Abstract
Background:
Chronic nonbacterial osteomyelitis (CNO) is a pediatric autoinflammatory disorder presenting with sterile inflammatory bone lesions. Whole-body MRI (WBMRI) has most recently emerged for disease assessment, but data are limited.
Purpose:
The purpose is to evaluate the imaging findings and patterns of CNO on WBMRI in a series of Greek pediatric patients.
Material and Methods:
Whole-body magnetic resonance imaging studies of all children with documented CNO, performed in a single tertiary center, were retrospectively reviewed. WBMRI included coronal T1 and short-tau inversion recovery (STIR), whole spine sagittal STIR, and ankle/foot sagittal STIR images. High signal intensity lesions on STIR images corresponding to bone marrow edema were recorded. The SPSS v.20 statistical package was used for descriptive statistics.
Results:
Twenty children were included (mean age: 12, range: 6–16 years) with 1–31 lesions (mean: 11.8) on WBMRI. Two children had unifocal disease localized at the clavicle, three paucifocal (1–4 lesions), and 15 multifocal bone involvement. All but two children presented with ankle pain and exhibited lesions at the bones of the ankle joint (90%) followed by the knee (50%) and pelvis (10%). The tibia was the most frequently affected bone (70%) followed by calcaneus (60%), fibula (50%), femur (45%), talus, and metatarsals (45%). No lesions in the cervical, thoracic, lumbar spine, and mandible were documented. Only small sacral lesions were seen in 25% of patients with the extensive peripheral disease. Bilateral metaphyseal and epiphyseal involvement with transphyseal extension were common, but the periosteal reaction and well-defined lesion margins were rare.
Conclusion:
Frequent involvement of the foot and ankle and paucity of substantial spinal involvement were seen in Greek pediatric patients with CNO.
Keywords: chronic nonbacterial osteomyelitis, whole-body magnetic resonance imaging
Introduction
Chronic recurrent multifocal osteomyelitis (CRMO) or chronic nonbacterial osteomyelitis (CNO) is an autoinflammatory disorder primarily affecting the skeletal bones of children and adolescents, with a median age of approximately 10 years, but it can occur in a wide age range even in adults, albeit rarely.1–3 The term autoinflammatory bone disease includes a spectrum of spontaneous activation of the immune system, leading to non-specific inflammatory processes in bones. This disorder is gaining medical momentum in recent years3–5 and is considered the clinical and pathophysiologic counterpart of SAPHO syndrome in adults, 6 while associated with seronegative arthritides.7–9 CNO can affect almost any bone type, most commonly tibial and femoral metaphyses, followed by pelvic bones, spine, and clavicle,8,10–13 and is characterized by spontaneous remissions and exacerbations. Prompt diagnosis obviates unnecessary investigations and averts chronic skeletal pain and possible future complications, such as vertebral fractures and limb length discrepancies. 13
Some years ago, the diagnosis of CNO/CRMO was based on the exclusion of other underlying causes, based on imaging findings and chronic non-specific inflammatory changes on histology.8,13 Most recently, whole-body magnetic resonance imaging (WBMRI) has emerged as the imaging modality of choice, often obviating bone biopsy providing scanning of the whole skeleton within an acceptable examination time and revealing multiple bone lesions14–17 many of them being asymptomatic.5,18
During our clinical practice, we noticed some variations in WBMR imaging patterns of our patients with CNO, all of them being of Greek origin, compared with previous studies, such as paucity of spinal lesions except for the sacrum and involvement of the bones of ankles and feet in even higher frequency than previously described. In this retrospective study, we attempted to evaluate the imaging findings and patterns of CNO on WBMRI in a series of Greek pediatric patients.
Materials and methods
IRB approval information
Approval of the ethics committee was not mandated according to current practice for retrospective studies in our institution when only a secondary review of imaging data is undertaken.
Patient population
We retrospectively reviewed the whole-body MR imaging (WBMRI) studies of all children with a final diagnosis of CNO, addressed to our Radiology Department for a period of approximately 3 years, from September 2018 to June 2021, and attended in a tertiary Pediatric Rheumatology Unit at our institution. All pediatric patients in our study were collected consecutively. Images were retrieved and viewed from the picture archiving and communication system PaxeraHealth’s, Paxera Ultima 360 Enterprise Imaging Suite. The working diagnosis of CNO for all children had been based on “Bristol criteria” which include a combination of typical clinical and MRI findings; bone biopsy and pathologic confirmation were not performed in any patient as considered not necessary to establish the diagnosis (Table 1). 3 All patients included in this study were of Greek origin, as well as first, second, and third generation ancestors, according to the medical records of the Pediatric Rheumatology Unit of our hospital. No patient of non-Greek origin and a final diagnosis of CNO have undertaken a WBMRI study during the same period of time.
Table 1.
“Bristol” criteria for CNO diagnosis (adapted from Ref. 3).
| 1. Typical clinical findings: Bone pain with or without localized swelling Without significant local or systemic symptoms of inflammation or infection |
|---|
| AND |
| 2. Typical radiological findings on X-ray or, preferably, MRI- STIR images: Bone marrow edema with or without bone expansion and periosteal reaction |
| AND |
| 3. Either 3a. > 1 bone lesions without significantly raised CRP (CRP<30 g/L) OR 3b. if unifocal bone disease, other than clavicle, or CRP>30 g/L and inflammatory changes on bone histology without bacterial growth and without receiving antibiotic treatment |
Imaging evaluation—technique
Whole-body MR imaging (WBMRI) was performed in all 20 patients; in 16 of them on a 1.5T MRI scanner (Ingenia Philips, Philips, Best, The Netherlands) using the dStream Whole Body coil system including a head/neck, total spine, and two surface body coils achieving total overage 200 cm and combining 108 channels, whereas four patients were scanned on a 3T MRI scanner (AchievaTx, Philips, Best, The Netherlands) using the Body coil. All patients had been positioned supine with their arms parallel to their bodies. The imaging protocol included multi-station coronal T1 turbo spin-echo (TSE) [for the 1.5T scanner: repetition time (TR) = 510–580 ms, time echo (TE) = 11 ms, matrix size = 800 x 800, slice thickness = 4 mm; for the 3.0T scanner: TR = 500–600 ms, TE = 10 ms, matrix size = 480 x 480, slice thickness = 4 mm] and multi-station coronal T2 short-tau inversion recovery (STIR) [for the 1.5T scanner: TR = 3500–3900 ms, TE = 90 ms, inversion time (TI) = 135 ms, matrix size = 864 x 864, slice thickness = 4 mm; for 3.0T scanner: TR = 3700–4000 ms, TE = 80 ms, inversion time (TI) = 200 ms, matrix size = 512 x 512, slice thickness = 4 mm] sequences. Additionally, total spine images were acquired: sagittal T2 STIR images [ for 1.5T scanner: TR = 2500 ms, TE = 60 ms, TI = 170 ms, matrix size = 480 x 480, slice thickness = 4 mm; for 3.0T scanner: TR = 3600 ms, TE = 60 ms, TI = 190 ms, matrix size = 512 x 512, slice thickness = 4 mm]; as well as sagittal fat-suppressed T2 weighted images to image ankle joint up to forefoot [for 1.5T scanner: (T2w STIR) TR = 2400 ms, TE = 50 ms, TI = 160 ms, matrix size = 320 x 320, slice thickness = 4 mm; for 3.0T scanner: T2w with spectral adiabatic inversion recovery pulse fat suppression(SPAIR): TR = 3000 ms, TE = 80 ms, TI = 140 ms, matrix size = 720 x 720, slice thickness = 4 mm]. A total of 6 stations were required for whole-body imaging for each patient. Total scanning time ranged between 40 and 50 min, depending upon the height and compliance of each patient. WBMRI was well tolerated by all patients and sedation was deemed unnecessary.
Imaging evaluation—review
All studies were reviewed by a panel of three radiologists: one musculoskeletal and two pediatric radiologists with 18, 24, and 3 years of experience in pediatric musculoskeletal imaging. The agreement of at least two members of the panel was necessary to decide on the presence of a lesion.16,17 The time elapsed from the original WBMRI interpretation was at least 2 months.
Imaging evaluation -criteria
We recorded lesions of high signal intensity on STIR sequences corresponding to bone marrow edema and, also, the location of long bone lesions at epiphysis, metaphysis, and diaphysis as defined by Fritz et al. 15 and the presence of clavicular and spinal lesions. Particularly for the assessment of feet, in order to differentiate between expected for age red marrow and bone marrow edema lesions, we arbitrarily considered plantar vein signal intensity on STIR images as internal standard, whereas the age of the patients, the size, and the location of the hyperintense area, that is, less frequent red marrow from hindfoot to forefoot, were taken into consideration. 19 The phalanges of hands and feet were not consistently visualized so they were excluded from the evaluation. We also considered the presence or not of periosteal reaction and of well-delineated or hazy margins of the lesion.
Statistical analysis
We created a data base in which we recorded the lesion distribution for each patient. Then we calculated the lesion percentage frequency for each anatomical location in our CNO patient sample and they were graphically represented using SPSS version 20. We also performed a one sample chi-square test to estimate the patterns’ distribution. Statistical analysis was conducted with SPSS version 20.
Results
Patient information
Our study group comprised of 20 patients, eleven males and nine females, aged from 6 to 16 years (mean: 12 ± 3.22 years), with a final diagnosis of CNO, based on the Bristol criteria (Table 1) and WBMRI findings. The most frequent indication for referral to the pediatric rheumatologist unit and then for imaging was lower extremities dolor, most commonly at ankles/feet. One child had psoriatic skin lesions. Only initial WBMRI studies have been selected although most of the patients have been under follow-up during these years.
Imaging findings
Lesion distribution/patterns
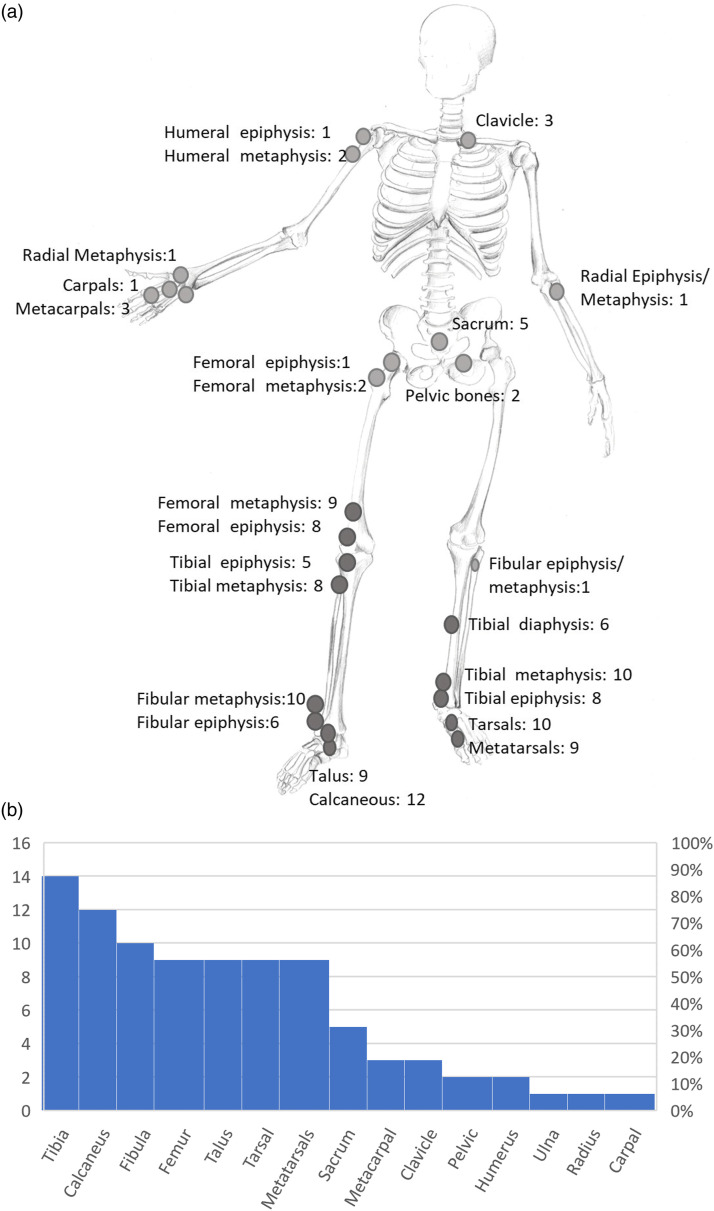
Figure 1 and Table 2 present the distribution of CNO lesions in the skeleton. A total of 236 lesions were recorded, ranging from 1 to 31 per patient (mean: 11.8 ± 9.06 SD). Unifocal involvement was found in two female patients (10% of the patients) with clavicular involvement, paucifocal (1–4 lesions) in three male patients (15% of the patients) with lower extremity involvement, and multifocal in the remaining 15 patients (9 males and 6 females; 75% of the patients).
Figure 1.
(a): Distribution of bone lesions in skeleton and number of patients with CNO lesions at a bone site. (b): Lesion percentage frequency across CNO patients.
Table 2.
Number of patients (PTS No) with at least 1 lesion at bone type (ABT), distribution of lesions at proximal and distal metaphyses, and number of patients with bilateral and transphyseal involvement at bone type (ABT).
| Affected bone type | PTS no, at least 1 lesion/ABT | PTS no, bilateral lesions/ABT | PTS no proximal metaphysis | PTS no. proximal epiphysis | PTS no, distal metaphysis | PTS no, distal epiphysis | PTS no, transphyseal extension ABT | Pts no, diaphysis |
|---|---|---|---|---|---|---|---|---|
| Pelvic bones | 2 | 2 | 2 | |||||
| Femur | 9 | 5 | 2 | 1 | 9 | 8 | 4 | — |
| Tibia | 14 | 10 | 8 | 5 | 10 | 8 | 6 | 6 |
| Fibula | 10 | 4 | 1 | 1 | 10 | 6 | 5 | — |
| Talus | 9 | 6 | ||||||
| Calcaneus | 12 | 9 | ||||||
| Tarsal bones | 10 | 6 | ||||||
| Metatarsals | 9 | 7 | ||||||
| Humerus | 2 | 1 | 2 | 1 | — | — | 1 | |
| Ulna | 1 | 1 | 1 | 1 | 1 | |||
| Radius | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Carpal bones | 1 | 1 | ||||||
| Metacarpals | 3 | 2 | ||||||
| Clavicle | 3 | — | ||||||
| Sacrum | 5 | — | ||||||
| Spine except sacrum | ||||||||
| Mandible, Ribs, sternum, and scapula |
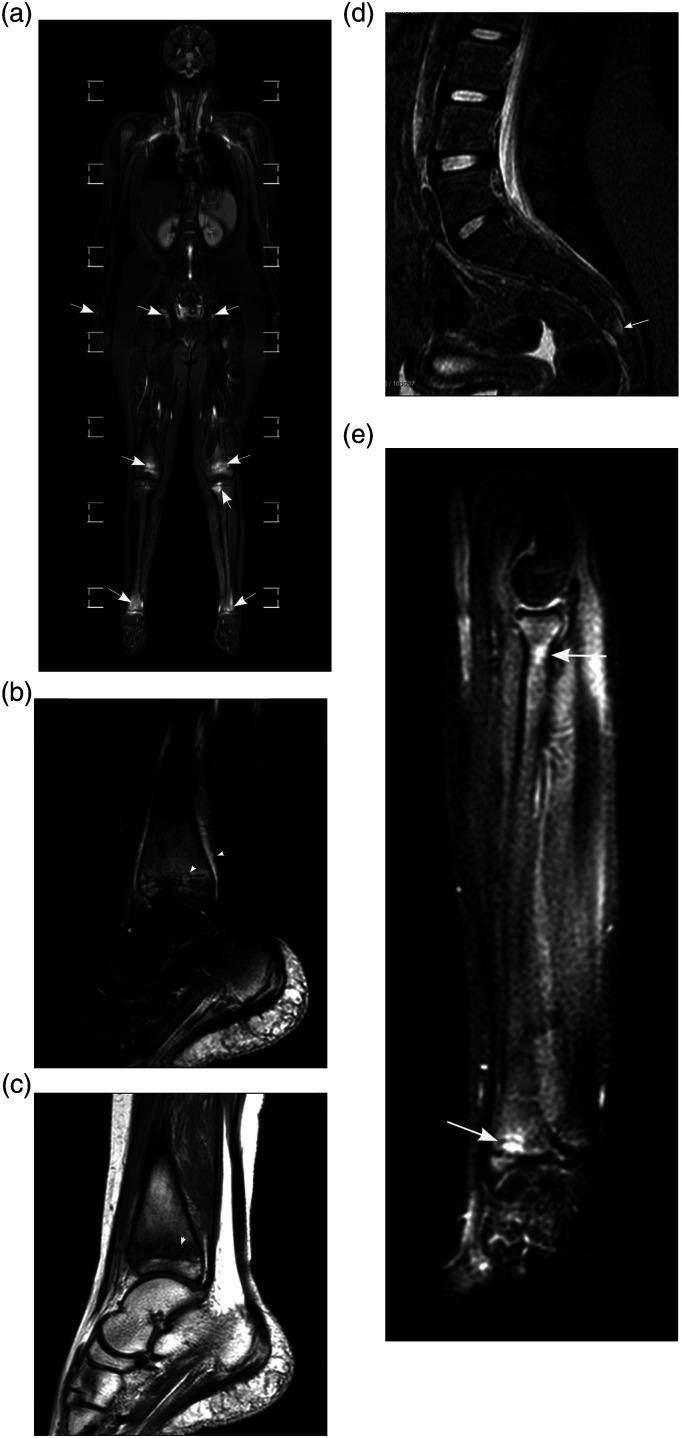
The vast majority of the lesions were noted in the bones of the ankle joint (at least one bone at one site in 90% of the patients) followed by the foot (65%) and the knee (60%), whereas the hips, the wrist, and elbows were significantly less affected (20%, 10%, and 5%, respectively). The tibia was the most frequent site of lesions as at least one tibial lesion was observed in 14 (70%) of the patients, more frequently the distal tibia, followed by the calcaneus (60%), fibula (50%), femur, talus, and metatarsals (45%, respectively, Table 2, Figure 1(b)). Upper extremity involvement, at least in one bone, was observed only in 3 (15%) patients in total, and sacral involvement in 5 (25%) all of them with extensive disease at the lower extremities (Figure 2). On the other hand, clavicle was affected in three patients (15%), but in two of them, clavicle was the only site of the disease. Noteworthy, none of the patients exhibited any lesion at the thoracic, lumbar or cervical spine, sternum, ribs, and mandible, whereas spinal involvement was limited to solitary sacral lesions, all of them <20 mm in diameter (Figure 2(d). Transphyseal extension was common, especially in distal tibial and distal femoral lesions (Table 2, Figure 2(b) and (c)) (Figure 3).
Figure 2.
12-year-old girl with pain at the ankle joints and knees. (a) A coronal WBMRI “stitched” image allows fast inspection of the skeleton and shows unilateral involvement of the left proximal femoral metaphysis, bilateral involvement of the distal femurs, proximal and distal tibias and acetabuli as well as of the right distal radius (arrows). (b, c) A sagittal SPAIR (B) and a sagittal T1W (C) image of the right ankle and foot exhibit transphyseal involvement of the distal tibia. Metaphyseal lesions close to physis show well-defined margins (arrowheads) whereas the upper border of the physis is indistinct on T1W images (C). There is mild ancillary periosteal reaction at the distal tibia (B, arrow). (d) A coronal STIR image denotes a small area of bone marrow edema in S4 vertebra (arrow) that was not evident on coronal images. (e) A STIR image of the right forearm shows bone marrow edema at the proximal radius and a hyperintense lesion with hypointense margin at the distal radial metaphysis adjacent to the physis. Positioning of the forearm at the side is suboptimal, so does visualization of the right hand and wrist. Placement of hands under the buttocks should be preferable.
Figure 3.
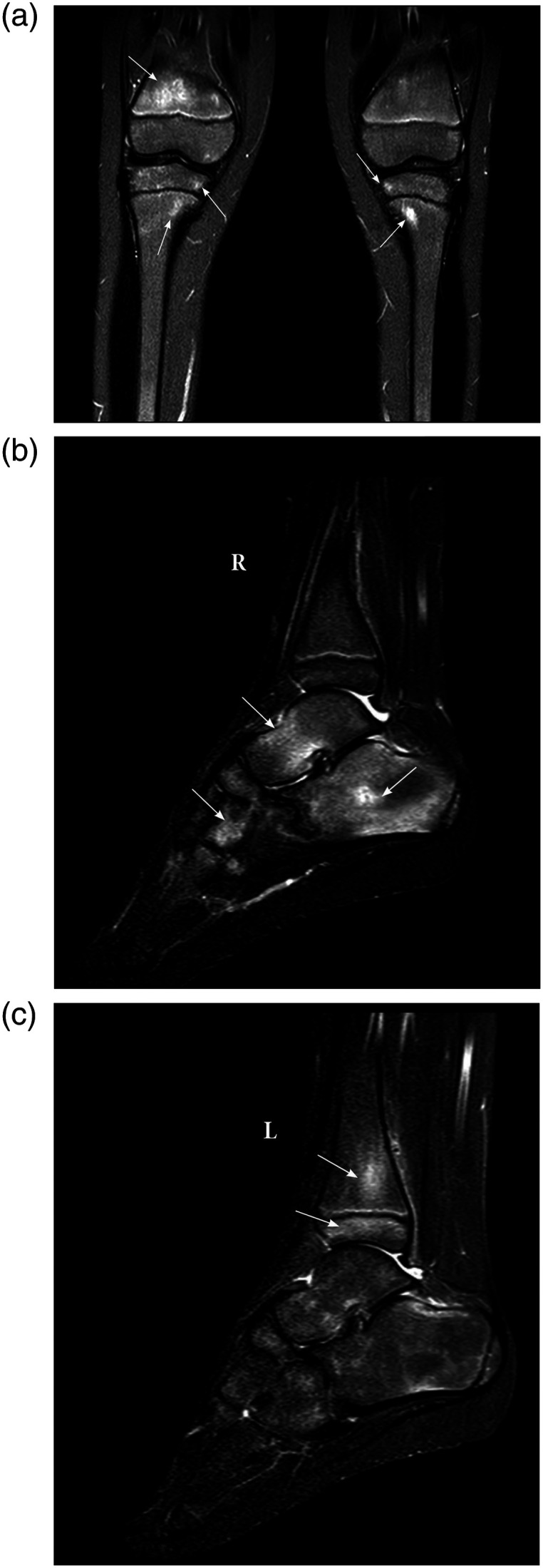
6-year-old girl with pain at ankle joints. (a) A coronal STIR image demonstrates unilateral involvement of the right distal femoral metaphysis and foci of hyperintense signal on tibial metaphyses and epiphyses bilaterally. All visualized physes of this patient remained intact. (b, c) Sagittal STIR images of the right (b) and left ankle/foot (c) denote bone marrow edema occupying most of the right calcaneus, the body of the right talus and the right lateral cuneiform (arrows). Few slightly hyperintense foci at the left calcaneus, talus and tarsal bones were considered as expected for age and were not recorded as CNO lesions. Moreover, there is unilateral involvement of the left distal tibia (arrows), more extensive in epiphysis than in the ipsilateral metaphysis that is rather unusual.
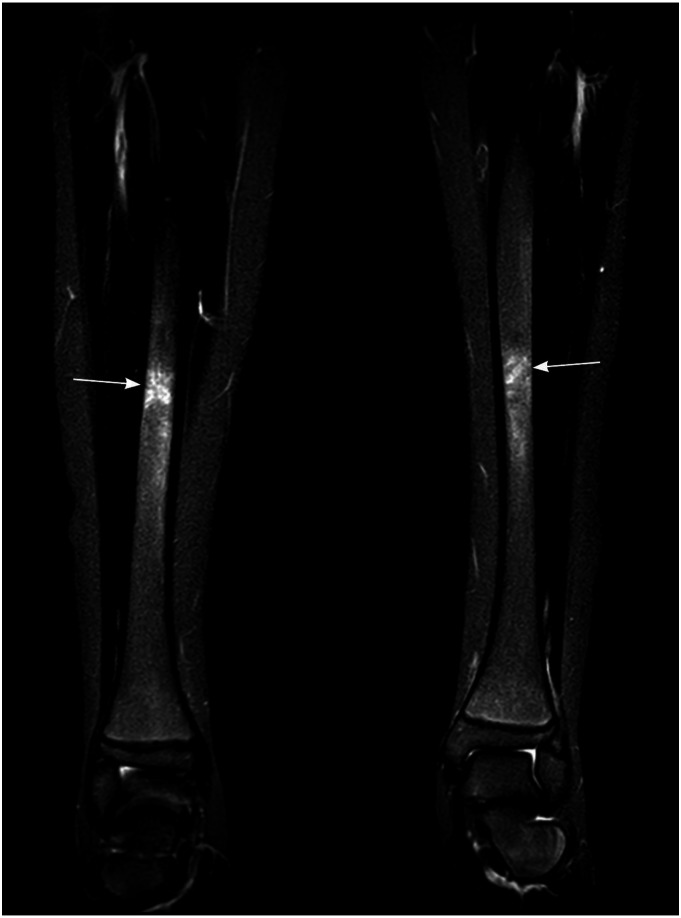
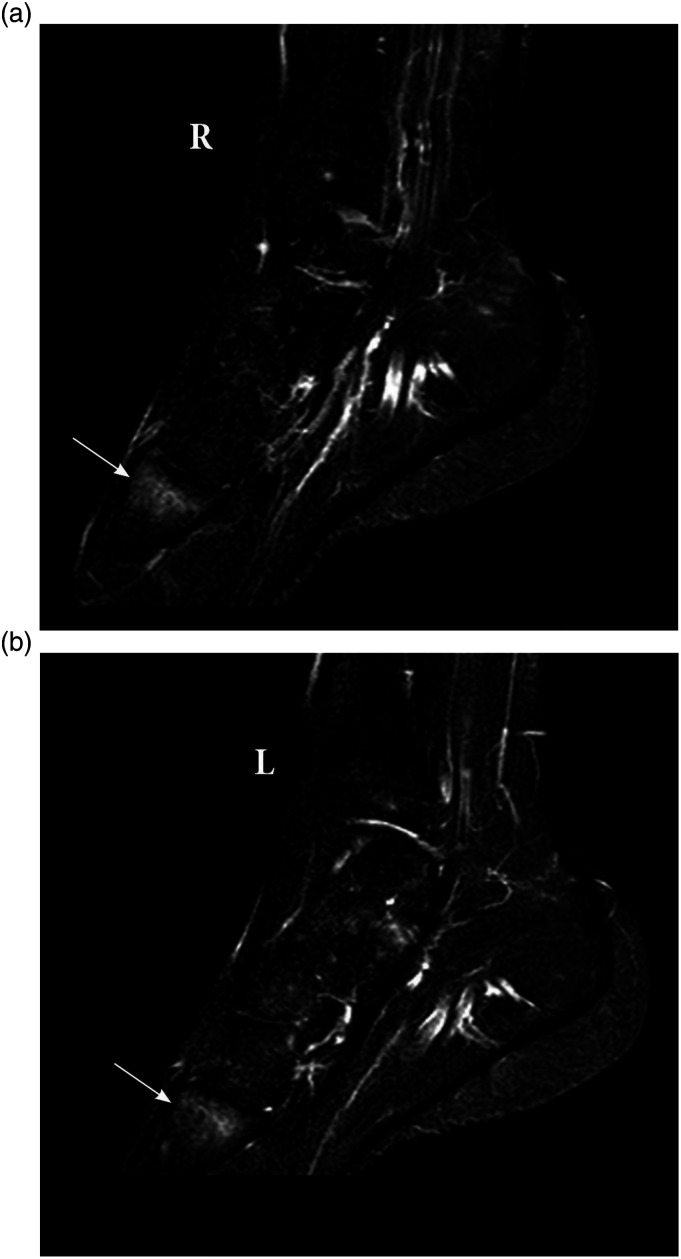
The most frequent bone types showing bilateral involvement were the distal tibia, followed by the talus, the calcaneus, distal femur, metatarsals, and tibial diaphysis (Figure 4). Among metatarsals, the most frequently affected was the first (in 6/9 patients); 5 patients showed bilateral metatarsal involvement with at least one same metatarsal involved in both the right and left side (Figure 5). The majority of bilateral lesions in skeleton were also symmetrical (86%).
Figure 4.
Coronal STIR image of the calves, in a 12-year-old boy, demonstrates hyperintense areas with indistinct borders at tibial diaphyses bilaterally (arrows).
Figure 5.
(a, b) Sagittal STIR images of the right (a) and left (b) ankle/foot in a 15-year-old boy with bilateral foot pain, show bilateral and symmetrical involvement of the base of the first metatarsal.
In view of our findings, we classified our patients into three distribution patterns, sharing similarities to the classification by Andronikou et al. 16 : (I) the central pattern, comprising the midline bone structures, that is, spine and thoracic cage, (II) the peripheral, comprising limbs and pelvis, and (III) the mixed pattern, including both axial and peripheral skeleton. The three patterns were not equally distributed [x2(2) = 9.7, p = 0.008]. The peripheral pattern was significantly the most common (65% of the total patients) compared to the mixed and central pattern (25% and 10%, respectively, of the total patients).
Lesion morphology/ancillary findings
Periosteal reaction was recorded in only 4 lesions and was seen in fibula (Figure 6), metatarsals (i.e., small tubular bones), clavicle, and tibia (Figure 2(b)), respectively. Most of the lesions exhibited hazy margins, whereas well-defined margins were observed in 17 (<1%) of the lesions (Figure 2(b) and (e)). We did not find any sclerotic/non-active lesions, which were expected to be hypointense on both T1 and STIR images. Mild joint effusion was seen in 5 patients (25%), with nearby bones were affected (three ankles, one hip, and one knee joint).
Figure 6.
Coronal STIR image of an 8-year-old boy demonstrates hyperintense and expanded distal fibular metaphysis with periosteal reaction (arrow) and involvement of the adjacent physis and epiphysis.
Discussion
Our study group, with all patients of Greek origin, presented some discrepancies from previous studies, the most striking being the lack of any lesion in the cervical, thoracic, lumbar spine, chest wall, or mandible, although whole spine sagittal and coronal images were acquired.12,14,17 Spine, mostly the thoracic spine, was affected in 19 to 36% in the previous series.12,18,20–25 We noticed only subtle sacral lesions in one-fourth of the patients all of them presenting with very extensive peripheral involvement, in contrast to Andronikou et al., who reported a claviculo-spinal pattern—without significant peripheral involvement—in 24% of their patients. 16 We, also, recorded a slightly higher frequency of foot involvement. We found an even higher predominance of bones of the ankle joint and foot which were affected in all but two patients (90%) followed by bones of the knee (60%) and hip joint (20%).
To our opinion, this discrepancy may be due to three factors: differences in interpretation of normal high signal areas on STIR images in hindfoot and midfoot, variations in WBMRI technique, and probable ethnicity-related phenotypic differences. Sozeri et al. claimed that probable genetic differences in different ethnic groups may account for variations in clinical phenotype and response to treatment. 24 Previous cohorts of CNO patients hardly include any patients of Greek origin. Different clinical phenotypes related to various ethnicities might be further explored using as a benchmark WBMRI acquired with the same technique and interpretation principles.
Hyperintense solitary or confluent foci are a common finding in hindfoot and midfoot of children; these areas are usually symmetric and disappear after the age of fifteen. 19 There are no established standards to discriminate between normally expected and abnormally increased bone marrow signals in different age groups12,26; we considered hyperintense areas of the foot as pathologic when there was an association with clinical findings, had considerable size, were isointense to foot veins, and were not limited only in expected for age positions for each bone as reported by Shabshin et al. 19
Distal tibial metaphyses or distal femoral metaphyses, most often with transphyseal extension, were the most frequently affected sites in all cohorts, followed by pelvic bones, spine, and clavicle.10,12,14–18,20–25 Bhat et al. found distal tibia as the most frequent site of disease, affecting 49.6% of their patients in a large series of 122 CNO patients with WBMRI, 24 while D’Angelo et al. reported femur and tibia as the most frequently affected sites (61.3% and 64.5%, respectively) followed by pelvis and spine in a series of 75 children. 12
Andronikou et al., in a cohort of 37 patients in the United Kingdom, described three phenotypic patterns: a tibio-appendicular multifocal pattern without clavicle involvement, that was seen in more than half of their patients, a claviculo-spinal paucifocal pattern without tibial involvement comprising one-fourth of their patients and a tibia—clavicular cross over pattern that was a combination of tibial and clavicular involvement and comprised about 15% of their patients. 16 We noticed similar patterns denoting a peripheral pattern comprising the majority of our patients, a central pattern that included only the two patients with unifocal clavicular involvement, and a mixed pattern encompassing bones of both the axial and peripheral skeleton. We classified the patients with peripheral and sacral lesions into a mixed pattern, although sacral involvement was very limited and peripheral lesions predominated.
We found epiphyseal involvement common but rarely exclusive in accordance with previous studies,12,14,16 whereas diaphyseal involvement was seen only at tibias. Periosteal reaction without mass effect has been considered part of the CNO spectrum14–16; however, we observed periosteal reaction rarely, in accordance with D' Angelo et al. 12 Well-defined margins were also uncommon, whereas we did not encounter any chronic/non-active lesions in the context of hypointensity on both T1 and STIR images over the entire lesion. 14
One-fifth of preteens and teenagers have been experiencing non-specific musculoskeletal pain not associated with trauma, presumably, a considerable number of these cases may be due to CNO whose real incidence has been underestimated for a long time.27,28 The term “CRMO” (chronic recurrent multifocal osteomyelitis) has been alternatively used whereas the currently preferred “CNO” is an umbrella term encompassing both focal and multifocal disease while denoting the inflammatory but nonbacterial background of the disease. 11 The disease usually presents with insidious and non-specific symptoms, while inflammatory markers are often raised3,10,20,21,29 and usually associated with the severity of the disease. 12 Treatment includes nonsteroidal anti-inflammatory drugs as first-line medication, with methotrexate, TNF inhibitors, and bisphosphonates as second-line treatment.7,11
In recent years, WBMRI has emerged as a pivotal diagnostic tool in establishing the diagnosis of CNO by documenting the multifocality of the disease, the location, symmetry, and size of bone marrow lesions12,14–18 and therefore the total inflammatory burden. 10 WBMRI is more sensitive than radiography and scintigraphy and lacks ionizing radiation whereas stitching of images provides a fast overall inspection of the skeleton.2,15,20–22 WBMRI technique is based on a water-sensitive sequence, which is usually a short-tau inversion recovery (STIR) sequence in most studies.30–32 The application of the T1 sequence remains controversial 31 ; we applied the T1 sequence, at the expense of time, for differential diagnostic purposes, that is, to be able to distinguish bone marrow edema from normal erythropoietic marrow 32 and replacement disorders17,33 and, also, to assess the chronicity of the lesions. 14 Diffusion-weighted imaging (DWI) could theoretically be more sensitive in revealing additional bone marrow lesions but, so far, it does not seem to outbalance the standard STIR sequence.2,34 Homogeneity of WBMRI technique and reporting among radiologists would ensure comparability between studies, whereas standardization of MR imaging interpretation of the normal pediatric skeleton is warranted 26 in order to discriminate between abnormal and expected age and location MR signal.
Limitations of our study include its retrospective nature, the limited number of patients, and the lack of sufficient clinical and laboratory data to correlate with imaging findings. We are currently underway a longitudinal study to identify clinical phenotypes in Greek patients based on clinical, laboratory, and imaging findings. Interobserver agreement was not explored; since the three reviewers were aware of the imaging findings, so we considered that repeat reviews by the same reviewers should be biased, and estimation of interobserver agreement (kappa) would not be accurate.
In conclusion, in our study group of pediatric patients of Greek origin, there was the absence of substantial spinal involvement, whereas the involvement of the lower extremities particularly bones around the ankle joint predominated in even higher frequencies compared to previous cohorts.
Acknowledgments
The authors would like to thank Mrs Dimitra Labretsa, medical artist, for her contribution in drawing the skeleton in Figure 1.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Olympia Papakonstantinou https://orcid.org/0000-0003-0331-207X
Spyridon Prountzos https://orcid.org/0000-0001-9651-8338
References
- 1.Buch K, Thuesen AKB, Brøns C, et al. Chronic non-bacterial osteomyelitis: a review. Calcif Tissue Int 2019;104:544-553. [DOI] [PubMed] [Google Scholar]
- 2.Andronikou S, Kraft JK, Offiah AC, et al. Whole-body MRI in the diagnosis of paediatric CNO/CRMO. Rheumatology (Oxford) 2020;59:2671-2680. [DOI] [PubMed] [Google Scholar]
- 3.Roderick MR, Shah R, Rogers VA. et al. Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis. Pediatr Rheumatol 2016;14:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hedrich CM, Morbach H, Reiser C, et al. New insights into adult and paediatric chronic non-bacterial osteomyelitis CNO. Curr Rheumatol Rep 2020;22:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schaal MC, Gendler L, Ammann B, et al. Imaging in non-bacterial osteomyelitis in children and adolescents: diagnosis, differential diagnosis and follow-up: an educational review based on a literature survey and own clinical experiences. Insights Imaging 2021;12:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jurik AG, Klicman RF, Robinson P, et al. SAPHO and CRMO: the value of imaging. Semin Musculoskelet Radiol 2018;22:207-224. [DOI] [PubMed] [Google Scholar]
- 7.Moreno-Mateo F, Perea SH, Onel KB. Chronic recurrent multifocal osteomyelitis: diagnosis and treatment. Curr Opin Pediatr 2021;33:90-96. [DOI] [PubMed] [Google Scholar]
- 8.Roderick MR, Sen ES, Ramanan AV. Chronic recurrent multifocal osteomyelitis in children and adults: current understanding and areas of development. Rheumatology (Oxford) 2018;57:41-48. [DOI] [PubMed] [Google Scholar]
- 9.Schiettecatte E, Jans L, Jaremko JL, et al. MR imaging of rheumatic diseases affecting the pediatric population. Semin Musculoskelet Radiol 2021;25:082-093. [DOI] [PubMed] [Google Scholar]
- 10.Zhao Y, Chauvin NA, Jaramillo D, et al. Aggressive therapy reduces disease activity without skeletal damage progression in chronic nonbacterial osteomyelitis. J Rheumatol 2015;42:1245-1251. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Y, Ferguson PJ. Chronic nonbacterial osteomyelitis and chronic recurrent multifocal osteomyelitis in children. Pediatr Clin N Am 2018;65:783-800. [DOI] [PubMed] [Google Scholar]
- 12.D’ Angelo P, Tanturri de Horatio L, Toma P, et al. Chronic nonbacterial osteomyelitis — clinical and magnetic resonance imaging features. Pediatr Radiol 2021;51:282-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khanna G, Sato TSP, Ferguson P. Imaging of chronic recurrent multifocal osteomyelitis. RadioGraphics 2009;29:1159-1177. [DOI] [PubMed] [Google Scholar]
- 14.Arnoldi AP, Schlett CL, Douis H, et al. Whole-body MRI in patients with non-bacterial Osteitis: radiological findings and correlation with clinical data. Eur Radiol 2017;27:2391-2399. [DOI] [PubMed] [Google Scholar]
- 15.Fritz J, Tzaribatchev N, Claussen CD, et al. Chronic recurrent multifocal osteomyelitis: comparison of whole-body MR imaging with radiography and correlation with clinical and laboratory data. Radiology 2009;252:842-851. [DOI] [PubMed] [Google Scholar]
- 16.Andronikou S, Mendes da Costa T, Hussien M, et al. Radiological diagnosis of chronic recurrent multifocal osteomyelitis using whole-body MRI-based lesion distribution patterns. Clin Radiol 2019;74:737-737.e15. [DOI] [PubMed] [Google Scholar]
- 17.Sato TS, Watal P, Ferguson PJ. Imaging mimics of chronic recurrent multifocal osteomyelitis: avoiding pitfalls in a diagnosis of exclusion. Pediatr Radiol 2020;50:124-136. [DOI] [PubMed] [Google Scholar]
- 18.Von Kalle T, Heim N, Hospach T, et al. Typical patterns of bone involvement in Whole-Body MRI of patients with chronic recurrent multifocal osteomyelitis (CRMO). Rofo 2013;185:655-661. [DOI] [PubMed] [Google Scholar]
- 19.Shabshin N, Schweitzer ME, Morrison WB, et al. High-signal T2 changes of the bone marrow of the foot and ankle in children: red marrow or traumatic changes? Pediatr Radiol 2006;36:670-676. [DOI] [PubMed] [Google Scholar]
- 20.Wipff J, Constantino F, Lemelle I, et al. A large national cohort of french patients with chronic recurrent multifocal osteomyelitis. Arthritis Rheumatol 2015;67:1128-1137. [DOI] [PubMed] [Google Scholar]
- 21.Girschick H, Finetti M, Orlando F, et al. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Rheumatology 2018;57:1203-1211. [DOI] [PubMed] [Google Scholar]
- 22.Falip C, Alison M, Boutry N, et al. Chronic recurrent multifocal osteomyelitis (CRMO): a longitudinal case series review. Pediatr Radiol 2013;43:355-375. [DOI] [PubMed] [Google Scholar]
- 23.Bhat CS, Anderson C, Harbinson A, et al. Chronic non-bacterial osteitis- a multicenter study. Pediatr Rheumatol 2018;16:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sözeri B, Ayaz NA, Atıkan BY, et al. Clinical experiences in turkish paediatric patients with chronic recurrent multifocal osteomyelitis. Turk J Pediatr 2019;61:879-884. [DOI] [PubMed] [Google Scholar]
- 25.Concha S, Hernández-Ojeda A, Contreras O, et al. Chronic nonbacterial osteomyelitis in children: a multicenter case series. Rheumatol Int 2020;40:115-120. [DOI] [PubMed] [Google Scholar]
- 26.Zadig P, von Brandis E, Lein RK, et al. Whole-body magnetic resonance imaging in children – how and why? A systematic review. Pediatr Radiol 2021;51:14-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Voit A, Arnoldi AP, Douis H, et al. Whole-body magnetic resonance imaging in chronic recurrent multifocal osteomyelitis: clinical longterm assessment may underestimate activity. J Rheumatol 2015;42:1455-1462. [DOI] [PubMed] [Google Scholar]
- 28.Schnabel A, Range U, Hahn G, et al. Unexpectedly high indices of chronic non-bacterial osteomyelitis in children. Rheumatol Int 2016;36: 1737-1745. [DOI] [PubMed] [Google Scholar]
- 29.Hofmann SR, Kapplusch F, Mabert K, et al. The molecular pathophysiology of chronic nonbacterial osteomyelitis (CNO): a systematic review. Mol Cell Pediatr 2017;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greer MLC. Whole-body magnetic resonance imaging: techniques and non-oncologic indications. Pediatr Radiol 2018;48:1348-1363. [DOI] [PubMed] [Google Scholar]
- 31.Merlini L, Carpentier M, Ferrey S, et al. Whole-body MRI in children: would a 3D STIR sequence alone be sufficient for investigating common paediatric conditions? A comparative study. Eur J Radiol 2017;88:155-162. [DOI] [PubMed] [Google Scholar]
- 32.Chan BY, Gill KG, Rebsamen SL, et al. MR imaging of pediatric bone marrow. RadioGraphics 2016;36:1911-1930. [DOI] [PubMed] [Google Scholar]
- 33.Menashe SJ, Aboughalia H, Zhao Y, et al. The many faces of pediatric chronic recurrent multifocal osteomyelitis (CRMO): A practical location and case-based approach to differentiate CRMO from its mimics. J Magn Reson Imaging 2021;54:391-400. [DOI] [PubMed] [Google Scholar]
- 34.Leclair N, Thörmer G, Sorge I, et al. Whole-Body diffusion-weighted Imaging in chronic recurrent multifocal osteomyelitis in children. PLoS One 2016;11:e0147523. [DOI] [PMC free article] [PubMed] [Google Scholar]