Abstract
Objective:
Our objective was to estimate the incidence of uterine leiomyosarcoma in patients with leiomyomas following laparoscopic supracervical hysterectomy and myomectomy procedures.
Study design:
For this study, we analyzed records of 13,964 women aged 25 to 64 years who underwent laparoscopic supracervical hysterectomies or myomectomies for leiomyomas from 2002–2011 using Clinformatics DataMart. Patient records were divided into 2 groups: history of laparoscopic supracervical hysterectomy and history of myomectomy. Subjects were tracked to identify diagnosis of leiomyosarcoma within one year of the procedure. We analyzed data from the 25–39, 40–49, and 50–64 age brackets. Evidence was obtained from a cohort study from national private insurance claims in the US.
Results:
Our results showed the incidence of occult leiomyosarcoma developing within 1 year following supracervical hysterectomy using a laparoscopic-assisted approach are 9.8, 10.7, and 33.4 per 10,000 for the 25–39, 40–49, and 50–64 age brackets, respectively; the overall incidence rate is 13.1 per 10,000. The incidence rate of occult leiomyosarcoma developing within 1 year following myomectomy using a laparoscopic-assisted approach are 0.0, 33.8, and 90.1 per 10,000 for the 25–39, 40–49, and 50–64 age brackets, respectively; the overall incidence rate is 17.3 per 10,000.
Conclusion:
Our analysis shows the overall risk of being diagnosed with occult leiomyosarcoma is 12.9 per 10,000 in laparoscopic-assisted supracervical hysterectomy and myomectomy for patients younger than 49.There is no evidence of occult leiomyosarcoma 1 year after operation for patients younger than 40 who underwent laparoscopic myomectomy.
Keywords: leiomyoma, leiomyosarcoma, incidence, laparoscopy
CONDENSATION
The purpose of this study is to obtain contributory data to estimate the incidence of ULMS in the US patient population to improve the current informed consent process.
INTRODUCTION
Uterine leiomyosarcoma (ULMS) is the most common type of uterine sarcoma, accounting for approximately 42%–60% of all uterine sarcomas.1 This condition comprises about 1.5% of all uterine malignancies.2 The women undergoing minimally invasive hysterectomies and myomectomies are at risk of being diagnosed with occult ULMS, with an incidence ranging from 0.09% to 0.39% (from 1 in 256 to 1 in 1100).3–5
Unfortunately, preoperative diagnostic modalities used to diagnose ULMS are not as reliable as those used to diagnose epithelial endometrial malignancies.6 Preoperative endometrial sampling has 64% sensitivity for the diagnosis of ULMS.7 Patients with ULMS have symptoms vaguely similar to patients with leiomyomas, with most ULMS cases diagnosed postoperatively.8 Other studies show that magnetic resonance imaging and serum measurement of lactate dehydrogenase have also demonstrated limitations in making a differentiated diagnosis of ULMS from benign uterine leiomyoma.9
In this study, we collected records of those who received laparoscopic supracervical hysterectomies (LSH) or laparoscopic myomectomies (LM), thereby providing contributory data to estimate the incidence of occult ULMS since morcellation technique was presumably used to remove the specimen in those cases and no special CPT coding exists for morcellation in any US database. In order to obtain informed consent on occult ULMS, we also identified the incidence rates of different age brackets to obtain more detailed information during the written consent process.
MATERIALS AND METHODS
Data Source
This retrospective cohort study was performed using 2002–2011 health insurance claims data from Clinformatics DataMart, which is a database consisting of geographically diverse, privately insured individuals in the United States.10 The database contains deidentified information on more than 45 million individuals, approximately 80% of whom purchased health insurance through their employers and each had at least 1 medical claim reported. The database does not contain information on patients’ socioeconomic status, race/ ethnicity, or morcellation status, but it contains geographic location and type of procedure.11
It has been estimated that the database contains a higher percentage of white, young, middle-aged adults than is present in the overall US population. Since the data is deidentified, Institutional Review Board approval was not required for this study.
Study Population
Figure 1 provides the flowchart of the cohort extract. Our study population consisted of women aged 25 to 64 years who were diagnosed with leiomyomas and underwent LSHs or LMs between 2002 and 2011. The individuals were divided into 2 groups: patients with a history of LSH and patients with a history of LM. The vast majority of these 2 groups most likely underwent surgical procedures with help of morcellation to remove the surgical specimens.
Figure 1.
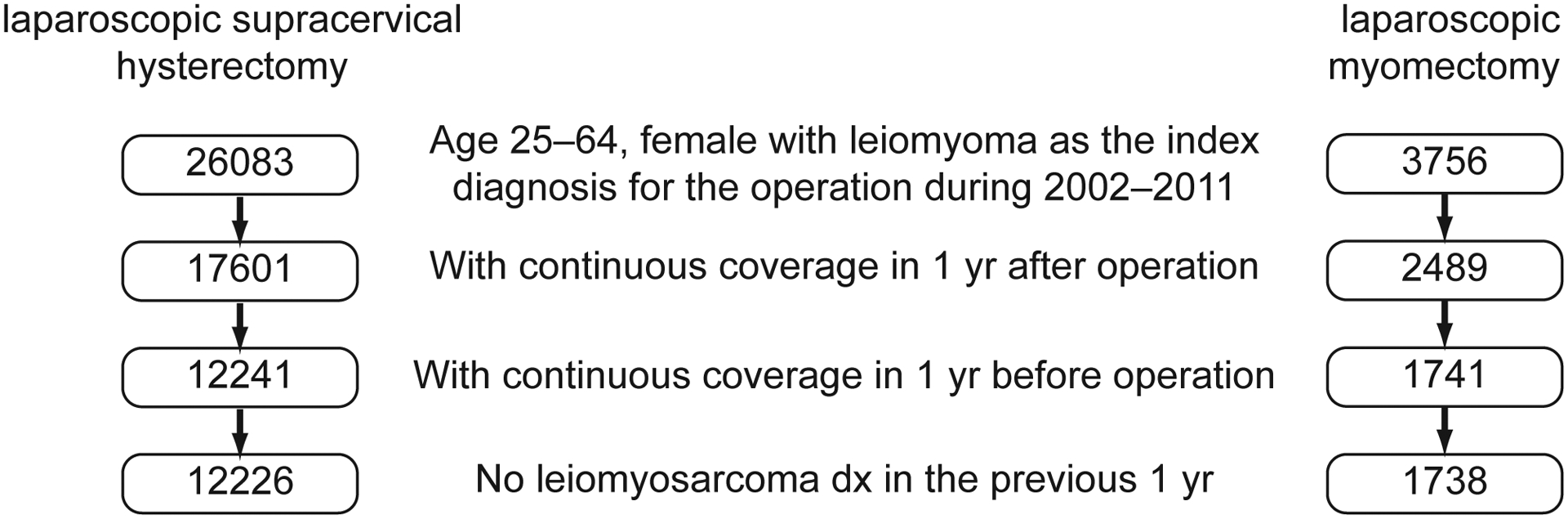
Flowchart of cohort extraction (2002–2011)
Diagnoses and procedures were identified based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), and Current Procedural Terminology (CPT) codes from patients’ medical claims. The ICD-9-CM codes that identify leiomyoma are 218, 218.0, 218.1, 218.2, 218.9, 219, 219.1, 219.8, and 219.9. Table 1 shows the ICD-9-CM and CPT codes for the 2 study groups.
Table 1.
Procedure codes
| ICD-9-CM Codes | CPT Codes | |
|---|---|---|
| laparoscopic supracervical hysterectomy | < 250 g uterus (68.31) | < 250 g uterus (58541, 58542) |
| > 250 g uterus (68.31) | > 250 g uterus (58543) | |
| > 250 g uterus with removal of tubes and/or ovaries (68.31) | > 250 g uterus with removal of tubes and/or ovaries (58544) | |
| laparoscopic myomectomy | < 250 g uterus (68.29) | < 250 g uterus (58545) |
| > 250 g uterus (68.29) | > 250 g uterus (58546) |
The robotic system was approved by the FDA for gynecologic surgeries in 2005. ICD codes indicating LSH and LM may have been used for robotic-assisted LSH and LM before 2008 because ICD codes did not exist for robotic procedures until 2008. In our study, we were unable to differentiate between laparoscopic- and robotic-assisted cases between 2005 and 2008, thus some overlap exists. However, cases operated with robotic systems after 2008 were not included to keep our data as homogenous as possible.
Initially, 26,083 LSHs and 3,756 LMs were extracted for the study. Subjects were excluded if they did not have continuous insurance coverage 1 year after the operation for LSH and LM (leaving 17,601 and 2,489), did not have continuous insurance coverage 1 year before the operation (leaving 12,241 and 1741), or had no diagnosis of ULMS in the previous year (leaving 12,226 and 1,738). After exclusions, a total of 12,226 LSHs and 1,738 LMs were included in the final cohort (total 13,964). Incorporating the one-year postoperative follow-up data maximized the accuracy of our results since a significant number of patients change their insurance companies over the long term.
Measures
Since the exact date of birth was not available, year of birth served as a proxy. Age is determined by subtracting year of birth from year of surgical procedure. Age was categorized into 3 groups: 25–39, 40–49, and 50–64. The geographic regions were categorized into 4 groups: Northeast, Midwest, South, and West. Year of surgical procedure was treated as a categorical variable (2002 to 2011). For each woman in the study, medical claims were tracked for 1 year after the operation. We identified those with a diagnosis of leiomyosarcoma (ICD-9-CM codes: 179, 171.9) and the date of their first clinical visit for ULMS treatment.
Statistical Analysis
Descriptive statistics were used to describe the distribution of study population by age, geographic region, and year of operation. The bivariate associations were assessed using chi-square tests. Unadjusted incidence was calculated for risk of ULMS for all subjects and for each study group. Multivariate logistic regression modeling was used to test the age effect on the risk of ULMS. Because of rare outcome events, the penalized likelihood method was used to estimate the logistic regression model. A 2-sided P value < 0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
A total of 13,964 women aged 26 to 64 years were included in the study. Mean standard deviation of age distribution of subjects was 40.9 ± 7.0 for all, 41.3 ± 7.0 for those with LSH, and 38.5 ± 6.6 for those with LM.
Table 2 shows the differences in patient characteristics between the 2 groups. There was an upward trend in the number of women who received LSH since 2006. On the other hand, LM cases showed consistent increments during the last 10 years, with 20.48% cases in 2011. The lack of extraction of LM cases in 2002 was due to fact that ICD codes were not introduced until 2003. This trend parallels the nationwide increase of minimally invasive gynecologic procedures in the last decade.12
Table 2.
Sample Characteristics
| All | laparoscopic supracervical hysterectomy | laparoscopic myomectomy | ||||
|---|---|---|---|---|---|---|
| N | Column % | N | Column % | N | Column % | |
| All | 13964 | 100.0 | 12226 | 100.0 | 1738 | 100.0 |
| Age * $ | ||||||
| 25–39 | 6150 | 44.04 | 5114 | 41.83 | 1036 | 59.61 |
| 40–49 | 6207 | 44.45 | 5616 | 45.93 | 591 | 34.00 |
| 50–64 | 1607 | 11.51 | 1496 | 12.24 | 111 | 6.39 |
| Region $ | ||||||
| Northeast | 1782 | 12.76 | 1612 | 13.19 | 170 | 9.78 |
| Midwest | 2598 | 18.60 | 2260 | 18.49 | 338 | 19.45 |
| South | 7617 | 54.55 | 6657 | 54.45 | 960 | 55.24 |
| West | 1954 | 13.99 | 1684 | 13.77 | 270 | 15.54 |
| Year $ | ||||||
| 2002 | 1027 | 7.35 | 1027 | 8.40 | 0 | 0.0 |
| 2003 | 1148 | 8.22 | 1079 | 8.83 | 69 | 3.97 |
| 2004 | 1251 | 8.96 | 1133 | 9.27 | 118 | 6.79 |
| 2005 | 1058 | 7.58 | 930 | 7.61 | 128 | 7.36 |
| 2006 | 1082 | 7.75 | 920 | 7.52 | 162 | 9.32 |
| 2007 | 1460 | 10.46 | 1282 | 10.49 | 178 | 10.24 |
| 2008 | 1658 | 11.87 | 1454 | 11.89 | 204 | 11.74 |
| 2009 | 1776 | 12.72 | 1548 | 12.66 | 228 | 13.12 |
| 2010 | 1770 | 12.68 | 1475 | 12.06 | 295 | 16.97 |
| 2011 | 1734 | 12.42 | 1378 | 11.27 | 356 | 20.48 |
Age distribution (mean ± standard deviation) of the subjects were 40.9 ± 7.0 for all, 41.3 ± 7.0 for those with laparoscopic supracervical hysterectomy, and 38.5 ± 6.6 those with for laparoscopic myomectomy
The 2 groups were significantly different in age, geographic region, and procedure year (P <.001). Because the analyses were overpowered due to large sample size, we emphasize the actual estimates instead of statistical significance.
Table 3 provides the incidence ratios for leiomyosarcoma by age group. The unadjusted overall incidence of ULMS was 14 per 10,000 (19 patients). The incidence rates for occult ULMS following LSH were 9.8, 10.7, and 33.4 per 10,000 for the 25–39, 40–49, and 50–64 age brackets, respectively. The incidence rates for occult ULMS following LM were 0.0, 33.8, and 90.1 per 10,000 for the 25–39, 40–49, and 50–64 age brackets, respectively. In the multivariate logistic regression, age was the only statistically significant factor. Ages 50–64 were associated with a significant increased risk of ULMS (OR = 1.5, 95% CI = 1.3–14.2 for all subjects; OR = 3.0, 95% CI = 0.9–10.5 for LSH; and OR = 33.8, 95% CI = 1.7, 100 + for LM, P < 0.05).
Table 3.
Incidence of leiomyosarcoma in 1 year after the operation, by age
| Number of leiomyosarcoma in 1 year after the operation, per 10,000 | OR (95% CI)* | |||||
|---|---|---|---|---|---|---|
| All | laparoscopic supracervical hysterectomy | laparoscopic myomectomy | All$ | laparoscopic supracervical hysterectomy¥ | laparoscopic myomectomy¥ | |
| All | 13.6 | 13.1 | 17.3 | n/a | n/a | n/a |
| Age | ||||||
| 25–39 | 8.1 | 9.8 | 0.0 | reference | reference | reference |
| 40–49 | 12.9 | 10.7 | 33.8 | 1.5 (0.5, 4.7) | 1.0 (0.3, 3.3) | 8.4 (0.7, > 100) |
| 50–64 | 37.4 | 33.4 | 90.1 | 4.2 (1.3, 14.2) | 3.0 (0.9, 10.5) | 33.8 (1.7, > 100) |
Because of rare outcome events, the penalized likelihood method was used for the estimation of the logistic regression model.
Adjusted for operation group, geographic region, and year of operation.
Adjusted for geographic region and year of operation
Table 4 shows the median time for diagnosis of ULMS after the operation appears on insurance database for the first time. This time period is calculated based on the difference from the day of surgery to the first clinical visit registered as ULMS diagnosis. About 47% of the group was diagnosed 1 month after the procedure. In the whole group, the median time for a registered ULMS diagnosis was 28 days (Interquartile range: 16–115 days).
Table 4.
Time of leiomyosarcoma registered diagnosis after operation
| Median (Interquartile Range), days | % diagnosed after 1 month | |||||
|---|---|---|---|---|---|---|
| All | laparoscopic supracervical hysterectomy | laparoscopic myomectomy | All | laparoscopic supracervical hysterectomy | laparoscopic myomectomy | |
| All | 28 (16–115) | 26 (14–103) | 26 (14–103) | 47.4% | 43.8% | 66.7% |
| Age | ||||||
| 25–39 | 24 (12–28) | 24 (12–28) | n/a | 20.0% | 20.0% | n/a |
| 40–49 | 70 (26–103) | 45 (16–91) | 146 (85–207) | 75.0% | 66.7% | 100.0% |
| 50–64 | 22 (22–126) | 22 (22–126) | 22 (22–22) | 33.3% | 40.0% | 0.0% |
n/a – not applicable due to no leiomyosarcoma case in this category
DISCUSSION
Despite 20 years of widespread acceptance and use of several morcellators in the US, there has been growing concern about the safety of power morcellators.13–15 The overall incidence of occult ULMS in presumed morcellation cases was 1.4 per 1000 in our study population. Wright et al recently published the rate of uterine malignancy as 2.7 per 1,000 in women undergoing hysterectomies using morcellation based on records of 36,470 patients registered in a prospective database.16 However, their study did not specify how many of the patients had uterine sarcomas, ULMS, or epithelial uterine cancer. They also calculated the prevalence ratio of a uterine malignancy based on age-brackets: 4.9 (95% CI, 1.9–12.9) in women 50–54 years, 19.3 (95% CI, 7.6–48.9) in women 55–59 years, 21.3 (95% CI, 7.2–63.2) in women 60–64 years, and 35.9 (95% CI, 14.1–91.5) in women 65 years or older, when women younger than 40 were accepted as the reference group. In the multivariate logistic regression, age was the only statistically significant factor affecting the odds of postoperative diagnosis of ULMS in our study. The prevalence ratio of occult ULMS in women over 50 years old was 3.0 (95% CI, 0.9–10.5) among patients who underwent LSH. However, LM cases showed an increase in the risk of being diagnosed with occult ULMS in those older than 40 years of age. In the LM group, while the prevalence ratio of occult ULMS was 0 in women younger than 40 years of age, this ratio was 8.4 in age group 40–49 (95% CI, 0.7– > 100) and 33.8 in age group 50–64 (95% CI, 1.7– > 100). A population-based study published by Mao et al emphasized that the sarcoma prevalence among patients with leiomyoma undergoing surgery were significantly associated with age. In their study, the prevalence was the lowest in women younger than 50 years of age, with 0.8–1.3 per 1000, whereas this rate was the highest in women older than 60 years of age, with 3.6–15.3 per 1000.17 A study recently examined 6,360 hysterectomies performed for benign indications.18 The incidence was 2.2 per 1,000 for patients younger than 55 years and 8.0 per 1,000 for patients 55 years or older, when uterine leiomyoma was accepted as the only indication in the calculation. In contrast to our study, their results included all types of uterine sarcomas, but, similar to our study, the age factor significantly influenced the risk of being diagnosed with uterine sarcoma after the surgery. Brohl et al reviewed the literature combining myomectomy and hysterectomy cases regardless of surgical techniques to estimate the risk of developing occult uterine sarcoma.19 The risk of ULMS was 1.78 cases per 1,000 in their study. They found a directly proportional relationship between age and the risk of having occult uterine sarcoma. The findings shown in previous studies were consistent with our study’s results.
The review by the FDA calculated that the prevalence of unsuspected uterine sarcoma and ULMS was 2.8 (95% CI: 1.8–4.5) per 1,000 (1 in 352) and 2.0 (95% CI: 1.1–3.8) per 1,000 (1 in 498), respectively, after hysterectomy or myomectomy performed for presumed benign leiomyoma.20 The FDA did not provide the risk assessment based on age brackets because no adequate data was likely presented by the studies to assess the risk of having uterine sarcoma or ULMS after surgery. We also provided the risk assessment for age groups. The overall incidence rate of occult ULMS was lower with 1.4 per 1000 in our study population compared to the rate calculated by FDA. This difference might have occurred because some studies included in the FDA review evaluated open hysterectomy or myomectomy cases as well.
In our study, the incidence rate of ULMS was higher in the myomectomy group than in the supracervical group. This difference may be due to the fact that the total number of patients included in this study was not equal between the 2 groups (12,226 LSHs and 1,738 LMs), and LSH was more commonly performed than LM in our database. In addition, since the incidence rate of ULMS was very low in the study group, it may partially reveal an exponential difference between the 2 groups.
Robot-assisted cases were not included in a separate group to maintain the homogeneity of the study data for the following reasons (considering our database included between 2002 and 2011): the FDA approved robotic-assisted hysterectomies in 2005, there were no special codes before 2008, and accuracy of robotic codes were questionable in the initial years of the CPT −9 and ICD-9 codes. At the same time, robotic surgery was a relatively new technology, which required an adaptation period for surgeons. During the learning curve, selection bias by surgeons might have been played a role in management of patients.
We recognize that the present study has some limitations. First, all of the subjects have insurance. Hence, the findings are only applicable to those with private insurance and not those with public insurance or without insurance. Second, claims-based data are constrained by coverage limitations that determine the data available and limit generalizability of results to managed-care patients. Patients can only be followed up when they have continual insurance coverage. Third, claims data are subject to coding errors. Presence of a diagnosis code for leiomyoma or ULMS on a medical claim is not positive proof of those diseases. Since the patient population was examined retrospectively, we could not definitely make sure whether a diagnosis of leiomyoma was correctly registered for every single patient in the data base or not. Last, the claims data are deidentified, so many factors are not provided that may influence risk of ULMS, eg, weight, race/ethnicity, and comorbidities. This study, however, has strengths. First, using claim database is helpful for studying rare diseases, such as ULMS. Second, claims database analysis allows for estimation of real-world private insurance treatment patterns. Third, it provides a large, geographically diverse population with complete episodes of care across different healthcare settings. Fourth, it contains longitudinal tracking at the patient level. Last, it provides detailed outpatient data.
CONCLUSIONS
In current gynecology practice, most hysterectomies are performed due to the presence of benign uterine leiomyomas.21,22 To date, there is no preoperative technique that reliably differentiates ULMS from uterine leiomyoma before the definitive surgery.23 LSH and LM are popular methods of treating uterine leiomyoma since laparoscopic surgery has various advantages, such as reduced blood transfusion, less surgical site infection, less venous thrombosis, shorter length of hospital admission, less postoperative pain, improved quality of life, and faster recovery when compared to laparotomy.24,25 Although the use of morcellation renders it possible to perform minimally invasive surgery in patients with leiomyoma, the morcellation of occult ULMS has been shown to be associated with adverse survival outcomes by potentially spreading an occult malignancy.26–28 Therefore, it is important to weigh the risk of occult ULMS before performing a laparoscopic procedure for a diagnosis of presumed leiomyoma.
Our analysis shows that the risk of postoperative diagnosis of occult ULMS increases after age of 50 in LSH cases. LM cases show similar increments after the age of 40. An effort to minimize the risk of developing occult ULMS after the surgery is needed because minimally invasive surgical approaches offer various advantages to patients. More definitive diagnostic and predictive tests or safer techniques that enable removal of surgical specimen may be helpful to overcome the concerns in LSH or LM cases. Our results study show that the use of age brackets may help us approximate risk to prevent dissemination of occult ULMS by avoiding minimally invasive surgery, which will also lead to a more accurate informed consent process.
Footnotes
The authors report no conflict of interest
REFERENCES
- 1.Kapp DS, Shin JY, Chan JK. Prognostic factors and survival in 1396 patients with uterine leiomyosarcomas: emphasis on impact of lymphadenectomy and oophorectomy. Cancer. 2008; 112(4): 820–30. [DOI] [PubMed] [Google Scholar]
- 2.Perri T, Korach J, Sadetzki S, Oberman B, Fridman E, Ben-Baruch G. Uterine leiomyosarcoma: does the primary surgical procedure matter? Int J Gynecol Cancer. 2009; 19(2): 257–60. [DOI] [PubMed] [Google Scholar]
- 3.Theben JU, Schellong AR, Altgassen C,Kelling K, Schneider S, Grosse-Drieling D. Unexpected malignancies after laparoscopic-assisted supracervical hysterectomies (LASH): an analysis of 1,584LASHcases. Arch Gynecol Obstet. 2013;287:455–462. [DOI] [PubMed] [Google Scholar]
- 4.Seidman MA, Oduyebo T, Muto MG, Crum CP, Nucci MR, Quade BJ. Peritoneal dissemination complicating morcellation of uterine mesenchymal neoplasms. PLoS One. 2012;7:e50058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinha R, Hegde A, Mahajan C, Dubey N, Sundaram M. Laparoscopic myomectomy: do size, number, and location of the myomas form limiting factors for laparoscopic myomectomy? J Minim Invasive Gynecol. 2008;15:292–300. [DOI] [PubMed] [Google Scholar]
- 6.Della Badia C, Karini H. Endometrial stromal sarcoma diagnosed after uterine morcellation in laparoscopic supracervical hysterectomy. J Minim Invasive Gynecol. 2010; 17(6): 791–3. [DOI] [PubMed] [Google Scholar]
- 7.Lin JF, Slomovitz BM. Uterine sarcoma 2008. Curr Oncol Rep. 2008; 10(6): 512–8. [DOI] [PubMed] [Google Scholar]
- 8.Gockley AA, Rauh-Hain JA, Del Carmen MG. Uterine leiomyosarcoma: a review article. Int J Gynecol Cancer. 2014; 24(9): 1538–42. [DOI] [PubMed] [Google Scholar]
- 9.Goto A, Takeuchi S, Sugimura K, Maruo T. Usefulness of Gd-DTPA contrast-enhanced dynamic MRI and serum determination of LDH and its isozymes in the differential diagnosis of leiomyosarcoma from degenerated leiomyoma of the uterus. Int J Gynecol Cancer. 2002; 12(4): 354–61. [DOI] [PubMed] [Google Scholar]
- 10.OPTUM. Clinformatics Data Mart [Internet]. 2014. [updated 2014; cited 2014 Nov 17]. Available from: https://www.optum.com/life-sciences/differentiate-products/marketing-analytics/clinformatics-data-mart.html.
- 11.Berenson AB, Tan A, Hirth JM, Wilkinson GS. Complications and continuation of intrauterine device use among commercially insured teenagers. Obstet Gynecol. 2013; 121(5): 951–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamasato K, Casey D, Kaneshiro B, Hiraoka M. Effect of robotic surgery on hysterectomy trends: implications for resident education. J Minim Invasive Gynecol. 2014; 21: 399–405. [DOI] [PubMed] [Google Scholar]
- 13.Senapati S, Tu FF, Magrina JF. Power morcellators: a review of current practice and assessment of risk. Am J Obstet Gynecol. 2015; 212(1): 18–23. [DOI] [PubMed] [Google Scholar]
- 14.Milad MP, Milad EA. Laparoscopic morcellator-related complications. J Minim Invasive Gynecol. 2014; 21(3): 486–91. [DOI] [PubMed] [Google Scholar]
- 15.Einstein MH, Barakat RR, Chi DS, et al. Management of uterine malignancy found incidentally after supracervical hysterectomy or uterine morcellation for presumed benign disease. Int J Gynecol Cancer. 2008; 18(5): 1065–70. [DOI] [PubMed] [Google Scholar]
- 16.Wright JD,. Tergas AI, Burke WM, Cui RR, Ananth CV, Chen L, Hershman DL. Prevalence of Uterine Pathology in Women Undergoing Minimally Invasive Hysterectomy Employing Electric Power Morcellation. JAMA. 2014; 312(12): 1253–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mao J, Pfeifer S, Zheng XE, Schlegel P, Sedrakyan A. Population-based estimates of the prevalence of uterine sarcoma among patients with leiomyomata undergoing surgical treatment. JAMA Surg. 2015; 150(4): 368–70. [DOI] [PubMed] [Google Scholar]
- 18.Mahnert N, Morgan D, Campbell D, Johnston C, As-Sanie S. Unexpected gynecologic malignancy diagnosed after hysterectomy performed for benign indications. Obstet Gynecol. 2015;125:397–405. [DOI] [PubMed] [Google Scholar]
- 19.Brohl AS, Li L, Andikyan V, Običan SG, Cioffi A, Hao K, et al. Age-stratified risk of unexpected uterine sarcoma following surgery for presumed benign leiomyoma. Oncologist. 2015;20:433–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Food and Drug Administration. Quantitative assessment of the prevalence of unsuspected uterine sarcoma in women undergoing treatment of uterine fibroids: summary and key findings. Available at: http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM393589.pdf. Accessed April 13, 2015.
- 21.Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol 2013;122(2 Pt 1):233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Congress of Obstetricians and Gynecologists. Women’s health stats & facts: 2011. 2011. Washington, DC, ACOG. [Cited 8-13-2014.] Available from URL: http://www.acog.org/w/media/NewsRoom/MediaKit.pdf [Google Scholar]
- 23.Sagae S, Yamashita K, Ishioka S, Nishioka Y, Terasawa K, Mori M, et al. Preoperative diagnosis and treatment results in 106 patients with uterine sarcoma in Hokkaido, Japan. Oncology 2004;67:33–9. [DOI] [PubMed] [Google Scholar]
- 24.Bhave Chittawar P1, Franik S, Pouwer AW, Farquhar C. Minimally invasive surgical techniques versus open myomectomy for uterine fibroids. Cochrane Database Syst Rev. 2014. Oct 21;10:CD004638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siedhoff MT, Wheeler SB, Rutstein SE, Geller EJ, Doll KM, Wu JM, Clarke-Pearson DL. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perri T, Korach J, Sadetzki S, Oberman B, Fridman E, Ben-Baruch G. Uterine leiomyosarcoma: does the primary surgical procedure matter? Int J Gynecol Cancer 2009;19:257–60. 10.1111/IGC.0b013e31819a1f8f. [DOI] [PubMed] [Google Scholar]
- 27.Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol 2011;122:255–9. [DOI] [PubMed] [Google Scholar]
- 28.George S, Barysauskas C, Serrano C, et al. Retrospective cohort study evaluating the impact of intraperitoneal morcellation on outcomes of localized uterine leiomyosarcoma. Cancer Jun 12 2014. 10.1002/cncr.28844 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]


