Abstract
The number of pets such as dogs, cats, rabbits, and parrots has increased in European families. Social benefits to owners such as decreasing feelings of loneliness and anxiety are provided by pets which are also used in Animal-assisted Therapy (AAT). Nevertheless, human-animal interactions are also associated with health problems including allergies, asthma, and zoonosis. Rabbits may carry potential pathogens for humans. One of the most common bacteria that colonizes the oro-pharynx and the upper respiratory tract of rabbits is Pasteurella (P.) multocida. Transmission of the infection to humans results from scratches, licks, and bites but it also can occur from the inhalation of air particles containing the microorganism. Immunocompromised people or persons with pulmonary disorders are particularly susceptible to the infection. Infected rabbits may carry P. multocida with or without clinical signs. In this paper, the sensitivity to antibiotics and the invasiveness ability of P. multocida identified in a farm of pet rabbits affected by severe pasteurellosis were investigated. The strain was P. multocida belonging to capsular type A which is the type most often detected in humans. The identified strain was susceptible to the tested antibiotics, but it appeared equipped with several virulence genes which are responsible for fimbriae production, adhesion processes to host cells, enzyme production, and are involved in iron acquisition processes. These findings are of particular interest because rabbits recovered from pasteurellosis very often become carriers of the bacteria. Therefore, we suggest considering P. multocida screening in the routine medical checks of rabbits, especially if they are meant to be companion animals for children and elder people, given that the transmission of the pathogen cannot be excluded.
Keywords: pet rabbit, Pasteurella multocida, virulence genes, vaccine
1. Introduction
In recent years, the presence of pets in European families has increased and their number nowadays exceeds 300 million [1]. After dogs and cats, unconventional animals such as small mammals (30 million) and pet birds (52 million) represent a significant part of the total number of pets [1]. In particular, rabbits are increasingly common in the home environment in some countries such as the United Kingdom [2]. Pets provide great social benefits to owners such as decreasing feelings of loneliness and anxiety and increasing opportunities for socialization [3]. Moreover, dogs, cats, horses, rabbits, and hamsters are frequently used in Animal-assisted Therapy (AAT). Despite these benefits, human-animal interactions are associated with risks of health problems, including allergies, asthma, animal bites, and scratches [4]. In addition, pets are not always able to provide a positive effect in case of mental illness or untreated stress in people [3]. Companion animals can also transmit potential pathogens to humans. Zoonotic agents can be transmitted both through direct contact with infected animals and indirectly through environmental contamination [2]. People aged over 65 years and children younger than 5 years are the most susceptible to such infections. Moreover, immunocompromised persons and pregnant women are particularly exposed to the risk of pet-induced zoonoses [5].
Psittacosis is the most known zoonosis transmitted by pet birds. Chlamydia (C.) psittaci can be present in 40% of pet birds, most prevalently parrots but also other species such as canary [6,7,8]. Infected birds spread C. psittaci by excreta, nasal, and ocular secretions. The transmission of C. psittaci to humans occurs through the inhalation of the pathogen spread in the air and dust contaminated by respiratory secretions and feces from infected birds. In addition, transmission via bird bites and transmission beak to mouth have been reported [9]. In humans, C. psittaci can cause asymptomatic infections or acute infections characterized by flu-like illness, mild to severe atypical pneumonia, and systemic disease, which can be fatal in untreated patients [10]. Pet birds may carry also other pathogens such as nontyphoidal Salmonella [11], Campylobacter jejuni [12], and Mycobacterium avium subs. avium [13] to humans.
Zoonoses are also associated with rabbits. Dermatophytosis in rabbits is caused by Trichophyton mentagrophytes, Microsporum (M.) canis, and M. gypseum which represent the most common agents of zoonosis in rabbits [2,14]. Rabbits can also carry several parasites such as Encephalitozoon cuniculi [15], Cryptosporidium spp. [16], Giardia spp. [17], and Tricostrongylus spp. [18] which can induce zoonoses.
Rabbits may also host viruses and bacteria which can be potential pathogens for humans. The hepatitis E virus has been recently identified in rabbits [19]. In France, a recent study reported evidence of natural SARS-CoV-2 infection in rabbits that was attributed to direct contact with human patients [20]. A recent study carried out in experimental conditions highlighted the evidence of viral shedding in infected rabbits, despite the low seroprevalence and the lack of clinical signs [21].
The detection of Mycobacterium avium subsp. hominissuis has been reported in domestic rabbits [22]. Moreover, three different Bartonella (B.) species, B. vinsonii subsp. berkhoffii, B. alsatica, and B. rochalimae, were identified in fleas from rabbits, although they were wild animals [23]. One of the most common bacteria of rabbits is Pasteurella (P.) multocida which colonizes the upper respiratory tract and the oro-pharynx. P. multocida is a small coccobacillus, pleomorphic, Gram-negative, facultative aerobic-anaerobic, asporigenous, immobile bacterium with a fermentative metabolism, belonging to the Pasteurellaceae family. P. multocida is characterized by considerable genetic and antigenic variability. The strains are classified into 5 capsular types or serogroups (A, B, D, E, and F), based on the antigenic characteristics of the capsule polysaccharides, which are further classified into 16 somatic serotypes, based on lipopolysaccharide antigens, using serological techniques. Infected rabbits may carry P. multocida without showing clinical signs or they may be affected by heavy clinical syndromes. Although the symptoms frequently develop when immunosuppression, stress, or adverse environmental conditions occur, the pathogenicity of P. multocida is influenced by the presence of several virulence factors (VFs) prevalently identified in capsule proteins and lipopolysaccharides [24,25]. Many other virulence genes that may be involved in the pathogenicity of P. multocida include fimbriae, adhesion, and colonization factors (ptfa, fimA, pfhA, and tadD), iron regulation factors and protein acquisition (exbB, exbD, tonB, hgbA, hgbB, tbpA, and fur), superoxide dismutase (sodA and sodC), dermonecrotic toxins (toxA), a variety of Outer Membrane Proteins (OMPs) as protective factors (ompA, ompH, omp87, and plpB), and neuraminidase (nanB and nanH) [25,26,27,28,29]. Therefore, the variability of the microorganism is also evident in the multiple clinical forms associated with pasteurellosis in rabbits, which mainly include respiratory tract diseases but also otitis, pyometra, mastitis, orchitis, abortions, subcutaneous abscesses, and acute septicemic forms [30]. Transmission of P. multocida to humans is usually due to bites, scratches, and licks by companion animals with the development of local inflammation and occasional abscess formation and, sometimes, ascending infection [5,9,31,32]. Wound infections may result in several other clinical forms such as lymphangitis, joint infections, cellulitis, pneumonia, endocarditis, meningitis, urinary infections, and sepsis [33,34]. Immunocompromised people or persons with pulmonary disorders are particularly susceptible to systemic infection [35]. Additionally, the transmission can occur following the inhalation of air particles containing the microorganism [31,36]. Therefore, P. multocida infections in humans are associated with respiratory symptoms, such as pneumonia, tracheobronchitis, lung abscesses, and pulmonary emphysema [37].
The significant increase in the number of families who choose a rabbit as a companion animal has led to giving more attention to Pasteurella multocida infection in rabbits as well. The aim of this work is to achieve more information on P. multocida from pet rabbits starting from a severe outbreak of pasteurellosis that occurred on a farm of pet rabbits routinely sold as companion animals and to discuss a preventive approach in order to reduce the spread of P. multocida among the animals.
2. Materials and Methods
2.1. History
The flock of pet rabbits was evaluated because they were suffering from respiratory syndrome cyclically for about two years. The flock was in Corato, BA, southern Italy, and consisted of about 100 rabbits, 90 females and 10 males, all reared to breed. The animals were Lion’s head and lop rabbits. They were housed in a shed where a climate control system ensured an ambient temperature of 15–18 °C and relative humidity of approximately 65%. The rabbits were fed with pellets, fresh vegetables, and hay. Each rabbit was housed in a single cage equipped with a drinking bottle and a feeder. Cages and sheds were regularly cleaned. The reproductive activity in the flock was scheduled throughout the year except for July and August, for the lacking demand for bunnies by customers in that period. The female animals were usually introduced in the cages of male rabbits and left for three days to allow natural mating and pregnancy. The rate of fertility was about 95%. The bunnies were regularly sold to private individuals and pet shops.
2.2. Clinical Findings
The respiratory syndrome occurred in both bunnies and adults. Conjunctivitis was the most evident clinical sign. This symptom was particularly observed in bunnies (Figure 1), and it usually appeared at 13–14 days of age, after a few days since the opening of the eyes.
Figure 1.
Left side of a bunny with severe clinical signs. Note the swollen eyelids and the purulent discharge on the hair around the nostrils.
Conjunctivitis started with catarrhal discharge, but the ocular discharge quickly became muco-purulent and occluded the eyelids (Figure 2).
Figure 2.
Left side of the head of a bunny with severe conjunctivitis. Note the purulent ocular discharge that occludes the eyelid.
Purulent rhinitis was frequently observed (Figure 3) and was often associated with the ocular lesion.
Figure 3.
Bunny with severe purulent rhinitis.
Affected bunnies were often undersized. The number of bunnies involved in the syndrome in each litter was variable. In fact, all the litter showed clinical signs in some cases, while only some bunnies were symptomatic in others. Sometimes, all the litter appeared healthy, but respiratory syndrome often appeared later, at the weaning time or after the sale of the bunnies. Breeders showed chronic rhinitis with muco-purulent discharge, but mothers of affected litters were not always symptomatic. Subcutaneous abscesses and torticollis were rarely observed only in adults. Moreover, some cases of late abortus were reported in lop rabbits. The animals were treated locally with ophthalmic ointments (chloramphenicol and chlortetracycline) by the owner which, cyclically, also administered trimethoprim/sulfamethoxazole via drinking water without improvements in the clinical conditions. Nasal and conjunctival swabs were collected from twelve symptomatic rabbits for laboratory investigations.
2.3. Bacteriology
Nasal and conjunctival swabs were plated on blood agar (Triptic Soy agar, Basingstoke, UK, supplemented with 5% sheep blood) and incubated at 37 °C for 24 h. Blood agar allows the growth of several different bacteria which can be associated with respiratory disorders (such as Pasteurella multocida, Bordetella bronchiseptica, and Staphylococcus aureus) or not associated with (Micrococcus spp., Staphylococcus spp., Streptococcus spp., and Pseudomonas spp.).
Three to five colonies from each plate were tested by Multiplex PCR according to [38] with some modifications to obtain the identification as Pasteurella multocida (P. multocida) and contextually to define the capsular type. Briefly, DNA extraction was carried out by boiling for 10 min. The primer set used in the PCR reaction is reported in Table 1. The PCR mixture consisted of 12.5 µL of 1X Platinum Mastermix (Thermo Scientific, Milan, Italy), containing 0.2 µL and 0.3 µL (50 pmol/µL primary concentration) of primer pair for specie identification and primer pairs for capsular types, respectively, and ultra-pure nuclease-free water (Thermo Scientific) until a final volume of 25 µL. Cycling conditions were as follows: 95 °C for 5 min, 35 cycles, each with 95 °C for 30 s, 55 °C for 30 s, 72 °C for 1 min and 10 s, and a final extension at 72 °C for 10 min. The PCR products were loaded for electrophoresis using a 1.5% agarose gel, which was stained with ethidium bromide. The reaction was visualized using the Gel Doc-It image analyzer (UVP, Upland, CA, USA).
Table 1.
Identification of Pasteurella multocida species and capsular type by Multiplex-PCR: Primers and corresponding oligonucleotides sequences.
| Target | Primers | Sequences | Amplimer Size |
|---|---|---|---|
| Pasteurella multocida specie | KMT1T7 | ATCCGCTATTTACCCAGTGG | 460 bp |
| KMT1SP6 | GCTGTAAACGAACTCGCCAC | ||
| Capsular type A | CAPA-FWD | TGCCAAAATCGCAGTCAG | 1044 bp |
| CAPA-REV | TTGCCATCATTGTCAGTG | ||
| Capsular type B | CAPB-FWD | CATTTATCCAAGCTCCACC | 760 bp |
| CAPB-REV | GCCCGAGAGTTTCAATCC | ||
| Capsular type D | CAPD-FWD | TTACAAAAGAAAGACTAGGAGCCC | 657 bp |
| CAPD-REV | CATCTACCCACTCAACCATATCAG | ||
| Capsular type E | CAPE-FWD | TCCGCAGAAAATTATTGACTC | 511 bp |
| CAPE-REV | GCTTGCTGCTTGATTTTGTC | ||
| Capsular type F | CAPF-FWD | AATCGGAGAACGCAGAAATCAG | 851 bp |
| CAPF-REV | TTCCGCCGTCAATTACTCTG |
2.4. Pathogenicity Genes Investigation
The presence of 15 different genes encoding for virulence factors of P. multocida was investigated starting from different studies focused on pathogenicity [26,27,39,40]. Despite the possible compatibility between the annealing temperatures of the different primers, three Multiplex-PCR protocols (named A, B, and C) were staged because of the similarity of the molecular weight of the different amplicons. Details about the primer set used in the different Multiplex-PCRs are reported in Table 2.
Table 2.
A, B, and C protocols of Multiplex-PCR: investigated virulence genes, corresponding primers and nucleotide sequences, and molecular weights of amplicons.
| Virulence Factor | Primer | Sequence | Amplimer Size | |
|---|---|---|---|---|
| A | Dermonecrotic toxin | ToxA-F ToxA-R | CTTAGATGAGCGACAAGGTT GGAATGCCACACCTCTATA | 865 bp |
| Trasferrin binding protein | TbpA-F TbpA-R | TTGGTTGGAAACGGTAAAGC TAACGTGTACGGAAAAGCCC | 728 bp | |
| Type 4 fimbriae | Fim4-F Fim4-R | TGTGGAATTCAGCATTTTAGTGTGTC TCATGAATTCTTATGCGCAAAATCCTGCTGG | 866 bp | |
| Superoxide dismutate | SodA-F SodA-R | TACCAGAATTAGGCTACGC GAAACGGGTTGCTGCCGCT | 361 bp | |
| Filamentous hemagglutinin | Pfha-F Pfha-R | AGCTGATCAAGTGGTGAAC TGGTACATTGGTGAATGCTG | 275 bp | |
| B | Iron acquisition | ExbB-F ExbB-R | TTGGCTTGTGATTGAACGC TGCAGGAATGGCGACTAAA | 283 bp |
| Hemoglobin binding protein | HgbB-F HgbB-R | ACCGCGTTGGAATTATGATTG CATTGAGTACGGCTTGACAT | 788 bp | |
| Neuroaminidase | NanB-F NanB-R | GTCCTATAAAGTGACGCCGA ACAGCAAAGGAAGACTGTCC | 554 bp | |
| Putative nonspecific tight adherence protein D | TadD-F TadD-R | TCTACCCATTCTCAGCAAGGC ATCATTTCGGGCATTCACC | 416 bp | |
| Lipoprotein B | PlpB-F PlpB-R | TTTGGTGGTGCGTATGTCTTCT AGTCACTTTAGATTGTGCGTAG | 282 bp | |
| Superoxide dismutate | SodC-F SodC-R | AGTTAGTAGCGGGGTTGGCA TGTGCTGGGTGATCATCATG | 235 bp | |
| C | Outer membrane protein 87 | Oma87-F Oma87-R | ATGAAAAAACTTTTAATTGCGAGC TGACTTGCGCAGTTGCATAAC | 948 bp |
| Fimbriae | FimA-F FimA-R | CCATCGGATCTAAACGACCTA AGTATTAGTTCCTGCGGGTG | 866 bp | |
| Neuroaminidase | NanH-F NanH-R | GAATATTTGGGCGGCAACA TTCTCGCCCTGTCATCACT | 360 bp | |
| ferric uptake regulation protein | Fur-R Fur-F |
GTTTACCGTGTATTAGACCA CATTACTACATTTGCCATAC | 244 bp |
The PCR mixture for Multiplex-PCRs consisted of 12.5 µL of 1X Platinum Mastermix (Thermo Scientific, Milan, Italy), 0.5 µL of each primer pair in a 50 pmol/µL primary concentration, and ultra-pure nuclease-free water (Thermo Scientific, Milan, Italy) until a final volume of 25 µL.
The thermal conditions previously reported in Pasteurella multocida identification paragraph (2.1.) were used for A, B, and C Multiplex-PCRs. All PCR products were visualized by agarose gel electrophoresis (1.5%) which was colored with ethidium bromide (0.5 μg/mL), using TBE (Tris-Borato-EDTA) as conductor. PCR results were read with Gel Doc-It (UVP) image analyzer.
2.5. Antibiotic Susceptibility Testing
The susceptibility of the identified bacterium to the antibiotics more frequently used in veterinary and human medicine to treat respiratory diseases and wounds from animals was evaluated. Therefore, the susceptibility to ciprofloxacin (CIP 5 μg/mL), sulfamethoxazole-trimethoprim (SXT 25 μg/mL), enrofloxacin (ENR 5 μg/mL), ampicillin (AMP 10 μg/mL), tetracycline (TE 30 μg/mL), nalidixic acid (NA 30 μg/mL), gentamicin (CN 10 μg/mL), amoxicillin-clavulanic acid (AMC 30 μg/mL), imipenem (IPM 10 μg/mL), cefotaxime (CTX 30 μg/mL), tilmicosin (TIL 15 μg/mL), amoxicillin (AX 25 μg/mL), doxycycline (DO 30 μg/mL), meropenem (MEM 10 μg/mL), azithromycin (AZM 15 μg/mL), and erythromycin (E 15 μg/mL) was determined. The standard Kirby–Bauer disk diffusion method on Muller–Hinton agar supplemented with 5% horse blood in aerobic and microaerophilic conditions was used according to European Committee on Antimicrobial Susceptibility Testing [41] and Clinical and Laboratory Standards Institute [42] standards. CLSI and EUCAST breakpoints were used to determine the susceptibility of the bacterium to the tested drugs.
3. Results
3.1. Pasteurella multocida Detection, Capsular Type, and Pathogenicity Pattern Identification
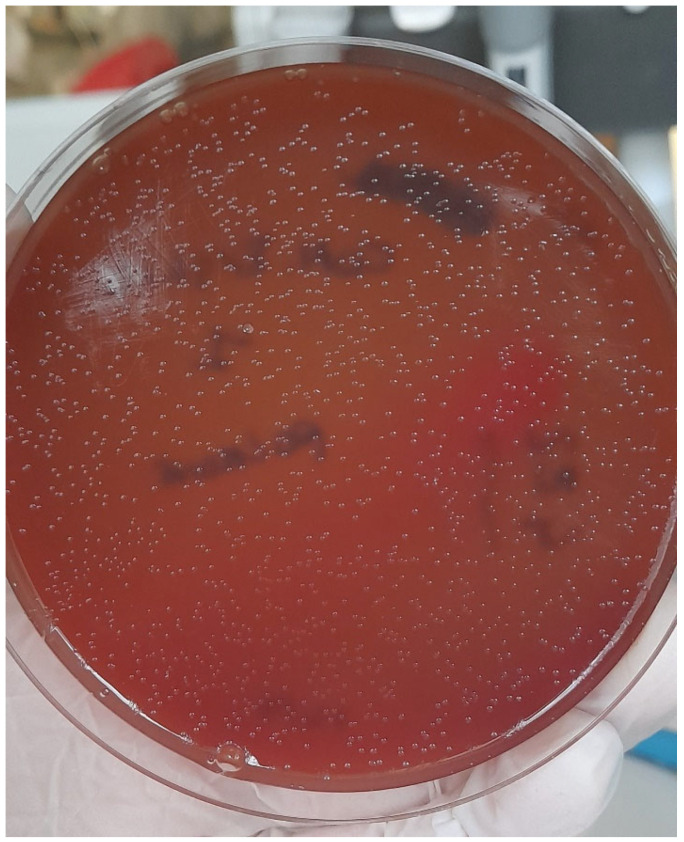
The colonies appeared morphologically compatible with Pasteurella spp. (gray, translucent, and no-haemolytic) (Figure 4). No other kind of colony was found.
Figure 4.
Microbiological findings from conjunctival sample: colonies were grown on blood agar and were identified as Pasteurella multocida.
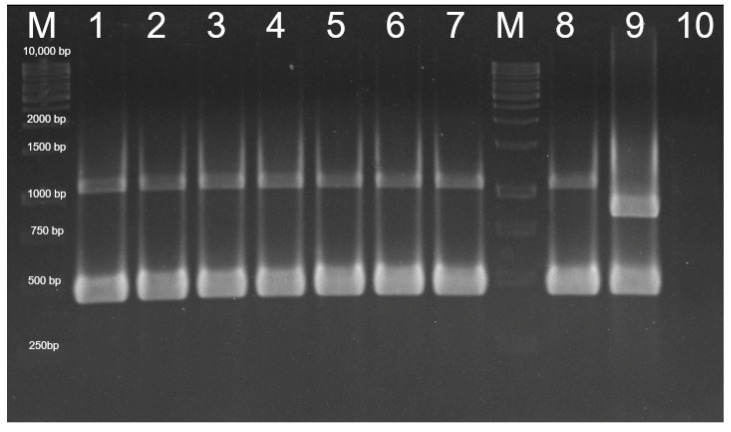
All tested colonies were identified as P. multocida belonging to capsular type A (Figure 5).
Figure 5.
Identification of P. multocida type A by PCR: M: Marker (O’ Gene Ruler 1kb DNA Ladder, Ready to use, 250–10,000 bp, Thermo Scientific Inc.). Lanes 1, 2, 3, 4: conjunctival samples; Lanes 5, 6, 7: nasal samples; M: Marker; Lane 8: P. multocida type A positive control; Lane 9: P. multocida type F positive control; and Lane 10: negative control.
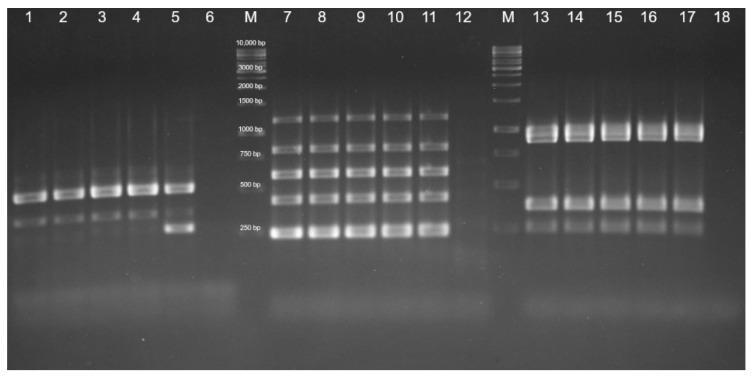
Each strain tested positive for 11 different virulence genes: fim4, fimA, and tadD, responsible for fimbriae production and adhesion processes to host cells; sodA, sodC, nanB1, and nanH1, responsible for enzyme production, hgbB, exbB, oma87, and fur, involved in iron acquisition processes (Figure 6).
Figure 6.
Detection of virulence genes of P. multocida by PCR. Protocol A: detection of SodA (361 bp), Fim4 (488 bp): Lanes 1, 2: conjunctival samples; Lanes 3, 4: nasal samples; Lane 5: positive control; Lane 6: negative control; M: Marker: O’ Gene Ruler 1kb DNA Ladder, Ready to use, 250–10,000 bp, Thermo Scientific Inc. Protocol B: detection of SodC (235 bp), TadD (416 bp), nanB1 (544 bp), HgbB (788 bp), ExbB (1144 bp): Lanes 7, 8: conjunctival samples; Lanes 9, 10: nasal samples; Lane 11: positive control; Lane 12: negative control; M: Marker. Protocol C: detection of Fur (244 bp), NanH1 (360 bp), FimA (866 bp), Oma87 (948 bp): Lanes 13, 14: conjunctival samples; Lanes 15, 16: nasal samples; Lane 17: positive control; and Lane 18: negative control.
3.2. Antibiotic Susceptibility Testing
Pasteurella multocida was susceptible in vitro to all the antibiotics tested both in aerobic and microaerophilic conditions. Details on the results of antimicrobial susceptibility tests are reported in Table 3.
Table 3.
Antibiotic susceptibility test performed on P. multocida detected in pet rabbit breeding.
| Diameter of Inhibition Zone (mm) | |||
|---|---|---|---|
| Antibiotic (Acronym) | Susceptibility Breakpoint | Aerobic Conditions | Microaerophilic Conditions |
| Ciprofloxacin (CIP) | 27 | 58 | 62 |
| Trimetophim-Sulfametoxazole (SXT) | 24 | 28 | 28 |
| Enrofloxacin (ENR) | 28 | 48 | 52 |
| Ampicillin (AMP) | 27 | 32 | 30 |
| Tetracycline (TE) | 24 | 46 | 44 |
| Nalidixic acid (NA) | 23 | 50 | 52 |
| Gentamicin (CN) | 20 | 22 | 26 |
| Amoxicillin-Clavulanic acid (AMC) | 27 | 36 | 30 |
| Imipenem (IPM) | 23 * | S | 40 |
| Cefotaxime (CTX) | 26 | S | 54 |
| Tilmicosin (TIL) | 14 | 28 | 27 |
| Amoxicillin (AX) | 17 | 33 | 36 |
| Doxycycline (DO) | 23 | 36 | 40 |
| Meropemem (MEM) | 23 * | 42 | 48 |
| Azitromycin (AZM) | 20 | 44 | 40 |
| Erytrhomycin (E) | 27 | 32 | 36 |
* Susceptibility breakpoint referred to Enterobacteriaceae due to lacking specific values for P. multocida.
3.3. Outcome
The disease observed in the flock of pet rabbits was caused by a capsular type A Pasteurella multocida strain provided with a consistent set of genes associated with virulence. Based on the results of tests of susceptibility to antibiotics, the involved strain was susceptible to all tested antibiotics. Enrofloxacin was chosen for treatment because it is one of the most effective drugs to control the clinical forms of Pasteurella multocida in rabbits and is also authorized for use in pets.
Given the high number of rabbits to be treated, enrofloxacin was administered by drinking water (200 mg/L) for 15 days, obtaining the remission of rhinitis and conjunctivitis in bunnies and the improvement of symptoms in adults. One month after the end of the therapy, an inactive commercial vaccine was used to immunize the rabbits, obtaining a complete remission of the clinical form in the following six months.
4. Discussion
The correct diagnosis in veterinary medicine is of relevance for both animal and human health, considering that some pathogens can be transmitted to humans. Pasteurella multocida was identified as responsible for the syndrome observed in a flock of pet rabbits. P. multocida can be spread by affected animals mainly through nasal discharge. The effectiveness of the therapy is crucial to reducing the clinical symptoms and decreasing the spread of the bacteria involved in the disease process.
In vitro, the identified strain was susceptible to the antibiotics more frequently used in veterinary and human medicine, but the applied therapy appeared only partially efficacious in rabbits. Although enrofloxacin is the most suitable drug for treatments against P. multocida infections in rabbits, its in vivo efficacy is known to be lower than its in vitro efficacy. Therefore, the antibiotic treatment led only to the improvement of clinical conditions of the most heavily affected or chronically infected rabbits. Additionally, enrofloxacin was administrated by drinking water due to the high number of animals to be treated. Drinking water treatment can lead to non-uniform dosages because of different water intake by sick animals. In addition, after the antibiotic treatment, clinically healed rabbits often become carriers of P. multocida, with the possibility that the clinical signs will reappear later when adverse conditions occur [43].
These events could lead to possible risks for owners that may acquire Pasteurella infection from injuries caused by pets, but also by direct exposure to the bacteria [5,9,31,32]. Currently, rabbits are largely reared as pets and usually live in close contact with their owners. Nevertheless, these animals are timid, and scratches can frequently occur because they are often picked up and pampered. In addition, rabbits are often territorial, and may sometimes bite their owner, particularly when he/she manipulates the feeder or other cage equipment. Although P. canis and P. dagmatis may be found in bites from dogs and cats, P. multocida is the most prevalent species associated with human infections due to bites from companion animals [44].
P. multocida capsular type A was identified in the affected rabbits in this study. Type A is the serogroup prevalently associated with pasteurellosis in rabbits [25] and, interestingly, it is almost the only one detected in strains from humans [44,45], even type F, also found to be responsible for infections in rabbits [46], has been sporadically identified in humans [44,45]. Rabbits are very susceptible to P. multocida infection, which seems to affect them independent of gender and age. The clinical presentation of pasteurellosis in rabbits includes rhinitis, sinusitis, conjunctivitis, dacryocystitis, and pleuropneumonia, as well as otitis, encephalitis, and abscesses of the subcutaneous tissues or internal organs, bones, joints, and genitalia [47,48]. Symptoms frequently develop when immunosuppression, stress, or adverse environmental conditions occur. Nevertheless, strains equipped with several genes encoding for different virulence mechanisms usually have greater survival and invasiveness capabilities in the host [49,50,51] and are more frequently prone to induce clinical forms [28].
Many virulence genes involved in the pathogenicity of P. multocida such as fimbriae, adhesion and colonization factors (ptfa, fimA, pfhA, and tadD), iron regulation factors and protein acquisition (exbB, exbD, tonB, hgbA, hgbB, tbpA, and fur), superoxide dismutase (sodA and sodC), dermonecrotic toxins (toxA), a variety of Outer Membrane Proteins (OMPs) as protective factors (ompA, ompH, omp87, and plpB), and neuraminidase (nanB and nanH) have been proposed as possible markers of virulence [25,26,27,28,29]. According to studies carried out on P. multocida strains identified as responsible for disease in humans and other species [25,44], the strain isolated from the affected rabbits tested positive for several different virulence genes: fim4, fimA, and tadD, responsible for fimbriae production and adhesion processes to host cells; sodA, sodC, nanB1, and nanH1, responsible for enzyme production, and hgbB, exbB, oma87, and fur, involved in iron acquisition processes. This finding seems to explain the evidence of symptoms observed in the affected rabbits as well as some difficulties related to achieving the complete resolution of the syndrome that was obtained in the rabbit flock about 6 months after using the vaccine. The use of vaccines to immunize the rabbits against P. multocida, in particular, is recommended to minimize the risk of outcomes of the clinical form, but also to reduce the spread of bacteria by the infected animals. Therefore, rabbits should be routinely vaccinated against P. multocida when considering that they are reared as household pets and the transmission of the pathogen to humans cannot be excluded. Nevertheless, the vaccine is not able to prevent the infection, and bunnies that are sold to individuals and pet shops may appear healthy, even when they carry the bacterium. Therefore, screening for P. multocida should be considered as a part of the routine medical check of rabbits, particularly when they are purchased as companion animals for children and elder people. Additionally, typing the detected strains of the bacteria is important to assess their pathogenic potential and, consequently, to increase hygienic measures in the management of pet rabbits.
5. Conclusions
This study provides more knowledge about Pasteurella multocida detected in pet rabbits. We suggest the routine use of vaccines in pet rabbits and screening for P. multocida in the routine veterinary examination of rabbits, particularly when they will be used for pet therapy or kept as companion animals for children and elder people, considering that the transmission of the pathogen to humans cannot be excluded.
Author Contributions
Conceptualization, E.C.; methodology, F.D., G.C. and E.C.; validation, G.B. and R.L.; formal analysis, F.D. and E.C.; investigation, F.D. and G.C.; resources, G.B. and A.C.; data curation, M.M.D. and E.C.; writing—original draft preparation, F.D., G.C. and E.C.; writing—review and editing, E.C.; visualization, A.C.; supervision, E.C.; project administration, E.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical review and approval were waived for this study because the samples were collected for diagnostic purposes to assess the correct clinical approach. Then, the authors performed the typing of the detected bacterial strains and the assessment of their sensitivity to the antibiotics.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rapporto Assalco-Zoomark ai Tempi del COVID-19. [(accessed on 17 November 2021)]. Available online: https://www.assalco.it/index.php?action=shownews&id=1&nid=10415.
- 2.Day M.J. Pet-related infections. Am. Fam. Phys. 2016;94:794–802. [PubMed] [Google Scholar]
- 3.Scoresby K.J., Strand E.B., Ng Z., Brown K.C., Stilz C.R., Strobel K., Barroso C.S., Souza M. Pet ownership and quality of life: A systematic review of the literature. Vet. Sci. 2021;8:332. doi: 10.3390/vetsci8120332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman E., Krause-Parello C.A. Companion animals and human health: Benefits, challenges, and the road ahead for human-animal interaction. Rev. Sci. Tech. 2018;37:71–82. doi: 10.20506/rst.37.1.2741. [DOI] [PubMed] [Google Scholar]
- 5.Centers of Disease Control and Prevention. [(accessed on 1 July 2021)]; Available online: https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html.
- 6.Smith K.A., Bradley K.K., Stobierski M.G., Tengenslen L.A. Compendium of measures to control Chlamydophila psittaci (formerly Chlamydia psittaci) infection among humans (psittacosis) and pet birds, 2005. J. Am. Vet. Med. Assoc. 2005;226:532–539. doi: 10.2460/javma.2005.226.532. [DOI] [PubMed] [Google Scholar]
- 7.Moroney J.F., Guevara R., Iverson C., Chen F.M., Skelton S.K., Messmer T.O., Plikaytis B., Williams P.O., Blake P., Butler J.C. Detection of chlamydiosis in a shipment of pet birds, leading to recognition of an outbreak of clinically mild psittacosis in humans. Clin. Infect. Dis. 1998;26:1425–1429. doi: 10.1086/516368. [DOI] [PubMed] [Google Scholar]
- 8.Circella E., Pugliese N., Todisco G., Cafiero M.A., Sparagano O.A., Camarda A. Chlamydia psittaci infection in canaries heavily infested by Dermanyssus gallinae. Exp. Appl. Acarol. 2011;55:329–338. doi: 10.1007/s10493-011-9478-9. [DOI] [PubMed] [Google Scholar]
- 9.Kimura R., Hayashi Y., Takeuchi T., Shimizu M., Iwata M., Tanahashi J., Makoto I. Pasteurella multocida septicemia caused by close contact with a domestic cat: Case report and literature review. J. Infect. Chemother. 2004;10:250–252. doi: 10.1007/s10156-004-0331-5. [DOI] [PubMed] [Google Scholar]
- 10.Rybarczyk J., Versteele C., Lernout T., Vanrompay D. Human psittacosis. A review with emphasis on surveillance in Belgium. Acta. Clin. Belg. 2020;75:42–48. doi: 10.1080/17843286.2019.1590889. [DOI] [PubMed] [Google Scholar]
- 11.Woodward D.L., Khakhria R., Johnson W.M. Human salmonellosis associated with exotic pets. J. Clin. Microbiol. 1997;35:2786–2790. doi: 10.1128/jcm.35.11.2786-2790.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padungton P., Kaneene J.B. Campylobacter spp in human, chickens, pigs and their antimicrobial resistance. J. Vet. Med. Sci. 2003;65:161–170. doi: 10.1292/jvms.65.161. [DOI] [PubMed] [Google Scholar]
- 13.Harris J.M. Zoonotic diseases of birds. Vet. Clin. North Am. Small Anim. Pract. 1991;21:1289–1298. doi: 10.1016/S0195-5616(91)50139-X. [DOI] [PubMed] [Google Scholar]
- 14.Moretti A., Agnoletti F., Mancianti F., Nardoni S., Righi C., Moretta I., Morganti G., Papini M. Dermatophytosis in animals: Epidemiological, clinical and zoonotic aspects. G. Ital. Dermatol. Venereol. 2013;148:563–572. [PubMed] [Google Scholar]
- 15.Dipineto L., Rinaldi L., Santaniello A., Sensale M., Cuomo A., Calabria M., Menna L.F., Fioretti A. serological survey for Antibodies to Encephalitozoon cuniculi in pets rabbits in Italy. Zoonoses Public Health. 2008;55:173–175. doi: 10.1111/j.1863-2378.2007.01097.x. [DOI] [PubMed] [Google Scholar]
- 16.Robinson G., Chalmers R.M. The European rabbit (Oryctolagus cuniculus), a source of zoonotic cryptosporidiosis. Zoonoses Public Health. 2010;57:7–8. doi: 10.1111/j.1863-2378.2009.01308.x. [DOI] [PubMed] [Google Scholar]
- 17.Rewatkar S., Deshmukh S., Kumar P., Maske D., Bhangale G. Occurrence of gastrointestinal helminths in rabbits with special reference to importance of giardia spp as parasitic zoonoses. J. Sci. Technol. 2013;2:142. doi: 10.4314/star.v2i3.98754. [DOI] [Google Scholar]
- 18.Broderson J.R., Gluckstein F.P. The Biology of the Laboratory Rabbit. 2nd ed. Academic Press; Cambridge, MA, USA: 1994. Chapter 16-Zoonoses and Occupational health Considerations; pp. 355–365. American College of Laboratory Animal Medicine. [DOI] [Google Scholar]
- 19.Cierniak F., von Arnim F., Heckel G., Ulrich R.G., Groschup M.H., Eiden M. A putative novel hepatitis E virus genotype 3 subtype identified in rabbit, Germany 2016. Viruses. 2021;13:1065. doi: 10.3390/v13061065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fritz M., de Riols de Fonclare D., Garcia D., Beurlet S., Becquart P., Rosolen S.G., Briend-Marchal A., Leroy E.M. First evidence of natural SARS-CoV-2 infection in domestic rabbits. Vet. Sci. 2022;9:49. doi: 10.3390/vetsci9020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mykytyn A.Z., Lamers M.M., Okba N.M., Breugem T.I., Schipper D., van den Doel P.B., van Run P., van Amerongen G., de Waal L., Koopmans M.P.G., et al. Susceptibility of rabbits to SARS-CoV-2. Emerg. Microbes Infect. 2021;10:1–7. doi: 10.1080/22221751.2020.1868951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klotz D., Barth S.A., Baumgärtner W., Hewicker-Trautwein M. Mycobacterium avium subsp. hominissuis Infection in a Domestic Rabbit, Germany. Emerg Infect Dis. 2018;24:596–598. doi: 10.3201/eid2403.171692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sato S., Brinkerhoff R.J., Hollis E., Funada S., Shannon A.B., Maruyama S. Detection of zoonotic bartonella pathogens in Rabbit Fleas, Colorado, USA. Emerg. Infect. Dis. 2020;26:778–781. doi: 10.3201/eid2604.191161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harper M., Boyce J.D., Adler B. Pasteurella multocida pathogenesis:125 years after Pasteur. FEMS Microbiol. Lett. 2006;265:1–10. doi: 10.1111/j.1574-6968.2006.00442.x. [DOI] [PubMed] [Google Scholar]
- 25.Massacci F.R., Magistrali C.F., Cucco L., Curcio L., Bano L., Mangili P., Scoccia E., Bisgaard M., Aalbæk B., Christensen H. Characterization of Pasteurella multocida involved in rabbit infections. Vet. Microbiol. 2018;213:66–72. doi: 10.1016/j.vetmic.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 26.Tang X., Zhao Z., Hu J., Wu B., Cai X., He Q., Chen H. Isolation, antimicrobial resistance, and virulence genes of Pasteurella multocida strains from swine in China. J. Clin. Microbiol. 2009;47:951–958. doi: 10.1128/JCM.02029-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ewers C., Lubke-Becker A., Bethe A., Kiebling S., Filter M., Wieler L.H. Virulence genotype of Pasteurella multocida strains isolated from different hosts with various disease status. Vet. Microbiol. 2006;114:304–317. doi: 10.1016/j.vetmic.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 28.Katoch S., Sharma M., Patil R.D., Kumar S., Verma S. In vitro and in vivo pathogenicity studies of Pasteurella multocida strains harbouring different ompA. Vet. Res. Commun. 2014;38:183–191. doi: 10.1007/s11259-014-9601-6. [DOI] [PubMed] [Google Scholar]
- 29.Hatfaludi T., Al-Hasani K., Boyce J.D., Adler B. Outer membrane proteins of Pasteurella multocida. Vet. Microbiol. 2010;144:1–17. doi: 10.1016/j.vetmic.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 30.Deeb J.B. Ferrets, Rabbits, and Rodents: Clinical Medicine and Surgery. 3rd ed. W.B. Saunders; Saint Louis, MO, USA: 2012. Chapter 17—Respiratory disease and pasteurellosis; pp. 172–182. [Google Scholar]
- 31.Weber D.J., Wolfson J.S., Swartz M.N., Hooper D.C. Pasteurella multocida infections. Report of 34 cases and review of the literature. Medicine. 1984;63:133–154. doi: 10.1097/00005792-198405000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Wilson B.A., Ho M. Pasteurella multocida: From zoonosis to cellular microbiology. Clin. Microbiol. Rev. 2013;26:631–655. doi: 10.1128/CMR.00024-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu W., Chemaly R.F., Tuohy M.J., LaSalvia M.M., Procop G.W. Pasteurella multocida urinary tract infection with molecular evidence of zoonotic transmission. Clin. Inf. Dis. 2003;36:58–60. doi: 10.1086/367649. [DOI] [PubMed] [Google Scholar]
- 34.Abrahamian F.M., Goldstein E.J. Microbiology of animal bite wound infections. Clin. Microbiol. Rev. 2011;24:231–246. doi: 10.1128/CMR.00041-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilkie I.W., Harper M., Boyce J.D., Adler B. Pasteurella multocida: Diseases and Pathogenesis. Springer; Heidelberg/Berlin, Germany: 2012. pp. 1–22. [DOI] [PubMed] [Google Scholar]
- 36.Holst E., Rollof J., Larsson L., Nielsen J.P. Characterization and distribution of Pasteurella species recovered from infected humans. J. Clin. Micobiol. 1992;30:2984–2987. doi: 10.1128/jcm.30.11.2984-2987.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klein N.C., Cunha B.A. Pasteurella multocida pneumonia. Semin. Respir. Infect. 1997;12:54–56. [PubMed] [Google Scholar]
- 38.Townsend K.M., Boyce J.D., Chung J.Y., Frost A.J., Adler B. Genetic organization of Pasteurella multocida cap Loci and development of a multiplex capsular PCR typing system. J. Clin. Microbiol. 2001;39:924–929. doi: 10.1128/JCM.39.3.924-929.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lainson F.A., Thomson N., Rowe H., Langford P.R., Aitchison K.D., Donachie W., Kroll J.S. Occurrence of [copper, zinc]-cofactored Superoxide dismutase in Pasteurella haemolytica and its serotype distribution. FEMS Microbiol. Lett. 1996;142:11–17. doi: 10.1111/j.1574-6968.1996.tb08400.x. [DOI] [PubMed] [Google Scholar]
- 40.Doughty S.W., Ruffolo C.G., Adler B. The type 4 fimbrial subunit gene of Pasteurella multocida. Vet. Microbiol. 2000;72:79–90. doi: 10.1016/S0378-1135(99)00189-3. [DOI] [PubMed] [Google Scholar]
- 41.The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 12.0. [(accessed on 1 January 2022)]. Available online: http://www.eucast.org.
- 42.Clinical Laboratory and Standards Institute M02-A12. Performance Standards for Antimicrobial Disk Susceptibility Tests-Twelfth Edition. [(accessed on 1 January 2015)]. Available online: https://clsi.org.
- 43.Broome R.L., Brooks D.L. Efficacy of enrofloxacin in the treatment of respiratory pasteurellosis in rabbits. Lab. Anim Sci. 1991;41:572–576. [PubMed] [Google Scholar]
- 44.Ujvári B., Weiczner R., Deim Z., Terhes G., Urbán E., Tóth A.R., Magyar T. Characterization of Pasteurella multocida strains isolated from human infections. Comp. Immunol. Microbiol. Infect. Dis. 2019;63:37–43. doi: 10.1016/j.cimid.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 45.Smith E., Miller E., Munoz Aguayo J., Figueroa C.F., Nezworski J., Studniski M., Wileman B., Johnson T. Genomic diversity and molecular epidemiology of Pasteurella multocida. PLoS ONE. 2021;16:e0249138. doi: 10.1371/journal.pone.0249138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jaglic Z., Kucerova Z., Nedbalcova K., Hlozek P., Bartos M. Identification of Pasteurella multocida serogroup F isolates in rabbits. J. Vet. Med. B. 2004;51:467–469. doi: 10.1111/j.1439-0450.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 47.Jekl V. Respiratory disorders in rabbits. Vet. Clin. North Am. Exot. Anim Pract. 2021;24:459–482. doi: 10.1016/j.cvex.2021.01.006. [DOI] [PubMed] [Google Scholar]
- 48.Lennox A.M. Respiratory disease and pasteurellosis. In: Quesenberry K.E., Carpenter J.W., editors. Ferrets, Rabbits, and Rodents. 3rd ed. Volume 41. WB Saunders Co; Philadelphia, PA, USA: 2012. pp. 205–216. [Google Scholar]
- 49.Ferreira T.S., Felizardo M.R., Sena de Gobbi D.D., Gomes C.R., de Lima Nogueira Filsner P.H., Moreno M., Paixao R., de Jesus Pereira J., Moreno A.M. Virulence genes and antimicrobial resistance profiles of Pasteurella multocida strains isolated from rabbits in Brazil. Sci. World. J. 2012;2012:1–6. doi: 10.1100/2012/685028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shirzad Aski H., Tabatabaei M. Occurrence of virulence-associated genes in Pasteurella multocida isolates obtained from different hosts. Microb. Pathog. 2016;96:52–57. doi: 10.1016/j.micpath.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 51.Atashpaz S., Shayegh J., Hejazi M.S. Rapid virulence typing of Pasteurella multocida by multiplex PCR. Res. Vet. Sci. 2009;87:355–357. doi: 10.1016/j.rvsc.2009.04.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.