Abstract
Purpose
To evaluate the 12-month outcomes of a novel posterior small incision sub-tenon ab interno technique of XEN stent insertion (‘Semi-open’).
Method
Consecutive eyes underwent XEN stent insertion with the Semi-open technique by two surgeons between 1st July 2018 and 30th September 2019. All cases received subconjunctival injection of 0.1 mL of mitomycin C 0.2 mg/mL. Eyes with primary open angle glaucoma (OAG), secondary OAG or pseudophakic primary angle closure glaucoma (PACG) were included. Exclusion criteria were phakic PACG, uveitic or neovascular glaucoma and postoperative follow-up <12 months. Primary outcomes were defined by World Glaucoma Association guidelines. Secondary outcomes included change in glaucoma medications, needling rates and complications.
Results
We included 37 consecutive eyes of 35 patients with primary OAG (n = 30), secondary OAG (n = 6) and pseudophakic PACG (n = 1). Thirty-one eyes (84%) received a standalone XEN implantation and 6 (16%) underwent XEN implantation combined with phacoemulsification. The IOP reduced from 19.6 ± 6.0 mmHg preoperatively to 11.2 ± 2.6 mmHg at 12 months (P < 0.01). The number of glaucoma agents reduced from 3.49 ± 1.14 preoperatively to 1.57 ± 1.36 at 12 months. At 12 months, qualified success was 97.3% and complete success was 32%, with one case requiring trabeculectomy. Needling was required in 19% of cases over the 12 month follow up. Complications included 19 cases of transient hypotony and 7 cases of transient choroidal effusion. There were no cases of exposure, bleb leak or bleb-related infection.
Conclusion
Semi-open XEN technique achieves high surgical success rate in the medium-term with relatively low post-operative bleb needling rate.
Subject terms: Outcomes research, Surgery
Introduction
Lowering of intraocular pressure (IOP) is currently the most robust treatment option in altering the course of disease progression in eyes with glaucoma. For patients where IOP is not controlled sufficiently with medications or selective laser trabeculopasty, glaucoma filtration surgery is often required. While traditional surgical techniques such as trabeculectomy have good success rates, they are also at risk of well-documented potential complications such as postoperative hypotony, bleb leakage, blebitis and endophthalmitis [1]. The postoperative recovery course from these procedures is also often prolonged, in contrast to the Minimally Invasive Glaucoma Surgeries (MIGS) that have gained popularity recently. One such MIGS procedure is the XEN stent device. It is a 6 mm long collagen gel stent with a 45 µm lumen implanted through the anterior chamber into the irido-corneal angle to connect the anterior chamber with the subconjunctival space. The standard technique involves insertion of the XEN stent ab interno with an introducer without conjunctival dissection. While studies have shown that the XEN has acceptable levels of success compared with trabeculectomy [2–4], it is often associated with a high rate of postoperative needling rate in the range of 30–70% [5–7]. Cases that underwent needling often require further needling procedures and a substantial number eventually undergo additional glaucoma filtration surgery [3].
Recent studies have provided some insight into the possible reasons for the high needling rates associated with XEN. Anterior segment OCT analysis showed that eyes with outer segment of the XEN stent in deeper layers (the intra‐ and sub-tenon group) achieved better success and reduced needling rates compared to eyes where the outer segment is superficial [5]. Microfluidic assessment has showed that an ab externo technique that employs sub-tenon dissection resulted in lower outflow resistance than an ab interno technique that does not employ a dissection step [8]. These studies suggests that the variable result from XEN may be due to the unpredictable placement of the outer part of the XEN stent following ab interno insertion and a lack of blunt dissection to assist with bleb formation. One solution is performing an open incisional surgical technique involving limbal peritomy and insertion of XEN either through ab interno or ab externo route. However, limbal conjunctival incision carries with it small risk of anterior bleb leak, especially when combined with the application of Mitomycin C (MMC). To avoid this issue, we have developed the surgical technique of making a small posteriorly placed incision to access the sub-tenon space, followed by sub-tenon dissection and finally ab interno XEN insertion (the ‘Semi-open’ technique). Here we report on the 12-month surgical outcome of this technique.
Methods
We performed a retrospective analysis of surgical outcomes of consecutive XEN stent procedures performed by two glaucoma specialists (Kong, Ang) using Semi-open technique between 1st July 2018 and 30th September 2019. The key time points for analysis were preoperatively and postoperatively at 1 day, 1 week, 2 weeks, 4 weeks, 2-months, 3-months, 6-months, 9-months and 12 months. Data were collected via FRB!Glaucoma Save Sight Registries (http://savesightregistries.org/) with Institutional Ethics Committee approval obtained (RANZCO HREC Ref No: 16.09 (09/73)). This research conformed to the provisions of the Declaration of Helsinki.
Demographics, baseline ocular characteristics, surgical details, post-operative managements and complications were recorded. Patients with open angle glaucoma (OAG) and primary angle closure glaucoma (PACG) with pseudophakic status were included. Exclusion criteria included angle closure glaucoma and phakic lens status, the diagnosis of uveitic glaucoma, neovascular glaucoma, juvenile glaucoma, presence of vitreous in the anterior chamber, presence of intraocular silicone oil, and previous intraocular inflammation/infection. Surgical outcomes were recorded based on definitions set out in Guidelines from World Glaucoma Association [9]. Briefly, surgical success is IOP controlled between 6 and 21 mmHg or reduction of IOP greater than 20% of baseline. Complete success is defined as success being achieved without medications and qualified success is defined as achieving success with or without adjunct medications. Failure is defined as not meeting the above criteria, or any return to operating theatre for glaucoma reoperation, stent removal, loss of vision to no light perception (NPL) or hypotony (defined as IOP < 6 mmHg on two occasion after three months from the operation). Bleb needling at the slit lamp and return to theatre for anterior chamber reformation were not considered as failures. All postoperative details for an operation were recorded until the final follow-up visit or when a secondary glaucoma surgery was performed.
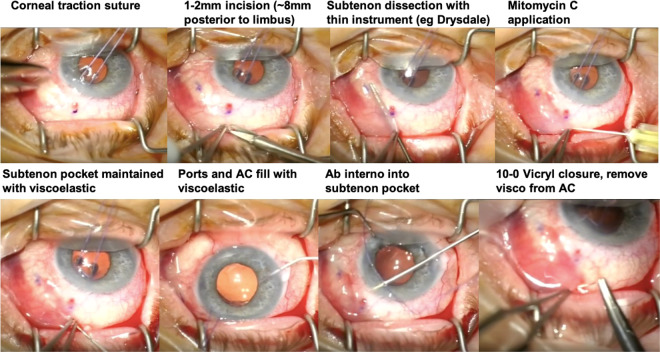
The Semi-open XEN stent implantation technique retains most of the essential steps described in the standard technique [6] and is illustrated in Fig. 1. The surgical steps are as follows: (1) placement of a corneal traction suture with 6–0 Vicryl (polyglactin) suture and pulling the eye inferotemporally; (2) marking 3 mm behind limbus in the superonasal quadrant; (3) making a 2 mm incision through the conjunctiva and tenons down to bare sclera, ~8 mm behind the limbus at one clock hour nasal to the 12 o’clock position; (4) performing a broad blunt dissection in the sub-tenon space using a long blunt instrument (such as an iris repositor or Drysdale paddle) in a sweeping motion; (5) subconjunctival injection of 0.1 mL of 0.2 mg/mL Mitomycin C; (6) injecting 0.1 mL of viscoelastic into the sub-tenon space to maintain this potential bleb-forming space; (7) relaxing the corneal traction suture and creating the corneal main and side ports and filling the anterior chamber with cohesive viscoelastic (Healon GV); (8) inserting the XEN stent ab interno as per standard technique, aiming for the trocar to exit into the viscoelastic filled sub-tenon pocket; (10) assessing subconjunctival outer XEN segment mobility and internal part of XEN with intraoperative gonioscopic lens as per standard technique; (11) closure of the posteriorly placed small conjunctival-tenon incision with a dissolvable 10–0 Vicryl suture; (12) removing viscoelastic from the anterior chamber; and (13) pressurising the anterior chamber to form a bleb. The need to perform a primary needling procedure is obviated.
Fig. 1. Surgical steps for the Semi-open XEN implantation technique.
Details of the technique is described in Methods section. In brief this involves placement of corneal traction suture and pulling eye inferior temporally (Top Row Panel 1). A small posterior incision down to bare sclera is made (Top Row Panel 2). Subtenon dissection is performed using blunt thin instrument through the small conjunctival/tenon incision (Top Row Panel 3). Mitomycin C is applied (Top Row Panel 4). Subtenon pocket is maintained using viscoelastic (Bottom Row Panel 1). Main wound and side port is made and anterior chamber (AC) is filled with viscoelastic (Bottom Row Panel 2). XEN45 stent is delivered ab interno into subtenon pocket (Bottom Row Panel 3). Conjunctival incision site is closed with a single 10-0 Vicyl suture and procedure is complete by removal of viscoelastic from AC (Bottom Row Panel 4).
In cases where cataract surgery was performed combined with XEN stent implantation, phacoemulsification was performed first before the placement of the XEN stent. No complications were encountered from the cataract surgery during the audit period, thus no cases were excluded as a result of cataract surgery complications.
Preoperatively there was no medication washout period. All cases had topical and systemic glaucoma medications ceased from the day of the operation, and commenced on topical chloramphenicol eye drop q.i.d, dexamethasone 1% q.2hrly and hydrocortisone 1% ointment nocte. Topical glaucoma medications were added to the treatment regimen based on clinical need. The topical steroid was weaned over a 4–9 months period. Postoperative sub-conjunctival injection of 5-Fluorouracil (5FU) was performed based on the assessment of bleb vascularity, while needling was performed based on clinical experience guided by published guidelines [10]. Needling procedures were performed at the slit-lamp with either a 30-gauge or 27-gauge needle after application of topical anaesthetic and topical ocular antiseptic solution. Subconjunctival injection of 5FU was performed at the end of the procedure. Any decision to perform additional glaucoma surgical procedures postoperatively when IOP was inadequately controlled was based on clinical judgement.
Data analysis was performed using SPSS for Windows, version 15.0.0 (SPSS Inc., Chicago, IL). Changes in intra-group outcomes were analysed using the paired t test or Wilcoxon Sign rank test. Univariate associations between two categorical variables were analysed using the Chi-Square test or Fisher’s exact test in cases of having any cell value less than 5 in cross tabulation. Kaplan–Meier survival analysis with Log-rank test was performed using SPSS with time to failure being the event. Alpha P value of <0.05 was considered statistically significant.
Results
A total of 37 cases were performed using the Semi-open technique. All patients completed 12 months of follow-up. Combined phacoemulsification was performed in 6 (16%) cases. Table 1 summarises the baseline demographics and ocular characteristics. In this case series, one case had previous cyclodiode laser, one case had previous failed trabeculectomy, and one case had previous Baerveldt tube.
Table 1.
Baseline demographic and ocular characteristics.
| Demographics and ocular characteristics | Semi-open (n = 37) |
|---|---|
| Median age at surgery (years ± SD) | 77.5 ± 10.6 |
| Female gender, n (%) | 20 (54%) |
| Ethnicity | |
| White, n (%) | 31 (84%) |
| Asian, n (%) | 6 (16%) |
| Type of glaucoma, n (%) | |
| Primary Open Angle | 30 (81%) |
| Secondary Open Angle | 6 (16%) |
| Primary Close Angle | 1 (3%) |
| Lens status, n (%) | |
| Phakic | 7 (19%) |
| Pseudophakic | 30 (81%) |
| Glaucoma Severity*, n (%) | |
| Severe | 18 (49%) |
| Moderate | 17 (46%) |
| Mild | 2 (5%) |
| Previous glaucoma procedure, n (%) | 3 (8.1%) |
| Mean preoperative IOP mmHg ± SD | 19.6 ± 6.0 |
| Preoperative number of glaucoma medications (topical and systemic ± SD) | 3.49 ± 1.15 |
| Preoperative BCVA, LogMAR ± SD | 0.41 ± 0.64 |
| Combined cataract XEN stent | 6 (16%) |
SD standard deviation, BCVA best corrected visual acuity.
*Glaucoma severity defined as Mild with Mean Deviation MD > −6 dB, Moderate −6 dB ≤ MD < −12 dB, Severe MD < −12 dB.
Intraocular pressure and surgical success
As shown in Table 2, IOP is reduced from 19.6 ± 6.0 mmHg pre-operatively to 7.2 ± 5.7 mmHg on day 1, 10.8 ± 4.0 mmHg at 1-month, 12.3 ± 3.8 mmHg at 3-months, 11.2 ± 2.9 mmHg at 6-months and 11.2 ± 2.6 mmHg at 12-months post op (P < 0.01 compared to baseline at all time points). The 12-months IOP represents a 42.9% reduction compared to preoperative IOP. The number of glaucoma agents reduced from average of 3.49 ± 1.14 agents pre-operatively to 1.41 ± 1.33 agents at 6-months and 1.57 ± 1.36 agents at 12-months (P < 0.001).
Table 2.
Intraocular pressure levels and number of glaucoma medications following XEN45 insertion.
| Time points | Intraocular pressure (n = 37) mmHg ± SD | Number of glaucoma agents (n = 37) Number ± SD |
|---|---|---|
| Preoperative | 19.6 ± 6.0 | 3.49 ± 1.14 |
| Day 1 | 7.2 ± 5.7 | 0 ± 0 |
| Week 1 | 8.6 ± 7.4 | 0 ± 0 |
| Week 2 | 10.8 ± 5.4 | 0.14 ± 0.59 |
| 1 Month | 10.8 ± 4.0 | 0.46 ± 0.87 |
| 2 Months | 11.1 ± 3.3 | 0.73 ± 0.96 |
| 3 Months | 12.3 ± 3.8 | 1.00 ± 1.20 |
| 4 Months | 11.8 ± 3.1 | 1.16 ± 1.34 |
| 6 Months | 11.2 ± 2.9 | 1.41 ± 1.33 |
| 9–10 Months | 12.1 ± 2.9 | 1.37 ± 1.01 |
| 11–12 Months | 11.2 ± 2.6 | 1.57 ± 1.36 |
SD Standard deviation.
At 12-months postoperatively, 36 cases achieved overall qualified success (97.3%) and 12 cases achieved complete success without topical medications (32%). One case (2.7%) required additional glaucoma surgery due to occlusion of the internal XEN lumen by peripheral iris that was not resolvable with Nd:YAG (Neodymium:Yttrium–Aluminium–Garnet) laser.
The number of combined cataract and XEN procedures was six cases (16%). The overall success rate was also not significantly different when performed as a stand-alone procedure (97%) or in combination with phacoemulsification (100%). While complete success is higher in stand-alone cases (39%) compared to combined cases (0%), this did not reach statistical significance (P = 0.15, Fisher’s exact test).
Needling rates and secondary outcomes
Postoperative needling was performed at the slit-lamp based on the clinical assessment of authors (Kong, Ang). Within the 12-month follow-up period, 7 cases required post-operative needling (19%), with most needling occurred between 2 to 4 months post-operation. Of the 7 cases requiring needling in the Semi-open group, 3 (43%) required additional needling.
There were no significant changes in visual acuity following operation, with BCVA being LogMar 0.41 ± 0.63 preoperatively and 0.39 ± 0.63 postoperatively at 12-months (P = 0.55).
Safety and complications
As shown in Table 3, there were no intraoperative complications in this case series. In the early postoperative period, the most common complication was transient numerical hypotony (IOP ≤ 5 mmHg) which occurred in 19 cases (51.4%), with transient choroidal effusion developing in 7 cases (18.9%). No cases required return to theatre for anterior chamber reformation and no cases of bleb leak. Early postoperative hyphaema occurred in three cases were also transient (7.1%).
Table 3.
Post operative complications following XEN 45 insertion.
| No. (%) | Semi-open (n = 37) |
|---|---|
| Intraoperative complications | |
| XEN complication | 0 (0%) |
| Cataract surgery complication | 0 (0%) |
| Post operative ≤3 months | |
| Transient hypotony ≤5 mmHg | 19 (51.4%) |
| Choroidal effusion | 7 (18.9%) |
| Shallow Anterior Chamber (AC) | 2 (5.4%) |
| Return to theatre for AC reformation | 0 (0%) |
| Hyphaema | 3 (7.1%) |
| Descemet’s membrane occlusion of XEN | 0 (0%) |
| Iris occlusion of XEN | 1 (2.7%) |
| Bleb leak | 0 (0%) |
| Post operative >3 months | |
| XEN exposure | 0 (0%) |
| Blebitis | 0 (0%) |
| Ptosis | 1 (2.7%) |
| Endophthalmitis | 0 (0%) |
There were no significant late complications in this series. There were no cases of XEN stent exposure, blebitis or endophthalmitis.
Discussion
The XEN stent was developed with the aim to achieve a standardised approach to lowering IOP by keeping the length and inner lumen of the device fixed, but studies have found that the surgical outcomes can be variable [3]. There is increasing evidence that the surgical outcomes are influenced by the position of the outer segment of the XEN stent, with deeper position of the XEN stent outer segment leading to decreased needling rates and better bleb function [5]. We found from experience in open revision of failed XEN procedures that the stents often fail due to the outer XEN segment being encased by a ‘sock’ of tenon tissue due to placement into tenon during the initial implantation. By removing the outer XEN segment from the ‘sock’ and placing it in the blunt dissected sub-tenon space, then resumption of function with formation of a diffuse slightly elevated filtration bleb can be seen. XEN stent implantation performed with the fornix-based open technique also produces a similar bleb appearance. This suggests that the variable behaviour of the XEN stent is likely attributed to the variable interaction between tenon and the XEN stent outer segment. The Semi-open technique therefore aims to produce a consistent sub-tenon placement of the XEN stent outer segment and avoid the risk of anterior conjunctival wound leak posed by the open technique.
Our success rate of 97.3% with the Semi-open XEN technique compares well with the APEX study which reported a clinical success rate of 67.6% at 12 months [6], and with other studies describing success rates ranging from 25% to 97.5% [2, 3, 6, 7, 11–16]. Some of these studies included secondary glaucomas such as neovascular glaucoma, juvenile glaucoma and uveitic glaucoma [3, 13, 15], which were specifically excluded from our series. Complete success (without glaucoma medications) at 12-months was 32%, this is lower than that reported in primary trabeculectomy (59%) in the Primary Tube-versus-Trabeculecotmy Study [17]. It is likely that the 45 micron diameter lumen in the XEN stent is a limiting factor in achieving sufficiently low IOP without assistance from topical glaucoma medications. It would be of interest to investigate whether 63 micron diameter lumen XEN would overcome this microfluidic limitation when it becomes available commercially in the future.
The published post-operative needling rate for XEN ranges between 30 and 70%, with most studies reporting between 40 and 50% rate of needling [3, 5–7]. Our needling rate of 19% for Semi-open group is among the lower range of reported values. This suggests that by blunt dissecting the subtenon plane and placing the XEN outer segment into this potential space, there is less requirement to perform needling postoperatively to free the XEN from surrounding tenon tissue. In fact, our needling rate compares favourably to the needling rate for trabeculectomy (17%) [18].
In our study, XEN implantation combined with cataract surgery showed no significant difference in qualified success in the Semi-open group. This is similar to findings from other studies which showed similar success rates between standalone XEN stent and phaco-XEN stent combination procedures [6, 12, 13].
In terms of post operative complications, the most common complication following Semi-open stent implantation was transient numerical hypotony which occurred in 51.4% of cases. The majority of these cases did not lead to clinically significant sequelae. Early transient numerical hypotony is a well-described phenomenon in XEN stent cases and is thought in part to be related to peri-tubular aqueous flow [10]. In high risk cases, prevention of early numerical hypotony can be achieved by leaving a small amount (~0.02 mL) of viscoelastic in the anterior chamber at the end of case.
Iris occlusion occurred in one case in this study series, which was managed initially with Nd:YAG laser clearance of iris near the internal opening of the XEN stent but eventually subsequently failed. It is possible that even after laser, a residual clump of iris tissue remained lodged within the lumen beyond the internal opening, thus occluding the lumen and preventing aqueous outflow through the stent. This complication can be reduced by avoiding implantation of the XEN stent with entry site too close to the iris root. There were no cases of bleb leak in this group of Semi-open XEN series, which compares well to the 11–14% wound leak rate reported in fornix-based trabeculectomy [17, 18]. Stent erosion is a significant complication in glaucoma device procedures because of high infection risk if not managed early. While the XEN stent was designed to be flexible and less likely to cause conjunctival erosion from upward force on the conjunctiva [19], this complication has been reported multiple times previously [6, 20–25]. XEN stent erosion in these cases is likely due to the outer segment of the XEN stent being located too superficially under conjunctiva which had been treated with MMC. In this case series we did not have any cases of XEN stent erosion. We believe that the Semi-open technique is able to provide better protection against stent erosion due to the combination of tenon and conjunctival tissue above the outer XEN segment.
One main limitation of this study is its retrospective nature. However, baseline demographics and baseline ocular characteristics are typical of patients requiring glaucoma filtration surgery in investigator surgeons’ practices, with significant proportion of eyes with moderate to severe glaucoma. Another limitation of case series is possible learning effect. However, in the chronologically earlier half of the cases (n = 18) there were three cases of needling (17%) while in the later half (n = 19) there were four cases of needling (21%) with no statistically significant difference (P = 1.00).
In conclusion, we demonstrate that the Semi-open technique for XEN stent implantation to be a safe procedure with good consistency in surgical outcomes, and relatively low needling rates at 1 year. Longer term follow-up will provide further information on the comparative outcome of this novel technique compared to standard close-conjunctival technique.
Summary
What was known before
XEN stent Minimally Invasive Glaucoma Surgery has been shown to have similar surgical success to trabeculectomy, however it is associated with higher post operative needling rates.
What this study adds
We developed a novel technique of XEN stent insertion to achieve consistent sub-tenon placement of XEN with minimal trauma to conjunctiva using a posterior small incision.
In this study we report the outcomes of 37 consecutive XEN45 cases using ‘Semi-open’ technique. We found at 12-month follow up the Semi-open group showed high overall success rate and lower needling rate (19%), with no risk of bleb leak.
Author contributions
Kong Yu Xiang George contributed by providing cases for the case series, data analysis and manuscript preparation. Ghee Soon Ang contributed by providing cases for case series and manuscript proof. Young Chung contributed to data entry and manuscript proof. FRB!Glaucoma Save Sight Registries (http://savesightregistries.org/) has provided support for data aggregation and summary analysis.
Competing interests
Kong Yu Xiang George receives continuing medical education funding from Allergan as part of the International Glaucoma Panel programme. Kong Yu Xiang George also act as a medical consultant for Allergan/Abbvie (China). Young Chung and Ghee Soon Ang have no conflicts of interest to disclose in relation to this study.
Footnotes
Précis The Semi-open sub-tenon XEN stent technique achieved high qualified surgical success rate, absence of bleb leak and low needling rates at 12 months.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gedde SJ, Schiffman JC, Feuer WJ, Herndon L, Brandt J, Budenz D, et al. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153:789–803.e2. doi: 10.1016/j.ajo.2011.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Gregorio A, Pedrotti E, Russo L, Morselli S. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. 2018;38:1129–34. doi: 10.1007/s10792-017-0571-x. [DOI] [PubMed] [Google Scholar]
- 3.Fea A, Durr G, Marolo P, Malinverni L, Economou M, Ahmed I. XEN gel stent: a comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020;14:1805–32. doi: 10.2147/OPTH.S178348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, et al. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124:1579–88. doi: 10.1016/j.ophtha.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Lenzhofer M, Strohmaier C, Hohensinn M, Hitzl W, Sperl P, Gerner M, et al. Longitudinal bleb morphology in anterior segment OCT after minimally invasive transscleral ab interno glaucoma gel microstent implantation. Acta Ophthalmol. 2019;97:e231–7. doi: 10.1111/aos.14111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reitsamer H, Sng C, Vera V, Lenzhofer M, Barton K, Stalmans I, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257:983–96. doi: 10.1007/s00417-019-04251-z. [DOI] [PubMed] [Google Scholar]
- 7.Theilig T, Rehak M, Busch C, Bormann C, Schargus M, Unterlauft J. Comparing the efficacy of trabeculectomy and XEN gel microstent implantation for the treatment of primary open-angle glaucoma: a retrospective monocentric comparative cohort study. Sci Rep. 2020;10:19337. doi: 10.1038/s41598-020-76551-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee RMH, Bouremel Y, Eames I, Brocchini S, Khaw PT. The implications of an ab interno versus ab externo surgical approach on outflow resistance of a subconjunctival drainage device for intraocular pressure control. Transl Vis Sci Technol. 2019;8:58. doi: 10.1167/tvst.8.3.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaarawy TM, Sherwood MB, Grehn F, ed. WGA guidelines on design and reporting of glaucoma surgical trials. Amsterdam: Kugler Publications; 2008.
- 10.Vera V, Ahmed IIK, Stalmans I, Reitsamer H. Gel stent implantation—recommendations for preoperative assessment, surgical technique, and postoperative management. US Ophthalmic Rev. 2018;11:38–46. doi: 10.17925/USOR.2018.11.1.38. [DOI] [Google Scholar]
- 11.Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, Gargallo-Benedicto A, Osorio-Alayo V, Barreiro-Rego A, et al. Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 2016;91:415–21. doi: 10.1016/j.oftal.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Heidinger A, Schwab C, Lindner E, Riedl R, Mossböck G. A Retrospective Study of 199 XEN45 Stent Implantations From 2014 to 2016. J Glaucoma. 2019;28:75–9. doi: 10.1097/IJG.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 13.Hengerer FH, Kohnen T, Mueller M, Conrad-Hengerer I. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017;26:1130–6. doi: 10.1097/IJG.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 14.Grover DS, Flynn WJ, Bashford KP, Lewis RA, Duh YJ, Nangia RS, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi: 10.1016/j.ajo.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 15.Tan SZ, Walkden A, Au L. One-year result of XEN45 implant for glaucoma: efficacy, safety, and postoperative management. Eye. 2018;32:324–32. doi: 10.1038/eye.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansouri K, Gillmann K, Rao HL, Guidotti J, Mermoud A. Prospective evaluation of XEN gel implant in eyes with pseudoexfoliative glaucoma. J Glaucoma. 2018;27:869–73. doi: 10.1097/IJG.0000000000001045. [DOI] [PubMed] [Google Scholar]
- 17.Gedde SJ, Feuer WJ, Lim KS, Barton K, Goyal S, Ahmed IIK, et al. Treatment outcomes in the primary tube versus trabeculectomy study after 3 years of follow-up. Ophthalmology. 2020;127:333–45. doi: 10.1016/j.ophtha.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ, et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology. 2013;120:2532–9. doi: 10.1016/j.ophtha.2013.07.049. [DOI] [PubMed] [Google Scholar]
- 19.Yu DY, Morgan WH, Sun X, Su EN, Cringle SJ, Yu PK, et al. The critical role of the conjunctiva in glaucoma filtration surgery. Prog Retin Eye Res. 2009;28:303–28. doi: 10.1016/j.preteyeres.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Sng CC, Wang J, Hau S, Htoon HM, Barton K. XEN-45 collagen implant for the treatment of uveitic glaucoma. Clin Exp Ophthalmol. 2017;46:339–34. doi: 10.1111/ceo.13087. [DOI] [PubMed] [Google Scholar]
- 21.Arnould L, Theillac V, Moran S. Recurrent exposure of XEN gel stent implant and conjunctival erosion. J Glaucoma. 2019;28:e37–40. doi: 10.1097/IJG.0000000000001146. [DOI] [PubMed] [Google Scholar]
- 22.Karimi A, Lindfield D, Turnbull A, Dimitriou C, Bhatia B, Radwan M, et al. A multi-centre interventional case series of 259 ab-interno XEN gel implants for glaucoma, with and without combined cataract surgery. Eye. 2019;33:469–77. doi: 10.1038/s41433-018-0243-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arnljots TS, Economou MA. XEN gel stent exposure 7mo after primary implantation: a case report. Int J Ophthalmol. 2019;12:689–91. doi: 10.18240/ijo.2019.04.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim R, Sethi M, Morley AMS. Ophthalmic manifestations of xeroderma pigmentosum: a perspective from the United Kingdom. Ophthalmology. 2017;124:1652–61. doi: 10.1016/j.ophtha.2017.04.031. [DOI] [PubMed] [Google Scholar]
- 25.Buffault J, Baudouin C, Labbé A. Is the XEN® Gel Stent really minimally invasive? Am J Ophthalmol Case Rep. 2020;19:100850. doi: 10.1016/j.ajoc.2020.100850. [DOI] [PMC free article] [PubMed] [Google Scholar]