Key Points
Question
How did postpartum care access change during the COVID-19 pandemic, and were these changes different by maternal race and ethnicity?
Findings
In this cohort study of 45 588 women, the overall postpartum care attendance rate decreased from 75.2% in January to December 2019 (prepandemic) to 41.7% in January to March 2020 (early pandemic) and subsequently rebounded to 60.9% in April 2020 to November 2021 (late pandemic). Black and Hispanic women showed slower reductions in nonscheduling rates during April 2020 to November 2021 compared with their White counterparts.
Meaning
The study highlights racial and ethnic disparities in postpartum care access both before and after the onset of the pandemic, raising concerns about disparities in postpartum care–associated maternal and infant outcomes.
This cohort study examines the association between the COVID-19 and racial and ethnic disparities in postpartum care access.
Abstract
Importance
Racial and ethnic disparities in postpartum care access have been well identified in the United States. Such disparities could be exacerbated by the COVID-19 pandemic because of amplified economic distress and compromised social capital among pregnant women who belong to racial or ethnic minority groups.
Objective
To examine whether the COVID-19 pandemic is associated with an increase in the existing racial and ethnic disparity in postpartum care access.
Design, Setting, and Participants
This was a retrospective cohort study using electronic health records data. Multinomial logistic regressions in an interrupted time series approach were used to assess monthly changes in postpartum care access across Asian, Hispanic, non-Hispanic Black (hereafter, Black), non-Hispanic White (hereafter, White) women, and women of other racial groups, controlling for maternal demographic and clinical characteristics. Eligible participants were women who gave live birth at 8 hospitals in the greater Boston, Massachusetts, area from January 1, 2019, to November 30, 2021, allowing for tracking 90-day postpartum access until March 1, 2022.
Exposures
Delivery period: prepandemic (January to December 2019), early pandemic (January to March 2020), and late pandemic (April 2020 to November 2021).
Main Outcomes and Measures
Postpartum care within 90 days after childbirth was categorized into 3 groups: attended, canceled, and nonscheduled.
Results
A total of 45 588 women were included. Participants were racially and ethnically diverse (4735 [10.4%] Asian women, 3399 [7.5%] Black women, 6950 [15.2%] Hispanic women, 28 529 [62.6%] White women, and 1269 [2.8%] women of other race or ethnicity). The majority were between 25 and 34 years of age and married and had a full-term pregnancy, vaginal delivery, and no clinical conditions. In the prepandemic period, the overall postpartum care attendance rate was 75.2%, dropping to 41.7% during the early pandemic period, and rebounding back to 60.9% in the late pandemic period. During the months in the late pandemic, the probability of not scheduling postpartum care among Black (average marginal effect [AME], 1.1; 95% CI, 0.6-1.6) and Hispanic women (AME, 1.3; 95% CI, 0.9-1.6) increased more than among their White counterparts.
Conclusions and Relevance
In this cohort study of postpartum care access before and during the COVID-19 pandemic, racial and ethnic disparities in postpartum care were exacerbated following the onset of the COVID-19 pandemic, when postpartum care access recovered more slowly among Black and Hispanic women than White women. These disparities require swift attention and amelioration to address barriers for these women to obtain much needed postpartum care during this pandemic.
Introduction
The postpartum period is a critical time for women to recover from childbirth and adapt to multiple biological, psychological, and social transitions.1 This “fourth trimester” is critical for their long-term well-being.1 Most importantly, high-quality postpartum care can enhance maternal and infant health2 through prevention, early detection, and treatment of physical and mental complications that lead to maternal morbidity and mortality.3,4 The American College of Obstetricians and Gynecologists (ACOG) has recommended that women should seek comprehensive postpartum care no later than 90 days after delivery.5 However, postpartum care visits may have been interrupted during the COVID-19 pandemic with large-scale social distancing measures.6,7 Compared with women who delivered before the pandemic, women who delivered in the early pandemic (April 2020) were 7.8% less likely to attend postpartum care.8 Postpartum care interruption might put new mothers at risk of life-threatening health complications, as approximately 61% of maternal deaths occur in the postpartum period.9 Women who delay or skip postpartum care miss valuable opportunities to address challenging health concerns,10 resulting in frequent emergency department visits, disproportionate hospitalizations,11 and undiagnosed postpartum depression.12 The COVID-19 pandemic has been evolving and changing dramatically, which can deteriorate pregnancy outcomes post partum.
Prior to the COVID-19 pandemic, racial disparities in postpartum care and maternal health outcomes persisted.13 Black mothers had the highest risks and the fastest increasing rate in pregnancy-related mortality and morbidity across all race and ethnicity groups.14,15 Compared with White individuals, Black individuals were 3 to 4 times more likely to die from pregnancy-related complications,16 had 3-fold higher severe maternal morbidity rates,17 and were more than 2 times as likely to be diagnosed with postpartum depression,18,19,20 the long-term effects of which would impact their offspring.21,22 Lack of adequate postpartum care access likely contributed to these maternal health disparities facing Black patients,23 who were 3.5% less likely than White patients to attend postpartum visits.24 Nearly half of racial and ethnic minority individuals, compared with only 9% of White individuals, reported unmet postpartum care needs.25
During the COVID-19 pandemic, Black and Hispanic pregnant people have been more than twice as likely as non-Hispanic White pregnant people to be infected and/or die from COVID-19,26 putting these racial and ethnic minority women at increased risk of adverse postpartum behaviors and outcomes. As stated in the United Nations Secretary-General’s policy, the COVID-19 pandemic has exposed vulnerabilities in social, political, and economic systems, widening preexisting inequalities.27 The impacts of the pandemic were amplified among populations that earn less, save less, hold less secure jobs, and have less access to social protection.27 The fear of infection risk,28 the stress of constrained health care supply,29 the limited access to transportation,7 and the reduced outside support due to social isolation,30—all of which disproportionately affected Black pregnant individuals31,32—have complicated postpartum care during the pandemic.
Postpartum care access and its racial disparities during the COVID-19 pandemic have not been well explored,33 making it difficult to remedy the disparities in postpartum care access and its associated maternal health burden. Using electronic health records (EHR) data from a large health system, this study aimed to examine the changes in postpartum care access before and during the COVID-19 pandemic, overall and by maternal race.
Methods
Data Sources and Study Participants
This study analyzed EHR data of women visiting and giving birth in 8 hospitals with obstetric units in the Mass General Brigham (MGB) system (previously named Partners Health System) in Massachusetts. The EHR provided information on women’s delivery year and month, demographic characteristics, pregnancy-related characteristics, clinical conditions, and maternal residential county, linking to 2017-2019 American Community Surveys34 for county-level social vulnerability index.35
To obtain access to the data set and ensure confidentiality of patient information, researchers at MGB deidentified patient information and provisionally approved data access by the team at the University of South Carolina (UofSC). The research protocol has been exempted by the institutional review board of both UofSC and MGB. This study followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Eligible women (1) gave live birth between January 1, 2019, and November 30, 2021, and (2) had health records from labor and delivery to 90 days post partum. Cases were selected based on delivery month because (1) the time point is the baseline of the outcome of interest (postpartum care access) and (2) the time point reflects the length of COVID-19 exposure during postpartum. Among 50 097 eligible cases, 4509 duplications were removed, yielding a total of 45 588 women in the final analysis.
Measures
Postpartum Care Access
Postpartum care access was identified by the record of postpartum encounter status at 90 days post partum. Encounters were categorized into 3 groups: (1) attended, (2) scheduled but canceled, and (3) never scheduled.
Maternal Race and Ethnicity
Race and ethnicity information was recorded in the EHR data. It was categorized into Asian (n = 4735), Hispanic (n = 6950), non-Hispanic Black (hereafter, Black; n = 3399), non-Hispanic White (hereafter, White; n = 28 526), and other races, including American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and multiple races (n = 1269).
Delivery Month
To assess racial and ethnic differences of postpartum care access from January 2019 to November 2021, delivery month was considered continuous with 2 cutoffs: January 2020, when the first US reproductive-age woman was confirmed with COVID-1926 and when COVID-19 was declared a public health emergency globally by the World Health Organization (WHO),36 and April 2020, when MGB launched units for COVID-19 tests and treatments for patients.37 Delivery month was therefore categorized into 3 periods: prepandemic (January to December 2019), early pandemic (January to March 2020), and late pandemic (April 2020 to November 2021).
Covariates
Covariates were selected based on Andersen behavioral model of health services use.38 Demographic information included age (<18, 18-24, 25-34, 35-44, and ≥45 years) and marital status (single, married or life partner, and other). Pregnancy-related and obstetric characteristics included prenatal care attendance39 (timely [if the first prenatal care visit occurred during the first trimester] and delayed [if the first prenatal care visit occurred after the first trimester or no prenatal care] prenatal care), gestational age at delivery (<28, 28-36, and ≥37 weeks), delivery mode (natural vaginal, cesarean, vaginal birth after cesarean [VBAC], and others [eg, induction]). Clinical and behavioral indicators included any severe maternal morbidity,40 diabetes, hypertension, depression, and smoking. Residence county–level characteristics included social vulnerability index (bottom quartile, second quartile, third quartile, top quartile). A higher quartile indicates greater negative effects on communities caused by external stresses on human health.35
Statistical Analysis
Descriptive statistics (frequencies and percentages) are presented to describe distributions of postpartum women in terms of their maternal characteristics by race and ethnicity. Bivariate analyses of the association between maternal characteristics and postpartum care access in different time periods were conducted using χ2 tests. Multinomial logistic regression in an interrupted time series approach was used to assess monthly changes in postpartum care access across racial groups, controlling for the aforementioned covariates. To compare monthly trends between race and ethnicity subgroups in each of the periods, contrast statements were used for each interaction of race and ethnicity and delivery month.
Descriptive statistics and bivariate analyses were performed with SPSS statistical software version 26.0 (IBM Corp). Multinomial logistic regression was performed with Stata version 15 (StataCorp). Average marginal effects (AMEs) and 95% CIs were estimated. A 2-tailed P < .05 was used to indicate statistical significance.
Results
The 45 588 women who delivered between January 2019 and November 2021 were racially and ethnically diverse (4735 [10.4%] Asian; 3399 [7.5%] Black; 6950 [15.2%] Hispanic; 28 526 [62.6%] White, and 1269 [2.8%] other races). Overall, women were predominantly aged 25 to 34 years and married and had full-term pregnancies, vaginal deliveries, and no clinical conditions, while the distributions varied across racial and ethnic groups (Table 1). As shown in Figure 1,41 the proportion of women attending, canceling, and not scheduling postpartum care within each race and ethnicity group was relatively stable during prepandemic period, from January to December 2019. In the early pandemic (January to March 2020), among all race and ethnicity groups, the attending rate rapidly dropped (from 75.2% to 41.7%), while the canceling and nonscheduling rates correspondingly increased. In the late pandemic (April 2020 to November 2021), the crude attending rate rebounded gradually (to 60.9%), and the crude canceling and nonscheduling rates started to diminish. However, as of November 2021, the crude attending rates were still lower than prepandemic rate within each racial group. Crude cancelation rates as of November 2021 were still higher than those in November 2019.
Table 1. Maternal Characteristics by Race and Ethnicity Among 45 588 Women Who Delivered Between January 2019 and November 2021 in the Mass General Brigham System.
| Characteristic | Race and ethnicity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Asian | Black | Hispanic | Othera | White, No. (%) | |||||
| No. (%) | P valueb | No. (%) | P valueb | No. (%) | P valueb | No. (%) | P valueb | ||
| Childbirths | 4735 (10.4) | NA | 3399 (7.5) | NA | 6950 (15.2) | NA | 1269 (2.8) | NA | 28 526 (62.6) |
| Age | |||||||||
| <18 | 2 (<0.1) | <.001 | 14 (0.4) | <.001 | 87 (1.3) | <.001 | 6 (0.5) | <.001 | 19 (0.1) |
| 18-24 | 102 (2.2) | 402 (11.8) | 1455 (20.9) | 140 (11.0) | 1028 (3.6) | ||||
| 25-34 | 2955 (62.4) | 1927 (56.7) | 3862 (55.6) | 720 (56.7) | 17 264 (60.5) | ||||
| 35-44 | 1652 (34.9) | 1029 (30.3) | 1533 (22.1) | 397 (31.3) | 10 082 (35.3) | ||||
| ≥45 | 24 (0.5) | 27 (0.8) | 13 (0.2) | 6 (0.5) | 133 (0.5) | ||||
| Marital status | |||||||||
| Single | 357 (7.5) | <.001 | 1622 (47.7) | <.001 | 3243 (46.7) | <.001 | 281 (22.1) | <.001 | 3913 (13.7) |
| Married or life partner | 4334 (91.5) | 1677 (49.3) | 3453 (49.7) | 945 (74.5) | 24 190 (84.8) | ||||
| Other | 44 (0.9) | 100 (2.9) | 254 (3.7) | 43 (3.4) | 423 (1.5) | ||||
| PNC attendance | |||||||||
| Delayed PNC | 1325 (28.1) | .25 | 1567 (46.3) | <.001 | 2983 (43.1) | <.001 | 430 (34.0) | <.001 | 7742 (27.2) |
| Timely PNC | 3398 (71.9) | 1817 (53.7) | 3942 (56.9) | 835 (66.0) | 20 676 (72.8) | ||||
| GA at delivery, wk | |||||||||
| <28 | 9 (0.2) | .46 | 30 (0.9) | <.001 | 28 (0.4) | <.001 | 0 | .04 | 55 (0.2) |
| 28-36 | 307 (6.5) | 341 (10.1) | 597 (8.7) | 107 (8.5) | 1991 (7.0) | ||||
| ≥37 | 4387 (93.3) | 2989 (89.0) | 6271 (90.9) | 1154 (91.5) | 26 275 (92.8) | ||||
| Delivery mode | |||||||||
| Natural vaginal | 3157 (66.7) | .03 | 2056 (60.5) | <.001 | 4642 (66.8) | <.001 | 811 (63.9) | .03 | 18 873 (66.2) |
| Cesarean | 1466 (31.0) | 1244 (36.6) | 2115 (30.4) | 432 (34.0) | 8978 (31.5) | ||||
| VBAC | 104 (2.2) | 95 (2.8) | 188 (2.7) | 26 (2.0) | 550 (1.9) | ||||
| Other | 8 (0.2) | 4 (0.1) | 4 (0.1) | 0 | 121 (0.4) | ||||
| Severe maternal morbidityc | |||||||||
| Positive | 53 (1.1) | .45 | 88 (2.6) | <.001 | 101 (1.5) | <.001 | 15 (1.2) | .52 | 285 (1.0) |
| Negative | 4682 (98.9) | 3311 (97.4) | 6849 (98.5) | 1254 (98.8) | 28 241 (99.0) | ||||
| Diabetes | |||||||||
| Positive | 811 (17.1) | <.001 | 462 (13.6) | <.001 | 710 (10.2) | <.001 | 138 (10.9) | <.001 | 2142 (7.5) |
| Negative | 3924 (82.9) | 2937 (86.4) | 6240 (89.8) | 1131 (89.1) | 26 384 (92.5) | ||||
| Hypertension | |||||||||
| Positive | 302 (6.4) | <.001 | 525 (15.4) | <.001 | 709 (10.2) | <.001 | 129 (10.2) | .02 | 3551 (12.4) |
| Negative | 4433 (93.6) | 2874 (84.6) | 6241 (89.8) | 1140 (89.8) | 24 975 (87.6) | ||||
| Depression | |||||||||
| Positive | 98 (2.1) | <.001 | 162 (4.8) | <.001 | 381 (5.5) | <.001 | 84 (6.6) | .03 | 2379 (8.3) |
| Negative | 4637 (97.9) | 3237 (95.2) | 6569 (94.5) | 1185 (93.4) | 26 147 (91.7) | ||||
| Smoking | |||||||||
| Positive | 8 (0.2) | <.001 | 40 (1.2) | .55 | 61 (0.9) | .004 | 15 (1.2) | .72 | 371 (1.3) |
| Negative | 4727 (99.8) | 3359 (98.8) | 6889 (99.1) | 1254 (98.8) | 28 155 (98.7) | ||||
| County-level social vulnerability, quartiled | |||||||||
| Bottom | 35 (0.7) | <.001 | 40 (1.2) | <.001 | 146 (2.1) | <.001 | 20 (1.6) | .001 | 516 (1.8) |
| Second | 1228 (26.0) | 1820 (53.6) | 4209 (60.6) | 429 (34.0) | 8465 (29.7) | ||||
| Third | 256 (5.4) | 73 (2.2) | 149 (2.1) | 38 (3.0) | 1313 (4.6) | ||||
| Top | 3205 (67.8) | 1461 (43.0) | 2442 (35.2) | 776 (61.4) | 18 183 (63.9) | ||||
| Hospital | |||||||||
| BWH | 1782 (37.6) | <.001 | 2022 (59.5) | <.001 | 2944 (42.4) | <.001 | 493 (38.8) | <.001 | 9766 (34.2) |
| CDH | 93 (2.0) | 37 (1.1) | 217 (3.1) | 53 (4.2) | 1116 (3.9) | ||||
| MGH | 1167 (24.6) | 673 (19.8) | 1830 (26.3) | 343 (27.0) | 5687 (19.9) | ||||
| MVH | 5 (0.1) | 32 (0.9) | 8 (0.1) | 68 (5.4) | 291 (1.0) | ||||
| NCH | 4 (0.1) | 24 (0.7) | 95 (1.4) | 18 (1.4) | 200 (0.7) | ||||
| NWH | 1409 (29.8) | 379 (11.2) | 518 (7.5) | 182 (14.3) | 7561 (26.5) | ||||
| SLM | 169 (3.6) | 195 (5.7) | 1261 (18.1) | 66 (5.2) | 1375 (4.8) | ||||
| WDH | 105 (2.2) | 37 (1.1) | 74 (1.1) | 46 (3.6) | 2518 (8.8) | ||||
Abbreviations: BWH, Brigham and Women’s Hospital; CDH, Cooley Dickinson Hospital; GA, gestational age; MGH, Massachusetts General Hospital; MVH, Martha’s Vineyard Hospital; NA, not applicable; NCH, Nantucket Cottage Hospital; NWH, Newton-Wellesley Hospital; PNC, prenatal care; SLM, Salem Hospital; VBAC, vaginal birth after cesarean; WDH, Wentworth Douglass Hospital.
Other racial groups include American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and multiple races.
Differences in maternal characteristics across race groups were calculated with χ2 tests, with non-Hispanic White as the reference group.
Severe maternal morbidity was identified with the US Centers for Disease Control and Prevention list of 21 indicators, including acute myocardial infarction, aneurysm, acute kidney failure, adult respiratory distress syndrome, amniotic fluid embolism, cardiac arrest or ventricular fibrillation, conversion of cardiac rhythm, disseminated intravascular coagulation, eclampsia, heart failure or arrest during surgery or procedure, puerperal cerebrovascular disorders, pulmonary edema or acute heart failure, severe anesthesia complications, sepsis, shock, sickle cell disease with crisis, air and thrombotic embolism, blood products transfusion, hysterectomy, temporary tracheostomy, and ventilation.
Social vulnerability was indicated by the social vulnerability index and was categorized into quartiles. Higher quartile indicates greater vulnerability.
Figure 1. Trends in Postpartum Care Attendance, Cancellation, and Nonscheduling by Delivery Month Between January 2019 and November 2021.
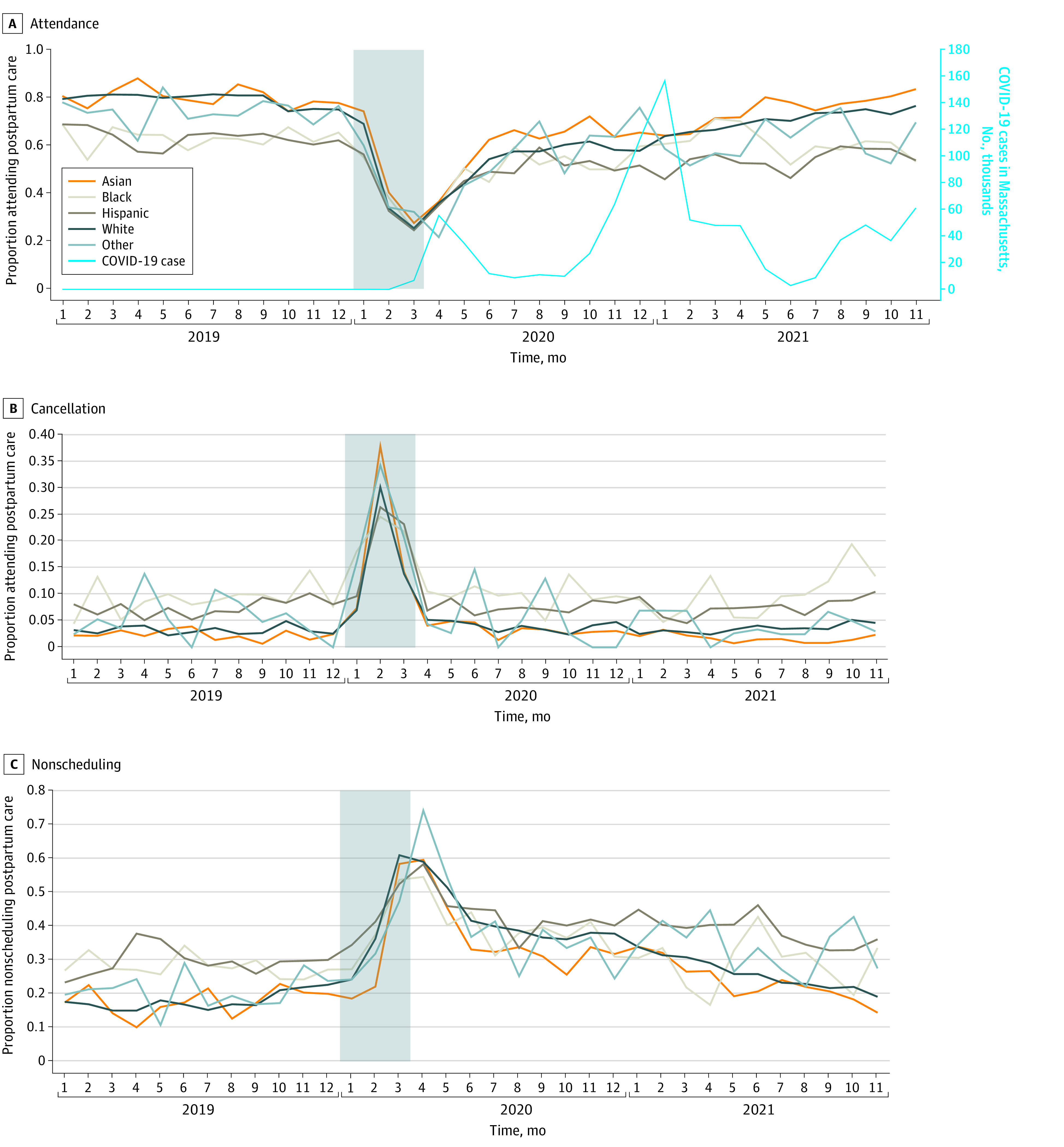
Number of COVID-19 cases in Massachusetts per month were derived from Centers for Disease Control and Prevention (CDC).41 Shaded area indicates early pandemic period.
Associations Between Maternal Characteristics and Postpartum Care Access Over Time
Black and Hispanic women consistently had lower attending rates over the 3 time periods compared with their White counterparts. From prepandemic to early pandemic periods, the canceling rate among Black and Hispanic women increased from 9.1% to 21.5% and from 7.4% to 19.5%, respectively, while that among White women increased from 3.2% to 16.6%. Yet, from the early pandemic to late pandemic periods, White women had stronger improvements in postpartum care access, with a relatively larger drop in canceling rates (from 16.6% to 3.7%), than Black women (from 21.5% to 10.0%) and Hispanic women (from 19.5% to 7.6%). Most maternal demographic characteristics and clinical conditions were associated with postpartum care access regardless of time periods. For example, women who were married or had a life partner had a higher rate of attending postpartum care than single women. A few maternal characteristics showed varied associations with postpartum care access across time. For example, women who had severe maternal morbidity were significantly less likely to not schedule postpartum care compared with women who had no severe maternal morbidity (28.7% vs 34.5%; P < .001) during the late pandemic period, but not during the prepandemic or early pandemic periods (Table 2).
Table 2. Bivariate Associations Between Maternal Characteristics and Postpartum Care Access Among 45 588 Women Who Delivered Between January 2019 and November 2021 in the Mass General Brigham Systema.
| Characteristic | Postpartum care access | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prepandemic period (n = 15 677) | Early pandemic period (n = 3987) | Late pandemic period (n = 25 924) | ||||||||||
| No. (row %) | P value | No. (row %) | P value | No. (row %) | P value | |||||||
| Attended | Canceled | Nonscheduled | Attended | Canceled | Nonscheduled | Attended | Canceled | Nonscheduled | ||||
| Women | 11 785 (75.2) | 671 (4.3) | 3221 (20.5) | NA | 1664 (41.7) | 717 (18.0) | 1606 (40.3) | NA | 15787 (60.9) | 1214 (4.7) | 8923 (34.4) | NA |
| Race and ethnicity | ||||||||||||
| Asian | 1396 (80.1) | 41 (2.4) | 305 (17.5) | <.001 | 201 (47.0) | 87 (20.3) | 140 (32.7) | .004 | 1752 (68.3) | 64 (2.5) | 749 (29.2) | <.001 |
| Blackb | 756 (63.2) | 109 (9.1) | 331 (27.7) | 119 (39.3) | 65 (21.5) | 119 (39.3) | 1071 (56.4) | 190 (10.0) | 639 (33.6) | |||
| Hispanic | 1538 (63.1) | 181 (7.4) | 717 (29.4) | 229 (38.1) | 117 (19.5) | 255 (42.4) | 2034 (52.0) | 298 (7.6) | 1581 (40.4) | |||
| White | 7608 (79.2) | 306 (3.2) | 1693 (17.6) | 1057 (42.4) | 413 (16.6) | 1024 (41.1) | 10 333 (62.9) | 612 (3.7) | 5480 (33.4) | |||
| Other | 340 (74.6) | 24 (5.3) | 92 (20.2) | 39 (40.2) | 24 (24.7) | 34 (35.1) | 419 (58.5) | 32 (4.5) | 265 (37.0) | |||
| Age, y | ||||||||||||
| <18 | 18 (35.3) | 9 (17.6) | 24 (47.1) | <.001 | 2 (25.0) | 1 (12.5) | 5 (62.5) | <.001 | 23 (28.8) | 6 (7.5) | 51 (63.8) | <.001 |
| 18-24 | 559 (54.0) | 99 (9.6) | 378 (36.5) | 80 (27.2) | 56 (19.0) | 158 (53.7) | 815 (43.3) | 176 (9.3) | 892 (47.4) | |||
| 25-34 | 7050 (75.6) | 369 (4.0) | 1912 (20.5) | 1019 (43.2) | 388 (16.5) | 951 (40.3) | 9492 (61.5) | 676 (4.4) | 5274 (34.2) | |||
| 35-44 | 4084 (78.9) | 192 (3.7) | 898 (17.4) | 555 (42.3) | 270 (20.6) | 488 (37.2) | 5386 (64.0) | 352 (4.2) | 2674 (31.8) | |||
| ≥45 | 74 (87.1) | 2 (2.4) | 9 (10.6) | 8 (57.1) | 2 (14.3) | 4 (28.6) | 71 (66.4) | 4 (3.7) | 32 (29.9) | |||
| Marital status | ||||||||||||
| Single | 1883 (61.3) | 286 (9.3) | 902 (29.4) | <.001 | 284 (34.5) | 164 (19.9) | 375 (45.6) | <.001 | 2849 (50.5) | 493 (8.7) | 2305 (40.8) | <.001 |
| Married or life partner | 9690 (79.3) | 360 (2.9) | 2167 (17.7) | 1343 (43.9) | 539 (17.6) | 1180 (38.5) | 12 699 (64.7) | 672 (3.4) | 6247 (31.8) | |||
| Other | 212 (54.5) | 25 (6.4) | 152 (39.1) | 37 (36.3) | 14 (13.7) | 51 (50.0) | 239 (36.3) | 49 (7.4) | 371 (56.3) | |||
| PNC attendance | ||||||||||||
| Delayed | 1733 (36.7) | 323 (6.8) | 2670 (56.5) | <.001 | 293 (21.4) | 142 (10.3) | 937 (68.3) | <.001 | 2419 (29.0) | 501 (6.0) | 5416 (65.0) | <.001 |
| Timely | 9992 (91.9) | 345 (3.2) | 535 (4.9) | 1365 (52.5) | 574 (22.1) | 663 (25.5) | 13 336 (76.1) | 711 (4.1) | 3467 (19.8) | |||
| GA at delivery, wk | ||||||||||||
| <28 | 31 (72.1) | 4 (9.3) | 8 (18.6) | .005 | 4 (33.3) | 3 (25.0) | 5 (41.7) | .07 | 49 (73.1) | 8 (11.9) | 10 (14.9) | <.001 |
| 28-36 | 945 (77.5) | 86 (7.1) | 188 (15.4) | 147 (45.2) | 71 (21.8) | 107 (32.9) | 1205 (63.3) | 150 (7.9) | 548 (28.8) | |||
| ≥37 | 10 741 (75.4) | 575 (4.0) | 2933 (20.6) | 1504 (41.6) | 640 (17.7) | 1473 (40.7) | 14 491 (60.9) | 1052 (4.4) | 8264 (34.7) | |||
| Delivery mode | ||||||||||||
| Natural vaginal | 7645 (73.7) | 427 (4.1) | 2300 (22.2) | <.001 | 1010 (39.3) | 467 (18.2) | 1090 (42.5) | <.001 | 10 241 (60.0) | 790 (4.6) | 6027 (35.3) | <.001 |
| Cesarean | 3806 (78.3) | 226 (4.6) | 830 (17.1) | 613 (46.9) | 226 (17.3) | 467 (35.8) | 5205 (62.7) | 397 (4.8) | 2697 (32.5) | |||
| VBAC | 260 (70.8) | 18 (4.9) | 89 (24.3) | 33 (34.4) | 22 (22.9) | 41 (42.7) | 307 (59.4) | 27 (5.2) | 183 (35.4) | |||
| Other | 73 (97.3) | 0 | 2 (2.7) | 8 (53.3) | 2 (13.3) | 5 (33.3) | 33 (70.2) | 0 | 14 (29.8) | |||
| Severe maternal morbidity | ||||||||||||
| Positive | 126 (78.3) | 8 (5.0) | 27 (16.8) | .47 | 22 (52.4) | 8 (19.0) | 12 (28.6) | .27 | 223 (62.8) | 30 (8.5) | 102 (28.7) | <.001 |
| Negative | 11 659 (75.1) | 663 (4.3) | 3194 (20.6) | 1642 (41.6) | 709 (18.0) | 1594 (40.4) | 15 564 (60.9) | 1184 (4.6) | 8821 (34.5) | |||
| Diabetes | ||||||||||||
| Positive | 1004 (77.2) | 76 (5.8) | 220 (16.9) | <.001 | 167 (48.3) | 64 (18.5) | 115 (33.2) | .01 | 1735 (64.8) | 151 (5.6) | 793 (29.6) | <.001 |
| Negative | 10 781 (75.0) | 595 (4.1) | 3001 (20.9) | 1497 (41.1) | 653 (17.9) | 1491 (41.0) | 14 052 (60.5) | 1063 (4.6) | 8130 (35.0) | |||
| Hypertension | ||||||||||||
| Positive | 1261 (78.9) | 77 (4.8) | 260 (16.3) | <.001 | 232 (51.2) | 66 (14.6) | 155 (34.2) | <.001 | 2162 (66.7) | 155 (4.8) | 926 (28.6) | <.001 |
| Negative | 10 524 (74.7) | 594 (4.2) | 2961 (21.0) | 1432 (40.5) | 651 (18.4) | 1451 (41.1) | 13 625 (60.1) | 1059 (4.7) | 7997 (35.3) | |||
| Depression | ||||||||||||
| Positive | 715 (73.8) | 64 (6.6) | 190 (19.6) | .001 | 93 (40.8) | 36 (15.8) | 99 (43.4) | .52 | 1128 (58.0) | 149 (7.7) | 668 (34.3) | <.001 |
| Negative | 11 070 (75.3) | 607 (4.1) | 3031 (20.6) | 1571 (41.8) | 681 (18.1) | 1507 (40.1) | 14 659 (61.1) | 1065 (4.4) | 8255 (34.4) | |||
| Smoking | ||||||||||||
| Positive | 86 (48.9) | 25 (14.2) | 65 (36.9) | <.001 | 17 (28.8) | 7 (11.9) | 35 (59.3) | .01 | 92 (34.5) | 24 (9.0) | 151 (56.6) | <.001 |
| Negative | 11 699 (75.5) | 646 (4.2) | 3156 (20.4) | 1647 (41.9) | 710 (18.1) | 1571 (40.0) | 15 695 (61.2) | 1190 (4.6) | 8772 (34.2) | |||
| Social vulnerability, quartile | ||||||||||||
| Bottom | 205 (78.8) | 28 (10.8) | 27 (10.4) | <.001 | 34 (43.6) | 18 (23.1) | 26 (33.3) | .08 | 267 (61.2) | 44 (10.1) | 125 (28.7) | <.001 |
| Second | 4126 (71.6) | 282 (4.9) | 1351 (23.5) | 558 (40.5) | 258 (18.7) | 562 (40.8) | 5543 (59.4) | 534 (5.7) | 3252 (34.9) | |||
| Third | 565 (80.1) | 33 (4.7) | 107 (15.2) | 62 (39.2) | 40 (25.3) | 56 (35.4) | 671 (67.6) | 73 (7.4) | 249 (25.1) | |||
| Top | 11 752 (75.2) | 666 (4.3) | 3219 (20.6) | 1661 (41.7) | 713 (17.9) | 1606 (40.4) | 15 762 (60.9) | 1210 (4.7) | 8921 (34.5) | |||
| Hospital | ||||||||||||
| BWH | 5032 (83.4) | 359 (6.0) | 639 (10.6) | <.001 | 775 (53.1) | 253 (17.3) | 432 (29.6) | <.001 | 7684 (78.9) | 735 (7.6) | 1315 (13.5) | <.001 |
| CDH | 499 (89.4) | 25 (4.5) | 34 (6.1) | 68 (51.5) | 22 (16.7) | 42 (31.8) | 585 (66.5) | 46 (5.2) | 249 (28.3) | |||
| MGH | 3426 (91.2) | 223 (5.9) | 106 (2.8) | 354 (41.0) | 316 (36.6) | 194 (22.5) | 2814 (53.7) | 270 (5.1) | 2161 (41.2) | |||
| MVH | 1 (0.7) | 0 | 149 (99.3) | 0 | 0 | 36 (100.0) | 0 | 0 | 227 (100.0) | |||
| NCH | 88 (73.9) | 19 (16.0) | 12 (10.1) | 20 (69.0) | 3 (10.3) | 6 (20.7) | 171 (87.7) | 9 (4.6) | 15 (7.7) | |||
| NWH | 2110 (57.3) | 18 (0.5) | 1554 (42.2) | 302 (34.9) | 91 (10.5) | 473 (54.6) | 2993 (53.9) | 80 (1.4) | 2477 (44.6) | |||
| SLM | 590 (50.6) | 26 (2.2) | 549 (47.1) | 85 (28.8) | 32 (10.8) | 178 (60.3) | 696 (38.9) | 73 (4.1) | 1018 (57.0) | |||
| WDH | 38 (17.7) | 0 | 177 (82.3) | 60 (19.9) | 0 | 241 (80.1) | 840 (36.6) | 1 (<0.1) | 1456 (63.4) | |||
Abbreviations: BWH, Brigham and Women’s Hospital; CDH, Cooley Dickinson Hospital; GA, gestational age; MGH, Massachusetts General Hospital; MVH, Martha’s Vineyard Hospital; NA, not applicable; NCH, Nantucket Cottage Hospital; NWH, Newton-Wellesley Hospital; PNC, prenatal care; SLM, Salem Hospital; VBAC, vaginal birth after cesarean; WDH, Wentworth Douglass Hospital.
Differences in maternal characteristics across postpartum care access groups were calculated with χ2 tests. The prepandemic period was January to December 2019; early pandemic, January to March 2020; and late pandemic, April 2020 to November 2021. Social vulnerability was indicated by the social vulnerability index and was categorized into quartiles. Higher quartile indicates greater vulnerability.
Other racial groups include American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and multiple races.
Level Changes in Early and Late Pandemic Periods Compared With the Prepandemic Period by Race and Ethnicity
As reported in Table 3, compared with the last month in the prepandemic period (December 2019), the probability of canceling and not scheduling postpartum care increased immediately within each race and ethnicity group in the first month of the early pandemic period (January 2020). The probabilities of canceling increased by 8.1 percentage points (95% CI, 4.9-11.2 percentage points; P < .001) among Asian women, 5.2 percentage points (95% CI, 0.5-9.9 percentage points; P = .03) among Black women, 6.6 percentage points (95% CI, 4.3-8.9 percentage points; P < .001) among Hispanic women, and 4.8 percentage points (95% CI, 0.8 to 8.9 percentage points; P = .02) among White women; the probabilities of nonscheduling increased by 10.3 percentage points (95% CI, 7.7-13.0 percentage points; P < .001) among Asian women, 16.2 percentage points (95% CI, 11.3-21.1 percentage points; P < .001) among Black women, 15.0 percentage points (95% CI, 10.1-19.8 percentage points; P < .001) among Hispanic women, 16.2 percentage points (95% CI, 13.2-19.1 percentage points; P < .001) among White women, and 15.4 percentage points (95% CI, 7.0-23.8 percentage points; P < .001) among women of other racial groups. Yet, in the first month of the late pandemic period, the probability of not scheduling postpartum care dropped within each race and ethnicity group compared with the last month in prepandemic period, with a decrease of 2.7 percentage points (95% CI, −3.5 to −2.0 percentage points; P < .001) among Asian women, 1.3 percentage points (95% CI, −2.3 to −0.3 percentage points; P = .01) among Black women, 1.0 percentage points (95% CI, −1.6 to −0.3 percentage points; P = .002) among Hispanic women, 3.0 percentage points (95% CI, −3.3 to −2.8 percentage points; P < .001) among White women, and 2.5 percentage points (95% CI, −4.1 to −0.9 percentage points; P = .002) among women of other racial groups. Overall, during the late pandemic period, the probability of not scheduling postpartum care among Black women and Hispanic women increased more than among their White counterparts (Black women: AME, 1.1; 95% CI, 0.6-1.6; Hispanic women: AME, 1.3; 95% CI, 0.9-1.6).
Table 3. Average Marginal Effects of Cancelling or Nonscheduling Relative to Attending Postpartum Care Visits in Multinomial Logistic Regressiona.
| Characteristic | Canceled vs attended | Nonscheduled vs attended | ||
|---|---|---|---|---|
| Average marginal effect (95% CI) | P value | Average marginal effect (95% CI) | P value | |
| Race and ethnicity | ||||
| Asian | −1.2 (−2.3 to 0.0) | .05 | −1.1 (−2.1 to −0.1) | .03 |
| Black | 1.9 (−0.4 to 4.2) | .11 | 1.6 (0.2 to 3.0) | .02 |
| Hispanic | 1.9 (−0.2 to 4.0) | .07 | 3.7 (2.6 to 4.9) | <.001 |
| White | [Reference] | [Reference] | ||
| Otherb | 0.0 (−2.2 to 2.2) | .99 | −0.6 (−3.0 to 1.8) | .61 |
| Delivery month | 0.1 (0.0 to 0.2) | .06 | 0.7 (0.5 to 0.8) | <.001 |
| Time periodc | ||||
| Prepandemic | [Reference] | [Reference] | ||
| Early pandemic | 1.2 (−1.0 to 3.4) | .27 | 33.7 (27.8 to 39.5) | <.001 |
| Late pandemic | 0.4 (−0.4 to 1.2) | .34 | 22.2 (20.2 to 24.2) | <.001 |
| Level changes | ||||
| Early pandemic vs prepandemic | ||||
| Asian | 8.1 (4.9 to 11.2) | <.001 | 10.3 (7.7 to 13.0) | <.001 |
| Black | 5.2 (0.5 to 9.9) | .03 | 16.2 (11.3 to 21.1) | <.001 |
| Hispanic | 6.6 (4.3 to 8.9) | <.001 | 15.0 (10.1 to 19.8) | <.001 |
| White | 4.8 (0.8 to 8.9) | .02 | 16.2 (13.2 to 19.1) | <.001 |
| Otherb | 4.5 (−4.2 to 13.2) | .31 | 15.4 (7.0 to 23.8) | <.001 |
| Late pandemic vs prepandemic | ||||
| Asian | −0.1 (−0.4 to 0.1) | .33 | −2.7 (−3.5 to −2.0) | <.001 |
| Black | −0.1 (−1.0 to 0.7) | .79 | −1.3 (−2.3 to −0.3) | .01 |
| Hispanic | −0.3 (−1.1 to 0.4) | .40 | −1.0 (−1.6 to −0.3) | .002 |
| White | 0.0 (0.0 to 0.1) | .35 | −3.0 (−3.3 to −2.8) | <.001 |
| Otherb | 0.0 (−0.2 to 0.3) | .91 | −2.5 (−4.1 to −0.9) | .002 |
| Changes in monthly trend | ||||
| Prepandemic | ||||
| White | [Reference] | [Reference] | ||
| Black | 0.1 (−0.2 to 0.5) | .47 | −0.3 (−1.0 to 0.4) | .40 |
| Hispanic | 0.2 (−0.1 to 0.4) | .24 | −0.3 (−0.7 to 0.2) | .22 |
| Asian | −0.1 (−0.2 to 0.1) | .54 | 0.0 (−0.5 to 0.4) | .84 |
| Otherb | −0.1 (−0.5 to 0.3) | .75 | 0.0 (−0.9 to 0.9) | .99 |
| Early-pandemic | ||||
| Asian | −1.8 (−7.0 to 3.4) | .49 | 6.7 (−2.2 to 15.6) | .14 |
| Black | −1.1 (−5.7 to 3.5) | .64 | −4.4 (−17.9 to 9.2) | .53 |
| Hispanic | 2.7 (−1.0 to 6.3) | .15 | −12.0 (−20.5 to −3.5) | .006 |
| White | [Reference] | [Reference] | ||
| Otherb | −1.0 (−11.5 to 9.5) | .85 | −2.3 (−24.5 to 20.0) | .84 |
| Late pandemic | ||||
| Black | 0.1 (−0.1 to 0.2) | .21 | 1.1 (0.6 to 1.6) | <.001 |
| Hispanic | 0.03 (−0.1 to 0.1) | .56 | 1.3 (0.9 to 1.6) | <.001 |
| Asian | −0.1 (−0.2 to 0.0) | .17 | 0.1 (−0.3 to 0.6) | .54 |
| White | [Reference] | [Reference] | ||
| Otherb | −0.1 (−0.2 to 0.1) | .42 | 0.4 (−0.2 to 1.0) | .23 |
Models controlled for maternal demographic and clinical characteristics, including age, marital status, gestational age at delivery, delivery mode, severe morbidity, diabetes, hypertension, depression, smoking, prenatal care attendance, county-level social vulnerability, and delivery hospital. The full model with covariates can be found in the eTable in the Supplement.
Other racial groups include American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, and multiple races.
Prepandemic period was January to December 2019; early pandemic period, January to March 2020; late pandemic period, April 2020 to November 2021.
Racial and Ethnic Disparity in Monthly Trends of Postpartum Care Access
During the prepandemic period (January to December 2019), White women experienced a slightly increasing trend in not scheduling postpartum care; with every 1 month, the probability of not scheduling postpartum care among White women increased by 0.7 percentage points (95% CI, 0.5-0.8 percentage points; P < .001) (Figure 2). No differential trend of postpartum care access during the prepandemic and early pandemic periods was found across racial and ethnic groups.
Figure 2. Adjusted Monthly Trends of Postpartum Care Access Probabilities From January 2019 to November 2021.
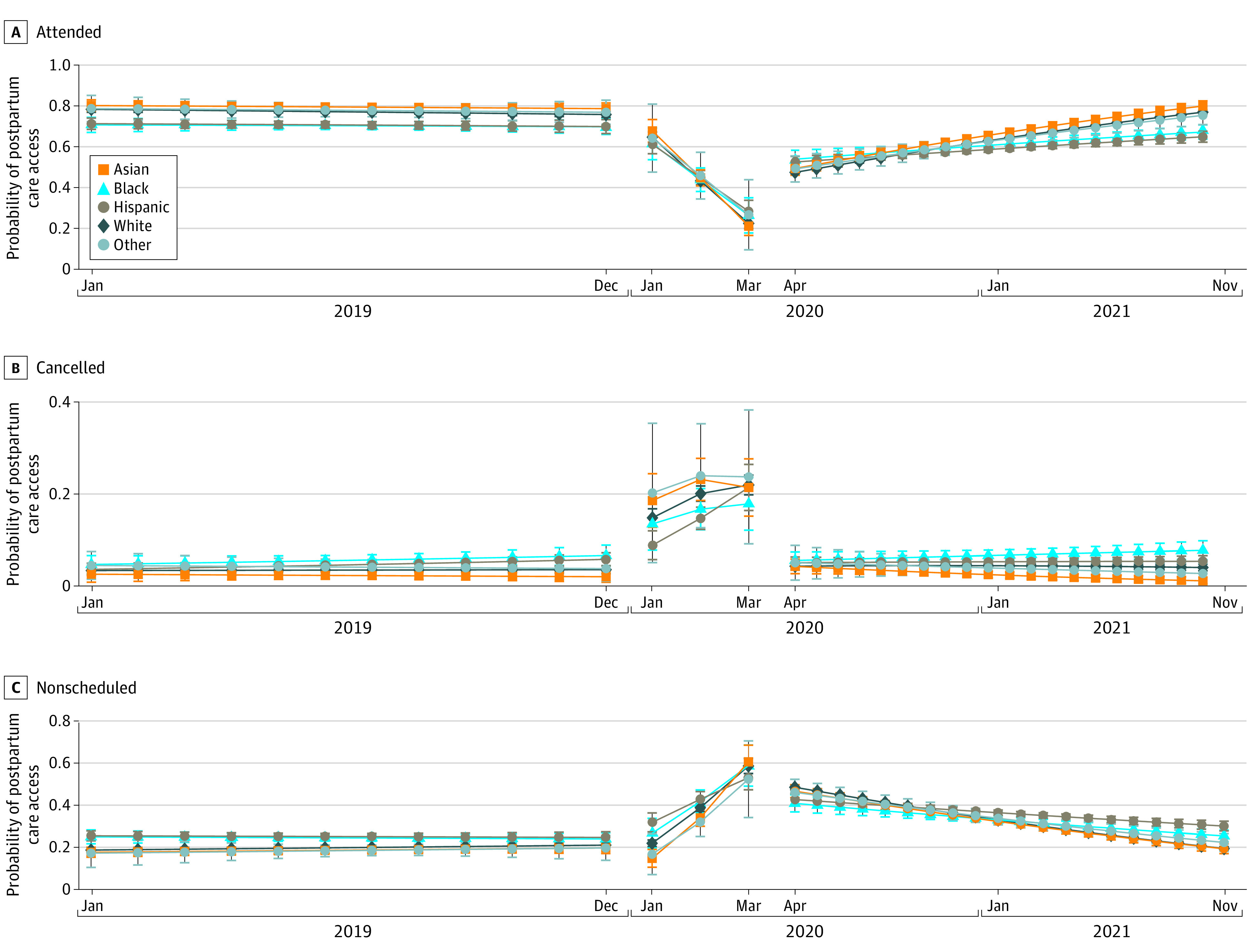
Probabilistic margins of the probabilities of attending, canceling, and nonscheduling postpartum care by delivery month in terms of pandemic phases, estimated using a multinomial logistic model with adjustment for age, marital status, gestational age at delivery, delivery mode, severe morbidity, diabetes, hypertension, depression, smoking, prenatal care attendance, county-level social vulnerability, and delivery hospital, with clustering at the residential zip code level. Whiskers indicate the 95% CIs.
During the late pandemic period, compared with the monthly trends for White women, rates of not scheduling postpartum care among Black women increased more rapidly, with 1.1 percentage (95% CI, 0.6-1.6; P < .001) per month. Among Hispanic women, the rate increased 1.3 percentage more rapidly (95% CI, 0.9-1.6; P < .001) than White women.
Discussion
This exploratory study quantified the change in postpartum care access during 3 phases of the COVID-19 pandemic. In the prepandemic period (January to December 2019), the overall postpartum care attendance rate was 75.2%, while it dropped to 41.7% during the early pandemic period (January to March 2020) and rebounded back to 60.9% in the late pandemic period (April 2020 to November 2021). All participating women experienced immediate increases in the probability of postpartum care cancelation or nonscheduling in the early pandemic. Black and Hispanic women experienced a slower reduction in nonscheduling in the late pandemic compared with White women. Higher canceling or nonscheduling rates were also found among women who were younger (18-24 years), were single, had a preterm birth, smoked, and had a delayed prenatal care attendance, compared with older, married, nonsmoking women who initiated prenatal care during the first 12 gestational weeks.
Postpartum care access has been disrupted during the COVID-19 pandemic despite new obstetric precautions being adopted to maintain maternal health care services.42 Such disruption is of particular concern given the vital role of access to care on a number of maternal and neonatal health outcomes.43 A few studies have documented similar findings to the current study.8,42 A pre-post study revealed a 7.8% decrease in postpartum care attendance between April 2019 and April 2020.8 A cross-sectional survey study found 62% of pregnant and postpartum women reported health care disruptions due to COVID-19 between May and June 2020.42 Of these participants, 29% stated that at least 1 appointment had been canceled42 as a result of intentional avoidance of health care facilities,44 the feeling of being unsupported and isolated,45 concerns around childcare issues, and availability of personal protective equipment.42 Extending beyond a few months during the pandemic, the current study found similar postpartum care disruption during the early pandemic but a moderate rebounding trend in postpartum care attendance during the late pandemic.
Although the overall rates of postpartum care attendance, canceling, and nonscheduling have been gradually recovering toward the prepandemic level, adaptation to the COVID-19 pandemic has not been universally equal. The canceling and nonscheduling rates of postpartum care visits decreased more slowly in Black and Hispanic women compared with White women, highlighting the racial and ethnic disparity in adaptation to the pandemic. The delay and absence of postpartum care visits have evidently hindered the prevention against maternal mortality, emergency department visits, the control of childbirth complications, and postpartum depression,2,11,12 which were consistently more likely to happen among Black and Hispanic individuals even prior to the pandemic.16,17,18,19,20 Little attention has been paid to how intersectional vulnerabilities heighten the risks for serious adverse maternal outcomes, when the populations that suffer long-standing structural inequities are also disproportionately affected by the COVID-19 pandemic.46 The current result showed that Black and Hispanic women not only had the highest canceling and nonscheduling rates before the pandemic but also acclimated to the pandemic more slowly than other racial and ethnic groups. These racial and ethnic disparities in postpartum care both before and after the onset of the pandemic raise concerns about the potential increases in disparities in postpartum care–associated maternal and infant outcomes because of the pandemic.
A lack of access to postpartum care was disproportionately prevalent among vulnerable populations, signaling amplified challenges in health care access during the COVID-19 pandemic among the most in need.12 This study found that women who were younger than 24 years old, single, multipara, and smoking and who had a preterm delivery were more likely to cancel or not schedule postpartum care visits than their counterparts. In line with previous studies, younger age was associated with postpartum care nonattendance, and it was a particular concern for adolescents.12,47 Single or divorced mothers are also well documented to have a higher risk of postpartum care nonattendance compared with married mothers.48 Marital status was considered a proxy for spouse support. Encouragement from spouses and/or family members could facilitate women’s ability and motivation to schedule postpartum care visits.48 This study highlighted higher cancelation and nonscheduling rates among mothers who smoked and had a preterm birth, in line with previous studies in which low postpartum care attendance was attributed to pregnancy-related factors such as poor birth outcomes.48,49,50,51 Efforts aiming to reduce barriers to care and encourage health-seeking behavior are greatly needed to mitigate the negative effects of postpartum care nonattendance among these vulnerable women.
Limitations
This study has limitations. First, the EHR data were from 8 hospitals in a large health system in Massachusetts. Postpartum care data for women who returned to other care settings were unavailable to us, potentially hindering our ability to differentiate attending postpartum care from nonscheduled postpartum care. Nevertheless, our study revealed different postpartum care access status by maternal race, ethnicity, and SES during the pandemic. Second, insurance information was unavailable. It is well documented that women with Medicaid insurance had a higher risk (37%-55%) of not returning for postpartum care compared with women using private insurance (3%).47,52 While higher SES is positively associated with private insurance coverage,53 we controlled for county-level income, education, broadband access, and racial residential segregation as the proxies. Despite these limitations, the current study contributes to the extant literature by using longitudinal EHR data in a 24-month timeframe, capturing the trend of postpartum care access before, during, and after the onset of the COVID-19 pandemic. In this racially diverse sample, our results emphasized that racial and ethnic disparities in perinatal care might have been exacerbated by the pandemic. Although overall postpartum care access has gradually rebounded toward the prepandemic level, the attendance rate was still lower than before the pandemic, with Black and Hispanic women lagging behind. Initiatives have been launched to raise awareness and to recommend adaptations during COVID-19 by ACOG,54 the Royal College of Obstetrician and Gynecologists,55 and WHO.56 Yet, some adaptations (eg, temporary birth centers, help hotlines, virtual consultations) might better serve low-risk mothers57 than those who require high-acuity care. Our study highlighted the need for greater system-level support from health care professionals and organizations to ensure postpartum care access for vulnerable women and ensure effective adaptation to the pandemic for all.
Conclusions
This cohort data study highlights exacerbating racial disparities in postpartum care access immediately during and following the onset of the COVID-19 pandemic in early 2020. Of all racial and ethnic groups, Black women showed the slowest reduction in canceling rate, and Hispanic women had the slowest reduction in nonscheduling rate in late pandemic period, indicating slower adaptation to the pandemic. Understanding barriers and facilitators for postpartum care access among Black and Hispanic women is necessary to promote equitable postpartum care access for women most vulnerable to adverse outcomes. Maternal health practitioners and policy makers involved in pandemic adaptation should pay closer attention to avoid potential inequities and the unintentional consequences for marginalized populations.
eTable. Full Model of Multinomial Logistic Regression With Covariates
References
- 1.Shaw E, Levitt C, Wong S, Kaczorowski J; McMaster University Postpartum Research Group . Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. 2006;33(3):210-220. doi: 10.1111/j.1523-536X.2006.00106.x [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO Recommendations on Postnatal Care of the Mother and Newborn. World Health Organization; 2014. [PubMed] [Google Scholar]
- 3.Bodnar-Deren S, Klipstein K, Fersh M, Shemesh E, Howell EA. Suicidal ideation during the postpartum period. J Womens Health (Larchmt). 2016;25(12):1219-1224. doi: 10.1089/jwh.2015.5346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burlingame J, Horiuchi B, Ohana P, Onaka A, Sauvage LM. The contribution of heart disease to pregnancy-related mortality according to the pregnancy mortality surveillance system. J Perinatol. 2012;32(3):163-169. doi: 10.1038/jp.2011.74 [DOI] [PubMed] [Google Scholar]
- 5.McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;132(3):784-785. doi: 10.1097/AOG.0000000000002849 [DOI] [PubMed] [Google Scholar]
- 6.Pfitzer A, Lathrop E, Bodenheimer A, et al. Opportunities and challenges of delivering postabortion care and postpartum family planning during the COVID-19 pandemic. Glob Health Sci Pract. 2020;8(3):335-343. doi: 10.9745/GHSP-D-20-00263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osanan GC, Vidarte MFE, Ludmir J. Do not forget our pregnant women during the COVID-19 pandemic. Women Health. 2020;60(9):959-962. doi: 10.1080/03630242.2020.1789264 [DOI] [PubMed] [Google Scholar]
- 8.Sangtani A, Clifford C, Hesson A, Greco P, Stout MJ, Langen ES. 702 Postpartum depression screening during the COVID-19 pandemic. Am J Obstet Gynecol. 2021;224(2):S440. doi: 10.1016/j.ajog.2020.12.725 [DOI] [Google Scholar]
- 9.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5-12. doi: 10.1097/AOG.0000000000000564 [DOI] [PubMed] [Google Scholar]
- 10.Kleppel L, Suplee PD, Stuebe AM, Bingham D. National initiatives to improve systems for postpartum care. Matern Child Health J. 2016;20(1)(suppl 1):66-70. doi: 10.1007/s10995-016-2171-1 [DOI] [PubMed] [Google Scholar]
- 11.Brousseau EC, Danilack V, Cai F, Matteson KA. Emergency department visits for postpartum complications. J Womens Health (Larchmt). 2018;27(3):253-257. doi: 10.1089/jwh.2016.6309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilcox A, Levi EE, Garrett JM. Predictors of non-attendance to the postpartum follow-up visit. Matern Child Health J. 2016;20(1)(suppl 1):22-27. doi: 10.1007/s10995-016-2184-9 [DOI] [PubMed] [Google Scholar]
- 13.Grobman WA, Parker CB, Willinger M, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b) Network* . Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol. 2018;131(2):328-335. doi: 10.1097/AOG.0000000000002441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68(18):423-429. doi: 10.15585/mmwr.mm6818e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moaddab A, Dildy GA, Brown HL, et al. Health care disparity and state-specific pregnancy-related mortality in the United States, 2005–2014. Obstet Gynecol. 2016;128(4):869-875. doi: 10.1097/AOG.0000000000001628 [DOI] [PubMed] [Google Scholar]
- 16.Callaghan WM. Overview of Maternal Mortality in the United States. Elsevier; 2012:2-6. [DOI] [PubMed] [Google Scholar]
- 17.Howell EA, Egorova NN, Janevic T, et al. Race and ethnicity, medical insurance, and within-hospital severe maternal morbidity disparities. Obstet Gynecol. 2020;135(2):285-293. doi: 10.1097/AOG.0000000000003667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu CH, Tronick E. Rates and predictors of postpartum depression by race and ethnicity: results from the 2004 to 2007 New York City PRAMS survey (Pregnancy Risk Assessment Monitoring System). Matern Child Health J. 2013;17(9):1599-1610. doi: 10.1007/s10995-012-1171-z [DOI] [PubMed] [Google Scholar]
- 19.Melville JL, Gavin A, Guo Y, Fan M-Y, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064-1070. doi: 10.1097/AOG.0b013e3181f60b0a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital-based care associated with postpartum depression. J Racial Ethn Health Disparities. 2021;8(1):220-229. doi: 10.1007/s40615-020-00774-y [DOI] [PubMed] [Google Scholar]
- 21.Van den Bergh BRH, van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2020;117:26-64. doi: 10.1016/j.neubiorev.2017.07.003 [DOI] [PubMed] [Google Scholar]
- 22.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141-148. doi: 10.1097/YCO.0b013e3283503680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiel de Bocanegra H, Braughton M, Bradsberry M, Howell M, Logan J, Schwarz EB. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47.e1-47.e7. doi: 10.1016/j.ajog.2017.02.040 [DOI] [PubMed] [Google Scholar]
- 24.HealthyPeople.gov . Mothers attending a postpartum care visit (percent). Accessed August 28, 2021. https://www.healthypeople.gov/2020/data-search/Search-the-Data?objid=4855
- 25.Zittel-Palamara K, Rockmaker JR, Schwabel KM, Weinstein WL, Thompson SJ. Desired assistance versus care received for postpartum depression: access to care differences by race. Arch Womens Ment Health. 2008;11(2):81-92. doi: 10.1007/s00737-008-0001-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769-775. doi: 10.15585/mmwr.mm6925a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.United Nations . Policy brief: the impact of COVID-19 on women. April 9, 2020. Accessed May 3, 2022. https://www.un.org/sexualviolenceinconflict/wp-content/uploads/2020/06/report/policy-brief-the-impact-of-covid-19-on-women/policy-brief-the-impact-of-covid-19-on-women-en-1.pdf
- 28.Mizrak Sahin B, Kabakci EN. The experiences of pregnant women during the COVID-19 pandemic in Turkey: a qualitative study. Women Birth. 2021;34(2):162-169. doi: 10.1016/j.wombi.2020.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gausman J, Langer A. Sex and gender disparities in the COVID-19 pandemic. J Womens Health (Larchmt). 2020;29(4):465-466. doi: 10.1089/jwh.2020.8472 [DOI] [PubMed] [Google Scholar]
- 30.Diamond RM, Brown KS, Miranda J. Impact of COVID-19 on the perinatal period through a biopsychosocial systemic framework. Contemp Fam Ther. 2020;42(3):205-216. doi: 10.1007/s10591-020-09544-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gur RE, White LK, Waller R, et al. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res. 2020;293:113475. doi: 10.1016/j.psychres.2020.113475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yusuf KK, Dongarwar D, Ibrahimi S, Ikedionwu C, Maiyegun SO, Salihu HM. Expected surge in maternal mortality and severe morbidity among African-Americans in the era of COVID-19 pandemic. Int J MCH AIDS. 2020;9(3):386-389. doi: 10.21106/ijma.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oskovi-Kaplan ZA, Buyuk GN, Ozgu-Erdinc AS, Keskin HL, Ozbas A, Moraloglu Tekin O. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q. 2021;92(2):675-682. doi: 10.1007/s11126-020-09843-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.United States Census Bureau . Racial and ethnic residential segregation in the United States: 1980-2000. Accessed September 9, 2021. https://www.census.gov/library/publications/2002/dec/censr-3.html
- 35.Agency for Toxic Substances and Disease Registry . CDC/ATSDR Social Vulnerability Index. Accessed April 10, 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- 36.World Health Organization . Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). January 30, 2020. Accessed May 3, 2022. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 37.Brigham and Women’s Hospital . MGB Center for COVID Innovation. Accessed August 24, 2021. https://www.brighamandwomens.org/covid-19/center-for-covid-innovation
- 38.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: a systematic review of studies from 1998-2011. Psychosoc Med. 2012;9:Doc11-Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The American College of Obstetricians and Gynecologists . Guidelines for prenatal care. Accessed April 5, 2022. https://www.acog.org/clinical-information/physician-faqs/-/media/3a22e153b67446a6b31fb051e469187c.ashx
- 40.Centers for Disease Control and Prevention . How does CDC identify severe maternal morbidity? Accessed April 10, 2021. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm
- 41.US Centers for Disease Control and Prevention . COVID-19 case surveillance public data access, summary, and limitations. Accessed April 15, 2022. https://data.cdc.gov/Case-Surveillance/United-States-COVID-19-Cases-and-Deaths-by-State-o/9mfq-cb36
- 42.Brislane Á, Larkin F, Jones H, Davenport MH. Access to and quality of healthcare for pregnant and postpartum women during the COVID-19 pandemic. Front Glob Womens Health. Published online February 10, 2021. doi: 10.3389/fgwh.2021.628625 [DOI] [PMC free article] [PubMed]
- 43.Nicoloro-SantaBarbara J, Rosenthal L, Auerbach MV, Kocis C, Busso C, Lobel M. Patient-provider communication, maternal anxiety, and self-care in pregnancy. Soc Sci Med. 2017;190:133-140. doi: 10.1016/j.socscimed.2017.08.011 [DOI] [PubMed] [Google Scholar]
- 44.Levene R, Fein DM, Silver EJ, Joels JR, Khine H. The ongoing impact of COVID-19 on asthma and pediatric emergency health-seeking behavior in the Bronx, an epicenter. Am J Emerg Med. 2021;43:109-114. doi: 10.1016/j.ajem.2021.01.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DeYoung SE, Mangum M. Pregnancy, birthing, and postpartum experiences during COVID-19 in the United States. Front Sociol. 2021;6:611212. doi: 10.3389/fsoc.2021.611212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ebor MT, Loeb TB, Trejo L. Social workers must address intersecting vulnerabilities among noninstitutionalized, black, Latinx, and older adults of color during the COVID-19 pandemic. J Gerontol Soc Work. 2020;63(6-7):585-588. doi: 10.1080/01634372.2020.1779161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baldwin MK, Hart KD, Rodriguez MI. Predictors for follow-up among postpartum patients enrolled in a clinical trial. Contraception. 2018;98(3):228-231. doi: 10.1016/j.contraception.2018.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers. J Pregnancy. 2014;2014:530769-530769. doi: 10.1155/2014/530769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weir S, Posner HE, Zhang J, Willis G, Baxter JD, Clark RE. Predictors of prenatal and postpartum care adequacy in a Medicaid managed care population. Womens Health Issues. 2011;21(4):277-285. doi: 10.1016/j.whi.2011.03.001 [DOI] [PubMed] [Google Scholar]
- 50.Nkwabong E, Ilue EE, Bisong CE. Factors associated with poor attendance at the postpartum clinic six weeks after delivery in Cameroon. Int J Gynaecol Obstet. 2015;129(3):248-250. doi: 10.1016/j.ijgo.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 51.Masho SW, Cha S, Karjane N, et al. Correlates of postpartum visits among Medicaid recipients: an analysis using claims data from a managed care organization. J Womens Health (Larchmt). 2018;27(6):836-843. doi: 10.1089/jwh.2016.6137 [DOI] [PubMed] [Google Scholar]
- 52.Simmons KB, Edelman AB, Li H, Yanit KE, Jensen JT. Personalized contraceptive assistance and uptake of long-acting, reversible contraceptives by postpartum women: a randomized, controlled trial. Contraception. 2013;88(1):45-51. doi: 10.1016/j.contraception.2012.10.037 [DOI] [PubMed] [Google Scholar]
- 53.Peiris V, Singh TP, Tworetzky W, Chong EC, Gauvreau K, Brown DW. Association of socioeconomic position and medical insurance with fetal diagnosis of critical congenital heart disease. Circ Cardiovasc Qual Outcomes. 2009;2(4):354-360. doi: 10.1161/CIRCOUTCOMES.108.802868 [DOI] [PubMed] [Google Scholar]
- 54.American College of Obstetricians & Gynaecologists . Coronavirus (COVID-19), pregnancy, and breastfeeding: a message for patients. Accessed August 19, 2021. https://www.acog.org/womens-health/faqs/coronavirus-covid-19-pregnancy-and-breastfeeding
- 55.Royal College of Obstetricians & Gynaecologists . Coronavirus infection and pregnancy. Accessed August 19, 2021. https://www.rcog.org.uk/globalassets/documents/guidelines/2020-07-24-coronavirus-covid-19-infection-in-pregnancy.pdf
- 56.World Health Organization . Maternal, newborn, child and adolescent health, and ageing—COVID-19: resources for pregnancy, childbirth, postnatal care. Accessed August 19, 2021. https://www.who.int/teams/maternal-newborn-child-adolescent-health-and-ageing/covid-19/mca-and-covid-19-pregnancy-childbirth-postnatal-care
- 57.Pant S, Koirala S, Subedi M. Access to maternal health services during COVID-19. Europasian Journal of Medical Sciences. 2020;2:46-50. doi: 10.46405/ejms.v2i2.110 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Full Model of Multinomial Logistic Regression With Covariates


