Abstract
A number of pharmaceuticals have been identified as potential adjuvants to speech language therapy following stroke, but it is also important to consider which pharmaceuticals may result in a less robust recovery. Here we examine whether post-stroke language recovery was meaningfully impeded by cholinergic, GABAergic, or dopaminergic medications patients received. Eighty participants with left hemisphere stroke were examined retrospectively to see whether the use of one of these three classes of medication prior to admission for acute stroke, during their inpatient stay, or at discharge was associated with differences in recovery on three common measures of language. While prescription of any of the candidate drugs was relatively uncommon, groups were very well matched for many common factors that impact performance. When age, education, and acute lesion volume were controlled, there were no significant differences in performance among those taking cholinergic, GABAergic, or dopaminergic medications and those who were not. Those who experienced a “good recovery” of language (≥10% improvement on any one language measure over time) had similar exposure to these drugs to those with a poor recovery. This work represents a first look at these drug classes with regard to their effects on the recovery of language after stroke and should not be interpreted as resolving all potential for concern, but these results do offer modest reassurance that these common classes of pharmacotherapy, when given for short periods in this population, do not appear to have marked deleterious effects on post-stroke recovery of language.
Introduction
Speech and language therapy is the standard treatment of post-stroke aphasia [1]. A number of pharmaceuticals have been identified as potential adjuvants to speech language therapy, leading to numerous active lines of research [see 2, for review, 3]. Most notably, there is evidence that cholinergic [NCT04134416; 4–6], GABAergic [NCT00227461; 7–11], and serotonergic mechanisms [NCT03843463; 12–14] may facilitate plasticity-dependent recovery of language. Given such findings, it is at least as important to consider underlying mechanisms of pharmaceuticals that may result in a less robust recovery from stroke.
Barbiturates [15–18], alpha blockers [19], benzodiazepines [20], dopamine antagonists [21–23], and norepinephrine-dopamine reuptake inhibitors [20] all have demonstrated deleterious effects on post-stroke recovery. Moreover, recent work has sparked enthusiastic investigation of cholinergic antagonists for their contribution to cognitive decline when taken long term [24–28]. This research has been spurred in part by the mild beneficial effect of cholinesterase inhibitors on reducing the rate of cognitive decline in Alzheimer’s disease.
These concurrent observations of pharmaceutical activity associated with recovery along with the potential for detrimental cognitive effects of other medications has led to the present investigation. Here we examine whether post-stroke recovery in our patients with left hemisphere strike was meaningfully impeded by medications they received to address co-morbid diagnoses or manage symptoms. Three candidate mechanisms were examined in our longitudinal retrospective cohort of patients with left-hemisphere stroke: cholinergic (e.g., competitive nicotinic acetylcholine (ACh) receptor antagonists, "reversible" carbamate inhibitors, muscarinic receptor antagonists), GABAergic (e.g., benzodiazepines, barbiturates), and dopaminergic (e.g., DAT ligands, 5-HT2A and D2 antagonists, triptans).
Methods
Records reviewed
A total of 80 participants with left hemisphere ischemic lesions were identified through an ongoing longitudinal protocol investigating stroke recovery that were approved by the Johns Hopkins University School of Medicine Institutional Review Board. All participants provided written consent and were 18+ year-old proficient English speakers with normal or corrected-to-normal vision and hearing and did not demonstrate history of neurologic conditions affecting the brain other than stroke. In order to be included in this analysis, participants had to have been evaluated during the acute phase of recovery, and then again during the chronic phase of recovery, using one or more of three classic outcome measures of aphasia: the aphasia quotient (AQ, i.e., severity) from the Western Aphasia Battery [WAB, an omnibus measure of language; 29], the Boston Naming Test (BNT; picture naming of nouns), and the amount of previously identified and normed content (“content units”; CUs) provided when describing the Cookie Theft picture from the Boston Diagnostic Aphasia Examination [30].
The acute phase of recovery is defined as within the first week following stroke, often the same day as admission (Mean = 3 days after stroke ± 3 days). The chronic phase of recovery is defined as at least 6 months after stroke. Per the longitudinal protocol, patients were contacted for follow up during the chronic phase at 6 and 12 months after stroke; although, a small number were evaluated two or more years after stroke (N = 9; 11%). Performance during the chronic period generally has stabilized; thus, if a participant was seen for more than one evaluation after 6 months, their performance across these timepoints was averaged. Change was then quantified by calculating the difference in performance scores between the acute and chronic phases, divided by the acute score to normalize the change regardless of initial acute severity. Where acute scores were 0, an artificial minimal score of 1 on the WAB was used to calculate the corrected improvement.
During the period of longitudinal data collection, the classic Cookie Theft image was replaced with a more contemporary, color image [31]. 42 patients described only the classic Cookie Theft image, 12 patients described only the new image, and 10 patients described both. These images are not interchangeable, with the updated version containing significantly greater total content. However, change in CU divided by baseline CU is comparable, and was statistically similar in this sample (Old: Mean change in content units = 2 units, SD = 4; New: Mean = 2, SD = 4 units; t(62) = 0.10, p = 0.91). Therefore, in order to maximize sample size, performance on either the old or new Cookie Theft was used and, if both pictures were administered, the change in each was calculated separately and then averaged.
Prescription records
Prescription records were obtained from the electronic medical records at three distinct time points. Medications prior to stroke were deduced from initial neurology history and physical notes at admission and cross referenced with discharge summary notes, as many patients are unable to communicate medical history at admission but later may improve or have family who provide additional history. Scheduled inpatient medications were found in the electronic Medication Administration Record (MAR). For 26 patients (those whose hospitalization was before January 2015), these records could not be accessed due to a change in the underlying electronic record system. Discharge medications were found in the discharge summaries. Though we recognize the possibility that discharged patients could choose not to comply with prescriptions, it was assumed that prescribed medications were used in the intervening months between hospitalization and follow-up. Prescription drug lists for candidate mechanisms are shown in S1 File. Drug list, informed by Goodman & Gilman’s [32], DailyMed (https://dailymed.nlm.nih.gov/dailymed/), and U.S. Food and Drug Administration approval history. There were 153 drugs identified.
Lesion/infarct segmentation
Acute ischemic lesions were delineated and quantified manually by researchers and clinicians experienced in lesion segmentation using standard of care diffusion weighted images (DWI; N = 75). Trained study team members manually traced lesions on DWI scans using MRIcron or MRIcroGL (available at nitrc.org). Tracings then were verified by experienced researchers. We used routines from SPM12 (Statistical Parameter Mapping; https://www.fil.ion.ucl.ac.uk/spm/software/spm12/) to warp each patient’s DWI b0 image to a healthy older adult template [33] and subsequently applied the normalization parameters to the lesion map. We calculated the volume of the normalized lesion map (in mm3) using NiiStat (https://www.nitrc.org/projects/niistat/).
Statistical analysis
Two complementary analyses were planned. First, a multivariable analysis of variance was conducted in which the Western Aphasia Battery AQ, Boston Naming Test, and Cookie Theft content units were dependent variables and whether a cholinergic, GABAergic, or dopaminergic drug was administered at any point (i.e., collapsing across pre-stroke, scheduled during hospitalization, and discharge time points) were fixed factors (α = 0.05/3 = 0.017). Given the small samples available for each permutation of mechanism and time point, we decided to collapse across timepoints for a given drug mechanism.
In a complementary analysis done to maximize the analyzable data, standardized differences in WAB-AQ, BNT, and CU were dichotomized into individuals with 10% or greater improvement on any of the three measures (“good recovery”) and those who did not show at least 10% improvement on any of the three measures (“poor recovery”). This allowed for much more similar group numbers for comparison. Recovery groups then were examined for the likelihood of taking a drug with a given mechanism. Data are available in S2 File.
Results
Description of groups
Overall, prescription of any of the candidate drugs was relatively uncommon in our sample and included only 26 of the 153 identified products (Table 1). Despite a fairly large number of records available, only 13 individuals had been on a cholinergic at any time, 14 had been on a GABAergic medication, and 16 had been on a dopaminergic medication. A total of 31 individuals had been prescribed any of the three at any time point examined. One patient, a 62-year-old male who received both a GABAergic and dopaminergic scheduled during admission experienced a recovery on the WAB from an AQ of 0.3 (global aphasia) to an AQ of 51.5 at 6 months post-stroke (standardized improvement of 171.67). In order to utilize this patient in analysis, an artificial minimal score of 1 on the WAB was used to calculate the corrected improvement. This outlier patient was not included in Fig 1.
Table 1. N prescriptions by drug class.
| Drug | Admission | Inpatient | Discharge | Total |
|---|---|---|---|---|
| Cholinergic | 6 | 8 | 9 | 23 |
| Nicotine | 1 | 5 | 3 | 9 |
| Ipratropium | 1 | 1 | 2 | 4 |
| Cyclobenzaprine | 2 | 0 | 1 | 3 |
| Carisoprodol | 1 | 1 | 0 | 2 |
| Dicyclomine | 1 | 0 | 1 | 2 |
| Scopolamine | 0 | 1 | 0 | 1 |
| Solifenacin | 0 | 0 | 1 | 1 |
| Tiotropium | 0 | 0 | 1 | 1 |
| GABAergic | 4 | 15 | 3 | 22 |
| Lorazepam | 0 | 8 | 0 | 8 |
| Alprazolam | 1 | 1 | 0 | 2 |
| Midazolam | 0 | 2 | 0 | 2 |
| Valproate | 0 | 1 | 0 | 1 |
| Zolpidem | 1 | 0 | 0 | 1 |
| Gabapentin | 2 | 2 | 3 | 7 |
| Zonisamide | 0 | 1 | 0 | 1 |
| Dopaminergic | 13 | 9 | 10 | 32 |
| Pramipexole | 2 | 1 | 2 | 5 |
| Quetiapine | 2 | 1 | 2 | 5 |
| Trazodone | 1 | 2 | 2 | 5 |
| Bupropion | 1 | 1 | 2 | 4 |
| Duloxetine | 1 | 1 | 1 | 3 |
| Ondansetron | 1 | 2 | 0 | 3 |
| Amphetamine | 1 | 0 | 1 | 2 |
| Asenapine | 1 | 1 | 0 | 2 |
| Methylphenidate | 1 | 0 | 0 | 1 |
| Nortriptyline | 1 | 0 | 0 | 1 |
| Sumatriptan | 1 | 0 | 0 | 1 |
N refers to number of prescriptions summed across timepoints, not number of people with a prescription, and were not necessarily mutually exclusive cases.
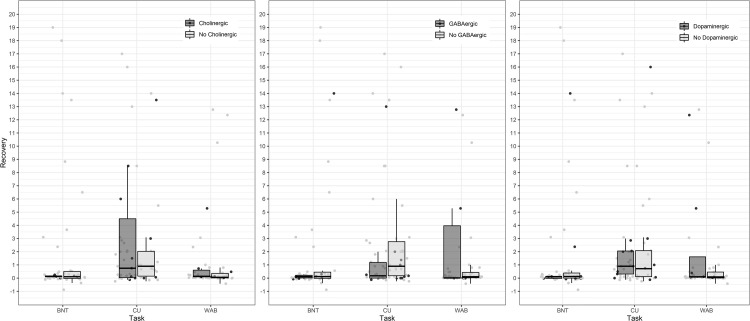
Fig 1. Change in performance by group.
Scores in the table reflect standardized difference scores between acute performance and average chronic performance. In each case, the drug group is represented by the darker grey, while the no drug group is represented in lighter grey. Data points are jittered slightly on the x-axis to increase visibility of overlapping scores (within task x-axis differences are not meaningful). The outlier patient previously described with an improvement in WAB AQ of 51.5 was not included in the figure.
Cholinergic
Individuals who had received a cholinergic prescription were age-matched to individuals who did not receive a cholinergic (t(77) = 1.29, p = 0.20). They had similar levels of education (t(75) = 1.71, p = 0.09). Where available (N = 75) acute lesion volume (t(73) = 1.75, p = 0.08) between the two groups was considered and also found not to be significantly different between groups. There were no differences based on Fisher’s exact tests of sex (p = 0.11), handedness (p = 1.0), likelihood of having diabetes (DM; p = 1.0), hypertension (HTN; p = 1.0), or psychiatric diagnoses (Psy; p = 1.0). Groups also were matched on acute aphasia severity as measured by WAB AQ (Drug: 66.3±37.7, No Drug: 75.4±30.0, t(51) = 0.79, p = 0.43).
GABAergic
Those taking a GABAergic prescription tended to be younger at the time of their stroke (t(77) = 2.76, p = 0.007). There were no differences in sex (p = 0.37), handedness (p = 0.42), DM (p = 1.0), HTN (p = 0.63), or psychiatric diagnoses (p = 0.61), education (t(75) = 0.70, p = 0.48), or lesion volume (t(73) = 0.56, p = 0.58). Groups also were matched on acute aphasia severity as measured by WAB AQ (Drug: 68.5±44.3, No Drug: 75.3±27.3, t(51) = 0.63, p = 0.53).
Dopaminergic
Individuals with and without dopaminergic prescriptions were matched in all dimensions examined: age (t(77) = 1.87, p = 0.07), education (t(75) = 0.18, p = 0.86), lesion volume (Levene’s F = 2.5, p = 0.037, corrected t(13.68) = 0.93, p = 0.37), sex (p = 0.83), handedness (p = 0.47), DM (p = 1.0), HTN (p = 0.35), and Psy (p = 0.18). Groups also were matched on acute aphasia severity as measured by WAB AQ (Drug: 65.9±40.1, No Drug: 76.2±28.2, t(51) = 1.01, p = 0.32).
Multivariate analysis of variance
Improvement on each measure by individuals in each drug group is summarized in Table 2. When age, education, and acute lesion volume were controlled, Pillai’s trace was not significant for any substance: cholinergic (V = 0.07; F(3, 10) = 0.23, p = 0.87), GABAergic (V = 0.04; F(3, 10) = 0.13, p = 0.94) or dopaminergic (V = 0.02; F(3, 10) = 0.06, p = 0.98). The assumption of homogeneity of variances was upheld for all contrasts.
Table 2. Demographic and performance summary by mechanism.
| M:F | Age | Edu | Hand | Vol | DM | HTN | Psy | WAB | BNT | CU | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cholinergic | 7:5 | 12 | 13 | 12;1 | 12 | 4;8 | 11;1 | 1;11 | 7 | 5 | 11 |
| 56.5±13.90 | 13.08±2.14 | 51475±74118 | 0.98±1.92 | 0.13±0.09 | 3.03±4.49 | ||||||
| No Cholinergic | 30:37 | 67 | 64 | 58;7 | 63 | 23;44 | 60;7 | 7;59 | 39 | 40 | 43 |
| 61.5±12.09 | 14.51±2.85 | 24111±43950 | 2.49±8.66 | 2.27±5.09 | 2.47±4.4 | ||||||
| GABAergic | 9:5 | 14 | 13 | 12;1 | 14 | 5;9 | 12;2 | 2;11 | 7 | 7 | 11 |
| 52.79±14.05 | 13.77±2.35 | 38049±75911 | 9.94±18.94 | 2.07±5.26 | 1.62±3.84 | ||||||
| No GABAergic | 28:37 | 65 | 64 | 58;7 | 61 | 22;43 | 59;6 | 6;59 | 39 | 38 | 43 |
| 62.45±11.44 | 14.37±2.87 | 26296±43060 | 0.88±2.55 | 2.02±4.83 | 2.83±4.51 | ||||||
| Dopaminergic | 8:8 | 16 | 14 | 13;2 | 13 | 5;11 | 13;3 | 3;12 | 9 | 9 | 13 |
| 55.63±13.68 | 14.14±2.25 | 45146±75961 | 7.76±16.92 | 1.84±4.63 | 2.25±4.26 | ||||||
| No Dopaminergic | 29:34 | 63 | 63 | 57;6 | 62 | 22;41 | 58;5 | 5;58 | 37 | 36 | 41 |
| 62.03±11.83 | 14.29±2.90 | 24997±43256 | 0.92±2.67 | 2.07±4.95 | 2.68±4.46 |
Continuous variables are reported as N Mean ± Standard Deviation. Edu: Education (in years). Hand: Handedness right: left. Vol: Acute lesion volume (mm3). DM: Diabetes mellitus present;absent. HTN: hypertension present;absent. Psy: mental health diagnosis in chart at the time of admission present;absent. For assessments, scores in the table reflect standardized difference scores between acute performance and average chronic performance. Higher numbers are associated with greater recovery. WAB: Western Aphasia Battery Aphasia Quotient (omnibus measure of language). BNT: Boston Naming Test (picture naming of nouns). CU: Cookie Theft content units (content provided when describing a picture).
As shown in Fig 1, there was a large range in recovery scores for each test, for patients with each of the potentially detrimental medications. Although there might appear to exist a slight trend for patients without GABAergic drugs to show more improvement in CU and less improvement on the WAB, the opposite directions of the trends make it likely that these trends are not reliable or meaningful. As indicated by the individual data points, these trends are probably due to 1–2 outliers, like the apparent trend for patients on cholinergic antagonists to show more improvement in CU.
Likelihood of good recovery
Of the 80 patients examined, half were identified as having made a good recovery (≥ 10% improvement on any of the three language measures examined). Recovery groups were matched in age at the time of stroke (t(77) = 1.02, p = 0.31), education (t(75) = 0.71, p = 0.48), lesion volume (t(73) = 1.1, p = 0.27), sex (p = 0.82), handedness (p = 0.10); DM (p = 1.0); HTN (p = 1.0), and likelihood of a mental health diagnosis (p = 0.26; Table 3). Individuals who experienced a good recovery had nearly identical likelihoods to those with poor recovery of have been taking a cholinergic (p = 1.0), GABAergic (p = 0.77), or dopaminergic (0.40) drug (Table 4). When explored, pre-admission, scheduled inpatient, and discharge timepoints considered separately were not associated with any significant differences.
Table 3. Demographic and performance summary by recovery group.
| M:F | Age | Edu | Hand | Vol | DM | HTN | Psy | WAB | BNT* | CU* | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Good recovery | 19:20 | 39 | 37 | 32; 6 | 37 | 13;26 | 35;4 | 2;36 | 19 | 20 | 27 |
| 62.2±12.74 | 14.5±2.93 | 34983±42770 | 5.16±11.98 | 4.61±6.44 | 4.80±5.34 | ||||||
| Poor recovery | 18:22 | 40 | 40 | 38;2 | 38 | 14;26 | 36;4 | 6;34 | 27 | 25 | 27 |
| 59.33±12.07 | 14.05±2.65 | 22167±56665 | 0.22±1.02 | -0.03±0.21 | 0.36±0.54 |
*p < 0.01. Continuous variables are reported as N Mean ± Standard Deviation. Edu: Education (in years). Hand: Handedness right; left. Vol: Acute lesion volume (mm3). DM: Diabetes mellitus present; absent. HTN: hypertension present; absent. Psy: mental health diagnosis in chart at the time of admission present; absent. For assessments, scores in the table reflect standardized difference scores between acute performance and average chronic performance. Higher numbers are associated with greater recovery. WAB: Western Aphasia Battery Aphasia Quotient (omnibus measure of language). BNT: Boston Naming Test (picture naming of nouns). CU: Cookie Theft content units (content provided when describing a picture).
Table 4. Patient grouping by recovery group and drug mechanism.
| Good | Poor | |
|---|---|---|
| N = 40 | N = 40 | |
| Cholinergic | 6 | 7 |
| No Cholinergic | 34 | 33 |
| GABAergic | 6 | 8 |
| No GABAergic | 34 | 32 |
| Dopaminergic | 6 | 10 |
| No Dopaminergic | 34 | 30 |
Discussion
In this investigation, we examined whether three candidate drug classes with the mechanistic potential to interrupt or impede neuroplasticity were associated with measurable differences in language recovery after stroke, as measured using an omnibus language assessment (WAB), picture naming task (BNT), and picture description task (Cookie Theft). When controlling for other important group differences in demographic factors and health status, neither a general linear model-based analysis nor an analysis of the contingency tables produced evidence that there was a detrimental effect (or, indeed, any effect) of cholinergic, GABAergic, or dopaminergic prescriptions on language recovery. Overall, there were relatively few individuals within our sample who had been prescribed the drugs under consideration whether prior to admission, during hospitalization, or at discharge. This low signal within our sample led us to adopt a multi-pronged statistical approach.
Recently there has been more interest in studying potential beneficial pharmaceuticals such as serotonergic drugs [12] and neuro-stimulants [34, 35] in a controlled clinical trial setting to promote post-stroke recovery. It is equally crucial to avoid medications that may interfere with the post-stroke recovery in accordance with the “first, do no harm” principle. However, it is unethical to design a research study in which potentially harmful medications are tested directly. Thus, despite the inherent limitations and biases of retrospective analysis, these studies play a crucial role in guiding treating clinicians in their therapeutic armamentarium when dealing with various post-stroke impairments and complications in a balanced fashion.
Although the goal of the study was not to study drug prescription patterns after stroke, we observed that GABAergic medications were prescribed more commonly for younger patients. We speculate that the treating clinicians might have liberally chosen pharmacotherapy over other methods (e.g., physical restraint) to control post-stroke agitation and/or anxiety. Larger studies matching clinical indications for GABAergic medications are needed to further investigate prescription patterns and their potential effect on post-stroke recovery in different age groups. It also is interesting to note that certain drugs perceived to enhance cognitive performance were not readily prescribed in our sample despite recognized safety and efficacy profiles in the acute stroke period [36, 37]. This reinforces the notion that continuing research on the pharmacotherapy of post-stroke aphasia is imperative to gain further knowledge on the detrimental and beneficial drugs for poststroke aphasia and eventually translating research findings to clinical practice [38]. Important initiatives in this direction are ongoing [39, 40].
This work represents a first look at these drug classes with regard to their effects on the recovery of language after stroke and should not be interpreted as resolving all potential for concern. There are some important limitations of this work that temper our ability to generalize from these findings. First, these analyses are likely underpowered. Relatively few individuals in our sample had any record of having taken any of the drugs we examined. Nevertheless, there were no strong trends that would suggest that a significant effect would emerge with greater power. Second, there were a number of potential sources of variability we were unable to control due to small sample size. We did not examine patients’ over-the-counter drug or substance use, nor did we have the information with which to ensure patients had complied with drugs prescribed at admission or discharge. We have not included drug route of administration and dosages in the analysis, and we were forced to collapse across time points we did have (admission versus inpatient versus discharge) in order to maximize the usable data. It seems plausible that effect sizes are sufficiently small that only over long-term/life-long exposure are candidate mechanisms worthy of concern and that the window in which we examined our patients–from admission to discharge–was too narrow for an effect to be seen. Finally, certain information about these patients was unavailable, namely the administration of hyperacute rTPA and the availability or duration of behavioral speech-language therapy. We feel it is safe to presume that rTPA would have been used if consented to among patients for whom it was appropriate and that the amount, character, and duration of speech therapy was provided as clinically indicated.
Nevertheless, these results offer modest reassurance that these common classes of pharmacotherapy, when given for short periods in this population do not appear to have marked deleterious effects on post-stroke recovery of language. Additional prospective analyses with greater specificity with regard to mechanism and duration are needed to fully appreciate the relationship these drugs may play in plasticity-dependent recovery of language in the post-stroke period.
Supporting information
(DOCX)
(XLSX)
Acknowledgments
We are grateful for the tireless efforts of the numerous research assistants who have assisted in the collection of acute and chronic data over many years.
Data Availability
The minimal underlying data set is included in the Supporting Information.
Funding Statement
This work is supported by National Institutes of Health/National Institute on Deafness and Other Communication Disorders (NIH/NIDCD): R01 DC005375 and P50 DC011739 and was approved by the Johns Hopkins University School of Medicine Institutional Review Board (NA_00042097). The MRI equipment in this study was funded by NIH grant 1S10OD021648. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kurland J, Pulvermüller F, Silva N, Burke K, Andrianopoulos M. Constrained versus unconstrained intensive language therapy in two individuals with chronic, moderate-to-severe aphasia and apraxia of speech: behavioral and fMRI outcomes. Am J Speech Lang Pathol. 2012. doi: 10.1044/1058-0360(2012/11-0113) [DOI] [PubMed] [Google Scholar]
- 2.Stockbridge MD. Better language through chemistry: Augmenting speech-language therapy with pharmacotherapy in the treatment of aphasia. Handbook of Clinical Neurology: Aphasia. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keser Z, Francisco GE. Neuropharmacology of poststroke motor and speech recovery. Physical Medicine and Rehabilitation Clinics. 2015;26(4):671–89. doi: 10.1016/j.pmr.2015.06.009 [DOI] [PubMed] [Google Scholar]
- 4.Zhang X, Shu B, Zhang D, Huang L, Fu Q, Du G. The Efficacy and Safety of Pharmacological Treatments for Post-stroke Aphasia. CNS & Neurological Disorders—Drug Targets. 2018;17(7):509–21. doi: 10.2174/1871527317666180706143051 [DOI] [PubMed] [Google Scholar]
- 5.Berthier ML, Green C, Higueras C, Fernandez I, Hinojosa J, Martín M. A randomized, placebo-controlled study of donepezil in poststroke aphasia. Neurology. 2006;67(9):1687–9. doi: 10.1212/01.wnl.0000242626.69666.e2 [DOI] [PubMed] [Google Scholar]
- 6.Berthier ML, Hinojosa J, del Carmen Martín M, Fernández I. Open-label study of donepezil in chronic poststroke aphasia. Neurology. 2003;60(7):1218–9. doi: 10.1212/01.wnl.0000055871.82308.41 [DOI] [PubMed] [Google Scholar]
- 7.Tanaka Y, Albert ML, Yokoyama E, Nonaka C, Aketa S, Hujita K, et al. 126th Annual Meeting, American Neurological Association Rehabilitation, Regeneration, and Recovery: 200. Cholinergic Therapy for Anomia in Fluent Aphasia [abstract]. Ann Neurol. 2001;50(3S):S61–S2. [Google Scholar]
- 8.Huber W. The role of piracetam in the treatment of acute and chronic aphasia. Pharmacopsychiatry. 1999;32(S 1):38–43. doi: 10.1055/s-2007-979235 [DOI] [PubMed] [Google Scholar]
- 9.Enderby P, Broeckx J, Hospers W, Schildermans F, Deberdt W. Effect of piracetam on recovery and rehabilitation after stroke: a double-blind, placebo-controlled study. Clin Neuropharmacol. 1994;17(4):320–31. doi: 10.1097/00002826-199408000-00003 [DOI] [PubMed] [Google Scholar]
- 10.Huber W, Poeck K, Weniger D, Willmes K. Der Aachener Aphasie Test. Göttingen, Germany: Hogrefe-Verlag; 1982. [Google Scholar]
- 11.Berthier ML, Pulvermüller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nature Reviews Neurology. 2011;7(2):86. doi: 10.1038/nrneurol.2010.201 [DOI] [PubMed] [Google Scholar]
- 12.Hillis AE, Beh YY, Sebastian R, Breining B, Tippett DC, Wright A, et al. Predicting recovery in acute poststroke aphasia. Ann Neurol. 2018;83(3):612–22. doi: 10.1002/ana.25184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hillis AE, Tippett DC. Stroke recovery: Surprising influences and residual consequences. Advances in medicine. 2014;2014. doi: 10.1155/2014/378263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorge RE, Acion L, Moser D, Adams HP, Robinson RG. Escitalopram and enhancement of cognitive recovery following stroke. Arch Gen Psychiatry. 2010;67(2):187–96. doi: 10.1001/archgenpsychiatry.2009.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linn L, Stein M. Sodium amytal in treatment of aphasia; preliminary report. Bulletin of the US Army Medical Department United States Army Medical Department. 1946;5:705–8. [PubMed] [Google Scholar]
- 16.Linn L. Sodium amytal in treatment of aphasia. Arch Neurol Psychiatry. 1947;58(3):357–8. doi: 10.1001/archneurpsyc.1947.02300320108007 [DOI] [PubMed] [Google Scholar]
- 17.Bergman PS, Green M. Aphasia: effect of intravenous sodium amytal. Neurology. 1951;1(11–12):471–5. doi: 10.1212/wnl.1.11-12.471 [DOI] [PubMed] [Google Scholar]
- 18.D’Asaro MJ. An experimental investigation of the effects of sodium amytal on communication of aphasic patients: University of Southern California; 1955. [Google Scholar]
- 19.Llano DA, Small SL. Biological approaches to treatment of aphasia. In: Hillis AE, editor. The handbook of adult language disorders. 2nd ed. New York, NY: Psychology Press; 2015. p. 435. [Google Scholar]
- 20.Darley FL, Keith RL, Sasanuma S, editors. The effect of alerting and tranquilizing drugs upon the performance of aphasic patients. Clinical Aphasiology: Proceedings of the Conference 1977; 1977: BRK Publishers.
- 21.Feeney DM, Gonzalez A, Law WA. Amphetamine, haloperidol, and experience interact to affect rate of recovery after motor cortex injury. Science. 1982;217(4562):855–7. doi: 10.1126/science.7100929 [DOI] [PubMed] [Google Scholar]
- 22.Feeney DM, Hovda DA. Amphetamine and apomorphine restore tactile placing after motor cortex injury in the cat. Psychopharmacology. 1983;79(1):67–71. doi: 10.1007/BF00433018 [DOI] [PubMed] [Google Scholar]
- 23.Porch B, Wyckes J, Feeney D, editors. Haloperidol, thiazides and some antihypertensives slow recovery from aphasia. Soc Neurosci Abstr; 1985. [Google Scholar]
- 24.Gray SL, Anderson ML, Dublin S, Hanlon JT, Hubbard R, Walker R, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA internal medicine. 2015;175(3):401–7. doi: 10.1001/jamainternmed.2014.7663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chuang Y-F, Elango P, Gonzalez CE, Thambisetty M. Midlife anticholinergic drug use, risk of Alzheimer’s disease, and brain atrophy in community-dwelling older adults. Alzheimer’s & Dementia: Translational Research & Clinical Interventions. 2017;3(3):471–9. doi: 10.1016/j.trci.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell NL, Lane KA, Gao S, Boustani MA, Unverzagt F. Anticholinergics influence transition from normal cognition to mild cognitive impairment in older adults in primary care. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2018;38(5):511–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.López-Álvarez J, Sevilla-Llewellyn-Jones J, Agüera-Ortiz L. Anticholinergic drugs in geriatric psychopharmacology. Front Neurosci. 2019;13:1309. doi: 10.3389/fnins.2019.01309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marzoughi S, Banerjee A, Jutzeler CR, Prado MA, Rosner J, Cragg JJ, et al. Tardive neurotoxicity of anticholinergic drugs: A review. J Neurochem. 2021. doi: 10.1111/jnc.15244 [DOI] [PubMed] [Google Scholar]
- 29.Kertesz A. Western aphasia battery. New York: Grune & Stratton. 1982. [Google Scholar]
- 30.Goodglass H, Kaplan E, Weintraub S. BDAE: The Boston Diagnostic Aphasia Examination: Lippincott Williams & Wilkins; Philadelphia, PA; 2001. [Google Scholar]
- 31.Berube S, Nonnemacher J, Demsky C, Glenn S, Saxena S, Wright A, et al. Stealing cookies in the twenty-first century: Measures of spoken narrative in healthy versus speakers with aphasia. Am J Speech Lang Pathol. 2019;28(1S):321–9. doi: 10.1044/2018_AJSLP-17-0131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brunton LL, Hilal-Dandan R, Knoll M, Bjorn C, editors. Goodman and Gilman’s: The Pharmacological Basis of Therapeutics. 13 ed. New York: McGraw-Hill; 2018. [Google Scholar]
- 33.Rorden C, Bonilha L, Fridriksson J, Bender B, Karnath H-O. Age-specific CT and MRI templates for spatial normalization. Neuroimage. 2012;61(4):957–65. doi: 10.1016/j.neuroimage.2012.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker-Batson D. Amphetamine and post-stroke rehabilitation: indications and controversies. Eur J Phys Rehabil Med. 2013;49(2):251–60. [PubMed] [Google Scholar]
- 35.Keser Z, Dehgan MW, Shadravan S, Yozbatiran N, Maher LM, Francisco GE. Combined dextroamphetamine and transcranial direct current stimulation in poststroke aphasia. Am J Phys Med Rehabil. 2017;96(10):S141–S5. doi: 10.1097/PHM.0000000000000780 [DOI] [PubMed] [Google Scholar]
- 36.Zhang J, Wei R, Chen Z, Luo B. Piracetam for aphasia in post-stroke patients: a systematic review and meta-analysis of randomized controlled trials. CNS Drugs. 2016;30(7):575–87. doi: 10.1007/s40263-016-0348-1 [DOI] [PubMed] [Google Scholar]
- 37.Barrett KM, Brott TG, Brown RD Jr, Carter RE, Geske JR, Graff-Radford NR, et al. Enhancing recovery after acute ischemic stroke with donepezil as an adjuvant therapy to standard medical care: results of a phase IIA clinical trial. J Stroke Cerebrovasc Dis. 2011;20(3):177–82. doi: 10.1016/j.jstrokecerebrovasdis.2010.12.009 [DOI] [PubMed] [Google Scholar]
- 38.Berthier ML. Ten key reasons for continuing research on pharmacotherapy for post-stroke aphasia. Aphasiology. 2021;35(6):824–58. [Google Scholar]
- 39.Ali M, Ben Basat AL, Berthier M, Blom Johansson M, Breitenstein C, Cadilhac D, et al. Protocol for the development of the international population registry for aphasia after stroke (I-PRAISE). Aphasiology. 2021:1–21.35002009 [Google Scholar]
- 40.Stockbridge MD, Fridriksson J, Sen S, Bonilha L, Hillis AE. Protocol for Escitalopram and Language Intervention for Subacute Aphasia (ELISA): A randomized, double blind, placebo-controlled trial. PLoS One. 2021;16(12):e0261474. doi: 10.1371/journal.pone.0261474 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(XLSX)
Data Availability Statement
The minimal underlying data set is included in the Supporting Information.