Abstract
Background:
An assessment of the level of adherence of patients diagnosed with hypertension to therapy has not been conducted in Central Asia yet. It includes the lack the information on the impact of digital technologies on hypertension management.
Objective:
The study aimed at the evaluation of the effect of using a mobile application on adherence to therapy in patients with diagnosed arterial hypertension.
Methods:
A multi-centre randomized controlled study was conducted on 517 patients with diagnosed arterial hypertension (in the out-patient clinic, Almaty, Kazakhstan). Patients were randomly assigned to intervention (IG) and control (CG) groups. IG patients used a mobile application, which allowed creating an individual schedule for taking medications, including visual and audio notifications. The assessment of adherence to antihypertensive treatment was carried out using the Lebanese Medication Adherence Scale-14 (LMAS-14), consisting of 14 items. Data were collected before therapy (T1), 3 months (T2), 6 months (T3) and 12 months (T4) followed the first dose. Adherence was assessed on 101 patients in the CG group and 165 respondents in the IG group.
Results:
In the period T1 in both groups CG and IG, a moderate adherence to treatment was recorded with indices equal to 35.9 ± 1.2 and 35.9 ± 1.3, respectively (p ≤ 0.05). A decrease in adherence in the CG group was determined after 3 months (35.9 ± 1.2) (p ≤ 0.05) and six months later (36.5 ± 3.2) in comparison with relatively high adherence among respondents in the IG group in periods T2 (39.5 ± 1.2) and T3 (40.5 ± 1.2) (p ≤ 0.001). After 12 months (T4) on the adherence scale in patients who used the mobile application “MyTherapy” (IG), despite a slight decrease in scores, the results were relatively higher (40.3 ± 1.3) compared with the CG group (33.6 ± 1.9) (p ≤ 0.001).
Conclusion:
The analysis of adherence of patients with primary health care in Almaty (Kazakhstan) with chronic arterial hypertension showed the effectiveness of using the ‘MyTherapy’ mobile application in increasing patient adherence. The obtained data on the positive effect of the use of digital technologies require further research to assess the possibility of wider implementation in healthcare.
Keywords: Telemedicine, adherence, arterial hypertension, mobile app
1. BACKGROUND
Non-communicable diseases are the cause of forty-one million deaths annually, which is equivalent to 71% of all deaths in the world. Cardiovascular diseases account for 17.9 million deaths per year (1). The increase in the number of chronic diseases resulted in the growth of financial expenditures in the healthcare systems worldwide (2) . One of the reasons for the increase in mortality rate from certain diseases has been associated with low adherence to therapy (3) as a result of lack of proper cooperation between doctor and patient (4). Non-adherence to therapy is a critical factor contributing to the low success of therapy in many chronic diseases (5).
A similar situation has been observed with arterial hypertension. This chronic disease can be treated by lifestyle changes and a high adherence to prescribed therapy (6). Thus, adherence to antihypertensive drugs remains a key modifiable factor in the treatment of hypertension. In fact, the lack of adherence to treatment is not only a known behavioural, but also an underestimated factor contributing to inadequate blood pressure control in the treatment of hypertensive patients (7).
Despite the significant progress in the diagnostics and treatment of hypertension almost 30 % of adult patients taking antihypertensive drugs have uncontrolled blood pressure, which may indicate a low therapeutic adherence (8). According to the available data, many factors can affect the adherence of patients with hypertension such as a low educational level, side effects of drugs, cognitive impairment, socioeconomic status, unavailability of drugs and the lack of proper instructions for the use of medicines (7, 9). According to a meta-analysis conducted by Abegaz et al. (28 studies with only arterial hypertension patients conducted in 15 countries), the frequency of non-compliance with medical recommendations in patients with arterial hypertension is 45.2% that indicates a rather low proportion of patients adherence to treatment (10).
Digital technologies are showing their effectiveness and applicability in improvement of medication adherence of some chronic diseases (11). Previously published studies assessing the effectiveness of the use of digital technologies (mHealth by using phone calls and text messaging) for monitoring cardiovascular diseases showed a positive effect of increasing adherence compared to patients who received standard health care (12). In particular, some studies demonstrated that the use of mobile applications for controlling the adherence of patients with arterial hypertension can be effective (13). Such mobile apps encompass hypertension education, monitoring blood pressure levels, and tools to promote medication adherence (14). However, the effectiveness of mobile apps is not clear (15).
COVID-19 pandemic forced commercial companies and higher educational institutions to make a sharp transition to a remote format of work using video conferencing and other digital solutions (16). However, the healthcare system is still coping with this crisis using classic approaches such as risky patient visits (17). Despite the recent progress in digital health technologies, the full capacity of telemedicine has not been exploited and implemented worldwide yet (18). At present, mobile gadgets continue to expand their functionality with more intelligent and versatile developments, including mobile applications for e-health (19). In regard to the epidemiological situation with COVID-19, healthcare institutions have been gaining experience in the wider implementation of telemedicine in the process of providing medical care to patients (20).
However, there are still problems with patients’ access to virtual communication tools (21) and regulation of this type of medical care at the governmental level (18, 22). The digital revolution in the medical field opens up great prospects, but success depends not only on timely implementation, but also on its productivity and efficacy in daily practice (23).
In this regard, the effective implementation and practical application of such electronic applications in primary healthcare facilities are highly critical, particularly during the COVID-19 pandemic (17, 24). Health digital technologies can help to reduce the number of patient’ visits to medical institutions (25), thus reducing the risk of infection (26, 27). Nevertheless, there is a lack of studies covering at least 12 month follow-up period of using health digital technologies (28).
It should be also noted that some studies have been mainly focussed on the assessment of the effectiveness of telemedicine and remote interaction for monitoring the conditions of patients with arterial hypertension (29). So there is still a need for further research to determine the effect of innovative technologies on clinical outcomes (30).
To the best of our knowledge, nationwide research on the prevalence of arterial hypertension has not been conducted on the territory of Kazakhstan yet. Nonetheless, there are a few studies, which were limited to a small cohort of the population. The results of such studies demonstrated a high frequency of registration of hypertension and inadequate adherence to the prescribed treatment (31, 32). Apart from that, it should be also mentioned that the assessment of the level of adherence of patients with hypertension to therapy, as well as the impact of digital technologies on its improvement, has not been conducted in Central Asia yet.
2. OBJECTIVE
The aim of this study was to validate the possibility of using a mobile application and its impact on adherence to therapy in patients with diagnosed arterial hypertension (in the out-patient clinic). In addition, the validity and reliability of a structured scale for assessing adherence in patients with arterial hypertension was also scrutinized.
3. PATIENTS AND METHODS
3.1. Study design
A multi-centre randomized clinical trial was conducted in Almaty city (Republic of Kazakhstan). The object of the study was persons with diagnosed arterial hypertension who were treated in the outpatient policlinics of Almaty, the largest city in the Republic of Kazakhstan. Almaty city consists of eight districts (Bostandyk, Auezov, Almaly, Medeu, Turksib, Zhetysu, Alatau, and Nauryzbay). Healthcare for all districts is provided by 34 policlinics. Seven policlinics refused to participate in the study. We randomly selected two policlinics from each district, except Bostandyk district.
3.2. Ethical Issues
The study was approved by the High Ethics committee of S.D. Asfendiyarov Kazakh National Medical University, Almaty, Kazakhstan (Local Ethics Commission Approval No 13(104), dated 25.11.2019).
3.3. Study participants
Patients aged 18 to 75 years old diagnosed with arterial hypertension were allowed to participate in the study. The presence of high blood pressure was confirmed by recorded systolic blood pressure of 140 mm Hg, and diastolic blood pressure of 90 mm Hg (measured on both hands in sitting position) (33).
Inclusion criteria were as follows: the signed informed consent for participation in the study, patients with a confirmed diagnosis of arterial hypertension, the administration of at least one antihypertensive drug regimen, and the possession of a smartphone with an Android or iOS operating systems. Exclusion criterion: children under 18 years of age, pregnant women, disability due to mental or cognitive impairments, technical difficulties in downloading and using the mobile application.
The study design was based on the standard methodology developed by the CONSORT team. The study was conducted in accordance with the Consolidated Reporting Standards for Testing Electronic and Mobile Health and Online Telemedicine Applications. In this study a matched pairs design, considering age and period of illness as potential confounders was used. Thus, in our study, we controlled for two potential hidden variables–age and duration of the arterial hypertension.
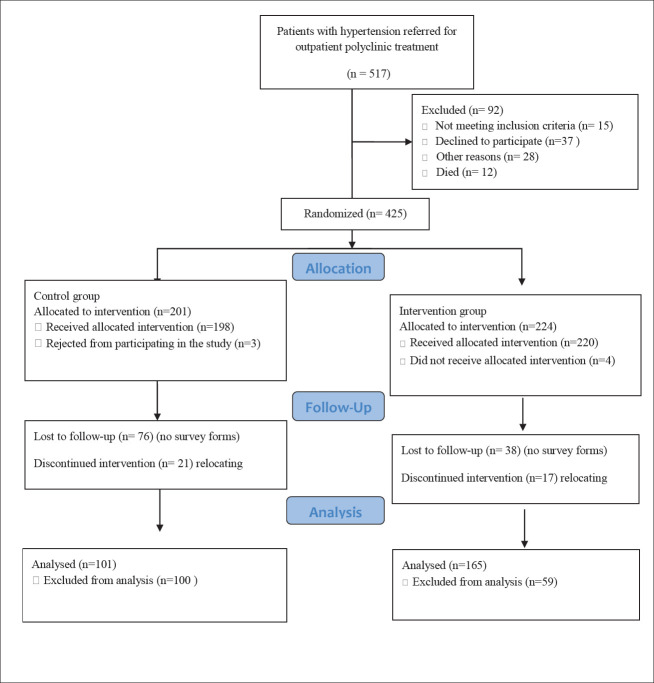
The flow-chart (Figure 1) of the study participants showed the number of patients with arterial hypertension who underwent outpatient treatment in the polyclinics of Almaty in the period 2019-2020 (n=517).
Figure 1. Block diagram of study participants.
Among all invited patients (n=517), n = 92 (17.8 %) patients were not included in the study. Some patients did not meet the inclusion / exclusion criteria (n=15 or 16.3 %), while n = 37 (40.2 %) refused to participate, and n=28 (30.4 %) rejected for other reasons. 12 patients died during the recruitment process (2.3 %). The cause of death in patients with hypertension was myocardial infarction (n=4 or 33.3 %), haemorrhagic stroke (n=3 or 25.0 %) and death from other concomitant diseases (n = 5 or 41.7 %).
Thus, 82.2 % (n=425) of patients were included in the study, The patients were randomly divided into two groups. Patients in the control group (CG) accounted for 47.3 % (n = 201), and in intervention group (IG) 52.7 % (n = 224). Demographic data, gender, body-mass index (BMI), bad habits (smoking), duration of hypertension, concomitant pathology (dyslipidemia, diabetes mellitus), history of cardio-vascular disorders incidence, atrial fibrillation and daily blood pressure measurements were analysed in both groups. During the study (2019-2020 period), three CG patients (1.4 %) refused to participate in the study. At the same time, 76 patients (37.8 %) did not fill out the adherence assessment questionnaires, while 21 patients (10.4 %) were unable to continue the study due to the move to another place of residence. In the intervention group (IG) n = 4 (1.7 %) refused to participate in the study, n = 38 (16.9 %) did not complete the adherence assessment questionnaires, n = 17 (7.5 %) were unable to continue the study in connection with moving to another place of residence. Based on the data obtained, the adherence score was determined for 101 (50.2 %) patients in the control group (CG) and 165 (73.6 %) patients in the interventional group (IG).
3.4. Adherence assessment
The assessment of adherence to antihypertensive treatment was carried out using an indirect method: the Lebanese Medication Adherence Scale-14 (LMAS-14) (34) (Table 1). The purpose of this validated questionnaire is to determine the frequency of non-adherence to prescribed drugs adherence to treatment in chronic diseases. LMAS contained 14 Likert scale questions with four options to answer each (coded from zero (less adherence) to three (higher adherence)) (34). Patient’s score may range from 0 (lowest adherence) to 42 (highest adherence) (35). Patients who scored 38-42 points were considered highly adherent, while the patients scored 35-37 points as moderately adherent, and less than 35 points as poorly adhered. Questions from the LMAS-14 questionnaire are presented in Table 1. Data were collected using SurveyMonkey © user-filled electronic questionnaires at standard time points or by using the telephone. Data were collected before therapy (T1), 3 months (T2), 6 months (T3), and 12 months (T4) after the first dose. In cases of not filling in the data, patients were called by phone. Patients who did not complete at least a one-time interval (T) were excluded from the adherence study according to Figure 1.
Table 1. Lebanese Medication Adherence Scale-14 (LMAS-14).
| № | Question | Points |
|---|---|---|
| 1 | Do you forget to take your medication when you are busy (intensive work or travel)? | 0-3 |
| 2 | Do you forget to take your medication if you are invited to lunch or dinner? | 0-3 |
| 3 | Do you forget to take your medication? | 0-3 |
| 4 | Do you get late when it comes to buying your medication packs when they become empty? | 0-3 |
| 5 | Do you stop taking your medication if it forbids you from eating certain food that you love because of possible food-medication interaction? | 0-3 |
| 6 | Will you stop taking your medication, without your doctor’s consultation, if your neighbor/relative took a prescription like yours for a long term and it caused them side effects? | 0-3 |
| 7 | Do you stop taking your medication without consulting your doctor if the laboratory tests show improvement during treatment period? | 0-3 |
| 8 | Do you stop taking your medication without consulting your doctor if you do not feel better during treatment period? | 0-3 |
| 9 | Do you stop taking your medication without consulting your doctor if you feel better during treatment period? | 0-3 |
| 10 | Do you decide to stop some of your medications without consulting your doctor if you noticed that you are taking too many medications every day? | 0-3 |
| 11 | Do you stop your chronic treatment if you get bored of it? | 0-3 |
| 12 | Do you stop taking your medication in case of side effects? | 0-3 |
| 13 | Do you stop taking your medication if your insurance does not cover it? | 0-3 |
| 14 | Will you stop buying your medication packs if you considered them expensive? | 0-3 |
Members of the CG and IG groups were individually familiarized with the rules for filling out the questionnaires during their visit to the attending physician.
3.5. Intervention
Study participants from the control group (CG) a received routine care according to the treatment protocols of the Ministry of Healthcare of Kazakhstan (33).
Intervention group (IG) members were given an access to the mobile phone app programme ‘MyTherapy’ version 3.71.1 (Munich, Germany). The mobile application was installed on the patient’s mobile device and made it possible to control the time of taking medications by notifying the patient in a convenient way (light signal, sound signal, or vibration) (36). The application allows the creation of an individual schedule of medication intake for each patient. It is freely available and it has no difficulties in use (https://www.mytherapyapp.com/ru/download). In addition, to work with the application, all IG members were given a short training on how to use the application and text instructions, including a short training video.
After 18 months, to examine the relationship between adherence according LMAS-14 questionnaire and blood pressure control, n-101 participants in the control group and n-165 participants in the intervention group were interviewed by phone to determine their «Day time BP». Among the patients who answered the call to determine the Day time BP, the study participants were instructed in the technique of measuring blood pressure (33). Only n-48 participants in the control group and n-37 participants in the intervention group had a blood pressure monitor to measure blood pressure, and the measured blood pressure of these patients was included in the analysis (Figure 1).
Statistical analysis
The results were statistically analysed using IBM SPSS Statistics Base 22.0 for Windows. Arithmetic mean (M) and standard deviation (SD) were calculated for quantitative variables. Data were presented as M ± SD. Qualitative attributes were described as absolute (n) and relative (%) values. Coefficients of variability were calculated. The Kolmogorov-Smirnov method was used to check the normality. The Student’s T test was used to compare the mean values. Treatment adherence, frequency, mean, median and standard deviations were calculated by the sum of the treatment adherence scale scores. Differences between the examined indices were considered statistically significant at p ≤ 0.05.
4. RESULTS
The general characteristics of the study participants are presented in Table 2. The average age of all 425 participants included in the study in both CG and IG groups was on average 62.4 ± 3.9 years.
Table 2. General characteristics of patients in the study groups.
| General characteristics | ||||
| Indicators | CG (n=201) | IG (n=224) | Total (n=425) | p- value |
| Age (avr.+ SD) | 62.8±4.1 | 63.9±2.9 | 62.4±3.9 | |
| Female (n,%) | 124 (61.7) | 67 (29.9) | 191 (44.9) | ≤0.001 |
| Male (n,%) | 77 (38.3) | 157 (70.1) | 234 (55.1) | ≤0.001 |
| Period of illness (AH) (n,%) | ||||
| ≥ 1 year | 3 (1.5) | 7 (3.1) | 10 (2.4) | |
| ≥ 3 years | 12 (6.0) | 6 (2.7) | 18 (4.2) | ≤0.05 |
| ≥ 5 years | 42 (20.9) | 32 (14.3) | 74 (17.4) | |
| ≥ 10 years | 144 (71.6) | 179 (79.9) | 323 (76.0) | |
| Dyslipidemia (n,%) | 120 (59.7) | 145 (64.7) | 265 (62.4) | |
| Body mass index (n,%) | ||||
| <25 | 17 (8.5) | 71 (31.7) | 88 (20.7) | ≤ 0.001 |
| 25-29,9 | 98 (48.7) | 112 (50.0) | 210 (49.4) | ≤0.05 |
| > 30 | 86 (42.8) | 41 (18.3) | 127 (29.8) | ≤0.001 |
| Diabetes (n,%) | 51 (25.4) | 28 (12.5) | 79(18.6) | ≤0.05 |
| Smoking (n,%) | ||||
| no | 176 (87.5) | 184 (82.1) | 360 (84.7) | |
| previous | 14 (7.0) | 16 (7.1) | 30 (7.1) | |
| current | 11 (5.5) | 24 (10.7) | 35 (8.2) | ≤ 0.05 |
| History of CVD (n,%) | 34 (16.9) | 26 (11.6) | 60 (14.1) | |
| History of AF (n,%) | 42 (20.9) | 29 (12.9) | 71 (16.7) | ≤0.05 |
| 24 hour BP (mm Hg; Wed + SD) | 168.4±21.2 / 92.1±14.3 | 163.3±17.8 / 90.4±15.5 | 165.1±24.1 / 90.8±11.7 | |
| Daytime blood pressure (mm Hg / Wed + SD) | 174.3±19.7 / 98.3±11.5 | 170.1±17.4 / 95.3±10.9 | 172.4±18.4 / 97.1±12.4 | |
| AH–arterial hypertension; history of CVD–cardiovascular disease (acute coronary syndrome, stroke); AF–atrial fibrillation | ||||
By gender, women prevailed in the CG group with indicators n = 124 (61.7 %) in comparison with the IG group (29.9 %). At the same time, the number of men was higher in the IG group (n = 157 or 70.1 %) with a statistically significant difference (p ≤ 0.001).
According to the duration of the manifestation of hypertension in both groups CG and IG, most patients (n = 265) had arterial hypertension for more than 10 years, 71.6 % and 79.9 %, respectively (without a statistically significant difference). Statistically significant differences were recorded in patients with a duration of chronic arterial morbidity more than ≥ 3 years, where there were twice as many patients in the CG group n = 12 (6.0 %) as in the IG group n = 6 (2.7 %) (p ≤ 0.05).
There were more patients with dyslipidemia in the IG group (n = 145) compared with the CG group (n = 120), with no statistically significant difference. In terms of BMI, patients with normal body weight (BMI < 25) prevailed in the IG group (n = 71 or 31.7 %), while obese participants (BMI > 30) were more common in the CG group (n = 86, 42.8 %), respectively (p ≤ 0.001). In addition, the overweight patients (BMI 25-29.9), who were most common among all participants, dominated the IG group (50 %) with little difference from the CG group (48.7 %) (p ≤ 0.05). Among concomitant diseases, diabetes mellitus was registered more often in the CG group n = 51 (25.4 %), in contrast to the IG n = 28 (12.5 %), in which the differences were considered statistically significant (p ≤ 0.05). In terms of smoking status, the overwhelming majority of the groups were non-smokers n = 360 (84.7 %). However, in the IG group, the number of active smokers was almost twice as high n = 24 (10.7 %) compared to the CG group n = 11 (5.5 %) (p ≤ 0.05).
The incidence of CVD (16.9 %) and the history of atrial fibrillation (20.9 %) were more recorded in the CG group respondents, in contrast to the IG patients, among whom the prevalence of AF was statistically significantly higher in the CG group (p ≤ 0.05).
The indicators of 24-hour BP monitoring in both groups averaged 165.1 ± 24.1 / 90.8 ± 11.7, and daytime BP was 172.4 ± 18.4 / 97.1 ± 12.4. According to the results of the assessment of adherence to therapy according to the LMAS-14 the results of the responses of respondents who completed the survey of all 4 periods (T1; T2; T3 and T4) of the study were included. Thus, the responses of 113 patients in the CG group and 165 respondents in the IG group were taken into account (Figure 2).
Figure 2. Assessment of adherence of patients in the control study (CG) and in an interventional study (IG) in periods T1; T2; T3; and T4.
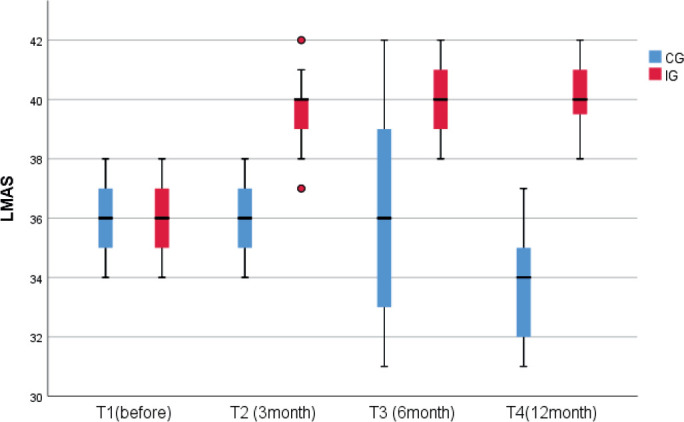
In the period T1 in both groups CG and IG, the moderate adherence to treatment was recorded with indices equal to 35.9 ± 1.2 and 35.9 ± 1.3, respectively (p ≤ 0.05). However, after 3 months (T2), patient adherence in both groups began to decline, although it remained relatively high in the IG (39.5 ± 1.2) in contrast to the CG group (35.9 ± 1.2) (p ≤ 0.05). This tendency of moderate adherence in the studied group CG persisted after six months later (36.5 ± 3.2) in comparison with higher adherence among the respondents in the IG group (40.0 ± 1.2) (p ≤ 0.001). After 12 months (T4) on the adherence scale in patients who used the mobile application “MyTherapy” (IG), despite a slight decrease in scores, in contrast to the initial stage, the results were relatively higher (40.3 ± 1.3) compared with the CG group (33.6 ± 1.9) (p ≤ 0.001).
5. DISCUSSION
To the best of our knowledge, this is the first study in Kazakhstan on the assessment of the adherence of patients to treatment with arterial hypertension using a mobile application. Good adherence to antihypertensive drugs is associated with a significantly higher likelihood of achieving blood pressure control and, therefore, with lower costs and less use of health care resources (37).
A difficult epidemiological situation with COVID-19 and the social distancing regime transformed healthcare systems worldwide. Moreover, pandemics have triggered the widespread use of digital technologies among people who require constant monitoring of their health status (38). Telemedicine provides some advantages associated with virtual communication, low costs for the patient, saving time and decreasing of risk of infections (24).
According to the results of previous studies, the function of telephone SMS reminder is one of the most effective ways to maintain the correct adherence of patients, resulting in a decrease in the rates of poor adherence by 43 % (39). It can be explained by the fact that the forgetfulness of patients is one of the main reasons for non-adherence to drug prescriptions (40).
In our study, the ‘MyTherapy’ mobile applications allowed the patients to conduct monitoring of blood pressure, fulfill the doctor’s prescriptions on time, and receive a one-click consultation on the issues. It created the possibility for effective communication between the patient and physician. According to our data, a decrease in adherence was recorded in both groups (with and without the use of a mobile application). However, patients using the ‘MyTherapy’ app, after 12 months, demonstrated relatively a high adherence to therapy that indicates the prevention of the development of cardiovascular complications. In fact, one of the important issues affecting the decrease in patient adherence is a socio-economic factor (41). In this regard, the availability and low cost of any digital health technologies play a crucial role. The tested mobile application provides functionality, accessibility and ease of use. In addition, it has shown the effectiveness of monitoring drug compliance.
In a randomized controlled trial conducted by Bloss et al., it was shown the effectiveness of a mobile application for monitoring chronic diseases (42). It was demonstrated that the usage of such an application led to the improvement of the self-control health indicators without increasing costs. Previous studies have also described the use of text messages via mobile communication, but this method of communication was associated with high expenses hampering widespread implementation (43). According to published data, 107 mobile applications for monitoring hypertension were available in the United States, of which 65.4 % were free of charge. However, only 1.7 % apps have functionality that ensures the attending physician’s control of adherence to patient treatment (14).
The results of the range of studies showed that duration of illness could also be a factor in reducing adherence to regular medication use. For example, unlike patients who have recently been diagnosed with arterial hypertension, patients with arterial hypertension for several years have low adherence (44). According to the results of our study, after one year of monitoring the conditions of patients with arterial hypertension, patients scored twice as high on the adherence scale. Moreover, the level of adherence was high in comparison with patients who did not use the ‘MyTherapy’ mobile application. Given the importance of patient’s engagement in the treatment process (45), the use of mobile apps also allows to monitor medication adherence in the long term period. The results obtained are consistent with previously published data, where the free “Alerhta” mobile application was used to increase the adherence of patients with hypertension. The adherence increased by 23.64 % after 12 months of usage compared with the control (46). It must be noted that specialized scales were not used in this study. The evaluation of adherence was performed by additional devices.
To summarize, despite the obvious benefits of mobile apps in healthcare and cardiology, there is a range of challenges and concerns regarding effectiveness, safety, reliability and ethical issues. Another big problem is the lack of official regulations and guidelines from medical organizations. It encompasses data privacy, standardization and unification of various digital protocols.
In addition, nowadays there is a lack of information regarding cost-effectiveness of mobile apps or other mobile health technologies (47). So that further research towards a wide implementation of mobile apps in cardiac practice, particularly among patients with hypertension is needed.
This study has some limitations. The sample size of participants was not large. However, the testing period of the effectiveness of mobile applications covers 12 months. So it can be considered as a strength of this study.
6. CONCLUSION
The analysis of adherence of patients with chronic arterial hypertension showed the effectiveness of using the ‘MyTherapy’ mobile application resulted in an increase in patient adherence. Our findings indicate the positive impact of the use of such digital technology for health monitoring. However, further research to assess the possibility of wider implementation in other areas of medical care is needed.
Acknowledgments:
The authors are thankful to Dr. Naylya Kozhekenova (from City Hospital “Alatau”, Almaty) for the help with preparing this manuscript.
Patient Consent Form:
All participants were informed about subject of the study.
Author’s Contribution:
S.N., K.K., L.K., A.T. and A.A. gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. G.K, L.A., M.A, I.F. and S.T. had a part in article preparing for drafting or revising it critically for important intellectual content. All authors gave final approval of the version to be published and agreed to be accountable
Conflicts of Interest:
There are no conflicts of interest.
Financial support and sponsorship:
The study was supported by the grant of the Ministry of Healthcare of the Republic of Kazakhstan “National Programme for the Introduction of Personalized and Preventive Medicine in The Republic of Kazakhstan (2021–2023)” (Grant number OR12165486)..
REFERENCES
- [1].WHO. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases N-cdAa .
- [2].Chapel JM, Ritchey MD, Zhang D, Wang G. Prevalence and Medical Costs of Chronic Diseases Among Adult Medicaid Beneficiaries. Am J Prev Med. 2017;53(6s2):S143–s54. doi: 10.1016/j.amepre.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ramli A, Ahmad NS, Paraidathathu T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer Adherence. 2012;6:613–622. doi: 10.2147/PPA.S34704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Campbell C, McGauley G. Doctor-patient relationships in chronic illness: insights from forensic psychiatry. BMJ (Clinical research ed) 2005;330(7492):667–670. doi: 10.1136/bmj.330.7492.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. doi: 10.1111/j.1365-2125.2012.04167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chaudri NA. Adherence to Long-term Therapies Evidence for Action. Annals of Saudi Medicine. 2004;24(3):221–222. [Google Scholar]
- [7].Corrao G, Parodi A, Nicotra F, Zambon A, Merlino L, Cesana G, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29(3):610–618. doi: 10.1097/HJH.0b013e328342ca97. [DOI] [PubMed] [Google Scholar]
- [8].Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Uchmanowicz B, Chudiak A, Uchmanowicz I, Rosińczuk J, Froelicher ES. Factors influencing adherence to treatment in older adults with hypertension. Clin Interv Aging. 2018;13:2425–2441. doi: 10.2147/CIA.S182881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: A systematic review and meta-analysis. Medicine (Baltimore) 2017;96(4):e5641. doi: 10.1097/MD.0000000000005641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Badawy SM, Barrera L, Sinno MG, Kaviany S, O’Dwyer LC, Kuhns LM. Text Messaging and Mobile Phone Apps as Interventions to Improve Adherence in Adolescents With Chronic Health Conditions: A Systematic Review. JMIR Mhealth Uhealth. 2017;5(5):e66. doi: 10.2196/mhealth.7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Vollmer WM, Owen-Smith AA, Tom JO, Laws R, Ditmer DG, Smith DH, et al. Improving adherence to cardiovascular disease medications with information technology. Am J Manag Care. 2014;20(11 Spec No. 17):Sp502–510. [PMC free article] [PubMed] [Google Scholar]
- [13].Xu H, Long H. The Effect of Smartphone App-Based Interventions for Patients With Hypertension: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth. 2020;8(10):e21759. doi: 10.2196/21759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kumar N, Khunger M, Gupta A, Garg N. A content analysis of smartphone-based applications for hypertension management. J Am Soc Hypertens. 2015;9(2):130–136. doi: 10.1016/j.jash.2014.12.001. [DOI] [PubMed] [Google Scholar]
- [15].Gong K, Yan YL, Li Y, Du J, Wang J, Han Y, et al. Mobile health applications for the management of primary hypertension: A multicenter, randomized, controlled trial. Medicine (Baltimore) 2020;99(16):e19715. doi: 10.1097/MD.0000000000019715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gonzalez T, de la Rubia MA, Hincz KP, Comas-Lopez M, Subirats L, Fort S, et al. Influence of COVID-19 confinement on students’ performance in higher education. PloS one. 2020;15(10):e0239490–e. doi: 10.1371/journal.pone.0239490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Keesara S, Jonas A, Schulman K. Covid-19 and Health Care’s Digital Revolution. N Engl J Med. 2020;382(23):e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- [18].Senbekov M, Saliev T, Bukeyeva Z, Almabayeva A, Zhanaliyeva M, Aitenova N, et al. The Recent Progress and Applications of Digital Technologies in Healthcare: A Review. Int J Telemed Appl. 2020;2020:8830200. doi: 10.1155/2020/8830200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ryu S. Book Review: mHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth (Global Observatory for eHealth Series, Volume 3) Healthcare Informatics Research. 2012;18(3):231–233. [Google Scholar]
- [20].Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Elkbuli A, Ehrlich H, McKenney M. The effective use of telemedicine to save lives and maintain structure in a healthcare system: Current response to COVID-19. The American journal of emergency medicine. 2021;44:468–469. doi: 10.1016/j.ajem.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ohannessian R, Duong TA, Odone A. Global Telemedicine Implementation and Integration Within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020;6(2):e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Padwal R, Wood PW. Digital Health Approaches for the Assessment and Optimisation of Hypertension Care Provision. Can J Cardiol. 2021;37(5):711–721. doi: 10.1016/j.cjca.2020.12.009. [DOI] [PubMed] [Google Scholar]
- [24].Garg SK, Rodbard D, Hirsch IB, Forlenza GP. Managing New-Onset Type 1 Diabetes During the COVID-19 Pandemic: Challenges and Opportunities. Diabetes Technol Ther. 2020;22(6):431–439. doi: 10.1089/dia.2020.0161. [DOI] [PubMed] [Google Scholar]
- [25].Clipper B. The Influence of the COVID-19 Pandemic on Technology: Adoption in Health Care. Nurse leader. 2020;18(5):500–503. doi: 10.1016/j.mnl.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Fagherazzi G, Goetzinger C, Rashid MA, Aguayo GA, Huiart L. Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers. J Med Internet Res. 2020. p. e19284. 22: ©Guy Fagherazzi, Catherine Goetzinger, Mohammed Ally Rashid, Gloria A Aguayo, Laetitia Huiart. Originally published in the Journal of Medical Internet Research ( http://www.jmir.org), 16.06.2020.; [DOI] [PMC free article] [PubMed]
- [27].Ting DSW, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nature Medicine. 2020;26(4):459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tian M AV, Dunzhu D, Hameed SS, Li X, Liu Z, et al. A cluster-randomized, controlled trial of a simplified multifaceted management program for individuals at high cardiovascular risk (SimCard Trial) in Rural Tibet, China, and Haryana, India. Circulation. 2015 Sep 1; doi: 10.1161/CIRCULATIONAHA.115.015373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Milani RV, Wilt JK, Milani AR, Bober RM, Malamud E, Entwisle J, et al. Digital Management of Hypertension Improves Systolic Blood Pressure Variability. Am J Med. 2020;133(7):e355–e9. doi: 10.1016/j.amjmed.2019.10.043. [DOI] [PubMed] [Google Scholar]
- [30].Pellegrini D, Torlasco C, Ochoa JE, Parati G. Contribution of telemedicine and information technology to hypertension control. Hypertens Res. 2020;43(7):621–628. doi: 10.1038/s41440-020-0422-4. [DOI] [PubMed] [Google Scholar]
- [31].Chan BT, Rauscher C, Issina AM, Kozhageldiyeva LH, Kuzembaeva DD, Davis CL, et al. A programme to improve quality of care for patients with chronic diseases, Kazakhstan. Bull World Health Organ. 2020;98(3):161–169. doi: 10.2471/BLT.18.227447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Supiyev A, Kossumov A, Utepova L, Nurgozhin T, Zhumadilov Z, Bobak M. Prevalence, awareness, treatment and control of arterial hypertension in Astana, Kazakhstan. A cross-sectional study. Public Health. 2015;129(7):948–953. doi: 10.1016/j.puhe.2015.02.020. [DOI] [PubMed] [Google Scholar]
- [33].Republican, Clinical Cfhd, of pfdatotMoHotR. Oct 3, “Arterial K, dated hN hwrkipe.
- [34].Bou Serhal R, Salameh P, Wakim N, Issa C, Kassem B, Abou Jaoude L, et al. A New Lebanese Medication Adherence Scale: Validation in Lebanese Hypertensive Adults. Int J Hypertens. 2018;2018:3934296. doi: 10.1155/2018/3934296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].El-Hajj M, Ajrouche R, Zein S, Rachidi S, Awada S, Al-Hajje A. Evaluation of risk factors and drug adherence in the occurrence of stroke in patients with atrial fibrillation. Pharmacy practice. 2020;18(2):1860. doi: 10.18549/PharmPract.2020.2.1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Carmody JK, Denson LA, Hommel KA. Content and Usability Evaluation of Medication Adherence Mobile Applications for Use in Pediatrics. J Pediatr Psychol. 2019;44(3):333–342. doi: 10.1093/jpepsy/jsy086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Elliott WJ. What factors contribute to the inadequate control of elevated blood pressure? J Clin Hypertens (Greenwich) 2008;10(1 Suppl 1):20–26. doi: 10.1111/j.1524-6175.2007.08028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Badawy SM, Radovic A. Digital Approaches to Remote Pediatric Health Care Delivery During the COVID-19 Pandemic: Existing Evidence and a Call for Further Research. JMIR pediatrics and parenting. 2020;3(1):e20049–e. doi: 10.2196/20049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Jeppesen MH, Ainsworth MA. Telephone reminders reduced the non-attendance rate in a gastroenterology outpatient clinic. Dan Med J. 2015;62(6) [PubMed] [Google Scholar]
- [40].Carlsen KH, Carlsen KM, Serup J. Non-attendance rate in a Danish University Clinic of Dermatology. Journal of the European Academy of Dermatology and Venereology. 2011;25(11):1269–1274. doi: 10.1111/j.1468-3083.2010.03962.x. [DOI] [PubMed] [Google Scholar]
- [41].George M. Adherence in Asthma and COPD: New Strategies for an Old Problem. Respir Care. 2018;63(6):818–831. doi: 10.4187/respcare.05905. [DOI] [PubMed] [Google Scholar]
- [42].Bloss CS, Wineinger NE, Peters M, Boeldt DL, Ariniello L, Kim JY, et al. A prospective randomized trial examining health care utilization in individuals using multiple smartphone-enabled biosensors. PeerJ. 2016;4:e1554. doi: 10.7717/peerj.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Conway CM, Kelechi TJ. Digital Health for Medication Adherence in Adult Diabetes or Hypertension: An Integrative Review. JMIR Diabetes. 2017;2(2):e20. doi: 10.2196/diabetes.8030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA. 2002;288(22):2880–2883. doi: 10.1001/jama.288.22.2880. [DOI] [PubMed] [Google Scholar]
- [45].Perski O, Blandford A, West R, Michie S. Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl Behav Med. 2017;7(2):254–267. doi: 10.1007/s13142-016-0453-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Márquez Contreras E, Márquez Rivero S, Rodríguez García E, López-García-Ramos L, Carlos Pastoriza Vilas J, Baldonedo Suárez A, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167–173. doi: 10.1080/03007995.2018.1549026. [DOI] [PubMed] [Google Scholar]
- [47].Badawy S, Kuhns L. Economic Evaluation of Text-Messaging and Smartphone-Based Interventions to Improve Medication Adherence in Adolescents with Chronic Health Conditions: A Systematic Review. JMIR mHealth and uHealth. 2016;4:e121. doi: 10.2196/mhealth.6425. [DOI] [PMC free article] [PubMed] [Google Scholar]