Abstract
The aim of this report was to determine the impact of flaxseed, soy and red clover, and their bioactive substances on the lipid profile in postmenopausal women in cardiovascular diseases prevention. We used the following databases: MEDLINE (PubMed), EMBASE and the Cochrane Library. Meta-analysis indicates that the intake of flaxseed by postmenopausal women is associated with a statistically significant reduction in total cholesterol (TC) levels (weighted-mean difference (WMD) = −0.26; 95% confidence interval (95% CI): −0.38 to −0.13; p = 0.0001), low-density lipoprotein cholesterol (LDL-C) levels (WMD = −0.19; 95% CI: −0.30 to −0.08; p = 0.0006), and high-density lipoprotein cholesterol (HDL-C) levels (WMD = −0.06; 95% CI: −0.11 to −0.01; p = 0.0150). The effect of soy protein on the lipid profile showed a significant decrease in TC levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0048, LDL-C levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0067, as well as a significant increase in HDL-C levels: WMD = 0.05; 95% CI: 0.02–0.08; p = 0.0034. Changes in the lipid profile showed a significant reduction in TC levels after the use of red clover (WMD = −0.11; 95% CI: −0.18–−0.04; p = 0.0017) and a significant increase in HDL-C levels (WMD = 0.04; 95% CI: 0.01 to 0.07; p = 0.0165). This meta-analysis provides evidence that consuming flaxseed, soy and red clover can have a beneficial effect on lipids in postmenopausal women and suggest a favorable effect in preventing cardiovascular diseases.
Keywords: flaxseed, soy, red clover, lipid profile, meta-analysis, cardiovascular disease, botanical supplements, postmenopausal woman
1. Introduction
Cardiovascular disease (CVD) is collection of disorders affecting the vasculature of the heart, brain and peripheral tissues, and remains the leading cause of death globally [1,2]. The most common cause of CV is atherosclerosis, which is initiated by an inflammatory reaction of the vascular endothelium [3]. The origins of these endothelial lesions are still not fully explained, but involved factors include: chronic elevations in blood pressure [4]; prolonged hyperglycemia and the resulting formation of advanced glycation end-products [5]; elevated lipoproteins, particularly molecules that have undergone oxidized modification [6]; and oxidative stress and inflammation [7]. With aging, a number of changes occur in the metabolism, known as the ‘metabolic syndrome’ [8]. Among others, these include the accumulation of fat mass in the abdominal compartment, transition to a more atherogenic lipid profile, hyperinsulinemia, insulin resistance and glucose intolerance [9,10]. The consequence of these changes is an enhanced risk of coronary heart disease, stroke and other atherosclerotic vascular diseases, including peripheral arterial disease, atherosclerotic aortic disease and carotid artery disease [11].
A bioactive effect on lipid metabolism involving lowering the level of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and triglycerides (TG), has been demonstrated during studies of some plant dietary items, such as: almonds [12], artichokes [13], barberry [14], curcumin [15], ginger [16], psyllium [17], sesame [18], cacao [19] and walnuts [20].
Women are at a higher risk of developing CVDs after menopause due to estrogen deficiency and dysregulated lipid metabolism [21]. Loss of ovarian endocrine function as a result of chronic hypoestrogenism is the main physiological symptom associated with menopause. The daily production of estrogen in postmenopausal women is 0.045 mg, compared with 0.35 mg during the reproductive period, which is reflected in serum estrogen concentrations of 10–20 µg/mL and 40–400 µg/mL, respectively [22]. Observed menopause-induced estrogen deficiency leads to various metabolic disorders including lipid metabolism. TC, LDL-C, and TG levels increase during the menopause and during the postmenopausal period. In turn, high-density lipoprotein cholesterol (HDL-C) levels, after an initial rise during the menopausal transition, gradually decline during late menopause [23,24,25] (of note, there were also studies showing no difference in HDL-C levels between premenopausal and postmenopausal women [26]). Dyslipidemia is one of the most important risk factors for CVD, which can be corrected and prevented. Botanical supplements as flaxseed, soybean and red clover are rich sources of bioactive compounds affecting lipid metabolism [27].
The benefits of consuming whole fractions of flaxseed (Linum usitatissimum L.) such as its protein, oil and mucilage, are related to the presence of specific bioactive substances. The flaxseed content of protein ranges from 10 to 31%, including higher amounts of arginine, aspartic and glutamic acids than other amino acids. Flaxseed also consists of 40% fat; and 25–28% fiber, of which 25% is in soluble form. Moreover, approximately 38–45% of flaxseed mass contains oil and 55–68% is meal. Flaxseed is a rich source of bioactive ingredients such as α-linolenic acid (ALA) and linoleic acid. Additionally, it contains phytochemicals such as lignan complex: secoisolariciresinol diglucoside (SDG), cinnamic acid glucoside and hydroxymethyl glutaric acid [28,29]. Flaxseed oil and active compounds, especially SDG and its metabolites, suppresses the inflammatory tissue damage caused by oxidative stress [30]. SDG may also directly lower serum cholesterol by modulating the enzymes 7α-hydroxylase and acyl-coenzyme A:cholesterol acyltransferases, both of which are involved in cholesterol metabolism [31]. The supplied ALA reduces the production of arachidonic acid (AA) and consequently, by decreasing proinflammatory eicosanoid, leads to a reduction in the inflammation process [32].
The soybean (Glycine max L.) is a significant source of protein (~36–40%), lipids (~20%) and dietary fiber (~9%) (based on the dry weight of mature raw seeds), and phytochemicals such as isoflavones, phytosterols and lecithins, which may act collectively or through independent mechanisms. The two major protein peptides, β-conglycinin (βCG) and glycinin, comprise 80–90% of the total protein in soybean, and affect lipid metabolism [33,34]. Additionally, soybeans are rich sources of essential fatty acids. Polyunsaturated (primarily linoleic acid, alpha-linolenic acid), monounsaturated (oleic acid) and saturated (primarily palmitic acid) fatty acids comprise approximately 63%, 23%, and 14%, respectively, of the total fat content of soybeans, and have an impact on the level of lipids [35]. The other major bioactive compounds in soybeans are isoflavones, which are associated with soy proteins. Isoflavones occur in large values in soybean as glycoside, such as genistin, daidzin and glycitin, or their aglycone forms, genistein, diadzein and glycitein [36]. Soy isoflavones, with structural similarities to the endogenous 17β-estradiol, reveal their biological effects via activating estrogen receptors (ER) with a higher affinity to ER-β, in comparison to ER-α. Although the affinity for the estrogen receptor by soy isoflavones is 100–1000 times less than that of natural estrogen, more than a thousand-fold greater isoflavone concentrations can appear in the plasma than those of endogenous estrogen [37]. Isoflavones, by binding to ERs, lead to gene activation and beneficial effects on lipid metabolism [38].
A number of other mechanisms regulating lipid metabolism without the mediation of the estrogen receptor have been recorded—including the increased expression of 3-hydroxy−3-methylglutaryl-CoA reductase (HMGCR), which leads to decreased cholesterol and TG levels; the enhanced expression of peroxisome proliferator-activated receptor (PPAR) and the activation of AMP-activated protein kinase (AMPK), which results in increased expression of genes involved in lipoprotein metabolism; the decreased expression of sterol regulatory-element binding protein-lc (SREBP-1) and increased expression of SREBP-2, which suppresses cholesterol synthesis and absorption in the liver; the inhibition of the expression and activity of the sterol regulatory element binding protein-1c (SREBP-1c) and carbohydrate response element binding protein-1 (ChREBP), which are proteins that enhance the expression of lipogenic genes and key enzymes involved in de novo lipogenesis; the promotion of the HDL-C metabolism and of the uptake, utilization and catabolism of fatty acids; and the modulation of the effects on several enzymes important in lipid transformation, such as lipoprotein lipase (LPL), hepatic lipase (HL) (also called hepatic triglyceride lipase (HTGL)), and 7alpha-hydroxylase [39,40,41,42,43,44].
Red clover (Trifolium pratense L.) contains a certain amount of protein and fat that is irrelevant from the point of view of human nutrition. It is also rich in bioactive substancesused in medicine. Red clover isoflavones show a different mechanism of action on lipid metabolism than that of soy isoflavones, which is due to the different composition of the contained isoflavones. Grains of red clover contain higher concentrations of formononetin and biochanin A and lower concentrations of daidzein and genistein than soy [45]. This composition suggests that an equal production status may be less relevant [46]. Isoflavones with structural similarities to endogenous 17-β-estradiol reveal their biological effects via activating estrogen receptors (ER) with a higher affinity to ER-β, in comparison to ER-α, which mediates the cholesterol metabolism [47,48]. In addition, a number of non-hormonal effects have been reported in its isoflavones, including tyrosine kinase inhibition, antioxidant activity, and effects on ion transport [49]. Red clover extract and the isoflavones genistein and biochanin A can also regulate lipid metabolism without the mediation of estrogen receptors, as well as increase the expression of PPAR alpha and activate AMPK, which results in the enhanced activity of genes involved in lipoprotein metabolism [50].
The purpose of this study was to determine the impact of flaxseed, soy and red clover and their bioactive substanceson the lipid profile in postmenopausal women in cardiovascular prevention.
2. Materials and Methods
2.1. Search Strategy and Study Selection
This systematic review and meta-analysis was designed in accordance with The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement [51] to identify randomized controlled trials (RCTs) assessing the effects of flaxseed, soy protein, soy isoflavones and red clover isoflavones on the level of serum lipids.
The electronic databases MEDLINE (PubMed), Embase, and the Cochrane Library were searched for the identification of randomized controlled trials until December 2018. The following search terms were used for all databases in various combinations: (“flax” OR “flaxseed” OR “linseed” OR “Linum usitatissimum” OR “soybean” OR “Glycine max” OR “soy proteins” OR “soy isoflavones” OR “red clover” OR “Trifolium pratense”) AND (“lipid profile” OR “lipids” OR “total cholesterol” OR “HDL cholesterol” OR “LDL cholesterol” OR “triglycerides”) AND (“menopause” OR “postmenopause”).
The search was limited to papers published in English and was conducted up to December 2018. References to selected research and review articles related to the topic of the work were also searched in order to identify additional studies.
The initial selection included the analysis of the titles and/or abstracts of all citations. After an independent and double analysis of the full texts of selected works, a decision was then made to include or exclude them. In turn, works were qualified for meta-analysis and collection of data on the clinical and methodological characteristics of the described clinical trials and for statistical evaluation.
Randomized controlled trials (RCTs) were considered eligible for inclusion if they met all of the following criteria: parallel-group design, or crossover design that contained data for the first period; a comparison with a placebo or with a no-intervention group; a follow-up period was at least 3 months; post-menopausal women as participants; appropriate interventions using flaxseed, soy or red clover and the presentation of sufficient information on plasma-lipid levels at baseline and after supplementation, or the net change values in both study arms. The exclusion criteria were as follows: men or premenopausal women as participants, no control group in the study, lack of sufficient information, and a study duration of less than 12 weeks. The results were reported as graphics or percent changes, and as duplicated reports.
2.2. Data Extraction
The data were extracted by the lead author and subsequently reviewed by co-authors for accuracy. Eligible studies were reviewed and the following data were abstracted: first author’s name; year of publication; study location (country); follow-up period of the study; study design; number of participants in the intervention and control group; health characteristics of the population (age, menopausal status, body mass index); daily amount of flaxseed, soy protein, soy isoflavones and red clover isoflavones taken in the active arm; and data on baseline and follow-up TC, LDL-C, HDL-C and TG plasma levels.
2.3. Quality Assessment and Bias Risk of the Trials
The Jadad Scale is an Oxford system for assessing the quality of a clinical trial, designed to determine the minimum level of studies included in a systematic review/meta-analysis. The test may receive values from 0 (low quality) to 5 points (highest quality) [52]. This meta-analysis included studies that had a relatively high Jadad score. To explain the possible presence of bias publications, Begg’s rank correlation test (Kendall Tau) and Egger’s weighted regression test were applied [53,54].
2.4. Statistical Analysis and Meta-Analysis
The meta-analysis included all intervention groups from multi-arm studies. Moreover, to avoid the duplication of data from the same people in surveys covering multiple time points, only one such point was taken into account.
The data in each study were presented as numbers of subjects (N) and the mean ± standard deviations (SD). When the standard error of the mean (SEM) was employed, the conversion to SD was made according to the formula: SD = SEM × √N. If a 95% confidence interval (95% CI) was applied, SD conversion was: SD = sqrt (N) × (upper bound–lower bound)/(2u) (equal to 3.96). When the results from the studies were presented in mg/dL, they were converted into mmol/L using standard conversion factors (the value in mg/dL was multiplied by 0.02586 for TC, LDL-C and HDL-C, and by 0.01143 for TG).
The outcome measures were the differences in the mean (MD) of components of the lipid profile between baseline and the end values for both the intervention and control groups. The missing SDs of MD were imputed using the formula: SD = sqrt ((SD “initial”)2 + (SD “final”)2 − (SD “initial” × SD “final”) × 2R), where R is the correlation coefficient; we took an R value = 0.40 [55,56]. The outcome measures were the differences in the mean (net change in mmol/L) of elements of the lipid profile between the baseline and the end values for both the intervention and control groups.
Summary outcomes measures were presented as the mean differences between the intervention and control groups. A random-effects model was used to calculate the weighted-mean difference (WMD) and 95% confidence interval (CI) for each comparison, and the combined overall effect (p < 0.05 was considered statistically significant) according to DerSimonian and Laird [57]. Cochrane Q and I2 statistics were used to assess the heterogeneity. The I2 test determined whether the variance across studies was correct and not a result of a sampling error. The percentage of total variation indicated the degree of heterogeneity; I2 values of ≤25% were considered low; >25% as moderate; and ≥75% as high heterogeneity [58]. STATISTICA Medical Software v. 11.0 StatSoft, Krakow, Poland was used for all statistical analyses.
3. Results
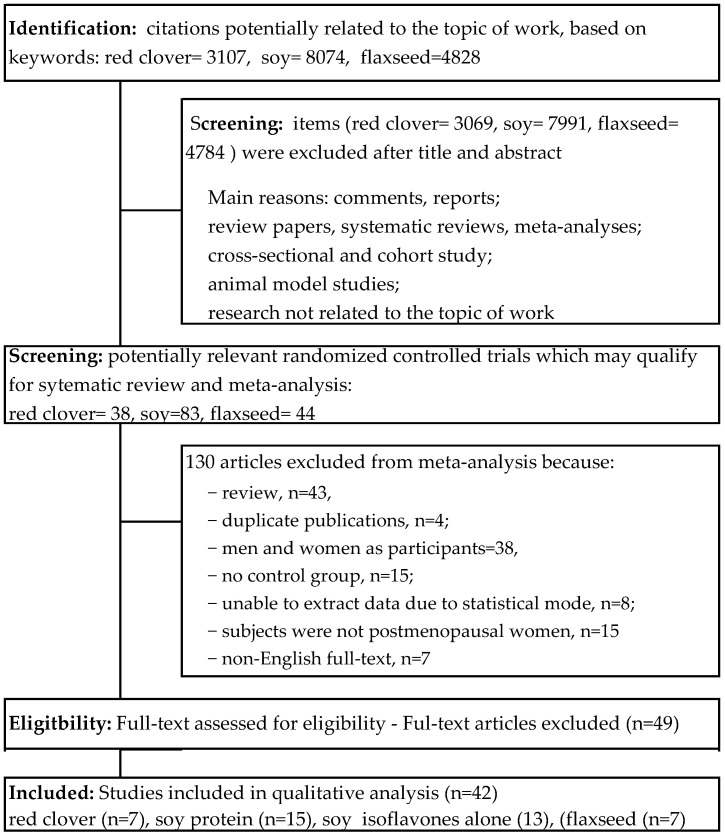
In total, a number of citations potentially related to the topic of work based on the key words—red clover = 3107; soy = 8074; and flaxseed = 4828—were identified. Building upon the title and/or abstract, exclusions were 3069 for red clover; 7991 for soy; and 4784 for flaxseed due to a lack of connection with the topic of this work. Consequently, 165 potentially relevant clinical trials qualified for further detailed qualitative analysis in the full-text assessment: red clover = 38; soy = 83; and flaxseed = 44. Among these, 130 studies were also discarded due to the failure to meet all inclusion criteria. As a result, 42 randomized controlled trials for meta-analysis. Detailed information about the literature search and study selection and identification can be found in Figure 1.
Figure 1.
Flowchart of the selection procedure for studies included in the current review and meta-analysis.
3.1. Characteristics of Included Trials
The characteristics of selected randomized controlled studies assessing the influence of flaxseed, soy protein, soy isoflavones, and red clover on lipid profile in postmenopausal women are presented in Table 1. The meta-analysis included 42 studies published in English from 1998 to 2018 [59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100].
Table 1.
Characteristics of selected randomized controlled studies assessing the influence of flaxseed, soy protein, soy isoflavones, and red clover on lipid profile in postmenopausal women.
| First Author [Ref.] Data Location |
Study Design Trial Duration |
Study Population Age (Mean ± SD) y, ysm, BMI, Health Condition |
Intervention (Daily Dose) |
GroUp Studied |
Number Sample | Baseline Lipids Values | Jadad Score | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Total-C mmol/L |
LDL-C mmol/L |
HDL-C mmol/L |
TAG mmol/L |
|||||||
| A. Flaxseed (Linum usitatissimum L.) | ||||||||||
| Arjmandi [59] 1998 United States |
Cross-over 6-week active phase 2-week washout. |
Age 56.3 ± 6.5, ysm N/A, BMI 29.2 ± 7.4, obesity, hypercholesterolemia |
WFX 38 g, ALA 8.5 g vs. placebo: sunflower seed (slice of bread or muffin) |
FG CG |
15 19 |
5.95 ± 1.44 5.92 ± 1.36 |
4.12 ± 1.39 4.06 ± 1.34 |
0.93 ± 0.23 1.08 ± 0.23 |
1.28 ± 0.92 1.27 ± 0.70 |
4 |
| Lucas [64] 2002 United States |
Parallel group 3-month follow-up |
Age 54 ± 8, ysm N/A, BMI 29.1 ± 7.1 obesity |
WFX 40 g vs. placebo, wheat-based 40 g |
FG CG |
20 16 |
5.76 ± 1.12 5.95 ± 1.12 |
3.21 ± 1.12 3.52 ± 1.12 |
1.89 ± 0.42 1.61 ± 0.40 |
1.48 ± 0.71 1.56 ± 0.76 |
4 |
| Dodin [62] 2005 Canada |
Parallel group 1-year follow-up |
Age 54.0 ± 4.0, ysm 4.7 ± 5.2, BMI 25.5 ± 4.5 healthy |
WFX 40 g, ALA 9.1 g vs. control, wheat germ (slice of bread or drinks) |
FG CG |
85 94 |
5.67 ± 0.75 5.78 ± 0.71 |
3.43 ± 0.69 3.50 ± 0.64 |
1.72 ± 0.33 1.74 ± 0.39 |
1.12 ± 0.45 1.16 ± 0.57 |
5 |
| Hallund [63] 2006 Denmark |
Cross-over 6-week active phase 6-week washout |
Age 61 ± 7, ysm >24 mo, BMI 25.5 ± 4.5 healthy |
Lignan complex, SDG 500 mg vs. control (in form muffins, 50 g) |
FG CG |
22 22 |
6.05 ± 1.03 6.03 ± 0.98 |
3.80 ± 1.03 3.79 ± 0.98 |
1.81 ± 0.42 1.82 ± 0.52 |
0.96 ± 0.28 0.93 ± 0.33 |
4 |
| Cornish [61] 2009 Canada |
Parallel group 6-month follow-up |
Age 59.7 ± 5.3, ysm N/A, BMI 27.1 ± 5.3 healthy |
Lignan complex, SGD 500 mg vs. placebo |
FG CG |
27 25 |
5.87 ± 0.88 6.14 ± 1.05 |
3.60 ± 0.88 3.77 ± 0.80 |
1.74 ± 0.42 1.54 ± 0.40 |
1.19 ± 0.68 1.77 ± 1.10 |
4 |
| Simbalista [65] 2010 Brazil |
Parallel group 3-month follow-up |
Age 52.0 ± 2.9, ysm 3.8 ± 2.3, BMI 26 ± 3.6, healthy |
GFX: WFX 25 g, SDG 46 mg, vs placebo: wheat bran (in form of slice bread) |
FG CG |
20 18 |
6.03 ± 0.87 5.18 ± 0.93 |
3.83 ± 0.89 2.87 ± 0.93 |
1.61 ± 0.31 1.86 ± 0.42 |
1.49 ± 0.80 1.00 ± 0.54 |
5 |
| Brache [60] 2015 Denmark |
Parallel group 6-week follow-up |
Age 60.6 ± 6.4 y, ysm ≥1 y, BMI 35.2 ± 4.5, obesity |
10 g flaxseed mucilage vs. placebo: maltodextrin (in form buns) |
FG CG |
19 16 |
6.39 ± 0.89 5.76 ± 0.69 |
4.11 ± 0.84 3.44 ± 0.74 |
1.40 ± 0.22 1.56 ± 0.42 |
1.51 ± 0.77 1.07 ± 0.32 |
3 |
| B. Soybean (Glycine max (L.) Merr.) | ||||||||||
| B. 1. Soy protein without and with isoflavones | ||||||||||
| Baum [68] 1998 United States |
Parallel groups 2-week run-in/ 12-week follow-up |
Age 60.8 ± 8.6 y, ysm N/A, BMI 27.8 ± 5.3, hypercholesterolemia |
a. SP 40 g: a. IAE 90 mg; b. SP 40 g; IAE 56 mg vs. control, CP + MP 40 g |
SG 90 SG 56 CG |
21 23 22 |
6.47 ± 0.88 6.57 ± 0.85 6.26 ± 0.67 |
N/A N/A 4.9 ± 0.8 |
1.38 ± 0.32 1.34 ± 0.28 1.38 ± 0.31 |
1.74 ± 0.75 1.89 ± 1.02 1.75 ± 1.11 |
3 |
| Vigna [80] 2000 Italy |
Parallel groups 12-week follow-up |
Age 53.4 ± 3.3, ysm 2.4 y, BMI 25.9 ± 3.5, healthy |
SP 40 g, IF 76 mg vs. control, CP 40 g |
SG CG |
40 37 |
6.37 ± 1.01 6.55 ± 0.93 |
4.13 ± 0.87 4.33 ± 0.87 |
1.57 ± 0.36 1.61 ± 0.38 |
1.47 ± 0.90 1.32 ± 0.77 |
4 |
| Gardner [72] 2001 United States |
Parallel groups 4-week run-in/ 12-week follow-up |
Age 59.9 ± 6.6, ysm N/A, BMI 26.3 ± 4.6, hypercholesterolemia |
a. SP 42 g b. SP 42 g (52 mg Gen, 25 mg Dai, 4 mg Gly) vs. control, MP 42 g. |
SG SG CG |
33 31 30 |
5.9 ± 0.7 5.9 ± 0.6 6.1 ± 0.6 |
3.9 ± 0.6 3.9 ± 0.6 4.0 ± 0.5 |
1.4 ± 0.3 1.5 ± 0.3 1.5 ± 0.4 |
1.3 ± 0.5 1.3 ± 0.8 1.3 ± 0.7 |
4 |
| Han [73] 2002 Brazil |
Parallel groups 4-month follow-up |
Age 48.5 ± 7.6, ysm 1.9 ± 1.6 y, BMI 24.3 ± 3.2, healthy |
SP 50.3 mg, IAE 23.3 mg Gen, 3.8 mg Gly, 6.2 mg Dai) vs. placebo |
SG CG |
40 40 |
5.83 ± 0.88 5.86 ± 1.26 |
3.45 ± 0.87 3.45 ± 1.32 |
1.04 ± 0.23 1.03 ± 0.21 |
2.31 ± 1.66 1.99 ± 1.66 |
5 |
| Dalais [71] 2003 Australia |
Parallel groups 3-month follow-up |
Age 60 ± 6.2, ysm N/A, BMI 25.3 ± 4.6, healthy |
SP 40 g, IC 118 mg (69 mg Agl) vs. control, CP 40 g |
SG CG |
38 40 |
6.12 ± 0.92 5.92 ± 0.88 |
4.00 ± 0.86 3.69 ± 0.88 |
1.63 ± 0.49 1.72 ± 0.51 |
1.09 ± 0.68 1.01 ± 0.57 |
5 |
| Steinberg [78] 2003 United States |
Cross-over 6-week active phase 4-week washout |
Age 5.49 ± 5.29, ysm N/A, BMI 24.6 ± 3.2, healthy |
a. SP 25 g b. SP 25 g, IAE 107 mg (55 mg Gen, 47 mg Dai, 5 mg Gly) vs. control, MP 25 g |
SG a SG b CG |
24 24 24 |
4.91 ± 0.49 4.91 ± 0.49 4.91 ± 0.49 |
2.89 ± 0.49 2.89 ± 0.49 2.89 ± 0.49 |
1.55 ± 0.49 1.55 ± 0.49 1.55 ± 0.49 |
1.03 ± 0.49 1.03 ± 0.49 1.03 ± 0.49 |
4 |
| Cuevas [70] 2003 Chile |
Cross-over 8-week active phase 4-week washout |
Age 59 y, ysm 10 y, BMI 29.3 ± 3.43, obesity, hypercholesterolemia |
SP 40 g, IAE 80 mg (60% Gen, 30% Dai, 10% Gly) vs. control, caseinate 40 g |
SG CG |
18 18 |
7.90 ± 0.74 7.90 ± 0.74 |
5.04 ± 0.66 5.04 ± 0.66 |
1.39 ± 0.27 1.39 ± 0.27 |
2.18 ± 0.83 2.18 ± 0.83 |
4 |
| Kreijkamp- Kaspers [75] 2004 Netherlands |
Parallel groups 12-month follow-up |
Age 66.6 ± 4.7, ysm 17.9 ± 6.9 y, BMI 26.1 ± 3.8, healthy |
SP 25.6 g, IAE 99 mg (52 mg Gen, 6 mg Gly, 41 mg Dai) vs. control, MP 25,6 mg |
SG CG |
88 87 |
6.21 ± 0.73 6.11 ± 0.95 |
4.16 ± 0.99 4.12 ± 0.88 |
1.55 ± 0.41 1.53 ± 0.34 |
1.36 ± 0.72 1.25 ± 0.59 |
4 |
| Teede [79] 2005 Australia |
Parallel groups 3-day run-in/ 3-month follow-up |
Age 59.5 ± 4.5, ysm N/A, BMI 25.9 ± 5.4, healthy |
SP 40 g, IC 118 mg (54 mg Gen, 3.6 mg Gly, 26 mg Dai) vs. control, CP 40 g |
SG CG |
19 21 |
6.2 ± 1.30 5.8 ± 0.92 |
4.0 ± 0.87 3.6 ± 0,92 |
1.6 ± 0.43 1.6 ± 0.46 |
1.0 ± 0.48 1.0 ± 0.63 |
3 |
| Allen [66] 2007 United States |
Parallel groups 4-week run-in/ 12-week follow-up |
Age 56.8 ± 5.6, ysm 9.4 ± 8.3 y, BMI 27.9 ± 4.7, hypercholesterolemia |
SP 20 g, IC 160 mg (~96 mg Agl) vs. control, MP 20 g |
SG CG |
93 98 |
5.80 ± 0.68 5.71 ± 0.64 |
3.67 ± 0.68 3.60 ± 0.57 |
1.56 ± 0,37 1.52 ± 0.31 |
1.25 ± 0.51 1.28 ± 0.60 |
5 |
| Maesta [77] 2007 Brazil |
Parallel group 16-week follow-up |
Age 61.3 ± 5,2, ysm 10.7 ± 4.9 y, BMI 27.2 ± 5.3 healthy |
SP 25 g, IAE 50 mg (32 mg Gen, 15 mg Dai, 3 mg Gly) vs. placebo, maltodextrine |
SG CG |
10 11 |
5.95 ± 0.71 5,76 ± 0.98 |
3.71 ± 0.72 3.56 ± 0.70 |
1.62 ± 0.34 1.32 ± 0.25 |
1.36 ± 0.52 1.95 ± 0.71 |
5 |
| Basaria [67] 2009 United States |
Parallel groups 12-week follow-up |
Age 55.7 ± 1.3, ysm 5.7 ± 0.9, BMI 26.1 ± 0.8, healthy |
SP 20 g, IC 160 mg (IAE: 64 mg Gen, 63 mg Dai, 34 mg Gly) vs. control, MP 20 g |
SG CG |
38 46 |
5.48 ± 0.14 5.69 ± 0.85 |
3.15 ± 0.75 3.21 ± 0.74 |
1.88 ± 0.46 2.02 0.46 |
1.03 ± 0.58 0.99 ± 0.46 |
4 |
| Campbell [69] 2010 United States |
Parallel groups 12-month follow-up |
Age 54.7 ± 5.5, ysm 5.5 ± 5.0, BMI 27.9 ± 5.9, hypercholesterolemia |
SP 25 g, 60 mg IF vs. control, CP 25 g |
SG CG |
35 27 |
5.97 ± 0,93 6.15 ± 0.91 |
3.88 ± 0.90 3.95 ± 0.87 |
1.47 ± 0.38 1.50 ± 0.36 |
1.34 ± 0.70 1.48 ± 0.67 |
4 |
| Jassi [74] 2010 India |
Parallel groups 12-week follow-up |
Age 51.1 ± 8.6, ysm 2.3 ± 1.2, BMI 23.4 ± 2.7, healthy |
SP 30 g, IF 60 mg vs. control, CP 30 g |
SG CG |
25 25 |
4.96 ± 0.36 4.69 ± 0.71 |
3.09 ± 0.37 2.83 ± 0.76 |
1.06 ± 0.15 1.06 ± 0.16 |
1.76 ± 0.28 1.76 ± 0.17 |
4 |
| Liu [76] 2012 Hong Kong SAR |
Parallel groups 2-week run-in/ 3-month follow-up |
Age 56.3 ± 4.3, ysm 5.9 ± 5.4, BMI 24.4 ± 3.6, prediabetes |
SP 15 g, IAE 100 mg (59 mg Gen,4 mg Gly, 35 mg Dai) vs. control, MP 15 g |
SG CG |
60 60 |
5.83 ± 0.94 5.63 ± 0.93 |
3.94 ± 0.67 3.81 ± 0.88 |
1.66 ± 0.31 1.65 ± 0.30 |
1.35 ± 1.19 1.30 ± 0.70 |
5 |
| B.2. Soy isoflavones preparations | ||||||||||
| Dewell [85] 2002 USA |
Parallel groups 2-month follow-up |
Age 69.5 ± 4.2 y, ysm N/A, BMI 25.0 ± 4,2, moderate hypercholesterolemia |
IC 150 mg (90 mg Agl: 45 mg Gen, 55% Dai and Gly) vs. placebo |
SG CG |
20 16 |
6.8 ± 0.9 6.3 ± 2.0 |
N/A N/A |
1.2 ± 0.5 1.2 ± 0.4 |
0.8 ± 0.5 1.3 ± 0.8 |
4 |
| Colacurci [93] 2005 Italy |
Parallel groups 6-month follow-up |
Age 55.1 ± 38 y, ysm 4.9 ± 0.6, BMI 25.9 ± 1.8, healthy |
IAE 60 mg (30 mg Gen, 30 mg Dai) vs. placebo |
SG CG |
29 28 |
NR NR |
3.7 ± 0.3 3.6 ± 0.4 |
1.06 ± 0.5 1.05 ± 0.5 |
1.5 ± 0.6 1.6 ± 0.8 |
4 |
| Garrido [87] 2006 Chile |
Parallel groups 12-week follow-up |
Age 55.5 ± 4.0 y, ysm N/A, BMI 26.9 ± 2.3, healthy |
IAE ~100 mg (46.8 mg Gen, 48.2 mg Dai) vs. placebo |
SG CG |
15 14 |
5.5 ± 1.0 4.8 ± 0.5 |
3.4 ± 0.4 2.9 ± 03 |
1.4 ± 0.3 1.8 ± 0.6 |
1.3 ± 0.2 1.4 ± 0.2 |
3 |
| Wu [92] 2006 Japan |
Parallel group 6-month follow-up |
Age 54.4 ± 2.9 y, ysm N/A, BMI 21.1 ± 2.4, healthy |
IC 75 mg (47 mg Agl: 38.3 mg Dai, 8.6 mg, 1 mg Gly) vs. placebo |
SG CG |
25 29 |
5.90 ± 0.76 5.88 ± 0.86 |
3.52 ± 0.72 3.59 ± 0.76 |
1.92 ± 0.47 1.85 ± 0.38 |
0.95 ± 0.43 1.16 ± 0.53 |
3 |
| Nahas [90] 2007 Brazil |
Parallel groups 4-week run-in 4-month follow-up |
Age 55.7 ± 6.8, ysm 6.9 ± 4.5, BMI 29.1 ± 5.0, obesity |
IC 100 mg (50% Gen, 35% Dai), vs. placebo |
SG CG |
38 36 |
5.56 ± 0.92 5.37 ± 0.97 |
3.47 ± 0.82 3.26 ± 0.82 |
1.29 ± 0.27 1.35 ± 0.34 |
1.73 ± 0.74 1.67 ± 0.89 |
3 |
| Ho [88] 2007 China |
Parallel groups 6-month follow up |
Age 54.2 ± 3.1, ysm 4,1 ± 2.4, BMI 24.1 ± 3.6, healthy |
a. IAE 80 mg, b. IAE 40 mg (46.4% Dai, 38.8 Gly, 14.7% Gen) vs. placebo |
SG 80 SG 40 CG |
67 68 68 |
5.86 ± 0.83 5.83 ± 0.84 5.93 ± 0.89 |
3.19 ± 0.74 3.23 ± 0.68 3.25 ± 0.73 |
1.89 ± 0.41 1.80 ± 0.39 1.86 ± 0.42 |
1.13 ± 0.56 1.32 ± 0.93 1.29 ± 0.96 |
4 |
| Aubertin-Leheudre [81] 2008 Canada |
Parallel groups 6-month follow-up |
Age 57.4 ± 5.4 y, ysm 8.6 ± 7.5, BMI 32.0 ± 12.5, obesity |
IAE 70 mg (44 mg Dai, 16 mg Gly, 10 mg Gen) vs. placebo |
SG CG |
21 18 |
5.41 ± 0.88 5.33 ± 0.83 |
3.17 ± 0.81 3.17 ± 0.78 |
1.55 ± 0.49 1.45 ± 0.37 |
1.51 ± 0.69 1.52 ± 0.69 |
4 |
| Özturk Turhan [91] 2009 Turkey |
Parallel groups 6-month follow-up |
Age 51.5 ± 5.1; ysm 3.6 ± 1.7, BMI 27.1 ± 3.1 |
IAE 40 mg (29.8 mg Gen, 7.8 mg Dai, 2.4 mg Gly) vs. placebo |
SG CG |
45 45 |
6.82 ± 0.96 6.30 ± 0.76 |
4.25 ± 0.73 4.01 ± 0.65 |
1.06 ± 0.15 1.06 ± 0.16 |
1.76 ± 0.28 1.76 ± 0.17 |
4 |
| Choquette [84] 2011 Canada |
Parallel groups 6-month follow-up |
Age 58.5 ± 5.5 y, ysm 9.0 ± 7.0, BMI 30.1 ± 2.7, obesity |
IAE 70 mg (44 mg Dai, 16 mg Gly, 10 mg Gen) vs. placebo |
SG CG |
23 22 |
5.40 ± 0.80 5.58 ± 0.86 |
3.34 ± 0.75 3.34 ± 0.81 |
1.49 ± 0.34 1.37 ± 0.32 |
1.47 ± 0.67 1.44 ± 0.73 |
5 |
| Kim [89] 2013 Republic of Korea |
Parallel groups 12-week follow-up |
Age 53.6 ± 3.4 y, ysm 3.6 ± 2,4, BMI 23.3 ± 2.5, healthy |
IC 70 mg (Glyc: 38 mg glycitin 20 mg daidzin, 12 mg genistin) vs. placebo |
SG CG |
42 43 |
5.13 ± 0.85 5.48 ± 1.03 |
2.97 ± 0.70 3.25 ± 0.92 |
1.48 ± 0.36 1.52 ± 0.37 |
1.26 ± 0.72 1.27 ± 0.66 |
4 |
| Chilibec [83] 2013 Canada |
Parallel groups 24-month follow-up |
Age 56.6 ± 68 y, yms N/A, BMI 27.1 ± 4.1, healthy |
IC 165 mg (150 mg Agl: Gen, Da and Gly in ratio of 1:1:0.5) vs. placebo |
SG CG |
72 73 |
5.87 ± 0.96 5.76 ± 0.91 |
3.68 ± 0.91 3.59 ± 0.89 |
1.58 ± 0.41 1.52 ± 0.44 |
1.41 ± 1.03 1.43 ± 0.79 |
4 |
| Engelbert [86] 2016 Germany |
Parallel groups 12-week follow-up |
Age 59.5 ± 6.03 y, yms ≥ 1 y, BMI 25.2 ± 3.8, healthy |
IAE 117.4 mg (49.7% Gen, 41.4% Dai, 9.0% Gly) vs. placebo, maltodextrin |
SG CG |
85 85 |
5.88 ± 0.89 5.80 ± 0.91 |
3.78 ± 0.89 3.67 ± 0.85 |
1.95 ± 0.44 1.99 ± 0.45 |
1.04 ± 0.39 1.04 ± 0.38 |
4 |
| Barrasa [82] 2018 Chile |
Parallel groups 1-week run-in 3-month follow-up |
Age 64.7 ± 4.6 y, ysm N/A, BMI 27.6 ± 0.9, healthy |
IAE 100 mg (52 mg Gen, 40 mg Dai, 8 mg Gly) vs. placebo |
SG CG |
20 15 |
5.13 ± 0.68 4.87 ± 0.62 |
3.10 ± 0.94 2.97 ± 0.50 |
1.30 ± 0.43 1.18 ± 0.38 |
1.53 ± 0.39 1.54 ± 0.36 |
4 |
| C. Red clover (Trifolium pratense L.) | ||||||||||
| Hale [96] 2001 Australia |
Parallel groups 3-month follow-up |
Age 47.2 ± 2.4 y, yms N/A, BMI 26.7 ± 4.6, healthy |
IAE 50 mg (big amount of Bio and small amount of For (no data)) vs. placebo |
RCG CG |
14 14 |
4.64 ± 0.78 4.19 ± 0.85 |
2.89 ± 0.61 2.49 ± 0.73 |
1.29 ± 0.24 1.34 ± 0.43 |
1.46 ± 0.67 1.61 ± 1.04 |
4 |
| Atkinson [94] 2004 United Kingdom |
Parallel groups 12-month follow-up |
Age 52.2 ± 4.8 y, yms N/A, BMI 25.3 ± 3.7, healthy |
IAE 40 mg (24.5 mg Bio, 8.0 mg For, 1 mg Gen, 1 mg Dai) vs. placebo |
RCG CG |
77 86 |
6.34 ± 1.19 6.08 ± 1.04 |
4.21 ± 0.94 3.88 ± 1.00 |
1.61 ± 0.41 1.66 ± 0.48 |
1.24 ± 0.71 1.19 ± 0.66 |
3 |
| Schult [100] 2004 USA |
Parallel groups 2-week run-in 12-week follow-up |
Age 52.3 ± 3.1 y, yms 3.2 ± 4.5, BMI 26.1 ± 4.9, healthy |
IAE 82 mg (49 mg Bio, 14 mg For, 8 mg Gen, 7 mg Dai). IAE 57 mg (44.6 mg For, 5.8 mg Bio, 0.8 mg Dai, 0.8 mg Gly) vs. placebo |
RCG 82 RCG 57 CG |
81 81 83 |
5.76 ± 0.92 5.77 ± 1.01 5.72 ± 0.83 |
3.77 ± 1.01 3.81 ± 1.14 3.72 ± 0.79 |
1.36 ± 0.37 1.34 ± 0.34 1.38 ± 0.40 |
1.32 ± 0.65 1.31 ± 0.77 1.22 ± 0.56 |
4 |
| Hilgado [97] 2005 Ecuador |
Cross-over 90-day active phase 7-day washout |
Age 51.3 ± 3.5 y, yms ≥ 1 y, BMI 26.1 ± 3.9, healthy |
IAE 80 mg (49 mg Bio, 16 mg For, 8 mg Gen, 7 mg Dai) vs. placebo |
RCG CG |
53 53 |
5.79 ± 0.97 5.79 ± 0.97 |
3.80 ± 0.77 3.80 ± 0.77 |
1.03 ± 0.30 1.03 ± 0.30 |
2.28 ± 0.89 2.28 ± 0.89 |
4 |
| Clifton-Bligh [95] 2015 Australia |
Parallel groups 1-month run-in 12-month follow-up |
Age 54.4 ± 3.9 y, yms ≥ 1 y, BMI 24.8 ± 4.3, healthy |
IAE 57 mg (44.6 mg For, 5.8 mg Bio, 1.9 mg Dai, 0.8 mg Gen, 0.8 Gly) vs. placebo |
RCG CG |
56 47 |
5.91 ± 1.05 5.80 ± 0.88 |
3.68 ± 0.94 3.43 ± 0.86 |
1.67 ± 0.35 1.82 ± 0.49 |
1.33 ± 0.60 1.11 ± 0.63 |
5 |
| Lambert [98] 2017 Denmark |
Parallel groups 12-week follow-up |
Age 52.5 ± 3.5 y, yms N/A, BMI 25.7 ± 4.3 healthy |
IEA 33.8 mg (19 mg For, 9 mg Bio, 2.2 mg Gen, 1.6 Dai) vs. placebo |
RCG CG |
30 29 |
5.38 ± 0.19 5.63 ± 0.10 |
3.36 ± 0.16 3.40 ± 0.17 |
1.76 ± 0.15 1.73 ± 0.10 |
1.20 ± 0.09 1.18 ± 0.10 |
6 |
| Lambert [99] 2017 Denmark |
Parallel groups 12-month follow-up |
Age 61.8 ± 6.4 y, amenorrhea ≥12 months, BMI 25.6 ± 4.5, healthy |
IEA 55.8 mg (31.4 mg For, 14.9 mg Bio, 6.9 mg Gen, 2.6 mg Dai) vs. placebo |
RCG CG |
38 40 |
5.54 ± 0.86 5.64 ± 1.01 |
3.28 ± 0.86 3.37 ± 0.89 |
1.81 ± 0.43 1.82 ± 0.51 |
1.16 ± 0.37 1.38 ± 0.63 |
5 |
Data are presented as mean ± standard deviation (SD). Abbreviations: Agl, aglycone; ALA, α-linolenic acid; Bio, biochanin; BMI, body mass index (kg/m2); CG, control group; CP, casein protein; Dai, daidzein; FG, flaxseed group; For, formononetin; FXO, flaxseed oil; Gen, genistein; GFX, ground flaxseed; Gly, glycitein; Glyc, glycoside; HDL-C, high-density lipoprotein cholesterol; IAE; IC, isoflavone conjugate containing aglycone and glycoside; IF, isoflavones (form and composition unknown); LDL-C, low-density lipoprotein cholesterol; MP, milk protein; N/A, not available, RCG, red clover group; ref., reference; SDG, secoisolariciresinol diglucoside; SG, soy group; SP, soy protein; TAG, triacylglycerols; Total-C, total cholesterol; WFX, whole flaxseed; y, year or years; ysm, years since sine menopause.
3.2. Associations between Flaxseed and Plasma Lipid Profiles
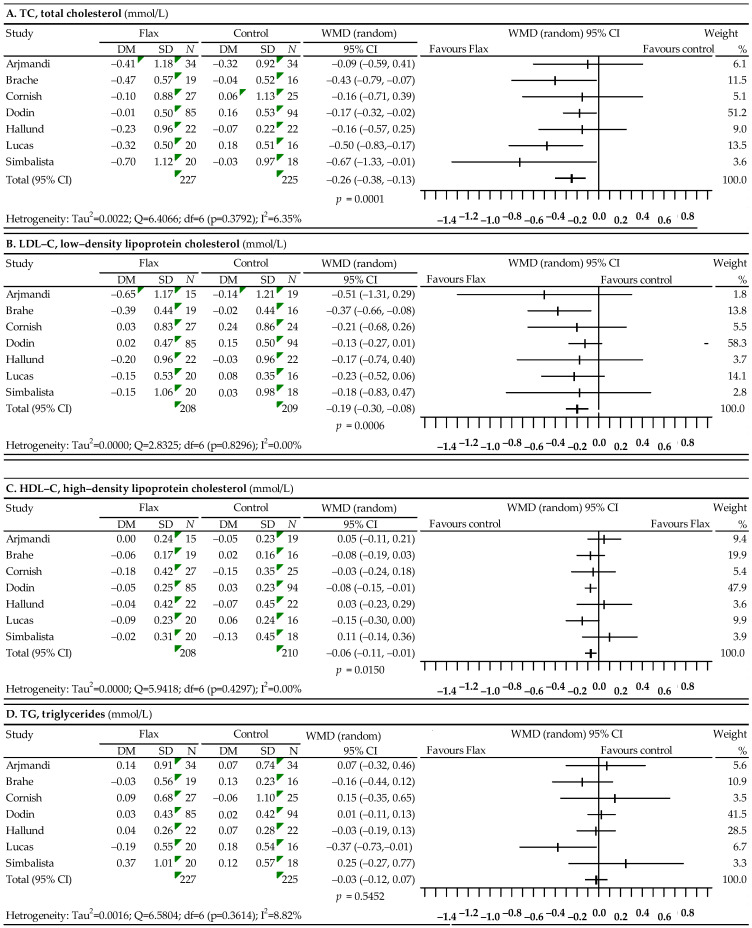
Changes in lipid profile after the use of flaxseed were analyzed on the basis of seven studies [59,60,61,62,63,64,65]. The results of the meta-analysis are presented in Figure 2. Compared to the control group, the use of flaxseed resulted in a statistically significant reduction in TC levels (WMD = −0.26; 95% CI: −0.38–−0.13; p = 0.0001), LDL-C levels (WMD = −0.19; 95% CI: −0.30–−0.08; p = 0.0006) and HDL-C levels (WMD = −0.06; 95% CI: −0.11–−0.01; p = 0.0150) and a slight, not statistically significant reduction in TG levels: WMD = −0.03; 95% CI: −0.12–0.07; p = 0.5452. The heterogeneity analysis performed for TC, LDL-C, HDL-C and TG did not show that the differences between the effects obtained in different studies were statistically significant. The Begg and Egger asymmetry tests showed no publication bias for TC (p-value 0.6523 and 0.3091, respectively), LDL-C (p-value 0.6523 and 0.1786, respectively), HDL-C (p-value 0.1765 and 0.1578, respectively) or TG (p-value 0.4527 and 0.9335, respectively).
Figure 2.
Forest plot representing the associations between flaxseed and lipid profiles. Data are presented as weighted mean difference with 95% CI.
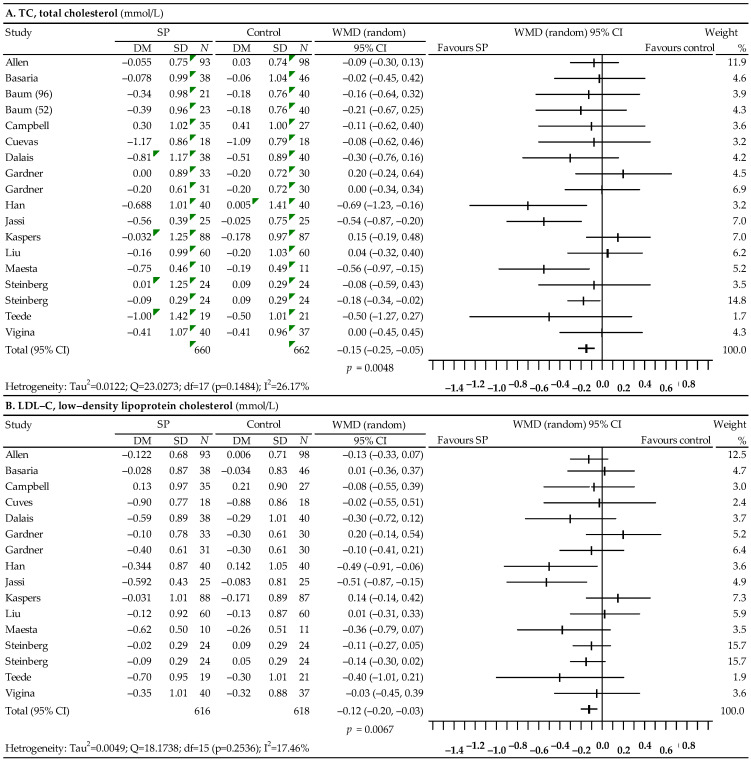
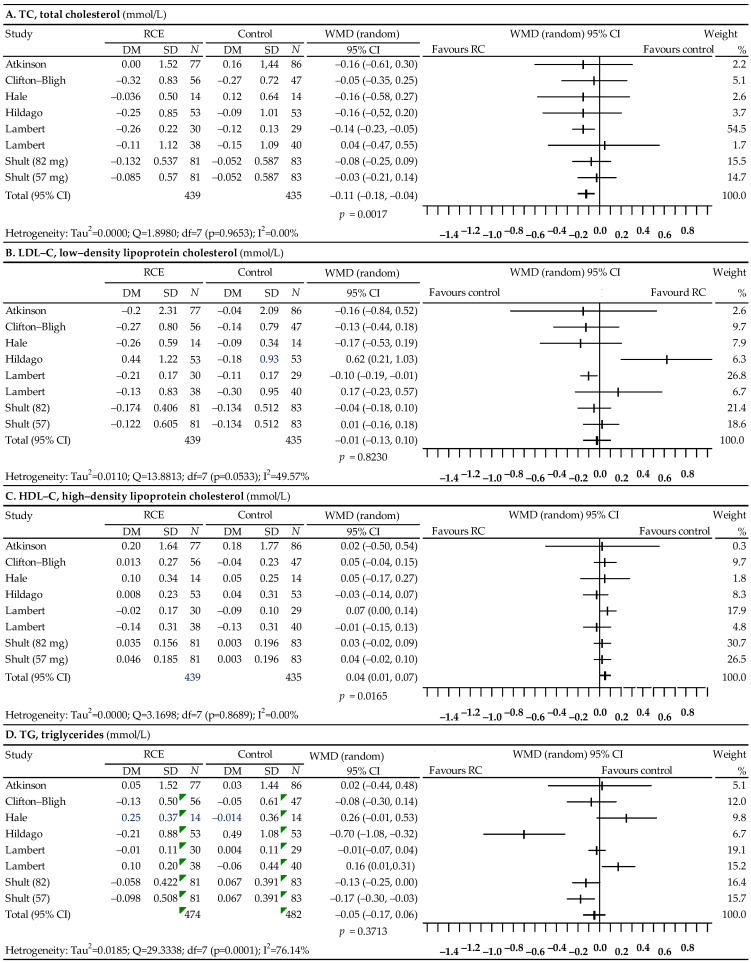
3.3. Associations between Soy Protein without and with Isoflavones and Lipid Profiles
Fifteen studies were used in the analysis of the effect of soy protein on the lipid profile [66,67,68,69,70,71,72,73,74,75,76,77,78,79,80], but the data from the study by Baum et al. did not allow for a comparison of the effect in the case of LDL-C levels [68]. The results of the meta-analysis are presented in Figure 3. Statistical analysis showed a significant decrease in TC levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0048, LDL-C levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0067, and a significant increase in HDL-C levels: WMD = 0.05; 95% CI: 0.02–0.08; p = 0.0034. There was also a slight reduction in TG levels, which, however, was statistically non-significant (WMD = −0.08; 95% CI: −0.19 to 0.03; p = 0.1462). The performed analysis of heterogeneity did not show statistically significant differences between the effects of the included studies for TC, LDL-C and HDL-C, but in the case of TG, the heterogeneity was high (I2 = 61.43%). Begg’s test gave a statistically non-significant result for TC (p = 0.2403), as well as LDL-C (p = 0.4421), HDL-C (p = 0.8196) and TG (p = 0.0945), which indicated no publication bias. Moreover, Egger’s test showed no publication bias for TC: p = 0.6815, LDL-C: p = 0.5596, HDL-C: p = 0.6843, and TG: p = 0.8158.
Figure 3.
Forest plot representing the associations between soy protein and lipid profiles. Data are presented as weighted mean difference with 95% CI.
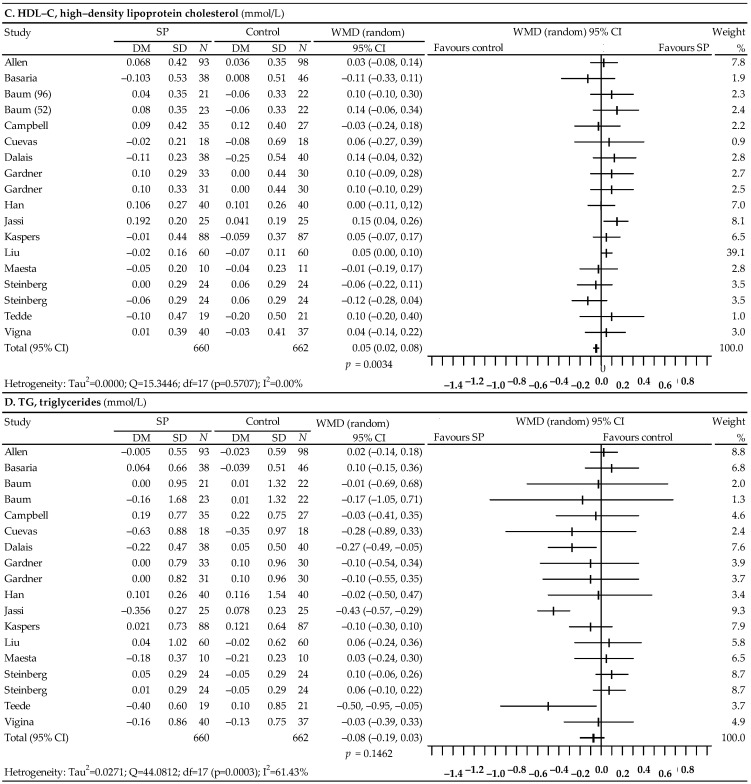
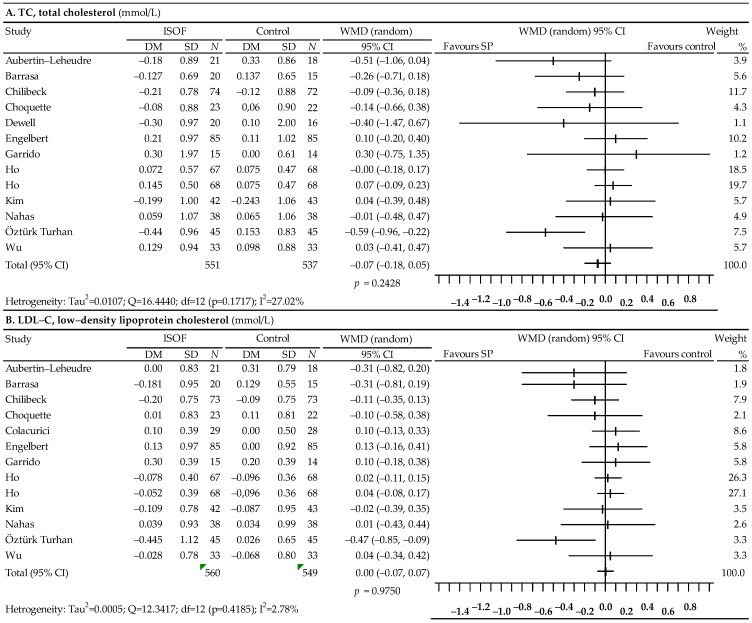
3.4. Associations between Soy Isoflavones Alone (Preparation) and Lipid Profiles
A total of 13 studies were selected to analyze the effect of soy isoflavones on the lipid profile [81,82,83,84,85,86,87,88,89,90,91,92], among which the data from the Colacurici et al. [93] did not allow for the analysis of the effect of isoflavones on TC, while in the study by Dewell et al. [85], there were insufficient data on LDL-C. The results of the meta-analysis are shown in Figure 4. A slight, statistically insignificant decrease in TC levels was observed: WMD = −0.07; 95% CI: −0.18–0.05; p = 0.2428, as well as TG: WMD = −0.04; 95% CI: −0.13–0.05; p = 0.4200. On the other hand, no effect of the use of isoflavones on LDL-C levels was noticed: WMD = 0.00; 95% CI: −0.07–0.07; p = 0.9750 and HDL-C: WMD = 0.01; 95% CI: −0.03–0.05; p = 0.6449. The heterogeneity of the studies was not significant in the case of TC, LDL-C and HDL-C, but it turned out to be high in the case of TG (I2 = 47.34%). The results for the asymmetry tests were not statistically significant for TC: Begg’s test—p = 0.0672; Egger’s test—p = 0.1619, LDL-C: Egger’s test—p = 0.0872, HDL-C: Begg’s test—p = 0.7016; Egger’s test—p = 0.9451 and TG: Begg’s test—p = 0.3520; Egger’s test—p = 0.3281. However, Begg’s test showed a statistically significant publication bias for LDL-C (p = 0.0281).
Figure 4.
Forest plot representing associations between isoflavones and lipid profiles. Data are presented as the weighted mean difference with 95% CI.
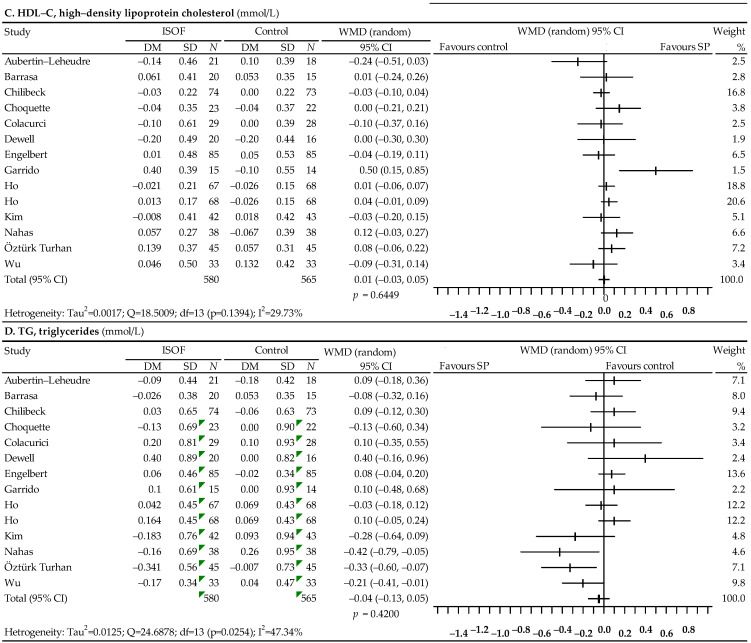
3.5. Associations between Red Clover and Lipid Profiles
The last analysis, presented in Figure 5, concerned the effect of red clover on the lipid profile, and included seven studies [94,95,96,97,98,99,100]. There was a significant reduction in TC levels after the use of red clover (WMD = −0.11; 95% CI: −0.18–−0.04; p = 0.0017) and a statistically significant increase in HDL-C levels (WMD = 0.04; 95% CI: 0.01 to 0.07; p = 0.0165). In the case of TC and HDL-C, no significant heterogeneity of the study effects was observed, and publication bias was not demonstrated. The p value of Begg’s test was 0.4579 for TC and 0.6207 for HDL-C, while the p value of Egger’s test was 0.3990 for TC and 0.5319 for HDL-C. In contrast, statistical analysis showed no significant changes in LDL-C levels after the use of red clover (WMD = −0.01; 95% CI: −0.13 to 0.10; p = 0.8230) and showed a slight decrease in TG levels, which was statistically insignificant (WMD = −0.05; 95% CI: −0.17–0.06; p = 0.3713). In the case of LDL-C and TG, the heterogeneity of the studies turned out to be high (I2 = 49.57% and I2 = 76.14%, respectively). The asymmetry tests showed no publication bias. The p value of Begg’s test was 0.4527 for LDL-C and 0.4527 for TG, while the p value of Egger’s test was 0.2560 for LDL-C and 0.6425 for TG.
Figure 5.
Forest plot representing associations between red clover and lipid profiles. Data are presented as weighted mean difference with 95% CI.
4. Discussion
The present meta-analysis indicates that the intake of flaxseed by postmenopausal women is associated with a statistically significant reduction in TC levels (WMD = −0.26; 95% CI: −0.38 to −0.13; p = 0.0001), LDL-C levels (WMD = −0.19; 95% CI: −0.30 to−0.08; p = 0.0006), HDL-C levels (WMD = −0.06; 95% CI: −0.11 to −0.01; p = 0.0150). These findings are consistent with previous published meta-analyses for the flaxseed effect. A meta-analysis by Hadi et al. incorporating 62 randomized trials involving dietary supplementation with flaxseed or flaxseed-derived products showed that flaxseed supplementation significantly reduced TC (WMD = −5.389 mg/dL; 95% CI: −9.483, −1.295, p = 0.010), TG (WMD = −9.422 mg/dL; 95% CI: −15.514, −3.330, p = 0.002), and LDL-C (WMD = −4.206 mg/dL; 95% CI: −7.260, −1.151, p = 0.007) concentrations. However, it had no effect on HDL-C (WMD = 0.047 mg/dL; 95% CI: −0.777, 0.872, p = 0.910) [101]. The meta-analysis of Yang et al. indicated that different flaxseed products showed different effects. Whole flaxseed supplementation significantly reduced TC (−11.85 mg/dL, 95% CI −20.12–−3.57, p = 0.005), LDL-C (− 10.51 mg/dL, 95% CI −14.96–−6.06, p < 0.001), TG (−19.77 mg/dL, 95% CI −33.61–−5.94, p = 0.005), TC/HDL-C (− 0.10, 95% CI −0.19–−0.003, p = 0.044), while lignans supplementation significantly reduced TC (− 17.86 mg/dL, p = 0.004), LDL-C (− 15.47 mg/dL, p < 0.001), and TC/HDL-C (− 0.45, p = 0.04). Flaxseed oil supplementation had no such lowering effect on lipid [102].
Our meta-analysis of the effect of soy protein on the lipid profile showed a significant decrease in TC levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0048, LDL-C levels: WMD = −0.15; 95% CI: −0.25–0.05; p = 0.0067, as well as a significant increase in HDL-C levels: WMD = 0.05; 95% from CI: 0.02 to 0.08; p = 0.0034. There was also a slight reduction in TG levels, which, however, was statistically non-significant (WMD = −0.08; 95% CI: from −0.19 to 0.03; p = 0.1462). The meta-analysis by Moradi et al. supports the hypercholesterolemic effect of soy lowering the serum TC levels. Soy consumption was associated with a significant decrease in TG: −5.04 mg/dL; 95% CI: −9.95, −0.13; p = 0.044), TC (MD: −3.02 mg/dL; 95% CI: −5.56, −0.47; p= 0.02), LDL-C (3.27 mg/dL; 95% CI: −6.01, −0.53; p = 0.019) and HDL-C (MD: −2.28 mg/dL; 95% CI: −4.27, −0.29; p = 0.025). The reductions in LDL-C, TG, and HDL-C were larger in subjects consuming isolated soy protein than taking-in isolated soy isoflavones [37]. The results of previous meta-analyses also revealed a significant decrease in serum TC, LDL-C, and TG concentrations after the consumption of soy protein containing isoflavones [103].
This meta-analysis showed a significant reduction in TC levels after the use of red clover (WMD = −0.11; 95% CI: from −0.18 to −0.04; p = 0.0017) and a significant increase in HDL-C levels (WMD = 0.04; 95% CI: from 0.01 to 0.07; p = 0.0165). However, the study demonstrated no significant changes in LDL-C levels (WMD = −0.01; 95% CI: from −0.13 to 0.10; p = 0.8230) and a slight statistically insignificant decrease in TG levels (WMD = −0.05; 95% CI: from −0.17 to 0.06; p = 0.3713) after the use of red clover. In their meta-analysis, Luis et al. verified that the consumption of red clover by perimenopausal and postmenopausal women results in a significant decrease in TC, LDL-C, and TG, together with a significant increase in HDL-C [104]. Furthermore, the meta-analysis by Kanadys et al. revealed changes in serum levels: TC, −0.29 (95 % CI: from −0.53 to −0.06) mmol/L, p = 0.0136; LDL-C, −0.13 (95 % CI: from −0.35 to 0.09) mmol/L, p = 0.2418; TG, −0.15 (95 % CI: from −0.32 to 0.01) mmol/L, p = 0.0592; and HDL-C, 0.14 (95 % CI: from −0.08 to 0.36) mmol/L, p = 0.2103—which suggest benefits from red clover consumption specific to correcting abnormal cholesterol levels [105].
Study Limitations
Despite the results obtained in this systematic review and its meta-analysis, some limitations were found. Because of the lack of standardization in some of the study designs, such as the ingredients and doses of isoflavones and the durations and outcomes of the trials, it currently remains difficult to draw overall conclusions for all aspects of isoflavone intake. These limitations warrant further investigation with regard to the use of isoflavone in women’s health. Study limitations can be also be found due to individual differences in the bioavailability of individual components of preparations as these were prepared in a variety of ways that were suitable for each study. Moreover, limitations were posed by potential publication bias, which is revealed via the asymmetry of the funnel plot and the Egger’s model. Publication bias suggests that some small studies with negative findings may have been missed or unpublished. Additionally, effects on vascular function have hardly been studied and more studies are needed to better establish what the effect of flaxseed, soy, red clover are on heart and vascular function.
5. Conclusions
This meta-analysis provides evidence that consuming flaxseed, soy, and red clover can have a beneficial effect on lipids in postmenopausal women. Their consumption could provide an important strategy to control dyslipidemia, and therefore, natural products can be an alternative to medicaments for preventing CVD, which has some clinical relevance in anti-atherosclerotic therapy. Our data also suggest that future well-designed studies with large sample sizes and adequate durations are needed to fully investigate the effectiveness of flaxseed, soy, and red clover.
Author Contributions
A.B. (Agata Błaszczuk): conceptualization, methodology, formal analysis, supervision, writing—original draft, review and editing; A.B. (Agnieszka Barańska): investigation, methodology, project administration, visualization, writing—review and editing; W.K.: conceptualization, investigation, formal analysis, methodology, visualization, writing—review and editing; M.M.: methodology and formal analysis. M.E.J.: resources; U.R. methodology and supervision; R.W.: investigation and project administration. J.H.: software and investigation. M.P.-D.: funding acquisition and supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li Z., Lin L., Wu H., Yan L., Wang H., Yang H., Li H. Global, Regional, and National Death, and Disability-Adjusted Life-Years (DALYs) for Cardiovascular Disease in 2017 and Trends and Risk Analysis From 1990 to 2017 Using the Global Burden of Disease Study and Implications for Prevention. Front. Public Health. 2021;9:559751. doi: 10.3389/fpubh.2021.559751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAloon C.J., Boylan L.M., Hamborg T., Stallard N., Osman F., Lim P.B., Hayat S.A. The changing face of cardiovascular disease 2000−2012: An analysis of the world health organization global health estimates data. Int. J. Cardiol. 2016;224:256–264. doi: 10.1016/j.ijcard.2016.09.026. [DOI] [PubMed] [Google Scholar]
- 3.Wautier J.L., Wautier M.P. Endothelial cell participation in inflammatory reaction. Int. J. Mol. Sci. 2021;22:6341. doi: 10.3390/ijms22126341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munakata M. Clinical significance of stress-related increase in blood pressure: Current evidence in office and out-of-office settings. Hypertens. Res. 2018;41:553–569. doi: 10.1038/s41440-018-0053-1. [DOI] [PubMed] [Google Scholar]
- 5.Veiraiah A. Hyperglycemia, lipoprotein glycation, and vascular disease. Angiology. 2005;56:431–438. doi: 10.1177/000331970505600411. [DOI] [PubMed] [Google Scholar]
- 6.Pirro M., Bianconi V., Paciullo F., Mannarino M.R., Bagaglia F., Sahebkar A. Lipoprotein(a) and inflammation: A dangerous duet leading to endothelial loss of integrity. Pharmacol. Res. 2017;119:178–187. doi: 10.1016/j.phrs.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Steven S., Frenis K., Oelze M., Kalinovic S., Kuntic M., Bayo Jimenez M.T., Vujacic-Mirski K., Helmstädter J., Kröller-Schön S., Münzel T., et al. Vascular inflammation and oxidative stress: Major triggers for cardiovascular disease. Oxid. Med. Cell Longev. 2019;2019:7092151. doi: 10.1155/2019/7092151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papakonstantinou E., Lambadiari V., Dimitriadis G., Zampelas A. Metabolic syndrome and cardiometabolic risk factors. Curr. Vasc. Pharmacol. 2013;11:858–879. doi: 10.2174/15701611113116660176. [DOI] [PubMed] [Google Scholar]
- 9.Abraham T.M., Pedley A., Massaro J.M., Hoffmann U., Fox C.S. Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Circulation. 2015;132:1639–1647. doi: 10.1161/CIRCULATIONAHA.114.015000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y., Cai X., Mai W., Li M., Hu Y. Association between prediabetes and risk of cardiovascular disease and all-cause mortality: Systematic review and meta-analysis. BMJ. 2016;355:i5953. doi: 10.1136/bmj.i5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearson G.J., Thanassoulis G., Anderson T.J., Barry A.R., Couture P., Dayan N., Francis G.A., Genest J., Grégoire J., Grover S.A., et al. Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can. J. Cardiol. 2021;37:1129–1150. doi: 10.1016/j.cjca.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 12.Phung O.J., Makanji S.S., White C.M., Coleman C.I. Almonds have a neutral effect on serum lipid profiles: A meta-analysis of randomized trials. J. Am. Diet Assoc. 2009;109:865–873. doi: 10.1016/j.jada.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Shahinfar H., Bazshahi E., Amini M.R., Payandeh N., Pourreza S., Noruzi Z., Shab-Bidar S. Effects of artichoke leaf extract supplementation or artichoke juice consumption on lipid profile: A systematic review and dose-response meta-analysis of randomized controlled trials. Phytother. Res. 2021;35:6607–6623. doi: 10.1002/ptr.7247. [DOI] [PubMed] [Google Scholar]
- 14.Hadi A., Arab A., Ghaedi E., Rafie N.A., Miraghajani M., Kafeshani M. Barberry (Berberis vulgaris L.) is a safe approach for management of lipid parameters: A systematic review and meta—Analysis of randomized controlled trials. Complement. Ther. Med. 2019;43:117–124. doi: 10.1016/j.ctim.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Sahebkar A. A systematic review and meta-analysis of randomized controlled trials investigating the effects of curcumin on blood lipid levels. Clin. Nutr. 2014;33:406–414. doi: 10.1016/j.clnu.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Pourmasoumi M., Hadi A., Rafie N., Najafgholizadeh A., Mohammadi H., Rouhani M.H. The effect of ginger supplementation on lipid profile: A systematic review and meta-analysis of clinical trials. Phytomedicine. 2018;43:28–36. doi: 10.1016/j.phymed.2018.03.043. [DOI] [PubMed] [Google Scholar]
- 17.Wei Z.H., Wang H., Chen X.Y., Wang B.S., Rong Z.X., Wang B.S., Su B.H., Chen H.Z. Time- and dose-dependent effect of psyllium on serum lipids in mild-to-moderate hypercholesterolemia: A meta-analysis of controlled clinical trials. Eur. J. Clin. Nutr. 2009;63:821–827. doi: 10.1038/ejcn.2008.49. [DOI] [PubMed] [Google Scholar]
- 18.Khalesi S., Paukste E., Nikbakht E., Khosravi-Boroujeni H. Sesame fractions and lipid profiles: A systematic review and meta-analysis of controlled trials. Br. J. Nutr. 2016;115:764–773. doi: 10.1017/S0007114515005012. [DOI] [PubMed] [Google Scholar]
- 19.Jia L., Liu X., Bai Y.Y., Li S.H., Sun K., He C., Hui R. Short-term effect of cocoa product consumption on lipid profile: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2010;92:218–225. doi: 10.3945/ajcn.2009.28202. [DOI] [PubMed] [Google Scholar]
- 20.Tuccinardi D., Farr O.M., Upadhyay J., Oussaada S.M., Klapa M.I., Candela M., Rampelli S., Lehoux S., Lázaro I., Sala-Vila A., et al. Mechanisms underlying the cardiometabolic protective effect of walnut consumption in obese people: A cross-over, randomized, double-blind, controlled inpatient physiology study. Diabetes Obes. Metab. 2019;21:2086–2095. doi: 10.1111/dom.13773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.da Silva I.T., de Almeida-Pititto B., Ferreira S.R.G. Reassessing lipid metabolism and its potentialities in the prediction of cardiovascular risk. Arch. Endocrinol. Metab. 2015;59:171–180. doi: 10.1590/2359-3997000000031. [DOI] [PubMed] [Google Scholar]
- 22.Meldrum D.R., Davidson B.J., Tataryn I.V., Judd J.L. Changes in circulating steroids with aging in postmenopausal women. Obs. Gynecol. 1981;57:624–628. [PubMed] [Google Scholar]
- 23.Derby C.A., Crawford S.L., Pasternak R.C., Sowers M., Sternfeld B., Matthews K.A. Lipid changes during the menopause transition in relation to age and weight: The Study of Women’s Health Across the Nation. Am. J. Epidemiol. 2009;119:1352–1361. doi: 10.1093/aje/kwp043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cho E.J., Min Y.J., Oh M.S., Kwon J.E., Kim J.E., Lee W.S., Lee K.J., Kim S.W., Kim T.H., Kim M.A., et al. Effects of the transition from premenopause to postmenopause on lipids and lipoproteins: Quantification and related parameters. Korean J. Intern. Med. 2011;26:47–53. doi: 10.3904/kjim.2011.26.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ambikairajah A., Walsh E., Cherbuin N. Lipid profile differences during menopause: A review with meta-analysis. Menopause. 2019;26:1327–1333. doi: 10.1097/GME.0000000000001403. [DOI] [PubMed] [Google Scholar]
- 26.Anagnostis P., Stevenson J.C., Crook D., Johnston D.G., Godsland I.F. Effects of menopause, gender and age on lipids and high-density lipoprotein cholesterol subfractions. Maturitas. 2015;81:62–68. doi: 10.1016/j.maturitas.2015.02.262. [DOI] [PubMed] [Google Scholar]
- 27.Ko S.H., Kim H.S. Menopause-associated lipid metabolic disorders and foods beneficial for postmenopausal women. Nutrients. 2020;12:202. doi: 10.3390/nu12010202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shim Y.Y., Gui B., Arnison P.G., Wang Y. Flaxseed (Linum usitatissimum L.) bioactive compounds and peptide nomenclature: A review. Trends Food Sci. Technol. 2014;38:5–20. doi: 10.1016/j.tifs.2014.03.011. [DOI] [Google Scholar]
- 29.Campos J.R., Severino P., Ferreira C.S., Zielinska A., Santini A., Souto S.B., Souto E.B. Linseed essential oil—Source of lipids as active ingredients for pharmaceuticals and nutraceuticals. Curr. Med. Chem. 2019;26:4537–4558. doi: 10.2174/0929867325666181031105603. [DOI] [PubMed] [Google Scholar]
- 30.Kitts D.D., Yuan Y., Wijewickreme A.N., Thompson L.U. Antioxidant activity of the flaxseed lignan secoisolariciresinol diglycoside and its mammalian lignan metabolites enterodiol and enterolactone. Mol. Cell. Biochem. 1999;202:91–100. doi: 10.1023/A:1007022329660. [DOI] [PubMed] [Google Scholar]
- 31.Sanghvi A., Divven W., Seltman H. Inhibition of rat liver cholesterol 7-alpha hydroxylase and Acylotransferaza acylo-CoA: Cholesterol activities by entrodiol and enterolactone. In: Kritchevsky D., editor. Proceedings of the Symposium on Drugs Affecting Lipid Metabolism. Plenum Press; New York, NY, USA: 1984. pp. 311–322. [Google Scholar]
- 32.Burdge G. a-Linolenic acid metabolism in men and women: Nutritional and biological implications. Curr. Opin. Clin. Nutr. Metab. Care. 2004;7:137–144. doi: 10.1097/00075197-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Agyei A. Bioactive proteins and peptides from soybeans. Recent Pat. Food Nutr. Agric. 2015;7:100–107. doi: 10.2174/2212798407666150629134141. [DOI] [PubMed] [Google Scholar]
- 34.Torres N., Torre-Villalvazo I., Tovar A.R. Regulation of lipid metabolism by soy protein and its implication in diseases mediated by lipid disorders. J. Nutr. Biochem. 2006;17:365–373. doi: 10.1016/j.jnutbio.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 35.Kim I.S. Current perspectives on the beneficial effects of soybean isoflavones and their metabolites for humans. Antioxidants. 2021;10:1064. doi: 10.3390/antiox10071064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vitale D.C., Piazza C., Melilli B., Drago F., Salomone S. Isoflavones: Estrogenic activity, biological effect and bioavailability. Eur. J. Drug Metab. Pharmacokinet. 2013;38:15–25. doi: 10.1007/s13318-012-0112-y. [DOI] [PubMed] [Google Scholar]
- 37.Moradi M., Daneshzad E., Azadbakht L. The effects of isolated soy protein, isolated soy isoflavones and soy protein containing isoflavones on serum lipids in postmenopausal women: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2020;60:3414–3428. doi: 10.1080/10408398.2019.1689097. [DOI] [PubMed] [Google Scholar]
- 38.Butteiger D.N., Hibberd A.A., McGraw N.J., Napawan N., Hall-Porter J.M., Krul E.S. Soy protein compared with milk protein in a western diet increases gut microbial diversity and reduces serum lipids in Golden Syrian Hamsters. J. Nutr. 2016;146:697–705. doi: 10.3945/jn.115.224196. [DOI] [PubMed] [Google Scholar]
- 39.Dang Z.C., Audinot V., Papapoulos S.E., Boutin J.A., Löwik C.W.G.M. Peroxisome proliferator-activated receptor gamma (PPARgamma) as a molecular target for the soy phytoestrogen genistein. J. Biol. Chem. 2003;278:962–967. doi: 10.1074/jbc.M209483200. [DOI] [PubMed] [Google Scholar]
- 40.Oliveira L.P.M., de Jesús R.P., Freire T.O., Oliveira C.P., Lyra A.C., Lyra L.G.C. Possible molecular mechanisms soy-mediated in preventing and treating nonalcoholic fatty liver disease. Nutr. Hosp. 2012;27:991–998. doi: 10.3305/nh.2012.27.4.5833. [DOI] [PubMed] [Google Scholar]
- 41.Dentin R., Girard J., Postic C. Carbohydrate responsive element binding protein (ChREBP) and sterol 42. regulatory element binding protein-1c (SREBP-1c): Two key regulators of glucose metabolism and lipid synthesis in liver. Biochimie. 2005;87:81–86. doi: 10.1016/j.biochi.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 42.Demonty I., Lamarche B., Deshaies Y., Jacques H. Role of soy isoflavones in the hypotriglyceridemic effect of soy protein in the rat. J. Nutr. Biochem. 2002;13:671–677. doi: 10.1016/S0955-2863(02)00214-0. [DOI] [PubMed] [Google Scholar]
- 43.Xue Z., Zhang Q., Yu W., Wen H., Hou X., Li D., Kou X. Potential lipid-lowering mechanisms of Biochanin A. Agric. Food Chem. 2017;65:3842–3850. doi: 10.1021/acs.jafc.7b00967. [DOI] [PubMed] [Google Scholar]
- 44.Andres S., Hansen U., Niemann B., Palavinskas R., Lampen A. Determination of the isoflavone composition and estrogenic activity of commercial dietary supplements based on soy or red clover. Food Funct. 2015;6:2017–2025. doi: 10.1039/C5FO00308C. [DOI] [PubMed] [Google Scholar]
- 45.Lemežiene N., Padarauskas A., Butkuté B., Ceseviĕciené J., Taujenis L., Norkeviĕciené E. The concentration of isoflavones in red clover (Trifolium pratense L.) at flowering stage. Zemdirb. Agric. 2015;102:443–448. doi: 10.13080/z-a.2015.102.057. [DOI] [Google Scholar]
- 46.Booth N.L., Overk C.R., Yao P., Burdette J.E., Nikolic D., Chen S.N., Bolton J.L., van Breemen R.B., Pauli G.F., Farnsworth N.R. The chemical and biologic profile of a red clover (Trifolium pratense L.) phase II clinical extract. J. Altern. Complement. Med. 2006;12:113–133. doi: 10.1089/acm.2006.12.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Booth N.L., Overk C.R., Yao P., Totura S., Deng Y., Hedayat A.S., Bolton J.L., Pauli G.F., Farnsworth N.R. Seasonal variation of red clover (Trifolium pratense L., Fabaceae) isoflavones and estrogenic activity. J. Agric. Food Chem. 2006;54:1277–1282. doi: 10.1021/jf052927u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akbaribazm M., Khazaei F., Naseri L., Pazhouhi M., Zamanian M., Khazaei M. Pharmacological and therapeutic properties of the Red Clover (Trifolium pratense L.): An overview of the new findings. J. Tradit. Chin. Med. 2021;41:642–649. doi: 10.19852/j.cnki.jtcm.20210324.001. [DOI] [PubMed] [Google Scholar]
- 49.Akiyama T., Ishida J., Nakagawa S., Ogawara H., Watanabe S., Itoh N., Shibuya M., Fukami Y. Genistein, a specific inhibitor of tyrosine-specific protein kinases. J. Biol. Chem. 1987;262:5592–5595. doi: 10.1016/S0021-9258(18)45614-1. [DOI] [PubMed] [Google Scholar]
- 50.Hobiger S., Jungbauer A. Red clover extract: A source for substances that activate peroxisome proliferator-activated receptor alpha and ameliorate the cytokine secretion profile of lipopolysaccharide-stimulated macrophages. Menopause. 2010;17:379–387. doi: 10.1097/gme.0b013e3181c94617. [DOI] [PubMed] [Google Scholar]
- 51.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Mark Petticrew M., Shekelle P., Stewart L.A. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jadad A.R., Moore R.A., Carroll D., Jenkinson C., Reynolds D.J., Gavaghan D.J., McQuay H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials. 1996;17:100–107. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 53.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 54.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (Updated July 2020) John Wiley; Hooboken, NJ, USA: 2019. [Google Scholar]
- 56.Follmann D., Elliott P., Suh I., Cutler J. Variance imputation for overviews of clinical trials with continuous response. J. Clin. Epidemiol. 1992;45:769–773. doi: 10.1016/0895-4356(92)90054-Q. [DOI] [PubMed] [Google Scholar]
- 57.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 58.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arjmandi B.H., AKhan D.A., Juma S., Drum M.L., Venkatesh S., Sohn E., Wei L., Derman R. Whole flaxseed consumption lowers serum LDL-cholesterol and lipoprotein(a) concentrations in postmenopausal women. Nutr. Res. 1998;18:1203–1204. doi: 10.1016/S0271-5317(98)00100-6. [DOI] [Google Scholar]
- 60.Brahe L.K., Le Chatelier E., Prifti E., Pons N., Kennedy S., Blaedel T., Hakansson J., Dalsgaard T.K., Hansen T., Pedersen O., et al. Dietary modulation of the gut microbiota—A randomized controlled trial in obese postmenopausal women. Br. J. Nutr. 2015;114:406–417. doi: 10.1017/S0007114515001786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cornish S.M., Chilibeck P.D., Paus-Jennsen L., Biem H.J., Khozani T., Senanayake V., Vatanparast H., Little J.P., Whiting S.J., Pahwa P. A randomized controlled trial of the effects of flaxseed lignan complex on metabolic syndrome composite score and bone mineral in older adults. Appl. Physiol. Nutr. Metab. 2009;34:89–98. doi: 10.1139/H08-142. [DOI] [PubMed] [Google Scholar]
- 62.Dodin S., Lemay A., Jacques H., Legare F., Forest J.C., Masse B. The effects of flaxseed dietary supplement on lipid profile, bone mineral density, and symptoms in menopausal women: A randomized, double-blind, wheat germ placebo-controlled clinical trial. J. Clin. Endocrinol. Metab. 2005;90:1390–1397. doi: 10.1210/jc.2004-1148. [DOI] [PubMed] [Google Scholar]
- 63.Hallund J., Ravn-Haren G., Bügel S., Tholstrup T., Tetens I. A lignan complex isolated from flaxseed does not affect plasma lipid concentrations or antioxidant capacity in healthy postmenopausal women. J. Nutr. 2006;136:112–116. doi: 10.1093/jn/136.1.112. [DOI] [PubMed] [Google Scholar]
- 64.Lucas E.A., Wild R.D., Hammond L.J., Khalil D.A., Juma S., Daggy B.P., Stoecker B.J., Arjmandi B.H. Flaxseed improves lipid profile without altering biomarkers of bone metabolism in postmenopausal women. J. Clin. Endocrinol. Metab. 2002;87:1527–1532. doi: 10.1210/jcem.87.4.8374. [DOI] [PubMed] [Google Scholar]
- 65.Simbalista R.L., Sauerbronn A.V., Aldrighi J.M., Arêas J.A.G. Consumption of a flaxseed-rich food is not more effective than a placebo in alleviating the climacteric symptoms of postmenopausal women. J. Nutr. 2010;140:293–297. doi: 10.3945/jn.109.113886. [DOI] [PubMed] [Google Scholar]
- 66.Allen J.K., Becker D.M., Kwiterovich P.O., Lindenstruth K.A., Curtis C. Effect of soy protein-containing isoflavones on lipoproteins in postmenopausal women. Menopause. 2007;14:106–114. doi: 10.1097/01.gme.0000229572.21635.49. [DOI] [PubMed] [Google Scholar]
- 67.Basaria S., Wisniewski A., Dupree K., Bruno T., Song M.Y., Yao F., Ojumu A., John M., Dobs A.S. Effect of high-dose isoflavones on cognition, quality of life, androgens, and lipoprotein in post-menopausal women. J. Endocrinol. Investig. 2009;32:150–155. doi: 10.1007/BF03345705. [DOI] [PubMed] [Google Scholar]
- 68.Baum J.A., Teng H., Erdman J.W., Jr., Weigel R.M., Klein B.P., Persky V.W., Freels S., Surya P., Bakhit R.M., Ramos E., et al. Long-term intake of soy protein improves blood lipid profiles and increases mononuclear cell low-density-lipoprotein receptor messenger RNA in hypercholesterolemic, postmenopausal women. Am. J. Clin. Nutr. 1998;68:545–551. doi: 10.1093/ajcn/68.3.545. [DOI] [PubMed] [Google Scholar]
- 69.Campbell S.C., Khalil D.A., Payton M.E., Arjmandi B.H. One-year soy protein supplementation does not improve lipid profile in postmenopausal women. Menopause. 2010;17:587–593. doi: 10.1097/gme.0b013e3181cb85d3. [DOI] [PubMed] [Google Scholar]
- 70.Cuevas A.M., Irribarra V.L., Castillo O.A., Yañez M.D., Germain A.M. Isolated soy protein improves endothelial function in postmenopausal hypercholesterolemic women. Eur. J. Clin. Nutr. 2003;57:889–894. doi: 10.1038/sj.ejcn.1601622. [DOI] [PubMed] [Google Scholar]
- 71.Dalais F.S., Ebeling P.R., Kotsopoulos D., McGrath B.P., Teede H.J. The effects of soy protein containing isoflavones on lipids and indices of bone resorption in postmenopausal women. Clin. Endocrinol. 2003;58:704–709. doi: 10.1046/j.1365-2265.2003.01771.x. [DOI] [PubMed] [Google Scholar]
- 72.Gardner C.D., Newell K.A., Cherin R., Haskell W.L. The effect of soy protein with or without isoflavones relative to milk protein on plasma lipids in hypercholesterolemic postmenopausal women. Am. J. Clin. Nutr. 2001;73:728–735. doi: 10.1093/ajcn/73.4.728. [DOI] [PubMed] [Google Scholar]
- 73.Han K.K., Soares J.M., Jr., Haidar M.A., de Lima G.R., Baracat E.C. Benefits of soy isoflavone therapeutic regimen on menopausal symptoms. Obstet. Gynecol. 2002;99:389–394. doi: 10.1016/s0029-7844(01)01744-6. [DOI] [PubMed] [Google Scholar]
- 74.Jassi H.K., Jain A., Arora S., Chitra R. Effect of soy proteins vs. soy isoflavones on lipid profile in postmenopausal women. Indian J. Clin. Biochem. 2010;25:201–207. doi: 10.1007/s12291-010-0036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kreijkamp-Kaspers S., Kok L., Grobbee D.E., de Haan E.H., Aleman A., Lampe J.W., van der Schouw Y.T. Effect of soy protein containing isoflavones on cognitive function, bone mineral density, and plasma lipids in postmenopausal women: A randomized controlled trial. JAMA. 2004;292:65–74. doi: 10.1001/jama.292.1.65. [DOI] [PubMed] [Google Scholar]
- 76.Liu Z.M., Ho S.C., Chen Y.M., Ho Y.P. The effects of isoflavones combined with soy protein on lipid profiles, C-reactive protein and cardiovascular risk among postmenopausal Chinese women. Nutr. Metab. Cardiovasc. Dis. 2012;22:712–719. doi: 10.1016/j.numecd.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 77.Maesta N., Nahas E.A.P., Nahas-Neto J., Orsatti F.L., Fernandes C.E., Traiman P., Burini R.C. Effects of soy protein and resistance exercise on body composition and blood lipids in postmenopausal women. Maturitas. 2007;56:350–358. doi: 10.1016/j.maturitas.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 78.Steinberg F.M., Guthrie N.L., Villablanca A.C., Kumar K., Murray M.J. Soy protein with isoflavones has favorable effects on endothelial function that are independent of lipid and antioxidant effects in healthy postmenopausal women. Am. J. Clin. Nutr. 2003;78:123–130. doi: 10.1093/ajcn/78.1.123. [DOI] [PubMed] [Google Scholar]
- 79.Teede H.J., Dalais F.S., Kotsopoulos D., McGrath B.P., Malan E., Gan T.E., Peverill R.E. Dietary soy containing phytoestrogens does not activate the hemostatic system in postmenopausal women. J. Clin. Endocrinol. Metab. 2005;90:1936–1941. doi: 10.1210/jc.2004-1428. [DOI] [PubMed] [Google Scholar]
- 80.Vigna G.B., Pansini F., Bonaccorsi G., Albertazzi P., Donegà P., Zanotti L., De Aloysio D., Mollica G., Fellin R. Plasma lipoproteins in soy-treated postmenopausal women: A double-blind, placebo-controlled trial. Nutr. Metab. Cardiovasc. Dis. 2000;10:315–322. [PubMed] [Google Scholar]
- 81.Aubertin-Leheudre M., Lord C., Khalil A., Dionne I.J. Effect of 6 months of physical activity and isoflavone supplementation on clinical cardiovascular risk factors in obese postmenopausal women: A randomized, double-blind study. Menopause. 2007;14:624–629. doi: 10.1097/gme.0b013e31802e426b. [DOI] [PubMed] [Google Scholar]
- 82.Barrasa G.R.R., Canete N.G., Boasi L.E.V. Age of postmenopause women: Effect of soy isoflavone in lipoprotein and inflammation markers. J. Menopausal. Med. 2018;243:176–182. doi: 10.6118/jmm.2018.24.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chilibeck P.D., Vatanparast H., Pierson R., Case A., Olatunbosun O., Whiting S.J., Beck T.J., Pahwa P., Biem H.J. Effect of exercise training combined with isoflavone supplementation on bone and lipids in postmenopausal women: A randomized clinical trial. J. Bone Miner Res. 2013;28:780–793. doi: 10.1002/jbmr.1815. [DOI] [PubMed] [Google Scholar]
- 84.Choquette S., Riesco É., Cormier É., Dion T., Aubertin-Leheudre M., Dionne I.J. Effects of soya isoflavones and exercise on body composition and clinical risk factors of cardiovascular diseases in overweight postmenopausal women: A 6-month double-blind controlled trial. Br. J. Nutr. 2011;105:1199–1209. doi: 10.1017/S0007114510004897. [DOI] [PubMed] [Google Scholar]
- 85.Dewell A., Hollenbeck C.B., Bruce B. The effects of soy-derived phytoestrogens on serum lipids and lipoproteins in moderately hypercholesterolemic postmenopausal women. J. Clin. Endocrinol. Metab. 2002;87:118–121. doi: 10.1210/jcem.87.1.8155. [DOI] [PubMed] [Google Scholar]
- 86.Engelbert A.K., Soukup S.T., Roth A., Hoffmann N., Graf D., Watzl B., Kulling S.E., Bub A. Isoflavone supplementation in postmenopausal women does not affect leukocyte LDL receptor and scavenger receptor CD36 expression: A double-blind, randomized, placebo-controlled trial. Mol. Nutr. Food Res. 2016;60:2008–2019. doi: 10.1002/mnfr.201600019. [DOI] [PubMed] [Google Scholar]
- 87.Garrido A., De la Maza M.P., Hirsch S., Valladares L. Soy isoflavones affect platelet thromboxane A2 receptor density but not plasma lipids in menopausal women. Maturitas. 2006;54:270–276. doi: 10.1016/j.maturitas.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 88.Ho S.C., Chen Y.M., Ho S.S.S., Woo J.L.F. Soy isoflavone supplementation and fasting serum glucose and lipid profile among postmenopausal Chinese women: A double-blind, randomized, placebo-controlled trial. Menopause. 2007;14:905–912. doi: 10.1097/gme.0b013e318032b2d3. [DOI] [PubMed] [Google Scholar]
- 89.Kim J., Lee H., Lee O., Lee K.H., Lee Y.B., Young K.D., Jeong Y.H., Choue R. Isoflavone supplementation influenced levels of triglyceride and luteunizing hormone in Korean postmenopausal women. Arch. Pharm. Res. 2013;36:306–313. doi: 10.1007/s12272-013-0059-9. [DOI] [PubMed] [Google Scholar]
- 90.Nahas E.A.P., Nahas-Neto J., Orsatti F.L., Carvalho E.P., Oliveira M.L.C.S., Dias R. Efficacy and safety of a soy isoflavone extract in postmenopausal women: A randomized, double-blind, and placebo-controlled study. Maturitas. 2007;58:249–258. doi: 10.1016/j.maturitas.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 91.Öztürk Turhan N.O., Duvan C.I., Bolkan F., Onaran Y. Effect of isoflavone on plasma nitrite/nitrate, homocysteine, and lipid levels in Turkish women in the early postmenopausal period: A randomized controlled trial. Turk. J. Med. Sci. 2009;39:367–375. [Google Scholar]
- 92.Wu J., Oka J., Tabata I., Higuchi M., Toda T., Fuku N., Ezaki J., Sugiyama F., Uchiyama S., Yamada K., et al. Effects of isoflavone and exercise on BMD and fat mass in postmenopausal Japanese women: A 1-year randomized placebo-controlled trial. J. Bone Miner Res. 2006;21:780–789. doi: 10.1359/jbmr.060208. [DOI] [PubMed] [Google Scholar]
- 93.Colacurci N., Chiàntera A., Fornaro F., de Novellis V., Manzella D., Arciello A., Chiàntera V., Improta L., Paolisso G. Effects of soy isoflavones on endothelial function in healthy postmenopausal women. Menopause. 2005;12:299–307. doi: 10.1097/01.GME.0000147017.23173.5B. [DOI] [PubMed] [Google Scholar]
- 94.Atkinson C., Oosthuizen W., Scollen S., Loktionov A., Day N.E., Bingham S.A. Modest protective effects of isoflavones from a red clover derived dietary supplement on cardiovascular disease risk factors in perimenopausal women, and evidence of an interaction with ApoE genotype in 49–65 year old women. J. Nutr. 2004;134:1759–1764. doi: 10.1093/jn/134.7.1759. [DOI] [PubMed] [Google Scholar]
- 95.Clifton-Bligh P.B., Nery M.L., Clifton-Bligh R.J., Visvalingam S., Fulcher G.R., Byth K., Baber R. Red clover isoflavones enriched with formononetin lower serum LDL cholesterol—a randomized, double-blind, placebo-controlled study. Eur. J. Clin. Nutr. 2015;69:134–142. doi: 10.1038/ejcn.2014.207. [DOI] [PubMed] [Google Scholar]
- 96.Hale G.E., Hughes C.L., Robboy S.J., Agarwal S.K., Bievre M. A double-blind randomized study on the effects of red clover isoflavones on the endometrium. Menopause. 2001;8:338–346. doi: 10.1097/00042192-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 97.Hidalgo L.A., Chedraui P.A., Morocho N., Ross S., San Miguel G. The effect of red clover isoflavones on menopausal symptoms, lipids and vaginal cytology in menopausal women: A randomized, double-blind, placebo-controlled study. Gynecol. Endocrinol. 2005;21:257–264. doi: 10.1080/09513590500361192. [DOI] [PubMed] [Google Scholar]
- 98.Lambert M.N.T., Thorup A.C., Hansen E.S.S., Jeppesen P.B. Combined red clover isoflavones and probiotics potently reduce menopausal vasomotor symptoms. PLoS ONE. 2017;12:e0176590. doi: 10.1371/journal.pone.0176590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lambert M.N.T., Thybo C.B., Lykkeboe S., Rasmussen L.M., Frette X., Christensen L.P., Jeppesen P.B. Combined bioavailable isoflavones and probiotics improve bone status and estrogen metabolism in postmenopausal osteopenic women: A randomized controlled trial. Am. J. Clin. Nutr. 2017;106:909. doi: 10.3945/ajcn.117.153353. [DOI] [PubMed] [Google Scholar]
- 100.Schult T.M., Ensrud K.E., Blackwell T., Ettinger B., Wallace R., Tice J.A. Effect of isoflavones on lipids and bone turnover markers in menopausal women. Maturitas. 2004;48:209–218. doi: 10.1016/j.maturitas.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 101.Hadi A., Askarpour M., Shekoufeh S., Ghaedi E., Symonds M.E., Miraghajani M. Effect of flaxseed supplementation on lipid profile: An updated systematic review and dose-response meta-analysis of sixty-two randomized controlled trials. Pharmacol. Res. 2020;152:104622. doi: 10.1016/j.phrs.2019.104622. [DOI] [PubMed] [Google Scholar]
- 102.Yang C., Xia H., Wan M., Lu Y., Xu D., Yang X., Yang L., Sun G. Comparisons of the effects of different flaxseed products consumption on lipid profiles, inflammatory cytokines and anthropometric indices in patients with dyslipidemia related diseases: Systematic review and a dose–response meta-analysis of randomized controlled trials. Nutr. Metab. 2021;18:91. doi: 10.1186/s12986-021-00619-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhan S., Ho S.C. Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am. J. Clin. Nutr. 2005;81:397–408. doi: 10.1093/ajcn.81.2.397. [DOI] [PubMed] [Google Scholar]
- 104.Luís A., Domingues F., Pereira L. Effects of red clover on perimenopausal and postmenopausal women’s blood lipid profile: A meta-analysis. Climacteric. 2018;21:446–453. doi: 10.1080/13697137.2018.1501673. [DOI] [PubMed] [Google Scholar]
- 105.Kanadys W., Baranska A., Jedrych M., Religioni U., Janiszewska M. Effects of red clover (Trifolium pratense) isoflavones on the lipid profile of perimenopausal and postmenopausal women—A systematic review and meta-analysis. Maturitas. 2020;132:7–16. doi: 10.1016/j.maturitas.2019.11.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.