Abstract
In April 2020, the Ministry of Health (MoH) in Oman, a high-income country in the Eastern Mediterranean Region (EMR), implemented a robust contact tracing (CT) system for COVID-19. To capitalise on Oman’s experience, EMRO has developed a case study presenting the methodology used to conduct the CT activities, main functions of the system, challenges encountered, lessons learnt, and the way forward. To develop the case study, a key informant interview was conducted virtually with the CT focal point in the MoH, using a semistructured questionnaire adapted from the WHO questionnaire for the assessment of CT activities. The Oman MoH launched a CT system based on three complementary digital tools: Tarassud plus, Medical Scout and HMushrif applications. Oman’s CT strategy classifies contacts into close and casual contacts. Only close contacts are listed using the Tarassud plus application, while casual contacts are requested to self-monitor for 14 days using the other two applications. With the evolution of the outbreak, Oman MoH implemented stricter policies and prioritised the follow-up of close contacts to keep the CT activity manageable. Community health workers and volunteers facilitated the CT activities through sensitisation of the local community to the follow-up process and reducing the COVID-19-associated stigma. Challenges encountered revolved around contact data management, given the offline in-operability of the applications, and lack of national risk communication guidelines to address community concerns and widespread rumours.
Keywords: COVID-19, epidemiology
Summary box.
The strengths of this case study include introduction of a novel approach integrates a locally developed digital tool to support contact tracing (CT) activities; approach to contact prioritisation during community transmission; and provision of a qualitative approach that allows in-depth analysis of CT strengths and weaknesses in Oman.
The major limitation of our case study is that data on CT indicators were available for 7 months only. Other challenges are; low laboratory capacity thus not all contacts were tested; poor offline capabilities of Tarassud plus; centralised data storing system; no national risk communication guidelines to address community concerns.
Introduction
COVID-19 is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus experience mild to moderate respiratory illness and recover without requiring special treatment. The virus can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing or breathe.1 SARS-CoV-2 infections have been attributed to relatively few individuals in high-transmission settings. Subsequently, case identification is a cornerstone for identifying further unrecognised chains of transmission and common points of exposure.2
Contact tracing (CT) is the process of identifying, assessing and managing people who have been exposed to someone who has been infected with the COVID-19 virus. CT and quarantine of contacts identified through CT aim at interrupting transmission between people and are essential public health tools for controlling the virus spread. CT also permits identifying earlier people who are at a higher risk of developing severe disease to get medical care quickly once they develop symptoms.3
CT has been identified by WHO as an effective intervention together with vigorous testing and proper management of cases to curb the transmission of COVID-19.2 Disease transmission will be prevented through a multi-levelled process of identifying, assessing and managing people who may be exposed to the disease.
COVID-19 is a disease that requires identification of those who may have been infected and who will need follow-up for 14 days after exposure. Despite the continuous vaccination efforts worldwide, it is essential to continue CT and quarantine contacts to control transmission.2
CT process for respiratory diseases such as COVID-19 requires extensive human and financial resources and should be implemented in a stepwise approach depending on the availability of these resources and transmission scenarios. Such a phased approach has been witnessed in many countries through prioritising specific high-risk settings with vulnerable individuals, such as hospitals, nursing homes (eg, dormitories).3
The WHO recommends prioritisation of CT activities according to country transmission scenarios. SARS-CoV-2 transmission status is characterised into four epidemiological scenarios, with the last one accommodating four sub-categories. Strategies for CT need to be tailored in accordance with the local transmission dynamics and response capacity and should have the dynamicity to adapt to the context and emerging trends (see table 1).3 4
Table 1.
COVID-19 transmission scenarios and implementation of CT activities, from the WHO guidance for contact tracing, 1 February 20216
| Epidemiological scenario | CT activities |
| No cases | Identifying and training existing personnel and preparing them for deployment and response. |
| Sporadic cases | Exhaustive strategies should be implemented. Case investigation for all cases is necessary for timely suppression of transmission. |
| Clusters | CT is required to suppress transmission within clusters and recognise events that contribute to transmission. These events can be mitigated by different Public Health and Social Measures. |
| Community transmission (including four subcategories of increasing incidence) | Despite challenges, CT remains crucial, particularly in high incidence scenarios. CT should continue and focus on high-risk exposure contacts in accordance with the available capacities |
CT in the Eastern Mediterranean Region (EMR) is facing a multitude of obstacles. According to an unpublished review conducted among EMR Member states, the main challenges identified are lack of resources (human and/or financial) for the sustainability of CT activities, difficulties for training CT teams because of physical distancing/ lockdown measures, difficulty to scale-up CT in emergency/conflict settings, and insufficient community compliance to contact follow-up and public health and social measure (PHSM).
SARS-CoV-2 was first detected in Oman on 24 February 2020. By 20 May 2021, 208 607 confirmed cases were reported, including 2239 deaths (case-fatality ratio of 1.1%).5 Five per cent of patients required hospitalisation. About 64% of the confirmed COVID-19 cases were between the ages of 25 and 44 years with overall male to female (M:F) ratio of 2.4. The M:F sex ratio was higher among expatriates,6 who constitute about 38% of Oman population7 (3.6 vs 1.5 for nationals).
During the first peak of the outbreak in Oman, which was reached in mid-July 2020, there were more than 65 000 confirmed cases and over 300 deaths.5 Then, the country transitioned into community transmission of COVID-19, and the number of contacts for follow-up grew exponentially. CT capacity has consequently been scaled up, including the use of digital proximity tracking solutions.8
This case study aims to describe Oman’s implementation of digital solutions and other strategies to augment CT activities during the widespread transmission of COVID-19. Annexes 1 and 2 provide details regarding the methods used.
Description of CT methodology in Oman
As part of their digital transformation away from traditional paper-based methods, the MoH launched a CT system based on three complementary digital tools: the Tarassud plus,9 Medical Scout and HMushrif applications.10 All contacts of laboratory-confirmed or probable COVID-19 cases were advised to instal all three applications that manage the different steps of CT synergistically on their smartphones.
Contact prioritisation
CT is conducted by the MoH Directorate General of Disease Surveillance and Control (DGDSC). Oman’s CT strategy classifies contacts into close and casual contacts. Close contacts are those who present with either of the following scenarios11 12:
Anyone within 2 m for >15 min of a COVID-19 patient.
Direct physical contact with a COVID-19 patient.
Provision of direct care for a COVID-19 patient at home without proper personal protective equipment (PPE).
An exposure through living in the same household with a COVID-19 patient within 14 days from the onset of symptoms in the patient.
Only close contacts are monitored and entered in Tarassud plus application, while casual contacts are requested to self-monitor for 14 days using the other two applications. With the evolution of the outbreak, Oman MoH implemented stricter policies and prioritised the follow-up of close contacts to keep the CT activity manageable.11
Contact identification and listing
Tarassud plus serves as the mandatory platform for contacts and case listing to ensure proper follow-up and documentation by public health authorities (primary healthcare unit).
All cases and close contacts are interviewed in person (face to face) or by telephone if an in-person meeting is not possible. Case investigation and contact listing forms have been developed for both cases and contacts, and adapted into the Tarassud plus application.
Contact follow-up
Prior to the initiation of contact follow-up, all contacts sign a consent form in which they agree to comply with CT directives. The Medical Scout application sends daily messages to contacts to inquire about any symptoms they may have developed, allows users to fill information on any comorbidities/risk factors (≥60 years old, diabetes, hypertension, chronic heart, lung, renal and liver diseases, immunosuppressed patients, pregnant women, etc) and performs an automated risk assessment.
In addition, the HMushrif application is used to track contacts, detect any violations of CT directives, and alert of potential new close contact with infected cases using the proximity tools.
A hotline has been launched to provide contacts with advice on quarantine and eventual testing if needed, and to collect information on non respect of mandatory isolation/quarantine measures. Furthermore, follow-up calls are conducted periodically during the 14-day quarantine to check for symptoms and ensure compliance.
Isolation and quarantine
Confirmed or probable cases are isolated at least 10 days after last contact with a COVID-19 case, including the 24 hours before symptoms, while contacts are quarantined for 14 days. If contacts develop symptoms, they are instructed to contact a medical facility to receive medical advice. Testing is not organised systematically for symptomatic contacts unless they have comorbidities that classify them as high-risk contacts; otherwise, they are classified as a probable case and isolated. Contacts are not quarantined in collective facilities but sign engagement forms to ensure compliance with self-quarantine.
CT indicators
Key COVID-19 CT indicators were collected from eleven governorates between 1 August 2020 and 28 February 2021 by the DGDSC. Most of the governorates reported high proportion of contact follow-up through the mobile applications.
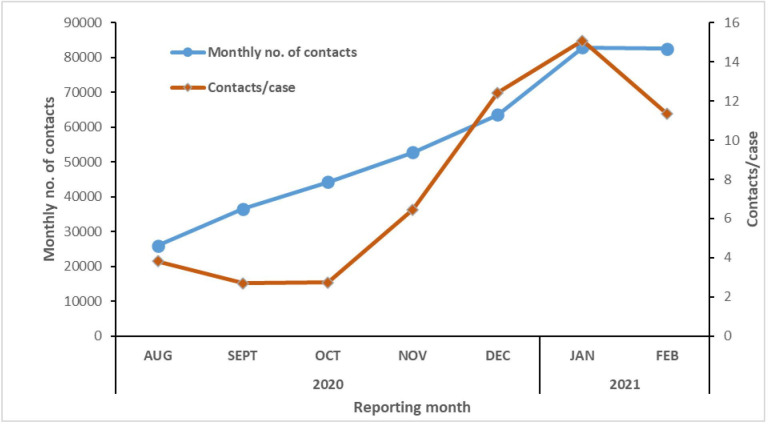
A total of 388 563 contacts for 62 649 probable and confirmed cases were followed up. The number of contacts under follow-up increased regularly from August 2020 to January 2021. In the meantime, the number of contacts per case has dropped from five at the beginning of the outbreak to around two in October 2020, then started to rise again from November 2020 to January 2021 (figure 1).
Figure 1.
Numbers of identified COVID-19 contacts and contacts per case overtime, Oman August 2020–February 2021.
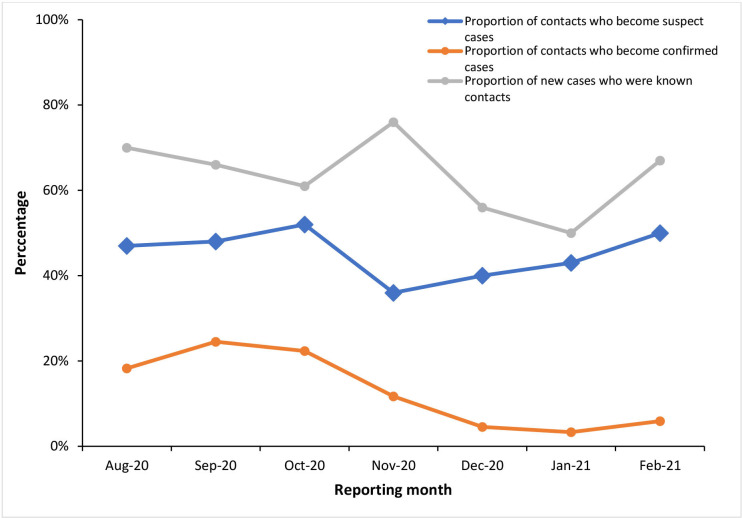
The monthly proportion of contacts who became suspect cases was stable around 50% in August–October 2020, then decreased and increased again to reach 50% in February 2021.
The monthly proportion of contacts who became confirmed cases was around 20% until October 2020 and then dropped to less than 10%.
A high proportion of new cases were under monitoring before they occurred: between 50% and 76% new cases were contacts under the follow-up (see figure 2).
Figure 2.
Contact tracing indicators, Oman, August 2020–February 2021
The average time from symptom onset to case confirmation among contacts was 24 hours (see table 2).
Table 2.
Key contact tracing indicators for COVID-19 in Oman (August 2020–February 2021)
| Proportion of contacts who become suspect cases | Proportion of contacts who become confirmed cases | Proportion of new cases who are known contacts | Time from symptom onset to case confirmation | |
| August-20 | 47% (12 299/25 906) | 18% (4738/25 906) | 70% (4738/6769) | Average 24 hours |
| September-20 | 48% (17 589/36 534) | 25% (8960/36 534) | 66% (8960/13 575) | |
| October-20 | 52% (23 087/44 284) | 22% (9901/44 284) | 61% (9901/16 231) | |
| November-20 | 36% (19 185/52 750) | 12% (6175/52 750) | 76% (6175/8174) | |
| December-20 | 40% (25 265/63 554) | 5% (2876/63 554) | 56% (2876/5116) | |
| January-21 | 43% (63 554/82 934) | 3% (2753/82 934) | 50% (2 753/5500) | |
| February-21 | 50% (40 898/82 601) | 6% (4873/82 601) | 67% (4873/7284) |
Best practices
Community-centred CT
Community health workers (CHWs), volunteers and local authorities facilitate CT activities through sensitisation of the local community to the follow-up process to reduce COVID-19-associated stigma. Community engagement was also done via traditional media (television, radio), social media and proximity sensitisation in schools. In parallel, CHWs advocated for enhancing CT compliance within their respective communities. The capacity building of contact tracers was transitioned from the national to sub-national levels, permitting the rapid deployment of a high number of CT teams. MoH developed guidelines for community CT and deisolation throughout the pandemic. Globally, the deployment of CHWs for CT has proven to be ‘invaluable’, helping the MOH to overcome myriad CT failures, leading to more successful outcomes.12
Adaptable strategic CT guidelines
Early in the COVID-19 pandemic, Oman’s MoH developed National Contact Tracing Guidelines. These guidelines were flexible enough to adopt modifications in the duration of isolation and quarantine periods based on the new and emerging evidence to limit unnecessarily prolonged isolation and overuse of limited laboratory resources. Furthermore, guidelines were adjusted to reflect the adoption of digital CT as a complement to traditional CT. Such agility and dynamicity of the CT response were pivotal to the outcomes achieved.
Redeploying workforce
CT is undertaken by primary healthcare staff in collaboration with the DGDSC team at the governorate level. It is the responsibility of the above-designated team to identify, follow and monitor the contacts. Initially, staff such as school nurses were mobilised to assist with CT activities at the governorate level. Subsequently, as community transmission set in, these staff were repurposed and assigned to COVID-19 treatment centres to help with case management.
Local digital solutions
Three apps were developed to support the CT activities. Tarassud plus application was developed by MoH, Medical Scout application was developed by a global company (Al Burkan Company), and HMushrif application was developed by a local company (E Mushrif Company). They were launched to replace paper-based data management systems. All three platforms were linked by a unique code (civil registration number) to facilitate interoperability. A significant strength of this data management platform is its accessibility to users. Community members can freely access the platform to update their information and view their COVID-19 test results or vaccination status. Another advantage is the ease of access by key stakeholders such as private hospitals, laboratories, etc. This allows for intersectoral collaboration and reduces the work burden on MoH staff. Before being implemented in Oman, this approach was not widespread in the EMR. However, similar approaches for CT were being used worldwide with each having their own tools to ensure the most feasible level of data protection possible.13
Ethical considerations
Anticipating concerns raised by digital CT, Oman’s MoH trained platform operators on the importance of privacy and confidentiality. Moreover, measures for data protection included; geographical restriction of access and voluntary user data sharing using a one-time pin. Oman MoH is the owner of the applications, and the only people that could access the data for health-related purposes.
Challenges
One of the main challenges encountered revolved around contacts data management, given the limited offline operability of the applications. In areas where internet connectivity is low, operators relied on a two-step approach, first collecting data on paper and subsequently entering it into the system.
In addition, Oman MoH lacked national risk communication guidelines to address community concerns and widespread rumours. Fatigue associated with the implementation of COVID-19 PHSMs tended to increase a feeling of distrust which manifests itself with a larger proportion of responders expressing fear, anxiety, distrust and who can at times be aggressive or reluctant to cooperate. However, community leaders played a great role in quelling such situations and facilitating access of tracers to cases/contacts within their communities.
Another issue is that the system is highly centralised, with all data stored on a single server. This leaves the system vulnerable to privacy breaches (piracy) and raises ethical concerns. However, measures have been put in place to restrict access of operators and their supervisors. At the moment, access restrictions have been put in place based on geographical location, that is, district level operators can only see data of cases within their district, governorate level supervisors only manage data of their governorate, and finally, the national level operators serves as system administrators.
CT indicators and lessons learnt
Proportion of contacts seen and proportion of contacts lost to follow-up
All of the identified contacts of COVID-19 cases that occurred between August 2020 and February 2021 were followed up. Despite this high value, it is worth mentioning that the number of identified contacts per case decreased progressively from five at the beginning of the outbreak to around two on October 2020, then started to rise again until January 2021. With all these changes in the situation, the system was efficient enough to keep the 100% completeness of contact follow-up. This could be attributed to the role played by the digital solutions that accommodated the increasing number of contacts over time, in addition to the acceptance and compliance of Oman population to the implemented follow-up modality.
Proportion of contacts who became suspect and confirmed cases
The monthly proportion of contacts who became suspect and confirmed cases ranged from 36% to 52% and 3% to 25%, respectively. These figures are highly dependent on the national COVID-19 testing strategies in Oman. It is worth mentioning that a progressive decline was observed in the monthly proportion of contacts who became confirmed cases as the monthly number of newly confirmed cases decreased.
Proportion of new cases who are known contacts
The proportion of new COVID-19 cases who were identified among contacts ranged from 50% to 76%. This demonstrates the importance of Oman’s CT strategy in early detection and isolation of secondary cases. This also means the contact history of 24%–50% has not been identified and may have played a role in spreading the virus and the persistence of community transmission of COVID-19. This proportion was a little bit higher than what was reported by the Virginia Department of Health in the United States, where the percent of cases with known contact history was almost around 50%.14
Conclusion
The COVID-19 pandemic has posed a significant burden on health systems worldwide. For this reason, the utilisation of digital technologies has become a necessity in managing the pandemic. Oman implemented a robust CT system for COVID-19 supplementing traditional CT with digital tools. In a bid to share its experience with other countries within the EMR, we have described their methodology, the main functions of the system, challenges encountered and lessons learnt. Although the implementation of CT remains a challenging process, Oman’s experience was remarkable as an evidence-based model adapted to the dynamic nature of the pandemic and could be replicated in other countries.
bmjgh-2022-008724supp001.pdf (75.8KB, pdf)
bmjgh-2022-008724supp002.pdf (83.5KB, pdf)
Acknowledgments
The authors are very thankful to Oman's MoH team and the Directorate General of Disease Surveillance and Control (DGDSC) for their valuable help in obtaining the required administrative authorisations. To be thanked too are all those who gave up their valuable time to participate in this work.
Footnotes
Handling editor: Seye Abimbola
Twitter: @ataboushady
Contributors: MS, FCA, MT, ATA and PN participated in study conception and design. MS, FCA, ATA, MT and BAA collected the data, conducted their analysis and drafted the manuscript. AAM, MA, LM and JJ reviewed and revised the manuscript. All authors read and approved the final manuscript. MS is the guarantor of this study.
Funding: This study was sponsored by the WHO Regional Office for the Eastern Mediterranean (WHO EMRO)
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
A formal ethical approval was not required for this work. However, administrative authorisations were obtained from Oman's MOH prior to interviews, and clearance was given by the WHO country and regional EMRO team. Ethical clearance was also obtained from all health district medical officers and health facility directories. All communications with the MOH were handled confidentially, and key informants provided informed consent before participating in interviews.
References
- 1.World Health Organization, COVID-19 [online], 2021. Available: https://www.who.int/health-topics/coronavirus#tab=tab_1 [Accessed 10 Dec 2021].
- 2.World Health Organization & UNICEF . The role of community health workers in COVID-19 vaccination: implementation support guide, 26 April 2021. Geneva: World Health Organization, 2021. [Google Scholar]
- 3.World Health Organization . Contact tracing in the context of COVID-19 [online], 2021. Available: https://www.who.int/publications/i/item/contact-tracing-in-the-context-of-covid-19
- 4.World Health Organization . Contact tracing [online], 2021. Available: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-contact-tracing [Accessed 10 Dec 2021].
- 5.World Health Organization EMRO . EMRO COVID-19 dashboard [online], 2021. Available: https://app.powerbi.com/view?r=eyJrIjoiN2ExNWI3ZGQtZDk3My00YzE2LWFjYmQtNGMwZjk0OWQ1MjFhIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9
- 6.WHO EMRO . Home EMFLU [online], 2021. Available: https://emflu.emro.who.int/
- 7.Oman National Center of Statistics and Information [online], 2021. Available: https://www.ncsi.gov.om/Pages/AllIndicators.aspx [Accessed 13 Oct 2021].
- 8.World Health Organization . Coronavirus disease (COVID-19). Situation report - 181 [online], 2021. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200719-covid-19-sitrep-181.pdf?sfvrsn=82352496_2
- 9.Oman Government Portal . Oman, MoH Tarassud plus [online], 2021. Available: https://omanuna.oman.om/en/government-mobile-apps/tarassud
- 10.Oman, Ministry of Health Mushrif . Registration [online], 2021. Available: https://covid19.emushrif.om/
- 11.Oman Minsitry of Health . Guideline for Home/Institutional Isolation For COVID-19. Muscat [online], 2021. Available: https://www.moh.gov.om/documents/10194/3903020/Isolation+guideline+April+5.pdf/d58faba3-fe33-58e0-b070-841ebb1e4e37
- 12.Oman, MoH Portal . Household & community contact tracing & de-isolation guideline for COVID-19 [online], 2021. Available: https://www.moh.gov.om/documents/10194/3903020/latest+contact+tracing+guideline.pdf/da85f413-56c6-4ea6-7a56-80c7367c1f4c
- 13.Budd J, Miller BS, Manning EM, et al. Digital technologies in the public-health response to COVID-19. Nat Med 2020;26:1183–92. 10.1038/s41591-020-1011-4 [DOI] [PubMed] [Google Scholar]
- 14.Virginia Department of Health . COVID-19 contact tracing indicators [online], 2021. Available: https://www.vdh.virginia.gov/coronavirus/covid-19-data-insights/covid-19-contact-tracing/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-008724supp001.pdf (75.8KB, pdf)
bmjgh-2022-008724supp002.pdf (83.5KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.