Abstract
Introduction:
To examine trends in telemedicine adoption for stroke and cardiac care among U.S. hospitals, specifically associations between hospital financial indicators and adoption of these telemedicine services.
Methods:
This is a retrospective analysis of data from the Health Information Management and System Society Dorenfest Database and Healthcare Cost Report Information System from 2012 to 2017. We used a pooled ordinary least squares model and reported results as average marginal effects (AMEs).
Results:
The number of hospitals with stroke or cardiac telemedicine services in urban and rural areas increased through our study period from 153 (7.30%) to 407 (19.42%) and from 127 (6.31%) to 331 (16.45%), respectively. In rural hospitals, being a for-profit hospital (AME = −10.49, 95% confidence interval [CI] = −14.01 to −6.98) and having an increase in Medicare inpatient mix (AME = −0.31, 95% CI = −0.42 to −0.20) were associated with the probability of telemedicine adoption for heart attack and stroke care. A couple of nonfinancial variables included in the model also were associated with adoption, specifically having one more licensed bed (AME = −0.02, 95% CI = −0.04 to −0.00) and higher number of emergency department visits (AME = 5.64, 95% CI = 2.83 to 7.20). In urban hospitals, being a for-profit hospital (AME = −8.94, 95% CI = −11.76 to −6.11) and having a higher total margin (AME = 0.17, 95% CI = 0.08 to 0.26) were associated with the probability of telemedicine adoption for heart attack and stroke care. Two nonfinancial variables also were statistically significant: having one more licensed bed (AME = 0.01, 95% CI = 0.041 to 0.02) and being closer to another telemedicine hospital (AME = 0.81, 95% CI = −1.62 to 0.01).
Discussions:
Telemedicine adoption rate for cardiac and stroke care has increased significantly in recent years. Financial status may be a bigger driver of adoption for urban hospitals than rural hospitals.
Keywords: telemedicine, rural health, health care financing, implementation, access to care
Introduction
Americans living in rural areas are more likely to die from heart attack and stroke than individuals residing in urban areas.1 Lack of access to timely care is one of the main reasons of such disparity.2 The geographic distance to care is a substantial barrier to access to care in a timely manner, which is critical for both cardiac emergencies and stroke.3,4 For example, while the American Stroke Association recommends a 60-min guideline for the “door-to-needle time” for stroke patients to benefit from intravenous tissue plasminogen activator (tPA) treatment,5 a recent study found that rural patients with acute ischemic stroke are significantly less likely to receive tPA compared to urban patients (4.2% vs. 9.2%, adjusted odds ratio, 0.55 [95% confidence interval {CI} = 0.51 to 0.59], p < 0.001).6
Telemedicine for cardiac and stroke care is an approach to increasing the provision of necessary timely treatment. The implementation of telestroke programs has increased tPA administration, shortened onset to door time and reduced door to computed tomography (CT) time consults,7–10 and decreased door-to-needle time11 and door-to-CT time.12,13 Telecardiology can also improve the timeliness of care, including evaluating, stabilizing, and triaging patients who may need to be transported/transferred.14–16 The benefits of telecardiology care can be realized both as prehospital in cardiovascular emergencies17–21 and within the hospital for facilitating consultation with tertiary care centers.22 Telemedicine for cardiac care demonstrates similar benefits, such as reducing in-hospital mortality, compared to usual care.18,20
Although telemedicine for stroke and cardiac care is highly effective, adoption has been low among rural hospitals, who may benefit the most from these programs. A study of 4,727 U.S. hospitals found that rural hospitals were less likely to have a telemedicine program for stroke or cardiac care compared to urban hospitals (35.2% vs. 42.1%).23 Another study found that urban hospitals were more likely to adopt telemedicine for stroke care compared to rural hospitals.24 While prior studies have identified some predictors of telestroke adoption among community hospitals,25 a gap remains in understanding the effect of hospital level factors, specifically financial indicators, on the adoption of telemedicine for stroke and cardiac care, given that cost of infrastructure, implementation, and maintenance is a substantial barrier, particularly for rural hospitals.26 For decision-makers, particularly in financially vulnerable rural hospitals, this gap is important because of the known potential benefits of telestroke adoption.
To address this gap, the objectives of this study were to examine trends in telemedicine adoption for stroke and cardiac care among U.S. hospitals from 2012 to 2017; associations between hospital financial indicators and adoption of these telemedicine services; and differences in associations, if any, between financial indicators and adoption of telemedicine services among rural and urban hospitals. In other words, the study aimed to address the following questions. Did adoption of telemedicine for stroke and cardiac care increase over the study period? Were increases in the telemedicine adoption positively associated with hospital financial indicators, specifically for-profit status, profitability, and payer mix? Were there differences in such associations between rural and urban hospitals? Findings from this study are expected to provide some unique insights into factors that may influence the use of telestroke and telecardiology, particularly in rural settings.
Materials and Methods
STUDY DESIGN AND DATA SOURCES
This is a retrospective analysis of data from the Health Information Management and System Society (HIMSS) Dorenfest Database and Healthcare Cost Report Information System (HCRIS) from 2012 to 2017. The HIMSS Database is a market intelligence tool that tracked demographic and information systems data for all nonfederal acute care facilities with 100 beds or more, all integrated health care delivery systems that own at least one short term, acute care, nonfederal hospital with at least 100 beds. The HIMSS survey collects data on Information Technology (IT) use in the health care organizations, captured hospital characteristics (e.g., location, size, system affiliation), data of hospital financial variables, and whether hospitals having telemedicine capability for stroke and cardiac care.
VARIABLES OF INTEREST
The primary outcome of interest for this study is an indicator of stroke and cardiac telemedicine adoption, measured as a dichotomous variable in the HIMSS data (i.e., telemedicine being used for cardiology, stroke, and heart attack). The key independent variables of this study were hospital profit status (i.e., for-profit vs. not-for-profit) and hospital profitability (i.e., total margin). Because many external factors may impact stroke and cardiac telemedicine adoption, we controlled for hospital characteristics associated with telemedicine adoption,25,27 such as size of the hospital and distance to the nearest hospital with a telemedicine program with stroke or cardiac care. A detailed list of the analytical variables included in the study can be found in Appendix Table A1.
STATISTICAL ANALYSES
Our unit of analysis was the hospital-year defined as each year for which we analyzed data for a particular hospital. First, we merged relevant variables from the 6 years of HIMSS and HCRIS data to create a balanced wide panel (i.e., longitudinal data). Creating the panel dataset enabled us to have data on both a cross-sectional and a time series dimension (i.e., the data of all hospitals were collected during the whole time period). Because the amount of missing data was low (e.g., <8%), we used complete case analysis approach to address the missing data.28 Missingness among explanatory variables was addressed using a separate category for missing data. To ensure the validity of the statistical methods, we ran the Hausman Test and Breusch–Pagan test.29 The results of the Hausman Test and Breusch–Pagan test indicated a robust estimator of standard errors and showed consistent results among pooled ordinary least squares (OLS) and nonlinear alternatives (e.g., fixed effect method, random effects method). Therefore, we select the pooled OLS method as it gave us the most efficient estimator. Next, we tested for multicollinearity of variables that might be highly correlated, such as number of licensed beds and emergency department (ED) visits. Due to skewness, we used a natural log transformation for the ED visit volume per year and the distance to the nearest hospital with a telemedicine program with stroke or cardiac care variables. Finally, we ran a pooled OLS model to determine the association between explanatory variables and stroke and cardiac telemedicine adoption.
We used Stata/MP 16 software (Stata Corp) to conduct the analyses. For all models, we used a significance level of α = 0.05. Results are presented as percentages with interquartile range (IQR), mean with standard deviation (SD), and average marginal effects (AMEs) with 95% CIs for ease of interpretation. The University of North Carolina at Chapel Hill Institutional Review Board approved this study (IRB # 19-2301).
Results
The sample of 4,108 hospitals in our dataset was distributed across all 50 states and the District of Columbia. In our sample, 129 (3.14%) hospitals were Academic Centers; 1,241 (29.21%) were Critical Access Hospital; 48 (1.17%) were General Medical; and 2,690 (65.48) were General Medical and Surgical. Furthermore, 985 (23.98%) were Government, nonfederal; 606 (14.75%) were investor owned; and 2,457 (59.81%) were non-Government, not-for-profit. Data on the ownership of 60 (1.46%) hospitals were missing. Regarding geographic location, 2,012 (48.98%) were rural and 2,096 (51.02%) were urban hospitals. The average of straight-line distance to the nearest hospital with a stroke and/or cardiac telemedicine service for rural and urban hospitals was 26.28 (SD: 17.84) and 7.84 (SD: 9.35) miles, respectively. In terms of size, the median number of annual ED visits was 21,078 (IQR: 7,739 to 42,894), and the median number of hospital beds was 106 (IQR: 25–260). Finally, in terms of financial variables, the median total margin was 0.04 (IQR: −0.01 to 0.09), the median return on equity was 0.07 (IQR: 0.003 to 0.15), the median of days cash on hand was 62.9 days (IQR: 11.4 to 163.5), and the median Medicare inpatient payer mix was 0.48 (IQR: 0.36 to 0.63). See Table 1 for a summary of hospital characteristics.
Table 1.
Summary of Hospital Characteristics Categorized by Adoption Phase and Rurality
| HOSPITAL CHARACTERISTICS | FULL ADOPTER |
PARTIAL ADOPTER |
NONADOPTER |
||||||
|---|---|---|---|---|---|---|---|---|---|
| RURAL (N = 105) | URBAN (N = 125) | p | RURAL (N = 278) | URBAN (N = 335) | p | RURAL (N = 1,625) | URBAN (N = 1,636) | p | |
| Mean ED visit volume per year | 17,054 | 57,512 | <0.001 | 13,565 | 47,373 | <0.001 | 11,471 | 44,219 | <0.001 |
| Mean number of licensed beds | 71 | 419 | <0.001 | 65 | 312 | <0.001 | 60 | 198 | <0.001 |
| Mean distance to nearest hospital with stroke and/or cardiology telemedicine | 25.15 | 5.91 | <0.001 | 25.23 | 7.36 | <0.001 | 26.46 | 8.08 | <0.001 |
| Mean total margin (%) | 4.01 | 8.01 | <0.001 | 3.01 | 5.01 | <0.001 | 2.01 | 5.01 | <0.001 |
| Mean days cash on hand | 125 | 147 | <0.001 | 144 | 109 | <0.001 | 108 | 99 | <0.001 |
| Mean Medicare inpatient mix | 0.56 | 0.37 | <0.001 | 0.59 | 0.38 | <0.001 | 0.63 | 0.39 | <0.001 |
| Hospital ownership | |||||||||
| Government, nonfederal (%) | 40 (38.10) | 21 (16.80) | <0.001 | 77 (27.21) | 26 (7.76) | <0.001 | 613 (37.73) | 209 (12.87) | <0.001 |
| Investor-owned, for-profit (%) | 0 (0.00) | 4 (3.20) | <0.001 | 12 (4.24) | 35 (10.45) | <0.001 | 169 (10.40) | 386 (23.59) | <0.001 |
| Nongovernment, non-for-profit (%) | 65 (61.90) | 98 (78.40) | <0.001 | 193 (68.20) | 265 (79.10) | <0.001 | 825 (50.77) | 1,011 (61.80) | <0.001 |
| Missing | 0 (0.00) | 2 (1.60) | <0.001 | 1 (0.35) | 9 (2.69) | <0.001 | 18 (1.11) | 30 (1.83) | <0.001 |
| Hospital type | |||||||||
| Academic (%) | 0 (0.00) | 11 (8.80) | <0.001 | 2 (0.70) | 25 (7.46) | <0.001 | 1 (0.06) | 90 (5.50) | <0.001 |
| Critical access (%) | 53 (50.48) | 8 (6.40) | <0.001 | 145 (51.24) | 29 (7.66) | <0.001 | 889 (54.70) | 118 (7.21) | <0.001 |
| General medical (%) | 2 (1.90) | 0 (0.00) | <0.001 | 1 (0.35) | 3 (0.90) | <0.001 | 29 (1.78) | 13 (0.78) | <0.001 |
| General medical and surgical (%) | 50 (47.62) | 106 (84.80) | <0.001 | 135 (47.70) | 278 (82.99) | <0.001 | 706 (43.45) | 1,415 (86.49) | <0.001 |
| Teaching hospital (%) | 7 (6.67) | 83 (66.40) | <0.001 | 10 (3.53) | 153 (45.67) | <0.001 | 59 (3.63) | 674 (41.20) | <0.001 |
ED, emergency department.
Regarding adoption of telemedicine during 2012–2017, 3,260 (79.4%) of hospitals had not adopted telemedicine for stroke and/or cardiac care during any year of the study (nonadopter), 230 (5.6%) had stroke and/or cardiac telemedicine in all 6 years of the study (full adopter), and 618 (15.0%) hospitals had stroke and cardiac telemedicine in at least 1 year between 2012 and 2017 (partial adopter). As can be seen in Table 1, the proportion of hospitals in each category differs significantly by rurality.
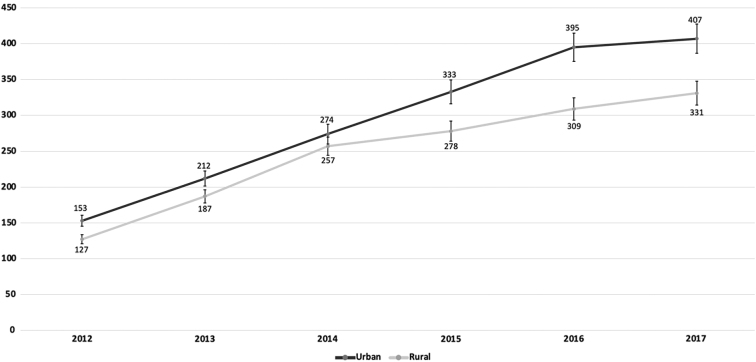
The number of hospitals in urban areas with stroke or cardiac telemedicine services increased through our study period from 153 (7.30%) in 2012 to 407 (19.42%) in 2017 (p < 0.001 for the trend). The number of hospitals in rural areas with stroke or cardiac telemedicine services increased through our study period from 127 (6.31%) in 2012 to 331 (16.45%) in 2017 (p < 0.001 for the trend). The trend in stroke and cardiac telemedicine adoption is shown in Figure 1. Between 2012 and 2017, 78 rural hospitals closed. The median number of beds in the closed hospitals was 31 (IQR: 25 to 49), and none of them provided telemedicine for heart attack or stroke care.
Fig. 1.
Number of U.S. Hospitals with Stroke and Cardiac Telemedicine Program, by urban versus rural.
As can be seen in Table 2, the association between hospitals' characteristics and stroke and cardiac telemedicine adoption varied based on the location of the hospital (e.g., urban vs. rural). In rural hospitals, controlling for other covariates, being a for-profit hospital (e.g., investor owned) was associated with a 10.49 percentage point lower probability of adopting telemedicine for heart attack and stroke care compared to a governmental hospital (AME = −10.49, 95% CI = −14.01 to −6.98). In addition, within rural hospitals, having one more licensed bed (AME = −0.02, 95% CI = −0.04 to −0.00) and a 1% increase in Medicare inpatient mix (AME = −0.31, 95% CI = −0.42 to −0.20) were associated with a decrease in the probability of telemedicine adoption for heart attack and stroke by 0.02 and 0.31 percentage points, respectively. In contrast, controlling for other variables, a higher number of ED visits (AME = 5.64, 95% CI = 2.83 to 7.20) was associated with an increase in the probability of telemedicine adoption for heart attack and stroke care.
Table 2.
Association between Hospital Characteristics and Stroke and Cardiac Telemedicine Adoption (N = 4,108)
| HOSPITAL CHARACTERISTICS | RURAL (N = 2,012) |
URBAN (N = 2,096) |
|---|---|---|
| AVERAGE MARGINAL EFFECT (95% CI) | ||
| Log (ED visit volume per year) | 5.64 (2.73 to 8.20)** | −0.98 (−2.59 to 0.62) |
| Number of licensed beds | −0.02 (−0.04 to 0.00)* | 0.01 (0.01 to 0.02)** |
| Log (distance to the nearest hospital with telemedicine for stroke/cardiac care) | 0.28 (−1.69 to 2.25) | −0.81 (−1.62 to −0.01)* |
| Total margin (%) | 8.0 (−6.01 to 22.02) | 17.01 (8.01 to 26.01)** |
| Days cash on hand | 0.01 (−0.01 to 0.01) | 0.01 (−0.01 to 0.01) |
| Medicare inpatient mix (%) | −31.01 (−42.01 to −20.2)** | 3.01 (−5.01 to 12.01) |
| Hospital teaching status | ||
| Nonteaching hospital | Ref. | |
| Teaching hospital | 4.22 (−1.08 to 9.52) | 1.65 (−0.38 to 3.69) |
| Ownership | ||
| Government, nonfederal | Ref. | |
| Investor owned, for-profit | −10.49 (−14.01 to −6.98)** | −8.94 (−11.76 to −6.11)** |
| Nongovernment, non-for- profit | 0.94 (−2.13 to 4.01) | 2.37 (−0.34 to 5.07) |
| Hospital type | ||
| Academic | Ref. | |
| Critical access hospital | 3.30 (−5.33 to 11.94) | −3.33 (−7.91 to 1.24) |
| General medical and surgical | 6.55 (−1.66 to 14.75) | 0.10 (−2.67 to 2.87) |
⁎p-Value <0.05.
⁎⁎p-Value <0.001.
In urban hospitals, adjusting for other covariates and on average, one more licensed bed (AME = 0.01, 95% CI = 0.041 to 0.02) and higher total margin (AME = 0.17, 95% CI = 0.08 to 0.26) were associated with an increase in the predicted probability of telemedicine adoption for heart attack and stroke care by 0.01 and 0.17 percentage points, respectively. In contrast, controlling for other variables and on average, being a for-profit hospital (AME = −8.94, 95% CI = −11.76 to −6.11) and being closer to another telemedicine hospital (AME = 0.81, 95% CI = −1.62 to 0.01) were associated with a decrease in the probability of telemedicine adoption for heart attack and stroke care. In addition, in urban hospitals, a for-profit hospital had an 8.94 percentage point lower probability of adopting telemedicine for heart attack and stroke care compared to a governmental hospital.
Discussion
The goal of this study was to assess trends in cardiac and stroke telemedicine adoption among U.S. hospitals from 2012 to 2017 and examine association between financial factors and cardiac and stroke telemedicine adoption. We found that while the vast majority of hospitals had not adopted cardiac and stroke telemedicine during any year in our study (around 80%), there was a significant increasing trend in adoption among both urban and rural hospitals (from 7.3% in 2012 to 19.4% in 2017). Some predictors of telemedicine adoption were different between urban and rural hospitals. For example, better financial status was positively associated with higher adoption for urban hospitals but was not a predictor for rural hospitals.
Although the overall rate of adoption for cardiac and stroke telemedicine in the study was low, our study found that adoption has significantly increased from 2012 to 2017, suggesting that some implementation barriers may have been reduced among urban and rural hospitals. One driver may be the increase in the availability of telestroke networks. Prior research suggests that the availability of telestroke networks has grown over time, from less than 22 in 2009 to at least 97 in 2012.9,30 In addition, previous studies showed that cost is among the most commonly cited reason for lack of adoption among hospitals, particularly rural hospitals.31,32 The advancement in telemedicine technology and lowering cost during the past decade may also explain the increase in the rate of telemedicine adoption. In addition, due to the 2009 Health Information Technology for Economic and Clinical Health Act, which provided financial incentives for electronic health records and information exchange, more hospitals now are capable of acquiring such technology. Prior studies also suggest that advances in mobile and cloud computing and mobile applications designed for cardiac care (e.g., screening tools for atrial fibrillation) have made telecardiology easier to implement.33–35 As technology continues to improve, it is possible that telemedicine for cardiac and stroke care will continue to increase. Lack of reimbursement has been a consistent barrier for telemedicine for cardiac care and stroke.36,37 However, this barrier may be changing due to recent legislation expanding Medicare reimbursement for telestroke services (e.g., Furthering Access to Stroke Telemedicine Act) and telemedicine more broadly due to the COVID-19 pandemic. As reimbursement barriers are addressed, telemedicine adoption for stroke and cardiac care may continue to increase.38,39
The positive association of financial status and adoption for urban hospitals, in addition to the negative association of for-profit status and adoption for both urban and rural hospitals, suggests that cardiac and stroke telemedicine services may not currently be feasible for less financially sound hospitals or are not viewed by hospital administrators as having the potential to be profitable. Furthermore, it is possible that profitable urban hospitals are more likely to serve as distant sites for telemedicine services compared to urban hospitals that are less profitable. Similarly, the lack of a statistically significant finding regarding financial status of rural hospitals could suggest that the availability of telemedicine services offered through another hospital that serves as the distant site and a partner in implementing the service may be more important than the hospital's financial status. Again, a changing reimbursement landscape may alter views on the financial feasibility of implementing these services, either as a distant or originating site.
Our findings also suggest that geographic distance between hospitals offering telestroke and telecardiology services may affect adoption of these services. For urban hospitals, being farther from another hospital with the telemedicine services for cardiac and stroke was negatively associated with adoption, suggesting that market competition from other hospitals may be a factor in the adoption decision. This finding is consistent with a prior study on telestroke adoption, suggesting that market competition may influence adoption of telestroke.25 One possible explanation is that the adoption of telestroke and telecardiology in rural hospitals could be contingent on affiliations for other purposes; for example, managing population health through mergers or acquisitions across the rural region, whereas pursuit of a local market competitive edge may be more important for urban hospitals.
Although telemedicine services can be accompanied by high operating costs, prior research suggests that the services also have the potential for significant cost savings for the patient and health system.40 Such savings can come through networks linking physicians and their patients in rural EDs to specialists15,34,40–44 which could increase the use of recommended interventions (e.g., tPA) and, subsequently, avoid unnecessary costs of care.41 Our finding that ED visit volume in rural hospitals is positively associated with telestroke/telecardiology adoption may suggest such efforts. Of course, increasing delivery of recommended interventions and realizing cost savings hinges upon such factors as adopting feasible technologies and processes,45,46 accounting for variation in acceptance and use of the technologies,47,48 and, ultimately, preparing users (both patients and providers) to effectively use the technologies.
LIMITATIONS
Our study has many strengths. The large sample of hospitals that were distributed across all 50 states and the District of Columbia increase the generalizability of the findings. We also developed a master data set that merges the financial information with characteristics of each hospital. Using such unique data set enabled us to include only significant financial factors in the final analysis. Our study also has some limitations. First, we were unable to define the extent to which telemedicine for cardiac and stroke care is deployed in each hospital (e.g., what proportion of patients are treated through telemedicine each year). Second, we were unable to separate stroke and cardiac care since these variables are captured together in the HIMSS dataset. Finally, our analysis does not differentiate between hospitals providing consultations through telemedicine (distant sites) and those receiving telemedicine consultations (originating sites), which may limit our ability to identify implications of results about geographic distance from other hospitals.
Conclusion
Our study found that telemedicine adoption for cardiac and stroke care is low among both urban and rural hospitals, although adoption has increased significantly in recent years. In addition, different factors appear to drive adoption of telestroke and telecardiology among rural and urban hospitals; for example, financial status may be a bigger driver of adoption for urban hospitals than rural hospitals.
Appendix
Appendix Table A1. The List of All Variables Included in the Study
| NAME | DESCRIPTION |
|---|---|
| Outcome variable | |
| Stroke or cardiac care program adoption | Yes, no |
| Explanatory variables | |
| ED visit volume per year | Number of emergency department visits each year |
| Number of beds | Number of beds in each hospital |
| Distance to nearest hospital with telemedicine for stroke and/or cardiac (in miles) | Distant sites are defined as medical centers that provide stroke or cardiac care through telehealth consultation services using synchronous live video to other hospitals |
| Total margin | Net income divided by total revenues (X 100) |
| Days cash on hand | (Cash + marketable securities + unrestricted investments) divided by [(total expenses-depreciation)/days in period] |
| Medicare inpatient payer mix | Medicare inpatient days divided by (total inpatient days − nursery bed days − NF swing bed days) (X 100) |
| Hospital ownership | Government, nonfederal; investor owned, for-profit; nongovernment, not-for-profit |
| Ruralitya | Short-term, nonfederal general facilities that were (1) located outside metropolitan core-based statistical areas, (2) within metropolitan areas and having rural-urban commuting area codes of four or greater, or (3) with critical access hospitalb status |
| Hospital type | Academic, critical access hospital, general medical, general medical and surgical |
| Teaching status | Teaching, nonteaching |
Rurality was defined according to the criteria specified by the Federal Office of Rural Health Policy and other federal programs (https://www.hrsa.gov/rural-health/about-us/definition/index.html).
Acute care hospitals were defined as short-term hospitals that provide care in a range of areas, including emergency medicine; therefore, hospitals that focus on longterm care or specialty care (e.g., cancer hospitals and substance use facilities) were not included.
ED, emergency department.
Disclosure Statement
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the article.
Funding Information
This study was supported by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) under cooperative agreement 6 UICRH29074-01-01. The information, conclusions, and opinions expressed in this brief are those of the authors and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred. Dr. Williams is partially supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of the National Telehealth Center of Excellence Award (U66 RH31458). Dr. Williams was also partially supported by the South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH—NCATS Grant Number UL1 TR001450. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, HRSA, HHS, or the U.S. Government.
REFERENCES
- 1. Garcia MC, Rossen LM, Bastian B, et al. Potentially excess deaths from the five leading causes of death in metropolitan and nonmetropolitan counties—United States, 2010–2017. MMWR Surveill Summ 2019;68:1–11. [DOI] [PubMed] [Google Scholar]
- 2. Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2015;132:873–898. [DOI] [PubMed] [Google Scholar]
- 3. Albright KC, Branas CC, Meyer BC, et al. ACCESS: Acute cerebrovascular care in emergency stroke systems. Arch Neurol 2010;67:1210–1218. [DOI] [PubMed] [Google Scholar]
- 4. Aneja S, Ross JS, Wang Y, et al. US cardiologist workforce from 1995 to 2007: Modest growth, lasting geographic maldistribution, especially in rural areas. Health Aff (Millwood) 2011;30:2301–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Flanders S. Advancing telestroke interventions in an urban ED. Nursing 2019;49:18–20. [DOI] [PubMed] [Google Scholar]
- 6. Hammond G, Luke AA, Elson L, Towfighi A, Joynt Maddox KE. Urban-rural inequities in acute stroke care and in-hospital mortality. Stroke 2020;51:2131–2138. [DOI] [PubMed] [Google Scholar]
- 7. Nathaniel TI, Gainey J, Blum B, Montgomery C, Ervin L, Madeline L. Clinical risk factors in thrombolysis therapy: Telestroke versus nontelestroke. J Stroke Cerebrovasc Dis 2018;27:2524–2533. [DOI] [PubMed] [Google Scholar]
- 8. Nguyen-Huynh MN, Klingman JG, Avins AL, et al. Novel telestroke program improves thrombolysis for acute stroke across 21 hospitals of an integrated healthcare system. Stroke 2018;49:133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: A scientific statement from the American Heart Association/American Stroke Association. Stroke 2009;40:2616–2634. [DOI] [PubMed] [Google Scholar]
- 10. Sharma R, Zachrison KS, Viswanathan A, et al. Trends in telestroke care delivery: A 15-year experience of an academic hub and its network of spokes. Circ Cardiovasc Qual Outcomes 2020;13:e005903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baratloo A, Rahimpour L, Abushouk AI, Safari S, Lee CW, Abdalvand A. Effects of telestroke on thrombolysis times and outcomes: A meta-analysis. Prehosp Emerg Care 2018;22:472–484. [DOI] [PubMed] [Google Scholar]
- 12. Bladin CF, Moloczij N, Ermel S, et al. Victorian stroke telemedicine project: Implementation of a new model of translational stroke care for Australia. Intern Med J 2015;45:951–956. [DOI] [PubMed] [Google Scholar]
- 13. Itrat A, Taqui A, Cerejo R, et al. Telemedicine in prehospital stroke evaluation and thrombolysis: Taking stroke treatment to the doorstep. JAMA Neurol 2016;73:162–168. [DOI] [PubMed] [Google Scholar]
- 14. Boggan JC, Shoup JP, Whited JD, et al. Effectiveness of acute care remote triage systems: A systematic review. J Gen Intern Med 2020;35:2136–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lewinski AA, Rushton S, Van Voorhees E, et al. Implementing remote triage in large health systems: A qualitative evidence synthesis. Res Nurs Health 2021;44:138–154. [DOI] [PubMed] [Google Scholar]
- 16. Satou GM, Rheuban K, Alverson D, et al. Telemedicine in pediatric cardiology: A scientific statement from the American Heart Association. Circulation 2017;135:e648–e678. [DOI] [PubMed] [Google Scholar]
- 17. Tabriz AA, Sohrabi M-R, Kiapour N, Yazdani S. Factors associated with delay in thrombolytic therapy in patients with ST-elevation myocardial infarction. J Tehran Heart Cent 2012;7:65–71. [PMC free article] [PubMed] [Google Scholar]
- 18. Brunetti ND, De Gennaro L, Correale M, et al. Pre-hospital electrocardiogram triage with telemedicine near halves time to treatment in STEMI: A meta-analysis and meta-regression analysis of non-randomized studies. Int J Cardiol 2017;232:5–11. [DOI] [PubMed] [Google Scholar]
- 19. Escobar-Curbelo L, Franco-Moreno AI. Application of telemedicine for the control of patients with acute and chronic heart diseases. Telemed J E Health 2019;25:1033–1039. [DOI] [PubMed] [Google Scholar]
- 20. Marcolino MS, Maia LM, Oliveira JAQ, et al. Impact of telemedicine interventions on mortality in patients with acute myocardial infarction: A systematic review and meta-analysis. Heart 2019;105:1479–1486. [DOI] [PubMed] [Google Scholar]
- 21. Tanguay A, Dallaire R, Hébert D, Bégin F, Fleet R. Rural patient access to primary percutaneous coronary intervention centers is improved by a novel integrated telemedicine prehospital system. J Emerg Med.2015;49:657–664. [DOI] [PubMed] [Google Scholar]
- 22. Molinari G, Molinari M, Di Biase M, Brunetti ND. Telecardiology and its settings of application: An update. J Telemed Telecare 2018;24:373–381. [DOI] [PubMed] [Google Scholar]
- 23. Ward MM, Ullrich F, Mueller K, Rural Health Research & Policy Centers, RUPRI Center for Rural Health Policy Analysis, University of Iowa College of Public Health, Department of Health Management and Policy. Extent of telehealth use in rural and urban hospitals. Rural Policy Brief 2014;4:1–4. [PubMed] [Google Scholar]
- 24. Richard JV, Wilcock AD, Schwamm LH, et al. Assessment of telestroke capacity in US hospitals. JAMA Neurol 2020;77:1035–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shea CM, Tabriz AA, Turner K, North S, Reiter KL. Telestroke adoption among community hospitals in North Carolina: A cross-sectional study. J Stroke Cerebrovasc Dis 2018;27:2411–2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McSweeney S, Pritt JA, Swearingen A, Kimble CA, Coustasse A. Telestroke: Overcoming barriers to lifesaving treatment in rural hospitals. Perspect Health Inform Manage 2017;Summer:1–18. [Google Scholar]
- 27. Adler-Milstein J, Kvedar J, Bates DW. Telehealth among US hospitals: Several factors, including state reimbursement and licensure policies, influence adoption. Health Aff (Millwood) 2014;33:207–215. [DOI] [PubMed] [Google Scholar]
- 28. Williams Jr D, Holmes GM, Song PH, Reiter KL, Pink GH. For rural hospitals that merged, inpatient charges decreased and outpatient charges increased: A pre-/post-comparison of rural hospitals that merged and rural hospitals that did not merge between 2005 and 2015. J Rural Health 2021;37:308–317. [DOI] [PubMed] [Google Scholar]
- 29. Yaffee, Robert. A Primer for Panel Data Analysis. 2005. Available at http://web.pdx.edu/~crkl/ec510/pda_yaffee.pdf (last accessed September 20, 2020).
- 30. Silva GS, Farrell S, Shandra E, Viswanathan A, Schwamm LH. The status of telestroke in the United States: A survey of currently active stroke telemedicine programs. Stroke 2012;43:2078–2085. [DOI] [PubMed] [Google Scholar]
- 31. Zachrison KS, Boggs KM, Hayden EM, Espinola JA, Camargo Jr CA. Understanding barriers to telemedicine implementation in rural emergency departments. Ann Emerg Med 2020;75:392–399. [DOI] [PubMed] [Google Scholar]
- 32. Shea CM, Turner K, Alishahi Tabriz A, North S. Implementation strategies for telestroke: A qualitative study of telestroke networks in North Carolina. Telemed J E Health 2019;25:708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Freedman B. Screening for atrial fibrillation using a smartphone: Is there an app for that? Am Heart Assoc 2016;5:e004000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Goldstein KM, Zullig LL, Dedert EA, et al. Telehealth interventions designed for women: An evidence map. J Gen Intern Med 2018;33:2191–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hsieh J-C, Li A-H, Yang C-C. Mobile, cloud, and big data computing: Contributions, challenges, and new directions in telecardiology. Int J Environ Res Public Health 2013;10:6131–6153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Switzer JA, Demaerschalk BM. Overcoming challenges to sustain a telestroke network. J Stroke Cerebrovasc Dis 2012;21:535–540. [DOI] [PubMed] [Google Scholar]
- 37. Weinstein RS, Lopez AM, Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: Opportunities and barriers. Am J Med 2014;127:183–187. [DOI] [PubMed] [Google Scholar]
- 38. CMS. Medicare telemedicine health care provider fact sheet. 2020. Available at https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (last accessed August 25, 2020).
- 39. Congress. S.431—Furthering Access to Stroke Telemedicine Act: 115th Congress (2017–2018). 2017. Available at https://www.congress.gov/bill/115th-congress/senate-bill/431 (last accessed August 25, 2020).
- 40. Whetten J, van der Goes DN, Tran H, Moffett M, Semper C, Yonas H. Cost-effectiveness of Access to Critical Cerebral Emergency Support Services (ACCESS): A neuro-emergent telemedicine consultation program. J Med Econ 2018;21:398–405. [DOI] [PubMed] [Google Scholar]
- 41. Halbert K, Bautista C. Telehealth use to promote quality outcomes and reduce costs in stroke care. Crit Care Nurs Clin North Am 2019;31:133–139. [DOI] [PubMed] [Google Scholar]
- 42. Nelson RE, Saltzman GM, Skalabrin EJ, Demaerschalk BM, Majersik JJ. The cost-effectiveness of telestroke in the treatment of acute ischemic stroke. Neurology 2011;77:1590–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nelson RE, Okon N, Lesko AC, Majersik JJ, Bhatt A, Baraban E. The cost-effectiveness of telestroke in the Pacific Northwest region of the USA. J Telemed Telecare 2016;22:413–421. [DOI] [PubMed] [Google Scholar]
- 44. Tabriz AA, Trogdon JG, Fried BJ. Association between adopting emergency department crowding interventions and emergency departments' core performance measures. Am J Emerg Med 2020;38:258–265. [DOI] [PubMed] [Google Scholar]
- 45. Scheuermeyer FX, Grunau BE, Findlay T, et al. Speed and accuracy of text-messaging emergency department electrocardiograms from a small community hospital to a provincial referral center. J Telemed Telecare 2016;22:105–113. [DOI] [PubMed] [Google Scholar]
- 46. Shetty R, Samant J, Nayak K, Maiya M, Reddy S. Feasibility of telecardiology solution to connect rural health clinics to a teaching hospital. Indian J Community Med 2017;42:170–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reddy R, Majmudar M, Dhopeshwarkar N, Vacaro V, Isselbacher E, Bhatt AB. Mobile health apps preferences and practice among ambulatory cardiovascular patients. Fut Cardiol 2018;14:381–388. [DOI] [PubMed] [Google Scholar]
- 48. Sears SF, Kropp CM, Tripp C, et al. Evaluation and acceptance of mobile-electrocardiogram use in implantable cardioverter defibrillator patients—Can I see my ECG? Pacing Clin Electrophysiol 2020;43:254–257. [DOI] [PubMed] [Google Scholar]