Summary
Background
The death toll after SARS-CoV-2 emergence includes deaths directly or indirectly associated with COVID-19. Mexico reported 325,415 excess deaths, 34.4% of them not directly related to COVID-19 in 2020. In this work, we aimed to analyse temporal changes in the distribution of the leading causes of mortality produced by COVID-19 pandemic in Mexico to understand excess mortality not directly related to the virus infection.
Methods
We did a longitudinal retrospective study of the leading causes of mortality and their variation with respect to cause-specific expected deaths in Mexico from January 2020 through December 2021 using death certificate information. We fitted a Poisson regression model to predict cause-specific mortality during the pandemic period, based on the 2015–2019 registered mortality. We estimated excess deaths as a weekly difference between expected and observed deaths and added up for the entire period. We expressed all-cause and cause-specific excess mortality as a percentage change with respect to predicted deaths by our model.
Findings
COVID-19 was the leading cause of death in 2020–2021 (439,582 deaths). All-cause total excess mortality was 600,590 deaths (38⋅2% [95% CI: 36·0 to 40·4] over expected). The largest increases in cause-specific mortality, occurred in diabetes (36·8% over expected), respiratory infections (33·3%), ischaemic heart diseases (32·5%) and hypertensive diseases (25·0%). The cause-groups that experienced significant decreases with respect to the expected pre-pandemic mortality were infectious and parasitic diseases (-20·8%), skin diseases (-17·5%), non-traffic related accidents (-16·7%) and malignant neoplasm (-5·3%).
Interpretation
Mortality from COVID-19 became the first cause of death in 2020–2021, the increase in other causes of death may be explained by changes in the health service utilization patterns caused by hospital conversion or fear of the population using them. Cause-misclassification cannot be ruled out.
Funding
This study was funded by Conacyt.
Keywords: Excess mortality, COVID-19, Mortality by causes, Mexico
Research in context.
Evidence before this study
The COVID-19 pandemic has affected mortality patterns throughout the world, and countries have made efforts both to contend with it and to measure the excess mortality directly and indirectly associated with it.
We searched for research literature about changes in excess deaths during the SARS-CoV-2 pandemic in Mexico and around the world. We found that the public health burden posed by COVID-19 is not readily estimated with certainty.
Some research and statistical networks have compiled information from different countries; however, comparison across countries is challenging. Furthermore, we found few articles reporting on excess mortality by specific causes. For Norway, a non-significant difference in the frequency of the major causes of death was reported. A study in the United States revealed significant increases in the number of deaths not caused directly by COVID-19, mainly cardiovascular diseases, Alzheimer's or dementia, and diabetes. While for China, cause specific excess mortality was reported for diabetes, myocardial infarction, and hypertension. For Mexico in 2020, 34.4% of excess mortality has not directly related to SARS-CoV-2 infection.
Added value of this study
Our study provides, to the best of our knowledge, the first analysis of cause specific excess mortality in a middle-income country during the COVID-19 outbreak. It makes important contributions to the understanding of COVID-19 attributable mortality, and changes in the proportional contributions of each cause of death to overall mortality in this kind of country. We also suggest different hypotheses to explain cause-specific increases; for instance, in the case of diabetes and ischaemic heart disease, where excess mortality could be associated with changes in health services availability and utilization.
Implications of all the available evidence
The excess mortality during the SARS-CoV-2 pandemic in Mexico is not due only to deaths directly associated with COVID-19, but with other causes, such as ischaemic heart diseases, diabetes, and hypertensive diseases as in other parts of the world. Disruption of health services and deferred health care could explain excess mortality for certain causes; although further research is needed to determine the factors behind these findings. Our study may be useful to understand how the emergence of COVID-19 has affected mortality in other middle-income countries in the Latin American region.
Alt-text: Unlabelled box
Introduction
More than two years after the emergence of the coronavirus (SARS-CoV-2) in Wuhan, China in late 20191 and the declaration of a pandemic by the World Health Organization (WHO) in March 2020,2 the number of people infected continues to rise. The global death toll is enormous, exceeding 6·1 million,3 although that number is subject to great uncertainty. It was estimated that by December 2021, 18·2 million people died worldwide due to the pandemic, as measured by excess mortality.4
Among the difficulties in determining the magnitude of mortality (directly or indirectly) associated with COVID-19 are the level of coverage by death certification, timeliness of reporting, and challenges of diagnostic confirmation, particularly in lower-resource countries. The public health burden posed by COVID-19 is a critical matter for decision-making but not readily estimated with a high degree of certainty. The standardization of estimation and reporting methods for excess all-cause and cause specific mortality is a global priority.5
Research and statistical networks, such as EUROMOMO,6 Our World in Data,7 and COVerAGE-DB,8 compiled information from different countries to monitor the daily mortality burden of COVID-19 at the global level; however, comparing across countries is challenged by structural differences in national reporting systems, differences in the age structures and prevalence of comorbidities, and the response capacities of different national health systems.9
Mexico belongs to the group of countries with the highest excess mortality during the pandemic, along with India, USA, Russia, Mexico, Brazil, Indonesia, and Pakistan in the world and Brazil, Chile, Ecuador, Guatemala, and Peru in the Latin American region.10,11 A study of all-cause excess mortality in Mexico estimated 1,050,383 deaths in 2020, with 326,610 excess deaths (45·1%) compared to the endemic channel of the previous five years.12 The Organization for Economic Cooperation and Development13 estimated a 52% increase. Another recent analysis of global mortality from COVID-19 estimated 798,000 excess deaths for Mexico by December 2021, placing it among the seven countries with the highest excess mortality in the world.4 This excess mortality is heterogeneous throughout the national territory and between sexes. García-Guerrero and Beltrán-Sánchez estimated that, in association with COVID-19, by December 2020, the Mexican population had lost about 2·5 and 3·6 years of life expectancy at birth for women and men, respectively. The biggest losses concentrated in the Northeastern, Central, and Southeastern states.14
Excess deaths from all causes include deaths from conditions that could be directly or indirectly associated with COVID-19. In the United States, 12·5% of the excess deaths in 2020 were not assigned to COVID-1915; the main associated diseases were cardiovascular diseases, Alzheimer's, and diabetes.16 In Italy, the main causes that contributed to the excess mortality not attributed to COVID-19 during 2020 were respiratory diseases, Alzheimer's disease, and diabetes mellitus17; in China, they were diabetes, hypertensive diseases, and myocardial infarction.18
According to Mexico's excess mortality bulletin, 34·4% of estimated excess mortality by causes was not directly associated to SARS-CoV-2 infection in 2020.19 Moreover, a higher ratio of excess mortality rate to reported COVID-19 mortality rate was revealed in Mexico compared to other countries,4 suggesting a higher proportion of excess deaths not attributable to COVID-19.
For public health planning and response, it is critical to have credible estimates of the excess deaths related to the pandemic, beyond those directly caused by COVID-19. This study analyses the changes in mortality patterns introduced by the emergence of COVID-19 in Mexico, a severely affected, middle-income country with 126 million inhabitants.
Estimating cause-specific excess mortality is particularly important for Mexico, to support public health decisions in a country with high prevalence of chronic diseases, such as obesity and diabetes, health conditions that have been differently related to the COVID-19 pandemic. Our results show changes in the mortality patterns in Mexico; this evidence could be useful to other middle-income countries to understand the effect of the pandemic in mortality composition.
Methods
Study design and data sources
We carried out a longitudinal retrospective study of the health records, in Mexico, to assess the excess mortality and its composition by leading causes of death and changes in their rates. We examined the absolute and percentage change of total observed deaths between January 1, 2020, and December 31, 2021, in comparison to the number of deaths predicted by a statistical model using the weekly mortality data series 2015–2019. After reviewing the available sources of information on mortality, we decided to use data from death certificates registered in the national Epidemiological and Statistical Subsystem of Deaths (SEED, acronym in Spanish),20 administered by the ministry of health, updated on March 14, 2022. We also considered mortality data from the National Institute of Statistics and Geography (INEGI, acronym in Spanish),21 epidemiological surveillance (SISVER), and the National Civil Registry Database (CRND) administered by the National Population Registry (RENAPO, acronym in Spanish). However, despite a little underreporting in SEED before 2019, from that year on, it behaves very well against both INEGI and the CRND. As INEGI only covers up to 2020 and the civil registry data is not ICD coded for cause of death, the best, and most comprehensive option was SEED.
To estimate mortality by specific group-causes, including COVID-19, we used all records from SEED.20 This database contains information about medical attention received, place of death, sociodemographic characteristics of the deceased, and the ICD-10 classification of cause of death.
We performed a relative comparison between the available databases to assess the difference, by state and calendar week, taking as reference 2015–2019, of the vital statistics data published by the INEGI,21 the civil registry (CRND),22 and SEED. We estimated that the latter had a death record of 96·5% in 2020 (data in supplemental material, page 5). Based on the United Nations Demographic Yearbook Vital Statistics Questionnaire (United Nations Statistics Division), Mexico had at least 90% coverage of death counts.
Procedures
We used information on cause of death from SEED, which was classified according to ICD-10 via a WHO-recommended automatic algorithm that uses the set of causes, chronological order of appearance, and duration since onset, annotated by the certifying physician on the death certificate.23 Experts from the General Directorate of Health Information and the General Directorate of Epidemiology and the Mexican Center for the Classification of Diseases provide overall quality control for the classification process. Deaths already coded based on the ICD-1024 were grouped according to 24 cause-groups based on the Global Burden of Disease (2010) classification.25 An additional category referring to COVID-19 was added to the lower respiratory infections subgroup (ICD-10 codes: U07·1 COVID-19, virus identified and U07·2 COVID-19, virus not identified)26 and also considered in the statistical analyses. Given their public health importance, we disaggregated cardiovascular diseases into four subgroups and injuries into two.
We described sociodemographic characteristics as recorded on the death certificates of people who died during the period of study: age, sex, occupation, educational level, institution where they received medical care, and place of death.
Statistical analysis
Using the 2015–2019 data, we fitted a Generalized Estimating Equations (GEE) model to estimate the weekly expected number of deaths and their 95% confidence intervals by specific cause-group in 2020 and 2021. This statistical methodology is an extension of Generalized Linear Models for grouped data in which a time-dependent structure may be considered,27 in our model we set a two-level structure with weekly mortality data nested within specific cause-groups. Our linear predictor included a secular trend parameterized with a linear splines function and an annual seasonality function based on Fourier series, both the secular trend and seasonality terms interacted with each of the 29 specific cause-groups indicator variables (our model was parameterized without a general constant). We specified the log as a link function between the linear predictor and the expected values of deaths, we set an autoregressive correlation structure of first order within cause-groups and a variance function for our outcome concordant with the Poisson distribution but with an extra scale parameter able to capture possible over dispersion. Further details of our model are available in the supplementary material (page 2).
After fitting the model to the 2015–2019 data, we predicted the mean number of deaths for each week during the 2020–2021 period for each specific cause-group following its estimated secular trend and seasonality functions, we set these predictions as reference value for calculating excess deaths for each week. We obtained cumulative excess deaths by summing weekly excess deaths during 2020–2021. We also obtained a P-score for cumulative excess deaths during 2020–2021 as ((observed /expected) -1) * 100. For selected groups of causes, we calculated the expected number of deaths as a group by adding up their specific estimates. Standard errors for cumulative expected number of deaths for both joined and specific cause-groups were obtained through the Delta method.
It should be noted that our excess mortality estimates reflect only the uncertainty regarding the predictions of the mean under our model, that is, the number of observed deaths were considered known during the pandemic period. In contrast, the weekly mean number of deaths, which is our reference value to calculate excess mortality, is estimated with our GEE model with its corresponding level of uncertainty. Our excess mortality definition, as a linear combination of a random variable and a realized or observed variable, only reflects the uncertainty of the mean estimation. For a formal description of our procedure, refer to the methodological appendix in the supplementary material (page2). We carried out all analyses using Stata/MP Version 17.0.
Role of funding source
This study was funded by Conacyt through the following programs: Investigadores por México y Estancias posdoctorales por México.
Results
Leading causes in total observed mortality 2020–2021
Mexico reported a total of 2,174,589 deaths between January 1, 2020, and December 31, 2021; 1,088,726 in 2020 and 1,085,863 in 2021 (Table 1). COVID-19 was the leading cause of death in 2020 (202,141 deaths, rate: 158·2 per 100,000) and 2021 (237,441 deaths, rate: 184·1 per 100,000). Ischaemic heart disease was the second cause of death in 2020 (166,002 deaths, rate 129·9 per 100,000) and 2021 (164,461 deaths, rate: 127·5 per 100,000). Next, we found diabetes mellitus (155,637 in 2020, rate: 121·8, and 143,020 in 2021, rate: 110·9); malignant neoplasms (92,008 in 2020, rate: 72, and 89,420 in 2021, rate: 69·3); digestive diseases (72,017 in 2020, rate: 56·4, and 74,208 in 2021, rate: 57·5), (Table 1).
Table 1.
Leading causes of death according to the classification of major causes in the Global Burden of Disease, Mexico 2019–2021.
| Disease subgroup | 2019 |
2020 |
2021 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | % | Rate | Deaths | % | Rate | Deaths | % | Rate | |
| II.G Cardiovascular diseases | 192,015 | 26·3% | 151·7 | 260,334 | 23·9% | 203·7 | 255,719 | 23·4% | 198·3 |
| II.G.03 Ischaemic heart disease | 110,989 | 15·2% | 87·7 | 166,002 | 15·2% | 129·9 | 164,461 | 15·0% | 127·5 |
| II.G.04 Cerebrovascular disease | 34,840 | 4·8% | 27·5 | 37,393 | 3·4% | 29·3 | 37,828 | 3·5% | 29·3 |
| II.G.02 Hypertensive diseases | 25,416 | 3·5% | 20·1 | 35,056 | 3·2% | 27·4 | 31,996 | 2·9% | 24·8 |
| I.B.01.b COVID-19 | 202,141 | 18·6% | 158·2 | 237,441 | 21·7% | 184·1 | |||
| II.C Diabetes mellitus | 104,265 | 14·3% | 82·4 | 155,637 | 14·3% | 121·8 | 143,020 | 13·1% | 110·9 |
| II.A Malignant neoplasms | 88,292 | 12·1% | 69·8 | 92,008 | 8·4% | 72·0 | 89,420 | 8·2% | 69·3 |
| II.I Digestive diseases | 70,365 | 9·6% | 55·6 | 72,017 | 6·6% | 56·4 | 74,208 | 6·8% | 57·5 |
| I.B Respiratory infections | 32,486 | 4·4% | 25·7 | 60,164 | 5·5% | 47·1 | 42,099 | 3·8% | 32·6 |
| II.H Respiratory diseases | 36,642 | 5·0% | 28·9 | 37,219 | 3·4% | 29·1 | 33,284 | 3·0% | 25·8 |
| III.B Intentional injuries | 32,281 | 4·4% | 25·5 | 33,981 | 3·1% | 26·6 | 32,428 | 3·0% | 25·1 |
| III.B.02 Injuries (homicide) | 26,328 | 3·6% | 20·8 | 27,268 | 2·5% | 21·3 | 25,449 | 2·3% | 19·7 |
| III.B.01 Intentionally self-inflicted injuries (suicides) | 5951 | 0·8% | 4·7 | 6713 | 0·6% | 5·3 | 6979 | 0·6% | 5·4 |
| III.A Accidents | 32,133 | 4·4% | 25·4 | 29,177 | 2·7% | 22·8 | 31,410 | 2·9% | 24·4 |
| III.A.01 Motor Vehicle Traffic Accidents | 8724 | 1·2% | 6·9 | 8280 | 0·8% | 6·5 | 8783 | 0·8% | 6·8 |
| II.J Genitourinary system diseases | 26,279 | 3·6% | 20·8 | 27,927 | 2·6% | 21·9 | 27,844 | 2·5% | 21·6 |
| I. A Infectious and parasitic diseases | 20,573 | 2·8% | 16·3 | 18,569 | 1·7% | 14·5 | 19,489 | 1·8% | 15·1 |
| II.E Mental disorders and nervous system diseases | 16,512 | 2·3% | 13·0 | 17,233 | 1·6% | 13·5 | 16,679 | 1·5% | 12·9 |
| II.D Other endocrine, metabolic, hematological, and immunological diseases | 10,261 | 1·4% | 8·1 | 13,247 | 1·2% | 10·4 | 13,367 | 1·2% | 10·4 |
| IV.0 Ill-defined causes | 11,026 | 1·5% | 8·7 | 12,289 | 1·1% | 9·6 | 13,246 | 1·2% | 10·3 |
| I.E Nutritional deficiencies | 10,092 | 1·4% | 8·0 | 11,191 | 1·0% | 8·8 | 11,319 | 1·0% | 8·8 |
| I.D Certain conditions originated in the perinatal period | 11,352 | 1·6% | 9·0 | 10,666 | 1·0% | 8·3 | 10,060 | 0·9% | 7·8 |
| III.C Events (injuries) of undetermined intent | 10,574 | 1·4% | 8·4 | 10,287 | 0·9% | 8·0 | 9335 | 0·9% | 7·2 |
| II.B Other neoplasms | 7080 | 1·0% | 5·6 | 6487 | 0·6% | 5·1 | 7059 | 0·6% | 5·5 |
| II.L Musculoskeletal disorders | 5206 | 0·7% | 4·1 | 5555 | 0·5% | 4·3 | 5708 | 0·5% | 4·4 |
| II.M Congenital birth defects | 5305 | 0·7% | 4·2 | 4993 | 0·5% | 3·9 | 4779 | 0·4% | 3·7 |
| II.K Skin diseases | 4391 | 0·6% | 3·5 | 3783 | 0·3% | 3·0 | 4232 | 0·4% | 3·3 |
| II.M Other congenital malformations | 3318 | 0·5% | 2·6 | 3021 | 0·3% | 2·4 | 2852 | 0·3% | 2·2 |
| I.C Maternal disorders | 598 | 0·1% | 0·5 | 581 | 0·1% | 0·5 | 652 | 0·1% | 0·5 |
| II.N Oral disorders | 163 | 0·0% | 0·1 | 169 | 0·0% | 0·1 | 168 | 0·0% | 0·1 |
| II.F Sense organ diseases | 41 | 0·0% | 0·0 | 50 | 0·0% | 0·0 | 45 | 0·0% | 0·0 |
| Total deaths | 731,250 | 100·0% | 1,088,726 | 100·0% | 1,085,863 | 100·0% | |||
Source: Prepared by the authors on information from the Epidemiological and Statistical Subsystem of Deaths (SEED), 2020–2021.
Crude rate with respect to the Mexican population in 2020. Conapo population projections.
Leading cause-groups of excess mortality
Cause-group specific mortality showed different behaviour during the pandemic period; 15 cause-groups increased with respect to predicted values to a total of 660,212 deaths. The rest of cause-groups decreased by a total of 59,620 deaths and were expressed as negative values and percentages. Thus, overall, the number of estimated excess deaths was 600,590 (95% CI: 575,125 to 626,056) which represented an increase of ((2,174,589 /1,573,999)-1)*100 = 38·2% (95% CI: 36·0 to 40·4) with respect to expected deaths. Consistently with total observed mortality, the five-leading cause-groups of excess mortality were COVID-19 with 439,582 deaths (439,558/600,590 = 73·2% of overall excess mortality), followed by ischaemic heart disease (81,136 deaths in excess, 13·5%), diabetes mellitus (80,294; 13·4%), other respiratory infections (25,571; 4·3%) and hypertensive diseases (13,430; 2·2%) (Table 2: % of overall excess). On the other hand, the five cause-groups with the largest absolute decrease in the pandemic period compared to predicted values were malignant neoplasms (-10,126; -1·7% of overall excess mortality), infectious and parasitic diseases (-9,992; -1·7% of overall excess mortality), non-traffic related accidents (-8,732; -1·5%), digestive diseases (-7,025; -1·2%) and chronic respiratory diseases (-5,590; -0·9%).
Table 2.
Difference between observed deaths 2020-2021, and their expected values from a model for 2015–2019 that includes seasonality and secular trend term.
| Periodo: 2020:01 a 2021:52 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Expected deaths |
Observed deaths | Excess deaths |
Percentage excess deaths |
% of overall excess | ||||
| Number | (IC95%) | (Observed-expected) | (IC95%) | % | (95% CI) | |||
| I.B.01.b COVID-19 | 0 | (0, 0) | 439,582 | 439,582 | (439,582 to 439,582) | - | - | 73·2 |
| II.G.03.0 Ischaemic heart diseases | 249,327 | (238,957 to 259,698) | 330,463 | 81,136 | (70,765 to 91,506) | 32·5 | (27·2 to 38·3) | 13·5 |
| II.G.04.0 Cerebrovascular disease | 70,595 | (65,439 to 75,752) | 75,221 | 4626 | (-531 to 9782) | 6·6 | (-0·7 to 14·9) | 0·78 |
| II.G.02.0 Hypertensive diseases | 53,622 | (49,005 to 58,239) | 67,052 | 13,430 | (8813 to 18,047) | 25 | (15·1 to 36·8) | 2·2 |
| II.G Other cardiovascular diseases | 40,439 | (36,633 to 44,244) | 43,317 | 2878 | (-927 to 6684) | 7·1 | (-2·1 to 18·2) | 0·5 |
| II.C Diabetes mellitus | 218,363 | (209,135 to 227,591) | 298,657 | 80,294 | (71,066 to 89,522) | 36·8 | (31·2 to 42·8) | 13·4 |
| I.B Respiratory infections | 76,692 | (70,716 to 82,667) | 102,263 | 25,571 | (19,596 to 31,547) | 33·3 | (23·7 to 44·6) | 4·3 |
| II.D Other endocrine, metabolic, hematological, and immunological diseases | 21,462 | (18,549 to 24,375) | 26,614 | 5152 | (2239 to 8065) | 24 | (9·2 to 43·5) | 0·9 |
| IV.0. Ill-defined causes | 22,259 | (19,328 to 25,190) | 25,535 | 3276 | (345 to 6207) | 14·7 | (1·4 to 32·1) | 0·5 |
| III.A Motor vehicle road injuries | 15,226 | (13,074 to 17,377) | 17,063 | 1837 | (-314 to 3989) | 12·1 | (-1·8 to 30·5) | 0·3 |
| I.E Nutritional deficiencies | 20,968 | (18,110 to 23,827) | 22,510 | 1542 | (-1317 to 4400) | 7·4 | (-5·5 to 24·3) | 0·3 |
| II.J.01.0 Nephritis and nephrosis | 38,467 | (34,457 to 42,477) | 39148 | 681 | (-3329 to 4691) | 1·8 | (-7·8 to 13·6) | 0·1 |
| I.C Maternal disorders | 1091 | (491 to 1692) | 1233 | 142 | (-459 to 742) | 13 | (-27·1 to 151·1) | 0·0 |
| II.F Sense organ diseases | 58 | (-55 to 170) | 95 | 37 | (-75 to 150) | 63·8 | (-44·1 to -272·7) | 0·0 |
| II.N Oral disorders | 309 | (-26 to 645) | 337 | 28 | (-308 to 363) | 9·1 | (-47·8 to -1396·2) | 0·0 |
| III.B.01.0 Self-harm (suicides) | 13,903 | (11,349 to 16,456) | 13,692 | -211 | (-2764 to 2343) | -1·5 | (-16·8 to 20·6) | 0 |
| II.L Musculoskeletal disorders | 11,922 | (9635 to 14,209) | 11,263 | -659 | (-2946 to 1628) | -5·5 | (-20·7 to 16·9) | -0·1 |
| III.B.02.0 Assaults (homicides) | 53,454 | (48,870 to 58,038) | 52,717 | -737 | (-5321 to 3847) | -1·4 | (-9·2 to 7·9) | -0·1 |
| I.D Certain conditions originated in the perinatal period | 22,015 | (19,223 to 24,808) | 20,726 | -1289 | (-4082 to 1503) | -5·9 | (-16·5 to 7·8) | -0·2 |
| II.E Mental disorders and nervous system diseases | 35,443 | (31,642 to 39,244) | 33,912 | -1531 | (-5332 to 2270) | -4·3 | (-13·6 to 7·2) | -0·3 |
| II.M Congenital birth defects | 17,232 | (14,712 to 19,753) | 15,645 | -1587 | (-4108 to 933) | -9·2 | (-20·8 to 6·3) | -0·3 |
| II.K. Skin diseases | 9716 | (7681 to 11,751) | 8015 | -1701 | (-3736 to 334) | -17·5 | (-31·8 to 4·3) | -0·3 |
| II.J Other genitourinary system diseases | 19,575 | (16,651 to 22,499) | 16,623 | -2952 | (-5876 to -28) | -15·1 | (-26·1 to -0·2) | -0·5 |
| II.B Other neoplasms | 17,175 | (14,256 to 20,094) | 13,546 | -3629 | (-6548 to -710) | -21·1 | (-32·6 to -5·0) | -0·6 |
| II.H Chronic respiratory diseases | 74,362 | (69,043 to 79,681) | 70,503 | -3859 | (-9178 to 1460) | -5·2 | (-11·5 to 2·1) | -0·6 |
| III.C. Events (injuries) of undetermined intent | 25,212 | (21,684 to 28,740) | 19,622 | -5590 | (-9118 to -2062) | -22·2 | (-31·7 to -9·5) | -0·9 |
| II.I Digestive diseases | 153,250 | (145,286 to 161,215) | 146,225 | -7025 | (-14,990 to 939) | -4·6 | (-9·3 to 0·6) | -1·2 |
| III.A Non-traffic related accidents | 52,256 | (47,495 to 57,016) | 43,524 | -8732 | (-13,492 to -3971) | -16·7 | (-23·7 to -8·4) | -1·5 |
| I.A Infectious and parasitic diseases | 48,050 | (43,325 to 52,776) | 38,058 | -9992 | (-14,718 to -5267) | -20·8 | (-27·9 to -12·2) | -1·7 |
| II.A Malignant neoplasms | 191,554 | (182,637 to 200,472) | 181,428 | -10,126 | (-19,044 to -1209) | -5·3 | (-9·5 to -0·7) | -1·7 |
| Total | 1,573,999 | (1,548,533 to 1,599,464) | 2,174,589 | 600,592 | (575,125 to 626,056) | 38·2 | (36·0 to 40·4) | 100 |
| I.B Respiratory infections + I.B.01.b COVID-19 | 76,692 | (70,716 to 82,667) | 541,845 | 465,153 | (459,178 to 471,129) | 60·5 | (55·5 to 66·2) | 77·4 |
| II.G Cardiovascular diseases (II.G + II.G.02.0 + II.G.03.0 + II.G.04.0) | 413,983 | (400,947 to 427,019) | 516,053 | 102,070 | (89,034 to 115,106) | 24·7 | (20·9 to 28·7) | 16·9 |
| Respiratory infections+Cardiovasculares+Diabetes mellitus+Covid-19 | 709,037 | (691,985 to 726,090) | 1,356,555 | 647,518 | (630,465 to 664,570) | 91·3 | (86·8 to 96·0) | 107·8 |
| II.J Genitourinary system diseases: Other genitourinary system diseases + Nephritis and nephrosis | 58,042 | (53,079 to 63,005) | 55,771 | -2271 | (-7234 to 2692) | -3·9 | (-11·5 to 5·1) | -0·3 |
| III.A Accidents: Motor vehicle road injuries + Other injuries | 67,481 | (62,257 to 72,706) | 60,587 | -6894 | (-12119 to -1670) | -10·2 | (-16·7 to -2·7) | -1·1 |
| III.B Intentional injuries: Self-harm (suicides)+ Assaults (homicides) | 67,357 | (62,110 to 72,604) | 66,409 | -948 | (-6195 to 4299) | -1·4 | (-8·5 to 6·9) | -0·16 |
Source: Prepared by the authors on information from the Epidemiological and Statistical Subsystem of Deaths (SEED), 2020–2021.
Percent change in cause-group specific mortality patterns
When analysing changes in cause-group specific mortality introduced by the pandemic (2020–2021) in comparison with the reference pre-pandemic period (2015–2019); we found that, besides the fact that COVID-19 became the leading cause of death in the country, ischaemic heart diseases increased by 32·5% (95% CI: [27·2 to 38·3]) with respect to predicted cause-group specific expected deaths and calculated as ((330,463/249,327)-1)*100 (Table 2). Diabetes mellitus increased by 36·8% (95% CI: [31·2 to 42·8]); respiratory infections by 33·3% (95% CI: [23·7 to 44·6]); and hypertensive diseases by 25·0% [95% CI: [15·1 to 36·8]). The cause-groups that experimented significant decreases with respect to the expected pre-pandemic mortality were: infectious and parasitic diseases -9,992 (-20·8%, 95% CI: [-27·9 to -12·2]); skin diseases -1,701 (-17·5%, 95% CI: [-31·8 to 4·3]), non-traffic related accidents -8,732 (-16·7%, 95% CI: [-23·7 to -8·4]) and malignant neoplasm -10,126 (-5·3%, 95% CI: [-9·5 to -0·7) (Table 2).
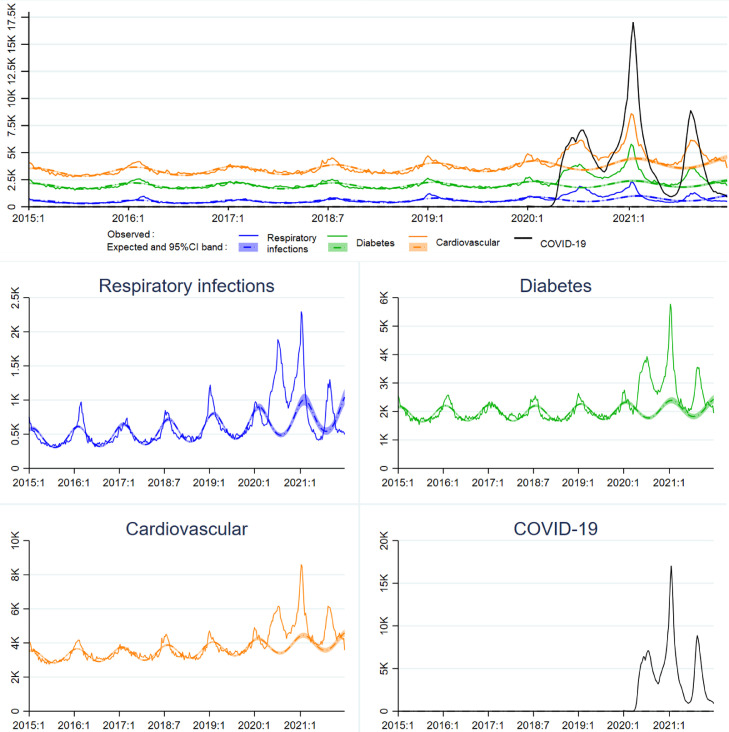
The upper panel of Figure 1 shows the time trends of the three leading cause-groups of death over the period 2015–2021 and COVID-19 (2020–2021); for clarity, we grouped all cardiovascular diseases into a single group. The temporal trend of excess deaths for each one of these cause-groups in the pandemic period follows closely that of COVID-19. Three epidemic peaks of great magnitude were observed in week 28 of 2020 and weeks three and 33 of 2021, coinciding with the maximum mortality peaks caused by COVID-19. The seasonal trend observed in these three cause-groups in the pre-pandemic period was disrupted in the pandemic period. The inferior panel shows the trend for each of the selected cause-groups, with independent scales for a clearer view of the trends of observed deaths, the expected deaths and their confidence intervals.
Figure 1.
Trends in leading causes of death, México 2015 – 2019.
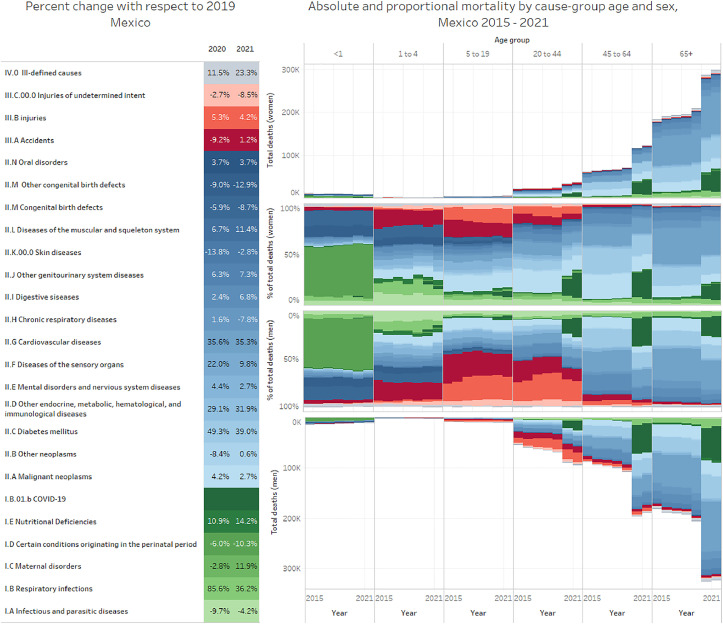
Figure 2 shows absolute and proportional mortality by sex, age-group cause-groups through 2015–2021. The left panel shows the percent change of years 2020 and 2021 with respect to 2019, it also serves as a colour scale to identify specific cause-groups in the composite graph of the right panel. The central section of the right panel shows proportional mortality by cause-group, sex and age-group through 2015 to 2021; the upper and lower sections of the right panel show absolute mortality. The effect of COVID-19, in absolute mortality, starts showing at the age-group 20–44 years with an increasing trend in older age-groups in men and women, although, proportionally, the most affected group was the 40–64 group in both men and women. Figure 2 also reflects the increases in cardiovascular diseases, diabetes mellitus and other respiratory infectious diseases; the latter showing an increase only in 2020. An interactive version of Figure 2 may be found in https://uisp.insp.mx/leadingcauses.html.
Figure 2.
Absolute and proportional mortality by sex, age-group cause-groups Mexico 2015–2021.
Sociodemographic characteristics and access to health care
Table 3 shows different sociodemographic characteristics and place where death occurred, as well as medical assistance received. The proportion of men who died from COVID-19 was higher than that of those who died from other causes (62·0% vs. 56·6%), the rest of the cause-groups behaved similarly to the pre-pandemic period.
Table 3.
Sociodemographic characteristics of COVID-19 decedents.
| 2015–2019 |
2020 & 2021 |
|||||
|---|---|---|---|---|---|---|
| All causes | COVID-19 | Remaining causes | ||||
| Sex | Deaths | % | Deaths | % | Deaths | % |
| Men | 1,892,945 | 55·6 | 272,488 | 62 | 981,546 | 56·6 |
| Women | 1,506,104 | 44·2 | 167,003 | 38 | 751,751 | 43·3 |
| Not specified | 6170 | 0·19 | 94 | 0 | 1600 | 0·0 |
| Age group | ||||||
| 65 and over | 1,947,850 | 57·1 | 214,149 | 48·7 | 1,012,895 | 58·4 |
| 45–64 | 823,580 | 24·2 | 176,846 | 40·2 | 443,437 | 25·6 |
| 20–44 | 439,941 | 12·9 | 46,982 | 10·7 | 208,875 | 12·0 |
| Less than 20 | 199,454 | 5·9 | 1608 | 0·4 | 69,690 | 4·0 |
| Education | ||||||
| Not specified | 2,311,433 | 67·8 | 55,516 | 12·6 | 371,236 | 21·4 |
| Incomplete high school or less | 199,104 | 5·8 | 114,244 | 26 | 265,616 | 15·3 |
| Completed high school or higher | 900,288 | 26·4 | 269,825 | 61·4 | 1,098,045 | 63·3 |
| Currently employed | ||||||
| Yes | 254,421 | 7·5 | 151,815 | 34·5 | 345,264 | 19·8 |
| No | 949,327 | 27·8 | 253,162 | 57·6 | 1,214,994 | 69·8 |
| Not specified | 2,207,150 | 64·7 | 34,608 | 7·9 | 181,286 | 10·4 |
| Place of death | ||||||
| Medical units | 1,538,341 | 45·1 | 364,693 | 82·9 | 568,684 | 32·8 |
| Household | 1,534,991 | 0·4 | 63,595 | 14·4 | 971,403 | 56·0 |
| Public Road | 151,927 | 4·5 | 764 | 0·2 | 65,149 | 3·8 |
| Not specified | 185,566 | 5·4 | 10,533 | 2·4 | 129,661 | 7·5 |
| Diabetes | ||||||
| Medical units | 217,312 | 43 | 364,693 | 83 | 69,550 | 23·3 |
| Household | 267,834 | 52·9 | 63,595 | 14·5 | 206,986 | 69·3 |
| Public Road | 1783 | 0·4 | 764 | 0·2 | 1086 | 0·4 |
| Not specified | 19,000 | 3·8 | 10,533 | 2·4 | 21,043 | 7·0 |
| Ischaemic heart diseases | ||||||
| Medical units | 119,390 | 24·4 | 364,693 | 83 | 42,987 | 13·0 |
| Household | 330,629 | 67·5 | 63,595 | 14·5 | 255,649 | 77·4 |
| Public Road | 8892 | 1·8 | 764 | 0·2 | 4037 | 1·2 |
| Not specified | 30,808 | 6·3 | 10,533 | 2·4 | 27,799 | 8·4 |
| Received medical care | ||||||
| No | 486,335 | 14·3 | 8202 | 1·9 | 250,457 | 14·4 |
| Yes | 2,726,993 | 80·0 | 418,673 | 95·2 | 1,393,471 | 80·3 |
| Not specified | 197,497 | 5·8 | 12,710 | 2·9 | 90,969 | 5·2 |
Source: Prepared by the authors on information from the Epidemiological and Statistical Subsystem of Deaths (SEED), 2020–2021.
In the pandemic period, the percentage distribution of deaths, caused by COVID-19, by age group was different from the distribution for the rest of the causes. In this age group, 40·2% of deaths were attributed to COVID-19, while 25·6% were attributed to the rest of the causes, similar to the percentage distribution in the pre-pandemic period. On the other hand, the proportion of deaths attributed to COVID-19 in the 65 years and over group, as well as the 20–44 age group were smaller compared to the proportion of deaths attributed to the rest of the causes in these age groups during the pandemic and pre pandemic period.
We found a higher educational level between those dying from COVID-19; the proportion of people who died from COVID-19 in this age group was 26·0% compared to 15·3% of those who died from other causes; these proportions are much larger compared to the proportion of people who died in this age group in the pre-pandemic period 5·8%. Independently of age and sex, the proportion of people who died from COVID-19 and were employed at the time of dead was more than 1·7 times higher (34·5%) than the employed people who died from other causes (19·8%). Moreover, the proportion of employed people who died from other causes in the pandemic period was more than 2·5 times higher than in the pre-pandemic period (7·5%).
COVID-19 deaths occurred mainly in hospitals (83·0%) compared to people who died from other caused (32·8%) and the majority received medical care whether in hospitals or outpatient services (95⋅2% vs. 80⋅6%) (Table 3).
The proportion of deaths by the rest of the causes that occurred in hospitals was lower in the 2020–2021 period (32·8%) compared to the pre-pandemic period (45·1%); this is most notable when analysed by cause of death. The proportion of deaths by diabetes and ischaemic heart disease that occurred in a hospital was 46% and 47% lower in the pandemic period compared to the pre-pandemic period, respectively (Table 3).
Death certificates without an underlying cause assigned accounted for 0⋅12% (n = 6605); of these 6560 occurred in 2021, which represents 0·6% of total deaths in that year, and they were not included in the model.
Discussion
This study makes important contributions to the understanding of changes in mortality during the COVID-19 outbreak in Mexico, whether these deaths are directly or indirectly attributed to COVID-19. We compared all-cause and cause-specific mortality, observed during three pandemic waves from January 2020 to December 2021, to the expected number of deaths (2020–2021), estimated with a statistical model, projecting cases using data from 2015 to 2019.
We documented an all-cause mortality excess of 38·2% for 2020–2021, which is smaller than the 45·1% previously reported for 2020.12 This could be explained by a slightly lower excess mortality in 2021; in addition, the 2020 study was performed with data from the CRND, also a different method to estimate expected deaths (2015–2019 endemic channel). Lima and colleagues have outlined great variability between different times of the pandemic and data sources.
The reported all-cause excess mortality during the pandemic has varied greatly among countries.28 A recent report29 found that for Germany, overall mortality was lower in 2020 than in four preceding years, whereas for Sweden and Spain, excess mortality was 3% and 15%, respectively. Latin America has been one of the most affected regions. Mexico is among the five countries with the highest excess mortality, along with Brazil, Peru, Colombia, and Ecuador.30 However, reported studies are difficult to compare, given the differences in the epidemic time and time span reported, age structures, comorbidities prevalence, or COVID-19 death reporting.
In our literature search, we found few articles reporting on excess mortality by specific cause, although some authors have shown interest in the proportion of excess mortality that cannot be directly associated with SARS-CoV-2 infection. For instance, in the United States, 12·5% of the excess deaths in 2020 were not assigned to COVID-19.15 In Italy, one of the countries most affected by the first pandemic wave, cause-specific excess mortality was studied for March and April 2020. The authors found notable increases for many of the main causes of death. Mortality from respiratory infections had the greatest increase. Other causes with remarkable excess mortality were Alzheimer's disease, diabetes mellitus, and hypertensive diseases.16,17
For Norway, Raknes et al.,31 reported a nonsignificant difference in the frequency of the major causes of death, and only a 4·1% increase for diabetes during the first wave. Reports from Guangzhou show increases for diabetes (10·2%), hypertension (14·5%), and myocardial infarction (8·6%).18 In Wuhan, during the first three months of the outbreak, Liu et al.32 reported an all-cause excess mortality of 56·0% and cause-specific mortality for diabetes (83·0%), myocardial infarction (23%), and hypertension (200%). The series that is more comparable to our data relates to cause-specific excess mortality reported for the United States, an all-cause mortality excess of 17·7% (505,976 deaths) and cause-specific mortality for cardiovascular diseases (4·8%) and diabetes (15·4%).33
A recent publication estimated 798,000 excess deaths for Mexico by December 2021, placing it among the seven countries with the highest excess mortality in the world.4 In this study, the authors developed an ensemble model to predict the expected number of deaths in 2020 and 2021 assuming the absence of COVID-19. They used a statistical model to estimate excess mortality for all countries. Our results suggest a smaller figure, 600,590 deaths in excess. We estimated expected deaths in 2020 and 2021 with a Poisson model that also incorporates the seasonal and secular trends; we also incorporated indicator terms to identify cause-groups according to GBD 2010 classification but, with data only from Mexico. We think that our more parsimonious model may be more accurate to estimate the excess of mortality in Mexico, given that we did not have to accommodate for the variability in data reporting observed in all countries. As Nepomuceno et al.34 outlined differences in the methods used to estimate the baseline can substantially change estimates of excess mortality, making comparison between studies somewhat difficult. Our results still put Mexico among the seven most affected countries in the world.
We found that COVID-19 became the first leading cause of death in Mexico, representing almost three-quarters of the estimated excess mortality in the period studied. This is in the high range of what has been reported in different countries.28, 29, 30 Excess mortality by other causes also increased substantially. Diabetes mellitus, ischaemic heart diseases, and respiratory infections increased more than one-third with respect to expected deaths; hypertensive diseases increased by one-quarter. To put this in perspective, during the last decade, diabetes mellitus and ischaemic heart diseases increased by 53% and 48%, respectively, compared to an increase of more than 30% in just one year. Excess mortality from diabetes mellitus and cardiovascular diseases may be attributed to multiple causes, either directly as a risk factor for COVID-19 mortality35 or indirectly, due to the lack of timely access to needed, ongoing health care treatment. The latter due to hospital conversion or medical care deferral. Furthermore, some patients may have avoided healthcare services due to the fear of contracting COVID-19. The consequences of these factors extend to mortality by respiratory infections, which follow the same trend as COVID-19 deaths. This is reflected by lower in-hospital mortality from non-communicable diseases during the pandemic period. The proportion of people who died of diabetes and ischaemic heart disease in a medical unit during the pandemic period (2020–2021) was almost half of the observed in the pre-pandemic period (2015–19). This consistent pattern undoubtedly reflects changes in healthcare services access and utilization caused by the pandemic. Moreover, a report estimates that during the first 9 months of the pandemic, outpatient consultations for diabetes and hypertension declined by 32% in Mexico´s Institute of Social Security, an institution that provides care for over 60 million Mexicans.36 The authors associated these changes with declines in blood sugar and blood pressure controls.
While declines in medical control of hypertension and diabetes could result in excess morbidity and mortality, it is difficult to quantify its real contribution to the excess mortality observed for these diseases. The concomitant variation among the epidemic curves of COVID-19, and those observed for diabetes and ischaemic heart diseases also suggest the possibility of misclassification in the cause of death, especially for those occurring at home, (55·9% of non-COVID-19 deaths took place in households). Furthermore, access to SARS-CoV-2 testing in Mexico was limited. In a Mexican study involving 1·15 million workers with a clinical diagnosis of COVID-19, only 34⋅5% had access to PCR testing.37
Another possible explanation for the observed increment in diabetes and ischaemic heart diseases could be that COVID-19 infection may have implications for the circulatory and/or metabolic systems; new emerging evidence points to a possible direct effect of SARS-CoV-2 infection, which can affect the endothelium in veins and arteries, as well as in islets of Langerhans, causing a decrease in insulin production.38
Contrary to what was expected, motor vehicle road injuries increased 12·1% with respect to expected number of deaths.39 This may be due to the fact that a hard lockdown in Mexico was in effect only between March 23 and June 1st, 2020. Supplemental material showing case-case group mortality trends and model predicted expected deaths in Mexico 2015–2021, clearly shows the effect of the lockdown reducing deaths from motor vehicle road injuries but, it increases quickly after June. In Italy, mortality due to external causes was also lower than that observed in the previous five years, but unlike what we found in Mexico, they outlined a remarkable drop in motor vehicle road injuries mortality rates.17 It should be noted that Italy adopted a hard national lockdown lasting for several months, driving to a drastic reduction in vehicle circulation. On the other hand, the reduction in non-traffic related accidents, one of the major causes of death in children as well as infectious and parasitic diseases, could be explained by school lock-down which lasted up to March 2022. This is also presented in the previously referred supplemental material.
Regarding sociodemographic characteristics, mortality in Mexico was higher in men than in women, consistent with observations in other countries40,41 and in previous studies for this country. Patterns of employment with implications for exposure to infectious agents likely contributed to the difference by sex. This excess in men may be due, in part, to their higher rates of employment; furthermore, as Dias et al. suggest, during the COVID-19 outbreak employers were much less likely to lay off fathers than mothers and non-parents, widening the gaps in employment rates between men and women.42 More women than men have stayed home during the pandemic, and as a result, they have been less likely to get infected. Additionally, several other factors may have contributed to the higher mortality rate in men, such as differences in the prevalence of some comorbidities, higher prevalence of smoking and drinking, and a longer delay in seeking medical care.43
Unlike other countries, the aged group 45 to 64 years experienced a higher proportion of deaths from COVID-19. This corroborates other studies’ findings, which report that in Mexico, the group aged 45 to 64 years was proportionally the most affected by this disease.12 In the same way, García Guerrero et al.14 reported greater loss of life expectancy at younger ages in regions most severely affected by the pandemic. However, this age-related pattern of excess deaths differs from other countries, where the most affected group has been people aged 65 years and over. The pattern in Mexico may be associated with the high prevalence of comorbidities such as diabetes,44 hypertension, and obesity at younger ages,45 all risk factors for mortality by COVID-19. As Glassman et al.46 suggest, in middle and low-income countries the most vulnerable population is not among older adults, but those with multi-morbidity which are mainly concentrated in younger adults. In Mexico, 39% of adults are obese, and estimations point out 10⋅3% prevalence of diabetes and 18⋅4% hypertension.47
Although the Mexican government has made efforts to improve the quality, coverage, and timeliness of mortality information through the SEED and the CRND, the SEED now shows an underreporting of 3% and the system still requires around two months to achieve this level of coverage. The gap could arise from unrecorded violent deaths. Public prosecutors’ offices register these deaths, and not all of them are incorporated into the SEED or the CRND databases. There is also variation in coverage by state. This could be addressed through the implementation of an online, real-time digital medical death certificate.
The epidemiological emergency caused by COVID-19 has demonstrated the importance of having information systems capable of real-time monitoring for emerging and re-emerging diseases that could become a national and/or global threat. The information systems also need the capacity to record contingency preparedness and mitigation actions in the setting of an emergency to evaluate, in real time, the impact of actions taken and to improve decision-making. Mexico has developed an early warning system for the surveillance of all-cause mortality based on information captured by the National Civil Registry, complemented with data from SEED. Maintaining this system would be a great asset to Mexico's health surveillance information system and could be easily implemented in other countries of the region.
The excess mortality during the SARS-CoV-2 pandemic in Mexico is due not only to deaths directly associated with COVID-19, but with other causes, such as ischaemic heart diseases, diabetes and hypertensive diseases as in other parts of the world.12,16 Lack of accessibility to health services or misclassification may contribute to this excess. Our results may be useful to understand how the emergence of COVID-19 has affected mortality in other middle-income countries in the Latin American region, and how to use timely data to estimate the burden of this and other emerging diseases. Also, we think that our results will contribute to increase knowledge to understand pandemic related elements such as changes in the health services utilization or deferred care.
Contributors
LSPM and JEHA were responsible for conceptualization, study design, literature search, formal analysis, supervision, data collection, analysis, and interpretation, writing original draft, reviewing, and editing. MHA contributed with conceptualization, formal analysis, data interpretation, writing, review, and editing. DDL and AB provided data curation, writing, review, and editing. ADQS contributed with formal analysis, data interpretation, visualization, writing, review, and editing. MAA, RCA, JWF, EVO, MCMT, OMO, ENL, IOH and KRG collaborated on writing, review, and editing. JMG, RLR, and HLGR came up with conceptualization, writing, review and editing. All authors had full access to all the data in the study and final responsibility for the decision to submit for publication.
Data sharing statement
Analysis files will be available at https://uisp.insp.mx/leadingcauses.html.
Declaration of interests
We declare no competing interests.
Acknowledgments
This study was funded by Conacyt.
MAA was receiving a scholarship from Conacyt through the program “Estancias posdoctorales por México” while this study was performed.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100303.
Appendix. Supplementary materials
References
- 1.Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel Coronavirus emerging in China — key questions for impact assessment. N Engl J Med. 2020;382(8):692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Systems Science and Engineering at Johns Hopkins University . Johns Hopkins University; Baltimore (MD): 2022. COVID-19 Dashboard.https://coronavirus.jhu.edu/map.html [Internet][updated 2022 Mar 25; cited 2022 Mar 25]. Available from: [Google Scholar]
- 4.Wang H, Paulson KR, Pease SA, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399(10334):1513–1536. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karlinsky A, Kobak D. The World Mortality Dataset: tracking excess mortality across countries during the COVID-19 pandemic. medRxiv [Preprint]. 2021. 10.1101/2021.01.27.21250604 [DOI] [PMC free article] [PubMed]
- 6.Vestergaard LS, Nielsen J, Richter L, et al. Excess all-cause mortality during the COVID-19 pandemic in Europe–preliminary pooled estimates from the EuroMOMO network, March to April 2020. Euro Surveill. 2020;25(26):1–6. doi: 10.2807/1560-7917.es.2020.25.26.2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ritchie H, Ortiz-Ospina E, Beltekian D, et al. OurWorldInData.org; 2020. Coronavirus Pandemic (COVID-19)https://ourworldindata.org/coronavirus [Internet][updated 2022; cited 2022 Mar 25] Available from: [Google Scholar]
- 8.Riffe T, Acosta E. Data resource profile: COVerAGE-DB: a global demographic database of COVID-19 cases and deaths. Int J Epidemiol. 2021;50(2):390. doi: 10.1093/ije/dyab027. –39. [DOI] [Google Scholar]
- 9.Corrao G, Rea F, Blangiardo GC. Lessons from COVID-19 mortality data across countries. J Hypertens. 2021;39(5):856–860. doi: 10.1097/hjh.0000000000002833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife. 2021;10:e69336. doi: 10.7554/eLife.69336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lima EEC, Vilela EA, Peralta A, et al. Investigating regional excess mortality during 2020 COVID-19 pandemic in selected Latin American countries. Genus. 2021;77(1):30. doi: 10.1186/s41118-021-00139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palacio-Mejia LS, Wheatley-Fernandez JL, Ordoñez-Hernandez I, et al. Estimación del exceso de mortalidad por todas las causas durante la pandemia del Covid-19 en México [Estimation of excess mortality from all causes during the Covid-19 pandemic in Mexico] Salud Publica Mex. 2021;63:211–224. doi: 10.21149/12225. [Spanish]. [DOI] [PubMed] [Google Scholar]
- 13.OECD . OECD iLibrary; 2021. Excess Mortality.https://www.oecd-ilibrary.org/sites/ec2de914-en/index.html?itemId=/content/component/ec2de914-en [Internet][updated 2022; cited 2022 Mar 25]. Available from: [Google Scholar]
- 14.García-Guerrero VM, Beltrán-Sánchez H. Heterogeneity in excess mortality and its impact on loss of life expectancy due to COVID-19: evidence from Mexico. Can Stud Popul. 2021;48:1–36. doi: 10.1007/s42650-021-00051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ackley CA, Lundberg DJ, Ma L, Elo IT, Preston SH, Stokes AC. County-level estimates of excess mortality associated with COVID-19 in the United States. SSM Popul Health. 2022;17 doi: 10.1016/j.ssmph.2021.101021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woolf SH, Chapman DA, Sabo RT, Zimmerman EB. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. 2021;325(17):1786–1789. doi: 10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grande E, Fedeli U, Pappagallo M, et al. Variation in cause-specific mortality rates in Italy during the first wave of the COVID-19 pandemic: a study based on nationwide data. Int J Environ Res Public Health. 2022;19(2):805. doi: 10.3390/ijerph19020805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li L, Hang D, Dong H, et al. Temporal dynamic in the impact of COVID- 19 outbreak on cause-specific mortality in Guangzhou, China. BMC Public Health. 2021;21(1):883. doi: 10.1186/s12889-021-10771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palacio-Mejía LS, Hernández-Avila JE. Grupo interinstitucional para la estimación del exceso mortalidad. Estimación del exceso de mortalidad por todas las causas en México 2020. [Estimate of excess mortality from all causes in Mexico 2020] [Internet] Boletín estadístico sobre el exceso de mortalidad por todas las causas durante la emergencia por COVID-19. 2022;1:1–43. https://uisp.insp.mx/dps/boletines/b_xxx/v2/index.html [Spanish]. Available from: Accessed 3 March 2022. [Google Scholar]
- 20.Dirección General de Información en Salud. Subsistema Epidemiológico y Estadístico de Defunciones. México City (MX): Secretaría de Salud; 2021.
- 21.Instituto Nacional de Estadística y Geografía . INEGI; México City (MX): 2015. 2019. Estadísticas Vitales de Mortalidad.https://www.inegi.org.mx/programas/mortalidad/ [Internet][cited 2021 March]Available from: [Google Scholar]
- 22.Registro Nacional de Población e Identidad. Actas de Defunciones . RENAPO; México City (MX): 2021. Base de Datos Nacional del Registro Civil 2019, 2020 y 2021. [Google Scholar]
- 23.Martins RC, Buchalla CM. Automatic coding and selection of causes of death: an adaptation of Iris software for using in Brazil. Rev Bras Epidemiol. 2015;18(4):883–893. doi: 10.1590/1980-5497201500040016. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization . 2nd Edition. World Health Organization; 2004. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. [Google Scholar]
- 25.Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 26.Centro Mexicano para la Clasificación de Enfermedades . Secretaría de Salud; Mexico City (MX): 2020. Correcto llenado del certificado de defunción. Muertos por virus SARS-COV2 (COVID-19)https://coronavirus.gob.mx/wp-content/uploads/2020/04/Correcto_llenado_del_certificado_de_defuncion_muertes_por_COVID-19.pdf Available from: [Google Scholar]
- 27.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 28.Kung S, Doppen M, Black M, et al. Underestimation of COVID-19 mortality during the pandemic. ERJ Open Res. 2021;7(1):00766–02020. doi: 10.1183/23120541.00766-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kowall B, Standl F, Oesterling F, et al. Excess mortality due to Covid-19? A comparison of total mortality in 2020 with total mortality in 2016 to 2019 in Germany, Sweden and Spain. PLoS One.2021;16(8):e0255540. 10.1371/journal.pone.0255540 [DOI] [PMC free article] [PubMed]
- 30.Cifuentes-Faura J. COVID-19 mortality rate and its incidence in Latin America: dependence on demographic and economic variables. Int J Environ Res Public Health. 2021;18(13):6900. doi: 10.3390/ijerph18136900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raknes G, Sorlie Strom M, Sulo G, Overland S, Roelants M, Benedikt Juliusson P. Lockdown and non-COVID-19 deaths: cause-specific mortality during the first wave of the 2020 pandemic in Norway: a population-based register study. BMJ Open. 2021;11(12) doi: 10.1136/bmjopen-2021-050525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu J, Zhang L, Yan Y, et al. Excess mortality in Wuhan city and other parts of China during the three months of the covid-19 outbreak: findings from nationwide mortality registries. BMJ. 2021;372:n415. doi: 10.1136/bmj.n415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nepomuceno MR, Klimkin I, Jdanov DA, Galarza AA, Shkolnikov V. Sensitivity analysis of excess mortality due to the COVID-19 pandemic. Popul Dev Rev. 2022;0(0):1–24. doi: 10.1111/padr.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dennis JM, Mateen BA, Sonabend R, et al. Type 2 diabetes and COVID-19–related mortality in the critical care setting: a national cohort study in England, March–July 2020. Diabetes Care. 2021;44(1):50–57. doi: 10.2337/dc20-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Doubova SV, Leslie HH, Kruk ME, Perez-Cuevas R, Arsenault C. Disruption in essential health services in Mexico during COVID-19: an interrupted time series analysis of health information system data. BMJ Glob Health. 2021;6(9) doi: 10.1136/bmjgh-2021-006204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hernández-Ávila M, Vieyra-Romero W, Gutiérrez-Díaz H, et al. Comportamiento epidemiológico de SARS-CoV-2 en población trabajadora afiliada al Instituto Mexicano del Seguro Social [Epidemiological behavior of SARS-CoV-2 in a working population affiliated with the Mexican Social Security Institute] Salud Publica Mex. 2021;63(5):607–618. doi: 10.21149/12495. [Spanish]. [DOI] [PubMed] [Google Scholar]
- 38.Lei Y, Zhang J, Schiavon CR, et al. SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE2. bioRxiv [Preprint]. 2020. doi:10.1101/2020.12.04.409144 [DOI] [PMC free article] [PubMed]
- 39.Gupta M, Pawar NM, Velaga NR. Impact of lockdown and change in mobility patterns on road fatalities during COVID-19 pandemic. Transport Lett. 2021;13(5–6):447–460. doi: 10.1080/19427867.2021.1892937. [DOI] [Google Scholar]
- 40.Shi C, Wang L, Ye J, et al. Predictors of mortality in patients with coronavirus disease 2019: a systematic review and meta-analysis. BMC Infect Dis. 2021;21(1):663. doi: 10.1186/s12879-021-06369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Islam N, Shkolnikov VM, Acosta RJ, et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137. doi: 10.1136/bmj.n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dias FA, Chance J, Buchanan A. The motherhood penalty and the fatherhood premium in employment during covid-19: evidence from The United States. Res Soc Stratif Mobil. 2020;69 doi: 10.1016/j.rssm.2020.100542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dahal S, Banda JM, Bento AI, Mizumoto K, Chowell G. Characterizing all-cause excess mortality patterns during COVID-19 pandemic in Mexico. BMC Infect Dis. 2021;21(1):432. doi: 10.1186/s12879-021-06122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Basto-Abreu A, Barrientos-Gutiérrez T, Rojas-Martínez R, et al. Prevalencia de diabetes y descontrol glucémico en México: resultados de la Ensanut 2016 [Prevalence of diabetes and poor glycemic control in Mexico: results from Ensanut 2016] Salud Publica Mex. 2020;62(1):50–59. doi: 10.21149/10752. [Spanish]. [DOI] [PubMed] [Google Scholar]
- 45.Campos-Nonato I, Hernández-Barrera L, Flores-Coria A, Gómez-Álvarez E, Prevalencia Barquera S. diagnóstico y control de hipertensión arterial en adultos mexicanos en condición de vulnerabilidad. Resultados de la Ensanut 100k [Prevalence, diagnosis and control of hypertension in Mexican adults with vulnerable conditions. Results of the Ensanut 100k] Salud Publica Mex. 2019;61(6):888–897. doi: 10.21149/10574. [Spanish]. [DOI] [PubMed] [Google Scholar]
- 46.Glassman A, Gaziano TA, Bouillon Buendia CP, Guanais de Aguiar FC. Confronting the chronic disease burden in Latin America and the Caribbean. Health Aff (Millwood) 2010;29(12):2142–2148. doi: 10.1377/hlthaff.2010.1038. [DOI] [PubMed] [Google Scholar]
- 47.Monterrubio-Flores E, Ramirez-Villalobos MD, Espinosa-Montero J, et al. Characterizing a two-pronged epidemic in Mexico of non-communicable diseases and SARS-Cov-2: factors associated with increased case-fatality rates. Int J Epidemiol. 2021;50(2):430–445. doi: 10.1093/ije/dyab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.