“Ms. A,” a 27-year-old, single, college-educated, primigravid Caucasian woman, was hospitalized after she crashed in an all-terrain vehicle and suffered a liver laceration. A urine drug screen detected benzodiazepines, methamphetamine, and marijuana. At her initial prenatal appointment 5 weeks later, she reported taking alprazolam on several occasions for anxiety but declined psychiatric referral. Over several weeks, she visited the emergency department several times to obtain opioid medications for pain.
At 21 weeks’ gestation, Ms. A presented to the emergency department requesting detoxification from opioids. She reported that she was currently taking approximately 60 mg of oxycodone daily and had an extensive history of prescription medication abuse, obtained from multiple providers as well as from friends and family. She had previously participated in methadone and buprenorphine maintenance programs. Ms. A had a history of anxiety and depression resulting in two psychiatric hospitalizations. She had been treated with alprazolam, fluoxetine, and bupropion, but she discontinued these medications, as she “felt better off of them.”
Physical examination, review of systems, and laboratory results were unremarkable. The examining physician discussed treatment options, including inpatient detoxification or stabilization and enrollment in an opioid maintenance program. After providing informed consent, Ms. A opted for enrollment in the buprenorphine maintenance program within the Women’s Mental Health Program (WMHP). The WMHP provides comprehensive treatment for neuropsychiatric illnesses during the perinatal period, with specialized services for substance use, including licit substances such as tobacco and alcohol. Ms. A denied use of tobacco and reported that she had discontinued use of alcohol when she learned that she was pregnant. On admission, her physician started her on buprenorphine, and her dosage was adjusted to 8 mg/day by the time of discharge. State laws regarding perinatal substance use were reviewed with the patient. Consistent with state law addressing drug testing in the postpartum period, no report to the Department of Human Services (DHS) was made during admission.
Course of Outpatient Treatment
Ms. A adhered to weekly medication management and group and individual therapy, and she had a negative urine drug screen for 3 weeks. At 26 weeks’ gestation, she developed pain in her right leg requiring hospitalization. After a diagnosis of deep vein thrombosis involving popliteal, femoral, and iliac veins, she was started on anticoagulant therapy. She participated in the buprenorphine program inconsistently for several weeks after that, presenting to the emergency department multiple times requesting pain medication. Eventually, she resumed weekly follow-up visits in maintenance treatment.
At 39 weeks’ gestation, Ms. A underwent routine induction and uncomplicated vaginal delivery. Drug testing of the neonate was negative, and no report was filed with DHS, in accordance with state law. Ms. A and her baby were discharged. She brought the baby to all postpartum maintenance clinic visits, appearing attentive and engaged with the baby. There was no evidence of mistreatment or neglect. Over the course of her treatment, Ms. A completed 18 urine drug screens during pregnancy through 6 months postpartum, with nine screens detecting opioids, benzodiazepines, or both, and one detecting methamphetamine.
Ms. A continued to struggle with opioid and benzodiazepine abuse, and she interacted with the DHS case worker completing ongoing assessments. She participated in weekly appointments in the WMHP buprenorphine program but declined referrals to residential substance use treatment. She left the program at 6 months postpartum.
DISCUSSION
Although much of the focus in treatment of psychiatric illness in pregnancy has been on mood disorders, the prevalence of substance abuse rivals that of major depressive disorder during pregnancy (1). A survey of drug use and health indicated that 5.4% of pregnant women ages 15–44 used illicit drugs (marijuana, cocaine, heroin, hallucinogens, inhalants, or nonmedical use of prescription medications) at the time of the study (2). Illicit drug use occurred more frequently during the first and second trimesters than during the third trimester, and it was highest among respondents ages 15–17 (2). However, the clinical identification of substance abuse during pregnancy largely relies on patient report, and the rigor and documentation of screening varies. Despite discordant data, evidence supports an increased potential for adverse effects associated with prenatal exposure to both licit and illicit substances (3).The long-term consequences of neonatal abstinence syndrome (NAS) are not well characterized, however. Prescription medication abuse represents an unknown hazard for the offspring, subject to scrutiny under the legal statutes for substance abuse in the perinatal period.
The prevalence of substance abuse, combined with its possible consequences, has led jurisdictions to adopt a variety of approaches in dealing with this problem. State supreme court rulings in Alabama, Mississippi, and New Jersey (4–7), along with legislation in Tennessee (8), spurred significant debate regarding the criminalization of perinatal substance abuse. Practitioners should be aware of their districts’ legal requirements involving perinatal substance abuse. The interface of legal issues and clinical care for this population has led many medical societies to publish position statements on this issue.
Legal Issues
Current statutes regarding substance abuse during pregnancy vary around the United States (Figures 1 and 2). According to the Guttmacher Institute (9), 18 states consider drug abuse during pregnancy to be child abuse; it is usually only deemed abuse when the substance is detected either during pregnancy or at birth, depending on the jurisdiction, and when there is a risk to the health of the child (9). Tennessee law holds that substance abuse during pregnancy is assault if the child is born addicted to or harmed by drug use (8, 9). Three states—Minnesota, South Dakota, and Wisconsin—consider substance abuse during pregnancy grounds for civil commitment, which can include inpatient drug treatment (9). Fifteen states require reporting of mothers suspected of substance abuse, and four states require testing of mothers suspected of substance abuse (9).
FIGURE 1.
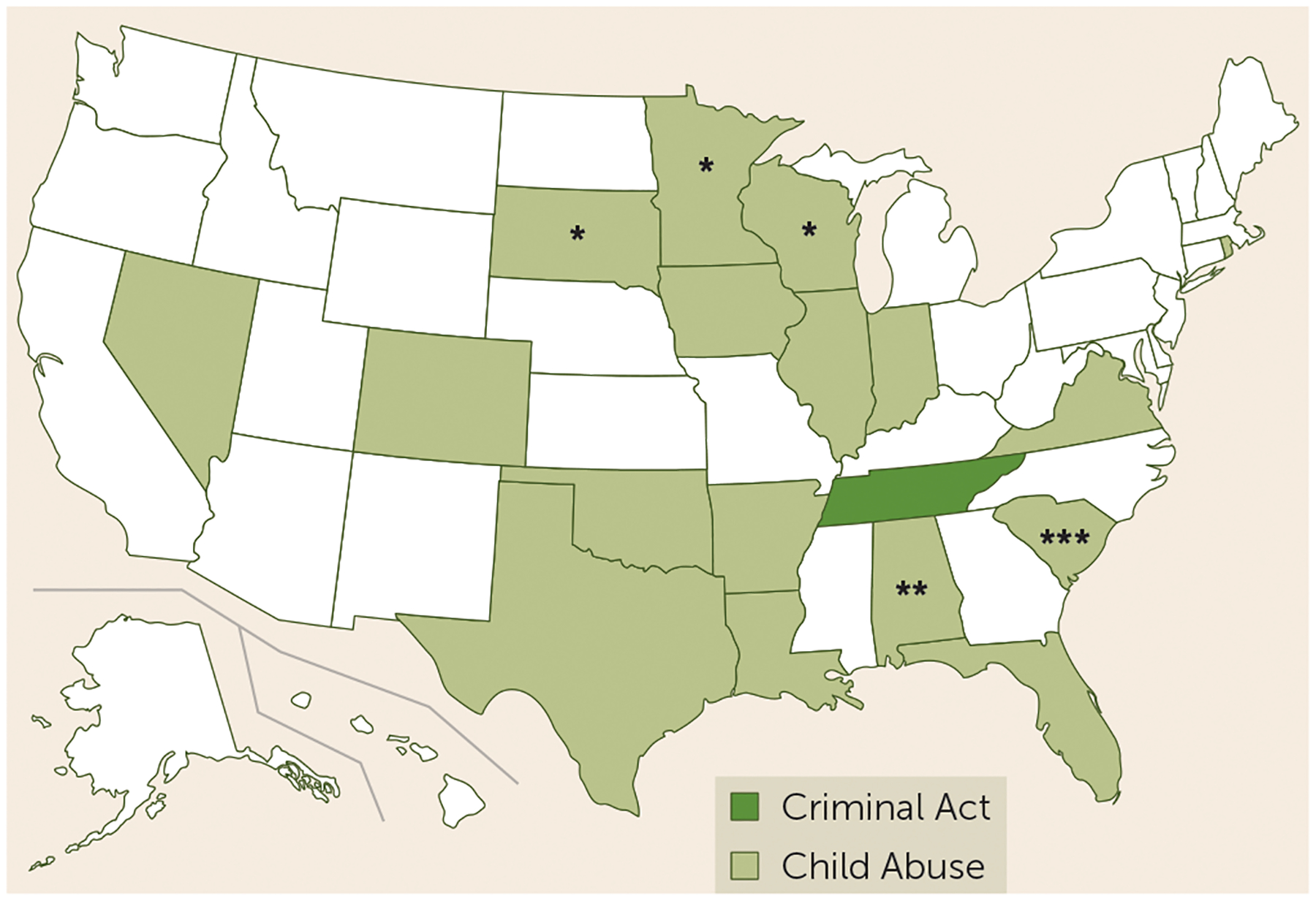
Pregnancy Substance Abuse Policies, by Statea
a Data are from reference 9.
*Grounds for civil commitment.
**Chemical endangerment of a child, per Alabama Supreme Court.
***Criminal child abuse, per South Carolina Supreme Court.
FIGURE 2.
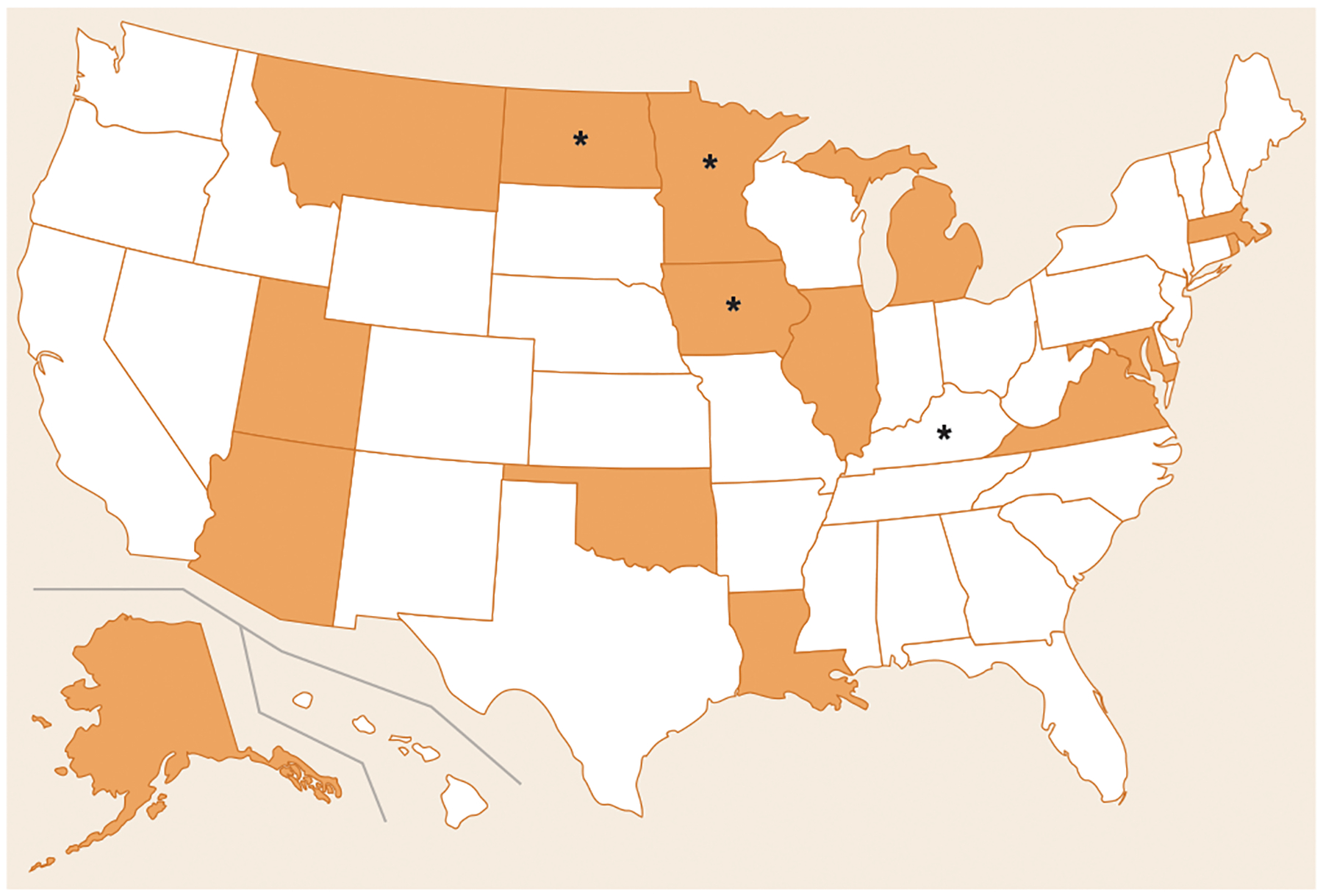
States With Mandatory Reporting of Suspected Substance Abuse During Pregnancya
a Data are from reference 9.
*Require testing if substance abuse during pregnancy is suspected.
Notably, there are statuary inconsistencies within states. For example, in Tennessee substance abuse during pregnancy is considered assault, yet no requirement exists for either reporting or testing of pregnant women suspected of substance abuse. Conversely, in Arizona, substance abuse is not defined as a criminal act or child abuse, yet there is a mandatory reporting requirement.
Not only do the state statutes vary, but case law varies as well, further complicating the clinician’s duties. For example, the Alabama Supreme Court ruled that substance abuse during pregnancy is “chemical endangerment of a child” (4,5), and the South Carolina Supreme Court held that substance abuse during pregnancy constitutes criminal child abuse (10). However, the New Jersey Supreme Court in 2013 ruled that substance abuse during pregnancy does not constitute abuse or neglect if there is no evidence of harm to the child (7).
The case of Ms. A in the vignette illustrates the need for clinicians to know their jurisdictions’ policies on substance use during pregnancy. In Arkansas, there is no law criminalizing substance use during pregnancy, and it is not considered child abuse. However, if a drug screen of Ms. A’s newborn had been positive, a Department of Human Services investigation would have been opened after mandatory reporting by the physician. In Tennessee, Alabama, or South Carolina, Ms. A could have been prosecuted. In Wisconsin, repeated drug use during pregnancy could have been used as grounds for involuntary commitment.
Official Positions of Professional Associations
In contrast to the legal variability, medical professional organizations have issued statements that carry common themes, focusing on noncriminalization and enhanced access to care.
American Psychiatric Association (APA).
The APA Board of Trustees published its “Position Statement on Care of Pregnant and Newly Delivered Women Addicts” in 2001 and reaffirmed it in 2007 (11). APA opposes criminal penalties for “pregnant and/or newly delivered women on child abuse charges based solely on the use of substances during pregnancy,” holding that penalties may be appropriate after the birth of the child if evidence of abuse and neglect is present. APA promotes “adequate prenatal care” for pregnant addicts “without fear of punitive consequences.” Additionally, APA supports a move away from criminal actions and toward the development and implementation of preventive and treatment options for women and children affected by addiction. Finally, “APA opposes involuntary commitment laws that are applied only to pregnant women in ways that do not apply to men or women who are not pregnant” (11).
American Academy of Addiction Psychiatry (AAAP).
The AAAP policy, revised in 2015, promotes “voluntary screening and testing of pregnant women for substance use disorders and mental illness for the purpose of providing prenatal care” and opposes mandatory reporting of substance abuse in pregnancy (12). Additionally, AAAP promotes voluntary treatment services for women who abuse substances during pregnancy. Finally, AAAP supports improved access to services as well as research and development of treatment methods for and prevention of substance abuse during pregnancy.
American Medical Association (AMA).
Current AMA policy parallels APA’s position, holding that “transplacental drug transfer should not be subject to criminal sanctions or civil liability” (13). AMA promotes education of the consequences of drug abuse during pregnancy and the need for treatment programs for mothers, while opposing criminal legislation of maternal substance abuse (13).
American College of Obstetricians and Gynecologists (ACOG).
The ACOG Committee on Health Care for Underserved Women presented a Committee Opinion, reaffirmed in 2014, regarding the “disturbing trend in legal actions and policies” involving the “criminalization of substance abuse during pregnancy when it is believed to be associated with fetal harm or adverse perinatal outcomes” (14). ACOG cites in-effectiveness of legal threats or actual incarceration in reducing alcohol or drug abuse during pregnancy and argues that addiction is a “biological and behavioral disorder with genetic components” and that imposing legal penalties implies that addiction is moral failing rather than a disease (14). Similar to APA and AMA, ACOG recommends that obstetricians and gynecologists work with governments to increase the development and availability of substance use treatment programs for pregnant women (14).
Schism Between Public Policy and Professional Opinion
Considerable discrepancies exist between jurisdictions’ statues regarding substance abuse during pregnancy and the official positions of professional associations. The schism between public policy and professional opinion is exemplified by the recent Tennessee legislation described above (8). This dichotomy between medical and legal arenas is difficult to explain.
A professional society’s opinion may be based largely on the scientific literature, and it has the luxury of being able, at times, to ignore philosophical issues. In contrast, legislators’ actions may be influenced by factors related to personal beliefs, public opinion, economic pressures, and the feasibility of implementing recommendations made by experts. Legislators may have to consider the philosophical and religious beliefs of their constituents, including the definition of personhood, the right to life, and fetal rights.
RECOMMENDATIONS
The breadth and variety of factors implicated in perinatal substance abuse complicates the practitioner’s dilemma. What is the physician’s role in the patient’s care? What are physicians’ liabilities for not reporting cases of perinatal substance abuse, either intentionally or unintentionally? Does prenatal exposure to legal substances such as alcohol and tobacco qualify under various statutes, and would the law differ for teen pregnancies? These are difficult questions that require both physician knowledge and possibly legal expertise. Clinicians unfamiliar with legalities regarding this issue should consult with the risk management or legal departments of their institutions. If practitioners lack access to such services, many legal codes are available online. Physicians can contact professional societies for advice on this issue or contact private legal counsel if necessary.
Decisions must also be made regarding patient care and reporting to Departments of Human Services or Child Protective Services when substance abuse is involved. Reporting to Child Protective Services can be damaging to a therapeutic relationship and become a further barrier to treatment (15, 16). Involvement is not always negative, and it has the potential to be used in guiding behavior and expanding treatment options, which may elicit more favorable outcomes. Decisions regarding drug testing, reporting of substance abuse in pregnancy, and subsequent state action may be applied disproportionately to low-income, southern, African American women compared with others (17). This underscores the potential for bias and the need for standard care in addressing substance abuse in the perinatal period.
Additionally, we recommend continued involvement of mental health professionals and medical societies in health policy research and education of lawmakers. Research involving the impact of public policy on health outcomes, a burgeoning area of investigation, is becoming an important and necessary field (18). The criminalization of substance abuse during pregnancy and its impact on maternal and neonatal outcomes has yet to be fully elucidated. Investigation is warranted, followed by education of leaders so that well-informed public health law can be instituted.
Supplementary Material
Acknowledgments
Dr. House has received research support from Janssen Pharmaceutica. Dr. Stowe has received research support from Janssen Pharmaceutica and Sage Therapeutics. Dr. Coker has received research support from University of Arkansas for Medical Sciences NIDA T32 grant UL1TR000039.
REFERENCES
- 1.Chaudron LH: Complex challenges in treating depression during pregnancy. Am J Psychiatry 2013; 170:12–20 [DOI] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration: Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2014 [Google Scholar]
- 3.Behnke M, Smith VC, Committee on Substance Abuse, et al. : Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics 2013; 131:e1009–e1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ankrom v Alabama (Ala; 2013) [Google Scholar]
- 5.Kimbrough v Alabama (Ala; 2013) [Google Scholar]
- 6.Mississippi v. Buckhalter (Miss; 2013) [Google Scholar]
- 7.NJ Div of Youth & Family Servs v AL (NJ; 2013) [Google Scholar]
- 8.108th Tennessee General Assembly: SB1391 (2014)
- 9.Guttmacher Institute: State policies in brief: substance abuse during pregnancy. March 1, 2016. http://www.guttmacher.org/statecenter/spibs/spib_SADP.pdf
- 10.Whitner v South Carolina (SC; 1997) [Google Scholar]
- 11.American Psychiatric Association: Policy statement on care of pregnant and newly delivered women addicts. 2007. http://www.psychiatry.org/File%20Library/Learn/Archives/Position-2007-Pregnant-Addiction.pdf
- 12.American Academy of Addiction Psychiatry: Use of illegal and harmful substances by pregnant women. 2015. http://www.aaap.org/wp-content/uploads/2015/06/AAAP-FINAL-Policy-Statement-Edits-Use-of-Illegal-Substances-by-Pregnant-Women-for-merge.pdf
- 13.American Medical Association: Perinatal Addiction: Issues in Care and Prevention H-420.962. 2016. https://searchpf.ama-assn.org/SearchML/searchDetails.action?uri5%2FAMADoc%2FHOD.xml-0-3705.xml
- 14.American College of Obstetricians and Gynecologists: Substance abuse reporting and pregnancy: the role of the obstetrician-gynecologist. 2011. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Health-Care-for-Underserved-Women/Substance-Abuse-Reporting-and-Pregnancy-The-Role-of-the-Obstetrician-Gynecologist [DOI] [PubMed]
- 15.Watson H, Levine M: Psychotherapy and mandated reporting of child abuse. Am J Orthopsychiatry 1989; 59:246–256 [DOI] [PubMed] [Google Scholar]
- 16.Poland ML, Dombrowski MP, Ager JW, et al. : Punishing pregnant drug users: enhancing the flight from care. Drug Alcohol Depend 1993; 31:199–203 [DOI] [PubMed] [Google Scholar]
- 17.Paltrow LM, Flavin J: Arrests of and forced interventions on pregnant women in the United States, 1973–2005: implications for women’s legal status and public health. J Health Polit Policy Law 2013; 38:299–343 [DOI] [PubMed] [Google Scholar]
- 18.Burris S, Wagenaar AC, Swanson J, et al. : Making the case for laws that improve health: a framework for public health law research. Milbank Q 2010; 88:169–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


