Abstract
Background
Numerous studies have reported an increase in mental disorders during the COVID-19 pandemic, but the exact reasons for this development are not well understood. In this study we investigate whether pandemic-related occupational and financial changes (e.g., reduced working hours, working from home, financial losses) were associated with increased symptoms of depression and anxiety compared with the situation before the pandemic.
Methods
We analyzed data from the German National Cohort (NAKO) Study. Between May and November 2020, 161 849 study participants answered questions on their mental state and social circumstances. Their responses were compared with data from the baseline survey before the pandemic (2014–2019). Linear fixed-effects models were used to determine whether individual changes in the severity of symptoms of depression (PHQ-9) or anxiety (GAD-7) were associated with occupational/ financial changes (controlling for various covariates).
Results
The prevalence of moderate or severe symptoms of depression and anxiety increased by 2.4% and 1.5%, respectively, during the COVID-19 pandemic compared with the preceding years. The mean severity of the symptoms rose slightly. A pronounced increase in symptoms was observed among those who became unemployed during the pandemic (+ 1.16 points on the depression scale, 95% confidence interval [0.91; 1.41], range 0–27). Increases were also seen for reduced working hours with no short-time allowance, increased working hours, working from home, insecurity regarding employment, and financial strain. The deterioration in mental health was largely statistically explained by the occupational and financial changes investigated in the model.
Conclusion
Depressive symptoms and anxiety disorders increased slightly in the study population during the first year of the COVID-19 pandemic. Occupational and financial difficulties were an essential contributory factor. These strains should be taken into account both in the care of individual patients and in the planning of targeted prevention measures.
The COVID-19 pandemic is a global crisis, impacting the living and working conditions of large numbers of people. Hence, it was suspected early on that the frequency of mental disorders and diseases could increase. (1– 3). From various countries studies with measurements before and during the pandemic have become available, indicating that the state of mental health of the population did indeed deteriorate compared to the situation before the pandemic (4– 9). Multiple potential risk factors for the increase in mental disorders have been discussed. These include social isolation, working from home, home schooling, fear of infection with the SARS-CoV-2 virus, actual infections, and lifestyle changes, such as increased substance use (e.g. alcohol), among others (10– 14). Moreover, collective social crises in general have the potential to put a strain on the mental health of people, even on those who are not directly impacted by their negative effects (15, 16). Furthermore, early empirical data suggest that pandemic-related changes in economic status and employment are associated with deterioration in mental health during the pandemic (17– 19). Factors such fear of becoming unemployed, financial worries and work-related strain due to increased working hours are known risk factors for various types of mental disorders (20– 23). Since economic life was also impaired as a result of the measures that had to be taken to contain the spread of the virus, such strains may have increased and influenced the prevalence of mental health problems. This would be in line with the experiences made during previous economic crises, such as the 2008 global financial crisis, when a population-level mental health decline was observed in many countries (24).
What specific changes actually exert an effect on mental health is difficult to determine, because research into mediating risk factors has rarely been based on longitudinal studies. For this reason, we analyzed data of the prospective, population-based German National Cohort (NAKO) Study to find out to what extent pandemic-related changes were associated with an increase in depressive and anxiety-related symptoms during the first wave of the COVID-19 pandemic (6). Our study focused on work-related changes and changes in income. In addition, sociodemographic, health-related and COVID-19-specific factors were taken into account as covariates. This research approach aimed to identify specific risks that should receive special attention in the provision of care during the current and in future crises and which could be the focus of supporting, mental health-promoting preventive actions, in addition to the required infection control measures.
Methods
Data
The population-based German National Cohort (NAKO) Study is with 205 185 participants Germany’s largest epidemiological cohort study. The baseline survey was conducted in 18 study centers in 13 German federal states (“Länder”) between 2014 and 2019. Random samples of the general population aged 20 to 69 years were drawn by the local registration offices and then used to recruit the study participants. The mean response rate was 18% (25). At each of the study centers, an ethics committee approval was available and the respondents agreed in writing to participate in the study after an informed consent discussion. A detailed description of the study design can be found in earlier publications (25– 27).
A special survey was conducted upon the onset of the COVID-19 pandemic (6). Participants with e-mail addresses received a link to an online survey, while the remaining participants were sent paper questionnaires. In both cases, the mailing took place between 30 April 2020 and 15 May 2020. Individuals known to be deceased or to have withdrawn their consent were excluded. A total of 197 834 individuals were contacted; of these 161 892 responded up to and including 30 November 2020 (response rate: 81.8%). 105 questionnaires of the special survey were not used because the dates of completion were invalid. Thus, the analyses below are based on 161 787 individuals for whom one observation before and one during the pandemic were available.
Instruments
During the baseline survey, sociodemographic data were obtained by means of a standardized interview and mental health information from a touchscreen questionnaire. In the COVID-19 special survey, online questionnaires and mailed paper questionnaires were used. The variables selected for the survey are outlined below and more detailed descriptions are provided in the eMethods section.
Mental disorders: Symptoms of depression were obtained using the Patient Health Questionnaire (PHQ-9) which surveyed the frequency of occurrence of nine symptoms over the last two weeks (28). Responses were added up to create a total score (range: 0–27, high values corresponded to high severity). Moderate or severe symptoms of depression were defined as scores ≥= 10. Anxiety was measured using the Generalized Anxiety Disorder Scale-7 (GAD-7) which measures the frequency of occurrence of seven symptoms of generalized anxiety disorder during the last four weeks (in the NAKO version) (29). Here, again, a total was calculated (range: 0–21) and moderate or severe symptoms of anxiety were defined as scores ≥= 10.
Work-related changes: Three indicators were used. Changes in employment situation were identified by first determining the employment status at both measurement points based on the workforce concept and then differentiating between employed, unemployed and inactive (pension, retirement, study, other) persons (30). Furthermore, pandemic-related work-specific changes were queried directly and combined with the employment status. In the follow-up survey, the options listed below were added to the category “working“: change of job, increase in working hours, reduction in working hours with and without short-time allowance, loss of job. In the “unemployed“ category, it was differentiated between unemployment before and due to the pandemic situation. Change in perceived job insecurity was the second indicator measured at both time points (31). Its four-item response scale was dichotomized and inactive persons were assigned to the “no job insecurity” category. The third indicator was the response to the question whether due to the pandemic working from home was required on all or some days.
Financial changes: As part of the COVID-19 special survey, the respondents reported whether their household‘s financial situation had improved, worsened, or remained the same since the start of the pandemic.
Covariates: A variety of characteristics were included in the study as potential confounders: age, gender, type of household, high-risk contact with a SARS-CoV-2 infected person, own SARS-CoV-2 infection, and self-reported health.
Statistical analysis
First, PHQ-9 and GAD-7 means as well as rates of occurrence of moderate or severe symptoms of depression or anxiety (cut-off ≥= 10) were calculated across the survey years. Given the differences in the sociodemographic characteristics of the respondents in the survey years of the baseline survey, adjustments were made for age, gender and study center. Changes in mental health were analyzed using linear panel data models with fixed effects (FE models). FE models look at intrapersonal changes of the dependent variable—in this case the symptoms— over time and relate them to changes in an independent variable, such as employment status. The intraindividual comparison ensures that effect estimates of FE models are controlled for both observed and unobserved time-constant confounders (characteristics with the same expression at all measurement points, such as gender) (32). For each outcome, three models were calculated. The first model estimated the individual changes in depression/anxiety during the pandemic in comparison with the baseline survey without adjustment. The second model included covariates (see above), complemented by indicators for occupational and financial changes in the final model. Missing values for dependent and independent variables were imputed, using a predictive mean matching method (etable 1) (33). In addition, because negative occupational and/or financial changes may have different effects in men and women, separate models were calculated by gender.
eTable 1. Frequency of missing data.
| Missing | Complete | Total | ||||
| n | % | n | % | n | % | |
| PHQ-9 (baseline survey) | 9 207 | 5.7 | 152 580 | 94.3 | 161 787 | 100.0 |
| PHQ-9 (COVID-19 survey) | 8 668 | 5.4 | 153 119 | 94.6 | 161 787 | 100.0 |
| GAD-7 (baseline survey) | 9 454 | 5.8 | 152 333 | 94.2 | 161 787 | 100.0 |
| GAD-7 (COVID-19 survey) | 8 390 | 5.2 | 153 397 | 94.8 | 161 787 | 100.0 |
| Positive SARS-CoV-2 test | 2 463 | 1.5 | 159 324 | 98.5 | 161 787 | 100.0 |
| Change to working from home | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Household type (baseline survey) | 91 | 0.1 | 161 696 | 99.9 | 161 787 | 100.0 |
| Household type (COVID-19 survey) | 3 189 | 2.0 | 158 598 | 98.0 | 161 787 | 100.0 |
| Employment status (baseline survey) | 145 | 0.1 | 161 642 | 99.9 | 161 787 | 100.0 |
| Employment status (COVID-19 survey) | 8 862 | 5.5 | 152 925 | 94.5 | 161 787 | 100.0 |
| High-risk contact with an infected person | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| General health (baseline survey) | 4 649 | 2.9 | 157 138 | 97.1 | 161 787 | 100.0 |
| General health (COVID-19 survey) | 2 579 | 1.6 | 159 208 | 98.4 | 161 787 | 100.0 |
| Job insecurity (baseline survey) | 12 653 | 7.8 | 149 134 | 92.2 | 161 787 | 100.0 |
| Job insecurity (COVID-19 survey) | 8 228 | 5.1 | 153 559 | 94.9 | 161 787 | 100.0 |
| Change in financial situation | 5 186 | 3.2 | 156 601 | 96.8 | 161 787 | 100.0 |
| Major occupational group (KldB 2010) | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| Occupational skill level (KldB 2010) | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| Occupational management responsibility (KldB 2010) | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| Occupational segment (KldB 2010) | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| Occupational sector (KldB 2010) | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| Major occupational group (ISCO-08) | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| Sub-major occupational group (ISCO-08) | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| Occupational sub-group (ISCO-08) | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| Skill level (ISCO-08) | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| System-relevant occupation | 8 279 | 5.1 | 153 508 | 94.9 | 161 787 | 100.0 |
| International Socio-Economic Index of Occupational Status (ISEI) | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| Standard International Occupational Prestige Scale | 9 498 | 5.9 | 152 289 | 94.1 | 161 787 | 100.0 |
| Self-employment | 3 895 | 2.4 | 157 892 | 97.6 | 161 787 | 100.0 |
| Relative household equivalence income | 10 098 | 6.2 | 151 689 | 93.8 | 161 787 | 100.0 |
| Civil servant | 3 895 | 2.4 | 157 892 | 97.6 | 161 787 | 100.0 |
| Age in years (baseline survey) | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Age in years (COVID-19 survey) | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Date of survey | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Interval between baseline survey and COVID-19 survey | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Gender | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Region of study center | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Person-time under risk | 0 | 0.0 | 161 787 | 100.0 | 161 787 | 100.0 |
| Migration background | 59 | 0.0 | 161 728 | 100.0 | 161 787 | 100.0 |
| Marital status | 84 | 0.1 | 161 703 | 99.9 | 161 787 | 100.0 |
| Partnership | 263 | 0.2 | 161 524 | 99.8 | 161 787 | 100.0 |
| Occupation | 3 895 | 2.4 | 157 892 | 97.6 | 161 787 | 100.0 |
| Weekly working hours | 40 691 | 25.2 | 121 096 | 74.8 | 161 787 | 100.0 |
GAD-7, Generalized Anxiety Disorder Scale-7; ISCO, International Standard Classification of Occupations; KldB, German Classification of Occupations (“Klassifikation der Berufe”); n, number of respondents;
PHQ-9, Patient Health Questionnaire
For the sensitivity analyses, both symptom scales were dichotomized (cut-off ≥= 10) to find out whether there were changes in the proportions of moderate or severe symptoms. Associations were investigated using a multi-level model with Poisson distribution and robust standard errors to calculate the relative risks (RR) for the probability of mental disease during the pandemic. Furthermore, the primary analysis of the changes in mean symptom severity was repeated, but in a stepwise fashion, adding the main effect, occupational changes, financial strains, and finally the covariates to uncover correlations among the dependent variables and to evaluate whether adjusting for covariates has changed the main results.
All calculations were performed using the statistical software package Stata 16.1 MP (64-bit, StataCorp LLC, College Station, TX, USA).
Results
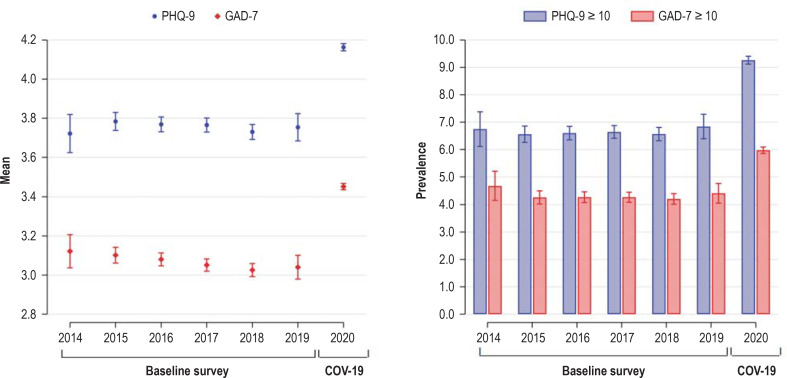
Table 1 shows the characteristics of the NAKO study participants at both survey times. Between the two surveys, the participants had advanced in age by almost three years on average, which corresponds to the average interval between the baseline survey and the special survey. The mean severity of symptoms of depression and anxiety increased slightly during this period. In addition, the proportion of participants with moderate or severe symptoms of depression and anxiety disorder increased from 7.1% to 9.5% (+2.4) and 4.8% to 6.3% (+1.5), respectively.
Table 1. Description of the participants according to sociodemographic and COVID-19-related characteristics.
| Baseline survey (2014 – 2019) | COVID-19 survey (2020) | |||
| n/(M) | %/(SD) | n/(M) | %/(SD) | |
| PHQ-9 (depressive symptoms) | ||||
| (M, SD; range: 0–27) | (3.81) | (3.62) | (4.11) | (4.03) |
| Proportion with a score ≥ 10 | 11 544 | 7.1 | 15 399 | 9.5 |
| GAD-7 (anxiety disorder) | ||||
| (M, SD; range: 0–21) | (3.11) | (3.16) | (3.40) | (3.54) |
| Proportion with a score ≥ 10 | 7 688 | 4.8 | 10 161 | 6.3 |
| Age (in years) | ||||
| (M, SD) | (50.4) | (12.6) | (53.1) | (12.9) |
| Age groups: | ||||
| 19–29 years | 14 338 | 8.9 | 9.699 | 6.0 |
| 30–39 years | 16 048 | 9.9 | 16 715 | 10.3 |
| 40–49 years | 41 766 | 25.8 | 32 189 | 19.9 |
| 50–59 years | 44 223 | 27.3 | 46 403 | 28.7 |
| 60–69 years | 41 951 | 25.9 | 42 009 | 26.0 |
| 70–79 years | 3 461 | 2.1 | 14 772 | 9.1 |
| Gender | ||||
| Male | 77 773 | 48.1 | 77 773 | 48.1 |
| Female | 84 014 | 51.9 | 84 014 | 51.9 |
| Type of household | ||||
| One-person household | 30 497 | 18.9 | 29 435 | 18.2 |
| Multiple-person household without children (<14 years) | 98 500 | 60.9 | 104 816 | 64.8 |
| Multiple-person household with children (<14 years) | 32 790 | 20.3 | 27 536 | 17.0 |
| High-risk contact with an infected person | ||||
| No | 161 787 | 100.0 | 156 391 | 96.7 |
| Yes | 0 | 0.0 | 5 396 | 3.3 |
| Tested positive for SARS-CoV-2 virus | ||||
| No | 161 787 | 100.0 | 161 295 | 99.7 |
| Yes | 0 | 0.0 | 492 | 0.3 |
| Poor general health | ||||
| No | 145 304 | 89.8 | 148 486 | 91.8 |
| Yes | 16 483 | 10.2 | 13 301 | 8.2 |
| Changes in employment situation | ||||
| Working: No pandemic-related change | 114 786 | 71.0 | 68 765 | 42.5 |
| Working: Change of job | 0 | 0.0 | 620 | 0.4 |
| Working: increased working hours | 0 | 0.0 | 11 233 | 6.9 |
| Working: Reduced working hours with short-time allowance | 0 | 0.0 | 13 417 | 8.3 |
| Working: Reduced working hours without short-time allowance | 0 | 0.0 | 19 066 | 11.8 |
| Unemployed prior to Corona | 3 968 | 2.5 | 2 835 | 1.8 |
| Unemployed due to Corona | 0 | 0.0 | 828 | 0.5 |
| Inactive person (pension, retirement, study) | 43 033 | 26.6 | 45 023 | 27.8 |
| Job Insecurity | ||||
| Low or not employed | 150 126 | 92.8 | 144 139 | 89.1 |
| High | 11 661 | 7.2 | 17 648 | 10.9 |
| Working from home since the pandemic | ||||
| No | 161 787 | 100.0 | 117 613 | 72.7 |
| Yes, always or on some days | 0 | 0.0 | 44 174 | 27.3 |
| Change in financial situation since the pandemic | ||||
| No change | 161 787 | 100.0 | 124 364 | 76.9 |
| Improvement | 0 | 0.0 | 5 174 | 3.2 |
| Deterioration | 0 | 0.0 | 32 249 | 19.9 |
| Total | 161 787 | 100.0 | 161 787 | 100.0 |
GAD-7, Generalized Anxiety Disorder Scale-7; M, mean;
PHQ-9, Patient Health Questionnaire; SD, standard deviation
Figure 1 graphically depicts the means of the symptom scales and the frequencies of moderate or severe symptoms for each of the years of the baseline survey (2014–2019) and for the COVID-19 special survey (2020).
Figure 1.
Mental health in the NAKO baseline survey and the COVID-19 special survey based on PHQ-9 (depressive symptoms) and GAD-7 (anxiety disorder). Means are shown on the left and frequencies are shown on the right by cut-off for moderate or severe disorder (each with 95% confidence interval); n = 161 787. The years 2014–2019 comprise the baseline survey (cross-sectional changes), the year 2020 comprise the COVID-19 special survey. The estimates were adjusted for age, gender and study center.
COV-19, COVID-19 special survey; GAD-7, Generalized Anxiety Disorder Scale-7; PHQ-9, Patient Health Questionnaire
Table 2 shows the results of the FE models with the correlation measures for all variables in the final model. A pronounced increase in severity on the PHQ-9 and GAD-7 scales was observed among those who became unemployed during the pandemic. For example, the scale value for depressive symptoms increase on average by 1.16 scale points. Likewise, a pandemic-related deterioration of the financial situation, job insecurity, change to working from home, increased working hours, as well as reduced working hours with no short-time allowance were associated with an increase in symptoms. In contrast, mental health improved with reduced working hours, when a short-time allowance was received, as well as with a change to inactive status. In general, mental health deteriorated especially in younger and middle-aged groups and in the presence of poor self-reported health.
Table 2. Changes in mental health in the NAKO study during the COVID-19 pandemic (2020) compared to the previous period (2014–2019).
| PHQ-9 (scores) | GAD-7 (scores) | |||||
| b | [95% CI] | p | b | [95% CI] | p | |
| Wave | ||||||
| Baseline survey | Reference category | Reference category | ||||
| COVID-19 survey | 0.03 | [0.00; 0.06] | 0.033 | 0.06 | [0.03; 0.08] | <0.001 |
| Occupational and financial changes during the pandemic | ||||||
| Change in employment situation | ||||||
| Working – no pandemic-related change | Reference category | Reference category | ||||
| Working – change of job | 0.29 | [−0.00; 0.57] | 0.051 | 0.38 | [0.12; 0.63] | 0.004 |
| Working – increased working hours | 0.78 | [0.71; 0.85] | <0.001 | 0.71 | [0.65; 0.77] | <0.001 |
| Working – reduced working hours with short-time allowance | −0.17 | [−0.24; −0.10] | <0.001 | −0.20 | [−0.26; −0.13] | <0.001 |
| Working – reduced working hours without short-time allowance | 0.09 | [0.03; 0.15] | 0.002 | 0.13 | [0.08; 0.18] | <0.001 |
| Unemployed prior to Corona | 0.61 | [0.51; 0.71] | <0.001 | 0.52 | [0.43; 0.61] | <0.001 |
| Unemployed due to Corona | 1.16 | [0.91; 1.41] | <0.001 | 0.66 | [0.44; 0.88] | <0.001 |
| Inactive person (pension, retirement, study) | −0.13 | [−0.18; −0.07] | <0.001 | −0.12 | [−0.17; −0.08] | <0.001 |
| Job Insecurity | ||||||
| High (reference category: ”low or not employed” | 0.77 | [0.72; 0.82] | <0.001 | 0.69 | [0.65; 0.74] | <0.001 |
| Working from home | ||||||
| Yes, always or on some days (reference category: “No“) | 0.41 | [0.36; 0.45] | <0.001 | 0.28 | [0.25; 0.32] | <0.001 |
| Change in financial situation | ||||||
| No change | Reference category | Reference category | ||||
| Improvement | −0.15 | [−0.25; −0.05] | 0.004 | −0.15 | [−0.24; −0.06] | 0.001 |
| Deterioration | 0.81 | [0.76; 0.86] | <0.001 | 0.75 | [0.71; 0.80] | <0.001 |
| Covariates | ||||||
| Age | ||||||
| 19–29 years | Reference category | Reference category | ||||
| 30–39 years | 0.12 | [0.01; 0.23] | 0.026 | 0.06 | [−0.03; 0.16] | 0.198 |
| 40–49 years | 0.22 | [0.06; 0.38] | 0.008 | 0.17 | [0.03; 0.31] | 0.018 |
| 50–59 years | 0.14 | [−0.04; 0.32] | 0.128 | 0.15 | [−0.01; 0.30] | 0.070 |
| 60–69 years | −0.23 | [−0.43; −0.03] | 0.023 | −0.11 | [−0.28; 0.07] | 0.238 |
| 70–79 years | −0.47 | [−0.68; −0.25] | <0.001 | −0.33 | [−0.52; −0.14] | 0.001 |
| Type of household | ||||||
| One-person household | Reference category | Reference category | ||||
| Multiple-person household without children (<14 years) | −0.18 | [−0.24;−0.13] | <0.001 | 0.07 | [0.02; 0.12] | 0.005 |
| Multiple-person household with children (< 14 years) | −0.13 | [−0.21;−0.05] | 0.001 | 0.22 | [0.15; 0.29] | <0.001 |
| High-risk contact with an infected person | ||||||
| Yes (reference category: “No“) | 0.24 | [0.14; 0.34] | <0.001 | 0.24 | [0.14; 0.34] | <0.001 |
| Tested positive for SARS-CoV-2 virus | ||||||
| Yes (reference category: “No“) | −0.03 | [−0.35; 0.30] | 0.865 | −0.03 | [−0.35; 0.30] | 0.865 |
| General health | ||||||
| Poor (reference category: “Good”) | 2.26 | [2.20; 2.31] | <0.001 | 2.26 | [2.20; 2.31] | <0.001 |
| Model information | ||||||
| R2 (intrapersonal) | 0.072 | 0.062 | ||||
| R2 (interpersonal) | 0.201 | 0.148 | ||||
| R2 (total) | 0.156 | 0.117 | ||||
| Individuals (n) | 161 787 | 161 787 | ||||
| Observations (n) | 323 574 | 323 574 | ||||
Mental health measured using PHQ-9 (depressive symptoms) and GAD-7 (anxiety disorder). The analyses are based on a linear fixed-effects model with jointly adjusted regression coefficient b.
Positive vales indicate deterioration of mental health (increase in symptom value), while negative values indicate improvement. The total R-squared value indicates the weighted mean of the explained variance between and within persons.
b, adjusted regression coefficient; GAD-7, Generalized Anxiety Disorder Scale-7; CI, confidence interval;
NAKO, German National Cohort Study; p, p-value; PHQ-9, Patient Health Questionnaire
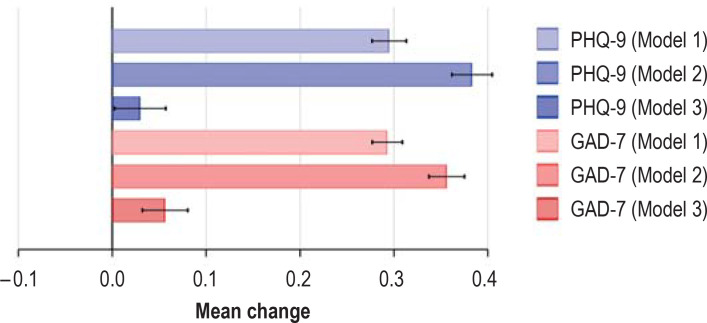
Figure 2 shows the change in mental health before and during the pandemic after stepwise control for covariates and independent variables. A comparison of the models shows that the mean symptom increase from the baseline survey to the COVID-19 survey, which is still discernable in Model 2, becomes significant after statistical control of occupational and financial changes. Thus, this increase is statistically almost entirely explained by these factors.
Figure 2.
Change in mental health (means of PHQ-9 and GAD-7 scales) during the COVID-19 pandemic compared to the previous period; in Model 1 non-adjusted, in Model 2 adjusted for age, household composition, general health, high-risk SARS-CoV-2 contact and infection, and in model 3 additionally adjusted for changes in employment situation, insecurity regarding employment, working from home, and change in financial situation. GAD-7, Generalized Anxiety Disorder Scale-7; PHQ-9, Patient Health Questionnaire
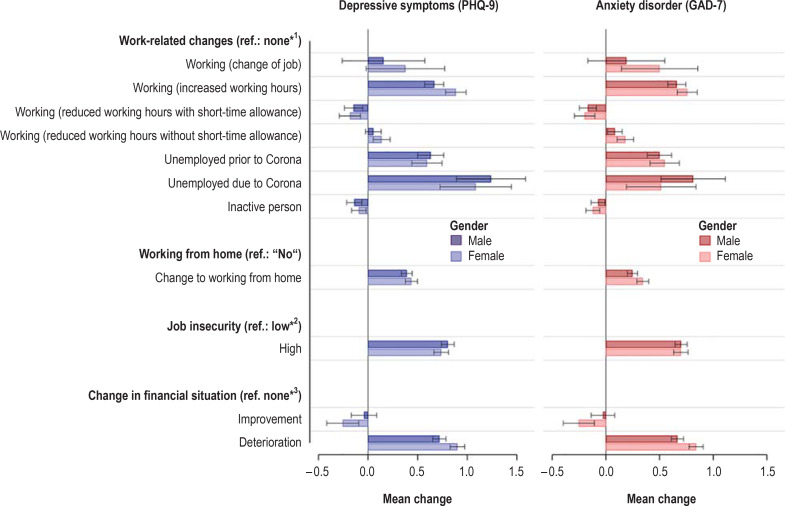
The eFigure shows the measures of association for occupational and financial changes in respect to mental health, stratified by gender. In general, the correlations were consistent for both sexes. However, in women increased working hours and a deteriorated financial situation had a greater negative impact on mental health. In contrast, becoming unemployed during the pandemic was more strongly associated with poorer mental health among men.
eFigure.
Associations between social and occupational changes and change in the severity of mental symptoms during the COVID-19 pandemic, stratified by gender and adjusted for covariates (see Table 2).
GAD-7, Generalized Anxiety Disorder Scale-7; PHQ-9, Patient Health Questionnaire; ref., reference category.
*1 Work-related changes (reference category: ”no change“)
*2 Job insecurity (reference category: ”low or not employed”)
*3 Change in financial situation (reference category: ”no change“)
Sensitivity analyses
eTable 2 shows results of a Poisson regression analysis based on cut-off values for moderate or severe mental disorders. While there are only minor deviations from the FE model, the effects of protective factors are less pronounced. Sensitivity analyses of the main effects of work-related changes—without simultaneously taking financial strain into account—showed that reduced working hours (with and without short-time allowance) generally affected mental health, consistent with a mediating effect of increased financial strain (eTable 3, eTable 4). An analysis of the main effects of financial and occupational changes without adjustment for covariates yielded comparable results (eTable 3, eTable 4).
eTable 3. Linear fixed-effects models for changes in PHQ-9 (depressive symptoms) in the NAKO study during the COVID-19 pandemic (2020) compared to the previous period (2014–2019)*1.
| M1 | M2 | M3 | M4 | |||||
| b | [95% CI] | b | [95% CI] | b | [95% CI] | b | [95% CI] | |
| Wave | ||||||||
| Baseline survey | Ref. | Ref. | Ref. | Ref. | ||||
| COVID-19 survey | 0.29*** | [0.28; 0.31] | 0.02 | [–0.00; 0.04] | –0.07*** | [–0.10; –0.05] | 0.03* | [0.00; 0.06] |
| Occupational and financial changes during the pandemic | ||||||||
| Change in employment situation | ||||||||
| Working – no pandemic-related change | Ref. | Ref. | Ref. | |||||
| Working – change of job | 0.32* | [0.03; 0.61] | 0.25 | [–0.04; 0.55] | 0.29 | [–0.00; 0.57] | ||
| Working – increased working hours | 0.86*** | [0.79; 0.93] | 0.83*** | [0.75; 0.90] | 0.78*** | [0.71; 0.85] | ||
| Working – reduced working hours with short-time allowance | 0.24*** | [0.17; 0.31] | –0.16*** | [–0.23; –0.08] | –0.17*** | [–0.24; –0.10] | ||
| Working – reduced working hours without short-time allowance | 0.31*** | [0.25; 0.37] | 0.10*** | [0.04; 0.16] | 0.09** | [0.03; 0.15] | ||
| Unemployed prior to Corona | 0.76*** | [0.66; 0.86] | 0.70*** | [0.60; 0.81] | 0.61*** | [0.51; 0.71] | ||
| Unemployed due to Corona | 1.64*** | [1.39; 1.90] | 1.19*** | [0.93; 1.45] | 1.16*** | [0.91; 1.41] | ||
| Inactive person (pension, retirement, study) | –0.14*** | [–0.19; –0.08] | –0.15*** | [–0.20; –0.10] | –0.13*** | [–0.18; –0.07] | ||
| Job insecurity | ||||||||
| High (ref.: “low or not employed“) | 0.95*** | [0.90; 1.00] | 0.80*** | [0.75; 0.85] | 0.77*** | [0.72; 0.82] | ||
| Working from home | ||||||||
| Yes, always or on some days (ref.: “No“) | 0.45*** | [0.41; 0.49] | 0.45*** | [0.41; 0.49] | 0.41*** | [0.36; 0.45] | ||
| Change in financial situation | ||||||||
| No change | Ref. | Ref. | ||||||
| Improvement | –0.13* | [–0.24; –0.03] | –0.15** | [–0.25; –0.05] | ||||
| Deterioration | 0.82*** | [0.77; 0.87] | 0.81*** | [0.76; 0.86] | ||||
| Model information | ||||||||
| R2 (intrapersonal) | 0.006 | 0.026 | 0.033 | 0.072 | ||||
| R2 (interpersonal) | 0.000 | 0.032 | 0.039 | 0.204 | ||||
| R2 (total) | 0.001 | 0.028 | 0.035 | 0.157 | ||||
| Individuals (n) | 161 787 | 161 787 | 161 787 | 161 787 | ||||
| Observations (n) | 323 574 | 323 574 | 323 574 | 323 574 | ||||
*1 Model 1: Main effect not adjusted; Model 2: main effect and occupational and financial changes; Model 3: additionally adjusted for financial strains;
Model 4: additionally adjusted for the following covariates: age, household composition, general health, SARS-CoV-2 high-risk contact and SARS-CoV-2 infection
Significance level: * p<0.05; ** p<0.01; *** p<0.001. The total R-squared value indicates the weighted mean of the explained variance between and within individuals.
b, adjusted regression coefficient; CI, confidence interval; M, model; NAKO, German National Cohort Study;
PHQ-9, Patient Health Questionnaire Patient Health Questionnaire; ref., reference category.
eTable 4. Linear fixed-effects models for change of GAD-7 (anxiety disorder) in the NAKO study during the COVID-19 pandemic (2020) compared to the previous period (2014–2019)*1.
| M1 | M2 | M3 | M4 | |||||
| b | [95% CI] | b | [95% CI] | b | [95% CI] | b | [95% CI] | |
| Wave | ||||||||
| Baseline survey | Ref. | Ref. | Ref. | Ref. | ||||
| COVID-19 survey | 0.29*** | [0.28; 0.31] | 0.06*** | [0.04; 0.08] | –0.02* | [–0.04; –0.00] | 0.06*** | [0.03; 0.08] |
| Occupational and financial changes during the pandemic | ||||||||
| Change in employment situation | ||||||||
| Working – no pandemic-related change | Ref. | Ref. | Ref. | |||||
| Working – change of job | 0.42** | [0.16; 0.68] | 0.36** | [0.11; 0.62] | 0.38** | [0.12; 0.63] | ||
| Working – increased working hours | 0.78*** | [0.72; 0.85] | 0.75*** | [0.69; 0.82] | 0.71*** | [0.65; 0.77] | ||
| Working – reduced working hours with short-time allowance | 0.19*** | [0.13; 0.25] | –0.18*** | [–0.24; –0.12] | –0.20*** | [–0.26; –0.13] | ||
| Working – reduced working hours without short-time allowance | 0.34*** | [0.28; 0.39] | 0.14*** | [0.09; 0.19] | 0.13*** | [0.08; 0.18] | ||
| Unemployed prior to Corona | 0.64*** | [0.55; 0.73] | 0.59*** | [0.50; 0.68] | 0.52*** | [0.43; 0.61] | ||
| Unemployed due to Corona | 1.11*** | [0.89; 1.33] | 0.69*** | [0.46; 0.91] | 0.66*** | [0.44; 0.88] | ||
| Inactive person (pension, retirement, study) | –0.13*** | [–0.17; –0.08] | –0.14*** | [–0.18; –0.09] | –0.12*** | [–0.17; –0.08] | ||
| Job insecurity | ||||||||
| High (ref.: “low or not employed“) | 0.86*** | [0.81; 0.90] | 0.71*** | [0.67; 0.76] | 0.69*** | [0.65; 0.74] | ||
| Working from home | ||||||||
| Yes, always or on some days (ref.: “No“) | 0.32*** | [0.28; 0.36] | 0.32*** | [0.29; 0.36] | 0.28*** | [0.25; 0.32] | ||
| Change in financial situation | ||||||||
| No change | Ref. | Ref. | ||||||
| Improvement | –0.13** | [–0.22; –0.04] | –0.15** | [–0.24; –0.06] | ||||
| Deterioration | 0.76*** | [0.72; 0.81] | 0.75*** | [0.71; 0.80] | ||||
| Model information | ||||||||
| R2 (intrapersonal) | 0.008 | 0.028 | 0.035 | 0.062 | ||||
| R2 (interpersonal) | 0.000 | 0.035 | 0.043 | 0.150 | ||||
| R2 (total) | 0.002 | 0.030 | 0.037 | 0.118 | ||||
| Individuals (n) | 161 787 | 161 787 | 161 787 | 161 787 | ||||
| Observations (n) | 323 574 | 323 574 | 323 574 | 323 574 | ||||
*1 Model 1: Main effect not adjusted; Model 2: main effect and occupational and financial changes; Model 3: additionally adjusted for financial strains;
Model 4: additionally adjusted for the following covariates: age, household composition, general health, SARS-CoV-2 high-risk contact and SARS-CoV-2 infection
Significance level: * p<0.05; ** p<0.01; *** p<0.001. The total R-squared value indicates the weighted mean of the explained variance between and within individuals.
b, adjusted regression coefficient; GAD-7, Generalized Anxiety Disorder Scale-7;
CI, confidence interval; M, model; NAKO, German National Cohort Study; ref., reference category
Discussion
This study investigated whether, and to what extent, occupational and financial changes due to the COVID-19 pandemic in spring and summer of 2020 were associated with increased severity of symptoms of depression and anxiety in 161 787 participants of the German National Cohort (NAKO) Study. Mental health was affected by pandemic-related job loss, reduced working hours with no short-time allowance, increased working hours, change to working from home, increased job insecurity, and deterioration of the financial situation. Overall, the increase in mental health problems was found significantly reduced after statistical control for work-related changes and financial strain. This suggests that the mean increase in symptom severity during the pandemic was largely due to an increase in occupational and financial strains. In general, this finding supports the importance of a stable employment and income situation for the mental health of individuals, not only in times of crisis.
For the most part, the results are in line with the current state of research. In particular, unemployment, perceived job insecurity and financial strain are established risk factors for impaired mental health (20– 22). Likewise, previous studies have demonstrated a slight increase in depressive symptoms associated with long working hours (34). Interestingly, we were able to show that the opposite, i.e. reduced working hours, were also associated with increased symptoms. However, these symptoms did not increase when short-time allowance was received and no financial strain was reported. This suggests that short-time allowance as a resource may have been effective. During the pandemic, other forms of social security, such as unemployment benefits, produced similar effects (35, 36). Also worth mentioning is the finding that working from home was also associated with increased mental symptoms. This association was previously known primarily from data of cross-sectional studies (37). As expected, our analysis also found known gender differences, with a higher prevalence of mental symptoms among women. However, the strength of the associations between mental symptoms and changes in professional and everyday life was similar for both sexes.
Limitations and strengths
Methodological limitations should be considered, when interpreting the results of our study. It is important to note that the NAKO sample is not representative of the general population in Germany (27). Even though the study participants were randomly selected, recruitment was limited to 18 centers in Germany. In addition, the baseline survey participation rate is low. While the low participation rate is unlikely to have an impact on measures of association, it prevents the generalization of incidence/prevalence rates to the total population of Germany. In terms of content, the study is limited by the fact that only a small number of changes were assessed due to the limited scope of the COVID-19 survey. Our study’s focus on professional life and financial situation means that other changes, for example in the areas of private contacts and recreational activities, are disregarded. Apart from the high significance of the studied social changes for the increase in mental health problems, the moderate R-squared value (<0.2) suggests that the model variables explain only a limited proportion of the total symptom severity variance over time. Another limitation of the study design is that the COVID-19 survey was conducted during and shortly after the first wave of the pandemic in spring and summer of 2020. It is conceivable that the deterioration of mental health leveled off over the further course of the pandemic or—quite the opposite—progressed even further.
The strengths of the study include the standardized pre-post measurement of depressive symptoms and generalized anxiety as well as the longitudinal study design in combination with FE modelling, which assessed intraindividual changes in mental health during the pandemic. Its estimate is robust to time-constant confounders. Another advantage of our study is the large population-based sample. Many previous studies have focused on subpopulations, such as the elderly, making it difficult to produce generalizable statements.
Conclusion
Our study shows that pandemic-related financial and occupational changes were associated with increased mental strain on the study participants. Whether this association persists in the long term remains to be determined by future studies. However, it is becoming obvious that the mental health of the population requires special attention in times of social crises. Our results suggest that the economic and work-related fallout of the pandemic may lead to an increased need for psychotherapeutic services. Key individual risk factors for need of psychotherapy include experiences of job loss and job insecurity as well as financial strain, but also strain due to changes how the work is organized (e.g., reduced working hours or working from home). Thus, these factors could be used to make adjustments aimed at cushioning crisis-related effects on the health of the population. Partial results of this analysis suggest that social security measures could help mitigate negative effects of the pandemic on mental health.
Supplementary Material
eMethods
Instruments
During the baseline survey for the German National Cohort (NAKO) Study, a wide variety of data, including clinical examinations and biospecimens, were collected. For this analysis, basic sociodemographic data obtained in a standardized interview conducted by trained study staff as well as basic information on mental health from a touchscreen questionnaire completed in the survey center were used. The COVID-19 special survey was conducted using online questionnaires (option selected by about two-third of the participants) or paper questionnaires sent by mail (option selected by about one-third of the participants).
Dependent variable/outcome
Mental disorders: At both survey times, depressive symptoms were recorded using the Patient Health Questionnaire (German: Gesundheitsfragebogen für Patienten; PHQ-9) and symptoms of anxiety using the Generalized Anxiety Disorder Scale-7 (German: Skala zur Messung der Generalisierten Angststörung; GAD-7). The PHQ-9 consists of nine questions querying the frequency of depressive symptoms (e.g., dejection, listlessness) within the last two weeks (28). These questions are summed to a total score (range: 0–27), where high scores represent higher severity. A score of 10 or more is considered moderate or severe symptoms of depression. The GAD-7 measures the frequency of seven symptoms of generalized anxiety over the last four weeks (e.g., nervousness, worries) (29). Here, again, a total is calculated (range: 0–21) and moderate or severe symptoms of anxiety are defined as scores of 10 or more.
Occupational and financial changes
Changes in employment situation: Changes were identified based on the comparison of employment status before the outbreak of the COVID 19 pandemic and during its course. First, the employment status at both measurement points was determined based on the workforce concept which differentiates between employed, unemployed and inactive persons (pension, retirement, study, other) (30). The special survey also covered work-specific changes due to the economic consequences of the pandemic („Did one or more of the following changes occur due to the impact of the coronavirus pandemic?“). This information was combined with the employment status to reflect changes. In the follow-up survey, the options listed below were added to the category “working“: change of job, increased working hours, reduced working hours with short-time allowance, and reduced working hours without short-time allowance. When both a change of job and a change in working hours were reported, we prioritized the latter. It was differentiated between two types of the “unemployed” category. Participants whose unemployment (unemployment benefit I or II) had already occurred before the start of the pandemic were assigned to the “unemployed prior to corona” category. Persons who reported to have become unemployed due to the corona pandemic were assigned to the “unemployed due to corona“ category.
Job insecurity
The perceived insecurity regarding employment as a measure for the likelihood of job loss (31) was measured at both time points with the following question: “My own job/professional existence is at risk: (1) do not agree at all, (2) do not agree, (3) agree, (4) agree completely“. From this, a binary variable with the expressions “no job insecurity” (answers 1–2) and “job insecurity“ (answers 3–4) was created. Inactive persons were assigned to the first category.
Working from home
The employed participants were asked whether they had always or on some days worked from home due to the pandemic (“yes” or “no“).
Financial changes
In the COVID-19 special survey, the respondents could state whether the financial situation of their household had improved, had stayed the same or had deteriorated since the beginning of the pandemic. The full question was: “Has the financial situation of your household changed due to the start of the coronavirus pandemic? no; yes, worsened; yes, improved”.
Covariates
Gender and age
Gender and age were recorded in the survey center during the baseline survey.
Type of household
At both points of measurement, household composition was measured based on the total number of household members and the number of children (<14 years of age) living in the household. Based on this information, it was distinguished whether respondents lived in one-person households, multiple-person households without children (<14 years of age) or multiple-person household with children (<14 years of age).
High-risk contact or infection
Since infections represent potentially life-threatening health events and thus may also have an impact on mental health, high-risk contacts and own SARS-CoV-2 infection (positive test result) were taken into account. A contact was considered a high-risk contact if respondents had close (distance of less than 1.5 meter) contact with a person with confirmed SARS-CoV-2 infection for at least 15 minutes since 1 February 2020. Whether a positive SARS-CoV-2 test was available was determined with the following question: “Since 1 February 2020, have you been tested for coronavirus in a doctor‘s office, testing center or hospital one or more times?“. In case they had been tested, the participants were then asked: “Was at least one test result positive?“ Based on this information, a dichotomous variable was created: (0) No test or a negative test; and (1) one positive test for SARS-CoV-2.
General health
Self-reported general health was measured using the first question of the Short-Form quality-of-life questionnaire (SF-12): “How would you describe your state of health in general?“ (Ware et al. 1996). The responses “not so good“ and “bad“ as well as “good“, “very good“ and “excellent“ were aggregated, respectively. The multivariable models took changes in general health into account, since health problems as confounders with variation over time on the one hand promote occupational changes (e.g., reduction of working hours) and on the other hand may have negative effects on mental health.
eTable 2. Multi-level Poisson regression analysis for probability of mental disorders*1.
| Moderate or severe depressive symptoms; PHQ-9 ( ≥ 10) | Moderate or severe anxiety disorder; GAD-7 (≥ 10) | |||
| Adj. RR | [95% CI] | Adj. RR | [95% CI] | |
| Wave | ||||
| Baseline survey | Ref. | Ref. | ||
| COVID-19 survey | 1.25*** | [1.17; 1.34] | 1.12* | [1.02; 1.23] |
| Occupational and financial changes during the pandemic | ||||
| Change in employment situation | ||||
| Working – no pandemic-related change | Ref. | Ref. | ||
| Working – change of job | 1.32** | [1.09; 1.60] | 1.36* | [1.07; 1.73] |
| Working – increased working hours | 1.53*** | [1.45; 1.61] | 1.63*** | [1.53; 1.74] |
| Working – reduced working hours with short-time allowance | 0.84*** | [0.79; 0.88] | 0.80*** | [0.74; 0.85] |
| Working – reduced working hours without short-time allowance | 1.05* | [1.00; 1.10] | 1.06* | [1.00; 1.13] |
| Unemployed prior to Corona | 1.88*** | [1.79; 1.97] | 1.90*** | [1.79; 2.03] |
| Unemployed due to Corona | 1.33*** | [1.18; 1.50] | 1.30*** | [1.11; 1.51] |
| Inactive person (pension, retirement, study) | 1.44*** | [1.39; 1.49] | 1.40*** | [1.34; 1.46] |
| Job insecurity | ||||
| High (ref.: “marginally or not employed“) | 1.90*** | [1.84; 1.96] | 2.01*** | [1.93; 2.09] |
| Working from home | ||||
| Yes, always or on some days (ref.: “No“) | 1.03 | [1.00; 1.07] | 1.05* | [1.00; 1.09] |
| Change in financial situation | ||||
| No change | Ref. | Ref. | ||
| Improvement | 1.07 | [0.98; 1.16] | 1.02 | [0.91; 1.14] |
| Deterioration | 1.56*** | [1.51; 1.62] | 1.65*** | [1.58; 1.73] |
| Covariates | ||||
| Age | ||||
| 19–29 years | Ref. | Ref. | ||
| 30–39 years | 0.88*** | [0.83; 0.94] | 0.88*** | [0.83; 0.94] |
| 40–49 years | 0.75*** | [0.70; 0.79] | 0.75*** | [0.70; 0.79] |
| 50–59 years | 0.66*** | [0.62; 0.70] | 0.66*** | [0.62; 0.70] |
| 60–69 years | 0.38*** | [0.36; 0.41] | 0.38*** | [0.36; 0.41] |
| 70–79 years | 0.24*** | [0.21; 0.26] | 0.24*** | [0.21; 0.26] |
| Gender | ||||
| Female (ref.: “male“) | 1.61*** | [1.47; 1.76] | 1.61*** | [1.47; 1.76] |
| Wave *Gender | ||||
| Increase compared to COVID-19 survey among women (ref.: “men“) | 1.05 | [1.00; 1.11] | 1.05 | [1.00; 1.11] |
| Type of household | ||||
| One-person household | Ref. | Ref. | ||
| Multiple-person household without children (<14 years of age) | 0.80*** | [0.78; 0.83] | 0.80*** | [0.78; 0.83] |
| Multiple-person household with children (<14 years of age) | 0.86*** | [0.82; 0.91] | 0.86*** | [0.82; 0.91] |
| High-risk contact with an infected person | ||||
| Yes (ref.: “No“) | 1.23*** | [1.12; 1.35] | 1.23*** | [1.12; 1.35] |
| Tested positive for SARS-CoV-2 virus | ||||
| Yes (ref.: “No“) | 0.92 | [0.69; 1.24] | 0.92 | [0.69; 1.24] |
| General health | ||||
| Poor (ref.: “good”) | 5.61*** | [5.47; 5.75] | 5.79*** | [5.61; 5.97] |
| Individuals (n) | 161 787 | 161 787 | ||
| Observations (n) | 323 574 | 323 574 | ||
*1 Mental disorders measured using PHQ-9 (depressive symptoms) and GAD-7 (anxiety disorder); jointly adjusted relative risks with robust standard errors
(Estimate for study center not shown). Legend: For a person who experienced the event “change of job“ during the COVID-19 survey, the probability of moderate or severe depressive symptoms has increased by 1.32 times.
Significance level: * p < 0.05; ** p < 0.01; *** p < 0.001
adj. RR, adjusted relative risks; GAD-7, Generalized Anxiety Disorder Scale-7; CI, confidence interval;
PHQ-9, Patient Health Questionnaire; ref., reference category
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Additional authors
Annette Peters, Miriam Engels, Börge Schmidt, Karin H. Greiser, Barbara Bohn, Steffi Riedel-Heller, André Karch, Rafael Mikolajczyk, Gérard Krause, Olga Lang, Leo Panreck, Marcella Rietschel, Hermann Brenner, Beate Fischer, Claus-Werner Franzke, Sylvia Gastell, Bernd Holleczek, Karl-Heinz Jöckel, Rudolf Kaaks, Thomas Keil, Alexander Kluttig, Oliver Kuß, Nicole Legath, Michael Leitzmann, Wolfgang Lieb, Claudia Meinke-Franze, Karin B. Michels, Nadia Obi, Tobias Pischon, Insa Feinkohl, Susanne Rospleszcz, Tamara Schikowski, Matthias B. Schulze, Andreas Stang, Henry Völzke, Stefan N. Willlich, Kerstin Wirkner, Hajo Zeeb, Wolfgang Ahrens
Affiliations of the additional authors
Institute of Epidemiology, Helmholtz Center Munich, Germany (AP, OL, SR)
Institute of Medical Sociology, Center for Health and Society, Medical Faculty, HHU Düsseldorf, Germany (ME)
Chair of Epidemiology, IBE, LMU München, Germany (AP, SR)
Dep. of Environ. Health, Harvard T. H. Chan School of Public Health, Boston, MA, USA (AP)
IMIBE, Medical Faculty, University Duisburg-Essen, University Hospital Essen, Germany (BS, KHJ, AS)
DKFZ, Division of Cancer Epidemiology, Heidelberg, Germany (KHG, RK)
NAKO e. V. Heidelberg, Germany (BB, LP)
ISAP, University of Leipzig, Germany (SRH)
Institute of Epidemiology and Social Medicine, University of Münster, Germany (AKa, NL)
Institute of Medical Epidemiology, Biometrics and Informatics, University of Halle-Wittenberg, Halle (Saale), Germany (RM, AKlu)
Department of Epidemiology, Helmholtz Center for Infection Research, Braunschweig, Germany (GK)
Department of Genetic Epidemiology in Psychiatry, Central Institute of Mental Health, Medical Faculty Mannheim, University of Heidelberg, Mannheim, Germany (MR)
DKFZ, Division of Clinical Epidemiology and Aging Research, Heidelberg, Germany (HB, BH)
Department of Epidemiology and Preventive Medicine, University of Regensburg, Germany (BF, ML)
Institute for Prevention and Tumor Epidemiology, Freiburg Medical Center, Medical Faculty, University of Freiburg, Germany (CWF, KBM)
NAKO Study Center Berlin-South/Brandenburg, Germany. Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany (SG)
Saarland Cancer Registry, Saarbrücken, Germany (BH)
Institute for Social Medicine, Epidemiology, and Health Economics, Charité – Universitätsmedizin Berlin, Germany (TK, SNW)
Institute for Clinical Epidemiology and Biometry, University of Würzburg, Germany (TK)
State Institute of Health, LGL, Erlangen, Germany (TK)
Institute of Biometry and Epidemiology, DDZ, Leibniz Center for Diabetes Research, Heinrich Heine University Düsseldorf, Germany (OK)
Institute of Epidemiology, University of Kiel, Germany (WL)
Institute of Community Medicine, University Medicine Greifswald, Gemany (CMF, HV)
Institute of Medical Biometry and Epidemiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany (NO)
Research Group Molecular Epidemiology, MDC, Berlin, Germany (TP, IF)
Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Germany (TP)
Biobank Technology Platform, MDC, Berlin, Germany (TP)
Berlin Institute of Health at Charité – Universitätsmedizin Berlin, Core Facility Biobank, Berlin, Germany (TP)
IUF gGmbH, Düsseldorf, Germany (TS)
Department of Molecular Epidemiology, German Institute of Human Nutrition Potsdam-Rehbruecke, Nuthetal, Germany (BS)
Institute for Nutritional Research, University of Potsdam, Germany (MBS)
IMISE, Medical Faculty. University of Leipzig, Germany (KW)
LIFE, University of Leipzig, Germany (KW)
BIPS, Bremen, Germany (HZ, WA)
Health Sciences Bremen, University of Bremen, Germany (HZ)
DZIF, Site Hannover-Braunschweig, Germany (GK)
Funding
This project was conducted with data of the German National Cohort (NAKO) Study (www.nako.de). The German National Cohort (NAKO) Study has been funded by the German Federal Ministry of Education and Research (BMBF, Bundesministerium für Bildung und Forschung) (grant number 01ER1301A/B/C und 01ER1511D), the Federal States (“Länder”) and the Helmholtz Association, as well as the participating universities and institutes of the Leibniz Association. The analysis was developed within the context of the MethodCoV method platform, which has been funded by the Federal Ministry of Education and Research (BMBF) (grant number 01KX2021). We thank all participants and staff members of the German National Cohort (NAKO) Study.
Compliance with ethical guidelines
All participants received detailed information and gave their informed consent to participate in the study in writing. The study program was carried out in accordance with national law and the 1975 Declaration of Helsinki (in the current, revised version).
Footnotes
Conflict of interest statement
Prof. Berger is honorary spokesman of the Expert Group “Neurological and Psychiatric Diseases” of the German National Cohort (NAKO) Study.
Prof. Dragano received third-party funding from the Federal Institute for Occupational Safety and Health for a study on COVID-19 and Occupation in the German National Cohort (NAKO) Study.
The remaining authors declare no conflict of interest.
References
- 1.Torales J, O‘Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 2.Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16 doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bäuerle A, Steinbach J, Schweda A, et al. Mental health burden of the COVID-19 outbreak in Germany: predictors of mental health impairment. J Prim Care Community Health. 2020;11 doi: 10.1177/2150132720953682. 2150132720953682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mata J, Wenz A, Rettig T, et al. Health behaviors and mental health before and during the COVID-19 pandemic: a longitudinal population-based survey. Soc Sci Med. 2021;287 doi: 10.1016/j.socscimed.2021.114333. 114333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters A, Rospleszcz S, Greiser KH, Dallavalle M, Berger K. The impact of the COVID-19 pandemic on self-reported health—early evidence from the German National Cohort. Dtsch Arztebl Int. 2020;117:861–867. doi: 10.3238/arztebl.2020.0861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahrens KF, Neumann RJ, Kollmann B, et al. Impact of COVID-19 lockdown on mental health in Germany: longitudinal observation of different mental health trajectories and protective factors. Transl Psychiatry. 2021;11 doi: 10.1038/s41398-021-01508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. 2021;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haas JG. Haas JG, editor. Die COVID-19 Pandemie und die menschliche Psyche COVID-19 und Psychologie: Mensch und Gesellschaft in Zeiten der Pandemie. Wiesbaden: Springer Fachmedien Wiesbaden. 2020:27–35. [Google Scholar]
- 11.Asmundson GJG, Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J Anxiety Disord. 2020;71 doi: 10.1016/j.janxdis.2020.102211. 102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giorgi G, Lecca LI, Alessio F, et al. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17217857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caroppo E, Mazza M, Sannella A, et al. Will nothing be the same again? Changes in lifestyle during COVID-19 pandemic and consequences on mental health. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18168433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riedel-Heller S, Richter D. COVID-19-Pandemie trifft auf Psyche der Bevölkerung: Gibt es einen Tsunami psychischer Störungen? Psychiatr Prax. 2020;47:452–456. doi: 10.1055/a-1290-3469. [DOI] [PubMed] [Google Scholar]
- 15.Guerriero RM, Pier DB, Gusmão de CM, et al. Increased pediatric functional neurological symptom disorders after the Boston marathon bombings: a case series. Pediatr Neurol. 2014;51:619–623. doi: 10.1016/j.pediatrneurol.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Karanikolos M, Heino P, McKee M, Stuckler D, Legido-Quigley H. Effects of the global financial crisis on health in high-income oecd countries: a narrative review. Int J Health Serv. 2016;46:208–240. doi: 10.1177/0020731416637160. [DOI] [PubMed] [Google Scholar]
- 17.Wright L, Steptoe A, Fancourt D. How are adversities during COVID-19 affecting mental health? Differential associations for worries and experiences and implications for policy. medRxiv. 2020 doi.org/10.1101/2020.05.14.20101717. [Google Scholar]
- 18.van der Velden PG, Contino C, Das M, van Loon P, Bosmans MWG. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J Affect Disord. 2020;277:540–548. doi: 10.1016/j.jad.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chandola T, Kumari M, Booker CL, Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med. 2020:1–10. doi: 10.1017/S0033291720005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62:686–691. doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 21.Milner A, Page A, LaMontagne AD. Cause and effect in studies on unemployment, mental health and suicide: a meta-analytic and conceptual review. Psychol Med. 2014;44:909–917. doi: 10.1017/S0033291713001621. [DOI] [PubMed] [Google Scholar]
- 22.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26:392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- 23.Amiri S. Unemployment associated with major depression disorder and depressive symptoms: a systematic review and meta-analysis. Int J Occup Saf Ergon. 2021:1–13. doi: 10.1080/10803548.2021.1954793. [DOI] [PubMed] [Google Scholar]
- 24.Frasquilho D, Matos MG, Salonna F, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. 2016;16 doi: 10.1186/s12889-016-2720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schipf S, Schöne G, Schmidt B, et al. Die Basiserhebung der NAKO Gesundheitsstudie: Teilnahme an den Untersuchungsmodulen, Qualitätssicherung und Nutzung von Sekundärdaten. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020;63:254–266. doi: 10.1007/s00103-020-03093-z. [DOI] [PubMed] [Google Scholar]
- 26.The German National Cohort (GNC) Consortium. The German National Cohort: aims, study design and organization. Eur J Epidemiol. 2014;29:371–382. doi: 10.1007/s10654-014-9890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krist L, Bedir A, Fricke J, Kluttig A, Mikolajczyk R. The effect of home visits as an additional recruitment step on the composition of the final sample: a cross-sectional analysis in two study centers of the German National Cohort (NAKO) BMC Med Res Methodol. 2021;21 doi: 10.1186/s12874-021-01357-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hinz A, Klein AM, Brähler E, et al. Psychometric evaluation of the generalized anxiety disorder screener GAD-7, based on a large German general population sample. J Affect Disord. 2017;210:338–344. doi: 10.1016/j.jad.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 30.19. Internationale Konferenz der Arbeitsstatistiker. Entschließung über Arbeitsstatistiken, Erwerbstätigkeit und die Unterauslastung des Arbeitskräfteangebots. www.ilo.org/wcmsp5/groups/public/–-dgreports/–-stat/documents/normativeinstrument/wcms_235273.pdf (last accessed on 1 March 2022) [Google Scholar]
- 31.Sverke M, Hellgren J, Näswall K. No security: A meta-analysis and review of job insecurity and its consequences. J Occup Health Psychol. 2002;7:242–264. [PubMed] [Google Scholar]
- 32.Brüderl J. Wolf C, Best H, editors. Kausalanalyse mit Paneldaten Handbuch der sozialwissenschaftlichen Datenanalyse. 1st ed. Wiesbaden. VS Verlag für Sozialwissenschaften. 2010:963–994. [Google Scholar]
- 33.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons. 1987 [Google Scholar]
- 34.Rugulies R, Sørensen K, Di Tecco C, et al. The effect of exposure to long working hours on depression: a systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ Int. 2021;155 doi: 10.1016/j.envint.2021.106629. 106629. [DOI] [PubMed] [Google Scholar]
- 35.Berkowitz SA, Basu S. Unemployment insurance, health-related social needs, health care access, and mental health during the COVID-19 pandemic. JAMA Intern Med. 2021;181:699–702. doi: 10.1001/jamainternmed.2020.7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Donnelly R, Farina MP. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Soc Sci Med. 2021;269 doi: 10.1016/j.socscimed.2020.113557. 113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health. 2020;20 doi: 10.1186/s12889-020-09875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Instruments
During the baseline survey for the German National Cohort (NAKO) Study, a wide variety of data, including clinical examinations and biospecimens, were collected. For this analysis, basic sociodemographic data obtained in a standardized interview conducted by trained study staff as well as basic information on mental health from a touchscreen questionnaire completed in the survey center were used. The COVID-19 special survey was conducted using online questionnaires (option selected by about two-third of the participants) or paper questionnaires sent by mail (option selected by about one-third of the participants).
Dependent variable/outcome
Mental disorders: At both survey times, depressive symptoms were recorded using the Patient Health Questionnaire (German: Gesundheitsfragebogen für Patienten; PHQ-9) and symptoms of anxiety using the Generalized Anxiety Disorder Scale-7 (German: Skala zur Messung der Generalisierten Angststörung; GAD-7). The PHQ-9 consists of nine questions querying the frequency of depressive symptoms (e.g., dejection, listlessness) within the last two weeks (28). These questions are summed to a total score (range: 0–27), where high scores represent higher severity. A score of 10 or more is considered moderate or severe symptoms of depression. The GAD-7 measures the frequency of seven symptoms of generalized anxiety over the last four weeks (e.g., nervousness, worries) (29). Here, again, a total is calculated (range: 0–21) and moderate or severe symptoms of anxiety are defined as scores of 10 or more.
Occupational and financial changes
Changes in employment situation: Changes were identified based on the comparison of employment status before the outbreak of the COVID 19 pandemic and during its course. First, the employment status at both measurement points was determined based on the workforce concept which differentiates between employed, unemployed and inactive persons (pension, retirement, study, other) (30). The special survey also covered work-specific changes due to the economic consequences of the pandemic („Did one or more of the following changes occur due to the impact of the coronavirus pandemic?“). This information was combined with the employment status to reflect changes. In the follow-up survey, the options listed below were added to the category “working“: change of job, increased working hours, reduced working hours with short-time allowance, and reduced working hours without short-time allowance. When both a change of job and a change in working hours were reported, we prioritized the latter. It was differentiated between two types of the “unemployed” category. Participants whose unemployment (unemployment benefit I or II) had already occurred before the start of the pandemic were assigned to the “unemployed prior to corona” category. Persons who reported to have become unemployed due to the corona pandemic were assigned to the “unemployed due to corona“ category.
Job insecurity
The perceived insecurity regarding employment as a measure for the likelihood of job loss (31) was measured at both time points with the following question: “My own job/professional existence is at risk: (1) do not agree at all, (2) do not agree, (3) agree, (4) agree completely“. From this, a binary variable with the expressions “no job insecurity” (answers 1–2) and “job insecurity“ (answers 3–4) was created. Inactive persons were assigned to the first category.
Working from home
The employed participants were asked whether they had always or on some days worked from home due to the pandemic (“yes” or “no“).
Financial changes
In the COVID-19 special survey, the respondents could state whether the financial situation of their household had improved, had stayed the same or had deteriorated since the beginning of the pandemic. The full question was: “Has the financial situation of your household changed due to the start of the coronavirus pandemic? no; yes, worsened; yes, improved”.
Covariates
Gender and age
Gender and age were recorded in the survey center during the baseline survey.
Type of household
At both points of measurement, household composition was measured based on the total number of household members and the number of children (<14 years of age) living in the household. Based on this information, it was distinguished whether respondents lived in one-person households, multiple-person households without children (<14 years of age) or multiple-person household with children (<14 years of age).
High-risk contact or infection
Since infections represent potentially life-threatening health events and thus may also have an impact on mental health, high-risk contacts and own SARS-CoV-2 infection (positive test result) were taken into account. A contact was considered a high-risk contact if respondents had close (distance of less than 1.5 meter) contact with a person with confirmed SARS-CoV-2 infection for at least 15 minutes since 1 February 2020. Whether a positive SARS-CoV-2 test was available was determined with the following question: “Since 1 February 2020, have you been tested for coronavirus in a doctor‘s office, testing center or hospital one or more times?“. In case they had been tested, the participants were then asked: “Was at least one test result positive?“ Based on this information, a dichotomous variable was created: (0) No test or a negative test; and (1) one positive test for SARS-CoV-2.
General health
Self-reported general health was measured using the first question of the Short-Form quality-of-life questionnaire (SF-12): “How would you describe your state of health in general?“ (Ware et al. 1996). The responses “not so good“ and “bad“ as well as “good“, “very good“ and “excellent“ were aggregated, respectively. The multivariable models took changes in general health into account, since health problems as confounders with variation over time on the one hand promote occupational changes (e.g., reduction of working hours) and on the other hand may have negative effects on mental health.