Abstract
Although health information technology (HIT) is essential in improving health outcomes and health care quality in the United States, current research lacks information regarding persuasive features (technology features designed to promote behavioral change) in HIT interventions for managing chronic diseases among older adults (aged 50 and older). To provide an overview of the persuasive features within current HIT interventions for managing chronic diseases among older adults, we conducted a systematic review to examine the use and efficacy of web-based chronic disease self-management for older adults. Persuasive system features included in HIT interventions were examined. Interventions presented in the final 24 studies were designed to improve health outcomes such as self-efficacy, self-care, and physical activity among participants with a chronic health condition. Examples of health conditions include diabetes, COPD, and arthritis. Among the 24 studies, several persuasive features were commonly used to support positive outcomes; 12 reported success in all measured outcomes and 10 reported a mix of both positive and unsuccessful outcomes pertaining to improvements in healthier lifestyles, self-management, chronic disease knowledge, blood pressure, and daily functioning. Only two of the studies included in our systematic review found no improvement in health outcomes and experienced high attrition rates after implementation of the persuasive systems intervention. It is important to identify specific persuasive features within interventions. Further research is needed in specifying persuasive features within technology-based interventions to help healthcare professionals modify interventions to improve chronic disease outcomes for older populations.
Keywords: Technology-based intervention, Chronic disease, Persuasive features, Self-management
1. Introduction
1.1. Chronic Disease, Older Adults and Health Information Technology
The number of older adults is increasing faster than ever before. By 2025, the global population over the age of 60 will reach an estimated 1.2 billion [1]. Because older adults are at greater risk for chronic disease, the prevalence of chronic conditions is also anticipated. Chronic diseases such as, cardiovascular diseases, hypertension, stroke, diabetes, cancer, chronic obstructive pulmonary disease, musculoskeletal conditions (such as arthritis and osteoporosis), mental health conditions (mostly dementia and depression), blindness and visual impairment, are the leading causes of death and disability among older people [1].
Health information technologies (HIT) are increasingly popular for the management of chronic disease among older adults. With continued advances in HIT, older patients have the opportunity to manage their own health with convenient, innovative technologies [2]. Computer-based health education has been shown to have positive impacts on clinical outcomes, including knowledge attainment, self-care management, and health related skill development [3]. Technology can also be used to persuade and motivate people to improve their health [4]. For example, web-based self-management programs can provide users with tailored interventions, one-on-one support, and provide feedback to encourage users to change their behaviors and/or attitudes. HIT interventions also give health care providers an opportunity to deliver care to hard to reach populations, while providing increased stability in intervention delivery [5], and overcoming barriers of time and mobility [6]. The use of online communication allows patients and health care providers to make connections with one another [7], and online support groups allow more patients with similar health challenges to connect with one another [8].
Although HIT offers new opportunities, there is little known about the design appropriateness or effectiveness of specific design approaches of HIT for disease management among older populations. Although many older adults use the internet [9, 10], increased literature related to older adults, computers, and internet usage [11] illustrates a potential lag in technology acceptance among older adults. This lag is commonly attributed to age-related physical impairments, financial barriers, security concerns, computer anxiety, low computer literacy, reduced self-efficacy, general lack of interest, and reduced benefit ratio [12–15]. Older computer users tend to be younger-older adults, more educated, have higher incomes and live independently [12, 13]. These users most frequently utilize the Internet for finance management, shopping, entertaining, education, travel planning and social contact, particularly with adult children. Concerns about older adults’ abilities to use, access, and evaluate online health information have also been raised [16–19]. However, HIT has been found to benefit older adults in activities of daily living and medical care needs [9], and highly beneficial with information access and enabling self-care [20]. Although older adults potentially have the most to gain through internet health promotion and HIT programming, older adults are at greatest risk of being left behind in the adoption of such technologies [19].
1.2. Web-based self-management and design theory
While commonly designed from health models, web-based self-management (SM) interventions often lack the incorporation of technology perspectives. For example, in an examination of participant engagement in a web-based SM trial, [21] found that participant utilization of the website and self-monitoring dramatically decreased after 6 months. Although efforts are made by web-based interventions to promote website engagement, interventions lack the qualities and design support features promoted by Fogg and his colleagues at Stanford’s Persuasive Tech Lab, who specifically explore the use of technology to change behaviors and attitudes, known as persuasive technology. While health promotion and technology perspectives have been developed separately, as health interventions continue to be technology-mediated, it will be increasingly important to integrate these perspectives.
1.2.1. Persuasive technology theory and the persuasive system design model
In addition to the health sector, there has been an increase in the development and use of technology systems and services being used to persuade users’ behaviors and/or attitudes [4]. This interactive information technology is known as persuasive technology because it is designed to persuade/change users’ attitudes or behavior. Many studies on user intention and behavior have been done using attitudinal theories to predict user acceptance of the information technology. However, attitudinal theories do not provide a systematic analysis or design methods for developing persuasive technology system. While Fogg has developed a widely used framework for understanding persuasive technology, the framework is too limited to develop and/or evaluate the persuasive system [22]. The Persuasive Systems Design (PSD) Model is a framework developed by Oinas-Kukkonen and Harjumaa to analyze, design and evaluate the persuasion context and related techniques in persuasive systems [23].
According to Oinas-Kukkonen and Harjumaa, there are several key issues that need to be focused on when designing or evaluating persuasive systems. The first key issue is information technology is never neutral, but instead is constantly motivating people to act or behave in a certain way. The second key issue is people like their views about the world to be organized and consistent, which deals with the idea of commitment and cognitive consistency. Commitment and cognitive consistency are both important in systems because they persuade users and motivate attitude change. The third key issue is direct and indirect routes are key persuasion strategies. Systems where direct and indirect routes are used are more likely to persuade more people, because people evaluate information differently [23].
The fourth key issue is persuasion is often incremental. This means, systems where people are instructed through a step-by-step process towards reaching a target behavior, are more persuasive than a system with a one step process. The fifth key issue is that persuasion through persuasive systems should always be open. So, any bias behind the persuasive system should be revealed so user persuasiveness is not lost or misled. The sixth key issue is persuasive systems should aim at unobtrusiveness, meaning systems should avoid disturbing users while users are completing tasks with the help of the system. The final key issue is persuasive systems should aim at being both useful and easy to use. Systems that are useless or hard to use, will not persuade users [23].
In addition to the key issues of persuasive systems, there is the persuasive context and persuasive design features. The persuasion context consists of three components: the intent, the event, and the strategy. The intent includes the persuader and the change type. The persuader is whoever develops the system and the change type is the behavior the system is targeting to change in the user of the system. The event includes the use, user, and technology contexts. The use context is important in analyzing the persuasion event. The use context is any feature that results from the problem area the system is aiming to change. The user context is parallel to understanding use context. The characteristics of individual users are referred to as the user context. Finally, any features and requirements of the technological platform and application of the system is referred to as the technology context. Each of these contexts are essential in analyzing and understanding the persuasion event. The final component of the persuasion context is the strategy, which has two elements when defining persuasion system strategies [23].
The first element is to analyze the message, which is the form and/or content used to deliver the intended change in behavior or attitude. For example, the context could be statistical data about the health risks of not exercising, and the information can be delivered to the user through a video or game. The second element in defining persuasion strategies is considering the route used, which is how the system will reach the user. The route can be a direct or indirect route to persuade users. Lastly are the persuasive design features, which are broken down into four categories [23].
Table 1 summarizes the principles, and features of the PSD model. The first category is the primary task support, which includes reduction, tunneling, tailoring, personalization, self-monitoring, simulation, and rehearsal. These features each focus on supporting the user’s primary task. The second category is dialogue support, which includes praise, rewards, reminders, suggestion, similarity, liking, and social role. These features focus on supporting the user and the system interaction with one another. The third category refers to credibility support, which includes trustworthiness, expertise, surface credibility, real world feel, authority, third party endorsement, and verifiability. These features focus on system credibility. The final category is social support, which includes social learning, social comparison, normative influence, social facilitation, cooperation, competition, and recognition These features focus on the system using social influence to motivate users [23].
Table 1.
| Principle | Feature | Definition |
|---|---|---|
| Primary Task | Reduction | Reducing complex behavior into simple tasks to help user perform the behavior |
| Tunneling | Guiding users through a process or experience | |
| Tailoring | Targeting information at potential needs, interests, personality, usage context, other factors relevant to a user group. | |
| Personalization | Offering personalized content or services | |
| Self-Monitoring | Keeping track of one’s own performance or status | |
| Simulation | Providing simulations to enable users to observe immediately the link between cause and effect regarding user’s behavior | |
| Rehearsal | Providing means to rehearse a behavior to enable user to change their attitudes or behavior | |
| Dialogue Support | Praise | Using praise via words, images, symbols or sounds to provide feedback on users behaviors |
| Rewards | Offering virtual rewards to give credit for performing behaviors | |
| Reminders | Using reminders to remind user of their behaviors | |
| Suggestions | Offering fitting suggestions for user to carry out behavior | |
| Similarity | System reminds user of themselves | |
| Liking | Visually attractive system that is appealing to users | |
| Social Role | Social Role | |
| Credibility Support | Trustworthiness | Providing information that is truthful and unbiased |
| Expertise | Providing information demonstrating knowledge, experience, and competence | |
| Credibility | Providing a reliable look | |
| Real-World Feel | Highlighting information about the organization and actual people | |
| Authority | Refers to people in a role of authority | |
| Third Party Endorsement | Including endorsements from well-known and respected sources | |
| Verifiability | Providing a means to verify the accuracy of the site contents | |
| Social Support | Social Learning | Providing means to observe others who are performing target behaviors and to see the outcomes of their behaviors |
| Social Comparison | Providing means for comparing performance with others | |
| Normative Influence | Leveraging peer pressure | |
| Social Facilitation | Providing a means for people to feel that others are performing the behavior along with them | |
| Cooperation | Providing means for people to cooperate with others | |
| Competition | Providing means for people to compete with others | |
| Recognition | Providing public recognition for users who perform target behavior |
1.3. Study objective
From a health perspective, older adults and their families have much to gain from web-based SM by providing unique opportunity for older adults to actively engage in their health in order to improve the general wellbeing of individuals [16, 25–27]. From an economic and public health perspective, the success of HIT would profoundly affect healthcare organizations and healthcare funders. Demonstrated intervention effectiveness and cost efficiency of web-based SM interventions could improve the health of patients using more affordable approaches, while reducing the need for clinical and acute care.
Although research on web-based SM is promising, few specifically target older adults and often lack technology considerations. There is yet to be a consistent framework outlining the components necessary to provide technology mediated health support for older adults. The purpose of this review is to analyze the persuasive system features and outcomes of web-based SM interventions, a popular HIT for managing chronic illnesses among various populations, specifically for older adults by applying the Persuasive Systems Design (PSD) model. While studies have been conducted using interventions that incorporate PSD features, there are no reviews to date that assess the connection between PSD features and outcomes of web-based SM interventions for older adults [28].
2. Methods
2.1. Overview
The persuasive systems design (PSD) model was used to review the persuasive features and outcomes of web-based self-management interventions for older adults (aged 50 and older) with chronic diseases. Persuasive systems is defined as “computerized software or information systems designed to reinforce, change or shape attitudes or behaviors or both without using coercion or deception” [24]. Web-based interventions are specific to online, internet, or web applications [29], while chronic diseases are ongoing diseases that have no complete cure [30]. Throughout our search, we examined studies with selected chronic diseases such as: heart disease, chronic obstructive pulmonary disease (COPD), arthritis, hypertension, and diabetes. However, additional studies of older adults with chronic diseases were included if the study met search criteria.
2.2. Search procedures
We used similar search procedures from a recent review that explicitly examined the efficacy of Web 2.0 chronic disease SM for older adults [28], yet expanded the criteria to include studies published from January 2004 to January 2015 (Fig. 1). The search databases included: ERIC, PsychINFO, PubMed, Academic Search Premier, and CINAHL. Methodology for search terms was completed by entering different combinations of search terms into each database, using specific vocabulary with the Boolean operators AND and OR. The search terms included: chronic disease, chronic illness, heart disease, diabetes, arthritis, hypertension, COPD, self-care, self-management, outcome, internet, online and website. To prevent exclusions of studies of older adults aged 50 and older, which is the age cut off defined by the world health organization [31], the terms “older adult” or “elderly” were not included in the search vocabulary.
Fig. 1.
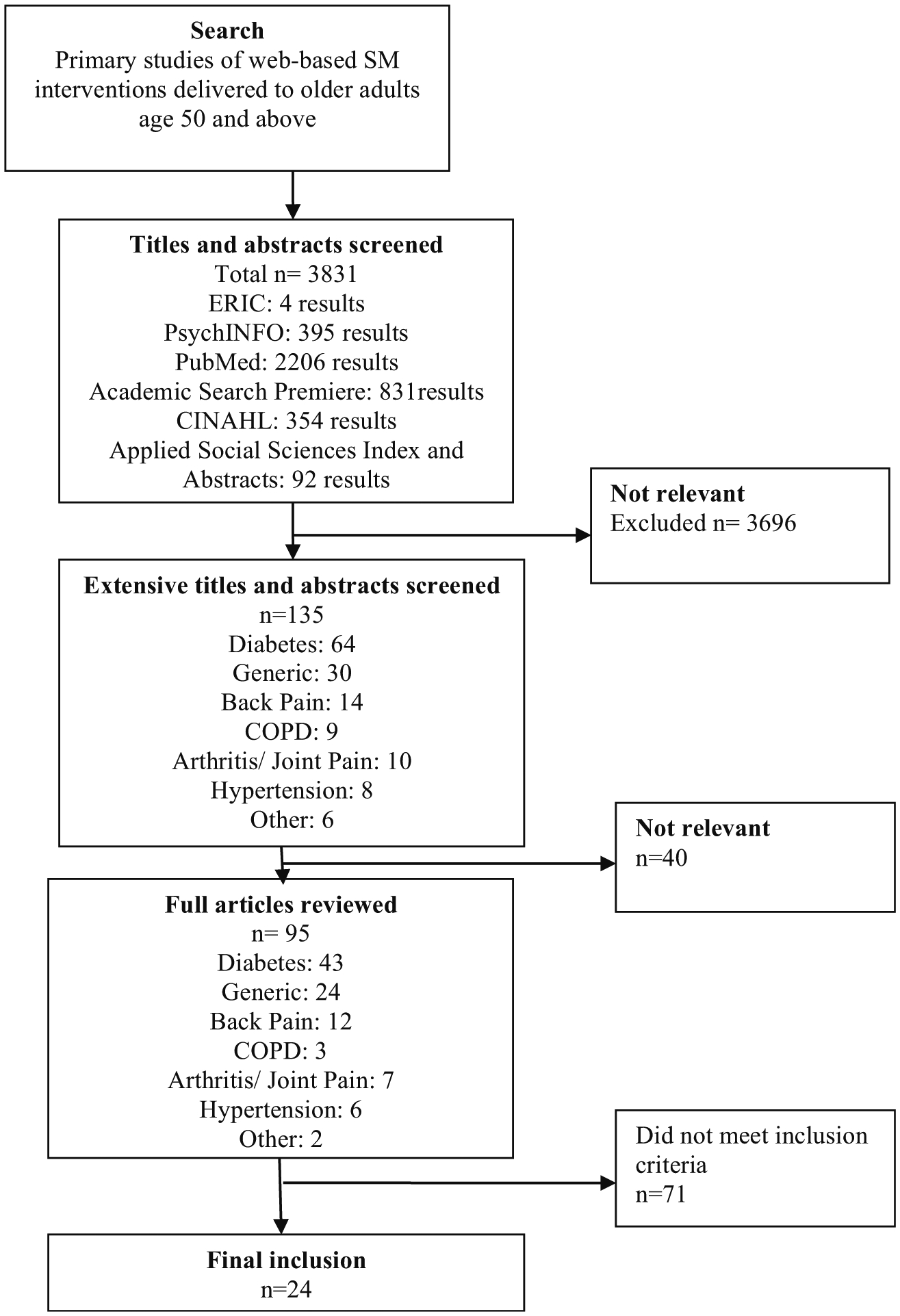
Article Selection Process
2.3. Selection criteria
Our first step was to identify studies of web-based chronic disease SM delivered to older adults ages 50 and older [28]. This search yielded 3831 results. After examining the titles and abstracts, 3696 studies were excluded because they were found to be irrelevant to our systematic review. Studies were irrelevant if they did not relate to chronic diseases, were not web-based interventions, did not target self-management behaviors, and if participants did not include those of the pre-specified age of 50 years and older. This left us with 135 relevant studies.
In order to be included in our systematic review, studies had to present a web-based intervention aimed to improve healthcare outcomes and self-management among older adults with a chronic disease. After further examination of reading the web-based interventions, we narrowed and excluded an additional 40 studies, which left us with 95 studies. These 40 studies were ineligible because the web-based intervention was not used by a patient with chronic disease or involved an intervention that was non-interactive.
Additional selection criteria included: studies that described the implementation and outcomes of the intervention used and English written peer reviewed studies [28]. Out of the 95 relevant studies, 71 more studies were excluded after reading the articles more in depth. These articles were excluded for the following reasons: unavailable through the institutional e-library, were written in a language other than English, had insufficient detail of research design and delivery, and outcomes were not discussed due to incomplete research protocols. This left us with our final inclusion of 24 studies, 15 that were from the self-management efficacy systematic review [32–45, 56], and 9 additional studies matching our selection criteria [46–54]. Although one study did not report the specific age of participants [36], it was included because the intervention targeted rheumatoid arthritis and was included by the original search procedures [28]. Figure 1 illustrates the search process.
In addition, if the study did not give a detailed description of the web-based intervention, we looked at additional articles so we could fully identify all of the PSD features in the intervention. One study was not fully described [32], therefore we identified an additional article for a better description of the Care for Me intervention [55]. We then examined the web-based SM interventions to identify PSD features and study whether the PSD features were connected to the outcomes in any way.
3. Results
3.1. Age of Participants in Web-Based Self-Management
All studies included people over the age of 50 years (per search inclusion criteria), however, only three studies targeted individuals over the age of 50 [37, 40, 46]. Most studies included any patient over the age of 18 or 21. The approximate average age of participants in the web-based SM interventions was 59 years, which is relatively young on the aging-continuum. Two studies did not report mean age, but rather age categories [44, 45]. In these cases, participants were primarily over the age of 55. While participants as young as 18 were involved in the web-based SM interventions, the youngest mean for a study was 51.34 years of age [51]. This suggests that web-based SM interventions that include older adults tend to have greater proportions of older participants. The oldest participant identified in the studies was 96 years of age [49], and Lorig et al. [45] had 21 participants over the age of 71.
3.2. Interventions
Interventions presented in the final 24 studies were designed to improve health outcomes such as self-efficacy, self-care, and physical activity among participants with a chronic health condition such as diabetes, COPD, and arthritis [32–47, 49–52, 54, 56]. For example, one study used an internet-based Arthritis Self-Management Program (ASMP) intervention. The goal of ASMP was to reduce pain and improve overall function among older adults. ASMP provided participants with exercise logs, medication diaries, and tailored exercise programs via the Internet [38]. Other interventions included The Diabetes Online Companion [54], The Online Diabetes Self-Management System [51], and the Wagner’s Chronic Care Model [36]. Interventions lasted anywhere from eight weeks [47] to two years [46, 50] with most interventions being implemented for one year [38–40, 45, 46, 53,56].
Of the 24 studies that included various interventions, 17 studies were randomized control trials [34–44, 46, 47, 49, 50, 53, 56], two were longitudinal studies [33, 51], two were pilot studies [32, 48], one was a feasibility study [52], and two were qualitative studies [45, 54]. Sample sizes of the studies varied greatly from 18 participants in a pilot study [32] up to 914 participants in a randomized control trial [49]. The studies most commonly had highly educated Caucasian participants who have been diagnosed with diabetes, rheumatoid arthritis, or chronic obstructive pulmonary disease (COPD) [21, 32–52, 56].
3.3. Persuasive Systems Design features
The PSD characteristics and primary outcomes are presented in Table 2. Although studies were not excluded from our systematic review based on PSD features, all 24 studies incorporated at least one feature from the PSD model (primary task support, dialogue support, systems credibility support, and social support).
Table 2.
| Study | Sample & Age | Primary Task Support | Dialogue Support | System Credibility Support | Social Support | Primary Outcomes |
|---|---|---|---|---|---|---|
| Bond et al. 2010 | N = 62 | Reduction | Reminders | Expertise | Social comparison | Positive Outcomes |
| Range: 60+ | Self-monitoring | Social role | Cooperation | |||
| Mean-Control: 68 | ||||||
| Mean-Intv: 66 | ||||||
| Brooks et al. [47] | N = 52 | Tailoring | Praise | Real-world feel | None | Positive Outcomes |
| Range: 33–76 | Personalization | Reminders | ||||
| Mean: 61 | Self-monitoring | Suggestion | ||||
| Rehearsal | Social Role | |||||
| Chen et al. [51] | N = 184 | Reduction | Reminders | Trustworthiness | Social learning | Positive Outcomes |
| Range: | Tailoring | Social Role | Authority | |||
| Mean: 51.34 | Personalization | |||||
| Self-monitoring | ||||||
| Cudney & Weinert, [35] | N = 123 | Reduction | Rewards | Trustworthiness | Social learning | Positive Outcomes |
| Range: 35–65 | Tailoring | Reminders | Real-world feel | |||
| Mean: 56.2 | Personalization | Suggestions | ||||
| Self-monitoring | Social role | |||||
| Rehearsal | ||||||
| Lorig et al. [38] | N = 855 | Reduction | Reminders | None | None | Positive Outcomes |
| Range: 22–89 | Tailoring | |||||
| Mean: 52.5 | ||||||
| Marziali, [32] | N = 18 | Tailoring | Similarity | None | None | Positive Outcomes |
| Range: | ||||||
| Mean: 60.8 | ||||||
| McKinstry et al. [50] | N = 401 | Tailoring | Praise | None | Social learning | Positive Outcomes |
| Range: 29–95 | Self-monitoring | Reminders | ||||
| Mean: 60.6 | Suggestion | |||||
| Social role | ||||||
| McMahon et al. [39] | N = 104 | Self-monitoring | Reminders | Expertise | None | Positive Outcomes |
| Range: 18+ | Authority | |||||
| Mean: 63 | ||||||
| Nguyen et al. [43] | N = 711 | Self-monitoring | None | Real-world feel | None | Positive Outcomes |
| Range: | Personalization | |||||
| Mean: 68.7 | Tailoring | |||||
| Sieber et al. [49] | N = 914 | Tunneling | Similarity | Expertise | Recognition | Positive Outcomes |
| Range: 21–96 | Tailoring | |||||
| Mean: 58 | ||||||
| Smarr et al. [36] | N = 33 | Tailoring | Reminders | Trustworthiness | Normative influence | Positive Outcomes |
| Range: | Personalization | Social Role | Expertise | Social facilitation | ||
| Mean: | Self-monitoring | Authority | ||||
| Bossen et al. [46] | N = 100 | Tailoring | Praise | None | Cooperation | Mixed Outcomes |
| Range: 50–75 | Self-monitoring | Reminders | ||||
| Mean: 62 | Personalization | Liking | ||||
| Rehearsal | Social Role | |||||
| Glasgow et al. [21] | N = 463 | Tailoring | Praise | Expertise | Social comparison | Mixed Outcomes |
| Range: 25–75 | Personalization | Reminders | Real-world feel | |||
| Mean: 58.4 | Self-monitoring | Suggestion | Verifiability | |||
| Simulation | Liking | |||||
| Social Role | ||||||
| Glasgow et al. [42] | N = 463 | Tailoring | Praise | Expertise | Social comparison | Mixed Outcomes |
| Range: 25–75 | Personalization | Reminders | Real-world feel | |||
| Mean: 58.4 | Self-monitoring | Suggestion | Verifiability | |||
| Simulation | Liking | |||||
| Social Role | ||||||
| Johnson et al. [48] | N = 20 | Reduction | Reminders | Expertise | Social learning | Mixed Outcomes |
| Range: 39–56 | Tailoring | Suggestions | Real-world feel | Recognition | ||
| Mean: 53 | Personalization | Liking | Authority | |||
| Self-monitoring | Social Role | Third-party | ||||
| Rehearsal | endorsements | |||||
| Lorig et al. [41] | N = 732 | Tailoring | Rewards | Trustworthiness | Social comparison | Mixed Outcomes |
| Age Range: | Personalization | Reminders | Expertise | Social facilitation | ||
| Mean Age: 54.3 | Self-monitoring | Authority | Recognition | |||
| Third-party | ||||||
| endorsements | ||||||
| Lorig et al. [45] | N = 254 | Self-monitoring | None | Expertise | Social facilitation | Mixed Outcomes |
| Range: | Personalization | Trustworthiness | ||||
| <40: 15.6 % | Tailoring | |||||
| 41–55: 40.9 % | ||||||
| 56–70: 36.2 % | ||||||
| >71:8.3 % |
3.3.1. Primary task support
Among the 24 studies, tailoring [33–37, 39–43, 45–54, 56] self-monitoring [33–37, 39–43, 45–54, 56], and personalization [33–36, 38, 40, 41, 43, 45–48, 51, 56] were the most commonly used primary task support principles in web-based interventions with older adults. Web-based interventions were tailored and personalized to participants in various ways. The web-based intervention Women to Women used personalization by addressing each participant personally when logging onto the website [35]. The My Path intervention tailored each participant’s goals and action plans to meet specific needs [29]. Participant’s goals and motivational messages were also tailored for each participant in the intervention, Stepping Up Towards Health [18]. Self-monitoring was frequently used in the web-based intervention to help participants keep track of their performance and progress [38]. The Diabetes Coach intervention used self-monitoring so participants could monitor their weight, blood glucose level, blood pressure, and cholesterol [33] While the majority of the studies that used tailoring [33–36, 38, 40, 41, 43, 45–51, 56], personalization [33–36, 38, 40, 41, 43, 45–48, 51, 56] and self-monitoring [33–37, 39–43, 45–52, 56] in their web-based intervention had positive outcomes, two studies that used tailoring and self-monitoring reported no positive outcomes [53, 54].
Studies where web-based interventions used reduction [35, 37, 38, 40, 48, 51] in order to help participants reduce a complex behavior into simple tasks [23], all showed positive outcomes for participants [35, 37, 38, 40, 48, 51]. Tunneling was only found in three web-based interventions [33, 40, 49], which guided participants through a process and provided opportunities to persuade the participant to better manage their chronic disease [23]. Two studies were promoting better self-management in diabetes [33, 49], while one was promoting better self-management for older adults with COPD [40]. The principal of rehearsal was used so participants could rehearse a behavior in order to change their attitude or behavior in the real world [23]. Studies where interventions incorporated rehearsal into their interventions showed improvement in self-management of chronic diseases [35, 48], decreases in pain [47] and increases in daily functioning and physical activity [46, 47]. Simulation was only used in one study, and allowed participants to immediately observe the link between their consumption of unhealthy and healthy foods [56].
3.3.2. Dialogue support
Reminders were the most frequently used dialogue support within the studies [35–39, 41, 46–48, 50, 51, 53, 54, 56]. Reminders allow participants to be updated on their target behaviors and therefore participants are more likely to achieve the goals they have set [23]. Web-based interventions used reminders in several ways. For example, the Therapeutic Exercise Resource Center (TERC) intervention sent participants automated messages reminding them the importance of exercising [47]. The Second Life Impact Diabetes Education and Self-Management (SLIDES) intervention used pop up messages on health promotion and disease prevention [48]. Every time participants logged in, they were reminded the importance of managing their diabetes [48]. Social role was also a commonly used dialogue support feature [33–37, 41, 46–48, 50, 51, 53, 56]. The use of social role allows participants to receive information from specialists via the Internet and use that information for persuasive purposes [23]. Every web-based intervention within our study that used social role, implemented it by providing participants with access to online support from a specialist [33–37, 41, 46–48,50, 51, 53, 56].
Praise, suggestion, rewards, liking and similarity were the dialogue support principles used the least. Praise as a dialog support was used in eight studies [34, 40, 42, 46, 47, 50, 53, 56]. The web-based interventions used praise by sending words and images as a way to provide feedback to participants who reached their goals [34, 40, 42, 46, 47, 50, 53, 56]. Suggestion was used in seven studies [34, 35, 47, 48, 50, 53, 56] as a way to suggest that participants carry out a particular behavior. For example, the Stepping Up to Health intervention had a daily tip on the website, which gave participants a suggestion on how to increase healthy behaviors. Dialogue support principles used the least were rewards, liking, and similarity. Rewards were used in four studies [34, 35, 41, 44], along with liking [46, 48, 52, 56], and similarity was used in only one study [32, 49].
3.3.3. Systems credibility support
The principles under the systems credibility support category describe how to design an intervention that is more credible and therefore, more persuasive [23]. Among the seven principles under systems credibility support category, expertise was most commonly used within the studies [33, 34,36, 37, 39–41, 45, 48, 49, 52, 56]. Expertise is incorporated within the system to increase persuasion [23]. Studies incorporated expertise into the technology-based intervention by allowing participants to either have instant messaging [37], e-mail [37], or face-to-face discussions with a health profession through a computer [45] or over the telephone [36, 41]. Expertise was also used by providing participants with the company website, which gave information about the company’s background and knowledge [39, 49]. The next most commonly used systems credibility support was trustworthiness [33–36, 41, 45, 51, 54]. Trustworthiness is used to increase persuasion and provide unbiased information [23]. For example, the Women to Women intervention was viewed as trustworthy because the website provided additional links for participants who wanted more information on a particular topic [35]. The DiabetesCoach intervention also provided information that was truthful, fair, and unbiased by showing all of their information and guidelines were in accordance with the diabetes care standards and protocols in Netherlands [33]. Real-world feel was used in eight studies to increase persuasion [21, 33, 35, 43, 47, 48]. When a technology-based intervention shows the people or company behind its services, the intervention is more credible [23]. For example, the Stepping Up to Health intervention gave participants a link to contact specific people to provide feedback or ask questions [34]. Authority can also enhance the power to persuade [23]. Of the 24 studies, seven used authority [33, 36, 39–41, 48, 51]. For example, two interventions had quotes from doctors and the government health office [39, 40]. There were also four studies that used third-party endorsements [33, 34,41, 48], and only one study used surface credibility [44] and one used verifiability [21] to increase persuasion.
3.3.4. Social supports
Social supports were used less frequently than persuasive task support, dialogue support, and systems credibility support in order to increase persuasion among participants [23]. Social learning was the most commonly used social support among the studies [34, 35, 40, 48, 50, 51]The Stepping Up to Health intervention used social learning by allowing participants to view one another’s daily step count [34]. Social learning allows participants to observe other participants performing a behavior and thus increases personal motivation [23]. Five studies used social comparison [34, 40, 41,47, 56] and recognition [34,40,41,48,49] where participants could compare their performance with other participants and be offered recognition. One intervention used social comparison by allowing participants to share and compare information related to their diet and exercise [37]. Four studies used social facilitation [34, 36, 41, 45] and cooperation [34, 46, 47, 54], and only one study used normative influence [36] and competition [34] to persuade participants. For example, the Stepping Up to Health intervention used competition as a means for users to compete with one another in order to generate more activity [34].
3.4. PSD Features and outcomes
Of the 24 studies included in our systematic review, 12 reported success in all measured outcomes [32, 35–37, 39, 42, 44, 47, 49–52], and 10 reported a mix of both positive and unsuccessful outcomes [33, 34, 38, 41, 43, 45, 46, 48, 54, 56] pertaining to improvements in healthier lifestyles, self-management, chronic disease knowledge, blood pressure, and daily functioning [32–39, 41–52, 56]. Only two of the studies included in our systematic review found no improvement in health outcomes and experienced high attrition rates after implementation of the persuasive systems intervention [40, 53].
When looking at PSD features, primary task supports were used 69 times in the 24 studies examined, making it the most utilized PSD feature category. Dialogue support was used 53 times in the 24 studies, making it the second most utilized PSD feature. Next, systems credibility was used 42 times in the 24 studies, making it the third most utilized PSD feature. Lastly, social supports were used only 26 times in the 24 studies, making it the least utilized PSD feature included in the systematic review. Self-monitoring, reminders, expertise, and social learning were the most commonly specific features from the four categories of features [32–47, 49–52, 56].
We were unable to identify clear pattern between the studies with all successful outcomes and the studies with all unsuccessful outcomes. All of the studies (with all successful or all unsuccessful outcomes) used PSD features from each category (primary task support, dialogue support, system credibility support, social support) [32, 35–37, 39, 40, 42, 44, 47, 49–52, 54]. However, upon closer examination of the two studies with no successful outcomes, one study split participants into two groups, where both groups were given two different interventions [40]. This finding is a possible explanation to the large number of PSD features present in the study because two interventions were being compared with one another [40].
Studies where outcomes were all successful [32,35–37,39, 40, 42, 44, 49–52], all had least one primary task support principal (reduction, tunneling, tailoring, personalization, self-monitoring, simulation, rehearsal) and at least one dialogue support principal (praise, rewards, reminders, suggestion, similarity, liking, social role) present within the web-based intervention. Several studies had mixed results [21, 33, 38, 41, 43, 45, 48, 54]. Common themes among these studies were the outcomes of self-management and self-efficacy. Five of the studies had improvements in both self-management and self-efficacy [38, 41, 43, 45, 48], while only three studies showed improvements in self-management, but not self-efficacy [33, 54, 56].
When looking at PSD features among the studies with mixed outcomes, all of the studies had two or more primary outcome principles [33, 38, 41, 43, 45, 48, 54, 56]. The most commonly used primary outcome principles within these studies included tailoring [33, 38, 41, 43, 45, 48, 54, 56] self-monitoring [33, 38, 41, 45, 48, 54, 56], and personalization [33, 38, 41, 43, 45, 48, 56]. This finding among the mixed-result studies was expected since both the primary task support and dialogue support categories focus on self-management and self-efficacy [23].
4. Discussion
To our knowledge, this is the first systematic review to examine PSD features within web-based interventions among older adults managing chronic diseases. Although many older adults use the Internet [9, 10], there is an increase in literature arguing technology is not designed to meet the needs of older adults [11]. This literature review was conducted to initially assess PSD features used and connections between PSD feature use and intervention outcomes to inform future design of HIT that can better meet the needs of older adults with chronic diseases.
Technology-based interventions offer the opportunity to allow participants to be reached more easily, saving participants time and money. However, technology-based interventions also must include PSD features to persuade and motivate participants to become active in managing their chronic disease and develop healthier behaviors [23]. Incorporating PSD features into technology-based interventions, such as the principles of tailoring and personalization, allows participants to be more involved in their treatment and management of chronic disease by adapting the intervention to meet individual needs [23, 48]. The PSD feature, social facilitation, is used in interventions to create a sense of community and commonality among participants diagnosed with similar chronic diseases [23, 34]. By incorporating the principle reduction, participants are able to lower the likelihood of developing future chronic diseases [23]. Without the persuasive component, participants are less likely to change their attitudes or behaviors; therefore PSD features are essential to technology-based interventions for chronic diseases [23].
Often times, older adults with chronic diseases are at higher risk of health disparities, such as depression, isolation, and physical inactivity [37]. Technology-based interventions need to include PSD features so that older adult participants are persuaded to better manage their chronic disease, resulting in reduction of health disparities [23, 37]. Current literature on technology-based interventions utilizes PSD features; however, researchers do not identify specific features [34–44, 46,47, 49, 50, 53, 56]. It is important to identify specific PSD features within interventions because we found PSD features are linked to successful outcomes. Further research is needed in specifying PSD features within technology-based interventions to help healthcare professionals modify interventions for older adults with chronic diseases in order to achieve better outcomes.
5. Limitations
There are limitations worth noting in our systematic review. Although we conducted a thorough search of studies using web-based interventions among older adults with chronic diseases, some studies may have been overlooked due to researchers being limited to searching for studies through the university’s database. Also, studies included PSD features but did not use the same terminology for the features, therefore leaving interpretation up to the researchers and creating possible bias. Lastly, most studies only included highly educated, Caucasian participants; therefore the results are not generalizable to all populations.
Footnotes
Conflict of interest Jennifer Portz, Amy Miller, Brittany Foster, and Lindsey Laudeman, declare that they have no conflict of interest.
References
- 1.World Health Organization, Active Aging: A Policy Framework. [Online]. Available: http://apps.who.int/iris/bitstream/10665/67215/1/WHO_NMH_NPH_02.8.pdf. [Accessed: 9-Feb-2016].
- 2.Healthcare Business Technology, Medical Technology. [Online]. Available: http://www.healthcarebusinesstech.com/medical-technology/. [Accessed: 13-Apr-2015].
- 3.Forkner-Dunn J, Internet-based Patient Self-care: The Next Generation of Health Care Delivery, J. Med. Internet Res, vol. 5, no. 2, p. e8, May 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lehto T and Oinas-Kukkonen H, Persuasive Features in Web-Based Alcohol and Smoking Interventions: A Systematic Review of the Literature, J. Med. Internet Res, vol. 13, no. 3, Jul. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aronson ID, Marsch LA, and Acosta MC, Using findings in multimedia learning to inform technology-based behavioral health interventions, Transl Behav Med, vol. 3, no. 3, pp. 234–243, May 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis D Computer-based approaches to Patient Education. J Am Med Inform Assoc JAMIA. 1999;6(4):272–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Consumer Use of Computers for Health Care Needs. [Online]. Available: http://aspe.hhs.gov/sp/reports/2009/consumerhit/index.shtml. [Accessed: 14-Apr-2015].
- 8.Center For Practice Improvement & Innovation American College Of Physicians - Reviews & Brand Information - American College of Physicians, Inc. Philadelphia, PA - Serial Number: 77766294. [Online]. Available: http://www.trademarkia.com/center-for-practice-improvement-innovation-american-college-of-physicians-77766294.html. [Accessed: 23-Apr-2015]. [Google Scholar]
- 9.Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, Dijkstra K, Fisk AD, Rogers WA, Sharit J Older Adults Talk Technology: technology usage and attitudes. Comput Hum Behav. Nov. 2010;26(6):1710–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith A, Older Adults and Technology Use, Pew Research Center’s Internet & American Life Project. [Google Scholar]
- 11.Lam JCY, Lee MKO Digital inclusiveness-longitudinal study of internet adoption by older adults. J Manag Inf Syst. Apr. 2006;22(4):177–206. [Google Scholar]
- 12.Carpenter BD, Buday S Computer use among older adults in a naturally occurring retirement community. Comput Hum Behav. Nov. 2007;23(6):3012–24. [Google Scholar]
- 13.Gatto SL, Tak SH Computer, internet, and E-mail use among older adults: benefits and barriers. Educ Gerontol. Aug. 2008;34(9):800–11. [Google Scholar]
- 14.Kim YS Reviewing And Critiquing Computer learning and usage among older adults. Educ Gerontol. Jul. 2008;34(8):709–35. [Google Scholar]
- 15.Wagner N, Hassanein K, Head M Computer use by older adults: A multi-disciplinary review. Comput Hum Behav. Sep. 2010;26(5): 870–82. [Google Scholar]
- 16.Bertera EM, Bertera RL, Morgan R, Wuertz E, and Attey AMO, Training Older Adults to Access Health Information., Educ. Gerontol, vol. 33, no. 6, pp. 483–500, Jun. 2007. [Google Scholar]
- 17.Bickmore TW, Caruso L, Clough-Gorr K, Heeren T It’s just like you talk to a friend relational agents for older adults. Interact Comput. Dec. 2005;17(6):711–35. [Google Scholar]
- 18.Chu A, Huber J, Mastel-Smith B, Cesario S ‘partnering with seniors for better Health’: computer use and internet health information retrieval among older adults in a low socioeconomic community. J Med Libr Assoc JMLA. Jan. 2009;97(1):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shapira N, Barak A, and Gal I, Promoting older adults’ wellbeing through internet training and use, Aging Ment Health, vol. 11, no. 5, pp. 477–484, Sep. 2007. [DOI] [PubMed] [Google Scholar]
- 20.LeRouge C, Van Slyke C, Seale D, and Wright K, Baby Boomers’ Adoption of Consumer Health Technologies: Survey on Readiness and Barriers, J. Med. Internet Res, vol. 16, no. 9, p. e200, Sep. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glasgow RE, Christiansen SM, Kurz D, King DK, Woolley T, Faber AJ, Estabrooks PA, Strycker L, Toobert D, and Dickman J, Engagement in a Diabetes Self-management Website: Usage Patterns and Generalizability of Program Use, J. Med. Internet Res, vol. 13, no. 1, Jan. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fogg BJ Persuasive Technology: Using Computers to Change What We Think and Do. San Francisco: Morgan Kaufmann Publishers; 2003. [Google Scholar]
- 23.Oinas-Kukkonen H and Haijumaa M, Persuasive Systems Design: Key Issues, Process Model, and System Features, Commun. Assoc. Inf Syst, vol. 24, no. 1, 2009. [Google Scholar]
- 24.Oinas-Kukkonen MHH, Towards Deeper Understanding of Persuasion in Software and Information Systems, pp. 200–205, 2008. [Google Scholar]
- 25.Cresci MK, Yarandi HN, Morrell RW Pro-nets versus No-nets: differences in Urban Older Adults’ predilections for internet use. Educ Gerontol. May 2010;36(6):500–20. [Google Scholar]
- 26.Flynn KE, Smith MA, and Freese J, When do older adults turn to the internet for health information? findings from the wisconsin longitudinal study, J Gen Intern Med, vol. 21, no. 12, pp. 1295–1301, Dec. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Selwyn N, Gorard S, Furlong J, and Madden L, Older adults’ use of information and communications technology in everyday life, Ageing Soc, vol. 23, no. 05, pp. 561–582, Sep. 2003. [Google Scholar]
- 28.Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, Sriram PS, and Zagora J, Web 2.0 chronic disease self-management for older adults: a systematic review, J. Med. Internet Res, vol. 15, no. 2, p. e35, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lau PWC, Lau EY, Wong DP, and Ransdell L, A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents, J. Med. Internet Res, vol. 13, no. 3, p. e48, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO | Noncommunicable diseases, WHO. [Online]. Available: http://www.who.int/topics/noncommunicable_diseases/en/. [Accessed: 14-Apr-2015].
- 31.WHO | Definition of an older or elderly person, WHO. [Online]. Available: http://www.who.int/healthinfo/survey/ageingdefnolder/en/. [Accessed: 14-Apr-2015].
- 32.Marziali E, E-health program for patients with chronic disease., Telemed. J. E-Health Off’. J. Am. Telemed. Assoc, vol. 15, no. 2, pp. 176–81,2009. [DOI] [PubMed] [Google Scholar]
- 33.Nijland N, van Gemert-Pijnen JEWC, Kelders SM, Brandenburg BJ, and Seydel ER, Factors influencing the use of a Web-based application for supporting the self-care of patients with type 2 diabetes: a longitudinal study, J. Med. Internet Res, vol. 13, no. 3, p. e71, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, Mehari KS, Fortlage LA, Resnick PJ, Zikmund-Fisher BJ, Strecher VJ, and Piette JD, An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial, J. Med. Internet Res, vol. 12, no. 4, p. e71, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cudney S, Weinert C An online approach to providing chronic illness self-management information. Comput Inform Nurs CIN. Feb. 2012;30(2):110–7. [DOI] [PubMed] [Google Scholar]
- 36.Smarr KL, Musser DR, Shigaki CL, Johnson R, Hanson KD, Siva C Online self-management in rheumatoid arthritis: a patient-centered model application. Telemed J E-Health off J Am Telemed Assoc. Mar. 2011;17(2):104–10. [DOI] [PubMed] [Google Scholar]
- 37.E. G, Burr RL, Wolf FM, and Feldt K, The Effects of a Web-Based Intervention on Psychosocial Well-Being Among Adults Aged 60 and Older With Diabetes A Randomized Trial, Diabetes Educ., vol. 36, no. 3, pp. 446–456, May 2010. [DOI] [PubMed] [Google Scholar]
- 38.Lorig KR, Ritter PL, Laurent DD, Plant K The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum. Jul. 2008;59(7):1009–17. [DOI] [PubMed] [Google Scholar]
- 39.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM-J, Levine BA, Conlin PR Web-based care management in patients with poorly controlled diabetes. Diabetes Care. Jul. 2005;28(7):1624–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nguyen HQ, Donesky-Cuenco D, Wolpin S, Reinke LF, Benditt JO, Paul SM, and Carrieri-Kohlman V, Randomized Controlled Trial of an Internet-Based Versus Face-to-Face Dyspnea Self-Management Program for Patients With Chronic Obstructive Pulmonary Disease: Pilot Study, J. Med. Internet Res, vol. 10, no. 2, p. e9, Apr. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lorig K, Ritter PL, Laurent DD, Plant K, Green M, Jernigan VBB, Case S Online diabetes self-management program: a randomized study. Diabetes Care. Jun. 2010;33(6):1275–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, Woolley T, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, Ritzwoller D Twelve-month outcomes of an internet-based diabetes self-management support program. Patient Educ Couns. Apr. 2012;87(1):81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen HQ, Donesky D, Reinke LF, Wolpin S, Chyall L, Benditt JO, Paul SM, Carrieri-Kohlman V Internet-based dyspnea self-management support for patients with chronic obstructive pulmonary disease. J Pain Symptom Manag. Jul. 2013;46(1):43–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Solomon M, Wagner SL, and Goes J, Effects of a Web-Based Intervention for Adults With Chronic Conditions on Patient Activation: Online Randomized Controlled Trial, J. Med. Internet Res, vol. 14, no. 1, Feb. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lorig K, Ritter PL, Plant K, Laurent DD, Kelly P, Rowe S The South Australia health chronic disease self-management internet trial. Health Educ Behav off Publ Soc Public Health Educ. Feb. 2013;40(1):67–77. [DOI] [PubMed] [Google Scholar]
- 46.Bossen D, Veenhof C, Van Beek KE, Spreeuwenberg PM, Dekker J, and De Bakker DH, Effectiveness of a Web-Based Physical Activity Intervention in Patients With Knee and/or Hip Osteoarthritis: Randomized Controlled Trial, J. Med. Internet Res, vol. 15, no. 11, p. e257, Nov. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brooks MA, Beaulieu JE, Severson HH, Wille CM, Cooper D, Gau JM, and Heiderscheit BC, Web-based therapeutic exercise resource center as a treatment for knee osteoarthritis: a prospective cohort pilot study, BMC Musculoskelet. Disord, vol. 15, no. 1, p. 158, May 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnson C, Feinglos M, Pereira K, Hassell N, Blascovich J, Nicollerat J, Beresford HF, Levy J, and Vorderstrasse A, Feasibility and Preliminary Effects of a Virtual Environment for Adults With Type 2 Diabetes: Pilot Study, JMIR Res. Protoc, vol. 3, no. 2, p. e23, Apr. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sieber W, Newsome A, Lillie D Promoting self-management in diabetes: efficacy of a collaborative care approach. Fam Syst Health J Collab Fam Healthc. Dec. 2012;30(4):322–9. [DOI] [PubMed] [Google Scholar]
- 50.McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, Sheikh A, Krishan A, Stoddart A, Padfield P Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013;346:f3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen L, Chuang L-M, Chang C-H, Wang C-S, Wang I-C, Chung Y, Peng H-Y, Chen H-C, Hsu Y-L, Lin Y-S, Chen H-J, Chang T-C, Jiang Y-D, Lee H-C, Tan C-T, Chang H-L, andF. Lai, Evaluating Self-Management Behaviors of Diabetic Patients in a Telehealthcare Program: Longitudinal Study Over 18 Months, J. Med. Internet Res, vol. 15, no. 12, p. e266, Dec. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCusker J, Cole M, Yaffe M, Sussman T, Lavoie KL, Strumpf E, Sewitch M, Sahin D, de Raad M A feasibility study of a telephone-supported self-care intervention for depression among adults with a comorbid chronic physical illness in primary care. Ment Health Fam Med. Dec. 2012;9(4):257–73. [PMC free article] [PubMed] [Google Scholar]
- 53.Thiboutot J, Sciamanna CN, Falkner B, Kephart DK, Stuckey HL, Adelman AM, Curry WJ, and Lehman EB, Effects of a web-based patient activation intervention to overcome clinical inertia on blood pressure control: cluster randomized controlled trial, J. Med. Internet Res, vol. 15, no. 9, p. e158, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu CH, Parsons JA, Mamdani M, Lebovic G, Hall S, Newton D, Shah BR, Bhattacharyya O, Laupacis A, and Straus SE, A web-based intervention to support self-management of patients with type 2 diabetes mellitus: effect on self-efficacy, self-care and diabetes distress, BMC Med. Inform. Decis. Mak, vol. 14, Dec. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marziali E and Donahue P, Caring for others: internet videoconferencing group intervention for family caregivers of older adults with neurodegenerative disease, The Gerontologist, vol. 46, no. 3, pp. 398–403, Jun. 2006. [DOI] [PubMed] [Google Scholar]
- 56.Glasgow RE, Kurz D, King DK, Dickman J, Faber AJ, Halterman E, Wooley T, Toobert PD, Strycker L, Estabrooks A, Osuna D, and Ritzwoller D. Outcomes of Minimal and Moderate Support Versions of an Internet-Based Diabetes Self-Management Support Program, J. General Int. Med, vol. 25, no. 12, p. e1315, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]


