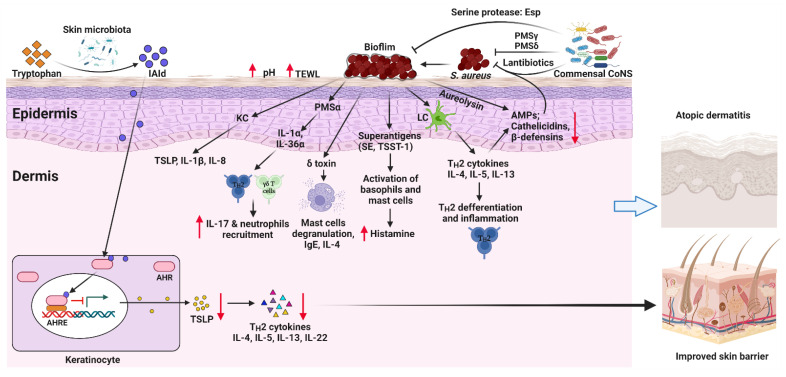
Figure 1.
Mechanisms of how skin microbiota regulates AD pathogenesis. Excessive S. aureus colonization on the skin leads to the formation of biofilms and the secretion of virulence factors. These virulence factors facilitate mast cell degranulation, enhance inflammatory cytokine productions and the release of histamine, and increase IgE levels. In addition, S. aureus directly stimulates keratinocytes (KC) and Langerhans cells (LC) to release proinflammatory cytokines, including TH2 cytokines, TSLP, IL-8, and IL-1β, thus inducing TH2 differentiation and inflammation. Together, excessive cutaneous S. aureus colonization promotes AD pathogenesis. Conversely, commensal Coagulase-negative staphylococci (CoNS) inhibit the colonization of S. aureus by producing lantibiotics, PSMγ, and PSMδ. They also inhibit S. aureus biofilm formation by producing the serine protease glutamyl endopeptidase (Esp). Tryptophan metabolites derived from skin microbiota can activate AHR, thus inhibiting TSLP production by KCs and improving the epidermal barrier of the skin. AHR, aryl hydrocarbon receptor; AHRE, AHR element; AMPs, antimicrobial peptides; CoNS, Coagulase-negative staphylococci; IAId, indole-3-aldehyde; IL, interleukin; ILC3, lymphoid cells type 3; KC, keratinocyte; LC, Langerhans cell; PSM, phenol-soluble modulin, TSLP, thymic stromal lymphopoietin; SE, Staphylococcal enterotoxin; TSST-1, toxic shock syndrome toxin-1. Created with BioRender.com (accessed on 4 May 2022).