Abstract
Cancers represent a significant cause of morbidity and mortality worldwide. They also impose a large economic burden on patients, their families, and health insurance systems. Notably, cancers and the adverse reactions to their therapeutic options, chemotherapy and radiotherapy, dramatically affect the quality of life of afflicted patients. Therefore, developing approaches to manage chemotherapy- and radiotherapy-induced adverse reactions gained greater attention in recent years. Glycyrrhiza glabra (licorice), a perennial plant that is one of the most frequently used herbs in traditional Chinese medicine, has been heavily investigated in relation to cancer therapy. Licorice/licorice-related regimes, used in combination with chemotherapy, may improve the adverse effects of chemotherapy. However, there is little awareness of licorice-containing herbs alleviating reactions to radiotherapy and chemotherapy, or to other induced adverse reactions in cancer treatment. We aimed to provide a descriptive review, and to emphasize the possibility that licorice-related medicines could be used as an adjuvant regimen with chemotherapy to improve quality of life (QoL) and to reduce side effects, thus, improving compliance with chemotherapy. The experimental method involved searching different databases, including PubMed, the Cochrane Library, and Wang Fang database, as of May 2022, to identify any relevant studies. Despite a lack of high-quality and large-scale randomized controlled trials, we still discovered the potential benefits of licorice-containing herbs from published clinical studies. These studies find that licorice-containing herbs, and their active ingredients, reduce the adverse reactions caused by chemotherapy and radiotherapy, and improve the QoL of patients. This comprehensive review will serve as a cornerstone to encourage more scientists to evaluate and develop effective Traditional Chinese medicine prescriptions to improve the side effects of chemotherapy and radiation therapy.
Keywords: licorice, cancers, adverse effects, chemotherapy, radiotherapy
1. Introduction
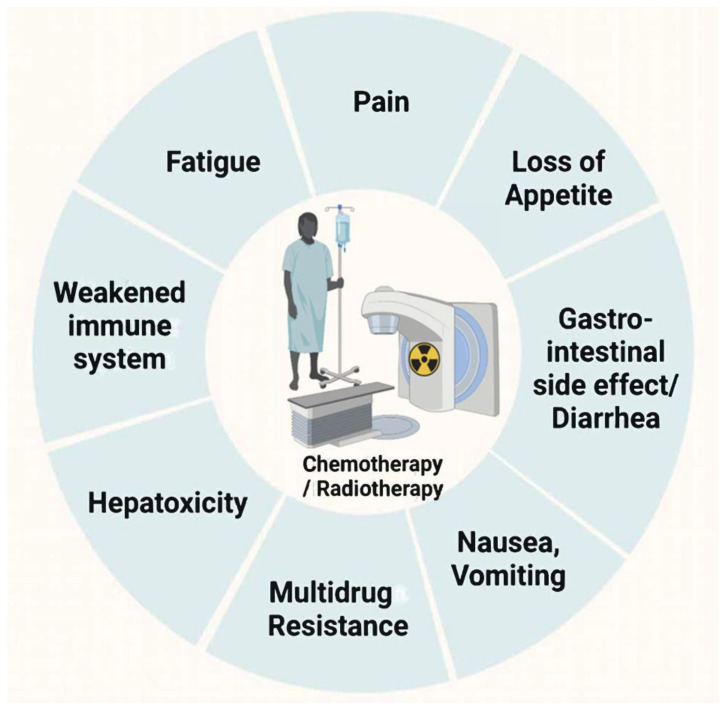
Cancer is one of the leading causes of premature death and a significant barrier to increasing life expectancy in almost every country in the world. In 2020, 19.,3 million new cancer cases were estimated, as well as almost 10 million cancer deaths [1]. Traditionally, standard cancer therapies include surgery, cytotoxic chemotherapy, and radiation therapy. Nevertheless, oncology treatment regimens, especially for chemotherapy/radiotherapy, may lead to other complications, such as fatigue (50~90%), chronic pain (50~70%), oral mucositis, anorexia (~85%), gastrointestinal toxicity, hepatotoxicity, nephrotoxicity, insomnia (30~60%), edema, depression/anxiety (24%/24%), or constipation (30~80%) [2,3,4,5]. These complications may decrease therapeutic compliance, lead to treatment interruption, or reduce the quality of life (QoL) (Figure 1) [6]. Nowadays, pharmacologic antiemetic therapy has become a major supportive care initiative [7]; however, its therapeutic effects remain extremely limited in improving vomiting and other complications. It is, therefore, important to develop more effective therapeutic strategies, or adjuvant treatments, to synergistically enhance the efficacy and reduce the toxicity of chemotherapy and radiotherapy.
Figure 1.
Side effects of chemotherapy and radiotherapy.
After undergoing chemotherapy/radiation, quality of life (QoL) is impacted by several symptoms: vomiting/nausea, diarrhea/constipation, and immunodeficiency.
The chemical compounds of chemotherapy, largely purified from plants, are important for cancer treatment [8]. Cancer relapses, one of the major causes of death in cancer, occur because cancers develop resistance to classical chemotherapeutic agents, or even novel targeted drugs, over time. Therefore, it is essential to discover more therapeutic agents [9]. Moreover, some natural products also possess the ability to reduce the complications induced by chemotherapy and radiotherapy.
Recent studies demonstrate that licorice, as well as licorice-purified compounds, has the potential to abrogate the onset and progression of different malignancy cancers, both in vitro and in vivo [10,11,12,13,14,15]. Moreover, previous studies also suggest that licorice is a beneficial medicine plant used as a cure for nausea and vomiting [16]. In contrast, consuming excessive quantities of licorice is also associated with hypertension, hypokalemia, cardiac arrhythmias, and metabolic alkalosis. These effects may be due to the alternation of the renin–angiotensin–aldosterone system [17,18]. However, the present review aims to make an overview of the licorice-containing herbs that have the potential to alleviate the adverse reactions induced by radiotherapy and chemotherapy.
2. Utility of Licorice-Containing Herbs in Cancer
2.1. Licorice Introduction
Licorice belongs to the genus Glycyrrhiza, and radix glycyrrhizae (RG) is the dried roots and rhizomes of licorice. Licorice is commonly used as a natural sweetener and in herbal medicine. It mainly acts as a supplement in Western countries, for products such as herbal teas, soft drinks, and tobacco products. However, it is regarded as a medicine in Asia. Licorice is utilized to relieve pain, phlegm, spasms, cough, and dyspnea. The abundant active ingredients in licorice demonstrate efficacy in many different biological and physiological functions. To date, more than 300 bioactive compounds have been identified in licorice, including ~100 types of triterpenoid saponins and sapogenins, and ~300 kinds of phenolic compounds [17]. However, it has been found that the cultivated geographical area, the state of plant maturity, environmental conditions (including the pH of the soil, temperature, and weather), harvesting, and processing all affect the content of the bioactive compounds in licorice [18]. For example, the triterpenoid saponins in licorice, especially glycyrrhizic acid (GL; approximately 1.84% to 9.82% of licorice, depending on the sources and methods of extraction), are the major constituents and bioactive ingredients of licorice [19,20,21]. Flavonoids (approximately 1.78% to 4.82% of licorice, depending on the sources and methods of extraction) are the other main bioactive compound found in licorice, including isoliquiritigenin (ISL), isoliquiritin, and liquiritigenin, etc. [19,22]. In the 2010 edition of the Chinese Pharmacopoeia, GL and isoliquiritigenin were selected as the biomarkers for licorice, and it is stated that their content should exceed 2% and 0.5%, respectively [23]. Interestingly, we found that these two major compounds (GL and ISL) appear in many studies related to chemotherapy, which will be discussed further in a later section.
Licorice can be simply categorized into three Glycyrrhiza species: Glycyrrhiza uralensis Fisch., Glycyrrhiza glabra L., and Glycyrrhiza inflata Bat. [24]. In China, G. uralensis, G. glabra, and G. inflata are considered equivalent, and are combined and utilized as licorice without discrimination in the 2015 edition of the Chinese Pharmacopoeia. However, the morphological characteristics of the three Glycyrrhiza species show differences in the root, rhizome, seed, fruit, and inflorescence, as well as in the leaf and stem height. It is difficult to identify these licorice species accurately based only on their root or rhizome morphology [25].
There are significant differences between the species, which were established by the analytical methods of numerous studies aimed at separating and quantifying the active ingredients in licorice samples. These studies report that different licorice species have species-specific markers (Table 1); for example, the content of major flavonoids (liquiritin, liquiritigenin, and isoliquiritin) in G. uralensis is higher than that in G. glabra, and glycycoumarin only exists in G. uralensis [26,27,28,29,30]. Glycyrrhizin, 50 times sweeter than sugar and especially suitable for children, is evenly distributed in the three species [29]. The amount of isoliquiritigenin (2′,4′,4-trihydroxychalcone, ISL), one of the major bioactive compounds in licorice, is higher in G. uralensis than in G. glabra and G. inflata. [31,32].
Table 1.
Most common Glycyrrhiza species used as medicine.
| Glycyrrhiza Species | Region | Specific Content | Ref |
|---|---|---|---|
| Glycyrrhiza uralensis (Glycyrrhiza radix) | China Northeastern Far east Russia |
Owning the highest content of flavonoids (liquiritin, liquiritigenin, and isoliquiritin). Glycycoumarin only represented in G. uralensis. |
[26,27,28,29,30,43] |
| Isotrifloliol, licoricone, neoglycyrol, glycyrin, and licorisoflavan A in G. uralensis are higher. | [26] | ||
| Glyinflanin D/G and licoflavone B are absent. | [44] | ||
| Glycyrrhiza glabra | Italy Spain China Russia Iran Central Asia |
Owning the highest content of 18α-glycyrrhizic acid and 18β-glycyrrhizic acid. | [45] |
| Higher content of saponins–licorice saponin K2/H2, licorice saponin B2, and licorice saponin G2/yunganoside K2. Quercetin absent in G. glabra. |
[44,46,47] | ||
| The highest content of apiosides (liquiritin apioside, isoliquiritin apioside, licuraside). | [30] | ||
| Abundant 8-cyclized isoprenyl isoflavanes (e.g., glabridin and 4′-O-methylglabridin). | [29] | ||
| Polysaccharide content in G. glabra is the highest. | [48,49] | ||
| Glycyrrhiza | China, Asia | Highest content of triterpene saponins. | [25,29] |
| inflata | Chalcone derivatives such as licochalcone (A, B, C, E), kanzonol C, and echinatin in G. inflata are higher. | [29,44,50] | |
| The content of quercetin is higher than that in G. uralensis. | [44,46,47] | ||
| Highest content of prenylated chalcones. | [44] |
2.2. Chemopreventive Activities of Licorice
Licorice and its derivatives exert anti-inflammatory and antioxidant effects, suggesting their potential as chemopreventive or therapeutic agents. For example, licorice can be used for reducing inflammation and allergic responses, as well as preventing liver damage [24,33,34]. Licorice extract also acts as a moderate hypocholesterolemic nutrient, and a potent antioxidant agent, to prevent cardiovascular disease [35]. Clinical data suggest that licorice, or its bioactive components, prevent dyspepsia and hyperlipidemia [36,37]. When taken concurrently with a glycyrrhizin-containing product, licorice is shown to afford hepatoprotection during alcohol consumption [38]. Three randomized clinical trials claim that Glycyrrhiza acts as a mucoadhesive film, improving oral mucositis during radiotherapy [39,40,41]. Moreover, preoperative gargling with a licorice solution reduces postoperative sore throat, thus, revealing its analgesic properties [42]. The clinical trials of licorice are summarized in Table 2.
Table 2.
Licorice and its components applied in chemopreventive clinical trials.
| Name | Disease/Disorder | Dose/Duration | Trial | Location/ Identifier No. |
Ref | |||
|---|---|---|---|---|---|---|---|---|
| Patient (n) | Experiment Group |
Control Group |
Outcome | |||||
| Extract of G. glabra | Radiotherapy Head or neck |
Oral 100 c.c/Bid 2 weeks |
n = 37 | Extract of G. glabra | Placebo (radiotherapy) |
Prevent oral mucositis | IRCT201203012464N4 Iran Tehran University of medical science |
[39] |
|
G. glabra (yashtimadhu) |
Radiotherapy Head or neck |
Oral 5 g/Bid 6 weeks |
n = 127 | G. glabra | Placebo (radiotherapy) |
Prevent oral mucositis | Himalayan Institute of Medical Sciences, Dehradun, India | [40] |
| Licorice | Radiotherapy Head or neck |
Mouth wash |
n = 60 | Licorice mucoadhesive film | Placebo mucoadhesive film | Prevent oral mucositis | Isfahan University of Medical Sciences, Isfahan, Iran | [41] |
| Licorice extract |
Randomized Double-blind |
Oral 1 g/Tid |
n = 236 | +licorice extract |
Sugar water | Pain relieving | NCT02968823 | [42] |
| Licorice | Dyspepsia | 380 mg/Bid 4 weeks |
n = 120 | +licorice | N.A. | Improved H. pylori eradication | IRCT2014061718124N | [36,37] |
| Glycyrrhizin | Alcohol consuming | Oral 0.1–0.3% 12 days |
n = 24 | +Licorice | Placebo (alcohol) |
Hepato-protection | N.A. | [38] |
2.3. Licorice Literature Search Strategy
2.3.1. Review Purpose
Licorice/licorice-related medicine, combined with chemotherapy, may potentially reduce the side effects of chemotherapeutics, such as mucositis, anemia, anorexia, and fatigue, and may offer cheaper and safer options than current conventional medication. In this review, we mainly focused on the use of licorice-related medicines, including licorice itself, licorice-mixed ingredients (prescriptions/Kampo), and purified compounds, in an attempt to summarize the current knowledge regarding licorice application in chemotherapy.
Our review mainly targets the questions below:
Does licorice/licorice-related medicine/purified compound combined with chemotherapy improve the adverse effects of chemotherapy?
What type of adverse effects are suitable for treatment with licorice-related medicine?
Do they have recorded adverse effects?
Does the additional application the improve quality of life (QoL) among those receiving conventional chemotherapy?
2.3.2. Search Database
The following databases were searched: PubMed, the Cochrane database, and Wang Fang database (in Chinese). In PubMed and the Cochrane database, references were included from the inception of each database to the end of May 2022. In vivo studies (clinical trials) were collected from the three databases. In vitro studies were mainly obtained from PubMed. To obtain the relevant studies, a three-step search strategy was followed. First, the “Title/Abstract” mode in the search engine was used. Next, a search of the identified keywords and index terms was undertaken across all included databases. For licorice, for example, “licorice[Title/Abstract]” was searched, then the second keyword was added “(licorice[Title/Abstract]) AND chemotherapy[Title/Abstract])”. Finally, clinical trials were found based on the previous search.
For licorice-related clinical trials, the following medical subject heading (MeSH) terms and keywords were used for the search: (licorice OR Glycyrrhiza) AND (cancer OR chemotherapy) AND (chemotherapy side effect OR mucositis OR anemia OR anorexia OR fatigue) AND (clinical trial), with slight modifications for individual searches to suit the instructions of different databases. The above terms were searched in Chinese characters and pinyin (Wang Fang database).
The searching strategy was more complicated for licorice-related medicine (also called Kampo or prescription). The same prescription can have different names in different countries. Taking TJ-41 as an example, hochuekkito, hochu-ekki-to, and TJ-41 are the common names in Japan, while it is known as bojunikgi-tang (bojungikki-tang) in Korea, and bu-zhong-yi-qi tang in China. Interestingly, with/without a hyphen in the name during the search leads to other results in the literature. The different names of each licorice-related medicine were checked in the databases, and the information is summarized in Table 3 and Table 4, respectively. Besides the name of the medicine, the following medical subject heading (MeSH) terms and keywords were applied for the search: AND (cancer OR chemotherapy) AND (mucositis OR anemia OR anorexia OR fatigue) AND (clinical trial). As above, the terms were searched in Chinese characters and pinyin (Wang Fang database).
Table 3.
Common Kampo prescriptions (including Glycyrrhiza) for cancer therapy.
| Name of Kampo | Other Name | Composition | Biological Activity/Treatment |
Evidence of the Activity | Ref. |
|---|---|---|---|---|---|
| TJ-84 | Daiokanzoto (in Japanese) Da-huang-gan-cao-Tang (in Chinese) |
Includes 2 herbs: Rhubarb and Glycyrrhiza |
|
Preclinical: (i) Purgative activity inhibits periodontopathogen via NF-κB pathway; (ii) reduces the secretion of pro-inflammatory cytokine (IL-6 and CXCL8) production; (iii) inhibits MMP-1 and MMP-9 catalytic activities, contributing to anti-inflammation; (vi) decreases AQP3 expression attributed to gut microbiota homeostasis; (v) attenuates 5-FU-induced cell death through the inhibition of mitochondrial ROS production. Clinical: (i) Alleviates cancer-related fatigue. Reduces adverse reactions to radiotherapy or chemotherapy; (ii) improves constipation (double-blind test in Japan); (iii) improves mucositis in esophageal cancer when combined with chemotherapy. |
[58,59,60,61,64,66,69,70] |
| TJ-41 | Bu-zhong-yi-qi tang (BZYQ) (in Chinese) Hochu-ekki-to (in Japanese) Bojungikki- tang (in Korean) |
Includes 7 herbs: Pinellia tuber, Scutellaria baicalensis, Zingiberis hizome, Zizyphi fructus, Coptidis hizome, Glycyrrhiza radix, and Panax ginseng |
|
Preclinical: (i) Reverses cisplatin resistance through induction of apoptosis and autophagy in lung cancer cells; (ii) inhibits 5-FU-induced intestinal mucositis via the suppression of inflammatory cytokine upregulation; (iii) increases lymphocyte cell-surface antigens: CD3+-cells and CD3+/CD4+ cells; (iv) inhibits TNF-α, IL-6, IL-10, TGF-1 and INFγ against chronic fatigue. Clinical: (i) Protective effect of intestine and hematopoietic organs against radiation damage; (ii) improves localized radiotherapy-induced immune deterioration; (iii) improves cancer-related fatigue and QOL; (iv) reduces radiation- or chemotherapy-induced adverse effects. |
[73,74,75,76,79,80,143,144,145] |
| TJ-43 | Rikkunshi-to (in Japanese) Liu-jun-zi tang (in Chinese) Yukgunja-tang (in Chinese) |
Includes 6 herbs: Ginseng radix, Poria cocos, Rhizoma atractylodis macrocephalae, Glycyrrhizae radix et rhizoma, Pinelliae rhizoma, Pericarpium citri, common ginger, and Jujube. |
|
Preclinical: (i) Improves cisplatin-induced anorexia (decreases plasma-acylated ghrelin level and enhances food intake) by acting as antagonists at the 5-HT2B/2C receptors. Clinical: (i) Improves CINV by mediating 5-HT2B/2C receptors and ghrelin receptor signaling; (ii) gastroprotective actions: enhances gastric motility through the 5-HT3 receptor-antagonistic effect; (iii) appetite-stimulating effect via mediating ghrelin receptor signaling (blocked by (D-Lys3)-GHRP-6). |
[95,100,101,102,103,104,108,109,111,112,117,146,147,148,149,150] |
| TJ-48 | Shi-quan-da-bu-tang (in Chinese) Juzen-taiho-to (in Japanese) |
Includes 10 herbs: Ginseng radix, Astragali radix, Angelicae radix, Rehmanniae radix, Atractylodis lanceae rhizoma, Cinnamomi cortex, Poria, Paeoniae radix, Ligustici rhizoma Glycyrrhizae radix |
|
Preclinical: (i) Alleviates bone marrow suppression caused by TS-1 in mice; (ii) reduces pro-inflammatory cytokines and oxidative stress in the liver; (iii) inhibits the production of IL-6, MCP-1, PYY and GLP-1; (iv) anti-tumor via enhanced CD8+ T cell-mediated immunity in CD1d−/− mice lacking NKT cells. Clinical: (i) Regulates T cells: decreases Foxp3+ Treg populations; (ii) inhibits B16 cell metastasis by inducing NK cell activity; (iii) inhibits osteoclast differentiation. |
[124,125,143,144,151] |
| PHY906 | KD018, YIV-906 Huang-qin-tang (HQT) |
Includes 4 herbs: Scutellaria baicalensis Georgi, Paeonia lactiflora Pall, Glycyrrhiza uralensis Fisch, Ziziphus jujuba Mill |
|
Preclinical: Enhances the antitumor activity of Sorafenib in nude mice bearing HepG2 xenografts, by targeting the inflammatory state of the tumor tissue microenvironment. Alleviates chemotherapy-induced side effects, such as diarrhea. Clinical: Enhances the antitumor efficacy of some anticancer drugs, but also alleviates chemotherapy or targeted therapy (e.g., CTP-11)–induced side effects. |
[132,133,134,135,136,141] |
Table 4.
Cancer-related clinical trial of Chinese herbal medicines that include Glycyrrhiza.
| Name of Kampo | Disease/Disorder | Dose/Duration | Trial | Location/Identifier No. | Ref | |||
|---|---|---|---|---|---|---|---|---|
| Patient (n) | Experiment Group |
Control Group |
Outcome | |||||
| TJ-84 | Esophageal cancer |
Oral Tid 2.5 g/bag |
n = 15 |
n = 7 +TJ-84 |
n = 9 DFP * therapy |
A beneficial effect for oral health. | Tokushima University Hospital, Japan | [61] |
| Nasopharyngeal carcinoma | Acupoint patch on the skin | n = 60 |
n = 30 +TJ-84 |
n = 30 ** (Cisplatin) |
Improves CINV and constipation. | Jiangxi Provincial People’s Hospital, China | [67] | |
| NSCLC | Acupoint patch on the skin | n = 116 |
n = 60 + TJ-84 |
n = 56 ** | Zhongshan Hospital, Shanghai, China | [68] | ||
| TJ-41 | Cancer-related fatigue | Oral 2.5 g/Tid 2 weeks |
n = 40 |
n = 20 TJ-41 |
n = 20 | Improves fatigue (experimental group vs. control group, p < 0.05) | Kyung Hee University (Korea) KHU-20090596 (Completed) | [76] |
| Cancer-related-fatigue | Oral 3.7 g/Bid 2 weeks |
n = 112 | n = 56 | n = 56 | No result yet. | Started Oct 2020 KCT0004967 (Ongoing) |
[152] | |
| Advanced NSCLC | Oral | n = 92 |
n = 46 TJ-41 |
n = 46 Chemotherapy |
Improves chemosensitivity, QoL and adverse effects of chemotherapy. | Changsha Traditional Chinese Medicine Hospital, China | [82] | |
| n = 124 |
n = 62 +TJ-41 |
n = 62 Chemo- and radio |
Improves chemosensitivity and immunity. | The 4th people’s Hospital of Shenyang, China | [83] | |||
| Gastric cancer Phase II/III |
Oral 7.5 g/day 4 + 2weeks |
n = 113 |
n = 56 TJ41 |
n = 57 (S1) S-1 *** |
Improves adverse effects of chemotherapy. | Kyoto University Japan UMIN000004701 |
[90] | |
| Gastric cancer | Oral | n = 50/90/60/90 |
n = 25/45/30/45 +TJ-41 |
n = 25/45/30/45 Chemo- |
Improves adverse effects of chemotherapy. | Jingjiang/Ruzhou/Yanling/Taihe, China | [84,85,86,87] | |
| Colon cancer |
Oral decoction 28 days |
n = 52 |
n = 27 +TJ41 |
n = 25 Chemo- |
Improves diarrhea and adverse effects of chemotherapy. | Nanjing University of Chinese Medicine, China | [89] | |
| TJ-43 | Cancer-related anorexia | Oral 3 g/Bid 4 weeks |
n = 56/4 n = 40 (total n = 90) |
n = 26 n = 20 + TJ-43 |
n = 26 n = 20 Chemotherapy or radiotherapy |
Improves dyspepsia and anorexia. | Daejeon Korean Medicine Hospital of Daejeon University KCT0002847 | [104,105] |
| Advanced esophagus cancer |
Oral 2.5 g/Tid 2 weeks |
n = 19 | n = 8 |
n = 10 DFP |
Improves CINV. | Tokushima University Hospital, Japan | [113] | |
| Esophagus cancer | Oral 2.5 g/Tid 22–35 days |
n = 18 | n = 9 |
n = 9 DFP |
Improves anorexia | Hiroshima University, Japan | [115] | |
| Relapsed gastric cancer | Oral 2.5 g/Tid 2 weeks |
n = 10 |
n = 5 +TJ43 |
n = 5 S-1 +CDDP |
Improves CINV. | Gunma University, Japan |
[112] | |
| Lung cancer | Oral 2.5 g/Tid 21–28 days |
n = 60 | n = 30 |
n = 30 CDDP |
Improves cisplatin-induced anorexia. | JAPIC CTI-142747 Takeda General Hospital, Fukushima, Japan |
[114] | |
| Oral 2.5 g/Tid 2 weeks |
n = 40 | n = 20 |
n = 20 CDDP |
UMIN000010748 Hiroshima University, Japan |
[116,117] | |||
| Oral 2.5 g/Tid 1 week |
n = 91 | n = 64 |
n = 27 CDDP |
Improves cisplatin-induced appetite. | Mito Medical Center Mito, Japan | [109] | ||
| Oral 84 days |
n = 100 | n = 50 | n = 50 | Improves CINV, appetite, and fatigue. | Jiading Hospital, Shanghai, China | [122] | ||
| Colon cancer |
Oral 6 months |
n = 70 | n = 36 |
n = 34 5-FU |
Improves CINV, diarrhea, and fatigue. | Jiading Hospital, Shanghai, China | [118] | |
| Oral 186 days |
n = 70 | n = 39 | n = 39 | Jiading Hospital, Shanghai, China | [121] | |||
| Oral Bid 1 month |
n = 60 | n = 30 | n = 30 | Improves immunity and fatigue. | Jiangnan University Affiliated Hospital Jiangsu, China |
[120] | ||
| Gastric cancer | Oral 42 days |
n = 64 | n = 32 | n = 32 | Improves CINV, immunity, and fatigue. | Chuzhou Hospital Jiangsu, China |
[119] | |
| TJ-43 | Cervical/corpus cancer | Oral 2.5 g/Tid 13 days |
n = 40 | n = 19 |
n = 17 CDDP + paclitaxel |
Improves CINV and anorexia. |
UMIN000011227 Phase II, 4 institutions, Hokkaido, Japan |
[111] |
| Dyspepsia | Oral 2.5 g/Tid 8 weeks |
n = 247 | + TJ-43 n = 125 |
Placebo n = 122 |
Improves dyspepsia, epigastric pain, and postprandial fullness. | UMIN Clinical Trials Registry, Number UMIN000003954 (Japan) | [102] | |
| TJ-48 | Cancer-related anorexia |
Oral 3 g/TID 4 weeks |
n = 40 | TJ-48 | Placebo | Improves appetite and survival. |
NCT02468141 (Korea) HI12C1889 (Completed) |
[126,127] |
| Cancer-related fatigue | Oral 3 g/TID 21 days |
n = 48 | + TJ-48 | Placebo | Improves fatigue (breast cancer). |
KCT0003442 (Korea) |
[153] | |
| HCC | Oral 7.5 g/day 6 years |
n = 48 |
n = 10 + TJ-84 |
n = 38 | Improves the recurrence-free survival. | University of Yamanashi Hospital (Japan) U19-ES11391 R01-AA16285 R01-ES12686 |
[124] | |
| Cancer-related fatigue | Oral 3 g/TID 56 days |
n = 48 | + TJ-48 | Placebo | Improves fatigue (breast cancer received doxorubicin and cyclophosphamide treatment). |
NCT02858856 (Korea) | [130] | |
| Cancer-related fatigue | Oral | n = 16 | + TJ-48 | N.A. | Improves QOL score. (NSCL) |
Japan | [154] | |
| Non-small cell lung cancer | Oral 2.5g/TID 14 days~2 months |
n = 45 |
n = 23 Chemo + TJ48 |
n = 22 Chemo- only | Improves the progression-free survival. Prevents nutritional disorders. Increases physical fitness. |
Akita Red Cross Hospital (approval no. H26-7) | [155] | |
| TJ-48 | Breast cancer | 3–5 g/TID 21 days |
n = 79 | +TJ-48 n = 13 |
Chemotherapy n = 66 |
Alleviates hepatotoxicity after chemotherapy. Enhances immune functions. |
TMUH-02-10-02 Taipei, Taiwan |
[156] |
| Pancreatic cancer | Oral 7 years |
n = 1 | A case report | N.A. | Prevents adverse effects. | Tohoku University (Institutional Review Board No. 18,910) |
[157] | |
| PHY 906 | Colorectal cancer | Oral 1.2 g/Bid 1.8 g/Bid 2.4 g/Bid 4 weeks |
n = 17 |
n = 5 CPT-11/5-FU/LV + PHY906 |
n = 12 PT-11/5-FU/LV + placebo |
Enhances efficacy of chemotherapy, reduces toxicity and alleviated side effects such as diarrhea, abdominal cramps, and vomiting. | PHY906-2000-1 (US)(Completed) Yale Cancer Center, HIC0808004167 |
[134,139] |
| CPT-11 + PHY906 | Placebo | PHY906-2002-1 (US) PHY906-2002-1-T (US) |
||||||
| HCC | Oral 800 mg/Bid |
n = 31 (Phase I/II) |
PHY906-+ Cape *** | Cape *** | Purpose: to evaluate the safety and efficacy of PHY906 NCT04000737 | PHY906-2007-1-T NCT00076609 (Completed) |
[142] | |
| Liver cancer | Oral 800 mg/Bid |
n = 125 (Phase I) |
PHY906 +Sorafenib |
Sorafenib | Enhances efficacy of chemotherapy, reduces toxicity and alleviated side effects. |
NCT04000737 (2020.03 updated) |
[132] | |
| Pancreatic cancer | Oral 800 mg/Bid |
n = 24 (Phase I/II) |
PHY906- +Cape *** | N.A. | Improves survival, enhances efficacy of chemotherapy, reduces toxicity and alleviates side effects. | Yale Cancer Center, NCT00076609 NCT00411762 HIC0512000905 (2015.03 completed) |
[135,137,140] | |
* Chemotherapy includes docetaxel, and low-dose 5-FU and cisplatin (CDDP). ** Treated with aprepitant–dexamethasone. *** S-1(dose: 80 mg/m2/d): includes capecitabine and oxaliplatin (CapeOX); and epirubicin, oxaliplatin and oxaliplatin (EOX).
The inclusion criteria were based on the following:
-
(1)
Type of participant: cancer patients treated with chemotherapy or radiation therapy;
-
(2)
Type of study: We tried to include as many as possible. As the number of licorice-related clinical trials is low, the study size is small-scale;
-
(3)
Type of intervention: Participants in the intervention groups were treated with licorice or licorice-related medicine combined with chemotherapeutic drugs. There was no concern about the forms of interventions (e.g., decoction, capsule, acupoint patch gel, and granule), the dosage, or the treatment duration. The control groups used chemotherapy alone, chemotherapeutic drugs plus a placebo, or chemotherapeutic drugs plus western medicine. The control groups used chemotherapy alone, chemotherapeutic drugs plus a placebo, or chemotherapeutic drugs plus western medicine;
-
(4)
Type of outcome measure: Mainly focusing on chemotherapy-induced side effects, such as fatigue, oral mucositis, anorexia, anemia, constipation, etc.
The exclusion criteria were as follows:
-
(1)
The study purpose is not related to chemotherapy-induced side effects;
-
(2)
Duplicate studies in a different database, review, animal experiments, and conference abstracts;
-
(3)
Misunderstandings, misleading studies, and inappropriate use/measurement;
-
(4)
Studies did not present clearly, including an inappropriate or unclear study design to collect data;
-
(5)
Lacking statistical analysis.
Description of Review Context
A total of 48 trials were included in this review; all of these trials took place in Asia (in China, Japan, Taiwan, and Korea) and were reported in English or Chinese. The details of the mechanism and the clinical trials are summarized in Table 3 and Table 4, respectively. A descriptive review is presented.
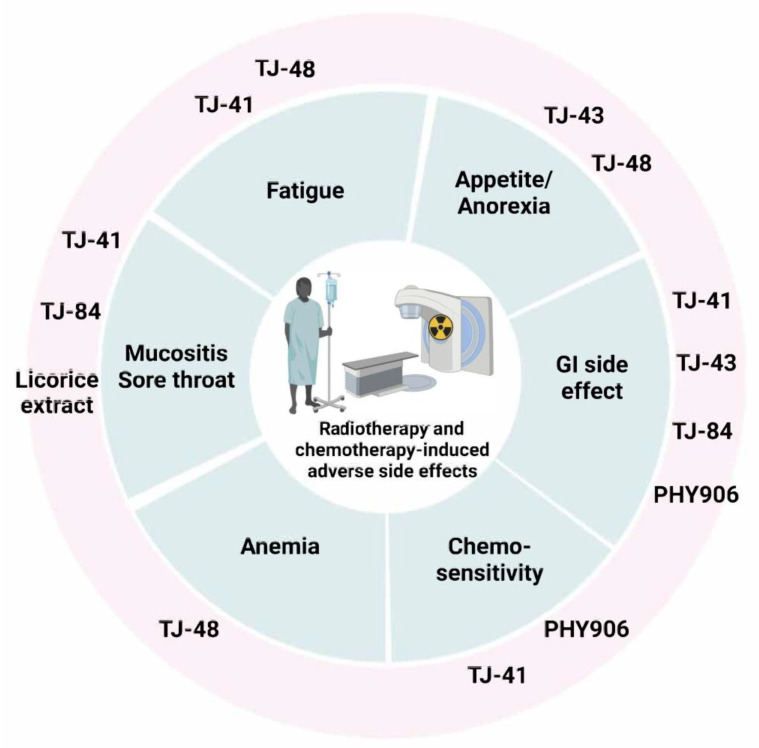
When Kampo medicine is combined with chemotherapy/radiation, it reduces the side effects induced by chemotherapy. For example, TJ-48 improves cancer-related fatigue, anorexia, and anemia. TJ-43 also mitigates anorexia and chemotherapy-induced GI problems. TJ-41 mainly acts on fatigue and mucositis.
3. Traditional Herbal Formulation
Traditional Chinese medicine (TCM), called Kampo in Japan, comprises a combination of compatible natural herbs. The Japanese Ministry of Health, Labor and Welfare officially approved the wide use of traditional herbal formulations as ethical pharmaceutical products [51,52]. Chinese herbal products are commonly applied for daily practice as dietary supplements. In China, numerous clinical studies explore TCM as an adjuvant cancer treatment during chemotherapy or radiotherapy [53,54]. TCM alleviates the toxicities of chemotherapy agents and controls the side effects, thus, improving compliance with chemotherapy and the patient’s QoL [6]. Licorice-related TCM contains many phytochemicals, including triterpenoid saponins, flavanones, chalcones, and coumarins and their glycosides, which exhibit a broad range of biological activities [55,56,57]. Here, we summarize a brief outline of the pharmacological effects of TCM containing licorice in Table 3, and the related clinical trials in Table 4 (Figure 2).
Figure 2.
Kampo combinations improve chemotherapy-induced side effects in clinical trials.
3.1. TJ-84
Daiokanzoto (DKT; also called da-huang-gan-cao-tang or TJ-84) is a Kampo medicine that is composed of crude extracts of rhubarb rhizomes and Glycyrrhiza roots. TJ-84 is mainly investigated for use on peptic ulcers, hepatitis C, and pulmonary and skin diseases [58,59,60,61]. Wang et al. study the chemical constituents in TJ-84, using the combination of LC–ESI-Q-TOF–MS and LC–ESI-IT–MS, and identify 104 compounds [62]. Flavonoids and triterpenoids are the major bioactive compounds present in Glycyrrhizae radix, and they exhibit diverse biological effects [63]. Furthermore, Takayama et al. identify that in Sennoside A (SA), rhein 8-O-β-D-glucopyranoside from rhubarb, and liquiritin (LQ) from glycyrrhiza, are the main active constituents in vivo that alleviate constipation [58,59,64,65]. TJ-84 exerts a purgative activity that may mediate gut microbiota against constipation [59,65], and clinical data reveal its effectiveness against constipation, vomiting, and nausea [59,64,65,66,67,68]. A 2019 retrospective cohort study confirms the same effect on constipation [69]. It is reported that TJ-41 possesses anti-inflammatory potential by mediating the secretion of pro-inflammatory cytokines (IL-6 and CXCL8) and tissue degrading enzymes matrix metalloproteinase (MMP-1 and MMP-9), in addition to preventing biofilm formation [70]. In another in vitro study, Yoshida et al. demonstrate that TJ-41 attenuates 5-fluorouracil-induced apoptosis, by inhibiting the production of mitochondrial reactive oxygen species [66]. This leads to the suggestion that TJ-41 could be used to treat oral mucositis in patients receiving chemotherapy [71]. A clinical study confirms that TJ-84 improves mucositis in esophageal cancer patients treated with chemotherapy [61].
3.2. TJ-41
Bu-zhong-yi-qi-tang (hochuekki-to or TJ-41 in Japanese, or bojungikki-tang in Korean) is prescribed to treat fatigue, visceroptosis, and chronic diarrhea. It contains seven herbs, including Pinellia tuber, Scutellaria baicalensis, Zingiberis rhizoma, Zizyphi fructus, Coptidis rhizoma, Glycyrrhiza radix, and Panax ginseng. Using High performance liquid chromatography-diode array detection (HPLC-DAD) guidance, liquiritigenin and ISL were found in the highest abundance in TJ-41 [72]. When TJ-41 is used to treat cancer patients after chemotherapy, with medication such as cisplatin or 5-FU, it improves chemosensitivity and inflammation [73,74]. Regarding cancer-related fatigue, Kuroda et al. (1985) demonstrate that treatment with TJ-41 results in a significant improvement in the quality of life (QoL) of 162 patients with cancer-related cachexia (i.e., anorexia and fatigue), especially targeting fatigue and anorexia [75]. In another pilot randomized clinical trial, the use of TJ-41 results in an improvement in chemotherapy-induced fatigue, without any significant adverse effects [76]. Based on the above, TJ-41 is a common prescription medicine for cancer patients in Japan, and its use results in improvements in cancer-related fatigue and quality of life in these patients [74,75]. As far as the molecular mechanism is known, TJ-41 may be attributed to peripheral immunity, suppressing the immune escape of tumors, and inducing immune deterioration [75,76,77]; for example, inhibiting the production of proinflammatory cytokines, particularly IL-6 [78]. Furthermore, TJ-41 may inhibit Tumor Necrosis Factor-α (TNF-α), Interleukin-6 (IL-6), IL-10, Transforming Growth Factor-1 (TGF-1), and Interferon (INF) production, in order to combat chronic fatigue syndrome [78,79,80]. During the search of the literature, we also found some clinical studies in Japan and China [81,82,83,84,85,86,87,88,89] that apply TJ-41 with chemotherapy, with the studies suggesting that TJ-41 reduces the adverse effects of chemotherapy and improves the overall QoL scores. A multicenter randomized phase II study from 2019 [90], targeting stage II/III gastric cancer patients with chemotherapy (n = 113), also supports the same suggestion [90]. Another study, in the form a retrospective review, includes 1412 advanced non-small cell lung cancer (NSCLC) patients divided into two groups. The control group received cisplatin treatment; while the other was treated with cisplatin and TJ-41. The results suggest that TJ-41 improves chemosensitivity, immunity, adverse effects, and overall QoL [91]. In summary, TJ-41 has potent immunomodulatory, anticancer, and fatigue-reducing actions.
3.3. TJ-43
Liu-jun-zi-tang (TJ-43 or rikkunshito in Japanese, yukgunja-tang in Korean) includes six herbs: Ginseng Radix, Poria cocos, Rhizoma atractylodis macrocephalae, licorice root, pinelliae tuber, pericarpium citri, common ginger, and jujube. TJ-43 is often prescribed for anorexia and upper gastrointestinal (GI) disorders [92,93]. Based on a components assay, TJ-43 shows 36 active components, with glycycoumarin, nobiletin, tangeretin, ISL, [8]-shogaol, glycyrrhetic acid, and hesperetin being dominant [94]. Some functioning active components are reported in TJ-43, such as hesperidin, ISL [95,96], and glycycoumarin [97]. In a preclinical study, high levels of liquiritigenin and its glycoside forms are identified in plasma and in the brain after a single oral administration of TJ-43 (1000 mg/kg) [98]. ISL is not only detected after the oral administration of TJ-43, but a comparable amount of ISL is also shown in plasma and brain distribution, especially compared with an ISL (5 mg~50 mg/kg) single treatment [94]. Magomi et al. suggest that ISL is one of the most important active components in TJ-43, acting as an antagonist to both CRF receptor 1 (CRFR1) and serotonin 2C receptor (5-HT2CR) in order to reduce ghrelin secretion, which further improves stress-induced anorexia [94,95,99]. In addition, several multi-center, double-blinded, randomized placebo-controlled studies were conducted to examine its effect with regard to improvements in upper GI disorders, such as dyspepsia [100,101,102,103]. Another randomized, controlled trial, pilot study (n = 40) was conducted by Ko et al. to estimate the efficacy and the safety of TJ-43 [104,105]. Generally speaking, chemotherapy-induced nausea and vomiting (CINV) occurs within 24 h after chemotherapy administration. Nausea and vomiting are two of the most common side effects experienced by patients [106]. Although the mechanism of chemotherapy-induced CINV is not thoroughly understood, cisplatin-related adverse effects are associated with the secretion of serotonin (5-hydroxytryptamine, 5-HT) and changes in ghrelin dynamics [107]. Therefore, 5-HT3 receptor antagonists are widely applied to prevent cisplatin-induced CINV. Even with a standard treatment, a three-drug combination of a 5-HT3 receptor antagonist, a neurokinin-1 receptor antagonist, and dexamethasone (as an aprepitant regimen) show only a 60~80% mitigation of CINV [107]. Seeking further improvement in CINV, some clinical studies recommend the co-administration of TJ-43 as an effective option for breakthrough CINV, as TJ-43 also acts as an antagonist at the 5-HT2B/C, 5-HT3 receptors and the ghrelin receptor [95,99,108,109,110]. TJ-43 combined with chemotherapy is shown to prevent CINV in esophagus, gastric, lung, cervical, and corpus cancer patients [111,112,113,114]. In addition, anorexia (loss of appetite) is also a common concomitant of cancer, especially in advanced cancer. Anorexia may be induced by cancer itself and cancer treatment. Both chemotherapy and radiation therapy can trigger varying degrees of anorexia. A few randomized controlled trials aimed to evaluate the efficacy and safety of TJ-43 for chemotherapy-induced anorexia or cancer-induced anorexia [104,105,114]. Many clinical studies indicate that TJ-43, co-administered with chemotherapy, improves anorexia and aids in maintaining food intake by mediating the 5-HT2B/C receptor or the ghrelin receptor [104,105,109,111,112,113,114,115,116,117]. Based on the above description, it is suggested that TJ-43 application mainly acts on CINV and anorexia. This conclusion was reached by different research groups (in China, Japan, and Korea) using the same receptors.
TJ-43, also called li-jun-zi-tang (LJZT) in China, has a long history of use for functional dyspepsia. The prescription originated hundreds of years ago (in the Ming Dynasty) in China. However, even though there are many clinical trials studying chemotherapy combined with TJ-43, only a small number of trials use validated international criteria to assess the side effects of chemotherapy. Many of them present with a considerable risk of bias. Based on these concerns, we only included three studies in this review [118,119,120,121,122].
Overall, all the relevant studies suggest that TJ-43 combined with chemotherapy can mitigate chemotherapy-induced CINV and anorexia.
3.4. TJ-48
Shi-quan-da-bu-tang (juzentaiho-to or TJ-48 in Japanese, or sipjeondaebo-tang in Korean) can be used to treat various kinds of diseases, such as anemia, rheumatoid arthritis, atopic dermatitis, chronic fatigue syndrome, and ulcerative colitis. TJ-48 is composed of 10 herb components, including Ginseng radix, Astragaliradix, Angelicae radix, Rehmanniae radix, Atractylodis lanceae rhizoma, Cinnamomi cortex, Poriacocos, Paeoniaeradix, Ligustici rhizoma and Glycyrrhizae radix. There are 36 major components in TJ-48, including flavonoids/flavonoid glycosides (liquiritin, isoliquiritin, etc.), triterpenoid saponins, iridoid glycosides, phthalides, and phenylpropionic acids, which were characterized using high-performance liquid chromatography / electrospray ionization mass spectrometry (HPLC–ESI–MS/MS) [123]. A study by Tsuchiya et al. (2008) suggests that TJ-48 functions as a hepatic protectant by hampering Kupffer cell-induced oxidative stress [124]. When Kupffer cells are inhibited, TJ-48 plays an important role in lowering pro-inflammatory cytokines and oxidative stress levels. A preclinical study shows that TJ-48 inhibits the production of IL-6, MCP-1, PYY, and GLP-1 and ameliorates cancer-induced anemia using a CT-26 tumor-bearing mouse cancer anorexia/cachexia model [125]. Overall, TJ-48 may be a better option for treating cancer associated with anorexia. TJ-48 is one of the most commonly used traditional herbal medicines in Asia, and is prescribed for patients who suffer from anemia, fatigue, and anorexia. Anorexia may result from the cancer, chemotherapy, or radiotherapy. A study implies that TJ-48 used as a treatment for anorexia regulates the levels of glucagon-like peptide-1 (GLP-1) and peptide tyrosine tyrosine (PYY), which are satiety stimulators [125]. Recently, two clinical studies apply TJ-48 as a treatment for anorexia to evaluate its efficacy [126,127]. Besides anorexia, TJ-48 ameliorates anemia [128], assisting patients receiving chemotherapy [129]. Fatigue is another frequent complaint after chemotherapy; thus, a few clinical studies related to fatigue were conducted [81,125,130]. In a study by Tsuchiya et al., which includes 48 hepatocellular carcinoma (HCC) patients treated with TJ-48 and then followed up for up to six years, it is suggested that TJ-48 improves HCC recurrence-free survival [124]. Concerning long-term survival, this tentative conclusion needs further detailed investigation in the future.
3.5. PHY906
PHY906 (YIV-906 or KD018) is derived from huangqin tang (HQT), which is composed of four herbs: Glycyrrhiza uralensis Fisch (G), Paeonia lactiflora Pall (P), Scutellaria baicalensis Georgi (S), and Ziziphus jujuba Mill (Z). Huangqin tang was first documented in Chinese texts 1800 years ago as being used in the treatment of GI disorders, including diarrhea, nausea, and vomiting, and abdominal cramps. Based on LC–MS analysis, its chemical profile contains 64 bioactive compounds, including flavonoids, triterpene saponins, and monoterpene glycosides [131]. One of the main components with anticancer activity is ISL. The preparation of PHY906, packaged in capsules, is conducted according to the current Good Manufacturing Practices (cGMPs), under the United States Food and Drug Administration (FDA) guidance. PHY906 demonstrates chemotherapeutic efficacy enhancement with a variety of anticancer agents in various cancers. PHY906 clinical trials indicate that PHY906 acts as an adjuvant to CTP-11, 5-fluorouracil (5-FU), leucovorin, and capecitabine in the treatment of advanced colorectal, pancreatic, and liver cancer [132,133,134,135,136,137,138,139,140,141]. PHY906 has additive antitumor activity, but does not alter the pharmacokinetics or toxicity of irinotecan, 5-FU, and leucovorin [134]. In a phase II clinical trial study, it is found that PHY906 enhances the capecitabine-induced antitumor activity and survival rate in Asian patients with hepatocellular carcinoma (HCC) and hepatitis B virus infection (n = 39) [142]. PHY906 plus capecitabine provides a safe and feasible salvage therapy in pancreatic cancer patients (n = 25) [135]. A combination of PHY906 and capecitabine could be an effective therapy elevating the median survival of Asian patients suffering from hepatocellular cancer [138]. PHY906 (800 mg BID) increases the therapeutic index of capecitabine in patients with advanced stage disease (APC) and other GI malignancies, by reducing side effects such as diarrhea (n = 24) [137]. Clinical trial results consistently suggest that PHY906 is one of the most extensive chemotherapeutic adjuvants. Advanced clinical trials (phase III) are needed to demonstrate the effectiveness of PHY906 as an adjuvant therapy for cancer patients undergoing chemotherapy.
4. Traditional Chinese Medicine as an Adjuvant Treatment to Improve the Side Effects of Cancer Therapy
Here, we summarize the use of TCMs to reduce some of the complications caused by chemotherapy or radiotherapy (Figure 2).
4.1. Fatigue
Fatigue is the most common side effect of cancer chemotherapy, and even adequate rest cannot alleviate the fatigue [158]. TJ-41 alleviates chemotherapy-induced fatigue, which may be attributed to the activation of the immune system [79]). In addition, TJ-41 alleviates chronic fatigue through the inhibition of interferon gamma (INF-γ), IL-6 and IL-1β [80], as well as halt the occurrence of inflammation [159]. Collectively, TJ-48, as a formulation, can be considered as enhancing health and immunity. Therefore, the combination of TJ-48 and chemotherapy could improve chemotherapy-induced malnutrition and prognosis, as it induces an improvement in nutritional intake that could increase physical strength [160].
4.2. Pain
Chronic pain is often seen after chemotherapy/radiotherapy treatments. Pain may result from cancer metastasis, or the nerve damage caused by cancer treatment [161]. More than 55% of patients suffer from pain during cancer treatment [162]. A previous study shows the ability of licorice to relieve pain in terminal cancer patients [163], and this may be due to the anti-inflammatory and antioxidative effects of licorice [164]. In chemotherapy treatment, paclitaxel is one of the most widely used chemotherapeutic drugs for several cancers. However, its side effects include the induction of neuropathic pain, which causes tingling and burning sensations [165]. Nuclear factor erythroid-2-related factor 2 (Nrf2) is considered as a regulator of antioxidant defense, and so its activation could ameliorate paclitaxel-induced pain [166]. The licorice-derived compound ISL, as a potential Nrf2 inducer, could upregulate Nrf2 expression and its downstream genes [167]. Licorice’s pain-relief potential may be due to its Nrf2-dependent transactivation ability and, thus, its antioxidant effect.
4.3. Mucosal Irritation
During clinical cancer treatment, radiotherapy and chemotherapy rapidly destroy high proliferative cells, including the proliferating cancer cells and the dividing epithelial cells [168]. In head and neck cancer patients, mucositis is the most common side effect of cancer therapy. In a double-blinded clinical trial, head and neck cancer patients received glycyrrhiza aqueous extract from the first day of radiotherapy, and it is found that this reduces the grade of mucositis and mucosal irritation after intervention [39]. Due to its anti-inflammatory effect, glycyrrhiza could inhibit macrophage activation, and decrease prostaglandin E2 levels and the secretion of free radicals in macrophages [169]. Moreover, its antioxidant action is able to scavenge free radicals and decrease the reactive oxygen species [170].
4.4. GI Side Effect
During chemotherapy treatment, toxicity causes GI side effects, including vomiting, diarrhea, and nausea [171]. The discomfort level may differ according to the type of chemotherapy, the duration, and the tolerance of patients. The emetogenic reagents include capecitabine [137], cisplatin, doxorubicin, and carboplatin [172]. In an in vivo study, PHY906 shows an ability to inhibit the nuclear factor kappa-light-chain-enhancer of activated B (NFκB), cyclooxygenase-2 (COX2), and inducible nitric oxide synthase (iNOS) pathways in CPT-11-induced intestinal inflammation [136]. Chemotherapy/radiotherapy-induced GI side effects could be reduced through the amelioration of the inflammatory factor.
4.5. Anemia
Anemia in cancer patients occurs during disease progression, or as a result of blood loss, malnutrition, bone marrow damage, and radiation treatment [173,174], which impair erythropoietin (EPO) production and shorten the half-life of red blood cells [175]. Patients with anemia may suffer from dizziness, edema, heart failure, or even severe cognitive dysfunction [176]. TJ-48, which is abundant in ginsenoside, paeoniflorin, eudesmol, and glycyrrhizic acid, can stimulate bone marrow cells, alleviating anemia and, thus, reducing the decrease in hemoglobin [177,178]. In chronic hepatitis C, TJ-48 affects T cell–related immunity by improving peripheral blood T-helper (Th)1 cells, highlighting that the potential effect of TJ-48 may be related to its immune regulatory response [179].
4.6. Anorexia–Cachexia
Anorexia–cachexia is defined as a syndrome related to loss of appetite, weight loss, and invulnerable weight loss or muscle loss, which mainly results from a decrease in energy intake [180]. Loss of appetite is related to taste change, and is one of the most common side effects of cancer treatment [181]. During either cancer treatment or cancer progression, the production of appetite-depressing factors is activated through resultant oxidative stress or cytokine secretion [182]. Cancer treatment induces cytotoxic damage, which causes a rapid decrease in the taste and smell receptors and in the secretion of saliva, which results in the sense of the flavor of food being affected [183,184]. Yashtimadhu (Glycyrrhiza glabra) effectively decreases chemotherapy/radiotherapy-induced oral mucositis [185]. Licorice is also reported to prevent dexamethasone-induced muscle loss [186], and could effectively decrease muscle degradation-related proteins, and muscle RING-finger protein-1 (MuRF1) and atrogin-1 protein expression, by relying on its anti-oxidative effects.
5. Traditional Chinese Medicine as an Adjuvant in Cancer Therapy
Chemotherapy/radiotherapy complications could be alleviated by several Kampo prescriptions. Moreover, several traditional herbal medicines are found to exert an adjuvant, anti-proliferative effect in cancer therapy. In a randomized controlled trial, adding TJ-41 for 2 weeks [76] not only improves cancer-related fatigue, but also decreases cancer therapy fatigue. These improvements may have benefits in different types of cancer, including breast, stomach, colorectal, and lung cancer.
In a placebo-controlled clinical trial, TJ-48 is shown to improve appetite and survival after 4 weeks of oral administration. PHY906 is used widely in the treatment of GI symptoms, and has additional anticancer properties, as shown in a clinical trial where a combination of PHY906 and capecitabine treatments was given to pancreatic and GI malignancy patients [137]. Results show that 800 mg BID of PHY906, combined with different dosages of chemotherapy capecitabine, for 14 days, results in a better tolerance of capecitabine treatments, without any discomfort. In a previous clinical trial, PHY906 combined with irinotecan and 5-FU/LV treatment, for the treatment of colorectal cancer, lowers the frequency of GI-related side effects [139] through its cytoprotective and antidiarrheal activity. Moreover, in an in vivo study, PHY906 enhances CPT-11’s antitumor activity by apoptosis induction [187]. In hepatocellular carcinoma clinical treatment, sorafenib, the only approved drug, has diarrhea as a serious side effect. Interestingly, the combination with PHY906 not only enhances the sorafenib-induced autophagy by increasing p-AMPKα and p-ULK1, but also alleviates diarrhea [132]. Similarly, licorice aqueous root extract, combined with radiotherapy, may prevent oral ulcers. In a double-blinded clinical trial, head and neck cancer patients received glycyrrhiza aqueous extract from the first day of radiotherapy, which reduces the grade of mucositis and mucosal irritation [39].
Taken together, licorice-containing Kampo not only has the ability to improve cancer treatment-related side effects, but also has potential benefits as a cancer adjuvant therapy.
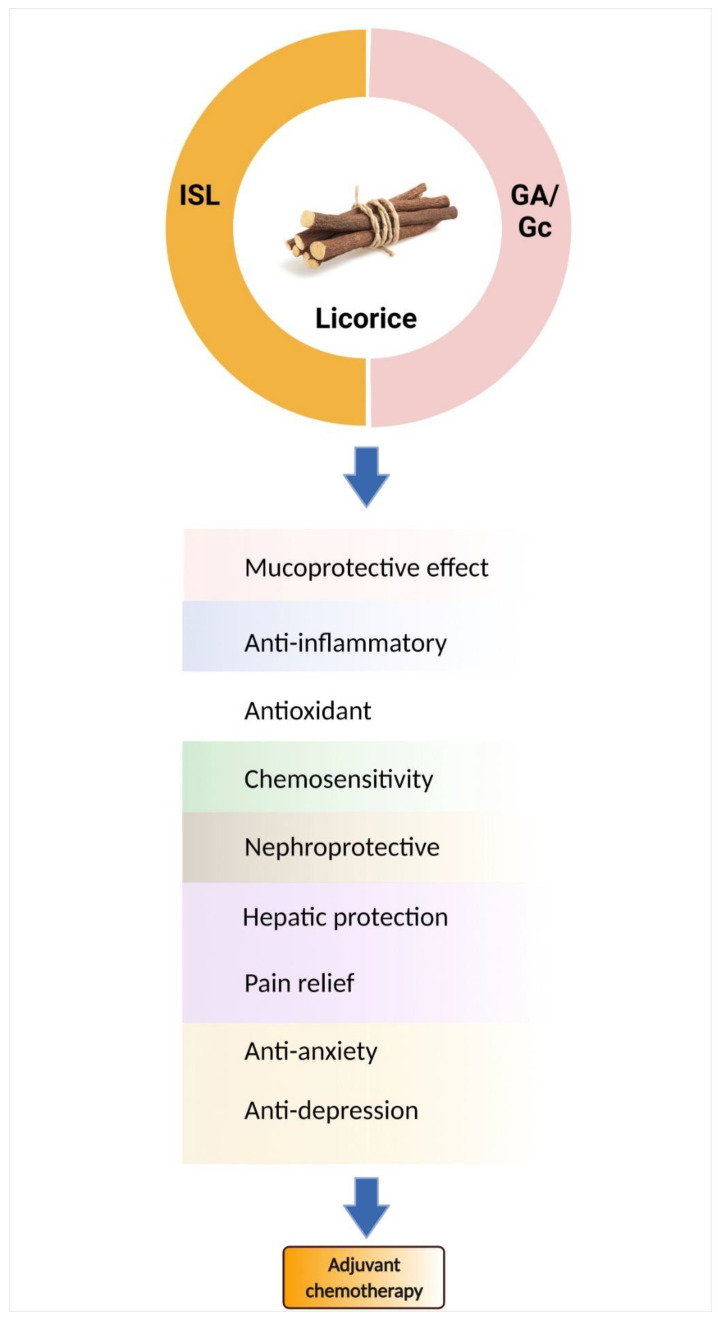
6. Bioactive Components of Licorice
Licorice root contains a variety of bioactive components, including alkaloids, polysaccharides, polyamines, triterpenes, phenolic acids, flavones, flavans, chalcones, flavonoids, and isoflavonoids. Among them, only a few can be characterized and isolated from licorice. In this review, only the components studied for chemoprevention are discussed (See Table 5), such as glycyrrhetic acid (GA) and chalcone-type derivative isoliquiritigenin (ISL) (Figure 3).
Table 5.
Licorice compounds, mechanisms of action and potential chemopreventions.
| Compounds | Pharmacological Group | Chemotherapy | Therapeutic Actions/Mechanism | Ref |
|---|---|---|---|---|
| Glycyrrhizinic acid | Triterpenoid saponin | 5-Fluorouracil |
|
[197,198] |
| Cisplatin |
|
[196] | ||
| Cisplatin/radiation |
|
[199,200,201] | ||
| Erlotinib/cisplatin |
|
[202] | ||
| Doxorubicin |
|
[204,205,210] | ||
| Paclitaxel |
|
[203,211] | ||
|
[206] | |||
| N.A. |
|
[212,213] | ||
| Glycyrrhizin | Cyclosporine (CsA) |
|
[214] | |
| Isoliquiritigenin | Trans-chalcone (flavonoid) | Cisplatin |
|
[208,215,216,217] |
|
[207,218] | |||
| 5-Fluorouracil |
|
[219] | ||
|
[220] | |||
| Doxorubicin |
|
[221] | ||
|
[222,223] |
Figure 3.
Licorice and its active components are candidates for chemo-combinations. Glycyrrhizin (Gc)/glycyrrhetic acid (GA) and isoliquiritigenin (ISL) mediate many mechanisms to improve chemotherapy-induced adverse effects.
Glycyrrhizin demonstrates immunomodulatory actions in vitro, stimulating T lymphocytes for IL-2 production [188]. An anti-inflammatory effect is associated with glycyrrhizinic and glycyrrhetic acid, via an inhibition of corticosteroid metabolism and production [189]. To extend the corticosteroid effects, it is broadly classified into immunological and metabolic effects [190]. From a metabolic perspective, the active form of glycyrrhizin, glycyrrhetic acid, influences energy metabolism and fat distribution by mediating fatty acid oxidation–related genes [191,192]. To emphasize the role of antioxidants, pretreatment with glycyrrhizinic acid could decrease free radicals and increase the level of reduced glutathione (GSH) [193,194]. Licorice extract and glycyrrhizic acid could reduce ROS-mediating p53 activation, and promote p21 expression against cisplatin-induced nephrotoxicity in vitro [195]. In an animal model, glycyrrhizic acid (GA) and 18β-glycyrrhetinic acid (18βGA) are represented as chemoprotectants, through the modulation of the NF-κB and Nrf2 pathways to reduce cisplatin-induced nephrotoxicity [196]. Overall, glycyrrhizin has been widely studied for combination chemotherapies involving cisplatin, 5-Fluorouracil, radiation, doxorubicin, paclitaxel, etc. [196,197,198,199,200,201,202,203,204,205,206].
Isoliquiritigenin, one of the major bioactive compounds found in licorice, shares the same basic pharmacologic effects as Glycyrrhiza and exerts more biological activity, especially in its anti-tumor effects [10]. In a CT-26 murine colon animal model, ISL suppresses cisplatin-induced kidney/liver damage by mediating nitric oxide, lipid peroxidation, and GSH levels [207]. Based on the antioxidant properties of ISL, it shows a protective effect on cisplatin-induced toxicity, through regulating the oxidative ER stress hormesis. [208]. In addition, to target the anti-inflammatory effects, ISL also inhibits IL-6, IL-12, and TNF-α production [209]. Many studies suggest that licorice extract or licorice-derived active components benefit chemotherapy (Figure 3). Table 5 summarizes the licorice components associated with chemopreventive activities, mainly focusing on glycyrrhizin and ISL. However, some components of licorice present unwanted side effects; therefore, Kampo medicine is another option to improve chemotherapy-induced adverse effects.
7. Conclusions
Currently, the utility of TCM in alleviating the adverse reactions induced by radiotherapy and chemotherapy in cancer treatment is gaining increased attention worldwide. Increasingly, evidence demonstrates that licorice-containing TCM can reduce chemotherapy- and radiotherapy-induced side effects, such as fatigue, appetite, GI toxicity, anemia, and mucositis. Collectively, licorice-containing TCM can improve patients’ QoL and reduce mortality. In this review, we conducted a descriptive study focusing on the role of the bioactive constituents in licorice-containing herbs in reducing the adverse effects of chemotherapy and radiotherapy. It is hoped that this comprehensive review will serve as a cornerstone to encourage more scientists to evaluate and develop effective TCM prescriptions, in order to improve the side effects of chemotherapy and radiotherapy.
Author Contributions
Writing—original draft preparation, Y.-C.Y. and K.-L.W.; references preparation, H.-Y.C., T.-M.S. and Y.-F.C.; writing—review and editing, M.A. and S.-M.H.; editing and approval of the final version of the manuscript, S.-M.H. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This work was supported by grants MOST110-2314-B-038-158, MOST110-2628-B-038-018, MOST110-2320-B-254-001, MOST109-2320-B-254-001, MOST109-2811-B-039-503, MOST108-2314-B-039-009-MY3, MOST108-2314-B-039-042-MY3, MOST108-2314-B-039-043-MY3, CMU109-MF-26, DMR-110-232, DMR-109-084, DMR-110-231, and DMR-109-019 from the Ministry of Science and Technology, Taiwan and China Medical University/Hospital, Taiwan.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Chung V.C.H., Wu X., Lu P., Hui E.P., Zhang Y., Zhang A.L., Lau A.Y.L., Zhao J., Fan M., Ziea E.T.C., et al. Chinese Herbal Medicine for Symptom Management in Cancer Palliative Care: Systematic Review And Meta-analysis. Medicine. 2016;95:e2793. doi: 10.1097/MD.0000000000002793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlson L.E., Angen M., Cullum J., Goodey E., Koopmans J., Lamont L., MacRae J.H., Martin M., Pelletier G., Robinson J., et al. High levels of untreated distress and fatigue in cancer patients. Br. J. Cancer. 2004;90:2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohandas H., Jaganathan S.K., Mani M.P., Ayyar M., Rohini Thevi G.V. Cancer-related fatigue treatment: An overview. J. Cancer Res. 2017;13:916–929. doi: 10.4103/jcrt.JCRT_50_17. [DOI] [PubMed] [Google Scholar]
- 5.Han Q.Q., Fu Y., Le J.M., Ma Y.J., Wei X.D., Ji H.L., Jiang H., Gao Y., Wu H. The Therapeutic Effects of Acupuncture and Electroacupuncture on Cancer-related Symptoms and Side-Effects. J. Cancer. 2021;12:7003–7009. doi: 10.7150/jca.55803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li S., So T.-H., Tang G., Tan H.-Y., Wang N., Ng B.F.L., Chan C.K.W., Yu E.C.-L., Feng Y. Chinese Herbal Medicine for Reducing Chemotherapy-Associated Side-Effects in Breast Cancer Patients: A Systematic Review and Meta-Analysis. Front. Oncol. 2020;10:599073. doi: 10.3389/fonc.2020.599073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mori-Vogt S., Blazer M. Palonosetron for the prevention of chemotherapy-induced nausea and vomiting. Expert Rev. Anticancer Ther. 2013;13:919–936. doi: 10.1586/14737140.2013.814412. [DOI] [PubMed] [Google Scholar]
- 8.Housman G., Byler S., Heerboth S., Lapinska K., Longacre M., Snyder N., Sarkar S. Drug resistance in cancer: An overview. Cancers. 2014;6:1769–1792. doi: 10.3390/cancers6031769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang X., Zhang H., Chen X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2019;2:141–160. doi: 10.20517/cdr.2019.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang K.L., Yu Y.C., Hsia S.M. Perspectives on the Role of Isoliquiritigenin in Cancer. Cancers. 2021;13:115. doi: 10.3390/cancers13010115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao T.T., Xu Y.Q., Hu H.M., Gong H.B., Zhu H.L. Isoliquiritigenin (ISL) and its Formulations: Potential Antitumor Agents. Curr. Med. Chem. 2019;26:6786–6796. doi: 10.2174/0929867325666181112091700. [DOI] [PubMed] [Google Scholar]
- 12.Chen H.Y., Chiang Y.F., Huang J.S., Huang T.C., Shih Y.H., Wang K.L., Ali M., Hong Y.H., Shieh T.M., Hsia S.M. Isoliquiritigenin Reverses Epithelial-Mesenchymal Transition Through Modulation of the TGF-beta/Smad Signaling Pathway in Endometrial Cancer. Cancers. 2021;13:1236. doi: 10.3390/cancers13061236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin P.H., Chiang Y.F., Shieh T.M., Chen H.Y., Shih C.K., Wang T.H., Wang K.L., Huang T.C., Hong Y.H., Li S.C., et al. Dietary Compound Isoliquiritigenin, an Antioxidant from Licorice, Suppresses Triple-Negative Breast Tumor Growth via Apoptotic Death Program Activation in Cell and Xenograft Animal Models. Antioxidants. 2020;9:228. doi: 10.3390/antiox9030228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang K.L., Hsia S.M., Chan C.J., Chang F.Y., Huang C.Y., Bau D.T., Wang P.S. Inhibitory effects of isoliquiritigenin on the migration and invasion of human breast cancer cells. Expert Opin. Ther. Targets. 2013;17:337–349. doi: 10.1517/14728222.2013.756869. [DOI] [PubMed] [Google Scholar]
- 15.Wu C.H., Chen H.Y., Wang C.W., Shieh T.M., Huang T.C., Lin L.C., Wang K.L., Hsia S.M. Isoliquiritigenin induces apoptosis and autophagy and inhibits endometrial cancer growth in mice. Oncotarget. 2016;7:73432–73447. doi: 10.18632/oncotarget.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim D.H., Kim J.S., Kim J., Jeong J.K., Son H.S., Park S.E., Jo J., Ryu S.M., Kim E.S., Lee S.J., et al. Therapeutic Effects of Licorice and Dried Ginger Decoction on Activity-Based Anorexia in BALB/c AnNCrl Mice. Front. Pharm. 2020;11:594706. doi: 10.3389/fphar.2020.594706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deutch M.R., Grimm D., Wehland M., Infanger M., Krüger M. Bioactive Candy: Effects of Licorice on the Cardiovascular System. Foods. 2019;8:495. doi: 10.3390/foods8100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pastorino G., Cornara L., Soares S., Rodrigues F., Oliveira M. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phytother. Res. 2018;32:2323–2339. doi: 10.1002/ptr.6178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Q., Ye M. Chemical analysis of the Chinese herbal medicine Gan-Cao (licorice) J. Chromatogr. A. 2009;1216:1954–1969. doi: 10.1016/j.chroma.2008.07.072. [DOI] [PubMed] [Google Scholar]
- 20.Ong E.S., Len S.M. Pressurized hot water extraction of berberine, baicalein and glycyrrhizin in medicinal plants. Anal. Chim. Acta. 2003;482:81–89. doi: 10.1016/S0003-2670(03)00196-X. [DOI] [Google Scholar]
- 21.Charpe T., Rathod V. Extraction of glycyrrhizic acid from licorice root using ultrasound: Process intensification studies. Chem. Eng. Processing Process Intensif. 2012;54:37–41. doi: 10.1016/j.cep.2012.01.002. [DOI] [Google Scholar]
- 22.Cui Y.M., Yu L.J., Ao M.Z., Yang Y., Hu J. [Studies on flavonoids extraction technology from Glycyrrhiza inflata and their bacteriostatic activities] Zhong Yao Cai. 2006;29:838–841. [PubMed] [Google Scholar]
- 23.The People’s Republic of China . Pharmacopoeia of the People’s Republic of China. China Medical Science Press; Beijing, China: 2010. [Google Scholar]
- 24.Yang R., Yuan B.C., Ma Y.S., Zhou S., Liu Y. The anti-inflammatory activity of licorice, a widely used Chinese herb. Pharm. Biol. 2017;55:5–18. doi: 10.1080/13880209.2016.1225775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tao W., Duan J., Zhao R., Li X., Yan H., Li J., Guo S., Yang N., Tang Y. Comparison of three officinal Chinese pharmacopoeia species of Glycyrrhiza based on separation and quantification of triterpene saponins and chemometrics analysis. Food Chem. 2013;141:1681–1689. doi: 10.1016/j.foodchem.2013.05.073. [DOI] [PubMed] [Google Scholar]
- 26.Zhu Z., Tao W., Li J., Guo S., Qian D., Shang E., Su S., Duan J.A. Rapid determination of flavonoids in licorice and comparison of three licorice species. J. Sep. Sci. 2016;39:473–482. doi: 10.1002/jssc.201500685. [DOI] [PubMed] [Google Scholar]
- 27.Xie J., Zhang Y., Wang W., Hou J. Identification and Simultaneous Determination of Glycyrrhizin, Formononetin, Glycyrrhetinic Acid, Liquiritin, Isoliquiritigenin, and Licochalcone A in Licorice by LC-MS/MS. Acta Chromatogr. 2014;26:507–516. doi: 10.1556/AChrom.26.2014.3.9. [DOI] [Google Scholar]
- 28.Kondo K., Shiba M., Nakamura R., Morota T., Shoyama Y. Constituent properties of licorices derived from Glycyrrhiza uralensis, G. glabra, or G. inflata identified by genetic information. Biol. Pharm. Bull. 2007;30:1271–1277. doi: 10.1248/bpb.30.1271. [DOI] [PubMed] [Google Scholar]
- 29.Song W., Qiao X., Chen K., Wang Y., Ji S., Feng J., Li K., Lin Y., Ye M. Biosynthesis-Based Quantitative Analysis of 151 Secondary Metabolites of Licorice to Differentiate Medicinal Glycyrrhiza Species and Their Hybrids. Anal. Chem. 2017;89:3146–3153. doi: 10.1021/acs.analchem.6b04919. [DOI] [PubMed] [Google Scholar]
- 30.Li G., Nikolic D., van Breemen R.B. Identification and Chemical Standardization of Licorice Raw Materials and Dietary Supplements Using UHPLC-MS/MS. J. Agric. Food Chem. 2016;64:8062–8070. doi: 10.1021/acs.jafc.6b02954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nomura T., Fukai T. Phenolic constituents of licorice (Glycyrrhiza species) Fortschr. Chem. Org. Nat. 1998;73:1–140. doi: 10.1007/978-3-7091-6480-8_1. [DOI] [PubMed] [Google Scholar]
- 32.Yang R., Li W., Yuan B., Ren G., Wang L., Cheng T., Liu Y. The genetic and chemical diversity in three original plants of licorice, Glycyrriza uralensis Fisch., Glycyrrhiza inflata Bat. and Glycyrrhiza glabra L. Pak. J. Pharm. Sci. 2018;31:525–535. [PubMed] [Google Scholar]
- 33.Li J.Y., Cao H.Y., Liu P., Cheng G.H., Sun M.Y. Glycyrrhizic acid in the treatment of liver diseases: Literature review. Biomed. Res. Int. 2014;2014:872139. doi: 10.1155/2014/872139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shin Y.W., Bae E.A., Lee B., Lee S.H., Kim J.A., Kim Y.S., Kim D.H. In vitro and in vivo antiallergic effects of Glycyrrhiza glabra and its components. Planta. Med. 2007;73:257–261. doi: 10.1055/s-2007-967126. [DOI] [PubMed] [Google Scholar]
- 35.Fuhrman B., Volkova N., Kaplan M., Presser D., Attias J., Hayek T., Aviram M. Antiatherosclerotic effects of licorice extract supplementation on hypercholesterolemic patients: Increased resistance of LDL to atherogenic modifications, reduced plasma lipid levels, and decreased systolic blood pressure. Nutrition. 2002;18:268–273. doi: 10.1016/S0899-9007(01)00753-5. [DOI] [PubMed] [Google Scholar]
- 36.Hajiaghamohammadi A.A., Zargar A., Oveisi S., Samimi R., Reisian S. To evaluate of the effect of adding licorice to the standard treatment regimen of Helicobacter pylori. Braz. J. Infect. Dis. 2016;20:534–538. doi: 10.1016/j.bjid.2016.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Madisch A., Holtmann G., Mayr G., Vinson B., Hotz J. Treatment of functional dyspepsia with a herbal preparation. A double-blind, randomized, placebo-controlled, multicenter trial. Digestion. 2004;69:45–52. doi: 10.1159/000076546. [DOI] [PubMed] [Google Scholar]
- 38.Chigurupati H., Auddy B., Biyani M., Stohs S.J. Hepatoprotective Effects of a Proprietary Glycyrrhizin Product during Alcohol Consumption: A Randomized, Double-Blind, Placebo-Controlled, Crossover Study. Phytother. Res. 2016;30:1943–1953. doi: 10.1002/ptr.5699. [DOI] [PubMed] [Google Scholar]
- 39.Najafi S., Koujan S.E., Manifar S., Kharazifard M.J., Kidi S., Hajheidary S. Preventive Effect of Glycyrrhiza Glabra Extract on Oral Mucositis in Patients Under Head and Neck Radiotherapy: A Randomized Clinical Trial. J. Dent. 2017;14:267–274. [PMC free article] [PubMed] [Google Scholar]
- 40.Mamgain R.K., Gupta M., Mamgain P., Verma S.K., Pruthi D.S., Kandwal A., Saini S. The efficacy of an ayurvedic preparation of yashtimadhu (Glycyrrhiza glabra) on radiation-induced mucositis in head-and-neck cancer patients: A pilot study. J. Cancer Res. Ther. 2020;16:458–462. doi: 10.4103/jcrt.JCRT_831_16. [DOI] [PubMed] [Google Scholar]
- 41.Pakravan F., Salehabad N.H., Karimi F., Isfahani M.N. Comparative Study of the Effect of Licorice Muco-adhesive Film on Radiotherapy Induced Oral Mucositis, A Randomized Controlled Clinical Trial. Gulf J. Oncol. 2021;1:42–47. [PubMed] [Google Scholar]
- 42.Ruetzler K., Fleck M., Nabecker S., Pinter K., Landskron G., Lassnigg A., You J., Sessler D.I. A randomized, double-blind comparison of licorice versus sugar-water gargle for prevention of postoperative sore throat and postextubation coughing. Anesth. Analg. 2013;117:614–621. doi: 10.1213/ANE.0b013e318299a650. [DOI] [PubMed] [Google Scholar]
- 43.Qiao X., Liu C.F., Ji S., Lin X.H., Guo D.A., Ye M. Simultaneous determination of five minor coumarins and flavonoids in Glycyrrhiza uralensis by solid-phase extraction and high-performance liquid chromatography/electrospray ionization tandem mass spectrometry. Planta Med. 2014;80:237–242. doi: 10.1055/s-0033-1360272. [DOI] [PubMed] [Google Scholar]
- 44.Rizzato G., Scalabrin E., Radaelli M., Capodaglio G., Piccolo O. A new exploration of licorice metabolome. Food Chem. 2017;221:959–968. doi: 10.1016/j.foodchem.2016.11.068. [DOI] [PubMed] [Google Scholar]
- 45.Yang R., Li W.D., Yuan B.C., Ma Y., Zhou S., Liu C.S., Liu Y. Simultaneous determination of 18 α-glycyrrhizic acid and 18 β-glycyrrhizic acid in three licorice samples from different origin by HPLC. Pharm. Anal. 2016;36:1065–1071. [Google Scholar]
- 46.Liao W.C., Lin Y.H., Chang T.M., Huang W.Y. Identification of two licorice species, Glycyrrhiza uralensis and Glycyrrhiza glabra, based on separation and identification of their bioactive components. Food Chem. 2012;132:2188–2193. doi: 10.1016/j.foodchem.2011.12.051. [DOI] [Google Scholar]
- 47.Farag M.A., Porzel A., Wessjohann L.A. Comparative metabolite profiling and fingerprinting of medicinal licorice roots using a multiplex approach of GC-MS, LC-MS and 1D NMR techniques. Phytochemistry. 2012;76:60–72. doi: 10.1016/j.phytochem.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 48.Wei L., Song X.B., Sun C.R., Xia Q. Content determination of polysaccharides in Radix Glycyrrhizae from three different species. Tianjin J. Tradit. Chin. Med. 2013;30:47–49. [Google Scholar]
- 49.Zhao L., Cheng Z.M., Shu-Yong M.U., Zhu J.W., Pan H.X. Content of Glycyrrhizic Acid and Polysaccharide of Cultivated Glycyrrhiza Root. Arid Land Geogr. 2005;28:843–848. [Google Scholar]
- 50.Fu Y., Chen J., Li Y.J., Zheng Y.F., Li P. Antioxidant and anti-inflammatory activities of six flavonoids separated from licorice. Food Chem. 2013;141:1063–1071. doi: 10.1016/j.foodchem.2013.03.089. [DOI] [PubMed] [Google Scholar]
- 51.Ito A., Munakata K., Imazu Y., Watanabe K. First nationwide attitude survey of Japanese physicians on the use of traditional Japanese medicine (kampo) in cancer treatment. Evid. Based Complement. Altern. Med. 2012;2012:957082. doi: 10.1155/2012/957082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Watanabe K., Matsuura K., Gao P., Hottenbacher L., Tokunaga H., Nishimura K., Imazu Y., Reissenweber H., Witt C.M. Traditional Japanese Kampo Medicine: Clinical Research between Modernity and Traditional Medicine-The State of Research and Methodological Suggestions for the Future. Evid. Based Complement. Altern. Med. 2011;2011:513842. doi: 10.1093/ecam/neq067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qi F., Li A., Inagaki Y., Gao J., Li J., Kokudo N., Li X.K., Tang W. Chinese herbal medicines as adjuvant treatment during chemo- or radio-therapy for cancer. Biosci. Trends. 2010;4:297–307. [PubMed] [Google Scholar]
- 54.Wang Z., Qi F., Cui Y., Zhao L., Sun X., Tang W., Cai P. An update on Chinese herbal medicines as adjuvant treatment of anticancer therapeutics. Biosci. Trends. 2018;12:220–239. doi: 10.5582/bst.2018.01144. [DOI] [PubMed] [Google Scholar]
- 55.Ehrman T.M., Barlow D.J., Hylands P.J. Phytochemical Informatics of Traditional Chinese Medicine and Therapeutic Relevance. J. Chem. Inf. Modeling. 2007;47:2316–2334. doi: 10.1021/ci700155t. [DOI] [PubMed] [Google Scholar]
- 56.Guldiken B., Ozkan G., Catalkaya G., Ceylan F.D., Ekin Yalcinkaya I., Capanoglu E. Phytochemicals of herbs and spices: Health versus toxicological effects. Food Chem. Toxicol. 2018;119:37–49. doi: 10.1016/j.fct.2018.05.050. [DOI] [PubMed] [Google Scholar]
- 57.Njeru S., Matasyohb J., Mwanikic C., Maina M., Kobiad G. A Review of some Phytochemicals commonly found in Medicinal Plants. Int. J. Med. Plants. 2013;105:135–140. [Google Scholar]
- 58.Miyoshi A. The clinical effect of Tsumura Daio-kanzo-to extract granules for ethical use (TJ-84) by double blind test against the constipation. Gastroenterology. 1994;18:14. [Google Scholar]
- 59.Takayama K., Takahara C., Tabuchi N., Okamura N. Daiokanzoto (Da-Huang-Gan-Cao-Tang) is an effective laxative in gut microbiota associated with constipation. Sci. Rep. 2019;9:3833. doi: 10.1038/s41598-019-40278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kon R., Yamamura M., Matsunaga Y., Kimura H., Minami M., Kato S., Ikarashi N., Sugiyama K. Laxative effect of repeated Daiokanzoto is attributable to decrease in aquaporin-3 expression in the colon. J. Nat. Med. 2018;72:493–502. doi: 10.1007/s11418-018-1174-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moriyama S., Hinode D., Yoshioka M., Sogawa Y., Nishino T., Tangoku A., Grenier D. Impact of the use of Kampo medicine in patients with esophageal cancer during chemotherapy:a clinical trial for oral hygiene and oral condition. J. Med. Investig. 2018;65:184–190. doi: 10.2152/jmi.65.184. [DOI] [PubMed] [Google Scholar]
- 62.Wang S., Chen P., Xu Y., Li X., Fan X. Characterization of the chemical constituents in Da-Huang-Gan-Cao-Tang by liquid chromatography coupled with quadrupole time-of-flight tandem mass spectrometry and liquid chromatography coupled with ion trap mass spectrometry. J. Sep. Sci. 2014;37:1748–1761. doi: 10.1002/jssc.201400061. [DOI] [PubMed] [Google Scholar]
- 63.Chen Q., Xiao S., Li Z., Ai N., Fan X. Chemical and Metabolic Profiling of Si-Ni Decoction Analogous Formulae by High performance Liquid Chromatography-Mass Spectrometry. Sci. Rep. 2015;5:11638. doi: 10.1038/srep11638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miyoshi A. The clinical effect of TSUMURA Daio-Kanzo-to Extract Granules for ethical use (TJ-84) against the constipation based on the new standard. Gastroenterology. 1996;22:314–328. [Google Scholar]
- 65.Matsui E., Takayama K., Sato E., Okamura N. The influence of glycyrrhiza and antibiotics on the purgative action of sennoside a from Daiokanzoto in mice. Biol. Pharm. Bull. 2011;34:1438–1442. doi: 10.1248/bpb.34.1438. [DOI] [PubMed] [Google Scholar]
- 66.Yoshida K., Yoshioka M., Okamura H., Moriyama S., Kawazoe K., Grenier D., Hinode D. Preventive effect of Daiokanzoto (TJ-84) on 5-fluorouracil-induced human gingival cell death through the inhibition of reactive oxygen species production. PLoS ONE. 2014;9:e112689. doi: 10.1371/journal.pone.0112689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang S., Yu S., Liu J., Yuan H., Qiao H. The Effect of Observation Rhubarb Licorice Decoction on Chemotherapy Vomiting. Pract. Clin. J. Integr. Tradit. Chin. West. Med. 2020;20:6–8. doi: 10.13638/j.issn.1671-4040.2020.10.003. [DOI] [Google Scholar]
- 68.Pan L., Wang J., Huang Y., Cao C., Liu Z., Qian Z., Xu X., Ge X., Hu R., Ge T. Effect of Dahuang Gancao Recipe and acupoInt. application on gastrointestinal reaction induced by chemotherapy for NSCLC. Chin. Med. Clin. 2021;21:2918–2922. doi: 10.11655/zgywylc2021.17.003. [DOI] [Google Scholar]
- 69.Yoshida A., Hirose T., Kuroda A., Mitsuoka M., Shinoda Y., Mori K., Kawachi Y., Tanaka K., Takeda A., Sugiyama T., et al. Evaluation and Comparison of Daiokanzoto and Lubiprostone for Constipation: A Retrospective Cohort Study. Biol. Pharm. Bull. 2019;42:680–684. doi: 10.1248/bpb.b18-00532. [DOI] [PubMed] [Google Scholar]
- 70.Fournier-Larente J., Azelmat J., Yoshioka M., Hinode D., Grenier D. The Daiokanzoto (TJ-84) Kampo Formulation Reduces Virulence Factor Gene Expression in Porphyromonas gingivalis and Possesses Anti-Inflammatory and Anti-Protease Activities. PLoS ONE. 2016;11:e0148860. doi: 10.1371/journal.pone.0148860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nguyen H., Sangha S., Pan M., Shin D.H., Park H., Mohammed A.I., Cirillo N. Oxidative Stress and Chemoradiation-Induced Oral Mucositis: A Scoping Review of In Vitro, In Vivo and Clinical Studies. Int. J. Mol. Sci. 2022;23:4863. doi: 10.3390/ijms23094863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim D.S., Roh J.H., Cho C.W., Ma J.-Y. Analysis of Bioconversion Compositions from Fermented Bojungikki-tangs. YAKHAK HOEJI. 2011;55:361–366. [Google Scholar]
- 73.Yu N., Xiong Y., Wang C. Bu-Zhong-Yi-Qi Decoction, the Water Extract of Chinese Traditional Herbal Medicine, Enhances Cisplatin Cytotoxicity in A549/DDP Cells through Induction of Apoptosis and Autophagy. BioMed Res Int. 2017;2017:3692797. doi: 10.1155/2017/3692797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gou H., Gu L.Y., Shang B.Z., Xiong Y., Wang C. Protective effect of Bu-Zhong-Yi-Qi decoction, the water extract of Chinese traditional herbal medicine, on 5-fluorouracil-induced intestinal mucositis in mice. Hum. Exp. Toxicol. 2016;35:1243–1251. doi: 10.1177/0960327115627686. [DOI] [PubMed] [Google Scholar]
- 75.Kuroda M., Kotake T., Sonoda T., Maekawa M., Okajima E., Okawa T., Ikoma F., Kurita T., Nakamura T., Itatani H., et al. The clinical evaluation of hochuekkito for symptoms of malignant neoplasm patients. Hinyokika Kiyo. 1985;31:173–177. [PubMed] [Google Scholar]
- 76.Jeong J.S., Ryu B.H., Kim J.S., Park J.W., Choi W.C., Yoon S.W. Bojungikki-tang for cancer-related fatigue: A pilot randomized clinical trial. Integr. Cancer Ther. 2010;9:331–338. doi: 10.1177/1534735410383170. [DOI] [PubMed] [Google Scholar]
- 77.Xu R., Wu J., Zhang X., Zou X., Li C., Wang H., Yuan M., Chen M., Sun Q., Liu S. Modified Bu-zhong-yi-qi decoction synergies with 5 fluorouracile to inhibits gastric cancer progress via PD-1/PD- L1-dependent T cell immunization. Pharm. Res. 2020;152:104623. doi: 10.1016/j.phrs.2019.104623. [DOI] [PubMed] [Google Scholar]
- 78.Yae S., Takahashi F., Yae T., Yamaguchi T., Tsukada R., Koike K., Minakata K., Murakami A., Nurwidya F., Kato M., et al. Hochuekkito (TJ-41), a Kampo Formula, Ameliorates Cachexia Induced by Colon 26 Adenocarcinoma in Mice. Evid. Based Complement. Altern. Med. 2012;2012:976926. doi: 10.1155/2012/976926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Satoh N., Sakai S., Kogure T., Tahara E., Origasa H., Shimada Y., Kohoda K., Okubo T., Terasawa K. A randomized double blind placebo-controlled clinical trial of Hochuekkito, a traditional herbal medicine, in the treatment of elderly patients with weakness N of one and responder restricted design. Phytomedicine. 2005;12:549–554. doi: 10.1016/j.phymed.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 80.Shin H.Y., Shin C.H., Shin T.Y., Lee E.J., Kim H.M. Effect of bojungikki-tang on lipopolysaccharide-induced cytokine production from peripheral blood mononuclear cells of chronic fatigue syndrome patients. Immunopharmacol. Immunotoxicol. 2003;25:491–501. doi: 10.1081/IPH-120026435. [DOI] [PubMed] [Google Scholar]
- 81.Ishiura Y., Yamamoto H., Shiba Y., Terasaki Y., Ishida Y., Tanikawa F., Hayase H., Maruyama K., Obata C., Ishikawa M., et al. Effect of Japanese traditional medicine, TJ-41, on quality of life of patients with non-small cell lung cancer receiving outpatient chemotherapy. Gan Kagaku Ryoho. 2013;40:913–916. [PubMed] [Google Scholar]
- 82.Liu D., Ou Y., Deng X., Dai P., Luo Q., Yi M. Effect analysis of chemotherapy combined with Buzhong Yiqi Decoction in the treatment of advanced non-small cell lung cancer. Chin. Community Dr. 2021;11:90–91. doi: 10.3969/j.issn.1007-614x.2021.11.042. [DOI] [Google Scholar]
- 83.Cai L. Observation of clinical efficacy and immune function of buzhong yiqi tang combined with radiotherapy and chemotherapy in patients with advanced non-small cell lung cancer. China Health Care Nutr. 2021;31:262. [Google Scholar]
- 84.Wen B., Jiang J.-P. Clinical outcomes observations: Combined Buzhong Yiqi with Chemotherapy in advanced gastric cancer. Home Med. 2019;10:109. [Google Scholar]
- 85.Hongmin C. Effect of Buzhong Yiqi Decoction Combined with XELOX in the Treatment of Advanced Gastric Cancer. Henan Med. Res. 2021;30:4160–4162. doi: 10.3969/j.issn.1004-437X.2021.22.041. [DOI] [Google Scholar]
- 86.Du H.-T. Clinical effect of Buzhong Yiqi Decoction Combined with capecitabine and oxaliplatin chemotherapy in the treatment of advanced gastric cancer patients. Cap. Med. 2021;28:156–157. doi: 10.3969/j.issn.1005-8257.2021.15.080. [DOI] [Google Scholar]
- 87.Qianshan Z., Lei L. Effect of Buzhong Yiqi Decoction Combined with Yiwei Decoction on the Efficacy and Quality of Life for Patients with Advanced Gastric Cancer Receiving Palliative Chemotherapy. J. Sichuan Tradit. Chin. Med. 2021;39:93–96. [Google Scholar]
- 88.Kexin G., Xiaokang W., Lixia L., Hongtao W. Effect of Buzhong Yiqi Guben Tang on Adverse Reactions and Quality of Life of Patients with Syndrome of Spleen-Qi Deficiency After Chemotherapy. J. New Chin. Med. 2021;53:109–113. doi: 10.13457/j.cnki.jncm.2021.20.027. [DOI] [Google Scholar]
- 89.Wang Z.-X., Li X. Clinical stuy: Combined Buzhong Yiqi with chemotherapy in advanced colon cancer. Shaanxi J. Tradit. Chin. Med. 2020;41:1414–1417. doi: 10.3969/j.issn.1000-7369.2020.10.020. [DOI] [Google Scholar]
- 90.Okabe H., Kinjo Y., Obama K., Hosogi H., Hata H., Asao Y., Harada H., Manaka D., Itami A., Teramukai S., et al. A Randomized Phase II Study of S-1 Adjuvant Chemotherapy With or Without Hochu-ekki-to, a Japanese Herbal Medicine, for Stage II/III Gastric Cancer: The KUGC07 (SHOT) Trial. Front. Oncol. 2019;9:294. doi: 10.3389/fonc.2019.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Qiu H., Zhou Y., Zhao Y., Zhang Y., Zheng J., Hou E. Meta-analysis of Efficacy and Side Effects of Buzhong Yiqi Decoction Combined with Platinum Chemotherapy for Advanced Non-Small Cell Lung Cancer. J. Pract. Tradit. Chin. Intern. Med. 2021;35:32–36. doi: 10.13729/j.issn.1671-7813.Z20201288. [DOI] [Google Scholar]
- 92.Fareed J., Walenga J.M., Baker W.H., Hayes A., Hoppensteadt D.A. Molecular markers of hemostatic activation in atherosclerosis: A new concept in diagnostic profiling of endogenous pathophysiologic transition. Semin. Thromb. Hemost. 1986;12:102–109. doi: 10.1055/s-2007-1003542. [DOI] [PubMed] [Google Scholar]
- 93.Freiman D.G. The pathology of sarcoidosis. Semin. Roentgenol. 1985;20:327–339. doi: 10.1016/0037-198X(85)90041-0. [DOI] [PubMed] [Google Scholar]
- 94.Mogami S., Sadakane C., Nahata M., Mizuhara Y., Yamada C., Hattori T., Takeda H. CRF receptor 1 antagonism and brain distribution of active components contribute to the ameliorative effect of rikkunshito on stress-induced anorexia. Sci. Rep. 2016;6:27516. doi: 10.1038/srep27516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Takeda H., Sadakane C., Hattori T., Katsurada T., Ohkawara T., Nagai K., Asaka M. Rikkunshito, an herbal medicine, suppresses cisplatin-induced anorexia in rats via 5-HT2 receptor antagonism. Gastroenterology. 2008;134:2004–2013. doi: 10.1053/j.gastro.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 96.Fujitsuka N., Asakawa A., Hayashi M., Sameshima M., Amitani H., Kojima S., Fujimiya M., Inui A. Selective serotonin reuptake inhibitors modify physiological gastrointestinal motor activities via 5-HT2c receptor and acyl ghrelin. Biol. Psychiatry. 2009;65:748–759. doi: 10.1016/j.biopsych.2008.10.031. [DOI] [PubMed] [Google Scholar]
- 97.Sadakane C., Muto S., Nakagawa K., Ohnishi S., Saegusa Y., Nahata M., Hattori T., Asaka M., Takeda H. 10-Gingerol, a component of rikkunshito, improves cisplatin-induced anorexia by inhibiting acylated ghrelin degradation. Biochem. Biophys. Res. Commun. 2011;412:506–511. doi: 10.1016/j.bbrc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 98.Yamada C., Saegusa Y., Nakagawa K., Ohnishi S., Muto S., Nahata M., Sadakane C., Hattori T., Sakamoto N., Takeda H. Rikkunshito, a Japanese kampo medicine, ameliorates decreased feeding behavior via ghrelin and serotonin 2B receptor signaling in a novelty stress murine model. BioMed Res. Int. 2013;2013:792940. doi: 10.1155/2013/792940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yamada C., Hattori T., Ohnishi S., Takeda H. Ghrelin Enhancer, the Latest Evidence of Rikkunshito. Front. Nutr. 2021;8:761631. doi: 10.3389/fnut.2021.761631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tominaga K., Kato M., Takeda H., Shimoyama Y., Umegaki E., Iwakiri R., Furuta K., Sakurai K., Odaka T., Kusunoki H., et al. A randomized, placebo-controlled, double-blind clinical trial of rikkunshito for patients with non-erosive reflux disease refractory to proton-pump inhibitor: The G-PRIDE study. J. Gastroenterol. 2014;49:1392–1405. doi: 10.1007/s00535-013-0896-9. [DOI] [PubMed] [Google Scholar]
- 101.Nakamura M., Nakamori M., Ojima T., Katsuda M., Hayata K., Iwahashi M., Yamaue H. The effects of rikkunshito on body weight loss after esophagectomy. J. Surg. Res. 2016;204:130–138. doi: 10.1016/j.jss.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 102.Suzuki H., Matsuzaki J., Fukushima Y., Suzaki F., Kasugai K., Nishizawa T., Naito Y., Hayakawa T., Kamiya T., Andoh T., et al. Randomized clinical trial: Rikkunshito in the treatment of functional dyspepsia—A multicenter, double-blind, randomized, placebo-controlled study. Neurogastroenterol. Motil. 2014;26:950–961. doi: 10.1111/nmo.12348. [DOI] [PubMed] [Google Scholar]
- 103.Tominaga K., Sakata Y., Kusunoki H., Odaka T., Sakurai K., Kawamura O., Nagahara A., Takeuchi T., Fujikawa Y., Oshima T., et al. Rikkunshito simultaneously improves dyspepsia correlated with anxiety in patients with functional dyspepsia: A randomized clinical trial (the DREAM study) Neurogastroenterol. Motil. 2018;30:e13319. doi: 10.1111/nmo.13319. [DOI] [PubMed] [Google Scholar]
- 104.Ko M.-H., Song S.-Y., Ha S.-J., Lee J.Y., Yoon S.W., Park J.-H., Park S.-J., Yoo H.-S. Efficacy and Safety of Yukgunja-Tang for Patients with Cancer-related Anorexia: A Randomized, Controlled Trial, Pilot Study. Integr. Cancer Ther. 2021;20:15347354211019107. doi: 10.1177/15347354211019107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kang H.-J., Jeong M.-K., Park S.-J., Jun H.-J., Yoo H.-S. Efficacy and safety of Yukgunja-Tang for treating anorexia in patients with cancer: The protocol for a pilot, randomized, controlled trial. Medicine. 2019;98:e16950. doi: 10.1097/MD.0000000000016950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hofman M., Morrow G.R., Roscoe J.A., Hickok J.T., Mustian K.M., Moore D.F., Wade J.L., Fitch T.R. Cancer patients’ expectations of experiencing treatment-related side effects: A University of Rochester Cancer Center-Community Clinical Oncology Program study of 938 patients from community practices. Cancer. 2004;101:851–857. doi: 10.1002/cncr.20423. [DOI] [PubMed] [Google Scholar]
- 107.Hesketh P.J., Grunberg S.M., Gralla R.J., Warr D.G., Roila F., de Wit R., Chawla S.P., Carides A.D., Ianus J., Elmer M.E., et al. The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: A multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin--the Aprepitant Protocol 052 Study Group. J. Clin. Oncol. 2003;21:4112–4119. doi: 10.1200/jco.2003.01.095. [DOI] [PubMed] [Google Scholar]
- 108.Yakabi K., Kurosawa S., Tamai M., Yuzurihara M., Nahata M., Ohno S., Ro S., Kato S., Aoyama T., Sakurada T., et al. Rikkunshito and 5-HT2C receptor antagonist improve cisplatin-induced anorexia via hypothalamic ghrelin interaction. Regul. Pept. 2010;161:97–105. doi: 10.1016/j.regpep.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 109.Oteki T., Ishikawa A., Sasaki Y., Ohara G., Kagohashi K., Kurishima K., Satoh H. Effect of rikkunshi-to treatment on chemotherapy-induced appetite loss in patients with lung cancer: A prospective study. Exp. Ther. Med. 2016;11:243–246. doi: 10.3892/etm.2015.2903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tominaga K., Kido T., Ochi M., Sadakane C., Mase A., Okazaki H., Yamagami H., Tanigawa T., Watanabe K., Watanabe T., et al. The Traditional Japanese Medicine Rikkunshito Promotes Gastric Emptying via the Antagonistic Action of the 5-HT(3) Receptor Pathway in Rats. Evid. Based Complement. Altern. Med. 2011;2011:248481. doi: 10.1093/ecam/nep173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ohnishi S., Watari H., Kanno M., Ohba Y., Takeuchi S., Miyaji T., Oyamada S., Nomura E., Kato H., Sugiyama T., et al. Additive effect of rikkunshito, an herbal medicine, on chemotherapy-induced nausea, vomiting, and anorexia in uterine cervical or corpus cancer patients treated with cisplatin and paclitaxel: Results of a randomized phase II study (JORTC KMP-02) J. Gynecol. Oncol. 2017;28:e44. doi: 10.3802/jgo.2017.28.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ohno T., Yanai M., Ando H., Toyomasu Y., Ogawa A., Morita H., Ogata K., Mochiki E., Asao T., Kuwano H. Rikkunshito, a traditional Japanese medicine, suppresses cisplatin-induced anorexia in humans. Clin. Exp. Gastroenterol. 2011;4:291–296. doi: 10.2147/CEG.S26297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Seike J., Sawada T., Kawakita N., Yamamoto Y., Yuasa Y., Yamai H., Takachi H., Yoshida T., Tangoku A. A New Candidate Supporting Drug, Rikkunshito, for the QOL in Advanced Esophageal Cancer Patients with Chemotherapy Using Docetaxel/5-FU/CDDP. Int. J. Surg. Oncol. 2011;2011:715623. doi: 10.1155/2011/715623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Inoue T., Takagi H., Owada Y., Watanabe Y., Yamaura T., Fukuhara M., Muto S., Okabe N., Matsumura Y., Hasegawa T., et al. The efficacy of the Kampo medicine rikkunshito for chemotherapy-induced anorexia (RICH trial): Study protocol for a randomized controlled trial. Trials. 2017;18:485. doi: 10.1186/s13063-017-2227-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hamai Y., Yoshiya T., Hihara J., Emi M., Furukawa T., Yamakita I., Ibuki Y., Okada M. Traditional Japanese herbal medicine rikkunshito increases food intake and plasma acylated ghrelin levels in patients with esophageal cancer treated by cisplatin-based chemotherapy. J. Thorac. Dis. 2019;11:2470–2478. doi: 10.21037/jtd.2019.05.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yoshiya T., Ito M., Misumi K., Hanaki H., Tsutani Y., Satoh K., Miyata Y., Okada M. The effect of rikkunshito, a traditional Japanese herbal medicine, on food intake and plasma acylated ghrelin levels in lung cancer patients treated with platinum-based chemotherapy. Ann. Oncol. 2016;27:vi510. doi: 10.1093/annonc/mdw390.41. [DOI] [Google Scholar]
- 117.Yoshiya T., Mimae T., Ito M., Sasada S., Tsutani Y., Satoh K., Masuda T., Miyata Y., Hattori N., Okada M. Prospective, randomized, cross-over pilot study of the effects of Rikkunshito, a Japanese traditional herbal medicine, on anorexia and plasma-acylated ghrelin levels in lung cancer patients undergoing cisplatin-based chemotherapy. Investig. New Drugs. 2020;38:485–492. doi: 10.1007/s10637-019-00836-x. [DOI] [PubMed] [Google Scholar]
- 118.Xu C., Yu X., Li M. Clinical Observation of Advanced Colorectal Cancer Patients Treated with FOLFIRI Chemotherapy Combined with Chinese Herbs Xiangsha Liujunzi Soup. Chin. J. Clin. Med. 2012;19:36–37. doi: 10.3969/j.issn.1008-6358.2012.01.014. [DOI] [Google Scholar]
- 119.Koufeng S. Clinical observation of the add-substract liujunzi decoction on alleviating adverse reaction and enhancing immunity during postoperative chemotherapy for gastric cancer. J. Clin. Med. Pract. 2017;21:38–41. doi: 10.7619/jcmp.201703012. [DOI] [Google Scholar]
- 120.Wang L., Xie Z., Xiao H., Lv Q. Clinical Observation on Guishao Liujunzi Decoction in the Treatment of Cancer-Related Fatigue of Colorectal Cancer Patients. Chin. Med. Mod. Distance Educ. China. 2016;14:70–73. doi: 10.3969/j.issn.1672-2779.2016.21.029. [DOI] [Google Scholar]
- 121.Xin T., Chuan X., Min L., Xiaowei Y., Meihua F., Zhihui T. The Influence of Modified Xiangsha Liujunzi Decoction for Patients of Postoperative Colorectal Cancer on Quality of Life. J. Yunnan Univ. Tradit. Chin. Med. 2017;40:37–40. doi: 10.19288/j.cnki.issn.1000-2723.2017.01.009. [DOI] [Google Scholar]
- 122.Tao Z., Tong X., Xu W., Zhou Z., Jin Y., Xu Z., Li M., Yu X. Clinical Observation of Chinese Medicine Combined with Chemotherapy on Reducing Toxicity and Increasing Efficiency of Sequential Therapy in the Treatment Non-smallcell Lung Cancer. World Chin. Med. 2021;16:477–481, 486. doi: 10.3969/j.issn.1673-7202.2021.03.021. [DOI] [Google Scholar]
- 123.Tao S., Chen G., Yang M.Y., Deng S., Zhang J., Guo D.-A. Identification of the Major Constituents in Shi-Quan-Da-Bu Decoction by HPLC-ESI-MS/MS. Nat. Prod. Commun. 2008;3:1934578X0800300. doi: 10.1177/1934578X0800300506. [DOI] [Google Scholar]
- 124.Tsuchiya M., Kono H., Matsuda M., Fujii H., Rusyn I. Protective effect of Juzen-taiho-to on hepatocarcinogenesis is mediated through the inhibition of Kupffer cell-induced oxidative stress. Int. J. Cancer. 2008;123:2503–2511. doi: 10.1002/ijc.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Choi Y.K., Jung K.Y., Woo S.M., Yun Y.J., Jun C.Y., Park J.H., Shin Y.C., Cho S.G., Ko S.G. Effect of Sipjeondaebo-tang on cancer-induced anorexia and cachexia in CT-26 tumor-bearing mice. Mediat. Inflamm. 2014;2014:736563. doi: 10.1155/2014/736563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cheon C., Yoo J.-E., Yoo H.-S., Cho C.-K., Kang S., Kim M., Jang B.-H., Shin Y.-C., Ko S.-G. Efficacy and Safety of Sipjeondaebo-Tang for Anorexia in Patients with Cancer: A Pilot, Randomized, Double-Blind, Placebo-Controlled Trial. Evid. Based Complement. Altern. Med. 2017;2017:8780325. doi: 10.1155/2017/8780325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cheon C., Park S., Park Y.L., Huang C.W., Ko Y., Jang B.H., Shin Y.C., Ko S.G. Sipjeondaebo-tang in patients with cancer with anorexia: A protocol for a pilot, randomised, controlled trial. BMJ Open. 2016;6:e011212. doi: 10.1136/bmjopen-2016-011212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nakamoto H., Mimura T., Honda N. Orally administrated Juzen-taiho-to/TJ-48 ameliorates erythropoietin (rHuEPO)-resistant anemia in patients on hemodialysis. Hemodial. Int. 2008;12((Suppl. 2)):S9–S14. doi: 10.1111/j.1542-4758.2008.00317.x. [DOI] [PubMed] [Google Scholar]
- 129.Ikemoto T., Shimada M., Iwahashi S., Saito Y., Kanamoto M., Mori H., Morine Y., Imura S., Utsunomiya T. Changes of immunological parameters with administration of Japanese Kampo medicine (Juzen-Taihoto/TJ-48) in patients with advanced pancreatic cancer. Int. J. Clin. Oncol. 2014;19:81–86. doi: 10.1007/s10147-013-0529-6. [DOI] [PubMed] [Google Scholar]
- 130.Cheon C., Kang S., Ko Y., Kim M., Jang B.H., Shin Y.C., Ko S.G. Sipjeondaebo-tang in patients with breast cancer with fatigue: A protocol for a pilot, randomised, double-blind, placebo-controlled, cross-over trial. BMJ Open. 2018;8:e021242. doi: 10.1136/bmjopen-2017-021242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ye M., Liu S.-H., Jiang Z., Lee Y., Tilton R., Cheng Y.-C. Liquid chromatography/mass spectrometry analysis of PHY906, a Chinese medicine formulation for cancer therapy. Rapid Commun. Mass Spectrom. 2007;21:3593–3607. doi: 10.1002/rcm.2832. [DOI] [PubMed] [Google Scholar]
- 132.Lam W., Jiang Z., Guan F., Huang X., Hu R., Wang J., Bussom S., Liu S.H., Zhao H., Yen Y., et al. PHY906(KD018), an adjuvant based on a 1800-year-old Chinese medicine, enhanced the anti-tumor activity of Sorafenib by changing the tumor microenvironment. Sci. Rep. 2015;5:9384. doi: 10.1038/srep09384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rockwell S., Grove T.A., Liu Y., Cheng Y.C., Higgins S.A., Booth C.J. Preclinical studies of the Chinese Herbal Medicine formulation PHY906 (KD018) as a potential adjunct to radiation therapy. Int. J. Radiat. Biol. 2013;89:16–25. doi: 10.3109/09553002.2012.717733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kummar S., Copur M.S., Rose M., Wadler S., Stephenson J., O’Rourke M., Brenckman W., Tilton R., Liu S.H., Jiang Z., et al. A phase I study of the chinese herbal medicine PHY906 as a modulator of irinotecan-based chemotherapy in patients with advanced colorectal cancer. Clin. Colorectal Cancer. 2011;10:85–96. doi: 10.1016/j.clcc.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 135.Saif M.W., Li J., Lamb L., Kaley K., Elligers K., Jiang Z., Bussom S., Liu S.H., Cheng Y.C. First-in-human phase II trial of the botanical formulation PHY906 with capecitabine as second-line therapy in patients with advanced pancreatic cancer. Cancer Chemother. Pharmacol. 2014;73:373–380. doi: 10.1007/s00280-013-2359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lam W., Bussom S., Guan F., Jiang Z., Zhang W., Gullen E.A., Liu S.H., Cheng Y.C. The four-herb Chinese medicine PHY906 reduces chemotherapy-induced gastrointestinal toxicity. Sci. Transl. Med. 2010;2:45ra59. doi: 10.1126/scitranslmed.3001270. [DOI] [PubMed] [Google Scholar]
- 137.Saif M.W., Lansigan F., Ruta S., Lamb L., Mezes M., Elligers K., Grant N., Jiang Z.L., Liu S.H., Cheng Y.C. Phase I study of the botanical formulation PHY906 with capecitabine in advanced pancreatic and other gastrointestinal malignancies. Phytomed. Int. J. Phytother. Phytopharm. 2010;17:161–169. doi: 10.1016/j.phymed.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 138.Yen Y., So S., Rose M., Saif M.W., Chu E., Liu S.H., Foo A., Jiang Z., Su T., Cheng Y.C. Phase I/II study of PHY906/capecitabine in advanced hepatocellular carcinoma. Anticancer Res. 2009;29:4083–4092. [PubMed] [Google Scholar]
- 139.Farrell M.P., Kummar S. Phase I/IIA randomized study of PHY906, a novel herbal agent, as a modulator of chemotherapy in patients with advanced colorectal cancer. Clin. Colorectal Cancer. 2003;2:253–256. doi: 10.3816/CCC.2003.n.007. [DOI] [PubMed] [Google Scholar]
- 140.Hoimes C.J., Lamb L., Ruta S., Elligers K., Mezes M., Grant N., Liu S., Lacy J., Cheng Y., Saif M.W. A phase I/II study of PHY906 plus capecitabine (CAP) in patients (pts) with advanced pancreatic cancer (APC) J. Clin. Oncol. 2008;26:15538. doi: 10.1200/jco.2008.26.15_suppl.15538. [DOI] [Google Scholar]
- 141.Liu S.H., Cheng Y.C. Old formula, new Rx: The journey of PHY906 as cancer adjuvant therapy. J. Ethnopharmacol. 2012;140:614–623. doi: 10.1016/j.jep.2012.01.047. [DOI] [PubMed] [Google Scholar]
- 142.Changou C.A., Shiah H.S., Chen L.T., Liu S., Luh F., Liu S.H., Cheng Y.C., Yen Y. A Phase II Clinical Trial on the Combination Therapy of PHY906 Plus Capecitabine in Hepatocellular Carcinoma. Oncologist. 2021;26:e367–e373. doi: 10.1002/onco.13582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hamada M., Fujii Y., Yamamoto H., Miyazawa Y., Shui S.M., Tung Y.C., Yamaguchi N. Effect of a kanpo medicine, zyuzentaihoto, on the immune reactivity of tumor-bearing mice. J. Ethnopharmacol. 1988;24:311–320. doi: 10.1016/0378-8741(88)90160-2. [DOI] [PubMed] [Google Scholar]
- 144.Saiki I. A Kampo medicine “Juzen-taiho-to”: Prevention of malignant progression and metastasis of tumor cells and the mechanism of action. Biol. Pharm. Bull. 2000;23:677–688. doi: 10.1248/bpb.23.677. [DOI] [PubMed] [Google Scholar]
- 145.Tatsumi K., Shinozuka N., Nakayama K., Sekiya N., Kuriyama T., Fukuchi Y. Hochuekkito improves systemic inflammation and nutritional status in elderly patients with chronic obstructive pulmonary disease. J. Am. Geriatr. Soc. 2009;57:169–170. doi: 10.1111/j.1532-5415.2009.02034.x. [DOI] [PubMed] [Google Scholar]
- 146.Lv L., Wang F.Y., Ma X.X., Li Z.H., Huang S.P., Shi Z.H., Ji H.J., Bian L.Q., Zhang B.H., Chen T., et al. Efficacy and safety of Xiangsha Liujunzi granules for functional dyspepsia: A multi-center randomized double-blind placebo-controlled clinical study. World J. Gastroenterol. 2017;23:5589–5601. doi: 10.3748/wjg.v23.i30.5589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Utumi Y., Iseki E., Murayama N., Nozawa M., Kumagai R., Matsubara Y., Ichimiya Y., Arai H. Effect of Rikkunshi-to on appetite loss found in elderly dementia patients: A preliminary study. Psychogeriatrics. 2011;11:34–39. doi: 10.1111/j.1479-8301.2010.00347.x. [DOI] [PubMed] [Google Scholar]
- 148.Naito T., Itoh H., Yasunaga F., Takeyama M. Rikkunshi-to raises levels of somatostatin and gastrin in human plasma. Biol. Pharm. Bull. 2001;24:841–843. doi: 10.1248/bpb.24.841. [DOI] [PubMed] [Google Scholar]
- 149.Qi F., Zhao L., Zhou A., Zhang B., Li A., Wang Z., Han J. The advantages of using traditional Chinese medicine as an adjunctive therapy in the whole course of cancer treatment instead of only terminal stage of cancer. BioSci. Trends. 2015;9:16–34. doi: 10.5582/bst.2015.01019. [DOI] [PubMed] [Google Scholar]
- 150.Fujitsuka N., Asakawa A., Uezono Y., Minami K., Yamaguchi T., Niijima A., Yada T., Maejima Y., Sedbazar U., Sakai T., et al. Potentiation of ghrelin signaling attenuates cancer anorexia-cachexia and prolongs survival. Transl. Psychiatry. 2011;1:e23. doi: 10.1038/tp.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Takaku S., Shimizu M., Takahashi H. Japanese Kampo Medicine Juzentaihoto Enhances Antitumor Immunity in CD1d(−/−) Mice Lacking NKT Cells. Integr. Cancer Ther. 2020;19:1534735419900798. doi: 10.1177/1534735419900798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Maeng C.H., Kim B.-H., Chon J., Kang W.S., Kang K., Woo M., Hong I.K., Lee J., Lee K.Y. Effect of multimodal intervention care on cachexia in patients with advanced cancer compared to conventional management (MIRACLE): An open-label, phase 2 trial. J. Clin. Oncol. 2021;39:TPS12134. doi: 10.1200/JCO.2021.39.15_suppl.TPS12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lee J.Y., Kim E.H., Yoon J.-H., Eo W., Yoon S.W. Traditional Herbal Medicine, Sipjeondaebo-Tang, for Cancer-Related Fatigue: A Randomized, Placebo-Controlled, Preliminary Study. Integr. Cancer Ther. 2021;20:15347354211040830. doi: 10.1177/15347354211040830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ishiura Y., Shiba Y., Terasaki Y., Hayase H., Hamada M., Izawa K., Sugimoto A., Hirokami K., Segawa M., Kasahara K., et al. Effect of Japanese Traditional Medicine, TJ-48, on the Quality of Life of Patients with Non-Small Cell Lung Cancer Receiving Outpatient Chemotherapy. Gan Kagaku Ryoho. 2016;43:331–334. [PubMed] [Google Scholar]
- 155.Kawai H., Saito Y. Combination of Juzentaihoto and chemotherapy improves the prognosis of patients with postoperative recurrence of non-small cell lung cancer. Mol. Clin. Oncol. 2020;13:13. doi: 10.3892/mco.2020.2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Huang S.-M., Chien L.-Y., Tai C.-J., Chiou J.-F., Chen C.-S., Tai C.-J. Effectiveness of 3-Week Intervention of Shi Quan Da Bu Tang for Alleviating Hematotoxicity Among Patients With Breast Carcinoma Receiving Chemotherapy. Integr. Cancer Ther. 2013;12:136–144. doi: 10.1177/1534735412450513. [DOI] [PubMed] [Google Scholar]
- 157.Shimizu M., Takayama S., Kikuchi A., Arita R., Ono R., Ishizawa K., Ishii T. Integrative therapy for advanced pancreatic cancer using Kampo and western medicine: A case report. Explore. 2021;17:255–258. doi: 10.1016/j.explore.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 158.Poulson M.J. Not just tired. J. Clin. Oncol. 2001;19:4180–4181. doi: 10.1200/JCO.2001.19.21.4180. [DOI] [PubMed] [Google Scholar]
- 159.Shinozuka N., Tatsumi K., Nakamura A., Terada J., Kuriyama T. The traditional herbal medicine Hochuekkito improves systemic inflammation in patients with chronic obstructive pulmonary disease. J. Am. Geriatr Soc. 2007;55:313–314. doi: 10.1111/j.1532-5415.2007.01057.x. [DOI] [PubMed] [Google Scholar]
- 160.Mori S., Usami N., Fukumoto K., Mizuno T., Kuroda H., Sakakura N., Yokoi K., Sakao Y. The Significance of the Prognostic Nutritional Index in Patients with Completely Resected Non-Small Cell Lung Cancer. PLoS ONE. 2015;10:e0136897. doi: 10.1371/journal.pone.0136897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Deng G. Integrative Medicine Therapies for Pain Management in Cancer Patients. Cancer J. 2019;25:343–348. doi: 10.1097/PPO.0000000000000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sheinfeld Gorin S., Krebs P., Badr H., Janke E.A., Jim H.S., Spring B., Mohr D.C., Berendsen M.A., Jacobsen P.B. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J. Clin. Oncol. 2012;30:539–547. doi: 10.1200/JCO.2011.37.0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wu T.H., Chiu T.Y., Tsai J.S., Chen C.Y., Chen L.C., Yang L.L. Effectiveness of Taiwanese traditional herbal diet for pain management in terminal cancer patients. Asia Pac. J. Clin. Nutr. 2008;17:17–22. [PubMed] [Google Scholar]
- 164.Ali A., Park Y., Lee J., An H.-J., Jin J.-S., Lee J.-H., Chang J., Kim D.-K., Goo B., Park Y.C., et al. In Vitro Study of Licorice on IL-1β-Induced Chondrocytes and In Silico Approach for Osteoarthritis. Pharmaceuticals. 2021;14:1337. doi: 10.3390/ph14121337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Massey R.L., Kim H.K., Abdi S. Brief review: Chemotherapy-induced painful peripheral neuropathy (CIPPN): Current status and future directions. Can. J. Anaesth. 2014;61:754–762. doi: 10.1007/s12630-014-0171-4. [DOI] [PubMed] [Google Scholar]
- 166.Zhou Y.Q., Liu D.Q., Chen S.P., Chen N., Sun J., Wang X.M., Cao F., Tian Y.K., Ye D.W. Nrf2 activation ameliorates mechanical allodynia in paclitaxel-induced neuropathic pain. Acta Pharm. Sin. 2020;41:1041–1048. doi: 10.1038/s41401-020-0394-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gong H., Zhang B.K., Yan M., Fang P.F., Li H.D., Hu C.P., Yang Y., Cao P., Jiang P., Fan X.R. A protective mechanism of licorice (Glycyrrhiza uralensis): Isoliquiritigenin stimulates detoxification system via Nrf2 activation. J. Ethnopharmacol. 2015;162:134–139. doi: 10.1016/j.jep.2014.12.043. [DOI] [PubMed] [Google Scholar]
- 168.Avritscher E.B., Cooksley C.D., Elting L.S. Scope and epidemiology of cancer therapy-induced oral and gastrointestinal mucositis. Semin. Oncol. Nurs. 2004;20:3–10. doi: 10.1053/j.soncn.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 169.Kim J.K., Oh S.M., Kwon H.S., Oh Y.S., Lim S.S., Shin H.K. Anti-inflammatory effect of roasted licorice extracts on lipopolysaccharide-induced inflammatory responses in murine macrophages. Biochem. Biophys. Res. Commun. 2006;345:1215–1223. doi: 10.1016/j.bbrc.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 170.Racková L., Jancinová V., Petríková M., Drábiková K., Nosál R., Stefek M., Kostálová D., Prónayová N., Kovácová M. Mechanism of anti-inflammatory action of liquorice extract and glycyrrhizin. Nat. Prod. Res. 2007;21:1234–1241. doi: 10.1080/14786410701371280. [DOI] [PubMed] [Google Scholar]
- 171.Sharma R., Tobin P., Clarke S.J. Management of chemotherapy-induced nausea, vomiting, oral mucositis, and diarrhoea. Lancet Oncol. 2005;6:93–102. doi: 10.1016/S1470-2045(05)01735-3. [DOI] [PubMed] [Google Scholar]
- 172.Doherty K.M. Closing the gap in prophylactic antiemetic therapy: Patient factors in calculating the emetogenic potential of chemotherapy. Clin. J. Oncol. Nurs. 1999;3:113–119. [PubMed] [Google Scholar]
- 173.Henry D.H. Epoetin alfa for the treatment of cancer- and chemotherapy-related anaemia: Product review and update. Expert Opin. Pharm. 2005;6:295–310. doi: 10.1517/14656566.6.2.295. [DOI] [PubMed] [Google Scholar]
- 174.Gilreath J.A., Stenehjem D.D., Rodgers G.M. Diagnosis and treatment of cancer-related anemia. Am. J. Hematol. 2014;89:203–212. doi: 10.1002/ajh.23628. [DOI] [PubMed] [Google Scholar]
- 175.Spivak J.L. Cancer-related anemia: Its causes and characteristics. Semin. Oncol. 1994;21:3–8. [PubMed] [Google Scholar]
- 176.Ludwig H., Strasser K. Symptomatology of anemia. Semin. Oncol. 2001;28:7–14. doi: 10.1016/S0093-7754(01)90206-4. [DOI] [PubMed] [Google Scholar]
- 177.Hisha H., Yamada H., Sakurai M.H., Kiyohara H., Li Y., Yu C., Takemoto N., Kawamura H., Yamaura K., Shinohara S., et al. Isolation and identification of hematopoietic stem cell-stimulating substances from Kampo (Japanese herbal) medicine, Juzen-taiho-to. Blood. 1997;90:1022–1030. doi: 10.1182/blood.V90.3.1022. [DOI] [PubMed] [Google Scholar]
- 178.Sho Y., Fujisaki K., Sakashita H., Yamaguchi K., Tahara K., Kubozono O., Ido A., Tsubouchi H. Orally administered Kampo medicine, Juzen-taiho-to, ameliorates anemia during interferon plus ribavirin therapy in patients with chronic hepatitis C. J. Gastroenterol. 2004;39:1202–1204. doi: 10.1007/s00535-004-1472-0. [DOI] [PubMed] [Google Scholar]
- 179.Amaraa R., Mareckova H., Urbanek P., Fucikova T. Immunological predictors of different responses to combination therapy with interferon alpha and ribavirin in patients with chronic hepatitis C. J. Gastroenterol. 2003;38:254–259. doi: 10.1007/s005350300044. [DOI] [PubMed] [Google Scholar]
- 180.Behzadmehr R., Dastyar N., Moghadam M.P., Abavisani M., Moradi M. Effect of complementary and alternative medicine interventions on cancer related pain among breast cancer patients: A systematic review. Complement. Ther. Med. 2020;49:102318. doi: 10.1016/j.ctim.2020.102318. [DOI] [PubMed] [Google Scholar]
- 181.Nishida K. Molecular Mechanisms of Taste Disorder in Oxaliplatin-administered Rats. Yakugaku Zasshi. 2016;136:1017–1021. doi: 10.1248/yakushi.15-00212. [DOI] [PubMed] [Google Scholar]
- 182.Ovesen L. Anorexia in patients with cancer with special references on its association with early changes in food-intake behavior chemotherapeutic treatment and adjuvant enteral nutrition. Int. J. Oncol. 1994;5:889–899. doi: 10.3892/ijo.5.4.889. [DOI] [PubMed] [Google Scholar]
- 183.Haverman T.M., Raber-Durlacher J.E., Rademacher W.M., Vokurka S., Epstein J.B., Huisman C., Hazenberg M.D., de Soet J.J., de Lange J., Rozema F.R. Oral complications in hematopoietic stem cell recipients: The role of inflammation. Mediat. Inflamm. 2014;2014:378281. doi: 10.1155/2014/378281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cohen J., Wakefield C.E., Laing D.G. Smell and Taste Disorders Resulting from Cancer and Chemotherapy. Curr. Pharm. Des. 2016;22:2253–2263. doi: 10.2174/1381612822666160216150812. [DOI] [PubMed] [Google Scholar]
- 185.Das D., Agarwal S.K., Chandola H.M. Protective effect of Yashtimadhu (Glycyrrhiza glabra) against side effects of radiation/chemotherapy in head and neck malignancies. Ayu. 2011;32:196–199. doi: 10.4103/0974-8520.92579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Yoshioka Y., Samukawa Y., Yamashita Y., Ashida H. 4-Hydroxyderricin and xanthoangelol isolated from Angelica keiskei prevent dexamethasone-induced muscle loss. Food Funct. 2020;11:5498–5512. doi: 10.1039/D0FO00720J. [DOI] [PubMed] [Google Scholar]
- 187.Wang E., Bussom S., Chen J., Quinn C., Bedognetti D., Lam W., Guan F., Jiang Z., Mark Y., Zhao Y., et al. Interaction of a traditional Chinese Medicine (PHY906) and CPT-11 on the inflammatory process in the tumor microenvironment. BMC Med. Genom. 2011;4:38. doi: 10.1186/1755-8794-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zhang Y.H., Isobe K., Nagase F., Lwin T., Kato M., Hamaguchi M., Yokochi T., Nakashima I. Glycyrrhizin as a promoter of the late signal transduction for interleukin-2 production by splenic lymphocytes. Immunology. 1993;79:528–534. [PMC free article] [PubMed] [Google Scholar]
- 189.Ojima M., Satoh K., Gomibuchi T., Itoh N., Kin S., Fukuchi S., Miyachi Y. The inhibitory effects of glycyrrhizin and glycyrrhetinic acid on the metabolism of cortisol and prednisolone--in vivo and in vitro studies. Nihon Naibunpi Gakkai Zasshi. 1990;66:584–596. doi: 10.1507/endocrine1927.66.5_584. [DOI] [PubMed] [Google Scholar]
- 190.Yoh T., Nakashima T., Sumida Y., Kakisaka Y., Nakajima Y., Ishikawa H., Sakamoto Y., Okanoue T., Mitsuyoshi H. Effects of glycyrrhizin on glucocorticoid signaling pathway in hepatocytes. Dig. Dis. Sci. 2002;47:1775–1781. doi: 10.1023/A:1016492527927. [DOI] [PubMed] [Google Scholar]
- 191.James B. The Use of Liquorice in Weight Reduction. Lancet. 1956;268:996. doi: 10.1016/S0140-6736(56)90359-2. [DOI] [Google Scholar]
- 192.Armanini D., Nacamulli D., Francini-Pesenti F., Battagin G., Ragazzi E., Fiore C. Glycyrrhetinic acid, the active principle of licorice, can reduce the thickness of subcutaneous thigh fat through topical application. Steroids. 2005;70:538–542. doi: 10.1016/j.steroids.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 193.Beskina O.A., Abramov A., Gabdulkhakova A.G., Miller A.V., Safronova V.G., Zamaraeva M.V. Possible mechanisms of antioxidant activity of glycyrrhizic acid. Biomed. Khim. 2006;52:60–68. [PubMed] [Google Scholar]
- 194.Armanini D., De Palo C.B., Mattarello M.J., Spinella P., Zaccaria M., Ermolao A., Palermo M., Fiore C., Sartorato P., Francini-Pesenti F., et al. Effect of licorice on the reduction of body fat mass in healthy subjects. J. Endocrinol. Investig. 2003;26:646–650. doi: 10.1007/BF03347023. [DOI] [PubMed] [Google Scholar]
- 195.Ju S.M., Kim M.S., Jo Y.S., Jeon Y.M., Bae J.S., Pae H.O., Jeon B.H. Licorice and its active compound glycyrrhizic acid ameliorates cisplatin-induced nephrotoxicity through inactivation of p53 by scavenging ROS and overexpression of p21 in human renal proximal tubular epithelial cells. Eur. Rev. Med. Pharm. Sci. 2017;21:890–899. [PubMed] [Google Scholar]
- 196.Wu C.H., Chen A.Z., Yen G.C. Protective Effects of Glycyrrhizic Acid and 18β-Glycyrrhetinic Acid against Cisplatin-Induced Nephrotoxicity in BALB/c Mice. J. Agric. Food Chem. 2015;63:1200–1209. doi: 10.1021/jf505471a. [DOI] [PubMed] [Google Scholar]
- 197.Kim M., Park S.C., Lee D.Y. Glycyrrhizin as a Nitric Oxide Regulator in Cancer Chemotherapy. Cancers. 2021;13:5762. doi: 10.3390/cancers13225762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zeeshan M., Atiq A., Ain Q.U., Ali J., Khan S., Ali H. Evaluating the mucoprotective effects of glycyrrhizic acid-loaded polymeric nanoparticles in a murine model of 5-fluorouracil-induced intestinal mucositis via suppression of inflammatory mediators and oxidative stress. Inflammopharmacology. 2021;29:1539–1553. doi: 10.1007/s10787-021-00866-z. [DOI] [PubMed] [Google Scholar]
- 199.Deng Q.P., Wang M.J., Zeng X., Chen G.G., Huang R.Y. Effects of Glycyrrhizin in a Mouse Model of Lung Adenocarcinoma. Cell Physiol. Biochem. 2017;41:1383–1392. doi: 10.1159/000467897. [DOI] [PubMed] [Google Scholar]
- 200.Wakamatsu T., Nakahashi Y., Hachimine D., Seki T., Okazaki K. The combination of glycyrrhizin and lamivudine can reverse the cisplatin resistance in hepatocellular carcinoma cells through inhibition of multidrug resistance-associated proteins. Int. J. Oncol. 2007;31:1465–1472. doi: 10.3892/ijo.31.6.1465. [DOI] [PubMed] [Google Scholar]
- 201.Zhu X., Cong J., Lin Z., Sun J., Yang B., Li A. Inhibition of HMGB1 Overcomes Resistance to Radiation and Chemotherapy in Nasopharyngeal Carcinoma. Onco Targets Ther. 2020;13:4189–4199. doi: 10.2147/OTT.S239243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kabe Y., Koike I., Yamamoto T., Hirai M., Kanai A., Furuhata R., Tsugawa H., Harada E., Sugase K., Hanadate K., et al. Glycyrrhizin Derivatives Suppress Cancer Chemoresistance by Inhibiting Progesterone Receptor Membrane Component 1. Cancers. 2021;13:3265. doi: 10.3390/cancers13133265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Shi L., Tang C., Yin C. Glycyrrhizin-modified O-carboxymethyl chitosan nanoparticles as drug vehicles targeting hepatocellular carcinoma. Biomaterials. 2012;33:7594–7604. doi: 10.1016/j.biomaterials.2012.06.072. [DOI] [PubMed] [Google Scholar]
- 204.Tian G., Pan R., Zhang B., Qu M., Lian B., Jiang H., Gao Z., Wu J. Liver-Targeted Combination Therapy Basing on Glycyrrhizic Acid-Modified DSPE-PEG-PEI Nanoparticles for Co-delivery of Doxorubicin and Bcl-2 siRNA. Front. Pharmacol. 2019;10:4. doi: 10.3389/fphar.2019.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wang Q.S., Gao L.N., Zhu X.N., Zhang Y., Zhang C.N., Xu D., Cui Y.L. Co-delivery of glycyrrhizin and doxorubicin by alginate nanogel particles attenuates the activation of macrophage and enhances the therapeutic efficacy for hepatocellular carcinoma. Theranostics. 2019;9:6239–6255. doi: 10.7150/thno.35972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Honda H., Nagai Y., Matsunaga T., Saitoh S., Akashi-Takamura S., Hayashi H., Fujii I., Miyake K., Muraguchi A., Takatsu K. Glycyrrhizin and isoliquiritigenin suppress the LPS sensor toll-like receptor 4/MD-2 complex signaling in a different manner. J. Leukoc. Biol. 2012;91:967–976. doi: 10.1189/jlb.0112038. [DOI] [PubMed] [Google Scholar]
- 207.Lee C.K., Son S.H., Park K.K., Park J.H., Lim S.S., Chung W.Y. Isoliquiritigenin inhibits tumor growth and protects the kidney and liver against chemotherapy-induced toxicity in a mouse xenograft model of colon carcinoma. J. Pharm. Sci. 2008;106:444–451. doi: 10.1254/jphs.FP0071498. [DOI] [PubMed] [Google Scholar]
- 208.Gómez-Sierra T., Medina-Campos O.N., Solano J.D., Ibarra-Rubio M.E., Pedraza-Chaverri J. Isoliquiritigenin Pretreatment Induces Endoplasmic Reticulum Stress-Mediated Hormesis and Attenuates Cisplatin-Induced Oxidative Stress and Damage in LLC-PK1 Cells. Molecules. 2020;25:4442. doi: 10.3390/molecules25194442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Li W., Sun Y.N., Yan X.T., Yang S.Y., Kim S., Lee Y.M., Koh Y.S., Kim Y.H. Flavonoids from Astragalus membranaceus and their inhibitory effects on LPS-stimulated pro-inflammatory cytokine production in bone marrow-derived dendritic cells. Arch. Pharm. Res. 2014;37:186–192. doi: 10.1007/s12272-013-0174-7. [DOI] [PubMed] [Google Scholar]
- 210.Lv X., Zhu Y., Deng Y., Zhang S., Zhang Q., Zhao B., Li G. Glycyrrhizin improved autophagy flux via HMGB1-dependent Akt/mTOR signaling pathway to prevent Doxorubicin-induced cardiotoxicity. Toxicology. 2020;441:152508. doi: 10.1016/j.tox.2020.152508. [DOI] [PubMed] [Google Scholar]
- 211.Lei X., Hu X., Zhang T., Zhang J., Wu C., Hong W., Jiang Y., Wang Q., Xie Y., Zhao Y., et al. HMGB1 release promotes paclitaxel resistance in castration-resistant prostate cancer cells via activating c-Myc expression. Cell. Signal. 2020;72:109631. doi: 10.1016/j.cellsig.2020.109631. [DOI] [PubMed] [Google Scholar]
- 212.Hisaoka-Nakashima K., Tomimura Y., Yoshii T., Ohata K., Takada N., Zhang F.F., Nakamura Y., Liu K., Wake H., Nishibori M., et al. High-mobility group box 1-mediated microglial activation induces anxiodepressive-like behaviors in mice with neuropathic pain. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2019;92:347–362. doi: 10.1016/j.pnpbp.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 213.Cao Z.Y., Liu Y.Z., Li J.M., Ruan Y.M., Yan W.J., Zhong S.Y., Zhang T., Liu L.L., Wu R., Wang B., et al. Glycyrrhizic acid as an adjunctive treatment for depression through anti-inflammation: A randomized placebo-controlled clinical trial. J. Affect. Disord. 2020;265:247–254. doi: 10.1016/j.jad.2020.01.048. [DOI] [PubMed] [Google Scholar]
- 214.Ren C.A., Li Y.X., Cui J.Y., Sheng Z.X., Ran X.H., Wang B.H., Zhang M.H. Efficacy of glycyrrhizin combined with cyclosporine in the treatment of non-severe aplastic anemia. Chin. Med. J. 2013;126:2083–2086. [PubMed] [Google Scholar]
- 215.Patricia Moreno-Londoño A., Bello-Alvarez C., Pedraza-Chaverri J. Isoliquiritigenin pretreatment attenuates cisplatin induced proximal tubular cells (LLC-PK1) death and enhances the toxicity induced by this drug in bladder cancer T24 cell line. Food Chem. Toxicol. 2017;109:143–154. doi: 10.1016/j.fct.2017.08.047. [DOI] [PubMed] [Google Scholar]
- 216.Hu F.W., Yu C.C., Hsieh P.L., Liao Y.W., Lu M.Y., Chu P.M. Targeting oral cancer stemness and chemoresistance by isoliquiritigenin-mediated GRP78 regulation. Oncotarget. 2017;8:93912–93923. doi: 10.18632/oncotarget.21338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Alshangiti A.M., Togher K.L., Hegarty S.V., Sullivan A.M., O’Keeffe G.W. The dietary flavonoid isoliquiritigenin is a potent cytotoxin for human neuroblastoma cells. Neuronal Signal. 2019;3:NS20180201. doi: 10.1042/NS20180201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Rui-Zhi T., Ke-Huan X., Yuan L., Xiao L., Bing-Wen Z., Tong-Tong L., Li W. Renoprotective effect of isoliquiritigenin on cisplatin-induced acute kidney injury through inhibition of FPR2 in macrophage. J. Pharm. Sci. 2022;148:56–64. doi: 10.1016/j.jphs.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 219.Jin H., Seo G.S., Lee S.H. Isoliquiritigenin-mediated p62/SQSTM1 induction regulates apoptotic potential through attenuation of caspase-8 activation in colorectal cancer cells. Eur. J. Pharm. 2018;841:90–97. doi: 10.1016/j.ejphar.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 220.Yamazaki S., Morita T., Endo H., Hamamoto T., Baba M., Joichi Y., Kaneko S., Okada Y., Okuyama T., Nishino H., et al. Isoliquiritigenin suppresses pulmonary metastasis of mouse renal cell carcinoma. Cancer Lett. 2002;183:23–30. doi: 10.1016/S0304-3835(02)00113-1. [DOI] [PubMed] [Google Scholar]
- 221.Al-Qahtani W.H., Alshammari G.M., Ajarem J.S., Al-Zahrani A.Y., Alzuwaydi A., Eid R., Yahya M.A. Isoliquiritigenin prevents Doxorubicin-induced hepatic damage in rats by upregulating and activating SIRT1. Biomed. Pharm. 2022;146:112594. doi: 10.1016/j.biopha.2021.112594. [DOI] [PubMed] [Google Scholar]
- 222.Zhou J.X., Wink M. Reversal of Multidrug Resistance in Human Colon Cancer and Human Leukemia Cells by Three Plant Extracts and Their Major Secondary Metabolites. Medicines. 2018;5:123. doi: 10.3390/medicines5040123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Youns M., Fu Y.J., Zu Y.G., Kramer A., Konkimalla V.B., Radlwimmer B., Sültmann H., Efferth T. Sensitivity and resistance towards isoliquiritigenin, doxorubicin and methotrexate in T cell acute lymphoblastic leukaemia cell lines by pharmacogenomics. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2010;382:221–234. doi: 10.1007/s00210-010-0541-6. [DOI] [PubMed] [Google Scholar]