this study.
Communication Skills Scale
This scale was developed in Turkish by Korkut31 in 1996 to determine how people evaluate their own communication skills. The 25 items are rated on a 5-point Likert-type scale from always (1) to never (5), yielding a total score ranging from 25 to 125. The scale consists of 5 subscales: basic skills and self-expression, following communication principles, attention to communication, willingness to communicate, and effective listening and nonverbal communication. Higher scores reflect a positive perception of one’s communication skills. The developer later conducted the validity and reliability study for the scale and reported a Cronbach’s alpha of 0.88. In this study, the Cronbach alpha value was 0.96.
Study Procedure
Intervention Group
Before the study, the motivational messages were reviewed by an expert panel consisting of 4 nurse academicians and 2 psychologists. The expert panel’s evaluation was based on the Davis technique.32 They scored each statement as irrelevant (1), needs major revision (2), relevant but needs minor modification (3), or very relevant (4). Necessary changes were made to the messages according to the panel’s feedback. The resulting 61 messages were determined to have a content validity index of 96%. The pretest was performed before the intervention on the first day of the study. For the next 21 days, participants in the intervention group were sent motivational messages via short message service to their mobile phones 3 times a day (7 am, 12 pm, and 4 pm). The head nurse allowed participants to take a short break (5-10 minutes) to access the messages when they heard the delivery notification sound. The participants received a different set of motivational messages each day. The post-test was performed at the end of the intervention. Examples of the daily motivational messages are presented in Table 1 and Supplementary Material.
Table 1.
Motivational message intervention program
| Time | Message purpose and example |
|---|---|
| 7 am | A good morning message to start the day with good energy
|
| 12 pm | Health-promoting message
|
| 4 pm | “Me time” message
|
Control Group
Participants in the control group underwent the same pretest and post-test assessments as the intervention group, but did not receive motivational messages during the intervention period.
Statistical Analysis
The study data were analyzed using SPSS for Windows version 22.0 (IBM Corp, Armonk, NY). Number, percentage, mean, and SD were used as descriptive statistical methods. Normal distribution was evaluated with kurtosis and skewness. The distribution of descriptive variables by group was evaluated using chi-square analysis. Continuous quantitative data were compared between independent groups using the t test, and within-group changes were analyzed using analysis of variance (ANOVA) with repeated measurement. The statement: “Mauchly’s test of Sphericity was used to decide whether prerequisite of sphericity is provided or not. As it was decided that prerequisite of sphericity was not provided, the difference between the repeated measures was decided by applying Greenhouse-Geise test.” was added to this section. A P value of < .05 was considered statistically significant.
Ethical Considerations
Permission to conduct this study was obtained from the COVID-19 Scientific Research Evaluation Commission within the Ministry of Health, General Directorate of Health Services (application date: March 18, 2021; approval number: T07_43_13). In addition, written permission to conduct the study was obtained from the participating hospitals (24.04.2021), and institutional ethics committee approval was obtained on May 6, 2021 (decision number: E-46418926-050.99). Written permission to use the scales used in this study was obtained from their owners. The study was conducted in compliance with the principles of the Declaration of Helsinki.
Results
The mean ages of the participants in the intervention and control groups were 29.8 (SD = 7.5) and 28.7 years (SD = 6.9), respectively. Females accounted for 53.3% of the nurses in the intervention group and 43.3% of those in the control group. In terms of education level, most nurses in both groups held bachelor’s degrees. Although 36.7% of participants in the intervention group had at least 10 years of professional experience, this rate was 20% in the control group. When their time working in the current unit was evaluated, 40% of the participants in the intervention group and 43.3% of those in the control group had 1 to 5 years of experience in the emergency department. Nearly all of the nurses in both groups worked over 40 hours per week. When asked if they consider the profession a good fit for them, 73.3% of participants in the intervention group and 66.7% of those in the control group said yes. Two-thirds of participants in the intervention group and 46.7% of participants in the control group stated they did not want to continue working in the emergency department. There were no significant differences between the intervention and control groups in terms of sociodemographic characteristics (P > .05) (Table 2 ).
Table 2.
Sociodemographic characteristics of the nurses (N = 60)
| Variable | Intervention group (n = 30) | Control group (n = 30) | Total | Chi-square test | P value | |||
|---|---|---|---|---|---|---|---|---|
| Age (y), mean (SD) | 29.86 (7.56) | 28.70 (6.95) | 0.60 | .895 | ||||
| n | % | n | % | n | % | |||
| Sex | ||||||||
| Female | 16 | 53.3 | 13 | 43.3 | 29 | 48.3 | 0.60 | .303 |
| Male | 14 | 46.7 | 17 | 56.7 | 31 | 51.7 | ||
| Education level | ||||||||
| High school | 6 | 20.0 | 4 | 13.3 | 10 | 16.7 | 4.72 | .193 |
| Associate degree | 5 | 16.7 | 4 | 13.3 | 9 | 15.0 | ||
| Undergraduate | 10 | 33.3 | 18 | 60.0 | 28 | 46.7 | ||
| Postgraduate | 9 | 30.0 | 4 | 13.3 | 13 | 21.7 | ||
| Professional experience | ||||||||
| <1 y | 2 | 6.7 | 7 | 23.3 | 9 | 15.0 | 4.36 | .224 |
| 1-5 y | 8 | 26.7 | 7 | 23.3 | 15 | 25.0 | ||
| 6-10 y | 9 | 30.0 | 10 | 33.3 | 19 | 31.7 | ||
| ≥10 y | 11 | 36.7 | 6 | 20.0 | 17 | 28.3 | ||
| Time working in current unit | ||||||||
| <1 y | 3 | 10.0 | 8 | 26.7 | 11 | 18.3 | 3.86 | .276 |
| 1-5 y | 12 | 40.0 | 13 | 43.3 | 25 | 41.7 | ||
| 6-10 y | 11 | 36.7 | 7 | 23.3 | 18 | 30.0 | ||
| ≥10 y | 4 | 13.3 | 2 | 6.7 | 6 | 10.0 | ||
| Weekly working hours | ||||||||
| <40 h | 5 | 16.7 | 2 | 6.7 | 7 | 11.7 | 1.45 | .212 |
| >40 h | 25 | 83.3 | 28 | 93.3 | 53 | 88.3 | ||
| Feels the profession suits them | ||||||||
| Yes | 22 | 73.3 | 20 | 66.7 | 42 | 70.0 | 0.31 | .389 |
| No | 8 | 26.7 | 10 | 33.3 | 18 | 30.0 | ||
| Intends to continue working | ||||||||
| Yes | 10 | 33.3 | 16 | 53.3 | 26 | 43.3 | 2.44 | .096 |
| No | 20 | 66.7 | 14 | 46.7 | 34 | 56.7 | ||
Comparison of mean job satisfaction scores between the groups showed no statistical difference in the pretest (t = −0.585, P > .05), whereas the intervention group had a significantly higher scores in the post-test (t = 3.7, P < .05). The job satisfaction measurement × group interaction was found to be significant (F = 81.181, P < .05). Job satisfaction scores in the intervention group increased significantly in the post-test compared with the pretest, whereas those in the control group decreased in the post-test compared with the pretest (P < .05) (Table 3 ).
Table 3.
Comparison of mean job satisfaction scores between the groups (N = 60)
| Variable | Intervention group (n = 30) |
Control group (n = 30) |
Test value | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min-Max | Mean | SD | Min-Max | |||
| Job satisfaction—pretest | 2.86 | 0.86 | 1-4.6 | 3.00 | 0.90 | 1.6-4.4 | −0.585∗ | .561 |
| Job satisfaction—post-test | 3.54 | 0.65 | 2.2-5 | 2.82 | 0.81 | 1.6-4.4 | 3.775∗ | < .001 |
| Measurement | F = 29.138†; P < .001 | |||||||
| Measurement × group | F = 81.181†; P < .001 | |||||||
Min-Max, minimum-maximum.
Independent groups t test.
Repeated measures analysis of variance.
Similarly, the groups showed no significant differences in Compassion Fatigue Scale total or subscale scores in the pretest (t = −0.405, −1.886, 0.364, respectively P > .05) but significant differences in mean total score and scores in the secondary trauma subscale and occupational burnout subscale appeared in the post-test (t = −4.35, −3.37, respectively P < .05). Score measurement × group interactions were significant for compassion fatigue, secondary trauma, and occupational burnout (P < .05). In the intervention group, compassion fatigue, secondary trauma, and occupational burnout scores decreased significantly from the pretest to the post-test, whereas scores in the control group increased significantly between the pretest and post-test, significantly for compassion fatigue and occupational burnout (P < .001) (Table 4 ).
Table 4.
Comparison of mean compassion fatigue scores between the groups (N = 60)
| Variable | Intervention group (n = 30) |
Control group (n = 30) |
Test value | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min-Max | Mean | SD | Min-Max | |||
| Compassion fatigue—pretest | 48.76 | 16.72 | 18-86 | 50.90 | 23.48 | 15-92 | −0.405∗ | .687 |
| Compassion fatigue—post-test | 36.73 | 12.43 | 16-61 | 54.53 | 21.78 | 16-92 | −3.887∗ | < .001 |
| Measurement | F = 37.296†; P < .001 | |||||||
| Measurement × group | F = 129.736†; P < .001 | |||||||
| Secondary trauma—pretest | 12.00 | 5.73 | 5-30 | 15.50 | 8.39 | 5-31 | −1.886∗ | .065 |
| Secondary trauma—post-test | 9.56 | 4.04 | 5-20 | 16.13 | 7.19 | 5-30 | −4.359∗ | < .001 |
| Measurement | F = 5.918†; P < .05 | |||||||
| Measurement × group | F = 17.177†; P < .001 | |||||||
| Occupational burnout—pretest | 36.76 | 12.33 | 12-56 | 35.40 | 16.45 | 10-62 | 0.364∗ | .717 |
| Occupational burnout—post-test | 27.16 | 9.40 | 11-42 | 38.40 | 15.63 | 11-63 | −3.371∗ | < . 001 |
| Measurement | F = 56.971†; P < .001 | |||||||
| Measurement × group | F = 207.639†; P < .001 | |||||||
Min-Max, minimum-maximum.
Independent groups t test.
Repeated measures analysis of variance.
In the pretest, there was no statistically significant difference between the groups in mean Communication Skills Scale total score or scores in the subscales of basic skills and self-expression, attention to communication, willingness to communicate, effective listening and nonverbal communication, and following communication principles (t = −0.93, −1.115, −1.659, −0.595, −0.043, −0.703, respectively P > .05). However, in the post-test, there were significant differences between the groups in all communication skills scores (t = 3.83, P < .05). There were significant changes in communication skills total and subscale scores between the pretest and post-test (P < .05). Score measurement × group interactions were significant for the Communication Skills Scale and its subscales (F = 131.714, P < .05). Total and subscale scores on the Communication Skills Scale increased significantly in the post-test in the motivational group but decreased in the control group compared with pretest scores (P < .05) (Table 5 ).
Table 5.
Comparison of mean communication skills scores between the groups (N = 60)
| Variable | Intervention group (n = 30) |
Control group (n = 30) |
Test value | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min-Max | Mean | SD | Min-Max | |||
| Total score—pretest | 89.40 | 11.46 | 72-113 | 92.83 | 16.56 | 59-118 | −0.933∗ | .355 |
| Total score—post-test | 100.9 | 9.31 | 86-125 | 88.36 | 15.37 | 63-123 | 3.830∗ | < .001 |
| Measurement | F = 25.693†; P < .001 | |||||||
| Measurement × group | F = 131.714†; P < .001 | |||||||
| Basic skills and self-expression—pretest | 31.83 | 4.12 | 24-41 | 33.20 | 5.30 | 22-41 | −1.115∗ | .270 |
| Basic skills and self-expression—post-test | 36.33 | 3.13 | 32-45 | 31.86 | 5.09 | 23-44 | 4.093∗ | < .001 |
| Measurement | F = 26.424†; P < .001 | |||||||
| Measurement × group | F = 89.664†; P < .001 | |||||||
| Attention to communication—pretest | 17.53 | 2.22 | 14-22 | 18.76 | 3.41 | 9-24 | −1.659∗ | .103 |
| Attention to communication—post-test | 19.66 | 1.98 | 16-25 | 17.56 | 3.08 | 9-24 | 3.136∗ | .003 |
| Measurement | F = 5 .818†; P < .05 | |||||||
| Measurement × group | F = 74.207†; P < .001 | |||||||
| Willingness to communicate—pretest | 10.76 | 2.06 | 8-15 | 11.13 | 2.67 | 6-15 | −0.595∗ | .554 |
| Willingness to communicate—post-test | 11.96 | 1.77 | 9-15 | 10.50 | 2.40 | 6-15 | 2.691∗ | .009 |
| Measurement | F = 4.836†; P < .05 | |||||||
| Measurement × group | F = 50.620†; P < .001 | |||||||
| Effective listening and nonverbal- communication—pretest | 18.66 | 2.57 | 14-25 | 18.70 | 3.37 | 12-23 | −0.043∗ | .966 |
| Effective listening and nonverbal- communication—post-test | 20.53 | 2.24 | 16-25 | 18.13 | 3.46 | 12-25 | 3.188∗ | .002 |
| Measurement | F = 10.294†; P < .01 | |||||||
| Measurement × group | F = 36.066†; P < .001 | |||||||
| Following principles of communication—pretest | 10.60 | 2.14 | 7-15 | 11.03 | 2.60 | 6-15 | −0.703∗ | .484 |
| Following principles of communication—post-test | 12.43 | 1.61 | 10-15 | 10.30 | 2.35 | 6-15 | 4.099∗ | < .001 |
| Measurement | F = 14.219†; P < .001 | |||||||
| Measurement × group | F = 77.416†; P < .001 | |||||||
Min-Max, minimum-maximum.
Independent groups t test.
Repeated measures analysis of variance.
Discussion
Emergency nurses are frontline workers facing serious risk, and factors such as growing patient numbers and extended working hours during the pandemic have taken a physical and psychological toll on this group. Nurses are showing negative psychological reactions such as stress-related anxiety and depression, and burnout; lower job satisfaction; and compassion fatigue owing to the increased workload. This demonstrates that nurses need physical, mental, and social support to reduce their psychological burden and enhance the response capacity of the health system.33
Maintaining high job satisfaction is strongly associated with organizational success, professional commitment, and quality care.34 In a cross-sectional study by Yu et al,35 health workers’ job satisfaction scores were found to be higher before the COVID-19 pandemic than during the pandemic. Nia et al36 also reported that the nurses in their study had reduced job satisfaction owing to the higher workload and stated that, to improve job satisfaction levels, nurses must be given adequate time for sleep and rest, and their social lives should be supported. Other authors have also recommended psychosocial interventions to increase levels of job satisfaction in nurses and other health care professionals.37 , 38 A randomized controlled study by Hersch et al39 indicated that a stress-oriented multidisciplinary education program improved job satisfaction among nurses caring for a tiring and challenging patient group. In addition, Choi et al40 reported that hospitals’ motivational plans and practices had positive effects on employees’ job satisfaction. In this study, we determined that emergency nurses who received motivational messages during the COVID-19 pandemic had significantly increased job satisfaction levels, whereas those who did not receive the messages showed a decline in job satisfaction. This suggests that motivation levels must be enhanced to promote high job satisfaction among health workers.
Compassion fatigue is an important issue in the nursing profession, which is based on the need for nurses who will be compassionate and caring toward patients. Preventing compassion fatigue is essential to ensure safe, quality patient care and increase patient and employee satisfaction.41 It has been reported that most emergency nurses experience compassion fatigue and nurses working in surgical units experience moderate burnout and secondary traumatic stress.42 , 43 Barmawi et al44 determined that intensive care nurses experienced compassion fatigue and use both mental and physical avoidance at and outside of work as a coping mechanism and that they needed counseling or motivation to address this. In a study conducted in the current pandemic, health workers in COVID-19 units and emergency departments were found to have higher levels of compassion fatigue than those in other units.45 In our study, we observed significantly lower compassion fatigue levels in emergency nurses who received motivational messages than those who did not. Although compassion fatigue was reported in the literature to be moderately positively associated with positive affect and other personal and social factors, the results of a randomized controlled study indicated that an awareness and training program reduced health workers’ occupational burnout and compassion fatigue.46 Therefore, we believe that in nursing, which is an emotionally and physically challenging profession, nurses must be adequately supported in their professional and social lives, especially during the pandemic, to enable them to work efficiently and avoid a negative impact on the quality of patient care.
Nurses are in direct and continuous contact with patients, and effective communication is both the way nurses provide holistic care to patients and a way to reduce nurses’ burnout and increase their job satisfaction.47 Norful et al48 observed that nurses’ communication and empathy skills declined as their workload increased and that good communication skills were associated with better performance. In another ED study, Rodrigues et al49 reported that after trainings and meetings to improve nursing care activities and restructure communication among the staff, ED dynamics improved significantly and the health care team demonstrated better cooperation and harmony. In a quasi-experimental study conducted with nursing students and aiming to enhance emergency response capability, quality communication and having up-to-date information improved the students’ professional development and had a favorable impact on their practitioner roles.50 In the present study, we observed that participants who received motivational messages had higher scores on the Communication Skills Scale and all of its subscales than those who did not. In line with these studies, it is seen that emergency nurses’ motivation is essential in terms of maintaining their psychosocial well-being. Methods such as asynchronous messaging, digital approaches, and in-person messaging can be used in motivational interventions to reach a wider audience. These are organizational communication methods commonly used to convey motivational interventions.49
Limitations
This study has several limitations. First, our results are limited to the participants in this study and cannot be generalized to all nurses working in emergency units during the COVID-19 pandemic. One reason for this is that shift systems and break times differ among institutions. Second, there may be a possibility of biased sampling. Randomization did not occur to achieve what was intended in equipoise between groups. Third, there may be deviations from the intended intervention (participant forgetting her phone, unable to read messages owing to unmeasurable/unknown clinical priorities, permission was obtained from the head nurse only once for the nurses to read the messages, and permission was not obtained each time). Fourth, the participants could not be blinded owing to the study design. This may cause demoralization in the control group and limit the validity of the results. In addition, the changes in nurses after the intervention could not be evaluated owing to self-report. Therefore, it is recommended to design a blinded study in the future. The fifth limitation is that the demographic characteristics of the nurses differ. Another limitation is that personal protective equipment negatively affects break times. Finally, the study included only day shift nurses. For this reason, it does not provide information about the effects of the intervention on compassion fatigue, job satisfaction, and communication skills among nurses working the night shift. Moreover, overall such messages have a short-term effect.
Implications for Emergency Nurses
Although the increased workload in the emergency services during the pandemic decreased nurses’ job satisfaction, it increased their compassion fatigue.4 Motivation has positive effects on employees.6 In this randomized controlled study, motivational messages were sent to the participants in the intervention group via SMS 3 times a day, and an increase in job satisfaction and communication skills and a decrease in compassion fatigue were found in emergency nurses. Motivation is important and should be provided to increase patient care quality and employee satisfaction. For this purpose, the use of different methods including professional support such as providing motivational interventions specific to workers’ needs and social support consisting of colleagues or head nurses’ solidarity can be considered.
Conclusion
The results of this study suggest that motivational messages sent to emergency nurses during the COVID-19 pandemic increase job satisfaction and improve communication skills while reducing compassion fatigue. Motivational techniques can have a major impact on the mental health of emergency nurses during the pandemic. For this reason, promoting and maintaining high motivation among nurses, especially those with a high work load and those in charge of the care and treatment of critical patient groups, are necessary to avoid psychosocial problems. It is considered that providing psychosocial support via SMS is simple and effective. Studies that provide professional support that is helpful in increasing nurses’ motivation are highly suggested. It is also strongly suggested to conduct studies that provide social support in the form of cooperation among colleagues and head nurses. Large-scale studies with longer follow-up and larger sample groups including night-shift workers are needed to determine the long-term and larger effects of motivational messages.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, (S.G. sonay.goktas@sbu.edu.tr) upon reasonable request.
Acknowledgments
We thank the emergency nurses who participated in the study.
Author Disclosures
Conflicts of interest: none to report.
Biographies
Sonya Goktas is an Associate Professor, Hamidiye Faculty of Nursing, University of Health Sciences Turkey, Istanbul, Turkey. ORCID identifier:https://orcid.org/0000-0002-8168-1287.
Elif Gezginci is an Assistant Professor, Hamidiye Faculty of Nursing, University of Health Sciences Turkey, Istanbul, Turkey. ORCID identifier:https://orcid.org/0000-0003-0392-5298.
Hilal Kartal is a Research Assistant, Ministry of Health, Emergency Health Services Turkey, Istanbul, Turkey. ORCID identifier:https://orcid.org/0000-0002-2432-8620.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jen.2022.06.001.
Supplementary Data
References
- 1.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schreyer K.E., Portal D.D., King L.L., et al. Emergency department management of the COVID-19 pandemic. J Emerg Med. 2020;59(6):946–951. doi: 10.1016/j.jemermed.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aciksari K., Kinik K. Process management and outcomes of the emergency department of a training and research hospital in Turkey during the coronavirus disease 2019 pandemic. Anatol Clin. 2020;25(1):263–283. doi: 10.21673/anadoluklin.740776. [DOI] [Google Scholar]
- 4.Gonzalez-Gil M.T., Blazquez C.G., Moreno A.I., Marcos A., Santos A.P., Garcia L.O. Nurses perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive Crit Care Nurs. 2020;62 doi: 10.1016/j.iccn.2020.102966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ilczak T., Rak M., Cwiertnia M., et al. Predictors of stress among emergency medical personnel during the COVID-19 pandemic. Int J Occup Med Environ Health. 2021;34(2):139–149. doi: 10.13075/ijomeh.1896.01688. [DOI] [PubMed] [Google Scholar]
- 6.Larana M.A., Rodriguez M.E., Hita J.M., Iriarte L.O. Motivation and incentives at work in nursing management. Rev Enferm. 2016;39(9):27–34. [PubMed] [Google Scholar]
- 7.Mudallal R.H., Othman W.M., Hassan N.A. Nurses burnout: the influence of leader empowering behaviors, work conditions, and demographic traits. Inquiry. 2017;54 doi: 10.1177/0046958017724944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Afshar M., Gandomani H.S., Alavi N.M. A study on improving nursing clinical competencies in a surgical department: a participatory action research. Nurs Open. 2020;7(4):1052–1059. doi: 10.1002/nop2.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han J., Kang H.J., Kwon G.H. Impact of intelligent healthscape quality on nurse job outcomes and job satisfaction: a test of the moderating effect of innovativeness. J Nurs Manag. 2020;28(1):43–53. doi: 10.1111/jonm.12875. [DOI] [PubMed] [Google Scholar]
- 10.Barleycorn D. Awareness of secondary traumatic stress in emergency nursing. Emerg Nurs. 2019;27(5):19–22. doi: 10.7748/en.2019.e1957. [DOI] [PubMed] [Google Scholar]
- 11.Nolte A.G., Downing C., Temane A., Tolsma M.H. Compassion fatigue in nurses: a metasynthesis. J Clin Nurs. 2017;26(23-24) doi: 10.1111/jocn.13766. [DOI] [PubMed] [Google Scholar]
- 12.Wentzel D., Brysiewicz P. The consequence of caring too much: compassion fatigue and the trauma nurse. J Emerg Nurs. 2014;40(1):95–97. doi: 10.1016/j.jen.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Sabo B. Reflecting on the concept of compassion fatigue. Online J Issues Nurs. 2011;16(1):1. doi: 10.3912/OJIN.Vol16No01Man01. [DOI] [PubMed] [Google Scholar]
- 14.Bulbuloglu S., Cınar F. The effect of compassion fatigue on care satisfaction in surgical nurses. J Anatolia Nurs Health Sci. 2021;24(2):255–263. doi: 10.1377/hlthaff.2020.00901. [DOI] [Google Scholar]
- 15.Hegney D.G., Craigie M., Hemsworth D., et al. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: study 1 results. J Nurs Manag. 2014;22(4):506–518. doi: 10.1111/jonm.12160. [DOI] [PubMed] [Google Scholar]
- 16.Peters E. Compassion fatigue in nursing: a concept analysis. Nurs Forum. 2018;53(4):466–480. doi: 10.1111/nuf.12274. [DOI] [PubMed] [Google Scholar]
- 17.Figley C.R. Compassion fatigue: psychotherapists’ chronic lack of self care. J Clin Psychol. 2002;58(11):1433–1441. doi: 10.1002/jclp.10090. [DOI] [PubMed] [Google Scholar]
- 18.Perregrini M. Combating compassion fatigue. Nursing. 2019;49(2):50–54. doi: 10.1097/01.NURSE.0000552704.58125.fa. [DOI] [PubMed] [Google Scholar]
- 19.Magnavita N., Soave P.M., Antonelli M. A one-year prospective study of work-related mental health in the intensivists of a COVID-19 hub hospital. Int J Environ Res Public Health. 2021;18(18):9888. doi: 10.3390/ijerph18189888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werner E.A., Aloisio C.E., Butler A.D., et al. Addressing mental health in patients and providers during the COVID-19 pandemic. Semin Perinatol. 2020;44(7) doi: 10.1016/j.semperi.2020.151279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Kalaldeh M., Amro N., Qtait M., Alwawi A. Barriers to effective nurse-patient communication in the emergency department. Emerge Nurse. 2020;28(3):29–35. doi: 10.7748/en.2020.e1969. [DOI] [PubMed] [Google Scholar]
- 22.Khoo V.P.H., Ting R.S.K., Wang X., et al. Risk and protective factors for the mental wellbeing of deployed healthcare workers during the COVID-19 pandemic in China: a qualitative study. Front Psychol. 2021;12:1–16. doi: 10.3389/fpsyg.2021.773510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirik A.M., Sonmez M. The examination of relationship between communication and happiness. INIF E Journal. 2017;2(1):15–26. [Google Scholar]
- 24.Kandemir H., Ozdasli K. The effect of positive ınformel communication on empowerment and work place happiness: a research on research assistants. International Journal of Euroasian Research. 2019;7(18):242–258. doi: 10.33692/avrasyad.695376. [DOI] [Google Scholar]
- 25.Shin K.Y., Lee J.M., Kang P., Seol G.H., Seol G.H. Effects of short-term ınhalation of patchouli oil on professional quality of life and stress levels in emergency nurses: a randomized controlled trial. J Altern Complement Med. 2020;26(11):1032–1038. doi: 10.1089/acm.2020.0206. [DOI] [PubMed] [Google Scholar]
- 26.True random number service. Haahr M. https://www.random.org/
- 27.Fernandez M.D., Pichardo J.D., Masero I., Troya J.C., Rega M.I., Galan A.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. 2020;29(21-22):4321–4330. doi: 10.1111/jocn.15469. [DOI] [PubMed] [Google Scholar]
- 28.Steinberg B.A., Klatt M., Duchemin A.M. Feasıbılıty of a mındfulness-based ınterventıon for surgıcal ıntensıve care unıt personnel. Am J Crit Care. 2020;26(1):10–18. doi: 10.4037/ajcc2017444. [DOI] [PubMed] [Google Scholar]
- 29.Keser A., Bilir B.O. Turkish reliability and validity study of job satisfaction scale. Kırklareli Unıversity J Soc Sci. 2019;3(3):229–239. [Google Scholar]
- 30.Dinc S., Ekinci M. Adaptation, validity and reliability of the compassion fatigue short scale into Turkish. Curr Approaches Psychiatry. 2019;11(1):192–202. doi: 10.18863/pgy.590616. [DOI] [Google Scholar]
- 31.Korkut-Owen F., Bugay A. Developing a communication skills scale: validity and reliability studies. J Mersin University Faculty of Education. 2014;10(2):51–64. [Google Scholar]
- 32.Davis L.L. Instrument review: getting the most from a panel of experts. Appl Nurs Res. 1992;5(4):194–197. doi: 10.1016/S0897-1897(05)80008-4. [DOI] [Google Scholar]
- 33.Karampelias V., Karonis D., Psaroudi V. The psycho-emotional impact of COVID-19 on surgical staff working in emergency departments. Eur J Trauma Emerg Surg. 2020;46(4):747–749. doi: 10.1007/s00068-020-01411-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Labrague L.J., Santos J.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. 2021;29(3):395–403. doi: 10.1111/jonm.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu X., Zhao Y., Li Y., et al. Factors associated with job satisfaction of frontline medical staff fighting against COVID-19: a cross-sectional study in China. Front Public Health. 2020;8:426. doi: 10.3389/fpubh.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nia H.S., Arslan G., Naghavi N., et al. A model of nurses’ intention to care of patients with COVID-19: mediating roles of job satisfaction and organisational commitment. J Clin Nurs. 2021;30(11-12):1684–1693. doi: 10.1111/jocn.15723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sperling D. Ethical dilemmas, perceived risk, and motivation among nurses during the COVID-19 pandemic. Nurs Ethics. 2020;28(1):9–22. doi: 10.1177/0969733020956376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Halcomb E., Smyth E., McInnes S. Job satisfaction and career intentions of registered nurses in primary health care: an integrative review. BMC Fam Pract. 2018;19(1):136. doi: 10.1186/s12875-018-0819-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hersch R.K., Cook R.F., Deitz D.K. Reducing nurses’ tress: A randomized controlled trial of a web-based stress management program for nurses. Appl Nurs Res. 2017;32:18–25. doi: 10.1016/j.apnr.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choi S.L., Goh C.F., Adam M.B.H., Tan O.K. Transformational leadership, empowerment, and job satisfaction: the mediating role of employee empowerment. Hum Resour Health. 2016;14(1):73. doi: 10.1186/s12960-016-0171-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bellagamba C., Gionta G., Senergue J., Bèque C., Cher-Michel M.P. Organizational factors impacting job strain and mental quality of life in emergency and critical care units. Int J Occup Med Environ Health. 2015;28(2):357–367. doi: 10.13075/ijomeh.1896.00121. [DOI] [PubMed] [Google Scholar]
- 42.Borges E.M., Fonseca C.I., Baptista P.C., Queiros C.M., Mosteiro M.B., Diaz M.P. Compassion fatigue among nurses working on an adult emergency and urgent care unit. Rev Lat-Am Enferm. 2019;27:3175. doi: 10.1590/1518-8345.2973.3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Babaei S., Haratian M. Compassion satisfaction and fatigue in cardiovascular nurses: a cross-sectional descriptive study. Iran J Nurs Midwif Res. 2020;25(3):212–216. doi: 10.4103/ijnmr.IJNMR_112_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barmawi M.A., Subih M., Salameh O., Sayyah N.S., Shogirat N., Jebbeh R.A. Coping strategies as moderating factors to compassion fatigue among critical care nurses. Brain Behav. 2019;9(4):1264. doi: 10.1002/brb3.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trumello C., Bramanti S.M., Ballarotto G., et al. Psychological adjustment of healthcare workers in Italy during the COVID-19 pandemic: differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. Int J Environ Res Public Health. 2020;17(22):8358. doi: 10.3390/ijerph17228358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Auseran G.A., Viscarret M.R., Goni C.F., Güeto Rubio V., Pascual Pascual P., Sainz de Murieta García de Galdeano E. Evaluation of the effectiveness of a mindfulness and self-compassion program to reduce stress and prevent burnout in primary care health professionals. Aten Prim. 2018;50(3):141–150. doi: 10.1016/j.aprim.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jurado M.D., Peco I.H., Fuentes-Perez M.C., et al. Communication and humanization of care: effects over burnout on nurses. PLoS One. 2021;16(6) doi: 10.1371/journal.pone.0251936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Norful A.A., Jacq K., Carlino R., Poghosvan L. Nurse practitioner-physician comanagement: a theoretical model to alleviate primary care strain. Ann Fam Med. 2018;16(3):250–256. doi: 10.1370/afm.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodrigues M.E., Belarmino A.C., Custodio L.L., Gomes I.L.V., Ferreira Júnior A.R. Communication in health work during the COVID-19 pandemic. Investig Educ Enferm. 2020;38(3):e09. doi: 10.17533/udea.iee.v38n3e09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kose S., Akin S., Mendi O., Goktas S. The effectiveness of basic life support training on nursing students’ knowledge and basic life support practices: a non-randomized quasi-experimental study. Afr Health Sci. 2019;19(2):2252–2262. doi: 10.4314/ahs.v19i2.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, (S.G. sonay.goktas@sbu.edu.tr) upon reasonable request.