Abstract
The Kunjin strain of West Nile virus (WNVKUN) is a mosquito-transmitted flavivirus that can infect farmed saltwater crocodiles in Australia and cause skin lesions that devalue the hides of harvested animals. We implemented a surveillance system using honey-baited nucleic acid preservation cards to monitor WNVKUN and another endemic flavivirus pathogen, Murray Valley encephalitis virus (MVEV), on crocodile farms in northern Australia. The traps were set between February 2018 and July 2020 on three crocodile farms in Darwin (Northern Territory) and one in Cairns (North Queensland) at fortnightly intervals with reduced trapping during the winter months. WNVKUN RNA was detected on all three crocodile farms near Darwin, predominantly between March and May of each year. Two of the NT crocodile farms also yielded the detection of MVE viral RNA sporadically spread between April and November in 2018 and 2020. In contrast, no viral RNA was detected on crocodile farms in Cairns during the entire trapping period. The detection of WNVKUN and MVEV transmission by FTATM cards on farms in the Northern Territory generally correlated with the detection of their transmission to sentinel chicken flocks in nearby localities around Darwin as part of a separate public health surveillance program. While no isolates of WNVKUN or MVEV were obtained from mosquitoes collected on Darwin crocodile farms immediately following the FTATM card detections, we did isolate another flavivirus, Kokobera virus (KOKV), from Culex annulirostris mosquitoes. Our studies support the use of the FTATM card system as a sensitive and accurate method to monitor the transmission of WNVKUN and other arboviruses on crocodile farms to enable the timely implementation of mosquito control measures. Our detection of MVEV transmission and isolation of KOKV from mosquitoes also warrants further investigation of their potential role in causing diseases in crocodiles and highlights a “One Health” issue concerning arbovirus transmission to crocodile farm workers. In this context, the introduction of FTATM cards onto crocodile farms appears to provide an additional surveillance tool to detect arbovirus transmission in the Darwin region, allowing for a more timely intervention of vector control by relevant authorities.
Keywords: mosquitoes, Kunjin virus, flaviviruses, surveillance, sentinel chickens, FTATM cards, virus isolation, saltwater crocodile
1. Introduction
Habitats containing permanent water sources that support mosquito breeding and natural vegetation and that provide sanctuary to wading birds are ideal for the transmission of mosquito-borne viruses. This type of environment is common in parts of tropical northern Australia including the Darwin region of the Northern Territory. Such habitats can be found on saltwater crocodile farms.
In 2016, the Kunjin strain of West Nile virus (WNVKUN), belonging to the genus Flavivirus and the family Flaviviridae, was detected in the skin lesions of farmed saltwater crocodiles (Crocodylus porosus) in the Northern Territory (NT) of Australia [1]. During the tanning process, these lesions caused by WNVKUN lead to an unevenly structured and dyed skin surface. As a result, crocodile skins found with these lesions are rejected, effecting extensive economic losses for the Australian industry [2].
The mosquito-borne WNVKUN is endemic in northern Australia and is occasionally associated with non-fatal cases of encephalitis in humans. However, the strain of WNVKUN infecting crocodiles is of special interest since it is genetically similar to WNVKUN NSW2011 [2], which was responsible for a large outbreak of fatal equine encephalitis in south-eastern Australia in 2011 [3,4]. The equine virus was shown to be a newly emerged strain that was more neuro-invasive in animal models of the WNVKUN disease, suggesting changes in the epidemiology and ecology of the virus [5].
WNVKUN is predominantly transmitted by the mosquito vector Culex annulirostris (Skuse), a ubiquitous species found throughout Australia [6,7,8], while wading birds, especially herons and egrets, are the vertebrate hosts for the virus [9,10]. In the context of human health, the endemic flaviviruses Murray Valley encephalitis virus (MVEV) and Kokobera virus (KOKV) are also transmitted by this vector in Australia [6,11,12,13]. While MVEV causes sporadic cases of severe and fatal encephalitis in humans, infected individuals mostly remain asymptomatic or present with mild symptoms [14]. KOKV infection also occurs occasionally in humans, and may cause acute polyarticular manifestations with febrile illness, taking several months to resolve in some cases [15]. However, these flaviviruses have the potential to emerge as more significant human pathogens, similar to WNVKUN, as environmental and societal changes could alter transmission cycles and influence human infections [4,14,15].
While Cx. annulirostris is the dominant species found on commercial crocodile farms in the NT, both Cx. quinquefasciatus (Theobald) and Cx. pullus (Theobald) have been detected breeding on these farms [16,17,18]. Cx. quinquefasciatus and Cx. pullus have also been implicated in flavivirus transmission. WNVKUN has occasionally been isolated from Cx. quinquefasciatus, a species that has been associated with WNV transmission to humans [19,20,21] and in North America with transmission to alligators [22,23]. Johansen et al. (2009) suggested that Cx. quinquefasciatus could transmit the virus from birds to humans, acting as a bridge vector [19]. Flaviviruses have also been isolated from field collected Cx. pullus, another ornithophilic species possibly maintaining flaviviruses in an enzootic cycle in birds [10,24]. Cx. gelidus (Theobald) is of interest as it has shown a high competency for transmitting WNV in laboratory experiments, such as the Australian subtype WNVKUN and to a lesser extent MVEV [25], and an Indian prototype of WNV [26]. However, to date, these flaviviruses have not been isolated from field collected specimens of these species in Australia.
We established a virus-mosquito surveillance system using passive sentinel mosquito arbovirus capture kits (SMACK traps) with honey-baited nucleic acid preservation cards (FTATM cards) in order to develop a simple, real-time system to rapidly detect mosquito transmission of WNVKUN on the crocodile farms [27]. In addition, we collected mosquitoes within close proximity using CO2-baited encephalitis virus surveillance (EVS) traps to assess the prevalence of vector species and to obtain isolates of WNVKUN for vector incrimination. With a “One Health” approach in mind, we were also interested in the detection of MVEV, which is not known to infect crocodiles, but similar to WNVKUN, can cause serious disease in humans [28].
This investigation aimed to establish a logistically convenient system to monitor mosquito-borne flavivirus activity on crocodile farms and develop recommendations for the timely implementation of control strategies. This also allowed us to further define the transmission dynamics of WNVKUN on crocodile farms by comparing data from FTATM detection with seroconversions to WNVKUN and MVEV in sentinel chicken flocks located in nearby locations around Darwin during the same time period.
2. Materials and Methods
2.1. Locations of Crocodile Farms
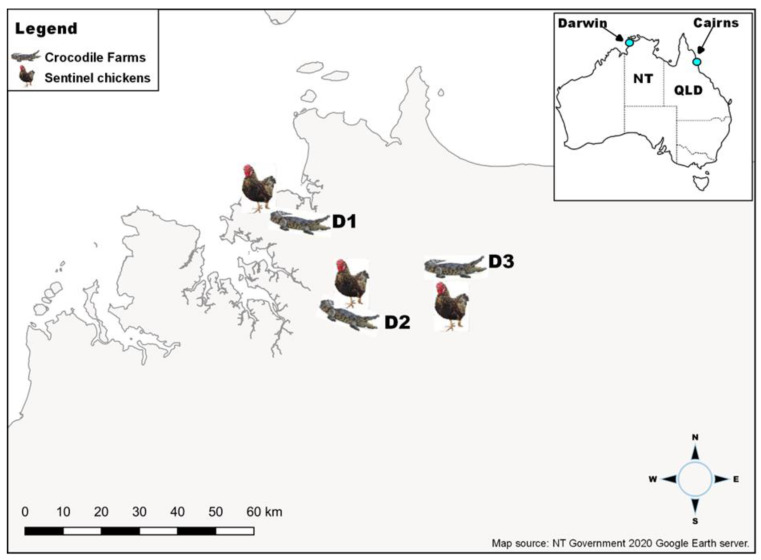
The investigation was conducted on three commercial crocodile farms, identified as Farms D1, D2, and D3, located in the rural areas of the Darwin region of the NT, Australia (Figure 1), and one farm in the Cairns region (Farm C1) in northern Queensland, Australia (Figure 1). Farms in the Darwin region are in close proximity to freshwater lagoons and wetlands, which are known productive Cx. annulirostris breeding areas. The crocodile farm in Cairns (C1) borders on saltwater mangrove environments with mosquitoes around the breeder pens.
Figure 1.
Map of Australia showing the relative locations of Darwin and Cairns in the tropical north of the continent (inset) and crocodile farms in Darwin (D1, D2, and D3) with neighbouring sentinel chicken flocks (main picture).
2.2. Flavivirus Surveillance Using Nucleic Acid Preservation Cards
To assess the presence of WNVKUN and other flaviviruses at the four crocodile farms, CO2-baited SMACK traps were deployed. SMACK has been successfully used in recent years, with honey-soaked nucleic acid preservation cards (FTATM) incorporated into these mosquito traps. The honey attracts trapped mosquitoes, and while feeding they expectorate saliva which also contains any transmissible virus. While the virus is quickly inactivated on the cards, its RNA is preserved. Cards are then sent to the laboratory by normal post and tested for viral RNA by qRT-PCR [27,29,30,31,32] (Figure 2).
Figure 2.
CO2-baited SMACK trap housing two honey-baited FTATM cards (arrows).
In Darwin, two traps were set at each farm in either vegetated areas, assessed to be mosquito harbourage sites, or close to crocodile breeder or grower pens, with the traps serviced and FTATM cards replaced approximately fortnightly during the high WNVKUN risk period between January and July [33]. Traps were first set on farms D2 and D3 on 21 February 2018 and on farm D1 on 27 February and all were operated until 1 July 2020. During that period, severe cyclone Marcus impacted both D1 traps set between 6 and 22 March 2018. They were replaced with a set running from 7 to 28 March with the following set running just over a week between 28 March and 5 April. During the low WNVKUN risk season, two traps remained operational at D2 and D3 between 2 July and 5 November 2018, before all 6 traps were re-deployed between 5 November 2018 and 1 July 2019. During the second off-season, only 1 trap at D2 was operated between 1 July to 5 November 2019, before starting at D1 on 6 January and at D3 on 7 January 2020 with all 6 traps operational until 1 July 2020. In total, 256 traps were set with 93 in 2018, 87 in 2019, and 76 in 2020, fitted with 2 FTATM cards per trap (Table S1).
In Cairns, two traps were run from 6 March to 26 June 2018, 13 February to 5 June 2019, and from 7 January to 26 March 2020, totalling 44 traps (16 traps each in 2018 and 2019 and 12 traps in 2020) set at C1 with 2 FTATM cards per trap (Table S1).
During the fortnightly trap service, mosquito numbers were visually estimated for each trap, then discarded. However, these estimates are not necessarily representative since mosquitoes could escape, or as on a few occasions, ants could find access into traps and eat the mosquitoes. Farms were also routinely sprayed to reduce mosquito numbers. The FTATM cards from each trap were placed in separate sealable plastic bags and stored at room temperature before being sent to the laboratory at Public Health Virology, Forensic and Scientific Services, Queensland Health, for testing. Surgical gloves were used during handling of the cards to avoid sample contamination.
2.3. Processing of FTATM Cards and Detection of Viral RNA
In the laboratory, cards were kept at ambient temperature but placed on ice as soon as processing began. Methods of elution as described in Hall-Mendelin et al. (2010) [27] were followed with two modifications: the cards were vortexed in molecular grade water to elute nucleic acids prior to extraction on a Qiagen BioRobot Universal System, and QIAamp One-For-All Nucleic Acid Kit (Qiagen, Clifton Hill, VIC, Australia) was used according to instructions. Viral RNA was detected by TaqMan RT-PCR using specific assays for WNVKUN and MVEV. WNVKUN RNA was amplified with the following primers and probe: Primer Kunjin-F AACCCCAGTGGAGAAGTGGA at 900 nM/µL, Primer Kunjin-R TCAGGCTGCCACACCAAA at 900 nM/µL, and Probe Kunjin MGB 6FAM-CGATGTTCCATACTCTGG-MGB at 150 nM/µL [34] (Finger, unpublished). MVEV RNA amplification was performed using MVE-FOR ATCTGGTGYGGAAGYCTCA at 900 nM/µL, MVE-REV CGCGTAGATGTTCTCAGCCC at 900 nM/µL, and MVEV-Probe 6FAM-ATGTTGCCCTGGTCCTGGTCCCT-TAMRA at 200 nM/µL [34]. Detection of both templates was performed in a 20 µL reaction volume in a Rotor-Gene Q real-time PCR cycler (Qiagen, Chadstone, VIC, Australia). Cycling conditions were set as follows: one cycle at 50 °C for 5 min, one cycle at 95 °C for 2 min, and 50 cycles at 95 °C for 3 s and 60 °C for 30 s using the Superscript III Platinum one-step quantitative qRT-PCR system (Invitrogen, Carlsbad, CA, USA) which was used as per the manufacturer’s instructions. Separate synthetic controls for primers and probe of both viruses, and no template controls were included in each Rotor-Gene run [35]. A sample was generally deemed positive with Ct values <40 and negative when Ct values were >40. These assays are NATA accredited.
2.4. Sentinel Chickens in Darwin
In order to issue timely public health warnings, sentinel chickens have been the primary method for flavivirus surveillance in the NT since 1992, with seroconversions to WNVKUN and/or MVEV recorded in most years [36], whereas Cairns (QLD) does not operate a sentinel animal program for arbovirus detection.
Four sentinel chicken flocks consisting of 8 to 12 chickens were used, with the Leanyer flock located 7 km from crocodile farm D1, the Beatrice Hill Farm (BHF) flock 10 km from crocodile farm D3, and the Howard Springs and Bees Creek flocks situated 12 km and 0.05 km, respectively, from crocodile farm D2. The Leanyer, Howard Springs, and BHF flocks are in close proximity to extensive wetlands and have been part of the NT flavivirus surveillance program since 1992–1993, while the Bees Creek flock was only established in early March 2020. Chickens were bled monthly during the high risk WNVKUN period (January to June), with an initial baseline bleed in December 2018 and 2019. Samples were tested for antibodies to viruses using standard flavivirus neutralisation tests as described [37]. Bleeding of sentinel chickens was carried out under ethics approval (monitoring sentinel animals for viruses of animal and human health significance number A11033. 100/annum) granted by the Charles Darwin University Research Ethics Committee.
2.5. Mosquito Collections
Following detection of WNVKUN on FTATM cards from SMACK traps, encephalitis virus surveillance (EVS) traps were then set at the same locations on the farms to maximise the chance of collecting mosquitoes carrying WNVKUN for virus isolation, with a total of 22 traps set in 2018 and 17 traps in 2019.
To maintain the required cold chain for virus isolation work, mosquito traps were transported from site in an insulated container with dry ice before mosquitoes were stored at −80 °C. Mosquito identification to species level was performed on cold tables at the Medical Entomology laboratory in Darwin using taxonomic keys [38,39,40,41,42,43]. Identified mosquito species were stored in vials up to 50 specimens, and blood fed specimens or specimens with mites attached were not processed.
2.6. Virus Isolation
Mosquito pools containing up to 50 individuals were shipped to the laboratory on dry ice and then stored at −80 °C until processing for flavivirus isolation. Pools of mosquitoes were then homogenised in 2 mL of medium (Opti-MEM, GIBCO, Life Technologies, Grand Island, NY, USA), supplemented with 3% fetal bovine serum (In Vitro Technologies, Australian origin), antibiotics, and antimycotics (GIBCO, Life Technologies, Grand Island, NY, USA), using one metal bead in a Tissue Lyser II (Qiagen, Hilden, Germany). After centrifugation, supernatants were filtered. We used 0.2 µm size syringe filters for pools containing < 5 mosquitoes and the 0.8/0.2 µm double filter units for larger pools (PALL Corporation, Ann Arbor, MI, USA). Sterile homogenates were inoculated in quadruplet, 50 µL per well, on duplicate 96-well plates coated with a monolayer of C6/36 cells. The cultures were incubated for 7 days at 28 °C, then fixed in cold 20% acetone after removal of supernatants which were stored at −80 °C. Fixed, dried plates were stored at −20 °C. Presence of flaviviruses was detected on the plates with an ELISA using monoclonal antibodies 4G2 (pan flavivirus anti-E) and 4G4 (pan flavivirus anti-NS1) [44]. Briefly, plates were blocked for 1 h with 100 µL per well of blocking buffer, prior to the addition of a cocktail of 4G2 and 4G4, each diluted 1:100 in blocking buffer, at 50 µL per well. After 1h incubation at room temperature, the plates were washed 6 times then anti-mouse IgG HPR conjugate (diluted 1/2000 in blocking buffer) was added at 50 µL per well. After further incubation and washing of plates, TMB substrate (50 µL/well) was added to visualise the reaction, and the reaction stopped with H2O2 buffer. Optical densities (OD) were measured with a plate reader (TECAN Minilyser Spectra II, Tecan Group Ltd., Maennedorf, Switzerland) at a wavelength of 450 nm and a reference wavelength of 620 nm. OD readings were called positive when they were three × standard deviation higher than the negative samples.
Supernatant from samples reacting in this ELISA were re-inoculated onto fresh C6/36 cultures and incubated for 4 days at 28 °C. Supernatants were collected and plates fixed as described above. A panel of mAbs specific for a range of medically significant flaviviruses previously detected in Northern Australia (WNVKUN-specific—3.1112G, 10A1, 3.101C, 3.91D; MVEV-specific—10C6; JEV-specific 989; and KOKV-specific—1C1) were used to identify virus in an ELISA system as described above. The identity of detected virus was confirmed by a KOKV-specific RT-PCR and Sanger sequencing of the amplicon. The reactive sample was also deep sequenced (HiSeq, Illumina, San Diego, CA, USA), using standard methods that we have previously used for sequencing viruses from mosquitoes captured in crocodile farms, published in [2].
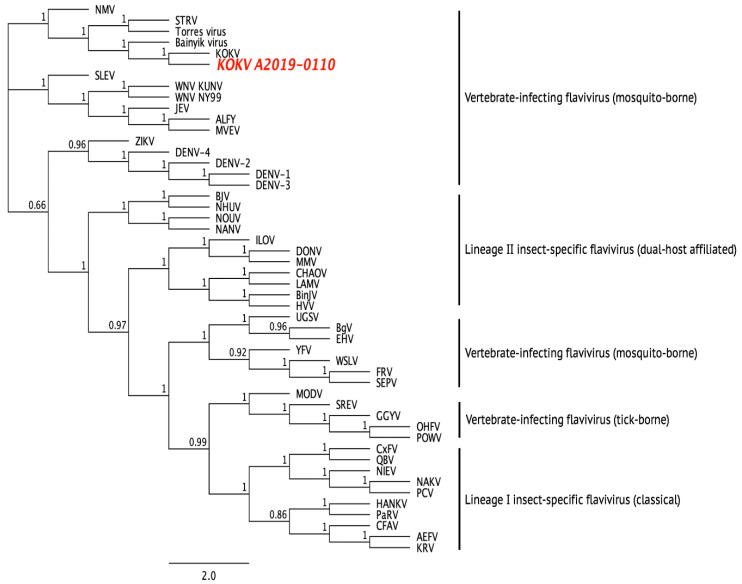
2.7. Phylogeny
Multiple amino acid sequence alignments of the new KOKV isolate (KOKVA2019-0110, accession number OL347997) and selected flaviviruses were performed with MAFFT v7.388 algorithm, using a scoring matrix of BLOSUM62, a gap open penalty of 1.53, and an offset value of 0.123 [45,46]. FastTree 2.1.5 was used to construct a phylogenetic tree that uses the maximum likelihood approximation method, with optimisation for Gamma20 likelihood selected, while the branch support values were calculated using a Shimodaira-Hasegawa test. Analyses were undertaken within the Geneious 11.1.5 package.
3. Results
3.1. WNVKUN and MVEV Surveillance on Crocodile Farms
Each trap contained two FTATM cards; a trap was classified as virus-positive when viral RNA was detected on at least one of the cards. Between Feb 2018 and July 2020, WNVKUN RNA was detected on FTATM cards in each year with the most detections occurring in the months of January to May (Table 1, Table S1), consistent with the increased mosquito activity during the monsoon season, late wet season, and the start of the dry season [47]. The most frequent WNVKUN activity was detected in March 2019 and April 2020, where traps on all three farms yielded positive cards, often with both cards in the trap positive for the virus, totaling 24 WNVKUN-positive and 8 MVEV-positive traps (Table S1).
Table 1.
WNVKUN- and MVE-positive FTATM cards from SMACK traps set between February 2018 and July 2020 compared to sentinel chicken seroconversions over the same period. Sentinel chicken program was run January to June.
| Croc Farm | Collection Period | Trap ID | Virus Detected (Positive Cards/Cards Set) |
Chicken Seroconversions Date; Chicken Farm; Virus |
|---|---|---|---|---|
| D1 | March–December 2018 | All Negative | April 2018; LF; MVEV | |
| January–February 2019 | 1 | WNVKUN (1/2) | ||
| February 2019 | 1 | WNVKUN (1/2) | ||
| February–March 2019 | 1 | WNVKUN (2/2) | ||
| 2 | WNVKUN (2/2) | |||
| May 2019 | 1 | WNVKUN (1/2) | ||
| April 2020 | 1 | WNVKUN (1/2) | January 2020; LF; WNVKUN | |
| 2 | WNVKUN (2/2) | |||
| D2 | March 2018 | 2 | WNVKUN (1/2) | |
| March–April 2018 | 1 | WNVKUN (1/2) | May 2018; HSF; MVEV | |
| June–July 2018 | 2 | MVEV (1/2) | ||
| February–March 2019 | 1 | WNVKUN (2/2) | ||
| 2 | WNVKUN (2/2) | March 2019; HSF; WNVKUN | ||
| July 2019 | 1 | WNVKUN (1/2), MVEV (1/2) | ||
| September–October 2019 | 1 | WNVKUN (2/2), MVEV (1/2) | ||
| April 2020 | 1 | WNVKUN (2/2), MVEV (1/2) | ||
| 2 | WNVKUN (1/2) | |||
| April–May 2020 | 1 | WNVKUN (1/2) | ||
| 2 | WNVKUN (1/2) | |||
| D3 | February –March 2018 | 1 | WNVKUN (1/2) | March 2018; BHF; WNVKUN |
| March–April 2018 | 2 | MVEV (2/2) | March 2018; BHF; MVEV | |
| April–May 2018 | 2 | MVEV (2/2) | May 2018; BHF; MVEV | |
| October–November 2018 | 1 | MVEV (1/2) | ||
| February–March 2019 | 1 | WNVKUN (2/2) | March 2019; BHF; WNVKUN | |
| 2 | WNVKUN (2/2) | |||
| January 2020 A | 2 | WNVKUN (1/2) | ||
| January 2020 B | 2 | WNVKUN (2/2) | ||
| April 2020 | 1 | WNVKUN (1/2) | ||
| May 2020 | 2 | MVEV (1/2) | ||
| June–July 2020 | 2 | WNVKUN (1/2) |
D1, D2, and D3 are crocodile farms in rural Darwin, NT; LF Leanyer Farm sentinel chicken flocks near D1; HSF Howard Springs Farm sentinel chicken flocks near D2; BHF Beatrice Hill Farm sentinel chicken flocks near D3.
In 2018, no virus was detected at crocodile farm D1 while WNVKUN RNA was detected at D2 in March and April and at D3 in March, with a total of three traps positive for WNVKUN RNA in the first year (Table 2). In 2019, WNVKUN RNA was detected in February, March, and May at D1; in March, July, and October at D2; and in March at D3, with a total of 11 traps positive for the virus (Table 2). In 2020, WNVKUN RNA was detected in January and again in July at D3, in April at all three crocodile farms, and in May at D2, with a total of 10 positive traps for this year (Table 2).
Table 2.
Number of SMACK traps set and numbers of virus-positive traps.
| 2018 | 2019 | 2020 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Farm Location |
# of Traps | WNVKUN
Pos |
MVEV Pos | # of Traps |
WNVKUN Pos | MVEV Pos | # of Traps |
WNVKUN Pos | MVEV Pos |
| D1 | 26 | 0 | 0 | 26 | 5 | 0 | 26 | 2 | 0 |
| D2 | 33 | 2 | 1 | 35 | 4 | 2 | 24 | 4 | 1 |
| D3 | 34 | 1 | 3 | 26 | 2 | 0 | 26 | 4 | 1 |
| 93 | 3 | 4 | 87 | 11 | 2 | 76 | 10 | 2 | |
| C1 | 16 | 0 | 0 | 16 | 0 | 0 | 12 | 0 | 0 |
D1, D2 and D3 are crocodile farms in rural Darwin, NT. C1 is a crocodile farm in rural Cairns, Qld.
Detections of MVEV RNA were sporadically spread between April and November over the two and a half years of trapping. Detection was most frequent in 2018, first appearing at D3 in April and in May and then again in November. It was detected once at D2 in July, with a total of four positive traps for MVEV RNA in this year (Table 2). In 2019, MVEV RNA was not detected until July and again in October, both times at D2. This correlated with the sporadic appearance of WNVKUN at D2, with both viruses detected in the same traps (Figure S1 and Table 2). In 2020, MVEV RNA was detected in April on the same cards as WNVKUN at D2 and was found in May on a single card at D3 (Table 2).
WNVKUN RNA was not detected on the Cairns crocodile farm (C1), where it was the only targeted virus.
In Darwin, detections of viral RNA on FTATM cards on the crocodile farms were compared with sentinel chicken seroconversion to flaviviruses at the Beatrice Hill Farm, the Leanyer, Howard Springs, and Bees Creek flocks (Figure 1). Between February 2018 and June 2020, five seroconversions to WNVKUN were detected: at Beatrice Hill Farm (near D3), a seroconversion was detected on 1 March 2018 and 7 March 2019; two at Howard Springs (near D2) on 13 March 2019; and one at Leanyer (near D1) on 8 January 2020 (Figure 1). Each of the seroconversions in 2018 and 2019 correlated with the detection of WNVKUN RNA on FTATM cards at nearby farms in the same time period. While there were no positive FTATM cards at D1 in January 2020 when seroconversion occurred in the nearby sentinel chicken flock at Leanyer, the FTATM cards were positive at D3 indicating WNVKUN activity in the general Darwin region.
Seroconversions to MVEV were only detected in 2018 (Table 1 and Table S1). At the Beatrice Hill Farm, sentinel chickens seroconverted to MVE on 29 March, and again on 3 May 2018. At Leanyer, one chicken seroconverted on 10 April 2018 and one at Howard Spring on 2 May 2018. The seroconversions at the Beatrice Hill Farm (29 March) correlated with MVEV being detected on cards in traps set on D3 (April-May). Sentinel chicken seroconversion to MVEV at the Beatrice Hill Farm on 29 March was also coincident with MVEV-positive FTATM cards detected in traps set at the nearby D3 farm (March–April). In the same locations, chicken seroconversion and positive FTATM cards correlated in April–May.
3.2. Virus Isolation
In 2018, 4380 mosquitoes were collected with the catches consisting mainly of Cx. annulirostris (62%) but also several other species, such as Mansonia uniformis, Anopheles bancroftii, Cx. palpalis, Cx. pullus, Cq. xanthogaster, and Cx. quinquefasciatus. When these mosquitoes were pooled and processed for virus isolation, no vertebrate-infecting flaviviruses such as MVE or WNVKUN were detected. However, several insect-specific viruses were isolated and will be reported elsewhere (Colmant et al. unpublished data).
In 2019, 6206 non-blood fed and identifiable mosquitoes from 17 EVS traps were tested for the presence of viruses, including 2620 Cx. annulirostris, 79 Cx. pullus, 42 Cx. quinquefasciatus, and 35 Cx. gelidus (Table 3). Other mosquito species tested, totalling 3430, are listed in Table 3. While no WNVKUN or MVEV was isolated, a flavivirus-like isolate was detected in one pool of Cx. annulirostris mosquitoes (A2019-0110) trapped at D3 on 28 March 2019 (Table 4). When culture supernatants from the cells inoculated with this sample were further passaged onto C6/36 cells and tested with a panel of mAbs specific for medically important flaviviruses, only the KOKV-specific mAb 1C1 was reactive to the fixed inoculated cells. The identity of this virus was confirmed as Kokobera by a KOKV-specific RT-PCR and whole genome sequencing. BLAST analysis of the genome contig derived from sequencing data showed a high degree of similarity with the prototype KOKV virus (accession number NC_009029 [48]). Sequence alignment of the complete ORF of the new isolate further confirmed its identity as a new strain of KOKV (Figure 3).
Table 3.
Mosquito species collected at Darwin crocodile farms in 2019.
| Mosquito Species | Number | Sub-Totals | |
|---|---|---|---|
| Known/potential WNVKUN vectors | Culex annulirostris | 2620 | |
| Cx. pullus | 79 | ||
| Cx. quinquefasciatus | 42 | ||
| Cx. gelidus | 35 | 2776 | |
| Other species | Mansonia uniformis | 1707 | |
| Cx. species | 620 | ||
| Anopheles bancroftii | 597 | ||
| Coquillettidia xanthogaster | 413 | ||
| Cx. squamosus | 67 | ||
| Cx. bitaeniorhynchus | 9 | ||
| Cx. hilli | 6 | ||
| Cx. vishnui group | 3 | ||
| Aedes kochi | 2 | ||
| Ae. vigilax | 1 | ||
| An. powelli | 1 | ||
| Cx. vishnui | 1 | ||
| Uranotaenia albescens | 1 | ||
| Ur. lateralis | 1 | ||
| Ur. nivipes | 1 | 3430 | |
| Total | 6206 | ||
Table 4.
Virus isolation attempts from Cx. annulirostris mosquitoes collected in EVS traps set on Darwin crocodile farms in 2019.
| Location | Date Traps Set | No. Cx. annulirostris Processed Mosquitoes/Pools | Virus Isolation Positive Pool ID; Virus |
|---|---|---|---|
| D1 | 5 March 2019 | 698/16 | None |
| 20 March 2019 | 93/5 | None | |
| D3 | 28 March 2019 | 951/21 | A2019-0110; KOKV |
| 12 April 2019 | 878/19 | None | |
| Total | 2620/61 | 1 |
D1 and D3 are crocodile farms in rural Darwin, NT; KOKV Kokobera virus.
Figure 3.
Dendrogram showing phylogenetic relationship between the prototype KOKV, KOKV A2019-0110, and other flaviviruses using a maximum-likelihood model and complete amino acid sequences. Sequences were derived using the following GenBank accession numbers: AEFV AB488408, ALFV AY898809, Bainyik virus KM225264, BgV KU308380, BinJV MG587038, BJV KC496020, CFAV KJ741267, CHAOV JQ308185, CxFV AB262759, DENV-1 U88536, DENV-2 U87411, DENV-3 AY099336, DENV-4 AF326825, DONV NC_016997, EHV DQ859060, FRV KM361634, GGYV DQ235145, HANKV NC_030401, HVV MN954647, ILOV KC734549, JEV NC_001437, KOKV AY632541, KOUV MN057643, KRV AY149905, LAMV KC692068, MMV MF139576, MODV AJ242984, MVEV AF161266, NAKV NC_030400, NANV MF139575, NHUV KJ210048, NIEV JQ957875, NMV KC788512, NOUV EU159426, OHFV AY193805, PaRV KT192549, PCV KC505248, POWV L06436, QBV FJ644291, SEPV DQ837642, SREV DQ235150, STRV KM225263, Torres virus KM225265, UGSV DQ859065, WNV KY229074, WSLV JN226796, YFV X03700, and ZIKV AY632535.
4. Discussion
In this study, we successfully established the FTATM card surveillance system on crocodile farms in the Northern Territory and north Queensland and detected WNVKUN and/or MVEV transmission on each farm except for north Queensland. As expected, transmission was most prevalent between January to May which is generally considered the period of peak arbovirus activity. We and others have previously validated FTATM cards as an effective arbovirus surveillance system for several mosquito-borne viruses in a range of environments and locations [27,30,32,49,50,51,52]. However, this was the first report of its use to monitor virus transmission in the context of farmed crocodilians and to guide the frequency and timing of mosquito control strategies (e.g., spraying). Indeed, when compared to a nearby concurrently run program based on the seroconversion of sentinel chickens, transmission was detected more frequently by FTATM cards on crocodile farms than by sentinel chicken surveillance conducted in the same timeframe. Discrepancies between the two surveillance systems may be attributed to random differences in the transmission frequency between the different locations of the sentinel chicken flocks relative to the crocodile farms within the Darwin region, or to a difference in sensitivity between the two systems. The increased detection of viral transmission on crocodile farms may also reflect the unique transmission dynamic of WNVKUN that can occur directly between farmed crocodilian species, thus providing additional sources of mosquito infection and transmission [2]. However, to date, this has only been demonstrated for alligators. Thus, regular testing of crocodile pen water for viral RNA should also be considered to monitor other avenues of WNVKUN transmission on farms.
Despite evidence of their presence on FTATM cards on the farms, we failed to isolate WNVKUN or MVEV from mosquitoes trapped in close proximity and within the same time frame of positive FTATM card detections. This suggested that there was a low prevalence of virus in the mosquito population, consistent with only one of four FTATM cards usually yielding a positive result on each farm at each transmission event and is further supported by the relatively high Ct scores (>35) that were generally observed. However, while EVS traps were set immediately after the FTATM cards were reported to be positive for WNVKUN or MVEV RNA, we cannot rule out the possibility that we had already missed a narrow window of transmission by the time the mosquitoes were collected. Reduced overall mosquito numbers from routine mosquito control measures (spraying) may also have reduced our ability to isolate these viruses.
Interestingly, no human cases due to WNVKUN infection were reported during our trapping period and only one case of MVEV infection occurred in early May 2018 (a resident of a remote area of Arnamland in NT, approximately >200 kms East of the Darwin region who was not associated with crocodile farms).
The isolation of Kokobera virus from a trap set at D3 in 2019 is worthy of further investigation. It is feasible that this flavivirus could infect and cause disease in crocodiles, even though it is considered a relatively benign virus and has only ever been associated with rare cases of a mild febrile illness in humans manifesting as polyarthralgia, headache, and skin lesions [15]. Furthermore, the detection of MVEV RNA on FTATM cards collected on the farms indicates that, in addition to WNVKUN, this virus could also be transmitted to crocodiles and cause disease. Future studies should be directed at sampling farmed crocodiles and testing for the presence of MVEV- and KOKV- specific antibodies in serum as evidence that these viruses can productively infect these animals.
While WNVKUN and/or MVEV activity was detected in all the investigated years by FTATM card surveillance on the crocodile farms in the Darwin region, the same surveillance program on farms in Cairns did not detect RNA from WNVKUN on any of the cards collected over the entire study period (cards were not tested for MVEV RNA). This is consistent with our understanding of the epidemiology of WNVKUN and MVEV, which are regularly detected in the region around Darwin in the Northern Territory and the northern and western regions of Cape York Peninsula in Queensland, but rarely detected on the eastern side of Cape York where Cairns is situated [25,29,30].
5. Conclusions
In conclusion, we have successfully established the FTATM card surveillance system on crocodile farms and have shown that it is a reliable indicator of the transmission of WNVKUN and MVEV on farms during times of peak activity around Darwin. This can provide a timely warning to implement control measures to reduce WNVKUN disease in crocodiles by vector control. The early detection of the transmission of these viruses on crocodile farms near Darwin also has important “One Health” implications, allowing more timely intervention of vector control measures to protect residents of the Darwin region from arboviral infections.
Acknowledgments
Thank you to P. Burtonclay from the cell culture unit at the Public Health Virology laboratory for preparing the C6/36 cell plates used for the virus isolation. We would like to acknowledge all Medical Entomology staff in Darwin involved in mosquito identifications and preparation for the virus isolation work.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/v14061342/s1, Table S1: Summary of FTA results and sentinel chicken data collected from Darwin region over the course of the study (2018–2019, sentinel chicken program run January–June).
Author Contributions
Conceptualization, S.H.-M., S.R.I., R.A.H., N.K.; methodology, S.H.-M., J.L.M., N.K., A.M.G.C., J.J.H., D.M.S., A.W.; formal analysis, J.L.M., N.K., S.H.-M., A.W., A.M.G.C., J.J.H.; investigation, N.K., S.H.-M., J.B., G.H., J.L.M., S.R.I., A.W., A.M.G.C., J.M., S.A.R., D.M.S., M.T., K.M.S.; resources, S.R.I., S.H.-M., F.M., J.L.M., R.A.H., N.K.; data curation, J.L.M., J.J.H.; writing—original draft preparation, N.K., S.H.-M., S.R.I., R.A.H., A.W., J.J.H.; writing—review and editing, all authors; project administration, S.R.I., S.H.-M., N.K., R.A.H.; funding acquisition, S.R.I., S.H.-M., R.A.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Charles Darwin University Research Ethics Committee.
Data Availability Statement
Data supporting the reported sentinel results can be found at: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/11788/1/Medical%20Entomology%20Annual%20Report%202019_2020.pdf. Date Accessed: 1 June 2022.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by a CRC for Developing Northern Australia grant CRC-P58588.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Isberg S.R., Moran J.L., De Araujo R., Elliott N., Davis S.S., Melville L. First evidence of Kunjin strain of West Nile virus associated with saltwater crocodile (Crocodylus porosus) skin lesions. Aust. Vet. J. 2019;97:390–393. doi: 10.1111/avj.12862. [DOI] [PubMed] [Google Scholar]
- 2.Habarugira G., Moran J., Colmant A.M., Davis S.S., O’Brien C.A., Hall-Mendelin S., McMahon J., Hewitson G., Nair N., Barcelon J., et al. Mosquito-Independent Transmission of West Nile virus in Farmed Saltwater Crocodiles (Crocodylus porosus) Viruses. 2020;12:198. doi: 10.3390/v12020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frost M.J., Zhang J., Edmonds J.H., Prow N.A., Gu X., Davis R., Hornitzky C., Arzey K.E., Finlaison D., Hick P., et al. Characterization of virulent West Nile virus Kunjin strain, Australia. Emerg. Infect. Dis. 2012;18:792–800. doi: 10.3201/eid1805.111720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prow N., Edmonds J., Williams D., Setoh Y., Bielefeldt-Ohmann H., Suen W., Hobson-Peters J., van den Hurk A., Pyke A., Hall-Mendelin S., et al. Virulence and evolution of West Nile Virus, Australia, 1960–2012. Emerg. Infect. Dis. 2016;22:1353–1362. doi: 10.3201/eid2208.151719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prow N. The changing epidemiology of Kunjin virus in Australia. Int. J. Environ. Res. Public Health. 2013;10:6255–6272. doi: 10.3390/ijerph10126255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackenzie J.S., Lindsay M.D., Coelen R.J., Broom A.K., Hall R.A., Smith D.W. Arboviruses causing human disease in the Australasian zoogeographic region. Arch. Virol. 1994;136:447–467. doi: 10.1007/BF01321074. [DOI] [PubMed] [Google Scholar]
- 7.Russell R. Vectors vs humans in Australia- who is on top down under? An update on vector-borne disease and research on vectors in Australia. J. Vect. Ecol. 1998;23:1–46. [PubMed] [Google Scholar]
- 8.Russell R., Dwyer D. Arboviruses associated with human disease in Australia. Microbes Infect. 2000;2:1693–1704. doi: 10.1016/S1286-4579(00)01324-1. [DOI] [PubMed] [Google Scholar]
- 9.Hall R.A., Broom A.K., Smith D.W., Mackenzie J.S. The ecology and epidemiology of Kunjin virus. Curr. Top. Microbiol. Immunol. 2002;267:253–269. doi: 10.1007/978-3-642-59403-8_13. [DOI] [PubMed] [Google Scholar]
- 10.Standfast H., Barrow G. Studies of the epidemiology of arthropod-borne virus infections at Mitchel River Mission, Cape York Peninsula, North Queensland. I. Mosquito collections, 1963–1966. Trans. R. Soc. Trop Med. Hyg. 1968;62:418–429. doi: 10.1016/0035-9203(68)90094-1. [DOI] [PubMed] [Google Scholar]
- 11.Doherty R., Carley J., Mackerras M., Marks E. Studies of arthropod-borne virus infections in Queensland III. Isolation and characterisation of virus strains from wild-caught mosquitoes in North Queensland. Austral. J. Exp. Biol. 1963;41:17–40. doi: 10.1038/icb.1963.2. [DOI] [PubMed] [Google Scholar]
- 12.Russell R. Arboviruses and their vectors in Australia: An update on the ecology and epidemiology of some mosquito-borne arboviruses. Rev. Med. Vet. Entomol. 1995;83:141–158. [Google Scholar]
- 13.Smith D., Speers D., Mackenzie J. The viruses of Australia and the risk to tourists. Travel Med. Infect. Dis. 2011;9:113–125. doi: 10.1016/j.tmaid.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Hall R., Aaskov J. Feigin and Cherry’s Textbook of Pediatric Infectious Diseases. 8th ed. Elsevier; Amsterdam, The Netherlands: 2017. Murray Valley encephalitis virus. [Google Scholar]
- 15.Boughton C., Hawkes R., Naim H. Illness caused by Kokobera-like virus in aouth-eastern Australia. Med. J. Aust. 1986;145:90–92. doi: 10.5694/j.1326-5377.1986.tb101087.x. [DOI] [PubMed] [Google Scholar]
- 16.Kurucz N. ((Centre for Disease Control Northern Territory Health, Atlanta, GA, USA)). Mosquito Investigation and Management Recommendations. Lagoon Crocodile Farm, March 2019. Personal Communication. 2019.
- 17.Kurucz N. ((Centre for Disease Control, Atlanta, GA, USA)). Mosquito Investigation and Management Recommendations. Janamba Crocodile Farm, March and April. Personal Communication. 2019.
- 18.Kurucz N. ((Centre for Disease Control, Atlanta, GA, USA)). Mosquito Investigation. Darwin Crocodile Farm, April and May. Personal Communication. 2019.
- 19.Johansen C., Power S., Broom A. Determination of mosquito (Diptera: Culicidae) bloodmeal sources in Western Australia: Implications for arbovirus transmission. J. Med. Ecol. 2009;46:1167–1175. doi: 10.1603/033.046.0527. [DOI] [PubMed] [Google Scholar]
- 20.Kay B., Fanning I., Carley J. Vector competence of Culex pipiens quinquefasciatus for Murray Valley encephalitis, Kunjin and Ross River viruses from Australia. Am. J. Trop. Med. Hyg. 1982;31:844–848. doi: 10.4269/ajtmh.1982.31.844. [DOI] [PubMed] [Google Scholar]
- 21.Webb C., Doggett S., Russell R. A Guide to Mosquitoes of Australia. CSIRO; Clayton South, VC, Canada: 2016. [Google Scholar]
- 22.Andrealis T. The contribution of Culex pipiens complex mosquitoes to transmission and persistance of West Nile virus in North America. J. Am. Mosqu. Control Assoc. 2012;28:137–151. doi: 10.2987/8756-971X-28.4s.137. [DOI] [PubMed] [Google Scholar]
- 23.Unlu I., Kramer W., Roy A., Foil L. Detection of West nile virus RNA in mosquitoes and identification of mosquito blood meals collected at Alligator Farms in Louisiana. J. Med. Entomol. 2010;47:625–633. doi: 10.1093/jmedent/47.4.625. [DOI] [PubMed] [Google Scholar]
- 24.Johansen C., Broom A., Lindsay M., Avery V., Power S., Dixon G., Sturrock K., Maley F., Mcfall S., Geerlings K., et al. Arbovirus and vector surveillance in Western Australia, 2004/05 to 2007/08. Arbovirus Res. Aust. 2009;10:76–81. [Google Scholar]
- 25.Johnson P., Hall-Mendelin S., Whelan P., Frances S., Jansen C., Mackenzie D., Northill J., van den Hurk A. Vector competence of Australian Culex gelidus Theobald (Diptera: Culicidae) for endemic and exotic arboviruses. Aust. J. Entomol. 2009;48:234–240. doi: 10.1111/j.1440-6055.2009.00711.x. [DOI] [Google Scholar]
- 26.Sudeep A., Ghodke Y., Gokhale M., George R., Dhaigude S., Bondre V. Replication potential and different modes of transmission of West nile virus in an Indian strain of Culex gelidus Theobald (Diptera: Culicidae) mosquitoes. J. Vector Borne Dis. 2014;51:333–338. [PubMed] [Google Scholar]
- 27.Hall-Mendelin S., Ritchie S., Johansen C., Zborowski P., Cortis G., Danbridge S., Hall R., van den Hurk A. Exploiting mosquito sugar feeding to detect mosquito-borne pathogens. Proc. Natl. Acad. Sci. USA. 2010;107:11255–11259. doi: 10.1073/pnas.1002040107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Floridis J., McGuinness S., Kurucz N., Burrow J., Baird R., Francis J. Murray Valley encephalitis virus: An ongoing cause of enceohalitis in Australia’s north. Trop. Med. Infect. Dis. 2018;3:49. doi: 10.3390/tropicalmed3020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson B., Kerlin T., Hall-Mendelin S., van den Hurk A., Cortis G., Doggett S., Toi C., Fall K., McMahon J., Townsend M., et al. Development and field evaluation of the sentiel mosquito arbovirus capture kit (SMACK) Parasites Vectors. 2015;8:509. doi: 10.1186/s13071-015-1114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurucz N., Wenham J., Hunt N., Melville L. Murray Valley encephalitis virus detection using honeybait cards in the Northern Territory in 2013. Mosq. Bites. 2014;1:14–16. [Google Scholar]
- 31.Ritchie S., Cortis G., Paton C., Townsend M., Shroyer D., Zborowski P., Hall-Mendelin S., van den Hurk A. A simple non-powered passive trap for the collection of mosquitoes for arbovirus surveillance. J. Med. Entomol. 2013;50:185–194. doi: 10.1603/ME12112. [DOI] [PubMed] [Google Scholar]
- 32.van den Hurk A., Hall-Mendelin S., Townsend M., Kurucz N., Edwards J., Ehlers G., Rodwell C., Moore F., McMahon J., Northill J., et al. Applications of a sugar-based surveillance system to track arboviruses in wild mosquito populations. Vector-Borne Zoonotic Dis. 2014;14:66–73. doi: 10.1089/vbz.2013.1373. [DOI] [PubMed] [Google Scholar]
- 33.Government N.T. Medical Entomology Annual Report 2013/14. Department of Health; Washington, DC, USA: 2015. [Google Scholar]
- 34.Pyke A., Smith I., van den Hurk A., Northill J., Chuan T., Westacott A., Smith G. Detection of Australasian Flavivirus encephalitic viruses using rapid fluorogenic TaqMan RT-PCR assays. J. Virol. Methods. 2004;117:161–167. doi: 10.1016/j.jviromet.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Smith G., Smith I., Harrower B., Warrilow D., Bletchly C. A simple method for preparing synthetic controls for conventional and real-time PCR for the identification of endemic and exotic disease agents. J. Virol. Methods. 2006;135:229–234. doi: 10.1016/j.jviromet.2006.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Knope K., Doggett S.L., Jansen C.C., Johansen C.A., Kurucz N., Feldman R., Lynch S.E., Hobby M.P., Sly A., Jardine A., et al. Arboviral Diseases and Malaria in Australia, 2014–2015: Annual Report of the National Arbovirus and Malaria Advisory Committee. Commun. Dis. Intell. 2019;43:1–69. doi: 10.33321/cdi.2019.43.14. [DOI] [PubMed] [Google Scholar]
- 37.Resources, Northern Territory Department of Primary Industry . Berrimah Virology Laboratory Virology Test. Methods Manual: Virus Neutralisation Tests, Issue 10. 2017. pp. 43–50. [Google Scholar]
- 38.Lee D., Hicks M., Griffiths M., Debenham M. The Culicidae of the Australasian Region. Volume 11 University of Queensland and University of Sydney in collaboration with Commonwealth Department of Community Services and Health; Canberra, Australia: 1989. [Google Scholar]
- 39.Lee D., Hicks M., Griffiths M., Debenham M., Bryan J., Marks E. The Culicidae of the Australasian Region. Volume 9 Commonwealth Department of Health and School of Public Health and Tropical Medicine; Canberra, Australia: 1988. [Google Scholar]
- 40.Lee D., Hicks M., Griffiths M., Debenham M., Bryan J., Russell R., Geary M., Marks E. The Culicidae of the Australasian Region. Volume 4 Commonwealth Department of Health and School of Public Health and Tropical Medicine; Canberra, Australia: 1987. [Google Scholar]
- 41.Lee D., Hicks M., Griffiths M., Debenham M., Bryan J., Russell R., Geary M., Marks E. The Culicidae of the Australasian Region. Volume 8 Commonwealth Department of Health and School of Public Health and Tropical Medicine; Canberra, Australia: 1988. [Google Scholar]
- 42.Lee D., Hicks M., Griffiths M., Russell R., Marks E. The Culicidae of the Australasian Region. Volume 2 Commonwealth Department of Health and Commonwealth Institute of Health, Incorporating School of Public Health and Tropical Medicine; Canberra, Australia: 1982. [Google Scholar]
- 43.Lee D., Hicks M., Griffiths M., Russell R., Marks E. The Culicidae of the Australasian Region. Volume 3 Commonwealth Department of Health and Commonwealth Institute of Health, Incorporating School of Public Health and Tropical Medicine; Canberra, Australia: 1984. [Google Scholar]
- 44.Broom A.K., Hall R.A., Johansen C.A., Oliveira N., Howard M.A., Lindsay M.D., Kay B.H., Mackenzie J.S. Identification of Australian arboviruses in inoculated cell cultures using monoclonal antibodies in ELISA. Pathology. 1998;30:286–288. doi: 10.1080/00313029800169456. [DOI] [PubMed] [Google Scholar]
- 45.Katoh K., Misawa K., Kuma K., Miyata T. MAFFT: A novel method for rapid multiple sequence alignment based on fast Fourier transform. Nucleic Acids Res. 2002;30:3059–3066. doi: 10.1093/nar/gkf436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Katoh K., Standley D. MAFFT Multiple Sequence Alignment Software Version 7: Improvements in Performance and Usability. Mol. Biol. Evol. 2012;30:772–780. doi: 10.1093/molbev/mst010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurucz N., Jacups S., Carter J. Determining Culex annulirostris larval densities and control efforts across a coastal wetland, Northern Territory, Australia. J. Vect. Ecol. 2016;41:271–278. doi: 10.1111/jvec.12222. [DOI] [PubMed] [Google Scholar]
- 48.Kuno G., Chang G.J. Biological transmission of arboviruses: Reexamination of and new insights into components, mechanisms, and unique traits as well as their evolutionary trends. Clin. Microbiol. Rev. 2005;18:608–637. doi: 10.1128/CMR.18.4.608-637.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wipf N., Guidi V., Tonolla M., Ruinelli M., Müller P., Engler O. Evaluation of honey-baited FTA cards in combination with different mosquito traps in an area of low arbovirus prevalence. Parasites Vectors. 2019;12:554. doi: 10.1186/s13071-019-3798-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Birnberg L., Temmam S., Aranda C., Correa-Fiz F., Talavera S., Bigot T., Eloit M., Busquets N. Viromics on Honey-Baited FTA cards as a New Tool for the Detection of circulating Viruses in Mosquitoes. Viruses. 2020;12:274. doi: 10.3390/v12030274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kurucz N., Minney-Smith C., Johansen C. Arbovirus surveillance using FTA cards in modified CO2-baited encephalitis virus traps in the Northern Territory, Australia. J. Vec. Ecol. 2019;44:187–194. doi: 10.1111/jvec.12343. [DOI] [PubMed] [Google Scholar]
- 52.Fynmore N., Luhken R., Maisch H., Risch T., Merz S., Kliemke K., Ziegler U., Schmidt-Chanasit J., Becker N. Rapid assessment of West Nile virus circulation in a German zoo based on honey-baited FTA cards in combination with box gravid traps. Parasites Vectors. 2021;14:449. doi: 10.1186/s13071-021-04951-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data supporting the reported sentinel results can be found at: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/11788/1/Medical%20Entomology%20Annual%20Report%202019_2020.pdf. Date Accessed: 1 June 2022.