Abstract
Background
Immune checkpoint inhibitors (ICIs) are promising agents for unresectable hepatocellular carcinoma (uHCC), but lack effective biomarker to predict outcomes. The gut microbiome can modulate tumor response to immunotherapy, but its effect on HCC remains unclear.
Methods
From May 2018 to February 2020, patients receiving ICI treatment for uHCC were prospectively enrolled; their fecal samples were collected before treatment. The fecal microbiota and metabolites were analyzed from 20 patients with radiology-proven objective responses (OR) and 21 randomly selected patients with progressive disease (PD). After March 2020, 33 consecutive Child-Pugh-A patients were recruited as a validation cohort. Additionally, feces from 17 healthy volunteers were collected for comparison of background microbes.
Results
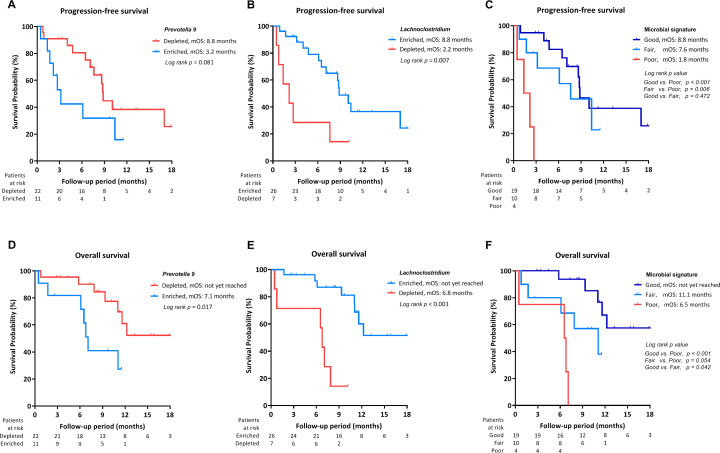
A significant dissimilarity was observed in fecal bacteria between patients with OR and patients with PD before immunotherapy. Prevotella 9 was enriched in patients with PD, whereas Lachnoclostridium, Lachnospiraceae, and Veillonella were predominant in patients with OR. Ursodeoxycholic acid and ursocholic acid were significantly enriched in the feces of patients with OR and strongly correlated with the abundance of Lachnoclostridium. The coexistence of Lachnoclostridium enrichment and Prevotella 9 depletion significantly predicted better overall survival (OS). In the validation cohort, better progression-free survival (PFS) and OS were noted in patients who had a preferable microbial signature in comparison with counter-group (PFS: 8.8 months vs 1.8 months; OS: not reached vs 6.5 months, both p<0.001).
Conclusions
Fecal microbiota and bile acids were associated with outcomes of immunotherapy for uHCC. These findings highlight the potential role of gut microbiota and metabolites as biomarkers to predict outcomes of ICI-treated HCC.
Keywords: immunotherapy, liver neoplasms
WHAT IS ALREADY KNOWN ON THIS TOPIC
Immunotherapies with immune checkpoint inhibitors (ICIs) are promising treatments for unresectable hepatocellular carcinoma (uHCC), but predictive biomarkers for treatment response are lacking.
Accumulating evidence implies that gut microbiota could modulate tumor responses to immunotherapies, but limited data have been reported on patients with HCC.
WHAT THIS STUDY ADDS
Baseline gut microbiota and fecal bile acids were distinct between ICI responders and non-responders in patients with unresectable HCC.
The signature of fecal microbiota with Lachnoclostridium enrichment and Prevotella 9 depletion could independently predict survival of patients with uHCC undergoing ICI treatment.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
Our findings suggest gut microbiota and metabolites as potential biomarkers to the clinical outcomes of ICI-treated uHCC.
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third leading cause of cancer-related death worldwide, which constitutes a major global health problem.1 2 Despite the implementation of universal hepatitis B vaccination, direct-acting antiviral agents for hepatitis C, and active surveillance for high-risk populations, a significant portion of patients still present with or progress to unresectable, advanced-stage diseases that require systemic therapy.2
Immunotherapies with immune checkpoint inhibitors (ICIs) have recently emerged as immunotherapeutic agents for unresectable HCC, including nivolumab and pembrolizumab that block programmed cell death-1 (PD-1), as well as atezolizumab, which blocks programmed death-ligand 1 (PD-L1).3–5 In general, the response rate of HCC to ICIs treatment is around 16%–20% for ICI monotherapy, and 30%–36% for ICI combinations.6 7 The PD-L1 expression level is not recommended as a selection marker for ICI treatment for HCC. CTNNB1 mutation represents an immune-exclusive subclass of HCC and may be resistant to immunotherapy, but further validation is required.8 On-treatment decline of alpha fetoprotein (AFP) has been reported to predict the tumor response to immunotherapy.9 To date, pretreatment tumor or host-related biomarkers associated with the outcomes of HCC to ICI treatment are unmet needs.
Humans harbor nearly 100 trillion gut bacteria that contribute to digestion, intestinal homeostasis and regulate the immune function of the host.10 Dysbiosis is defined as the imbalance between protective and pathogenic bacteria both in quality and quantity; it has been reported to be associated with carcinogenesis.10 Emerging studies also indicate that the gut microbiome has a role in response to cancer therapy across cancer types.11 12 For example, intestinal bacteria can regulate the efficacy of immunotherapy in a xenograft model of melanoma.13 A similar phenomenon was also observed in patients with melanoma that supported the correlation between microbial composition and clinical response.11 14 Despite accumulating evidence that gut microbiota could modulate tumor responses to immunotherapies, limited data have been demonstrated with regard to the concept of targeting the gut microbiota–liver axis for the treatment of HCC. In this study, we investigated the role of gut microbiota and metabolites in the treatment response to ICI therapy and outcomes of patients with unresectable HCC (uHCC).
Materials and methods
Patients
From May 2018 to February 2020, 94 ICI treatment-naïve patients with uHCC were prospectively enrolled from Taipei Veterans General Hospital in a biomarker study before starting ICI treatment as their first-line or second-line systemic treatment. The diagnosis of HCC was according to the criteria of American Association for the Study of Liver Diseases (AASLD) clinical practice guidelines for HCC; typical radiological characteristics and/or pathology in patients with cirrhosis and pathological confirmation in patients without cirrhosis were needed.15 During the study period, the ICIs approved by Taiwan Food and Drug Administration (FDA) for HCC were nivolumab and pembrolizumab.
Fecal samples were collected before immunotherapy from the enrollees if they had not taken antibiotics, probiotics, prebiotics, proton pump inhibitors, or ursodeoxycholic acids 4 weeks prior to ICI initiation. For patients who received second-line therapy, their fecal samples were collected 2 to 4 weeks after discontinuation of sorafenib and before starting ICI therapy. Finally, the fecal microbiota and metabolites were investigated in samples from all patients with radiology-proven objective tumor responses (OR) following immunotherapy (total 20 patients, including 3 complete responses and 17 partial responses), as well as 21 randomly selected patients who experienced progressive disease (PD) as best overall response to ICI treatment in a 1:1 ratio. The sample size was also calculated based on the assumption that 50% of patients with OR had preferable gut microbiota, and 10% of patients with PD had preferable gut microbiota, at least 20 cases in each arm were required for 80% power with 5% chance of alpha error. Tumor response was based on RECIST 1.1. After March 2020, 33 consecutive, ICI-naïve, Child-Pugh-A patients who received ICI as their first-line or second-line treatment for uHCC were recruited in the validation cohort. As immuno-oncology (IO) monotherapy was shifted to IO combination for uHCC after 2020, this cohort recruited 28 patients with IO combinations to validate the findings in the era of IO combinations.16 16S ribosomal RNA (rRNA) gene sequencing data were also collected from the feces of 17 healthy volunteers for comparison of background microbiota.17
Treatment and outcome assessment
ICIs were administered according to the recommended dosing and safety information (2–3 mg/kg, every 2 weeks for nivolumab and 2–3 mg/kg or 200 mg every 3 weeks for pembrolizumab).9 18 The safety assessment and grading were performed using the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE, V.5.0). Clinical evaluations were performed regularly during treatment, including Child-Pugh class, albumin-bilirubin grade,19 hemogram, serum chemistry, and AFP level. The tumor response was assessed using RECIST V.1.1 based on contrast-enhanced abdominal CT scans or MRI3 20; the objective response rate (ORR) as well as disease control rate (DCR) were analyzed. Image examinations were performed every 8 to 9 weeks during ICI treatment. The overall survival (OS) was measured from the date of starting ICIs until death.
Processing and analysis of fecal bacterial genomic data
Fresh feces were collected from patients or healthy volunteers at our hospital based on hygienic standard procedure and then frozen and stored at −80°C within 1 hour. Microbial genomic DNAs were extracted using the CatchGene Stool DNA Kit (CatchGene, New Taipei City, Taiwan) according to the manufacturer’s protocols, which included a bead-beating process for 1 min. The V3-V4 regions of bacterial 16S rRNA genes were amplified by PCR using 341F and 806R primers.21 Next-generation sequencing was performed by the Illumina MiSeq Desktop Sequencer following the standard protocol.22
The 16S rRNA gene sequencing raw reads were processed using Quantitative Insights into Microbial Ecology (QIIME) V.1.9.1,23 and annotated the taxonomy classification based on the SILVA database V.132.24 Taxonomic compositions were identified. Alpha diversities were examined by Shannon and PD whole tree indices and compared by Kruskal-Wallis test. The principal coordinate analysis (PCoA) of microbiota was measured by Bray-Curtis dissimilarity and compared by permutational multivariate analysis of variance (PERMANOVA) test. Linear discriminant analysis (LDA) effect size (LEfSe) analysis was performed with an α value of 0.05 (by Kruskal-Wallis and Wilcoxon rank-sum tests) and an effect size threshold of 3 for LDA to determine the most likely candidate taxa that could explain the differences between groups.24 In addition, Spearman’s rank correlation analysis was conducted between microbial taxa and metabolites.
Measurement of fecal bile acids
Fecal samples (25 mg) were extracted with 1000 µL extraction solution (MeOH:ACN:H2O=2:2:1) containing an internal standard mixture and then incubated at –40°C for 1 hour. Samples were then centrifuged at 12,000 g for 30 min at 4°C. The supernatant was transferred for bile acid (BA) analysis as described previously,25 using Waters ultra-high-performance liquid chromatography coupled with a Waters Xevo TQ-S mass spectrometer (Waters, USA) equipped with an electrospray ionization source operating in positive mode. The final concentration results were processed and quantified by TargetLynx software (Waters). Thirty-nine BAs were measured in the fecal samples using methods created from the retention times and mass spectra acquired from standard solutions, and were analyzed under the same conditions as the samples.
Measurement of fecal short-chain fatty acids
Lyophilized fecal samples (25 mg) were mixed with 500 µL of 70% methanol and sonicated for 30 min. The mixtures were centrifuged at 12,000 rpm for 10 min, and the supernatants were retrieved for derivatization and detection of short-chain fatty acids (SCFAs) as described previously.26 SCFAs were measured with a high-performance liquid chromatography (HPLC) system (SunFire C18 Column, 100 Å, 5 µm, 4.6mm × 250 mm, Waters) equipped with a UV detector (Agilent 1260 Infinity HPLC, USA). The derivatized SCFAs were quantified using the chromatogram area ratio to the internal standard (2-ethylbutyric acid, 1 mM). The peak integrations were calculated using Agilent ChemStation software (Agilent).
Statistical analysis
Continuous variables were expressed as the median (IQR), while categorical variables were analyzed as frequencies and percentages. Pearson χ2 analyses or Fisher’s exact tests were used to compare categorical variables, and Student’s t-tests or the Mann-Whitney U tests were applied for continuous variables. The optimal cut-off values of bacterial abundance to predict tumor response were assessed using the area under receiver operating characteristic curves (AUROC). The value with the highest Youden’s Index (sensitivity +specificity − 1) was considered as the optimal cut-off.27 OS or progression-free survival (PFS) from the beginning of ICI treatment to death or tumor progression was estimated by the Kaplan-Meier method and compared by the log-rank test. Additionally, Cox’s proportional-hazard model was used to identify prognostic factors for survival. Albumin-bilirubin grade and Child-Pugh class were not included in the same multivariate model to avoid the effect of collinearity. For all analyses, p<0.05 was considered statistically significant. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS V.26.0 for Windows, SPSS) and GraphPad Prism V.9 (GraphPad Software, San Diego, California, USA).
Results
Demographic characteristics of the study cohort
Patients were ICI-naïve and predominantly male (85.4%) and most had chronic hepatitis B virus infection (63.4%). On enrollment, most patients were at Child-Pugh class A (82.9%); but 63.4% of them were classified beyond ALBI grade 1. No significant differences in liver reserves were observed between patients with OR or PD to ICI treatment.
Twenty-eight patients were classified in BCLC stage C. The incidences of portal vein invasion or extrahepatic metastasis were comparable between two groups. Compared with patients with PD, more patients with OR were treated with combination therapy by ICI plus tyrosine kinase inhibitor (TKI) (60.0% vs 23.8%, p=0.019). The detailed baseline characteristics of patients are presented in table 1.
Table 1.
Characteristics of patients with HCC in the training cohort (before March 2020)
| Characteristics | Objective response | Progressive disease | P value |
| n=20 | n=21 | ||
| Age, years | 58.8 (55.0–68.4) | 67.3 (55.6–74.5) | 0.211 |
| Sex (male), n (%) | 18 (90.0) | 17 (81.0) | 0.663 |
| HBsAg-positive, n (%) | 14 (70.0) | 12 (57.1) | 0.393 |
| Anti-HCV-positive, n (%) | 6 (30.0) | 5 (23.8) | 0.655 |
| Max. tumor size, cm | 6.2 (3.3–9.8) | 3.8 (2.0–8.2) | 0.192 |
| Tumor >50% liver volume, n (%) | 4 (20.0) | 6 (28.6) | 0.719 |
| Multiple tumors, n (%) | 18 (90.0) | 19 (90.5) | 1.000 |
| Portal vein invasion, n (%) | 9 (45.0) | 9 (42.9) | 0.890 |
| Extrahepatic metastasis, n (%) | 7 (35.0) | 11 (52.4) | 0.262 |
| AFP, ng/mL | 67.4 (5.9–3118.4) | 469.7 (40.5–6492.5) | 0.175 |
| ≥400 ng/mL, n (%) | 7 (35.0) | 11 (52.4) | 0.262 |
| BCLC stage B/C, n (%) | 6/14 (30.0/70.0) | 7/14 (33.3/66.7) | 0.819 |
| Prothrombin time, INR | 1.13 (1.05–1.20) | 1.08 (1.01–1.27) | 0.705 |
| Platelet count, K/cumm | 144 (107–213) | 139 (71–180) | 0.268 |
| ALT, U/L | 32 (18–48) | 47 (30–70) | 0.124 |
| AST, U/L | 49 (30–71) | 64 (39–123) | 0.267 |
| Total bilirubin, mg/dL | 0.69 (0.52–0.89) | 0.81 (0.45–1.56) | 0.754 |
| Albumin, g/dL | 3.7 (3.2–4.1) | 3.8 (3.6–4.0) | 0.440 |
| Neutrophil-lymphocyte ratio | 3.47 (2.15–5.69) | 3.07 (2.37–4.52) | 0.958 |
| Presence of ascites, n (%) | 8 (40.0) | 7 (33.3) | 0.658 |
| Child-Pugh score | 6 (5–6) | 5 (5–6) | 0.346 |
| Child-Pugh class A/B/C, n (%) | 17/3/0 (85.0/15.0/0) | 17/4/0 (81.0/19.0/0) | 1.000 |
| ALBI grade 1/2/3, n (%) | 8/11/1 (40.0/55.0/5.0) | 7/14/0 (33.3/66.7/0) | 0.496 |
| First line systemic therapy, n (%) | 12 (60.0) | 6 (28.6) | 0.043 |
| Prior therapy to ICI, n (%) | |||
| Surgical resection | 8 (40.0) | 12 (57.1) | 0.272 |
| RFA | 5 (25.0) | 12 (57.1) | 0.058 |
| TACE | 11 (55.0) | 12 (57.1) | 0.890 |
| Sorafenib | 8 (40.0) | 15 (71.4) | 0.043 |
| Nivolumab/pembrolizumab, n (%) | 8/12 (40.0/60.0) | 16/5 (76.2/23.8) | 0.019 |
| Combined ICI with TKI, n (%) | 12 (60.0) | 5 (23.8) | 0.019 |
| Immune-related AEs | 4 (20.0) | 6 (28.6) | 0.523 |
The values of continuous variables are presented with median and IQR.
AEs, adverse events; AFP, alpha fetoprotein; ALBI grade, albumin-bilirubin grade; AL(S)T, alanine(aspartate) aminotransferase; BCLC stage, Barcelona-Clinic liver cancer stage; HBsAg, hepatitis B virus surface antigen; HCC, hepatocellular carcinoma; HCV, hepatitis C; ICI, immune checkpoint inhibitors; INR, international normalized ratio; NLR, neutrophil-lymphocyte ratio; RFA, radiofrequency ablation; TACE, trans-arterial chemoembolization; TKI, tyrosine kinase inhibitor.
Association of treatment response with gut microbial composition
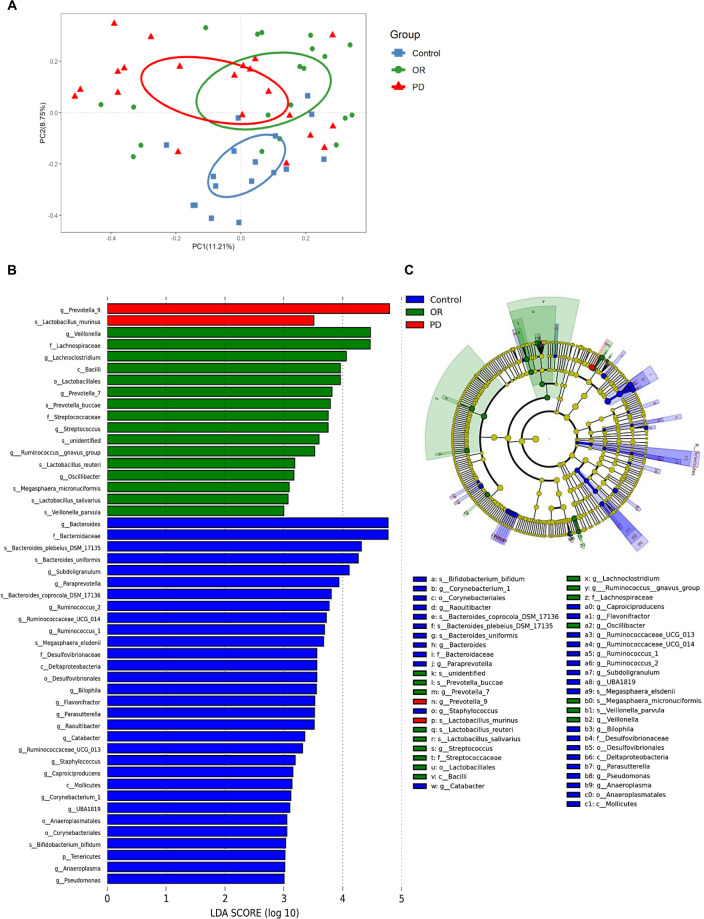
Generally, Firmicutes and Bacteroidetes were the most abundant fecal bacteria in patients with uHCC. At the family level, Lachnospiraceae and Veillonellaceae were enriched in the feces of patients with OR. In contrast, apparent increases of Prevotellaceae and Enterobacteriaceae but reduced abundance of Lachnospiraceae and Veillonellaceae were observed in patients with PD after immunotherapy (online supplemental figure 1A, B). The richness and evenness of microbiota measured by the Shannon index and the phylogenetic diversity whole tree index were not significantly different between patients with HCC and healthy controls (online supplemental figure 1C, D). The PCoA of Bray-Curtis metrics showed a significant microbial dissimilarity between these three groups (p=0.019, <0.001, and <0.001 according to PERMANOVA tests for patients with HCC with OR vs PD, healthy controls vs patients with OR HCC, and healthy controls vs PD HCC patients, respectively; figure 1A). The results of LEfSe analysis (figure 1B, C) showed a prominence of Prevotella 9 (LDA score [log10]>4) in the feces of patients with PD. In contrast, Veillonella, Lachnospiraceae and Lachnoclostridium were predominant in the feces of patients with OR to immunotherapy.
Figure 1.
The diversities and predominant fecal bacteria in patients received immune checkpoint inhibitor (ICI) treatment for unresectable hepatocellular carcinoma (HCC) and healthy controls. (A) Principle coordinates analysis of fecal microbiota by Bray-Curtis dissimilarity metrics. (B) Histograms and (C) cladogram of linear discriminant analysis (LDA) scores computed for differentially abundant taxa in the fecal microbiome. The length of each bar indicates the effect size associated with a taxon, which is significantly different when comparing to other groups. OR, objective response; PD, progressive disease.
jitc-2022-004779supp001.pdf (105.1KB, pdf)
jitc-2022-004779supp002.pdf (97.9KB, pdf)
The pattern of the microbial dissimilarity and the composition of gut microbiota were further analyzed for the subgroup of 24 patients receiving ICI monotherapy. A marginal microbial dissimilarity between OR and PD groups (p=0.075 by PERMANOVA test) was still observed in the PCoA of Bray-Curtis metrics (online supplemental figure 2A). Prevotellaceae, Prevotella 9, and Faecalibacterium were consistently predominant in patients with PD; whereas Veillonella, Lachnoclostridium, Lactobacillales, and linked taxa were predominant in patients with OR according to the LEfSe analysis (online supplemental figure 2B, C). On the other hand, no significant differences of microbial composition as well as alpha and beta diversities were identified between patients with prior experience of TKI (n=23) or not (n=18). Besides, the relative abundance of Prevotella 9 and Lachnoclostridium as well as the concentration of fecal bile acids were not significantly different according to the prior experience of TKI (online supplemental figure 3).
jitc-2022-004779supp003.pdf (246.8KB, pdf)
jitc-2022-004779supp004.pdf (301.9KB, pdf)
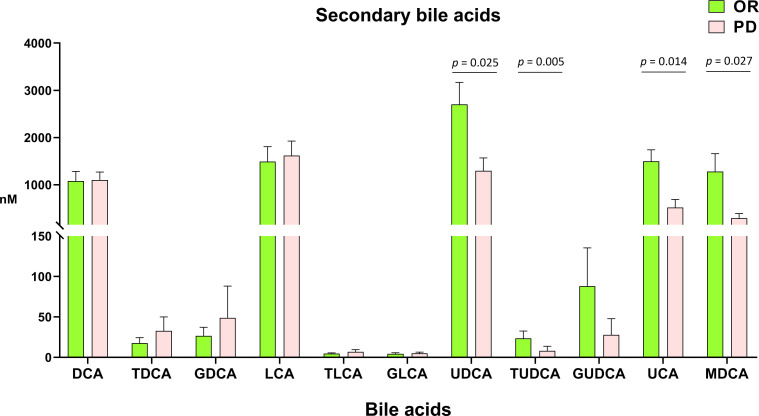
Association of treatment response with gut microbial metabolites
BAs, SCFAs, and other untargeted metabolites in the feces were measured to understand the metabolic profiles associated with tumor response to immunotherapy. Fecal concentrations of primary BAs were generally higher in the OR patients but the difference lacked statistical significance. Interestingly, secondary bile acids, including ursodeoxycholic acid (UDCA), tauro-UDCA, ursocholic acid (UCA), and murideoxycholic acid (MDCA) were significantly enriched in the feces of patients who had OR to immunotherapy compared with their counterparts (figure 2, online supplemental table 1).
Figure 2.
The concentration of secondary bile acids in the feces of patients received immune checkpoint inhibitor (ICI) treatment for unresectable hepatocellular carcinoma (HCC) and healthy controls. DCA, deoxycholic acid; G, glycine conjugated species; LCA, lithocholic acid; MDCA, murideoxycholic acid (murocholic acid); nM, nanomolar; T, taurine-conjugated species; UCA, ursocholic acid; UDCA, ursodeoxycholic acid.
jitc-2022-004779supp006.pdf (107.1KB, pdf)
Acetic acid was the most abundant fecal SCFA in both patients with OR and patients with PD followed by propionic acid and butyric acid. However, no significant differences in the fecal concentration of all detected SCFAs could be identified between these two patient groups. In addition, the non-target analysis also indicated certain metabolites with significant alterations in the feces of patients with OR such as increased concentration of isohyodeoxycholic acid and nutriacholic acid as well as reductions in oxypurinol, inosine, D-glucuronic acid, and so on (online supplemental figure 4).
jitc-2022-004779supp005.pdf (1.1MB, pdf)
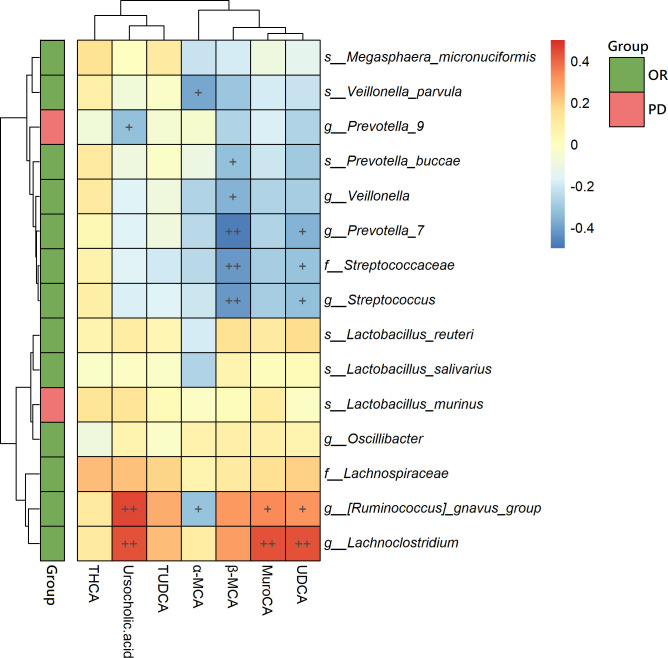
Positive association of fecal metabolites with bacterial species
According to the Spearman correlation analysis (figure 3), the fecal concentrations of UDCA, UCA, and MDCA had significantly positive correlations with the relative abundance of Lachnoclostridium. Positive correlations were also observed between these BAs and fecal Ruminococcus gnavus group (a prominent genus of gut microbe in patients with OR according to LEfSe analysis, LDA score [log10]: 3–4). In contrast, these secondary BAs were negatively correlated with the fecal abundance of Prevotella 9, which was predominant in patients with PD.
Figure 3.
Heatmap of the correlation analysis between the predominant bacterial taxa and fecal bile acids in patients with unresectable hepatocellular carcinoma (HCC). MCA, muricholic acid; MuroCA, murocholic acid (=murideoxycholic acid); THCA, taurohyocholic acid; (T) UDCA, (tauro)ursodeoxycholic acid. The red color indicates positive correlation and the blue color indicates negative correlation. +p<0.05; ++p<0.01.
The association between gut microbiome and survival
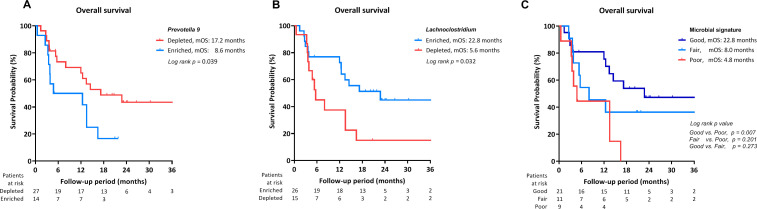
During a median follow-up period of 12.4 (IQR 3.8–21.4) months, the median OS of the study cohort was 13.5 months (95% C.I. 11.1 to 15.9). According to the ROC analyses, the genera Prevotella 9 and Lachnoclostridium were acceptable discriminating microbes to predict tumor response (AUROC: 0.698 and 0.700, respectively). Therefore, the abundances of these two taxa were investigated in survival analyses. Patients with enriched fecal Prevotella 9 had significantly worse OS than the counterparts (median OS: 8.6 months vs 17.2 months, p=0.039, figure 4A). A survival benefit was also observed in patients with enriched fecal Lachnoclostridium (median OS: 22.8 months vs 5.6 months, p=0.032, figure 4B). The best OS was identified in patients with coexistence of Lachnoclostridium enrichment and Prevotella 9 depletion in the feces (median OS: 22.8 months, figure 3C). Tumor volume, AST level, Child-Pugh class, gut microbial abundance, and fecal UDCA concentration were associated with survival in the univariate analysis. In the multivariate analysis, a good signature of fecal microbiota (coexistence of Lachnoclostridium enrichment and Prevotella 9 depletion) was a significant predictor of better OS (table 2).
Figure 4.
Overall survivals of patients with unresectable hepatocellular carcinoma (HCC) treated by checkpoint inhibitor (ICI). Overall survival depended on the relative abundance of (A) fecal Prevotella 9; (B) fecal Lachnoclostridium; and (C) signature of combined these two taxa. Good signature: coexistence of depleted Prevotella 9 and enriched Lachnoclostridium. Poor signature: coexistence of enriched Prevotella 9 and depleted Lachnoclostridium. Fair signature: coexistence of depleted both two bacteria or enriched both two bacteria.
Table 2.
Factors associated with overall survival in patients with HCC treated with immune checkpoint inhibitors
| Univariate | Multivariate (model 1)* | Multivariate (model 2)† | ||||||||
| HR | 95% CI | P value | HR | 95% CI | P | HR | 95% CI | P value | ||
| Age, years | >60 vs ≤60 | 0.643 | 0.242 to 1.706 | 0.375 | NA | NA | ||||
| Sex | Male vs female | 1.313 | 0.299 to 5.770 | 0.718 | NA | NA | ||||
| HBsAg-positive | Yes vs no | 1.152 | 0.404 to 3.286 | 0.791 | NA | NA | ||||
| Anti-HCV-positive | Yes vs no | 0.593 | 0.168 to 2.085 | 0.415 | NA | NA | ||||
| Tumor size, cm | >7 vs ≤ 7 | 2.121 | 0.792 to 5.674 | 0.134 | NA | NA | ||||
| Tumor number | Multiple vs single | 24.183 | 0.027 to 21 310.445 | 0.357 | NA | NA | ||||
| Tumor/Liver volume | >50% vs ≤50% | 2.974 | 1.067 to 8.293 | 0.037 | 0.927 | 0.225 to 3.821 | 0.916 | 0.877 | 0.221 to 3.481 | 0.852 |
| Portal vein invasion | Yes vs no | 2.663 | 0.979 to 7.238 | 0.055 | 1.254 | 0.375 to 4.197 | 0.999 | 1.338 | 0.388 to 4.609 | 0.645 |
| Extrahepatic metastasis | Yes vs no | 1.042 | 0.394 to 2.753 | 0.934 | NA | NA | ||||
| BCLC stage | Stage C vs B | 1.274 | 0.447 to 3.630 | 0.650 | NA | NA | ||||
| AFP, ng/mL | >400 vs ≤400 | 1.667 | 0.638 to 4.357 | 0.297 | NA | NA | ||||
| NLR | >2.5 vs ≤2.5 | 2.233 | 0.719 to 6.933 | 0.165 | NA | NA | ||||
| Prothrombin time, INR | >1.2 vs ≤1.2 | 1.268 | 0.464 to 3.461 | 0.644 | NA | NA | ||||
| Platelet count | >100K vs ≤100K | 0.722 | 0.254 to 2.053 | 0.541 | NA | NA | ||||
| ALT, U/L | >40 vs ≤40 | 1.825 | 0.699 to 4.766 | 0.220 | NA | NA | ||||
| AST, U/L | >40 vs ≤40 | 10.423 | 1.377 – 78/908 | 0.023 | 5.168 | 0.528 to 50.533 | 0.158 | 6.013 | 0.631 to 57.264 | 0.119 |
| Child-Pugh class | Class B vs A | 2.950 | 1.027 to 8.473 | 0.044 | 1.238 | 0.345 to 4.443 | 0.774 | NA | ||
| ALBI grade | Grade 2, 3 vs 1 | 2.062 | 0.715 to 5.946 | 0.181 | NA | 1.490 | 0.380 to 5.841 | 0.567 | ||
| Prior sorafenib treatment | Yes vs no | 0.841 | 0.324 to 2.185 | 0.722 | NA | NA | ||||
| Combined treatment† | Yes vs no | 0.778 | 0.288 to 2.102 | 0.621 | NA | NA | ||||
| Gut microbial abundance | ||||||||||
| Low Lachnoclostridium and high Prevotella 9 | 1 | – | – | 1 | – | – | 1 | – | – | |
| Intermediate status of abundance‡ | 0.253 | 0.064 to 0.996 | 0.049 | 0.234 | 0.047 to 1.176 | 0.078 | 0.216 | 0.043 to 1.076 | 0.061 | |
| High Lachnoclostridium and low Prevotella 9 | 0.239 | 0.080 to 0.715 | 0.010 | 0.283 | 0.088 to 0.908 | 0.034 | 0.279 | 0.088 to 0.890 | 0.031 | |
| Fecal UDCA concentration | High vs low | 0.324 | 0.114 to 0.919 | 0.034 | 0.470 | 0.114 to 1.940 | 0.296 | 0.357 | 0.079 to 1.601 | 0.178 |
| Immunotherapy-related AEs | Yes vs no | 1.401 | 0.481 to 4.082 | 0.536 | NA | NA | ||||
*Model 1 enrolled parameters with p value<0.2 in univariate analysis into multivariate analysis, except ascites and ALBI grade.
†Model 2 enrolled parameters with p value<0.2 in univariate analysis into multivariate analysis, except Child-Pugh class.
‡Combined treatment: combined immune checkpoint inhibitors with tyrosine kinase inhibitors, including sorafenib, lenvatinib, and regorafenib.
§Intermediate abundance of Lachnoclostridium and Prevotella 9: either both low abundance of these two taxa or both high abundance.
AEs, adverse events; AFP, alpha fetoprotein; ALBI grade, albumin-bilirubin grade; AL(S)T, alanine(aspartate) aminotransferase; BCLC stage, Barcelona-Clinic liver cancer stage; HBsAg, hepatitis B virus surface antigen; HCV, hepatitis C; ICI, immune checkpoint inhibitor; INR, international normalized ratio; NA, not adopted; NLR, neutrophil- lymphocyte ratio; UDCA, ursodeoxycholic acid.
Validation cohort
Of the 33 patients in the validation cohort (baseline characteristics in online supplemental table 2), fecal enrichment of Lachnoclostridium was significantly associated with a better ORR and DCR of HCC. The best ORR of 52.6% and DCR of 94.7% were observed in patients with a good microbial signature, in which depleted Prevotella 9 and enriched Lachnoclostridium were coexisted (online supplemental table 3). Patients with depleted Prevotella 9 or enriched Lachnoclostridium had better PFS than those without this signature (figure 5A, B); and the best PFS (8.8 months) was also observed in patients with a good microbial signature (figure 5C). Importantly, patients with a good microbial signature also had a significantly better OS than those with poor signature (coexistence of enriched Prevotella 9 and depleted Lachnoclostridium) or fair signature (coexistent depletion or enrichment of these two taxa) (figure 5D–F).
Figure 5.
Progression-free survival and overall survivals of patients in validation. Progression-free survival and overall survival depended on the relative abundance of (A, D) fecal Prevotella 9; (B, E) fecal Lachnoclostridium; and (C, F) signature of combined these two taxa.
Discussion
This is the first study including validation cohort to support the significant role of gut microbiota–liver axis in the treatment response to ICI treatment and survival in patients with uHCC. The gut microbiota and metabolites were distinct between immunotherapy responders and non-responders in patients with HCC. Furthermore, a fecal microbial signature with enrichment of Lachnoclostridium and depletion of Prevotella 9 was an independent survival factor.
Accumulating evidence suggests that gut microbiome and individual bacterial species contained in the intestine can profoundly affect the host immune system.11–13 A dysregulated gut microbiome is involved in tumorigenesis and progression through multiple regulatory pathways.28 Besides, the gut microbiota has a major impact on the response to immunotherapy in patients with cancer.29 In a melanoma orthotopic xenograft mouse model, commensal Bifidobacterium enhanced the anti-tumor immunity in vivo. Oral administration of Bifidobacterium alone improved tumor control to the same degree as PD-L1–specific antibody therapy, and combination treatment almost stopped tumor outgrowth.13 A human study demonstrated that patients with melanoma who were responders to anti-PD-1 immunotherapy had a higher alpha diversity of fecal microbiota and higher relative abundance of Ruminococcaceae than non-responders.11 Besides, reconstitution of germ-free mice with fecal material from responding patients could lead to improved tumor control, augmented T cell responses, and greater efficacy of anti-PD-L1 therapy.14
Concurrent administration of antibiotics or early exposure during immunotherapy can have controversial impacts on tumor response and survival in patients with advanced HCC, thus underscoring the role of gut dysbiosis in HCC immunotherapy.30 31 The association between gut microbiota and HCC immunotherapy was preliminarily reported in a small case series with only three responders and five non-responders to anti-PD-1 treatment.32 Our previous study with 10 ICI responders failed to reveal a positive association of gut microbiota with the response to ICI.33 In this study, we recruited 20 ICI responders and 21 non-responders for analysis, and a significant pretreatment microbial dissimilarity was observed between patients with OR and patients with PD. Furthermore, a preferable fecal signature with Lachnoclostridium enrichment and Prevotella 9 depletion was identified and validated to predict better survival benefits.
Lachnoclostridium belongs to family Lachnospiraceae and is highly homologous to Ruminococcus gnavus.34 The anti-inflammatory potential of Lachnoclostridium has been reported,35 but its role in tumor control has not been clarified. In addition, the benefits of Lachnospiraceae and Ruminococcaceae are well known in patients with chronic liver diseases and cirrhotic complications.36 In patients with HCC, decreased fecal levels of Lachnospiraceae and Ruminococcus were observed,37 38 whereas enrichment of Ruminococcus was found in three ICI-responding cases.32 Prevotella is genetically diverse between species, and many studies have linked increases in its abundance to inflammatory disorders, including chronic liver inflammation.39 The alterations of Lachnoclostridium and Prevotella 9 in HCC may affect inflammatory processes and are associated with tumor response to ICI treatment.
Maintenance of BA homeostasis is essential for the protection of the liver reserve.40 Accumulating evidence indicates that alterations in BAs, which are regulated by the gut microbiota, can affect hepatic metabolic homeostasis and contribute to the pathogenesis of liver cancer.41 42 Lithocholic acid is a secondary BA derived from the dehydroxylation of chenodeoxycholic acid (CDCA). It is toxic to hepatocytes and increases the risk of developing hepatic neoplasms.43 In contrast, UDCA, which is produced by epimerization of CDCA, is thought to be chemopreventive44; and dietary supplementation with UDCA was reported to reduce experimentally induced hepatic carcinogenesis in rats.45 In this study, the fecal concentration of UDCA was significantly higher in ICI responders compared with non-responders to immunotherapy, whereas the fecal concentration of lithocholic acid was increased in patients with PD. Besides, a strong positive correlation between UDCA and fecal abundance of Lachnoclostridium was observed. Clostridium scindens belongs to the genus Lachnoclostridium,46 and is known to convert CDCA to UDCA by oxidation and epimerization of specific hydroxy groups47; it may explain our findings in correlation analysis.
SCFAs, especially butyrate, are important for regulating gene expression, inflammation, differentiation, and apoptosis of host cells.48 They might be involved in the development of HCC.49 However, no significant association could be identified between fecal SCFAs and the treatment response of HCC to ICI treatment in this study.
ICI combinations can provide a higher tumor response rate and better survival and may be a potential bias in this microbiota study.5 6 However, the pattern of the microbial dissimilarity and the compositions of gut microbiota between responders and non-responders to ICI monotherapy remained the same. Combination treatment was not a significant factor associated with survival in the studied cohort. Besides, prior experience of TKI did not have significant confounding effects on microbial composition and fecal bile acids in our patients. In addition, the line of systemic treatment was not a significant factor to OS.
There are several limitations in this study. First, we could not determine the causal relationship between differential bacteria or metabolite and tumor outcomes. The mechanistic associations between Lachnoclostridium and secondary bile acids also need to be investigated in vitro. Second, dynamic investigations of gut microbiota or metabolites were not performed. However, our previous study showed that the composition of gut microbiota remained unchanged between paired fecal samples of the same patient collected at baseline and 8 weeks post-ICI treatment, thus indicating that ICI treatment would not alter the features of gut microbiome, and the effects of microbial changes might be less prominent on the treatment outcomes.33 Third, atezolizumab plus bevacizumab is currently the recommended first-line systemic therapy for uHCC. Whether our findings could be applied to predict the response to atezolizumab plus bevacizumab requires further exploration. Fourth, not all patients had paired peripheral blood mononuclear cells or biopsy samples before and after ICI treatment to identify ICI-induced immune changes correlated with the identified microbes or bile acids in our cohort. This would be an important study in the future. Fifth, most of the studied patients were viral-related HCC; whether these findings could be generalized to non-viral HCC patients on ICI therapy requires further study.50
In conclusion, the gut microbiome and fecal bile acids were associated with treatment response to ICIs in patients with uHCC. A preferable signature of fecal microbiota could independently predict the survival benefits of these patients. These findings highlight a potential therapeutic strategy to improve treatment outcomes of ICI-treated HCC by modifying the gut microbiota and metabolites.
Footnotes
Contributors: Study concept and design: Y-HH. Acquisition of data: P-CL, C-JW, Y-WH, CJL, C-TC, I-CL, J-CL, M-CH. Analysis and interpretation of data: P-CL, C-JW, KY-L, S-HC, Y-HH. Drafting of manuscript: P-CL, Y-HH. Critical revision: Y-HH. Study supervision: M-CH. Guarantor: Y-HH
Funding: This study was supported by grants from the Ministry of Science and Technology of Taiwan (MOST 108-2321-B-010 -017) and Taipei Veterans General Hospital (V109C-048, V110C-144, V111C-107).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
This study involves human participants and was approved by the Institutional Review Board of Taipei Veterans General Hospital (IRB numbers: 2017-09-007CC, 2019-07-007AC, and 2019-08-006B). Participants gave informed consent to participate in the study before taking part.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019;144:1941–53. 10.1002/ijc.31937 [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver . EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182–236. 10.1016/j.jhep.2018.03.019 [DOI] [PubMed] [Google Scholar]
- 3.El-Khoueiry AB, Sangro B, Yau T, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 2017;389:2492–502. 10.1016/S0140-6736(17)31046-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finn RS, Ryoo B-Y, Merle P, et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J Clin Oncol 2020;38:193–202. 10.1200/JCO.19.01307 [DOI] [PubMed] [Google Scholar]
- 5.Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 2020;382:1894–905. 10.1056/NEJMoa1915745 [DOI] [PubMed] [Google Scholar]
- 6.Finn RS, Ikeda M, Zhu AX, et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol 2020;38:2960–70. 10.1200/JCO.20.00808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yau T, Kang Y-K, Kim T-Y, et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the CheckMate 040 randomized clinical trial. JAMA Oncol 2020;6:e204564. 10.1001/jamaoncol.2020.4564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harding JJ, Nandakumar S, Armenia J, et al. Prospective genotyping of hepatocellular carcinoma: clinical implications of next-generation sequencing for matching patients to targeted and immune therapies. Clin Cancer Res 2019;25:2116–26. 10.1158/1078-0432.CCR-18-2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee P-C, Chao Y, Chen M-H, et al. Predictors of response and survival in immune checkpoint inhibitor-treated unresectable hepatocellular carcinoma. Cancers 2020;12:12010182. 10.3390/cancers12010182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology 2014;146:1513–24. 10.1053/j.gastro.2014.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gopalakrishnan V, Spencer CN, Nezi L, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 2018;359:97–103. 10.1126/science.aan4236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Routy B, Le Chatelier E, Derosa L, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 2018;359:91–7. 10.1126/science.aan3706 [DOI] [PubMed] [Google Scholar]
- 13.Sivan A, Corrales L, Hubert N, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science 2015;350:1084–9. 10.1126/science.aac4255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matson V, Fessler J, Bao R, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 2018;359:104–8. 10.1126/science.aao3290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018;67:358–80. 10.1002/hep.29086 [DOI] [PubMed] [Google Scholar]
- 16.CJ W, Lee PC, Hung YW. Lenvatinib plus pembrolizumab for systemic therapy-naïve and -experienced unresectable hepatocellular carcinoma. Cancer Immunol Immunother 2022. 10.1007/s00262-022-03185-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin X-H, Jiang J-K, Luo J-C, et al. The long term microbiota and metabolic status in patients with colorectal cancer after curative colon surgery. PLoS One 2019;14:e0218436. 10.1371/journal.pone.0218436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee P-C, Chao Y, Chen M-H, et al. Risk of HBV reactivation in patients with immune checkpoint inhibitor-treated unresectable hepatocellular carcinoma. J Immunother Cancer 2020;8:e001072. 10.1136/jitc-2020-001072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 2015;33:550–8. 10.1200/JCO.2014.57.9151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 21.Klindworth A, Pruesse E, Schweer T, et al. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res 2013;41:e1. 10.1093/nar/gks808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fadrosh DW, Ma B, Gajer P, et al. An improved dual-indexing approach for multiplexed 16S rRNA gene sequencing on the Illumina MiSeq platform. Microbiome 2014;2:6. 10.1186/2049-2618-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods 2010;7:335–6. 10.1038/nmeth.f.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quast C, Pruesse E, Yilmaz P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res 2013;41:D590–6. 10.1093/nar/gks1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarafian MH, Lewis MR, Pechlivanis A, et al. Bile acid profiling and quantification in biofluids using ultra-performance liquid chromatography tandem mass spectrometry. Anal Chem 2015;87:9662–70. 10.1021/acs.analchem.5b01556 [DOI] [PubMed] [Google Scholar]
- 26.Inoue H, Takayama K, Takahara C, et al. Determination of short-chain fatty acids in mouse feces by high-performance liquid chromatography using 2-Nitrophenylhydrazine as a labeling reagent. Biol Pharm Bull 2019;42:845–9. 10.1248/bpb.b18-01017 [DOI] [PubMed] [Google Scholar]
- 27.Fluss R, Faraggi D, Reiser B. Estimation of the Youden index and its associated cutoff point. Biom J 2005;47:458–72. 10.1002/bimj.200410135 [DOI] [PubMed] [Google Scholar]
- 28.Yi M, Yu S, Qin S, et al. Gut microbiome modulates efficacy of immune checkpoint inhibitors. J Hematol Oncol 2018;11:47. 10.1186/s13045-018-0592-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kroemer G, Zitvogel L. Cancer immunotherapy in 2017: the breakthrough of the microbiota. Nat Rev Immunol 2018;18:87–8. 10.1038/nri.2018.4 [DOI] [PubMed] [Google Scholar]
- 30.Cheung KS, Lam LK, Seto WK, et al. Use of antibiotics during immune checkpoint inhibitor treatment is associated with lower survival in hepatocellular carcinoma. Liver Cancer 2021;10:606–14. 10.1159/000518090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fessas P, Naeem M, Pinter M, et al. Early antibiotic exposure is not detrimental to therapeutic effect from immunotherapy in hepatocellular carcinoma. Liver Cancer 2021;10:583–92. 10.1159/000519108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng Y, Wang T, Tu X, et al. Gut microbiome affects the response to anti-PD-1 immunotherapy in patients with hepatocellular carcinoma. J Immunother Cancer 2019;7:193. 10.1186/s40425-019-0650-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shen Y-C, Lee P-C, Kuo Y-L, et al. An exploratory study for the association of gut microbiome with efficacy of immune checkpoint inhibitor in patients with hepatocellular carcinoma. J Hepatocell Carcinoma 2021;8:809–22. 10.2147/JHC.S315696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Komiyama S, Yamada T, Takemura N, et al. Profiling of tumour-associated microbiota in human hepatocellular carcinoma. Sci Rep 2021;11:10589. 10.1038/s41598-021-89963-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sehgal R, Bedi O, Trehanpati N. Role of microbiota in pathogenesis and management of viral hepatitis. Front Cell Infect Microbiol 2020;10:341. 10.3389/fcimb.2020.00341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bajaj JS, Khoruts A. Microbiota changes and intestinal microbiota transplantation in liver diseases and cirrhosis. J Hepatol 2020;72:1003–27. 10.1016/j.jhep.2020.01.017 [DOI] [PubMed] [Google Scholar]
- 37.Liu Q, Li F, Zhuang Y, et al. Alteration in gut microbiota associated with hepatitis B and non-hepatitis virus related hepatocellular carcinoma. Gut Pathog 2019;11:1. 10.1186/s13099-018-0281-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piñero F, Vazquez M, Baré P, et al. A different gut microbiome linked to inflammation found in cirrhotic patients with and without hepatocellular carcinoma. Ann Hepatol 2019;18:480–7. 10.1016/j.aohep.2018.10.003 [DOI] [PubMed] [Google Scholar]
- 39.Larsen JM. The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology 2017;151:363–74. 10.1111/imm.12760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chiang JYL, Ferrell JM. Bile acid metabolism in liver pathobiology. Gene Expr 2018;18:71–87. 10.3727/105221618X15156018385515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu L, Feng J, Li J, et al. The gut microbiome-bile acid axis in hepatocarcinogenesis. Biomed Pharmacother 2021;133:111036. 10.1016/j.biopha.2020.111036 [DOI] [PubMed] [Google Scholar]
- 42.Jia B, Jeon CO. Promotion and induction of liver cancer by gut microbiome-mediated modulation of bile acids. PLoS Pathog 2019;15:e1007954. 10.1371/journal.ppat.1007954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kitazawa S, Denda A, Tsutsumi M, et al. Enhanced preneoplastic liver lesion development under ’selection pressure' conditions after administration of deoxycholic or lithocholic acid in the initiation phase in rats. Carcinogenesis 1990;11:1323–8. 10.1093/carcin/11.8.1323 [DOI] [PubMed] [Google Scholar]
- 44.Gérard P. Metabolism of cholesterol and bile acids by the gut microbiota. Pathogens 2013;3:14–24. 10.3390/pathogens3010014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oyama K, Shiota G, Ito H, et al. Reduction of hepatocarcinogenesis by ursodeoxycholic acid in rats. Carcinogenesis 2002;23:885–92. 10.1093/carcin/23.5.885 [DOI] [PubMed] [Google Scholar]
- 46.Ridlon JM, Kang D-J, Hylemon PB, et al. Gut microbiota, cirrhosis, and alcohol regulate bile acid metabolism in the gut. Dig Dis 2015;33:338–45. 10.1159/000371678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baron SF, Franklund CV, Hylemon PB. Cloning, sequencing, and expression of the gene coding for bile acid 7 alpha-hydroxysteroid dehydrogenase from Eubacterium sp. strain VPI 12708. J Bacteriol 1991;173:4558–69. 10.1128/jb.173.15.4558-4569.1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Louis P, Flint HJ. Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiol Lett 2009;294:1–8. 10.1111/j.1574-6968.2009.01514.x [DOI] [PubMed] [Google Scholar]
- 49.Sheng L, Jena PK, Hu Y, et al. Hepatic inflammation caused by dysregulated bile acid synthesis is reversible by butyrate supplementation. J Pathol 2017;243:431–41. 10.1002/path.4983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pfister D, Núñez NG, Pinyol R, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature 2021;592:450–6. 10.1038/s41586-021-03362-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2022-004779supp001.pdf (105.1KB, pdf)
jitc-2022-004779supp002.pdf (97.9KB, pdf)
jitc-2022-004779supp003.pdf (246.8KB, pdf)
jitc-2022-004779supp004.pdf (301.9KB, pdf)
jitc-2022-004779supp006.pdf (107.1KB, pdf)
jitc-2022-004779supp005.pdf (1.1MB, pdf)
Data Availability Statement
Data are available upon reasonable request.