Abstract
Objective:
To study the utilization of emergency room (ER) services for health complaints of the musculoskeletal (MSK) system in older men and women.
Methods:
Data from all medical encounters at the ER of a teaching hospital for calendar years 2016–2020 were extracted from an electronic database. MSK encounters were defined as those with ICD-10-CM M and S codes in the primary diagnosis field of the database. Frequency distributions were calculated by year, sex, and age group for MSK and all encounters. The most frequent codes used by sex and age groups were assessed.
Results:
The number of unique patients with medical encounters at the ER during the five-year period was 94,346. There was a total of 220,153 encounters (median:1 encounter per patient; interquartile range:1–3). A 33.2% reduction in the number of encounters occurred in 2020 compared to 2019. The total number of unique patients in the 60 yr. and older group was 24,412 (25.9% of all unique patients). The total number of encounters in the group 60 yr. and older was 56,294 (25.6% of all encounters). Women accounted for 31,488 (56%) encounters in this age group. A total of 12,744 encounters (22.6%) in older adults involved the MSK system and this proportion decreased with increasing age. The most common MSK conditions included low back pain, pain in joints, and femoral fractures.
Conclusion:
Older adults with MSK health conditions represent a substantial portion of ER patients. Many MSK health conditions could be evaluated and treated in other health care settings.
Introduction:
A landmark report published by the World Health Organization (WHO) in 2015 (1) showed that the number of both men and women older than 60 yr. has increased in most countries. Furthermore, the WHO projected that, by the year 2050, many countries will have more than 30% of their population in this age group (1). In Puerto Rico (PR), although the absolute number of people older than 60 yr. will decrease from 909,934 to 860,823 in the same time period, a decline in the total population will translate into an increase in the proportion of the population in this age group from 28.5% in 2020 to 39.8% in 2050 (2). Partly because of the significant socioeconomic implications of these demographic changes, the WHO and the United Nations General Assembly have recently declared 2021–2030, the Decade of Healthy Ageing (3).
Health complaints of the musculoskeletal (MSK) system are major contributors to the high prevalence of disability and the need for rehabilitation in older populations (4). In addition, MSK disorders result in loss of mobility and independence, reduced quality of life, and increased mortality in older adults (5). Additionally, MSK pain is an important risk factor for falls in this age group (6). People with MSK complaints can receive care in multiple health care settings such as hospitals and ambulatory clinics. Because many MSK complaints are caused by trauma and acute pain is a common presenting symptom, older patients may present frequently to the emergency room (ER) for care. For example, a study of Medicare enrollees in the United States showed that injury or MSK complaints accounted for 31.4% of the diagnoses in older patients discharged from an ER (7). A retrospective study of the utilization of ER’s in the state of California from 2005 to 2015 showed an increase in the number of visits in adults older than 65 yr., with both MSK disorders and injuries (8). An increased utilization of ER services by older adults has also been reported in other countries (9, 10) including a five-year study in Iceland (11) where the most common causes of visits to the ER in this age group were MSK disorders. Increased utilization with age is particularly true for those aged 80 years and over and, in one study, they accounted for 15% of all visits to the ER and 32% of persons in this age group required ER services during the course of one year (12). After an ER encounter, many of these patients can be referred to clinics where exercise counseling is incorporated in a rehabilitation plan, an intervention that is known to have positive public health implications.
To our knowledge, the prevalence of MSK complaints in an older Hispanic population presenting to an ER has not been reported. Thus, our main purpose was to study the frequency and type of MSK complaints in Hispanic older individuals evaluated in an ER. We hypothesized that 1) older men and women account for a large proportion of patients and encounters in an ER, 2) most older people presenting to the ER are female, 3) many older adults visit an ER due to MSK-related complaints, and 4) the types of MSK health complaints differ among age sub-groups of older adults.
Methods and Materials:
This study is part of a larger research project (described briefly below) looking at the encounters in the ER of a major teaching hospital of the University of PR (13). In this report, we present an analysis of encounters due to musculoskeletal complaints in adult men and women 60 yr. or older.
Setting
As previously reported (13), the present study was conducted at Dr. Federico Trilla Hospital in Carolina, PR, with the approval of the Institutional Review Board. The hospital is a secondary level teaching institution associated with the University of PR, and is the primary training site for a residency training program in Emergency Medicine. The ER is staffed by 13 board-certified emergency medicine physicans and 30 residents. It has 42 acute care beds and 8 fast-track exam areas and offers a wide variety of services including bedside ultrasonography. The hospital has 234 staffed acute beds and provides care to the northeast region of the island with an estimated catchment area of 311,355 inhabitants in the neighboring towns (14). Adults 60 yr. or older represent 27.6% of the inhabitants in the region. The hospital offers comprehensive MSK care (physical medicine and rehabilitation, orthopedic surgery, and physical therapy) and radiological services for both sexes and all age groups.
Study design, data source, and collection
We conducted a retrospective analysis of administrative data from all encounters in the ER between January 1, 2016 and December 31, 2020. For the purpose of this report, we focused on data from medical encounters of patients 60 yr. and older. A unique patient was defined as a patient that had at least one ER encounter during the study period. An encounter was defined as a visit to the ER that resulted in the registration of a code in the administrative database. Data for each encounter were extracted from the ER’s electronic medical record system including date of the encounter, age and sex of the patient, as well as the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) code (15, 16). For patients with more than one encounter during the study period, age and sex assigned at their first encounter was used.
ICD-10-CM codes
We determined the frequency of all codes in the primary diagnosis field/column of the database from all encounters and all age groups. In addition, we calculated the frequency of all M (MSK system and connective tissue) or S (injury or certain other consequences of external causes) codes. M and S codes used in the secondary diagnoses field/column of the database (present in 8.1% of encounters) were not included in the analysis.
Statistical analysis
The number of total encounters per month was calculated for each year to explore seasonal variations. Medians and interquartile ranges (IQR’s) were used to describe age distributions and of encounters per patient. The Wilcoxon-Mann-Whitney test was used to statistically assess group differences in these distributions (17). Percents were used to describe categorical variables, including distributions by sex and code groups. The chi-square test and the chi-square test for linear trend were used to test differences and trends in proportions, respectively (18). Data management and statistical analysis were performed with R version 4.0.2 (19), RStudio version 1.3.1093 (20), and R Commander Version 2.7–0 (21).
Results:
All encounters, all age groups
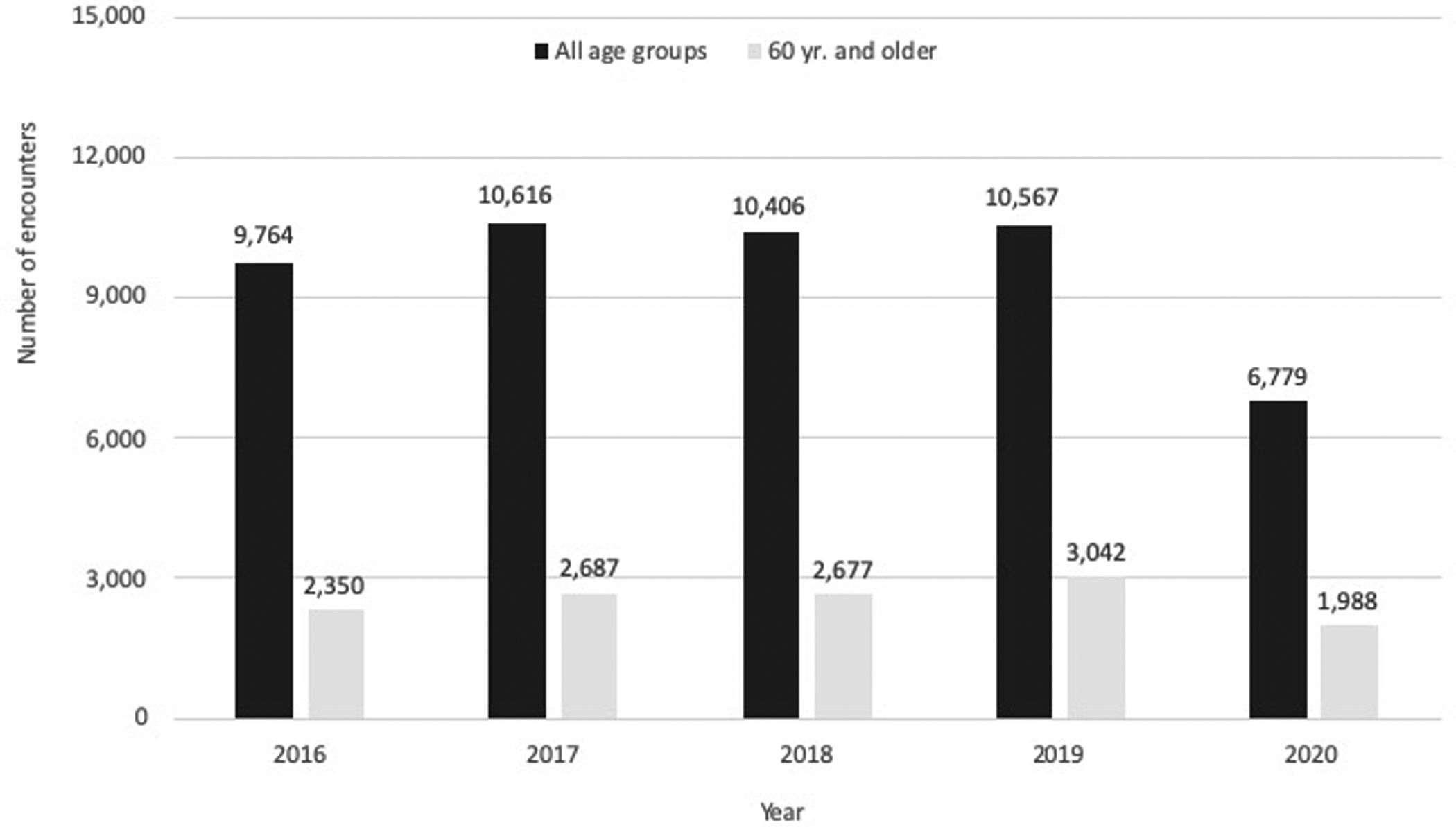
The total number of unique patients during the five year period was 94,346 and the total number of encounters was 220,153. Most unique patients were female (51,109; 54.2%; p < 0.0001). The median number of encounters per patient was 1 (IQR: 1 – 3). The distribution of total encounters per year is presented in Figure 1. There was a 33.2% reduction in the number of encounters in the year 2020 in comparison to the prior year starting during the month of March, and it was observed in both sexes and all age groups. The median age for all encounters was 39 years (IQR: 23 – 60) with a median of 38 for females (IQR: 23 – 59) and 42 for males (IQR: 22 – 61) (p < 0.0001). Females accounted for a majority of encounters (127,302; 57.9%; p < 0.0001). This proportion was similar for each of the five years (range: 57.0% - 59.0%). When considering the total number of encounters (all age groups, both sexes) the top five ICD-10 code categories were MSK codes (M+S = 48,132 encounters or 21.9% of total), R codes (symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified = 41,646 or 18.9%), J (diseases of the respiratory system = 21,089 or 9.6%), N (diseases of h genitourinary system = 15,720 or 7.1%), and K (diseases of the digestive system = 14,718 or 6.7%).
Figure 1.

Number of encounters in the Emergency Room per year (2016–2020) for all age group (n=220,153) and for those 60 yr. and older (n=56,294)
All encounters (all ICD-10-CM codes), 60 yr. and older group
The total number of unique patients in the 60 yr. and older group was 24,412 (25.9% of unique patients). The total number of encounters in the group 60 yr. and older was 56,294 (25.6% of all encounters), ranging from 10,734 (22.4%) in 2016 to 9,274 (28.7%) in 2020 (Figure 1). This age group showed a 29.5% reduction in the number of encounters in year 2020 compared to the year 2019. Finally, females accounted for 31,488 (56.0%; p < 0.0001) encounters in this age group.
MSK related encounters, all age groups
Of the total number of encounters in all age groups, 48,132 (21.9%) were due to MSK health conditions. Of these, 14,855 (30.9%) were classified as M codes (MSK and connective tissue) and 33,277 (69.1%) as injuries (S codes). The distribution of all MSK-related encounters per year is presented in Figure 2. The median age of all MSK-related encounters was 43 years (IQR: 24 – 61) with a median of 47 for females (IQR: 27 – 64) and 39 for males (IQR: 21 – 57) (p < 0.001). Females accounted for 24,711 (51.4%; p < 0.0001) of all encounters due to MSK complaints (range: 51.0%−53.6%). MSK complaints represented 19.4% and 25.2% of all encounters in females and males, respectively (p < 0.01).
Figure 2.
Number of encounters in the Emergency Room per year (2016–2020) due to musculoskeletal conditions for all age groups (n=48,132) and for those 60 yr. and older (n=12,744).
MSK related encounters, 60 yr. and older age group
In the 60 yr. and older group, a total of 12,744 encounters were related to MSK codes as registered in the primary diagnosis field of the database. This represents 22.6% of all encounters in this age group and 26.5% of all MSK encounters in all age groups. Of these encounters, 4,176 (32.8%) were classified as M codes and 8,568 (67.2%) were classified as S codes. The number of MSK encounters per month and year for this age group is presented in Figure 3. The median age was 72 (IQR: 65 – 79). The median age for females was 73 yr, (IQR: 66 – 80), and 70 yr. (IQR: 64 – 78) for males (p< 0.0001). Females accounted for 7,637 (59.9%) of these encounters.
Figure 3.

Total number of musculoskeletal encounters (n=12,744) per month for the 60 yr. and older age group for calendar years 2016–2020.
Table 1 shows the number of MSK encounters by age-subgroup. The proportion of MSK encounters was lower in the 20–29 yr age group (17.4%) and highest in the 50–50 yr. age group (25.4%). In the older age groups, the proportion of MSK encounters ranged between 20.9% and 24.1% shows a decreasing trend with increased age (p < 0.0001).
Table 1.
Total encounters and encounters due to musculoskeletal (MSK) conditions by age sub-group
| Age sub-group (yr.) | Total encounters | Percent | MSK encounters | MSK encounters as percent from encounters in age group * |
|---|---|---|---|---|
| 0–09 | 21,401 | 9.7 | 4,052 | 18.9 |
| 10–19 | 19,631 | 8.9 | 4,667 | 23.8 |
| 20–29 | 42,462 | 19.3 | 7,373 | 17.4 |
| 30–39 | 26,882 | 12.2 | 5,874 | 21.9 |
| 40–49 | 25,730 | 11.7 | 6,360 | 24.7 |
| 50–59 | 27,753 | 12.6 | 7,062 | 25.4 |
| Older age groups | ||||
| 60–69 | 22,736 | 10.3 | 5,479 | 24.1 |
| 70–79 | 18,731 | 8.5 | 4,132 | 22.1 |
| 80–89 | 11,606 | 5.3 | 2,443 | 21.0 |
| 90–99 | 3,087 | 1.4 | 662 | 21.4 |
| 100+ | 134 | 0.1 | 28 | 20.9 |
| Total | 220,134 | 100 | 48,132 | 21.9 |
Test for trend among older age groups: p value < 0.0001
Most frequent ICD-10-CM codes
The number and percent of encounters associated with the top five MSK codes in the 60 yr. and older adults is shown in Table 2. Overall, contusion and lacerations of head and scalp were the most frequent codes. This category included several codes that are not typically considered MSK health complaints but are coded in the S code group. Among the codes most commonly recognized as MSK, low back pain (M54.5) was the most frequent, followed by pain in knee (M25.56; all groups and females) and pain in shoulder (M25.51; males).
Table 2.
Five most-frequent ICD-10-CM musculoskeletal codes in all 60 yr. and older adults
| ICD-10-CM Code | Code text | Number of encounters (%)* |
|---|---|---|
| ** | Contusion/laceration of head or scalp | 1,700 (13.3%) |
| M54.5 | Low back pain | 1,115 (8.8%) |
| M25.56 | Pain in knee | 360 (2.8%) |
| M62.83 | Muscle spasm | 354 (2.8%) |
| M25.55 | Pain in hip | 251 (2.0%) |
| Females | ||
| ** | Contusion/laceration of head or scalp | 651 (8.6%) |
| M54.5 | Low back pain | 645 (8.4%) |
| M25.56 | Pain in knee | 257 (3.4%) |
| M25.55 | Pain in hip | 179 (2.3%) |
| S72.14 | Intertrochanteric fracture of femur | 174 (2.3%) |
| Males | ||
| ** | Contusion/laceration of head or scalp | 712 (14%) |
| M54.5 | Low back pain | 468 (9.2%) |
| M25.51 | Pain in shoulder | 118 (2.3%) |
| M62.83 | Muscle spasm | 111 (2.2%) |
| M25.56 | Pain in knee | 103 (2.0%) |
% of all musculoekeletal encounters in 60 yr. and older adults
Includes the following codes S00.83, S01.01, S00.93, S01.81, S09.90
Table 3 shows the top five ICD-10-CM codes in older adults for each age sub-group. In adults between 60 and 69 yr., the most frequent MSK health complaint was low back pain (M54.5). Femoral fractures became more common with advanced age and intertochanteric fracture of femur (S72.14) was the most common code in those 90 yr. and older.
Table 3.
Five most-frequent ICD-10-CM musculoskeletal codes in 60 yr. and older adults per decade
| ICD-10-CM Code | Code text | Number of encounters (%)* |
|---|---|---|
| 60 – 69 years old | ||
| M54.5 | Low back pain | 620 (11.3%) |
| M25.56 | Pain in knee | 194 (3.5%) |
| M62.83 | Muscle spasm | 150 (2.7%) |
| M25.51 | Pain in shoulder | 139 (2.5%) |
| S01.01 | Laceration without foreign body of scalp | 116 (2.1%) |
| 70 – 79 years old | ||
| ** | Contusion/Laceration of head or scalp | 577 (13.9%) |
| M54.5 | Low back pain | 350 (8.5%) |
| M25.56 | Pain in knee | 114 (2.8%) |
| S20.21 | Contusion of front wall of thorax | 85 (2.1%) |
| M25.55 | Pain in hip | 82 (2.0%) |
| 80 – 89 years old | ||
| ** | Contusion/Laceration of head or scalp | 484 (19.8%) |
| M54.5 | Low back pain | 124 (5.1%) |
| S72.14 | Intertrochanteric fracture of femur | 96 (3.9%) |
| M25.55 | Pain in hip | 57 (2.3%) |
| S72.00 | Fracture of unspecified part of neck of femur | 54 (2.2%) |
| 90 – 99 years old | ||
| ** | Contusion/Laceration of head or scalp | 163 (24.5%) |
| S72.14 | Intertrochanteric fracture of femur | 50 (7.6%) |
| S72.00 | Fracture of unspecified part of neck of femur | 26 (3.9%) |
| M54.5 | Low back pain | 18 (2.7%) |
| M25.55 | Pain in hip | 14 (2.1%) |
| 100 + years old | ||
| S72.14 | Intertrochanteric fracture of femur | 6 (21.4%) |
| M54.5 | Low back pain | 3 (10.7%) |
| S00.93 | Contusion of unspecified part of head | 3 (10.7%) |
| S72.24 | Nondisplaced subtrochanteric fracture of right femur | 2 (7.1%) |
| 14 tied | - | 1 (3.6%) |
% of all musculoskeletal encounters of the corresponding age sub-group
Includes the following codes S00.83, S01.01, S00.93, S01.81, S09.90
Discussion:
The most important findings of the present study were: 1) older adults represented a substantial portion (25.6%) of all encounters in the ER during the five-year period, 2) females were involved in most encounters (56%), 3) older adults represented 26.5% of all MSK encounters and females were involved in the majority of encounters (59.9%) in the 60 yr. and older group, 4) the proportion of encounters with MSK codes showed a reduction with increasing age, 5) the most common MSK condition was low back pain except in the oldest age sub-group (90 yr. and older) where fracture of the femur was predominant, and 6) a significant reduction in the number of all and MSK encounters was observed in 2020 in both sexes and all age groups that coincided with the beginning of the restrictions due to the pandemic.
Very few published studies are based on multi-year, large samples of encounters from older adults similar to ours. In a five-year study of encounters in the ER in the only academic medical center in Iceland, serving a population of approximately 318,000 (very similar to the population in the catchment area of our hospital), the total number of ER encounters was 373,000 and patients 67 yr. and older represented 20% of all visits (11). During the five years (2008–2012) of the study, most older patients were female (54%) with an average age of 78.6 yr. (men=77.3 yr.), MSK disorders represented 16% of all codes and were the most frequent amongst women. In comparison, in the present study, the total number of ER encounters was lower, but the distributions by sex (59.9% female) and age (median = 72 yr.) were similar. On the other hand, MSK complaints accounted for a larger proportion of encounters in our older population (22.6% vs. 16%). The proportion of encounters with MSK codes shows a decreasing trend with age amongst older age sub-groups (Table 1). Access to services in other health care settings with increasing age can be an explanation. It is also possible that other chronic conditions that require ER services increased proportionally. However, the severity of the top MSK conditions increased with age (Table 3).
In the present study, older men and women represented 25.6% of all encounters. This is similar to studies in various countries where adults older than 60 yr. represent between 20 and 30% of all ER encounters (11, 22, 23). However, some of the other countries have a younger general population. This high utilization amongst elderly may be associated with many factors including the presence of co-morbidities, financial barriers to regular care, absence of supportive and social care in the community, and inadequate access (including technology-based care) to health care facilities where non-urgent MSK complaints can be treated (9).
Treatment of MSK pain in older adults is important because pain is associated with a greater risk of falls (6). Furthermore, older people with MSK pain have more frailty, depression, and cognitive decline than people without pain (24). In the present study, most MSK health complaints in all age sub-groups were associated with pain (see Table 3). Low back pain was very frequent and, although non-specific in many cases, it must be evaluated and treated. Low back pain was also the most common complaint in a study of ER patients aged 80 years or over (age range 80–104 yr.) in Finland (12). In that study, hip fracture was more common among those requiring hospitalization. We should not forget that many of these patients require follow-up in rehabilitation clinics, a visit that presents an opportunity to include an exercise program, with important injury prevention components, in many intervention plans.
It was not our initial intent to examine the effect of the SARS-Cov-2 pandemic on the utilization of the ER by older adults. However, because of the importance of the topic, it is relevant and appropriate to comment on the substantial reduction (33.2%) of ER encounters during the calendar year 2020, which coincides with the lockdown in Puerto Rico. This reduction was noted in both sexes, all age groups, and in MSK health complaints. Our findings are consistent with other recent reports. For example, in the United States, the Centers for Disease Control and Prevention (CDC) reported a 42% reduction in visits to the ER during the first four weeks of the pandemic (March 29-April 25, 2020) in comparison to the same four-week period in 2019 (25). Included in that study were data from more than 3,500 ERs. A 15.8% reduction in ER encounters was also reported in a study conducted in the three largest hospitals in Finland (26) during a national lockdown. The number of ER encounters due to back or limb pain decreased the most. The drop in utilization of our ER can be explained by several factors including the implementation of a lockdown that limited most activities in the island, the recommendations for physical distancing, feelings of fear to get infected in an ER, and inability of relatives to accompany patients with health complaints to the ER, among others. A more detailed analysis of these results regarding the impact of the pandemic will be presented in a separate publication.
Several limitations of the present investigation must be acknowledged. Our study was based on the ICD-10-CM classification as recorded in the hospital’s administrative database. The selection of the code is therefore dependent on the judgement of multiple physicians and coders. However, our analysis included variables (age, sex) that are not likely to be confused, as well as codes in 2 groups (M and S) that can be clearly distinguished from other ICD-10-CM categories. Further, specific complaints frequently seen in our ER, such as low back pain and femur fractures, are not likely to be misclassified. The age group ≥ 60 yr. is very diverse and findings may be different in the oldest (≥ 80yr.) group. We selected 60 as the cut-off age because it is used by the WHO in many official reports. Further, we addressed this concern by including an analysis of older adults by age sub-groups (see Tables 1–3). Finally, due to the academic status of the hospital and the availability of specialized MSK services, it is possible that other ER’s may have a different patient mix and utilization pattern of services.
Conclusion
The utilization of ER services for MSK complaints by older adults is substantial. This is an important issue in light of the current and projected increase of the older population in the next few decades. ER encounters are resource intensive and expensive, particularly in this age group, adding to the relevance of our findings. Because many MSK disorders seen in the present study are not emergencies, alternative sites should be considered for the management of these health conditions at the appropriate level of care.
References:
- 1.World Health Organization. (2015). World report on ageing and health. World Health Organization. https://apps.who.int/iris/handle/10665/186463 [Google Scholar]
- 2.United States Census Bureau. Available at: https://www.census.gov/data-tools/demo/idb/#/pop?YR_ANIM=2020&COUNTRY_YR_ANIM=2015&FIPS_SINGLE=RQ&COUNTRY_YEAR=2015&menu=popViz&FIPS=RQ&popPages=BYAGE&ageGroup=O&POP_YEARS=2020,2050 Accessed September 30, 2021.
- 3.World Health Organization. Available at https://www.who.int/initiatives/decade-of-healthy-ageing. Accessed June 21, 2021.
- 4.Cieza A, Causey K, Kamenov K, et al. ; Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. Published Online December 1, 2020 10.1016/S0140-6736(20)32340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaudart C, Biver E, Bruyère O. Assessment of quality of life in Musculo-skeletal health. Aging Clin Exp Res 2018; 30:413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leveille SG, Jones RN, Kiely DK., et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 2009; 302:2214–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hastings SN, Whitson HE, Purser JL, Sloane RJ, Johnson KS. Emergency Department discharge diagnosis and adverse health outcomes in older adults. J Am Geriatr Soc 2009; 57:1856–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsia RY, Sabbagh SH, Guo J, Nuckton TJ, Niedzwiecki MJ. Trends in the utilization of emergency departments in California, 2005–2015: a retrospective analysis. BMJ Open 2018;8:e021392. doi: 10.1136/bmjopen-2017-021392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Or Z, Penneau A. A multilevel analysis of the determinants of emergency care visits by the elderly in France. Health Policy 2018; 122:908–914. [DOI] [PubMed] [Google Scholar]
- 10.Huang L-C, Chung W-F, Liu S-W, Wu J-C, Chen L-F, Chen Y-C. Characteristics of non-emergent visits in emergency departments; profiles and longitudinal pattern changes in Taiwan, 2000–2010. Int J Environ Res Public Health 2019; 16:1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gudmundsdottir E, Masdottir HR, Gudmundsdottir H, et al. : Variation in elderly people’s visits to the emergency departments in Iceland: a five-year population study. Int Emerg Nurs 2018; 37:6–12. [DOI] [PubMed] [Google Scholar]
- 12.Ukkonen M, Jämsen E, Zeitlin R, Pauniaho SL. Emergency department visits in older patients: a population-based survey. BMC Emerg Med 2019; 19:20. doi: 10.1186/s12873-019-0236-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fontánez R, Ramos Guasp W, Ramírez H, et al. ; Musculoskeletal conditions in the emergency room: a teaching opportunity for medical students and residents. P R Health Sci J 2021; 40:68–74. [PMC free article] [PubMed] [Google Scholar]
- 14.Puerto Rico Statistics Institute. Población total en municipios de Puerto Rico 2010–2019. Available at: https://censo.estadisticas.pr/estimadospoblacionales. Accessed June 11, 2021.
- 15.World Health Organization, International Classification of Diseases - Clinical Modification (ICD-10-CM), 10th revision, 2015, Geneva, Switzerland. Accessed December 12, 2020. [Google Scholar]
- 16.National Center for Health Statistics-Centers for Disease Control and Prevention, ICD-10-CM Official Guidelines for Coding and Reporting, Available at: https://www.cdc.gov/nchs/data/icd/10cmguidelines-FY2021. Accessed December 12, 2020.
- 17.Rosner B Fundamentals of Bioststistics,8th ed. Massachusetts: CENGAGE Learning, 2016, 352–358. [Google Scholar]
- 18.Rosner B Fundamentals of Bioststistics,8th ed. Massachusetts: CENGAGE Learning, 2016, 418–421. [Google Scholar]
- 19.R Core Team. R: A language and environment for statistical Computing. R Foundation for Statistical Computing. Vienna, Austria. 2020. (https://www.R-project.org) [Google Scholar]
- 20.RStudio Team. RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA. 2020. (https://www.rstudio.com/). [Google Scholar]
- 21.Fox J The R Commander: A Basic Statistics Graphical User Interface to R. Journal of Statistical Software 2005; 14(9): 1–42. [Google Scholar]
- 22.Fayyaz J, Khursheed M, Mir MU, Khan U. Pattern of emergency department visits by elderly patients: study from a tertiary care hospital, Karachi. BMC Geriatrics 2013; 13:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gulacti U, Lok U, Celik M, Aktas N, Polat H. The ED use and non-urgent visits of elderly patients. Turk J Emerg Med 2016;16:141–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blyth FM, Noguchi N. Chronic musculoskeletal pain and its impact on older people. Best Prac Res Clini Rheum 2017; 31:160–168. [DOI] [PubMed] [Google Scholar]
- 25.Hartnett KP, Kite-Powell A, DeVies JD, et al. : Impact of the COVID-19 pandemic on emergency department visits – United States, January 1, 2019-May 30, 2020. MMWR 2020;69:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuitunen I, Ponkilainen VT, Launonen AP, et al. : The effect of national lockdown due to COVID-19 on emergency department visits. Sacnd J Trauma Resusc Emerg Med 2020; 28:114. [DOI] [PMC free article] [PubMed] [Google Scholar]


